Abstract
Nephrocalcinosis refers to calcium deposition in the form of calcium oxalate or calcium phosphate in the renal parenchyma and tubules. After diagnosis, the cause of nephrocalcinosis must be established to carry out a comprehensive approach to this entity. Although this is a common finding, it can be underdiagnosed due to the lack of knowledge of the different presentation patterns that exist. Many causes have been described related to this disease.A pictorial review about the most common features of cortical and medullary nephrocalcinosis both in ultrasound and CT is presented in the present work as well as a review of its main causes and graphics to easily recognize each pattern.
Introduction
Nephrocalcinosis is defined as the presence of calcium oxalate or calcium phosphate deposits in the kidney and is closely associated with increased levels and hypercalciuria secondary to extrarenal causes, including increased intestinal calcium absorption or reabsorption in the renal tubules. 1 This term was first used by Fuller Albright in 1934. 2 When it is visible radiologically, it is called macroscopic nephrocalcinosis, whose most frequent cause is hypercalciuria, within which there is a wide spectrum of diseases. 2 A study showed that the study by ultrasonography has greater sensitivity with respect to CT using a convex transducer of 1–6 MHz in patients with hypoparathyroidism in early diseases, also, the use of high-resolution linear transducers may be useful (2–10 MHz) for its correct visualization. 3
This disorder predisposes to the formation of nephrolithiasis, which can manifest simultaneously with this entity and should not be confused. It is considered a rare, infrequent condition whose exact pathogenesis is unknown up to now. 4 The widely known classification standardizes three forms of presentation, according to their severity: the molecular one that manifests itself in patients with hypercalcemia, due to an increase in intracellular calcium, being reversible when treating the underlying cause, the microscopic one that is diagnosed by identifying mineral deposits by direct microscopic view of renal tissue in a biopsy sample and is a precursor of the third condition that is the most frequently diagnosed and used clinically when calcification is identifiable imaging either by abdominal X-ray or ultrasonography, making its confirmation by CT. 5
The course of this disease is chronic, asymptomatic, generally diagnosed as an incidental finding on imaging studies, however, diagnostic images play an important role for identifying the disease in patients with predisposing factors, such as hyperparathyroidism, hyperthyroidism, among other metabolic disorders. Abdominal radiography is insensitive for diagnosis due to its poor delimitation of the renal anatomy, as well as the interposition of intestinal gas. Abdomen ultrasound is the preferred imaging technique for diagnosis because of its cost-effectiveness as it is relatively inexpensive, does not require radiation, and is portable. It can be demonstrated using a high resolution probe when it has not been demonstrated by a conventional linear probe but both techniques should always be used.In cases in which concomitant nephrolithiasis is suspected, performing CT without contrast is indicated in order to obtain a better anatomical definition, as well as being a diagnostic option in patients with abundant adipose panniculus, or with an ultrasound window that impedes the visualization of the anatomical structures and calcifications by the interposition of gas
Regarding its location, it occurs in 97% of cases in the renal medulla, while its cortical is much rarer, being 20 times less frequent. The presence of the two entities has been seen at the same time in pathologies such as oxalosis, chronic pyelonephritis and kidney infections in patients with human immunodeficiency virus (HIV) infection. 6
Cortical nephrocalcinosis
It is an infrequent presentation of renal calcification located in the cortex. It occurs to a lesser extent than medullary nephrocalcinosis, so its identification is less frequent. The most frequent causes for the development and presentation of this condition are chronic glomerulonephritis and acute cortical necrosis, which is a sign of secondary renal damage, hypovolemic shock, sepsis, renal infarction, drug poisoning, 7 however, there are various etiologies of this entity within which are the group of infectious diseases both in immunocompetent patients with chronic pyelonephritis and in immunosuppressed patients due to HIV infection where opportunistic microorganisms generate kidney infections that predispose to this disease. Other possible causes are some metabolic diseases or diseases with a genetic component.
The diagnosis is usually incidental and is identified by means of diagnostic images, giving rise to the term macroscopic nephrocalcinosis, which is the global definition used for this disease. Calcifications in the renal parenchyma can be identified by abdominal radiography if the thickness is >2 mm, although it is detected earlier on CT and ultrasonography. Ultrasound findings appear as linear or punctiform hyperechogenic calcifications in the renal cortex that can generate posterior acoustic shadow depending on the calcium concentration they contain. 6
Three associated patterns have been described without any being specific for a disease. The most frequent are linear calcifications of the renal cortex in the form of a band that extends to the septal cortex (Figure 1). Another described pattern occurs secondary to the calcification of necrotic glomeruli and tubules in the renal cortex that can be distinguished as irregularly distributed punctiform calcifications. Finally, a pattern formed by two lines of parallel calcifications, also known as the tram sign that can be interrupted and generally occurs in patients with renal cortical necrosis 8 (Figure 2).
Figure 1.
Axial Non-contrast CT section of the kidneys: linear or “band” cortical nephrocalcinosis pattern. Bilateral cortical linear hiperdensities.
Figure 2.
Illustration of cortical nephrocalcinosis patterns: a. Linear or Banded, b: Punctate, c: Banded: “tram sign”.
Medullar nephrocalcinosis
It refers to the deposition of calcium in the renal pyramids, usually in the renal papilla. It is the most frequent form of presentation of this entity, representing up to 97% of cases. 5 Multiple causes associated with this entity have been described. In 1986, Patriquin and Robitaille described four patterns of presentation of this type of calcification by ultrasound. The first consists of a hyperechogenic band towards the periphery of the pyramid that spares the central portion (Figure 3). The second is characterized by being more hyperechogenic in the periphery with respect to the first pattern and an increase in echogenicity in the center of the pyramid. The third form of presentation consists of an increase in the echogenicity of the pyramid globally (Figure 4). Finally, in the fourth pattern, a focus of hyperechogenicity is identified at the tip of the renal pyramid along the margins of the fornix, which predisposes to the formation of kidney stones and is also known as the Anderson-Carr-Randall progression pattern (Figures 5 and 6), generating precipitation of calcium deposits in this location, which causes erosion towards the calyces and finally the formation of calculi 9 (Figure 7).
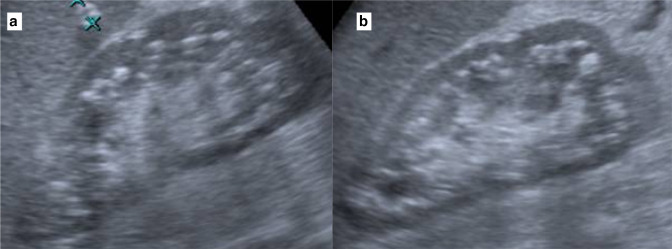
Figure 3.
(a) Axial non-contrast CT section of the right kidney and (b) axial non-contrast CT section of the left kidney: medullary nephrocalcinosis, with peripheral hyperechogenic band with central involvement pattern, the arrows indicate a peripheral calcification of the renal pyramid.
Figure 4.
Renal ultrasound: (a) sagittal slice and (b) coronal slice: Medullary nephrocalcinosis, showcasing a global increase in the echogenicity of the pyramid, the marked acoustic shadow can be distinguished.
Figure 5.
Renal ultrasound. (a) coronal slice and (b) sagittal slice: Medullary nephrocalcinosis. The arrows show global increase in echogenicity of the pyramid, without generating posterior acoustic shadow.
Figure 6.

Axial non-contrast CT section of the right kidney, Medullary nephrocalcinosis, Anderson-Carr-Randal pattern showing a linear echogenic focus at the tip of the renal pyramid along the margins of the fornix.
Figure 7.
Illustration patterns of medullary nephrocalcinosis presentation: (a) linear without compromising the papilla, (b) linear with more hyperechogenic in the middle of the renal pyramid, (c) global involvement of the pyramid, (d) Anderson-Carr-Randall pattern, calcification in the papilla and towards the fornixes.
On the other hand, presentation with diffuse increased echogenicity or hyperechogenic halos without posterior acoustic shadow surrounding the pyramids has been described before. In a more chronic course of this entity, calcifications of linear or punctiform morphology are identified in the medulla that can be accompanied by posterior acoustic shadow. 10 In diseases such as hyperparathyroidism or Type one renal tubular acidosis, a homogeneous calcium deposit with a bilateral and symmetrical presentation can be observed. While the asymmetric presentation is common in other entities such as renal medullary spongiosis (Figure 8 and Figure 9, Table 1).
Figure 8.
(a, b) Renal sagittal ultrasound slices showing mixed pattern of medullary nephrocalcinosis with involvement of the renal pyramids and fornix.
Figure 9.
Renal sagittal ultrasound slice showing medullary nephrocalcinosis, Anderson-Carr-Randall pattern: calcification towards the renal papilla is seen.
Table 1.
Radiological features of nephrocalcinosis
| Cortical nephrocalcinosis | Medullary nephrocalcinosis |
|---|---|
| Location: Located in the periphery and along the central septa of Bertin. Ultrasonography: Hyperechogenic images without acoustic shadowing, echogenic cortex. Patterns:
CT: High-attenuation of the cortex with calcifications |
Location: In the renal pyramids usually in the renal papilla. Ultrasonography: Bilateral stippled calcifications,pyramids are echogenic, with or without shadows. Patterns:
CT: High-attenuation calcifications in the medulla. |
Among the most frequent differential diagnoses is nephrolithiasis, which is the most common cause of renal calcification, characterized by the formation of hyperechogenic calculi of variable size that produce a posterior acoustic shadow on ultrasonography, usually manifesting with low back pain and an acute picture that differentiates it from nephrocalcinosis. Wall calcification of a simple cyst can resemble this entity, but it occurs in only 3% of cases. Some renal tumors, such as renal cell carcinoma, can produce calcifications and, in general, the presence of central calcifications in a renal mass is indicative of malignancy in more than 80% of cases. Subcapsular hematomas can become calcified and have a similar appearance to nephrocalcinosis. 11
Conclusion
The examples shown in this pictorial essay illustrate the different types of presentation of nephrocalcinosis, an entity that is diagnosed when it is identified through diagnostic imaging. It is a rare condition that encompasses a large number of etiological possibilities in both cortical and medullary presentation. The studies of choice are ultrasonography, which has a higher sensitivity for diagnosis, and CT, although in most cases this is an incidental finding that requires a study to establish the cause, so identifying it through images is of great importance.
Contributor Information
Juan Carlos Aldana, Email: bastidasnicolas6@gmail.com.
Laura C. Rodríguez, Email: nicolasbastidas64@gmail.com.
Nicolás Bastidas, Email: nicobasgu@hotmail.com.
Andrés Vásquez, Email: nicolasbagu@unisabana.edu.co.
REFERENCES
- 1. Oliveira B, Kleta R, Bockenhauer D, Walsh SB. Genetic, pathophysiological, and clinical aspects of nephrocalcinosis. American Journal of Physiology-Renal Physiology 2016; 311: F1243–52. doi: 10.1152/ajprenal.00211.2016 [DOI] [PubMed] [Google Scholar]
- 2. Vaidya SR, Yarrarapu SNS, Aeddula NR. Nephrocalcinosis. In: Statpearls [ Internet ] Treasure Island (Fl): Statpearls Publishing 2021. [Google Scholar]
- 3. Boyce AM, Shawker TH, Hill SC, Choyke PL, Hill MC, James R, et al. Ultrasound is superior to computed tomography for assessment of medullary nephrocalcinosis in hypoparathyroidism. J Clin Endocrinol Metab 2013; 98: 989–94. doi: 10.1210/jc.2012-2747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dickson FJ, Sayer JA. Nephrocalcinosis: A review of monogenic causes and insights they provide into this heterogeneous condition. IJMS 2020; 21: 369. doi: 10.3390/ijms21010369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Shavit L, Jaeger P, Unwin RJ. What is nephrocalcinosis? Kidney International 2015; 88: 35–43. doi: 10.1038/ki.2015.76 [DOI] [PubMed] [Google Scholar]
- 6. Ferreira A, Ferreira N, Leitão J, Santos J. Cortical Nephrocalcinosis asymmetrically involving the kidneys: A case report documenting the development via imaging. Port J NephrolHypert 2017; 31: 300–304. [Google Scholar]
- 7. Schepens D, Verswijvel G, Kuypers D, Vanrenterghem Y. Images in nephrology. Renal cortical nephrocalcinosis. Nephrol Dial Transplant 2000; 15: 1080–82. doi: 10.1093/ndt/15.7.1080 [DOI] [PubMed] [Google Scholar]
- 8. Pollack HM, Banner MP, Arger PH, Peters J, Mulhern CB Jr, Coleman BG. The accuracy of gray-scale renal ultrasonography in differentiating cystic neoplasms from benign cysts. Radiology 1982; 143: 741–45. doi: 10.1148/radiology.143.3.7079503 [DOI] [PubMed] [Google Scholar]
- 9. Daneman A, Navarro OM, Somers GR, Mohanta A, Jarrín JR, Traubici J. Renal pyramids: Focused sonography of normal and pathologic processes. RadioGraphics 2010; 30: 1287–1307. doi: 10.1148/rg.305095222 [DOI] [PubMed] [Google Scholar]
- 10. Martínez Huertas C, Gutiérrez Gallardo M, Jiménez Coronel V, Milena Muñoz A, Valero Rosa IC, Dávila Arias C. 2018. ECOGRAFÍA en El DIAGNóSTICO de la NEFROCALCINOSIS. seram. Available from: https://piper.espacio-seram.com/index.php/seram/article/view/705
- 11. Dyer RB, Chen MY, Zagoria RJ. Abnormal calcifications in the urinary tract. Radiographics 1998; 18: 1405–24. doi: 10.1148/radiographics.18.6.9821191 [DOI] [PubMed] [Google Scholar]