ABSTRACT
Singapore has one of the highest COVID-19 vaccination rates, however identifying vaccine-hesitant sub-groups and their concerns is vital given the need for future boosters in vulnerable populations. Furthermore, vaccine hesitancy remains a concern in the event of an emergence of a newer strain that necessitates the rolling out of a new vaccination programme. The aims of this study were to establish the extent of COVID-19 vaccine hesitancy and the factors influencing it among adults in Singapore using the Vaccine Hesitancy Scale (VHS). The study used a longitudinal methodology and participants were recruited in two waves from May 2020 to Sep 2022. In all 858 participants agreed to participate in both waves of the study. The two-factor structure of the VHS scale as established in earlier studies was tested using confirmatory factor analysis. The results revealed a two-factor structure of VHS comprising “lack of confidence” and “risks”. Those who had higher stress, resilience, and concerns that they might be infected with COVID-19 at wave 1 were significantly associated with lower ‘lack of confidence’ scores i.e. lower vaccine hesitancy. In comparison, those with higher concerns about inadequate government preventive measures and unemployment at wave 1 were significantly associated with higher ‘lack of confidence’ scores. Those with higher concerns about inadequate government preventive measures in wave 1 were significantly associated with higher ‘risks’ scores i.e. higher vaccine hesitancy. The findings point toward the need for a nuanced messaging that considers the fears expressed by the populace and addresses them directly using clear simple language.
KEYWORDS: Vaccine hesitancy, COVID-19, multi-ethnic, vaccine hesitancy scale, psychosocial factors
Introduction
Vaccine hesitancy has been defined as a “delay in acceptance or refusal of vaccination despite the availability of vaccination services.”1 Vaccine hesitancy has existed for many years, although evidence suggests that concerns have grown in recent years.2,3 Vaccine hesitancy is a major barrier to achieving herd immunity and increases the vulnerability and subsequent risk of severe outcomes in vulnerable populations to vaccine-preventable diseases such as flu, hepatitis B, and pneumococcal infections. The World Health Organization (WHO) identified vaccine hesitancy as one of the top 10 threats to global health in 2019, even before the era of the COVID-19 pandemic.4
As COVID-19 surged worldwide, in addition to protective measures such as physical distancing and quarantine, the development of vaccines occurred at an unprecedented pace, as it was acknowledged that they would be critical to control the pandemic.5 Several COVID-19 vaccines were developed within a year of the COVID-19 pandemic.6 However, vaccine hesitancy has remained a significant public health challenge, with a portion of the population remaining skeptical about vaccination’s safety and benefits7,8 and either refusing or delaying vaccination. In a survey investigating COVID-19 vaccine hesitancy globally in June 2021, individuals from 23 countries were surveyed.9 Slightly less than one-fourth (24.8%) of the 23,000 respondents reported vaccine hesitancy. The authors defined vaccine hesitancy as not having received even one dose of a COVID-19 vaccine and either “unsure/no opinion,” “somewhat disagree,” or “strongly disagree” with the question of whether they would take a COVID-19 vaccine when available to them. Of the countries surveyed, vaccine hesitancy was highest in Russia (48.4%), Nigeria (43%), and Poland (40.7%) and lowest in China (2.4%), the United Kingdom (U.K.) (18.8%), and Canada (20.8%).
Studies examining the correlates of vaccine hesitancy have largely found that younger people,10,11 women,10,11 people with low income,9,12 and people with lower levels of education13,14 were among those reluctant to be vaccinated. Interestingly, vaccine hesitancy was positively correlated with anxiety (in South Korea and the U.S.), whereas depression was correlated with vaccine hesitancy in South Africa.9 Similarly, a study in Japan showed that respondents with severe psychological distress were more likely to have vaccine hesitancy related to the COVID-19 vaccines.15 On the other hand, several studies have found that fear of COVID-19 infection and health consequences were associated with vaccine acceptance.16,17 Few studies have examined the role of resilience in vaccine hesitancy, and the literature shows mixed findings. Barbieri et al.18 found that vaccine hesitancy in a rural Italian population was predicted by high resilience, while in the urban population, resilience did not emerge as a significant predictor.19 Kilgore et al. similarly found that lower psychological resilience predicted vaccine acceptance in U.S. residents. In contrast, a study by Mo et al.20 among Chinese healthcare workers found that resilience was significantly associated with the intent to receive a COVID-19 vaccination. A study in Malaysia had similar findings, i.e., individual resilience was significantly associated with vaccine acceptance.21
Singapore launched one of the most successful vaccination programmes worldwide.22 The Singapore Government had allocated over SGD$1 billion (USD$750 million) for vaccine procurement,23 and Singapore was the first nation in Asia to receive the Pfizer-BioNTech COVID-19 vaccine. Vaccinations were free to all Singapore residents and the programme was progressively rolled out with priority given to frontline workers, older adults, and persons with chronic medical conditions. The two mRNA vaccines, Pfizer-BioNTech and Moderna, were made available widely through designated vaccination centers which were set up in the community as well as through general practitioners. Individuals could choose which of the two vaccines they preferred. The Sinovac vaccine was later made available at more than 20 private GP clinics to encourage vaccination among those desiring inactivated vaccines to mRNA vaccines. Vaccination was made available at home for persons who were unable to leave home (e.g., persons with disabilities, mobility difficulties, etc.) through Home Vaccination Teams.24 Data as of March 2023 shows that about 90% of Singapore’s population was fully vaccinated. These figures are lower than that from Macau, Brunei, United Arab Emirates, and Qatar where more than 99% of the population have been fully vaccinated. However, it is much higher than many other developed countries like the USA (68%), the U.K. (76%), Germany (76%), and Luxembourg (75%).25
Studies have found vaccine hesitancy despite the high vaccination rates in the Singapore population, especially in specific sub-populations: vaccine hesitancy was noticed among older adults, with about 25% of adults above the age of 60 remaining unvaccinated and not having booked appointments for vaccinations as of July 2021.26 A study by Griva et al.27 found that vaccine hesitancy was 9.9% at six months’ post-launch of the adult vaccination program. Vaccine hesitancy was higher among females, those aged 31 to 40 years, employed and earning an income between S$5,000 and S$12,999 with no chronic illnesses. In addition, subjects with vaccine hesitancy reported lower risk perception of COVID-19, were more distrustful and concerned about the vaccine, and perceived fewer benefits of the vaccine than those who were willing to be vaccinated. However, specific gaps remain in the understanding of vaccine hesitancy. First, few studies in Singapore employed a structured scale to measure vaccine hesitancy. Vaccine hesitancy was largely measured as those who had not received a vaccine to date and were unwilling/undecided to get vaccinated in the near future. Second, these were cross-sectional studies; hence, causal relationships could not be established.
The current study aims to address some of these gaps by following up on a longitudinal cohort established during the early phase of the COVID-19 pandemic and using a structured scale to examine vaccine hesitancy. This study is essential for several reasons. Firstly, in Singapore, the government has acknowledged that the endemic COVID-19 stage will not be static, and new infection waves should be expected occasionally. The Ministry of Health, Singapore encourages boosters one year after the last booster dose for persons aged 60 years and above, medically vulnerable persons, and residents of aged care facilities.28 Hence, vaccine hesitancy must be tackled even in the ‘endemic COVID-19’ stage. Identifying vaccine-hesitant sub-groups and their concerns is vital to ensure minimal morbidity and mortality. Secondly, in the event of an emergence of a newer strain that necessitates the rolling out of a new vaccination programme, there is a need for local data to augment the extant literature. Lastly, vaccine refusal is not vaccine hesitancy, so there is a need for a survey tool that can be used globally and would allow comparability across countries in future pandemics.
Specifically, the study aims to (1) establish the extent of COVID-19 vaccine hesitancy among adults in Singapore using the Vaccine Hesitancy Scale (VHS)29; (2) identify sociodemographic, clinical, and psychosocial factors associated with vaccine hesitancy toward COVID-19 vaccination.
Methodology
The study has been described in detail in an earlier article.30 Briefly, participants from a national psychiatric epidemiological study conducted in the general population of Singapore, the SMHS 2016,31 who had agreed to be re-contacted for future studies (n = 3370) were approached via phone and e-mail to seek their willingness to participate in the study. To be included in the survey, participants had to be (i) 18 years of age and above, (ii) Singapore residents, and (iii) able to speak in English, Chinese, or Malay. Exclusion criteria were (i) severe physical or mental disorders that limited participation in the study and (ii) not staying in Singapore during the survey period.
The study comprised two waves of interviews. The first wave was conducted from May 2020 to June 2021. 1129 participants agreed to participate in the study, giving a response rate of 54.8% (after excluding those whose contact details were invalid). Wave 1 of the study corresponded with the early phase of the pandemic in Singapore (circuit breaker lasting until June 2020, when people were asked to stay home and go out only if necessary, to June 2021, when Singapore remained in the heightened alert stage). During wave 1, vaccines were largely not available to the general public. These participants were followed up for the second wave of interviews between Oct 2021 and Sep 2022. In all, 858 participants agreed to participate in the second wave, giving a response rate of 76.0%. Wave 2 largely corresponded with the later mid-late stages of the pandemic (stabilization phase to transition phase) in Singapore, and vaccines were available to the public. The surveys were conducted by research staff with a degree/postgraduate qualification in psychology or social work. Two of the senior researchers M.S and Sa.S trained staff to administer consent and the survey. The survey was conducted as a structured interview, and minimal probes were used. All participants provided written informed consent using online software or in person (after lifting of physical-distancing restrictions). Interviews were conducted on the Zoom platform or in person, and data was captured using QuestionPro.
Questionnaires
Wave 1
General Anxiety Disorder −7 (GAD-7) was used to identify probable cases of anxiety.32 A cutoff score of ≥ 10 was used to determine caseness.
The Patient Health Questionnaire-9 (PHQ-9) was used to identify depression.33 A PHQ-9 sum score of ≥ 10 was used to define caseness.
The Depression Anxiety and Stress Scales (DASS) was used to capture stress.34 The Stress sub-scale assesses tension, agitation, and negative affect. A cutoff score of ≥ 15 was used to determine stress.
The 6-item Medical Outcomes Study Social Support Survey35 was used to measure social support. Mean scores across the six items were calculated, with higher scores indicating greater levels of social support.
The Brief Resilience Scale (BRS) was used to measure resilience. It is a 6-item instrument that assesses the ability of individuals to bounce back or recover from stress.36
We also examined sources of stress, including the risk of contracting COVID-19 by self or family, employability, and financial concerns. In addition, other COVID-19 related factors like exposure to COVID-19 cases in their neighborhood, and whether they had been placed under quarantine were assessed. Sociodemographic data was captured using a structured questionnaire.
Wave 2
The questionnaires used in Wave 1 were re-administered in Wave 2 with minor changes to accommodate newly implemented COVID-19 related regulation and policies.
Additional questionnaires included:
Vaccine Hesitancy Scale (VHS): The attitudes toward vaccination were measured using Thaker’s 14-item VHS,29 previously developed and validated elsewhere. The questions followed a prompt, “Regarding COVID-19 vaccines, how much do you agree or disagree with the following statements.” Eight items of the scale were from the previously validated 9-item VHS,37 and six new items were sourced from systematic reviews about vaccine hesitancy.38–40 All items were scored using a 5-point scale, from strongly disagree (1) to strongly agree (5), with neither agree nor disagree (3) as a mid-point. Total scores were generated by adding up the scores of the individual items. The seven items from the ‘lack of confidence’ domain were reverse coded so that higher scores indicate higher ‘lack of confidence’ and ‘risks’.41 No changes were made to the wording of the 14 items of the original scale. The scale was translated into Chinese and Malay using certified translators. Language experts in the team confirmed that the translations were appropriate. After the completion of the first five interviews in English, Malay and Chinese, participants were asked if they understood the questions and whether any words or phrases were difficult to understand. The participants did not identify any difficulties in understanding the scale.
Participants were asked about their current state of vaccination. They were also asked if they had made an appointment to get vaccinated. Receiving at least one vaccination dose or an appointment to receive the vaccine was taken as vaccine acceptance.
Statistical analyses
Descriptive statistics were calculated, including frequencies, percentages, means, and standard deviations of each item and the total scores across factors. The previous two-factor structure of the VHS scale29 was tested on the sample (n = 858) using confirmatory factor analysis (CFA). Polychoric correlations with robust weighted least squares (WLSMV) estimator were used. The model fit of the final model was assessed using the following indices: comparative fit index (CFI), root mean square error of approximation (RMSEA), standardized root mean square residual (SRMR), and Tucker – Lewis Index (TLI). CFI and TLI values ≥ 0.95 are considered to be a reasonably good fit, while RMSEA value ≤ 0.06 and SRMR value ≤ 0.08 are considered to be acceptable fit.42 Reliability in the context of the internal consistency of each subscale was evaluated using Cronbach’s alpha coefficient.
Subsequently, two multivariable linear regressions were conducted to explore the associations between sociodemographic factors and derived factors from the final model. A series of linear and multivariable linear regression analyses were also conducted to determine the relationship between the VHS scores and COVID-19 vaccine acceptance (collected in wave 2), as well as VHS scores collected in wave 2 and psychological distress (depression, anxiety and stress), resilience, social support, and COVID-19 related stressor scores determined in wave 1 and wave 2. A weighted analysis was used to ensure that the survey findings were representative of the Singapore adult population. All analyses were conducted using MPLUS and Stata 14.0. Statistical significance was set at 0.05 for all statistical tests.
Results
Table 1 presents the sociodemographic characteristics of the study participants. The participants’ mean (S.D.) age was 47.8 (15.9) years. The majority were ethnic Chinese (76.5%), married (63.3%), and employed (75.3%).
Table 1.
Sociodemographic characteristics of the sample (Wave 2; n = 858).
| N | Weighted % |
Singapore Census 2020 % |
||
|---|---|---|---|---|
| Age group (years) | 21–34 | 292 | 24.7 | 24.5 |
| 35–49 | 287 | 30.0 | 28.5 | |
| 50–64 | 171 | 27.2 | 27.8 | |
| 65+ | 88 | 18.1 | 19.2 | |
| Gender | Female | 393 | 48.9 | 51.7 |
| Male | 465 | 51.1 | 48.3 | |
| Ethnicity | Chinese | 322 | 76.5 | 76.1 |
| Malay | 197 | 11.5 | 12.4 | |
| Indian | 244 | 8.6 | 8.5 | |
| Others | 95 | 3.4 | 3.0 | |
| Marital | Never married | 264 | 26.8 | 26.9 |
| Married | 535 | 63.3 | 62.8 | |
| Divorced/Separated/Widowed | 59 | 9.9 | 10.3 | |
| Education | Primary and below | 31 | 11.8 | 16.3 |
| Secondary | 104 | 23.5 | 24.3 | |
| Post-Secondary | 293 | 25.8 | 27.1 | |
| Degree and above | 430 | 38.9 | 32.4 | |
| Employment | Employed | 696 | 75.3 | 63.8 |
| Economically inactive | 127 | 20.9 | 32.2 | |
| Unemployed | 35 | 3.8 | 4.0 | |
| Personal Income (SGD) | Below 2,000 or no income | 196 | 32.0 | - |
| 2,000 to 3,999 | 242 | 26.6 | - | |
| 4,000 to 5,999 | 194 | 18.8 | - | |
| 6,000 to 9,999 | 138 | 15.0 | - | |
| 10,000 and above | 78 | 7.6 | - |
Economically inactive – Students, homemakers and retirees.
SGD – Singapore dollar.
Factor validation
Factor loadings, intercorrelations between factors, goodness of fit indices, and Cronbach alpha of the VHS are presented in Supplementary Table S1. A two-factor model was tested and found to provide a good fit (CFI = 0.985, RMSEA = 0.051, SRMR = 0.040, and TLI = 0.982). The Cronbach’s α coefficient for the two factors were 0.93 and 0.79, respectively. The two factors were labeled as ‘lack of confidence’ and ‘risks’ in accordance with the factors identified by Thaker29 (Figure 1).
Figure 1.
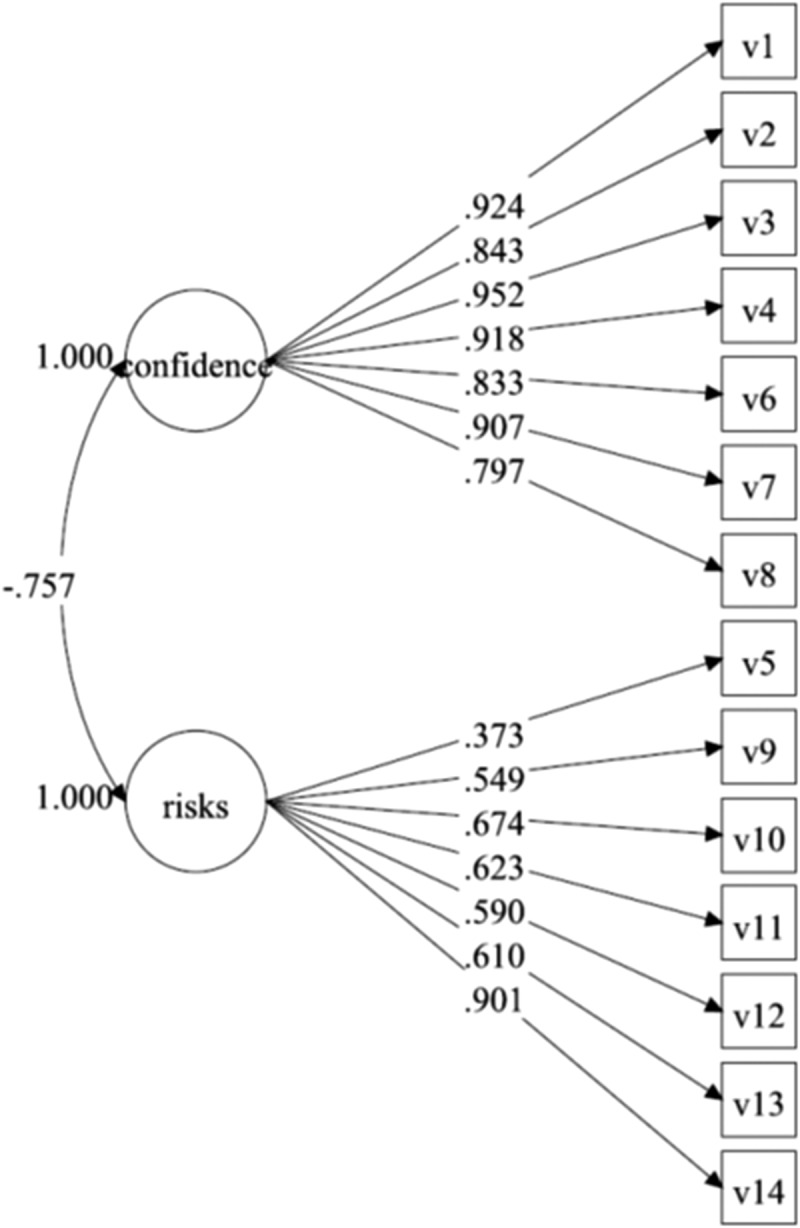
A two-factor structure of the VHS.
Item endorsement
Table 2 shows the endorsement of items on the ‘lack of confidence’ and ‘risks’ domains by the respondents. In terms of ‘lack of confidence’ the majority agreed (strongly agree/agree) that vaccines are – important for health (88.5%), effective (80.3%), and important for the health of others in the community (93.6%). Furthermore, the majority agreed that all vaccines offered by the government program in the community are beneficial (87.5%), information received about vaccines from the program is reliable (81%), getting vaccines is a good way to protect themselves from diseases (88.7%), and generally, they do what the doctor or healthcare provider recommends about vaccines (89.5%). In terms of ‘risks,’ only 7.6% stated that they agreed (strongly agree/agree) with the statement that vaccines cause diseases, 14.9% felt uncomfortable getting vaccinated, 43.4% were uncomfortable getting a vaccine that was rushed into production, and 25.8% stated that government over hypes the need for vaccines.
Table 2.
Percentage of extent of agreement with items of the ‘lack of confidence’ and ‘risks’ domains in the overall sample.
| Weighted % |
||||||
|---|---|---|---|---|---|---|
| Items | Strongly disagree | Disagree | Neither agree nor disagree |
Agree | Strongly agree | |
| 1. | Vaccines are important for my health. | 1.0 | 1.4 | 9.1 | 37.9 | 50.6 |
| 2. | Vaccines are effective | 1.3 | 3.6 | 14.8 | 50.3 | 30.0 |
| 3. | Vaccines are important for the health of others in my community | 0.8 | 1.0 | 4.6 | 44.1 | 49.5 |
| 4. | All vaccines offered by the government program in my community are beneficial | 1.1 | 2.2 | 9.2 | 46.3 | 41.2 |
| 5. | New vaccines carry more risks than older vaccines | 4.2 | 21.4 | 50.9 | 16.8 | 6.7 |
| 6. | The information I receive about vaccines from the program is reliable | 1.0 | 2.9 | 15.0 | 60.4 | 20.6 |
| 7. | Getting vaccines is a good way to protect myself from diseases | 1.6 | 1.1 | 8.6 | 47.7 | 41.0 |
| 8. | Generally I do what my doctor or healthcare provider recommends about vaccines | 1.4 | 1.8 | 7.3 | 54.0 | 35.5 |
| 9. | I am concerned about serious adverse effects about vaccines | 6.4 | 19.0 | 21.8 | 35.2 | 17.6 |
| 10. | Vaccines cause diseases | 21.3 | 40.7 | 30.4 | 6.7 | 0.9 |
| 11. | Government over hypes the need for vaccines | 12.5 | 41.7 | 19.9 | 20.0 | 5.8 |
| 12 | Corporations manufacturing vaccines only care for profit | 4.6 | 30.9 | 40.0 | 18.3 | 6.2 |
| 13. | I am uncomfortable getting a vaccine that was rushed into production | 5.7 | 26.0 | 25.0 | 31.9 | 11.5 |
| 14. | I feel uncomfortable getting vaccinated | 19.0 | 54.0 | 12.0 | 11.9 | 3.0 |
Sociodemographic correlates of lack of confidence and risks
Table 3 shows the correlates of the two vaccine hesitancy factor scores calculated by summing the items derived from the final CFA model. The scores ranged from 7 to 35. The mean and standard deviation of the ‘lack of confidence’ and ‘risks’ scores were 12.5 (4.6) and 19.6 (4.7), respectively.
Table 3.
Sociodemographic correlates of lack of confidence and risks.
| Lack of confidence |
Risks |
||||||
|---|---|---|---|---|---|---|---|
| b | 95% CI | P value | b | 95% CI | P value | ||
| Age | |||||||
| 21–34 | 1.0 | 1.0 | |||||
| 35–49 | 0.9 | (−0.4,2.3) | .180 | 1.6 | (0.4,2.8) | .008 | |
| 50–64 | 0.2 | (−1.3,1.8) | .785 | 0.7 | (−1,2.3) | .435 | |
| 65+ | 0.6 | (−1.1,2.4) | .474 | 1.3 | (−0.9,3.5) | .256 | |
| Gender | Female | 0.7 | (−0.2,1.6) | 0.133 | 0.4 | (−0.5,1.3) | .340 |
| Male | 1.0 | 1.0 | |||||
| Ethnicity | Chinese | 1.0 | 1.0 | ||||
| Malay | −1.1 | (−2,-0.2) | .015 | 0.6 | (−0.4,1.6) | .229 | |
| Indian | −0.5 | (−1.4,0.3) | .204 | 0.2 | (−0.8,1.1) | .750 | |
| Others | −2.2 | (−3.3,-1.0) | <.001 | −1.9 | (−3.5,-0.4) | .014 | |
| Marital | Married | 1.0 | 1.0 | ||||
| Never married | 0.9 | (−0.5,2.3) | .188 | 0.2 | (−1.1,1.4) | .781 | |
| Divorced/Separated/Widowed | 0.7 | (−1,2.4) | .417 | −0.2 | (−2,1.6) | .836 | |
| Education | Primary and below | −1.7 | (−3.7,0.4) | .112 | −1.1 | (−3.7,1.4) | .385 |
| Secondary | −0.3 | (−2,1.3) | .700 | −0.5 | (−2.2,1.3) | .615 | |
| Post-Secondary | 0.1 | (−1.1,1.3) | .904 | 0.5 | (−0.6,1.6) | .354 | |
| Degree and above | 1.0 | 1.0 | |||||
| Employment | Employed | 1.0 | 1.0 | ||||
| Unemployed | 1.2 | (−1.5,4.1) | .381 | −0.6 | (−4.0,2.7) | .727 | |
| Economically inactive | 1.4 | (0.002,2.9) | .050 | 0.7 | (−0.8,2.3) | .345 | |
| Personal income | Below 2,000 or no income | 0.3 | (−1.9,2.4) | .802 | 1.0 | (−1.5,3.5) | .441 |
| 2,000 to 3,999 | 1.7 | (0,3.5) | .056 | 1.5 | (−0.8,3.7) | .197 | |
| 4,000 to 5,999 | 1.3 | (−0.3,3) | .110 | 2 | (−0.1,4.1) | .062 | |
| 6,000 to 9,999 | 1 | (−0.7,2.7) | .253 | 1.5 | (−0.6,3.6) | .156 | |
| 10,000 and above | 1.0 | 1.0 | |||||
Economically inactive – Students, homemakers and retirees.
Multivariable linear regression analyses found that those of Malay and Others ethnicity (versus Chinese) were significantly associated with lower ‘lack of confidence’ scores while economically inactive i.e., the group comprising students, homemakers and retirees (versus employed) were significantly associated with higher ‘lack of confidence’ scores. We did not find any association of age, gender, marital status, education or personal income with ‘lack of confidence’ scores. Those aged 35 to 49 years (versus those aged 18–34 years) were significantly associated with higher ‘risks’ scores, while those of Others ethnicity were significantly associated with lower ‘risks’ scores. We did not find any association of gender, marital status, education, employment status or personal income with ‘lack of confidence’ scores.
Relationship between psychological distress factors, social support, resilience, COVID-19 stressors, vaccine acceptance, and ‘lack of confidence’ and ‘risks’ scores
In wave 2, we found that vaccine acceptance, resilience scores, and COVID-19 stressors were significantly associated with VHS’s ‘lack of confidence’ and ‘risks’ subscale scores (Table 4). After adjusting for ethnicity and employment in multivariable linear regression analyses, those who had higher vaccine acceptance, resilience scores, and concerns that family members might die due to COVID-19 were significantly associated with lower ‘lack of confidence’ scores. At the same time, those with higher concerns related to unemployment were significantly associated with higher ‘lack of confidence’ scores. Those with higher vaccine acceptance and resilience scores were significantly associated with lower ‘risks’ scores, while those with higher concerns related to unemployment and they might be infected with COVID-19 were significantly associated with higher ‘risks’ scores.
Table 4.
Relationship between psychological distress factors, resilience, COVID-19 stressors and lack of confidence and risks of VHS scores.
| Lack of confidencea |
Risksb |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Wave 2 |
Wave 1 |
Wave 2 |
Wave 1 |
|||||||||
| Predictors | Coef. | 95% CI | P | Coef. | 95% CI | P | Coef. | 95% CI | P | Coef. | 95% CI | P |
| Psychological distress | ||||||||||||
| Depression | −0.2 | (−2.3,2) | .877 | 0.6 | (−1,2.1) | .456 | −0.1 | (−2.1,1.9) | .91 | 0.6 | (−1,2.1) | .495 |
| Anxiety | 0.2 | (−1.7,2.2) | .808 | −0.3 | (−2,1.3) | .702 | 0.5 | (−1.5,2.6) | .599 | 0.03 | (−1.6,1.7) | .974 |
| Stress | −0.5 | (−2.2,1.3) | .593 | −1.7 | (−3.2,-0.2) | .025 | −2.1 | (−4.3,0.1) | .062 | −1.5 | (−3.2,0.3) | .103 |
| Resilience | −1.4 | (−2.1,-0.6) | <.001 | −1.2 | (−2.1,-0.3) | .012 | −1.4 | (−2.3,-0.6) | .001 | −0.7 | (−1.6,0.2) | .110 |
| Social support | −0.04 | (−0.5,0.4) | .856 | −0.4 | (−1,0.1) | .127 | 0.03 | (−0.5,0.5) | .899 | −0.4 | (−0.9,0.1) | .121 |
| Vaccine acceptance# | −16.8 | (−22.8,-10.7) | <.001 | - | - | - | −7.5 | (−10,-5) | <.001 | - | - | - |
| Any chronic condition | 0.4 | (−0.6,1.4) | .455 | −0.6 | (−1.5,0.2) | .119 | 0.7 | (−0.4,1.8) | .22 | −0.3 | (−1.1,0.5) | .433 |
| COVID-19 infection** | - | - | - | −0.6 | (−2,0.8) | .401 | - | - | - | −1.2 | (−2.7,0.3) | .124 |
| Quarantined** | - | - | - | −0.9 | (−2.5,0.6) | .242 | - | - | - | −0.5 | (−2.5,1.6) | .663 |
| COVID-19 Stressors | ||||||||||||
| 1. I might be infected with COVID-19 |
0.4 | (−0.5,1.2) | .369 | −1 | (−1.9,-0.05) | .038 | 1.1 | (0.1,2.1) | .024 | 0.04 | (−1,1.1) | .931 |
| 2. Family members or friends might be infected with COVID-19* |
- | - | - | −0.2 | (−1.3,0.8) | .667 | - | - | - | 0.4 | (−0.6,1.5) | .446 |
| 3. I might die due to COVID-19 |
0.5 | (−0.6,1.7) | .373 | 0.2 | (−1.1,1.6) | .709 | 0.2 | (−1.1,1.5) | .749 | −0.1 | (−1.4,1.2) | .876 |
| 4. Family members or friends might die due to COVID- 19 |
−1 | (−1.9,-0.1) | .024 | 0.4 | (−0.7,1.5) | .476 | −0.4 | (−1.5,0.7) | .432 | 0.9 | (−0.2,2.1) | .114 |
| 5. Overseas travel restrictions# |
−0.1 | (−1,0.8) | .851 | - | - | - | −0.3 | (−1.3,0.7) | .562 | - | - | - |
| 6. Working from home# | −0.8 | (−1.8,0.3) | .163 | - | - | - | −0.2 | (−1.4,1.1) | .812 | - | - | - |
| 7. Restriction on social gathering# |
−0.2 | (−1.1,0.7) | .659 | - | - | - | 0.1 | (−0.9,1.1) | .795 | - | - | - |
| 8. Unemployment | 1.3 | (0.4,2.3) | .005 | 1.4 | (0.4,2.4) | .004 | 1.8 | (0.7,2.8) | .001 | 0.7 | (−0.2,1.7) | .122 |
| 9. Financial loss, such as losing work opportunities or having to take unpaid leave* |
- | - | - | - | - | - | - | - | - | - | - | - |
| 10. School closure | −0.3 | (−1.5,0.8) | .578 | 0.1 | (−0.8,1) | .845 | −0.6 | (−1.8,0.6) | .334 | 0.5 | (−0.4,1.4) | .258 |
| 11. Inadequate preventive measures from government** |
- | - | - | 1.4 | (0.1,2.6) | .035 | - | - | - | 2.1 | (0.9,3.3) | .001 |
| 12. Inadequate stock of face mask** |
- | - | - | −1.1 | (−2.4,0.2) | .111 | - | - | - | 0.4 | (−0.9,1.7) | .527 |
| 13. Inadequate stock of food* ** |
- | - | - | - | - | - | - | - | - | - | - | - |
| 14. Inadequate daily necessities such as toilet papers** |
- | - | - | 0.5 | (−1,2) | .529 | - | - | - | −0.3 | (−2,1.4) | .745 |
aRegression coefficient was estimated using multivariable linear regression with adjustment for ethnicity and unemployment.
bRegression coefficient was estimated using multivariable linear regression with adjustment for age and ethnicity.
*Predictors were excluded in the regression analyses due to moderate multicollinearity (VIF = 2.04–2.12) with other covariates
#Not measured in wave 1; ** Not measured in wave 2.
Using data from wave 1, we found that those who had higher stress, resilience, and concerns that they might be infected with COVID-19 were significantly associated with lower ‘lack of confidence’ scores. In comparison, those with higher concerns about inadequate government preventive measures and unemployment were significantly associated with higher ‘lack of confidence’ scores. Those with higher concerns about inadequate government preventive measures were significantly associated with higher ‘risks’ scores (Table 4).
Discussion
Our study validated the VHS scale in the multi-ethnic population of Singapore. Both the original factor structure, high inter-correlation of the items, and its association with vaccine acceptance suggests that the scale would be of value as a generalized VHS in Singapore, which is similar to the results of the original scale development and validation exercise in New Zealand.29
This study has further provided a deeper understanding of the dimensions associated with vaccine hesitancy in this population. The ‘lack of confidence’ dimension was not a significant concern regarding COVID-19 vaccines in Singapore, as the two items ranked lowest in confidence still saw 80% of the population in agreement that the vaccine was effective and 81% of the population in agreement that the information they received about the vaccine was reliable. However, regarding risks, 52.8% of the sample agreed that they were worried about the vaccine’s side effects, and 43.4% agreed that they felt uncomfortable getting a vaccine that was rushed into production. Thus, ‘risks,’ i.e., concerns regarding the side effects and the rapid development of vaccines, were the main drivers of vaccine hesitancy, and these two factors have been similarly identified in several other studies.43–45 A qualitative study by Brown et al.46 revealed that the participants found it difficult to understand the rapid development of COVID-19 vaccine especially compared to older vaccines. This difficulty led to safety concerns such as whether they were tested well enough within this short period and if there were adverse side effects yet to be discovered. A study from Israel found that both healthcare workers and the general population were fearful of the vaccine’s safety profile, given its rapid development. Their safety concerns included quality control in the production of the vaccine, and the potential side effects of the vaccine.47 Rief48 suggests that it is important to acknowledge that vaccine side effects can happen, provide constructive information and ensure easy access to medical services to address such concerns. Furthermore, he suggested the need to balance the risk and benefit information and provide such information in a language that is easily understood by people. Thus, there is a need for rapid research using validated scales to understand the reasons for vaccine hesitancy and counter the misinformation regarding vaccines and provide evidence-based data to help people make informed choices, especially during epidemics and pandemics.
Unlike several other studies,10,11 our study failed to find any association between vaccine hesitancy and the younger age group or gender. Surprisingly, those aged 35 to 49 years (versus those aged 18–34 years) were significantly associated with higher ‘risks’ scores. Those in this age group were more likely to have young children, and studies have found that parents were more worried about the risks associated with vaccinating children.49,50 However, we did not capture any family composition data and hence were unable to analyze it further.
The study found an association between vaccine hesitancy and ethnicity with those of Malay and Others ethnicity (versus Chinese) significantly associated with lower ‘lack of confidence’ scores. A survey from the U.K., found that of the 12,035 participants who completed the survey, the highest vaccine hesitancy was seen among Black (71.8%), followed by Pakistani/Bangladeshi (42.4%) and Mixed (32.4%) ethnicity people.10 Lack of trust due to systemic discrimination,51,52 under-representation of minorities in health research and vaccine trials,53 and access to vaccinations have all been suggested to play a role. On the other hand, the Muslim religious groups in Singapore were proactive in supporting the importance of vaccination. In Dec 2020, the Muslim religious authority in Singapore issued a fatwa (Islamic religious ruling, regarding the issue of concern) saying that it is permissible to take the vaccine due to it being a basic necessity, and its safety and efficacy would have been ensured before being approved for public use. The Muslim community was encouraged to take the vaccine when it became available.54 The Government also ensured that the vaccination centers were located strategically near community centers, in primary care centers as well as in areas more likely to be frequented by the Malay community. These efforts highlight effective ways to engage minority groups and ensure that barriers to access are minimized, which in turn increases vaccine acceptance.
Data from both waves found that higher resilience was significantly associated with lower ‘lack of confidence’ and ‘risks’ scores, i.e., lower vaccine hesitancy. Research suggests that resilience encompasses positive adaptation to adversities.55 Using a stressful task involving risky investment decisions, Xing and Sun56 demonstrated that resilient individuals chose investment options associated with higher returns and experienced more positive affect. Thus, resilient people would be more likely to take the vaccine as a positive adaptation to counter the adverse consequences of a COVID-19 infection despite some of the potential risks of the vaccine. Additionally, those in wave 1 with higher stress and concerns of being infected by COVID-19 were significantly associated with lower vaccine hesitancy (‘lack of confidence’ scores). This finding is in line with previous literature.57–59 Vaccination reduces negative disease outcomes, so people who experience greater fears of becoming infected and having adverse complications following the infection may be more willing to receive it. Surprisingly, those with higher concerns related to unemployment in both the waves had higher ‘lack of confidence’ and ‘risks’ scores, i.e., higher vaccine hesitancy. Our finding is similar to that observed by Bendau et al.57 Their study found that economic fears (fear of the economic consequences of the pandemic) were significantly negatively correlated with vaccine acceptance. It is possible that those fearing unemployment may also have lower trust in the government’s ability to implement successful preventive measures (a concern that was associated with higher ‘lack of confidence’ and ‘risks’ scores in the current study). Thus, they may be skeptical about the vaccines, which were seen mainly as an initiative being led or supported by the government. The hesitancy may represent an overall distrust toward the preventive measures. It is also possible that those fearing unemployment may have been afraid of losing their jobs due to the vaccine’s side effects. They may have felt that while the infection was not within their control, getting vaccinated was a choice they could decline.
The main limitations of our study include the response rate of 54.8% in the first wave and the fact that the sample comprised a majority of younger people. While the response rate of 54.8% is satisfactory given the pandemic, older adults were reluctant to participate in the study as many were uncomfortable managing the Zoom platform and signing the consent form online. While we tried to approach them face-to-face once the restrictions were eased, many expressed fears of contracting the disease. Thus, the sample is limited in terms of its representativeness. About 25% of the population that participated in wave 1 refused to do so in wave 2. This is a substantial portion of the original sample and it is possible that our results would have been different in the absence of this attrition. Respondents may have been hesitant to express their views openly concerning vaccine hesitancy as the surveys were not conducted in an anonymized manner, i.e., the respondents were potentially identifiable. While not compulsory, vaccination was strongly encouraged in Singapore, which may have made it difficult for respondents to voice hesitation. Lastly, the study did not consider the the impact of vaccine hesitancy on the vaccinated population’s mental health,60 which is an important area of future research. The study’s strengths include the longitudinal study design, the high response rate in wave 2, the use of a structured scale to assess vaccine hesitancy and the administration of the survey in multiple languages, ensuring inclusivity.
In conclusion, our study validated the VHS in a multi-ethnic Asian country and identified the factors associated with vaccine hesitancy. Overall, vaccine hesitancy was low in Singapore, although some fears related to the rapid development of the vaccine were expressed. The pandemic has highlighted the importance of clear communication by government officials, public health and infectious disease experts who are trusted by the public. It is important that domain experts, communicate clearly in the face of an evolving pandemic and do not frequently change the message.61 To avoid misinformation, experts must communicate a more nuanced message to ensure that the complexity of an issue is understood and not rely on overtly simplistic messaging.
Furthermore, identifying resilience and the different roles of pandemic-related stressors as contributory factors is a significant contribution of this research, which has public health implications. Countries must consider initiatives to build resilience and mitigate stressors at the community and national level as an essential component of pandemic preparedness. This includes putting systems and strategies in place to face the next pandemic better, such as rapid deployment of widespread testing and contact tracing, creation of isolation centers, ensuring the availability of hospitals with sufficient intensive care beds, specialized healthcare workers, ventilators and antiviral therapies.61 The public must also be made aware of their roles and responsibilities including complying with the rules and regulations set forth by governments to control the spread of the pandemic, taking up vaccinations, and ensuring that misinformation is not spread but immediately debunked.61 Personal resilience can be strengthened by several psychological interventions, which must be evaluated, preferably using randomized-controlled trials as a part of emergency preparedness. Furthermore, extending the research to include rapid qualitative research62 would provide deeper insights into vaccine hesitancy and the development of culturally sensitive interventions for the multi-ethnic population.
Supplementary Material
Funding Statement
The funding for the study was made available by Temasek Foundation, Singapore, National Centre of Infectious Diseases and the Ministry of Health, Singapore.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Data availability statement
The data is available from the first author on request.
Ethics statement
Ethical approval for the study was provided by the National Healthcare Group Domain Specific Review Board.
IRB protocol number: 2020/00462 and 2021/00566
All participants signed a written informed consent.
Supplementary material
Supplemental data for this article can be accessed on the publisher’s website at https://doi.org/10.1080/21645515.2023.2235964.
References
- 1.MacDonald NE, SAGE Working Group on Vaccine Hesitancy . Vaccine hesitancy: definition, scope and determinants. Vaccine. 2015;33(34):4161–10. doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]
- 2.Cooper S, Betsch C, Sambala EZ, Mchiza N, Wiysonge CS.. Vaccine hesitancy – a potential threat to the achievements of vaccination programmes in Africa. Hum Vaccin Immunother. 2018;14(10):2355–7. doi: 10.1080/21645515.2018.1460987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sato APS. What is the importance of vaccine hesitancy in the drop of vaccination coverage in Brazil? Rev Saude Publica. 2018;52:96. doi: 10.11606/S1518-8787.2018052001199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization (WHO) . Ten threats to global health in 2019. [accessed 2023 Mar 4]. https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019.
- 5.Ball P. The lightning-fast quest for COVID vaccines - and what it means for other diseases. Nature. 2021;589(7840):16–18. doi: 10.1038/d41586-020-03626-1. [DOI] [PubMed] [Google Scholar]
- 6.Li M, Wang H, Tian L, Pang Z, Yang Q, Huang T, Fan J, Song L, Tong Y, Fan H. COVID-19 vaccine development: milestones, lessons and prospects. Signal Transduct Target Ther. 2022;7(1):146. doi: 10.1038/s41392-022-00996-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.De Figueiredo A, Simas C, Karafillakis E, Paterson P, Larson HJ. Mapping global trends in vaccine confidence and investigating barriers to vaccine uptake: a large-scale retrospective temporal modelling study. Lancet. 2020;396(10255):898–908. doi: 10.1016/S0140-6736(20)31558-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fadda M, Albanese E, Suggs LS. When a COVID-19 vaccine is ready, will we all be ready for it? Int J Public Health. 2020;65(6):711–2. doi: 10.1007/s00038-020-01404-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazarus JV, Wyka K, White TM, Picchio CA, Rabin K, Ratzan SC, Leigh JP, Hu J, El-Mohandes A. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat Commun. 2022;13(1):3801. doi: 10.1038/s41467-022-31441-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Robertson E, Reeve KS, Niedzwiedz CL, Moore J, Blake M, Green M, Katikireddi SV, Benzeval MJ. Predictors of COVID-19 vaccine hesitancy in the U.K. household longitudinal study. Brain Behav Immun. 2021;94:41–50. doi: 10.1016/j.bbi.2021.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Killgore WDS, Cloonan SA, Taylor EC, Dailey NS. The COVID-19 vaccine is here—now who is willing to get it? Vaccines (Basel). 2021;9(4):339. doi: 10.3390/vaccines9040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kadoya Y, Watanapongvanich S, Yuktadatta P, Putthinun P, Lartey ST, Khan MSR. Willing or hesitant? A socioeconomic study on the potential acceptance of COVID-19 vaccine in Japan. Int J Environ Res Public Health. 2021;18(9):4864. doi: 10.3390/ijerph18094864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ogilvie GS, Gordon S, Smith LW, Albert A, Racey CS, Booth A, Gottschlich A, Goldfarb D, Murray MCM, Galea LAM, et al. Intention to receive a COVID-19 vaccine: results from a population-based survey in Canada. BMC Public Health. 2021;21(1):1017. doi: 10.1186/s12889-021-11098-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Edwards B, Biddle N, Gray M, Sollis K, Di Gennaro F. COVID-19 vaccine hesitancy and resistance: correlates in a nationally representative longitudinal survey of the Australian population. PLoS One. 2021;16(3):e0248892. doi: 10.1371/journal.pone.0248892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okubo R, Yoshioka T, Ohfuji S, Matsuo T, Tabuchi T. COVID-19 vaccine hesitancy and its associated factors in Japan. Vaccines. 2021;9(6):662. doi: 10.3390/vaccines9060662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Willis DE, Andersen JA, Bryant-Moore K, Selig JP, Long CR, Felix HC, Curran GM, McElfish PA. COVID-19 vaccine hesitancy: race/ethnicity, trust, and fear. Clin Transl Sci. 2021;14(6):2200–7. doi: 10.1111/cts.13077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McElfish PA, Willis DE, Shah SK, Bryant-Moore K, Rojo MO, Selig JP. Sociodemographic determinants of COVID-19 vaccine hesitancy, fear of infection, and protection self-efficacy. J Prim Care Community Health. 2021;12:21501327211040746. doi: 10.1177/21501327211040746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Barbieri V, Wiedermann CJ, Lombardo S, Plagg B, Gärtner T, Ausserhofer D, Wiedermann W, Engl A, Piccoliori G. Rural-urban disparities in vaccine hesitancy among adults in South Tyrol, Italy. Vaccines. 2022;10(11):1870. doi: 10.3390/vaccines10111870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Killgore WDS, Cloonan SA, Taylor EC, Dailey NS. The COVID-19 vaccine is here-now who is willing to get it? Vaccines (Basel). 2021 Apr 1;9(4):339. doi: 10.3390/vaccines9040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mo PKH, She R, Yu Y, Li L, Yang Q, Lin J, Ye X, Wu S, Yang Z, Guan S, et al. Resilience and intention of healthcare workers in China to receive a COVID-19 vaccination: the mediating role of life satisfaction and stigma. J Adv Nurs. 2022. Aug;78(8):2327–233. doi: 10.1111/jan.15143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rosli N, Johar ER, Rosli N, Abdul Hamid NF. Psychological impact of COVID-19: assessing the COVID-19-related anxiety, individual’s resilience and conspiracy beliefs on attitudes to COVID-19 vaccination. Front Psychol. 2022 Aug 11;13:906914. doi: 10.3389/fpsyg.2022.906914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ritchie H, Edouard M, Rodés-Guirao L, Appel C, Giattino C, Ortiz-Ospina E, Hasell J, Macdonald B, Beltekian D, Roser M. Coronavirus pandemic (COVID-19). OurworldInData.org; 2020. https://ourworldindata.org/coronavirus.
- 23.A.P. News [Internet] . Singapore approves use of Pfizer’s COVID-19 vaccine. 2020 Dec 14 [accessed 2023 Jun 6]. https://apnews.com/article/science-singapore-coronavirus-pandemic-lee-hsien-loong-coronavirus-vaccine-5bf8461b9d2d32ec08d56fcf5958317a.
- 24.Ministry of Health Singapore . Covid-19 vaccination. [accessed 2023 June 6]. https://www.moh.gov.sg/covid-19/vaccination.
- 25.Josh Holder . Tracking coronavirus vaccinations around the world. The New York Times; 2023 Mar 13. https://www.nytimes.com/interactive/2021/world/covid-vaccinations-tracker.html.
- 26.Kurohi R. Ministers urge more seniors to get vaccinated against COVID-19 ahead of Singapore’s further reopening. The Straits Times; 2021. [accessed 2023 Mar 5]. https://www.straitstimes.com/singapore/ministers-urge-more-seniors-to-get-vaccinated-ahead-of-further-reopening.
- 27.Griva K, Tan KYK, Chan FHF, Periakaruppan R, Ong BWL, Soh ASE, Chen MI. Evaluating rates and determinants of COVID-19 vaccine hesitancy for adults and children in the Singapore population: strengthening our community’s resilience against threats from emerging infections (SOCRATEs) cohort. Vaccines (Basel). 2021;9(12):1415. doi: 10.3390/vaccines9121415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ministry of Health , Singapore. Singapore to exit acute phase of the pandemic. 2023. Feb 9 [accessed 2023 June 3]. https://www.moh.gov.sg/news-highlights/details/singapore-to-exit-acute-phase-of-pandemic.
- 29.Thaker J. The persistence of vaccine hesitancy: COVID-19 vaccination intention in New Zealand. J Health Commun. 2021;6(2):104–11. doi: 10.1080/10810730.2021.1899346. [DOI] [PubMed] [Google Scholar]
- 30.Subramaniam M, Abdin E, Shafie S, Wang P, Shahwan S, Satghare P, Chua BY, Ni MY, Lun P, Tey WL, et al. Risk and protective factors of mental health during the COVID-19 pandemic: a cross-sectional study in Singaore. Ann Acad Med Singapore. 2023;52(5):249–58. doi: 10.47102/annals-acadmedsg.202341. [DOI] [PubMed] [Google Scholar]
- 31.Subramaniam M, Abdin E, Vaingankar JA, Shafie S, Chua BY, Sambasivam R, Zhang YJ, Shahwan S, Chang S, Chua HC, et al. Tracking the mental health of a nation: prevalence and correlates of mental disorders in the second Singapore mental health study. Epidemiol Psychiatr Sci. 2020;29:E29. doi: 10.1017/S2045796019000179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. 2006;166(10):1092–7. doi: 10.1001/archinte.166.10.1092. [DOI] [PubMed] [Google Scholar]
- 33.Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. 2001;16(9):606–13. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP. Psychometric properties of the 42-item and 21-item versions of the depression anxiety stress scales in clinical groups and a community sample. Psychol Assess. 1998;10(2):176–81. doi: 10.1037/1040-3590.10.2.176. [DOI] [Google Scholar]
- 35.Holden L, Lee C, Hockey R, Ware RS, Dobson AJ. Validation of the MOS social support survey 6-item (MOS-SSS-6) measure with two large population-based samples of Australian women. Qual Life Res. 2014;23(10):2849–53. doi: 10.1007/s11136-014-0741-5. [DOI] [PubMed] [Google Scholar]
- 36.Smith BW, Dalen J, Wiggins K, Tooley E, Christopher P, Bernard J. The brief resilience scale: assessing the ability of bounce back. Int J Behav Med. 2008;5(3):194–200. doi: 10.1080/10705500802222972. [DOI] [PubMed] [Google Scholar]
- 37.Luyten J, Bruyneel L, Van Hoek AJ. Assessing vaccine hesitancy in the U.K. population using a generalized vaccine hesitancy survey instrument. Vaccine. 2019;37(18):2494–501. doi: 10.1016/j.vaccine.2019.03.041. [DOI] [PubMed] [Google Scholar]
- 38.Gidengil C, Chen C, Parker AM, Nowak S, Matthews L. Beliefs around childhood vaccines in the United States: a systematic review. Vaccine. 2019;37(45):6793–802. doi: 10.1016/j.vaccine.2019.08.068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hoffman J. Mistrust of a coronavirus vaccine could imperil widespread immunity. The New York Times; 2020. Sept 1. https://www. nytimes.com/2020/07/18/health/coronavirus-anti-vaccine.html.
- 40.Maisonneuve AR, Witteman HO, Brehaut J, Dubé È, Wilson K. Educating children and adolescents about vaccines: a review of current literature. Expert Rev Vaccines. 2018;17(4):311–21. doi: 10.1080/14760584.2018.1456921. [DOI] [PubMed] [Google Scholar]
- 41.Shapiro GK, Tatar O, Dube E, Amsel R, Knauper B, Naz A, Perez S, Rosberger Z. The vaccine hesitancy scale: psychometric properties and validation. Vaccine. 2018;36(5):660–7. doi: 10.1016/j.vaccine.2017.12.043. [DOI] [PubMed] [Google Scholar]
- 42.Hu L, Bentler PM. Cut-off criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Struct Equ Modeling. 1999;6(1):1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- 43.Hubach RD, Shannon B, Morgan KD, Alexander C, O’Neil AM, Ernst C, Giano Z. COVID-19 vaccine hesitancy among rural Oklahomans. Rural Remote Health. 2022;22:7128. doi: 10.22605/RRH7128. [DOI] [PubMed] [Google Scholar]
- 44.Kumari A, Mahey R, Kachhawa G, Kumari R, Bhatla N. Knowledge, attitude, perceptions, and concerns of pregnant and lactating women regarding COVID-19 vaccination: a cross-sectional survey of 313 participants from a tertiary care centre of North India. Diabetes Metab Syndr Clin Res Rev. 2022;16(3):102449. doi: 10.1016/j.dsx.2022.102449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Alibrahim J, Awad A. COVID-19 vaccine hesitancy among the public in Kuwait: a cross-sectional survey. Int J Environ Res Public Health. 2021;18(16):8836. doi: 10.3390/ijerph18168836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brown P, Waite F, Larkin M, Lambe S, McShane H, Pollard AJ, Freeman D. “It seems impossible that it’s been made so quickly”: a qualitative investigation of concerns about the speed of COVID-19 vaccine development and how these may be overcome. Hum Vaccin Immunother. 2022;18(1):2004808. doi: 10.1080/21645515.2021.2004808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dror AA, Eisenbach N, Taiber S, Morozov NG, Mizrachi M, Zigron A, Srouji S, Sela E. Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur J Epidemiol. 2020;35(8):775–9. doi: 10.1007/s10654-020-00671-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Rief W. Fear of adverse effects and COVID-19 vaccine hesitancy: recommendations of the treatment expectation expert group. JAMA Health Forum. 2021;2(4):e210804. doi: 10.1001/jamahealthforum.2021.0804. [DOI] [PubMed] [Google Scholar]
- 49.Goldman RD, Krupik D, Ali S, Mater A, Hall JE, Bone JN, Thompson GC, Yen K, Griffiths MA, Klein Klein A, et al. Caregiver willingness to vaccinate their children against COVID-19 after adult vaccine approval. Int J Environ Res Public Health. 2021;18(19):10224. doi: 10.3390/ijerph181910224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bell S, Clarke R, Mounier-Jack S, Walker JL, Paterson P. Parents’ and guardians’ views on the acceptability of a future COVID-19 vaccine: a multi-methods study in England. Vaccine. 2020;38(49):7789–98. doi: 10.1016/j.vaccine.2020.10.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Razai MS, Kankam HKN, Majeed A, Esmail A, Williams DR. Mitigating ethnic disparities in COVID-19 and beyond. BMJ. 2021;372:m4921. doi: 10.1136/bmj.m4921. [DOI] [PubMed] [Google Scholar]
- 52.Pertwee E, Simas C, Larson HJ. An epidemic of uncertainty: rumors, conspiracy theories and vaccine hesitancy. Nat Med. 2022;28(3):456–9. doi: 10.1038/s41591-022-01728-z. [DOI] [PubMed] [Google Scholar]
- 53.Grossman VA. The COVID-19 vaccine: why the hesitancy? J Radiol Nurs. 2021;40:116–19. doi: 10.1016/j.jradnu.2021.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Office of the Mufti . Religious position on COVID-19 vaccination. 2020. Dec 13 [accessed 2023 Mar 26]. https://www.muis.gov.sg/officeofthemufti/Irsyad/Part-11-Religious-position-on-COVID-19-vaccine-English.
- 55.Fletcher D, Sarkar M. Psychological resilience: a review and critique of definitions, concepts, and theory. Eur Psychol. 2013;18:12–23. doi: 10.1027/1016-9040/a000124. [DOI] [Google Scholar]
- 56.Xing C, Sun J. The role of psychological resilience and positive affect in risky decision-making. Int J Psychol. 2013;48:935–43. doi: 10.1080/00207594.2012.729840. [DOI] [PubMed] [Google Scholar]
- 57.Bendau A, Plag J, Petzold MB, Ströhle A. COVID-19 vaccine hesitancy and related fears and anxiety. Int Immunopharmacol. 2021;97:107724. doi: 10.1016/j.intimp.2021.107724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wu Y, Zhang T, Ye Z, Chen K, van der Kuijp J, Sun X, Han G, Zhao Y, Liu Y, Huang L. Public anxiety through various stages of COVID-19 coping: evidence from China. PLoS One. 2022;17(6):e0270229. doi: 10.1371/journal.pone.0270229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Józefacka NM, Podstawski R, Potoczny W, Pomianowski A, Kołek MF, Wrona S, Guzowski K. The importance of resilience and level of anxiety in the process of making a decision about SARS-CoV-2 vaccination. Int J Environ Res Public Health. 2023;20(2):999. doi: 10.3390/ijerph20020999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang X, Shen J, Li M, Shi Y, Wang Q, Chen F, Qin H, Zhao X. The association between socio-demographics and mental distress following COVID-19 vaccination-mediation of vaccine hesitancy. Vaccines (Basel). 2022;10(10):1697. doi: 10.3390/vaccines10101697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mercuri M, Baigrie B. The brave new world of pandemic resilience. J Eval Clin Pract. 2022. June;28(3):347–52. doi: 10.1111/jep.13667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.World Health Organization. Regional Office for Europe . Rapid qualitative research to increase COVID-19 vaccination uptake: a research and intervention tool. World Health Organization; Regional Office for Europe. 2022. https://apps.who.int/iris/handle/10665/351117.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data is available from the first author on request.


