Abstract
Background
Occupational Safety and Health is an important public health topic. Many employers may regard health promotion or prevention initiatives as an additional cost with few benefits. The aim of this systematic review is to identify the studies conducted on the return on investment (ROI) of preventive health interventions conducted within workplaces, and to describe their designs, topics and calculation methods.
Methods
We searched PubMed, Web of Science, Science Direct, National Institute for Occupational Safety and Health, International Labour Organization and Occupational Safety and Health Administration from 2013 to 2021. We included studies that evaluated prevention interventions in the workplace setting and reported an economic outcome or company-related benefits. We report the findings according to PRISMA reporting guidelines.
Results
We included 141 articles reporting 138 interventions. Of them, 62 (44.9%) had an experimental design, 29 (21.0%) had a quasi-experimental design, 37 (26.8%) were observational studies and 10 (7.2%) were modelling studies. The interventions’ objectives were mostly related to psychosocial risks (N = 42; 30.4%), absenteeism (N = 40; 29.0%), general health (N = 35; 25.4%), specific diseases (N = 31; 22.5%), nutrition (N = 24; 17.4%), sedentarism (N = 21; 15.2%) musculoskeletal disorders (N = 17; 12.3%) and accidents (N = 14; 10.1%). The ROI calculation was positive for 78 interventions (56.5%), negative for 12 (8.7%), neutral for 13 (9.4%) and undetermined for 35 (25.4%).
Conclusion
There were many different ROI calculations. Most studies have a positive result but randomized controlled trials have fewer positive results than other designs. It is important to conduct more high-quality studies so that results can inform employers and policy-makers.
Introduction
Occupational Safety and Health (OSH) has been a topic of research for many years. While previously the focus of OSH was linked to accidents and physical and chemical risks, in the last two decades the focus shifted towards an increased attention to prevention, which is reflected in the growing number of research articles published on the subject.1
The Third European Survey of Enterprises on New and Emerging Risks (ESENER 2019) report by the European Agency for Safety and Health at Work shows that employers are mostly that employers address health and safety issues mostly to fulfil legal obligations, and that maintaining or increasing productivity is the least important motivation for doing so.2 It suggest that many employers may regard health promotion or prevention initiatives in the workplace as an additional cost with few benefits.
In many other areas of public health research, such as infectious diseases or cancer, investing in prevention yields positive return on investment (ROI), as it saves money from further treatments.3–5 It would be interesting to verify if OSH prevention has similar results. ROI is a notion that may be described by many kinds of indicators: it describes the economic benefits as results of the investment but the indicators are not necessarily monetary figures, e.g. the reduction of lost hours or the increase in productivity and is often related to the cost of the investment itself. In this case, it may be illustrated by a ratio (profits/investment) or a duration (payback period). Several reviews have investigated the ROI of prevention initiatives, with mixed results. The limitation of those reviews is that they are either limited to one country, such as Canada,6 USA,5 and therefore are not applicable to other countries, or are either focused on occupational health and safety,7 workplace wellness programs (WWP), which are strategies used by employers to address risk factors for chronic diseases or workplace health promotion,6,8–10 or integrated workplace intervention that combine health promotion with health and safety. The results of those reviews are summarized in Supplementary appendix S1. We aimed to take a broader approach by including all studies that evaluate a prevention initiative on the spectrum of occupational health and safety and health promotion. We included all three types of prevention, primary, secondary and tertiary.
The aim of this systematic review is to identify the studies conducted on the ROI of preventive health interventions conducted within workplaces, and to describe their designs, topics and calculation methods.
Methods
Search strategy
We registered the study on Prospero (registration number CRD42021288927) and elaborated a protocol detailing the research question, databases, keywords, inclusion and exclusion criteria and data collection form prior to starting the search. No amendments were made to this protocol during the study. We searched six databases (three scientific and three grey literature databases): PubMed, Web of Science, Science Direct, National Institute for Occupational Safety and Health, International Labour Organization and Occupational Safety and Health Administration with a selection of keywords and MeSH terms (when applicable) related to prevention, workplace level and economic intervention, but excluding irrelevant items (managed care, occupational therapy, qualitative studies, children, etc.). We then screened the list of references of included articles to search for new articles. We have excluded articles related to epidemic situations. The exact selection of keywords is available in Supplementary appendix S2.
Inclusion and exclusion criteria
We included studies that evaluated a health promotion or prevention intervention in the workplace setting or directed at employees, and reported an economic outcome or company-related benefits. All types of intervention aimed at improving employees’ health or preventing health impairment were considered. The details are as follows:
Study type: we included articles evaluating an intervention of any design (experimental, quasi-experimental, observational and modelling studies) and excluded qualitative studies, protocols and reviews.
Interventions: we included articles reporting workplace intervention or directed at employees. That included any type of interventions aimed at improving employees’ health or preventing health impairment (organizational, environmental or individual interventions) and excluded interventions focusing solely on occupational therapy or articles that focused solely on the prevention of occupational infectious diseases.
Outcomes: we included articles reporting economic criteria (monetary and non-monetary) or company-related benefits such as reducing work-related injuries or reducing absenteeism, for example and excluded those that reported only health outcome and no economic outcome. Economic outcomes were classified as primary outcomes, while health outcomes were classified as secondary outcomes.
Participants: we included articles whose participants were adults (people over 18 years old) working for an organization, private or public, that implemented a workplace health promotion intervention and participants working or on sick leave and excluded studies with unemployed or retired participants or children.
Country: due to the differences in OSH and healthcare system, we restricted the analysis to high-income countries according to the World Bank classification.11
Publication dates: from 01 January 2013 to 31 August 2021, as the most ancient reviews we found are from 2013.
Study selection
Study selection was carried out by two researchers independently (AP and PE, then FT and PE) using the Rayyan platform.12 Results from the two databases were imported, duplicates were removed, then each title and abstract were screened for inclusion by two researchers independently, using ‘blind’ mode. Then we removed blind mode and compared results. In the event of a conflict, WD suggested a resolution and the final decision was made by consensus. A second study selection was operated when reading the full text of the articles. Studies were excluded if they initially appeared to fulfil inclusion criteria but details from the full text revealed that they did not; and we included extra articles based on references.
Data collection
Data were collected using a standard form on an Excel sheet. Information retrieved included type of intervention, objective of the intervention, data collection methodology, study design, work sector, type of company, health outcome measured, economic outcome measured and finally the results of the economic evaluation: gain, loss, neutral or undetermined (in our study neutral means that the results were neither positive nor negative, and undetermined means that the study could not conclude whether the results were positive or negative). The details of the health outcomes and economic outcomes are shown in Supplementary appendix S3. We collected the type of intervention and made a distinction between organizational interventions, technical interventions and human interventions. Organizational interventions are defined as those that aim to change organization or management, technical interventions are interventions that modify equipment or physical space (such as personal protective equipment, standing desks or ergonomic stretchers, etc.) and human interventions are health education interventions that aim to modify behaviour (such as training or coaching). We classified economic outcomes as primary outcomes and health outcomes as secondary outcomes. The details of the classification between organizational, technical and human interventions are in Supplementary appendix S3, as well as the details of economic and health outcomes. In cases where several articles reported the same intervention when it was conducted in different settings and populations, we analysed the results as several interventions. However, when several articles reported the same study conducted in a single setting and population, we counted them as one intervention.
Data analysis
We performed simple descriptive statistics on the characteristics of articles, and on the results of the ROI calculation. When an ROI was quantified, we reported it but did not calculate an average, as the calculation methods might have differed between studies.
We report the findings according to the updated 2020 PRISMA reporting guidelines, with the checklist in Supplementary appendix S4.13
Quality appraisal
We evaluated the quality of articles using the integrated quality criteria for review of multiple study designs (ICROMS).14 This appraisal tool has been created to evaluate the quality of multiple study designs within the same systematic review: randomized controlled trials, controlled or non-controlled before-after, controlled or non-controlled interrupted times series, cohorts and qualitative studies. For the economic evaluation studies, we used the consensus on health economic criteria (CHEC) checklist, which is a checklist routinely used to evaluate the methodological quality of economic evaluations.15
Results
Selection of articles
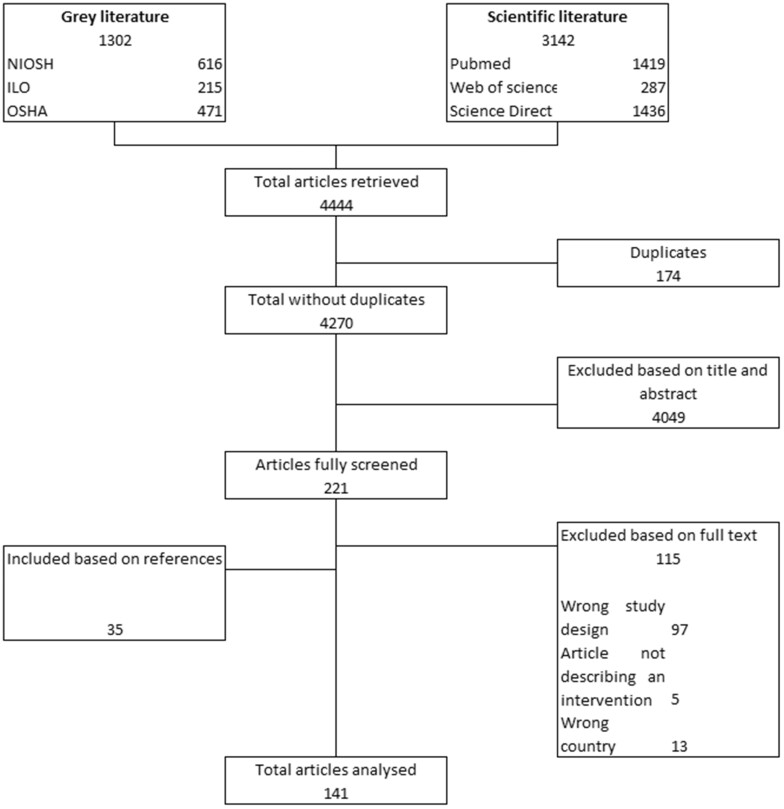
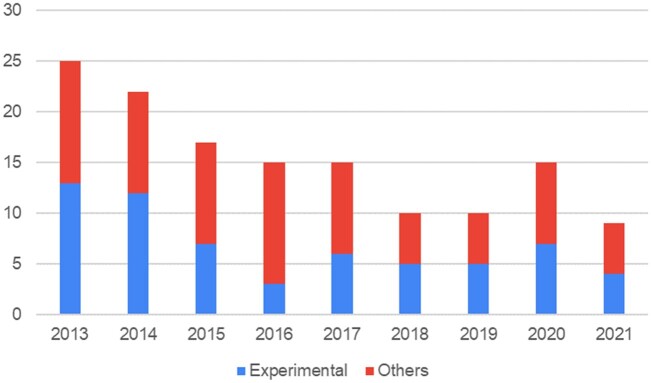
We retrieved 4270 articles from the six databases after removing duplicates, then excluded 4049 on the basis of title or abstract. Of the 221 articles screened, we excluded 115 on the basis of the full text and included 35 based on the references. A total of 141 articles were analysed. The results are shown in figure 1. The number of publications slightly declined over the years, as seen in figure 2. The full list of articles, as well as the name of interventions, is listed in Supplementary appendix S5.
Figure 1.
Flowchart of selected articles
Figure 2.
Number of publications per year and study design
We found three ‘duplicate’ studies: when two articles reported different results for the same study. In those cases, one article reported the results of the randomized controlled trial, and one article reported the results of the nested economic evaluation. We counted those results as one intervention. As a result, for a total of 141 articles, we found 138 interventions.
Of the 138 interventions studied, 62 (44.9%) had an experimental design (randomized controlled trials), 29 (21.0%) had a quasi-experimental design, 37 (26.8%) were observational studies and 10 (7.2%) were modelling studies.
Characteristics of interventions
Most interventions were conducted in the USA (N = 53; 38.4%), followed by the Netherlands (N = 26; 18.8%), the UK (N = 10; 7.2%), Sweden and Germany (N = 8; 5.8% each), Australia and Canada (N = 6; 4.3% each). Other countries are: Finland, South Africa, Italy, Denmark, Ireland, China, Israel, Switzerland, Spain, Taiwan, Portugal, Norway and Japan.
In terms of work sector, interventions were mostly conducted in any sector (N = 59; 39.1%), healthcare sector (N = 26; 18.8%), industry (N = 11; 8.0%), office-based work (N = 17; 12.3%), service (N = 14; 10.1%), mining, firefighting or gas industry (N = 4; 2.9%), construction (N = 4; 2.9%), agriculture (N = 4; 2.9%), transportation (N = 1; 0.7%) and other sectors (N = 12; 8.6%). The total exceeds 100% as 12 interventions were conducted in several types of organizations.
The interventions consisted of coaching (N = 84; 60.9%), training (N = 68; 49.3%), physical activity (N = 31; 22.5%), other human interventions (N = 29; 21.0%), care (N = 22; 15.9%), equipment (N = 18; 13.0%), screening (N = 20; 14.5%), other organizational interventions (N = 17; 12.3%), financial incentives (N = 17; 12.3%), measurement (N = 13; 9.4%), operatory modes (N = 6; 4.3%), other technical interventions (N = 4; 2.9%) and non-financial incentives (N = 4; 2.9%). In total 22 interventions (16%) had at least one organizational intervention; 49 interventions (36%) had at least one technical intervention and 125 interventions (91%) had at least one human intervention. Interventions can be classified as primary prevention interventions (N = 67; 48.6%), secondary prevention interventions (N = 3; 2.2%), or tertiary prevention interventions (N = 43; 31.2%). The results exceed 100% as 25 interventions (18.1%) cover more than one area of prevention: 10 interventions are primary and secondary prevention interventions (7.2%); 9 interventions are secondary and tertiary prevention interventions (6.5%); 4 interventions are primary and tertiary prevention interventions (2.9%) and 2 interventions cover the three levels of prevention (1.4%).
Interventions were mostly conducted in public organizations (N = 44; 31.9%), large organizations (more than 5000 employees) (N = 33; 23.9%) or small organizations (N = 12; 8.7%). For 39.9% of the interventions, the type of organization was not mentioned (N = 55). The total exceeds 100% as seven interventions were conducted in several types of organizations.
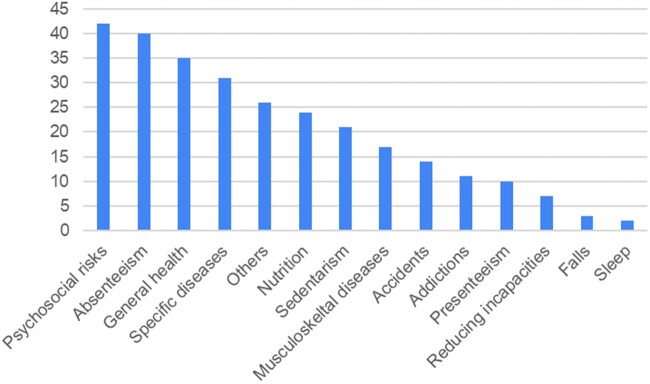
Almost half of the interventions had several objectives (N = 68; 49.3%). The interventions’ objectives were related to mostly psychosocial risks (N = 42; 30.4%), absenteeism (N = 40; 29.0%), general health (N = 35; 25.4%), specific diseases (N = 31; 22.5%), others (N = 26; 18.8%), nutrition (N = 24; 17.4%), sedentarism (N = 21; 15.2%), musculoskeletal disorders (N = 17; 12.3%), accidents (N = 14; 10.1%), addictions (N = 11; 8.0%), presenteeism (N = 10; 7.2%), reducing incapacities (N = 7; 5.1%), falls (N = 3; 2.2%) and sleep (N = 2; 1.4%). The results are shown in figure 3.
Figure 3.
Interventions’ objectives by number
When narrowing the results to randomized clinical trials, we found that the interventions’ objectives were related to mostly psychosocial risks (N = 24; 39%) and absenteeism (N = 25; 40%), general health (N = 12; 19%), nutrition (N = 9, 15%), others (N = 9, 15%), other specific diseases (N = 8; 13%), sedentarism (N = 9; 15%), presenteeism (N = 7; 11%), musculoskeletal disorders (N = 5; 8%), reducing incapacities (N = 5; 8%), accidents (N = 1; 2%) and falls (N = 1; 2%).
Outcomes
Nearly all studies reported a health outcome (N = 136; 98.6%). The most reported health outcomes were quality of life (N = 53; 38.4%), absenteeism (N = 48; 34.8%), psychosocial risks (N = 34; 24.6%), specific diseases (N = 30; 21.7%), presenteeism (N = 18; 13.0%) and other outcomes (N = 31; 22.5%).
The most reported economic outcomes were absence (N = 79; 57.2%), healthcare costs (N = 55; 39.9%), productivity (N = 50; 36.2%), costs (N = 48; 34.8%), ROI calculation (N = 14; 10.1%), accidents (N = 11; 8.0%), turnover (N = 6; 4.3%), time (N = 4; 2.9%) and other economic outcomes (N = 14; 10.1%). For both economic and health outcomes, the result exceeds 100% as most studies report several outcomes.
Quality appraisal
Of the 141 articles included, 111 were evaluated using the ICROMS tools and 30 using the CHEC checklist. The results are available in Supplementary appendix S6. Most studies designs scored the poorest for the sections measuring bias in outcome measurement and blinding, and bias in follow-up.
Evidence on return on investment
The ROI calculation was positive for 78 interventions (56.5%), negative for 12 (8.7%), neutral for 13 (9.4%) and undetermined for 35 interventions (25.4%). A total of 95 interventions (68.8%) reported a monetary quantification and 43 interventions did not (31.2%). A benefit cost ratio (BCR) was calculated for 26 interventions (18.8%). In those 28 studies, 8 calculated ROI using a cost–savings analysis (30.8%), 7 used a cost–benefits analysis (26.9%), 4 performed a cost-effectiveness analysis (15.4%), 4 used an incremental cost-effectiveness ratio (15.4%), 1 calculated the quality-adjusted life years (QALY), 1 used a cost–utility analysis and 1 used the Truven Health Analytics ROI model (3.8% each).
We sub-calculated the results according to the study design, level of prevention and type of prevention. Results are shown in table 1. In randomized controlled trials, the proportion of positive results is lower than for other designs.
Table 1.
ROI result by study design, level of prevention and type of intervention
| Positive ROI | Negative ROI | Neutral ROI | Undetermined ROI | Total | |
|---|---|---|---|---|---|
| Study design | |||||
| Experimental N (%) | 24 (39%) | 9 (15%) | 8 (13%) | 21 (34%) | 62 (100%) |
| Quasi-experimental N (%) | 22 (76%) | 1 (3%) | 3 (10%) | 3 (10%) | 29 (100%) |
| Observational N (%) | 25 (68%) | 1 (3%) | 1 (3%) | 10 (27%) | 37 (100%) |
| Modelling N (%) | 7 (70%) | 1 (10%) | 1 (10%) | 1 (10%) | 10 (100%) |
| Level of prevention | |||||
| Primary prevention N (%) | 48 (58%) | 7 (8%) | 11 (13%) | 17 (20%) | 83 (100%) |
| Secondary prevention N (%) | 14 (58%) | 1 (4%) | 1 (4%) | 8 (33%) | 24 (100%) |
| Tertiary prevention N (%) | 32 (55%) | 5 (9%) | 2 (3%) | 19 (33%) | 58 (100%) |
| Type of intervention | |||||
| Organizational N (%) | 11 (50%) | 1 (5%) | 1 (5%) | 9 (41%) | 22 |
| Technical N (%) | 27 (55%) | 6 (12%) | 4 (8%) | 12 (24%) | 49 |
| Human N (%) | 68 (54.4%) | 12 (9.6%) | 12 (9.6%) | 33 (26.4%) | 125 |
Discussion
Interpretation of results
The objective of our systematic review was to identify the studies conducted on the ROI of preventive health interventions conducted within workplaces, and to describe their designs, topics and calculation methods. We found that the most important topic of intervention was the improvement of mental health/psychosocial risks. The growing importance of psychosocial risks and work-related stress have been highlighted in a bibliometric study of occupational health research,1 as well as in the ESENER report.2 We found that the number of published articles has been decreasing from 2013 to 2019. It should be noted that in 2021, the selection was stopped in August, and in 2020, publication activity might have been modified because of the pandemic. Therefore, results in 2020 and 2021 might not be reflect the ongoing publication trends. This result is in contradiction with a bibliometric study of occupational health and safety research that found an increase in published articles.1 This difference might be due to the difference between topics. A large-scale bibliometric study on research on the return of investment of occupational research could give additional information. The publication bias should also be taken into account, as negative studies are less likely to be published.16 Most studies have a positive result, however, this result is nuanced, but still remains mainly positive when adjusting for the study type, as the proportion of positive results is lower for randomized controlled trials than for other study designs. Randomized controlled trials are the gold standard of health research and their level of evidence prevail over other study types. Applying a randomized controlled trial design in an occupational health study can present specific challenges.17 However, precisely because of the differences between occupational health research and clinical research, randomized controlled trials might not produce results that are close to real-life results or be generalizable to the entire working population. Including observational studies into systematic reviews is challenging. However, observational studies are common in public health interventions and help provide a comprehensive picture of the range of interventions and evidence available for some public health questions.18 The mechanism towards which WWP might be cost-effective is through preventing chronic diseases, as it has been established that work environment is one of the factors influencing chronic diseases.19
Our review has included studies from 26 different countries, all of them having a different health system.20 In some regimes, health insurance is mostly or entirely paid for by private insurers, while in others, health insurance is mostly or entirely provided by the state. This difference may influence how cost-effective it is for employers to implement prevention interventions.
We were not able to calculate an average ROI. The objective of our study was to have a broad view of prevention interventions and their results but we found that many ROI had different calculation methods or measures. Although the studies included mostly used cost-savings and cost-benefits analysis, the diversity of calculation methods used makes it difficult to draw conclusions. We need to stress that ROI is not a defined indicator but a notion that may be calculated in different ways and described by various specific indicators. This was confirmed by the diverse variables we observed in the reviewed articles: monetary quantities such as medical costs savings (in dollars, euros, etc.) but also non-monetary quantities not necessarily converted into monetary terms like number of days of sick leave saved. When converted, various ratios may be computed and referred to as ‘ROI’: BCR, net present value or profitability index. Although these indicators were not explicitly mentioned in the articles, the given data enable the reader to compute them. In this article, we chose to use the BCR (gains/costs) and refer to it as ‘ROP’: return on prevention.
Comparison with literature
Although we found mostly positive results, those results were nuanced when accounting for the study type with a less important proportion of positive results found for results of randomized controlled trials. This result is concordant with another systematic review8 that aimed to determine the relationship between ROI and quality of study methodology in workplace health promotion programs. One result is that a majority of studies have been conducted in the USA, which is in accordance with other studies of the same type.6,8,9,21 Previous studies have highlighted the variety of US state laws regulating WWP in the USA.22 Another systematic review examining the economic evaluations of interventions against influenza at workplaces found positive results with a diversity of calculation methods.23 Prevention is generally considered cost-effective in other areas of prevention, such as vaccination, cancer prevention or screening, smoking prevention or prenatal care, as it acts on the determinants of health and prevents further expensive treatments.24 Therefore, our results are consistent with previous reviews of the ROI of prevention. The mechanisms towards which workplace prevention might have a positive ROI is slightly different as prevention interventions in the workplace not only save expensive treatments and sick leave, it also ensures that the workforce remains healthy and productive.
Implication of results
A limitation of our review is that we did not study the details associated with the success or failure of the interventions. There is a variation in the results of the prevention interventions, which could be due to the nature of interventions, or to factors linked to the implementation. Further studies could take a more qualitative approach and examine those factors in order to draw recommendations for future intervention project. Another limitation of our study lies in our search strategy. We used only three scientific and three non-scientific databases. We did not use Google Scholar or results from systematic research, which might limit the comprehensiveness of our results. Finally, we found that the length of time between interventions and their observed impact varies between studies, which limits the comparison between studies.
The methodologies used to calculate the ROI are very diverse and more standardized designs would allow for comparisons and meta-analyses. More research should be conducted using a strong design, with a control group. Indeed, Grimani et al.7 argue that having a control group is an essential element of a full economic evaluation. Regarding the quality of included studies, we found that most studies scored the poorest for the sections measuring bias in outcome measurement and blinding, and bias in follow-up. This can be explained by the fact that most studies measured prevention interventions for which, unlike clinical trials, it is difficult, if not impossible to blind participants to the allocation group.
The results of this systematic review indicate a positive ROI of prevention interventions. But it should be noted that due to the limitations highlighted, those results are illustrations, rather than a demonstration of the return of investment of prevention. Those results suggest that investing in employees’ safety and health might be profitable and developing workplace prevention or health promotion initiatives might hold interest for both employers and employees. In many health systems, private insurers are involved in insuring employees’ health, either primarily, or to complement public health insurance. Those results might give a rationale for those private insurers to include prevention into their services and they could be of interest to policy-makers too.
Supplementary Material
Contributor Information
Frédérique Thonon, Laboratoire Modélisation Epidémiologie et Surveillance des Risques Sanitaires (MESuRS), Conservatoire national des Arts et Métiers (CNAM), Paris, France; Chaire Entreprise et santé, CNAM-Malakoff Humanis, Malakoff, France.
Anne-Sophie Godon-Rensonnet, Chaire Entreprise et santé, CNAM-Malakoff Humanis, Malakoff, France; Malakoff Humanis, Paris, France.
Anne Perozziello, Laboratoire Modélisation Epidémiologie et Surveillance des Risques Sanitaires (MESuRS), Conservatoire national des Arts et Métiers (CNAM), Paris, France.
Jérôme-Philippe Garsi, Laboratoire Modélisation Epidémiologie et Surveillance des Risques Sanitaires (MESuRS), Conservatoire national des Arts et Métiers (CNAM), Paris, France.
William Dab, Laboratoire Modélisation Epidémiologie et Surveillance des Risques Sanitaires (MESuRS), Conservatoire national des Arts et Métiers (CNAM), Paris, France.
Philippe Emsalem, Avyso, Paris, France.
Supplementary data
Supplementary data are available at EURPUB online.
Funding
This study was funded partially by a partnership between Malakoff Humanis and MESuRS research team (Chaire Entreprises et Santé).
Conflicts of interest: None declared.
Key points.
Many employers may regard health promotion or prevention initiatives in the workplace as an additional cost with few benefits.
The objective of this article is to identify the studies conducted on the ROI of preventive health interventions conducted within workplaces, and to describe their designs, topics and calculation methods.
We found that most included studies have positive results.
Those results suggest that investing in employees’ safety and health might be profitable and developing workplace prevention or health promotion initiatives might hold interest for employers, employees, health insurers and policy makers.
Most studies suffer from a poor quality.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
- 1. Wang Y, Chen H, Liu B, et al. A systematic review on the research progress and evolving trends of occupational health and safety management: a bibliometric analysis of mapping knowledge domains. Front Public Health 2020;8:81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. European Agency for Safety and Health at Work (EU-OSHA). Third European Survey of Enterprises on New and Emerging Risks (ESENER 3) [Internet]. November 2019: 15. Available at: https://osha.europa.eu/en/publications/third-european-survey-enterprises-new-and-emerging-risks-esener-3/view (15 juill 2021, date last accessed).
- 3. Khushalani JS, Song S, Calhoun BH, et al. Preventing leading causes of death: systematic review of cost-utility literature. Am J Prev Med 2022;62:275–84. [DOI] [PubMed] [Google Scholar]
- 4. Myran DT, Morton R, Biggs BA, et al. The effectiveness and cost-effectiveness of screening for and vaccination against hepatitis B virus among migrants in the EU/EEA: a systematic review. Int J Environ Res Public Health 2018;15:1898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Mühlberger N, Sroczynski G, Gogollari A, et al. Cost effectiveness of breast cancer screening and prevention: a systematic review with a focus on risk-adapted strategies. Eur J Health Econ 2021;22:1311–44. [DOI] [PubMed] [Google Scholar]
- 6. Jacobs JC, Yaquian E, Burke SM, et al. The economic impact of workplace wellness programmes in Canada. Occup Med Oxf Engl 2017;67:429–34. [DOI] [PubMed] [Google Scholar]
- 7. Grimani A, Bergström G, Casallas MIR, et al. Economic evaluation of Occupational Safety and Health interventions from the employer perspective: a systematic review. J Occup Environ Med 2018;60:147–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Baxter S, Sanderson K, Venn AJ, et al. The relationship between return on investment and quality of study methodology in workplace health promotion programs. Am J Health Promot 2014;28:347–63. [DOI] [PubMed] [Google Scholar]
- 9. Lerner D, Rodday AM, Cohen JT, Rogers WH. A systematic review of the evidence concerning the economic impact of employee-focused health promotion and wellness programs. J Occup Environ Med 2013;55:209–22. [DOI] [PubMed] [Google Scholar]
- 10. Rongen A, Robroek SJW, van Lenthe FJ, Burdorf A. Workplace health promotion: a meta-analysis of effectiveness. Am J Prev Med 2013;44:406–15. [DOI] [PubMed] [Google Scholar]
- 11. World Bank. World Bank Country and Lending Groups. Available at: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (9 mai 2023, date last accessed).
- 12. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for. Syst Rev 2016;5:210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. PLoS Med 2021;18:e1003583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Zingg W, Castro-Sanchez E, Secci FV, et al. Innovative tools for quality assessment: integrated quality criteria for review of multiple study designs (ICROMS). Public Health 2016;133:19–37. [DOI] [PubMed] [Google Scholar]
- 15. Evers S, Goossens M, de Vet H, et al. Criteria list for assessment of methodological quality of economic evaluations: consensus on health economic criteria. Int J Technol Assess Health Care 2005;21:240–5. [PubMed] [Google Scholar]
- 16. Dickersin K, Min YI. Publication bias: the problem that won’t go away. Ann N Y Acad Sci 1993;703:135–46. discussion 146–8. [DOI] [PubMed] [Google Scholar]
- 17. Schelvis RMC, Oude Hengel KM, Burdorf A, et al. Evaluation of occupational health interventions using a randomized controlled trial: challenges and alternative research designs. Scand J Work Environ Health 2015;41:491–503. [DOI] [PubMed] [Google Scholar]
- 18. Hilton Boon M, Burns J, Craig P, et al. Value and challenges of using observational studies in systematic reviews of public health interventions. Am J Public Health 2022;112:548–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sorensen G, Landsbergis P, Hammer L, Workshop Working Group on Worksite Chronic Disease Prevention, et al. Preventing chronic disease in the workplace: a workshop report and recommendations. Am J Public Health 2011;101:S196–207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Esping-Andersen G. The Three Worlds of Welfare Capitalism . Princeton, USA: Princeton University Press, 1990. [Google Scholar]
- 21. Baid D, Hayles E, Finkelstein EA. Return on Investment of Workplace Wellness Programs for Chronic Disease Prevention: A Systematic Review. Am J Prev Med 2021;61:256–66. [DOI] [PubMed] [Google Scholar]
- 22. Pomeranz JL, Garcia AM, Vesprey R, Davey A. Variability and limits of US state laws regulating workplace wellness programs. Am J Public Health 2016;106:1028–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ofori SK, Hung YW, Schwind JS, et al. Economic evaluations of interventions against influenza at workplaces: systematic review. Occup Med Oxf Engl 2022;72:70–80. [DOI] [PubMed] [Google Scholar]
- 24. Stepanek M, Hafner M, Taylor J, et al. The return of investment for preventive healthcare programmes: a calculation framework for GSK’s Partnership for Prevention (P4P). RAND Corporation, 2017. Available at: https://www.rand.org/pubs/research_reports/RR1787.html (5 September 2022, date last accessed).
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analysed during this study are included in this published article and its supplementary information files.