Abstract
Compared to endoscopic mucosal resection (EMR), colonoscopic endoscopic submucosal dissection (C-ESD) has the advantages of higher en bloc resection rates and lower recurrence rates of colorectal neoplasms. Therefore, C-ESD is considered an effective treatment method for laterally spread tumors and early colorectal cancer. However, C-ESD is technically more difficult and requires a longer procedure time than EMR. In addition to therapeutic efficacy and procedural difficulty, safety concerns should always be considered when performing C-ESD in clinical practice. Bleeding and perforation are the main adverse events associated with C-ESD and can occur during C-ESD or after the completion of the procedure. Most bleeding associated with C-ESD can be managed endoscopically, even if it occurs during or after the procedure. More recently, most perforations identified during C-ESD can also be managed endoscopically, unless the mural defect is too large to be sutured with endoscopic devices or the patient is hemodynamically unstable. Delayed perforations are quite rare, but they require surgical treatment more frequently than endoscopically identified intraprocedural perforations or radiologically identified immediate postprocedural perforations. Post-ESD coagulation syndrome is a relatively underestimated adverse event, which can mimic localized peritonitis from perforation. Here, we classify and characterize the complications associated with C-ESD and recommend management options for them.
Keywords: Colorectal neoplasms, Endoscopic submucosal dissection, Hemorrhage, Intestinal perforation, Intraoperative complications
INTRODUCTION
Endoscopic submucosal dissection (ESD) is an advanced therapeutic procedure for the removal of large, albeit superficial, colorectal neoplasia, such as laterally spreading tumors and early colorectal cancer.1 In comparison to endoscopic mucosal resection (EMR), ESD is advantageous owing to its high en bloc resection and reduced local recurrence rates. However, ESD is technically more challenging than conventional EMR for the treatment of colorectal lesions. The technical difficulty and anatomical features of the colorectum, including the thin wall layers, haustra, and long tubular structure with flexuosity, severely enhance the risk of complications, such as bleeding and perforation.2 Most complications related to colorectal ESD (C-ESD) can be treated medically and endoscopically, and surgical intervention is rarely required. Therefore, endoscopists should focus on the incidence, risk factors, and management of the major complications associated with C-ESD.
INTRAPROCEDURAL COMPLICATIONS
Bleeding
Bleeding is a frequent complication associated with C-ESD. Large vessels are more frequently exposed during C-ESD, compared with EMR and polypectomy, because submucosal dissection involves the deeper layer of the submucosa.1 Notably, a standardized definition of minor and major bleeding during C-ESD has not been established to date, and intraprocedural bleeding, which can be controlled by contact coagulation using the tip of a knife, is generally not considered a complication of C-ESD. Therefore, the intraprocedural bleeding rate has been poorly investigated and may have been underestimated in real-world clinical practice. Intraprocedural bleeding, defined as blood oozing or spurting during C-ESD, was reported in 1.8% (4/220) of cases.3
Bleeding can be controlled using either electrocoagulation or hemoclipping. The technique for hemostasis of intraprocedural bleeding during C-ESD is similar to that used for postpolypectomy or lower gastrointestinal bleeding. However, in contrast to postpolypectomy bleeding, electrocoagulation using hemostatic forceps is the first-choice technique in C-ESD, because the applied hemoclips may interfere with the next step of C-ESD. The bleeding point should be precisely localized to avoid excessive electrothermal injury to the bowel wall owing to delayed bleeding or perforation. When a bleeding point cannot be determined due to blood in the dependent area, a positional change may be helpful. For severe intraprocedural bleeding that cannot be controlled with electrocoagulation, clipping should be performed to achieve hemostasis.
Prophylactic hemostasis or electrocauterization of the exposed vessels in the submucosal layer is frequently required to prevent intraprocedural bleeding. Large-caliber vessels should be coagulated using hemostatic forceps in soft coagulation mode (Fig. 1).4 However, dissection and electrocauterization of the submucosal layer containing small-caliber vessels can be performed simultaneously using an endo-knife in swift or forced coagulation modes. In such cases, the speed of dissection should be reduced to enhance coagulation in the vessels.
Fig. 1.
Coagulation of large vessels in the submucosal layer. (A) During submucosal dissection, large vessels were exposed at the submucosal layer. (B) Vessels were coagulated with a coagrasper. (C) Coagulated vessels.
Perforation
Intraprocedural perforation is the most common complication associated with C-ESD; however, most perforations are now treated endoscopically. A multicenter study in Korea reported a perforation rate of 6.5% among 2,046 patients.5 Furthermore, a meta-analysis including 88 studies with a total of 14,584 patients reported a perforation rate of 5.2% (non-Asian countries, 8.6%; Asian countries, 4.5%).6 Experience of endoscopists, large tumor size >30 mm, and submucosal fibrosis are well-known risk factors of perforation in C-ESD.5,7-10 Occasionally, forceps biopsy on the lesions before C-ESD may result in fibrosis;11 hence, a cautious approach is required while performing biopsy before C-ESD. In terms of tumor location, the rectum is a safer location for perforation than other colonic segments (especially the right colon), because the rectal wall is thicker.10
The perforation rate of C-ESD is higher than that of gastric ESD,12,13 and, in general, C-ESD is technically more difficult than gastric ESD. Therefore, for beginners, C-ESD should be cautiously performed in the rectum only after gaining sufficient experience in gastric ESD.14,15 Endoscopists, who lack experience in gastric ESD, should perform C-ESD under the supervision of an experienced endoscopist, after having extensive colonoscopy training and multiple hands-on training sessions.16
The treatment of intraprocedural perforation during C-ESD is similar to that of colorectal perforation associated with other endoscopic interventions.17,18 Iatrogenic colonic perforation should be managed immediately, if recognized during endoscopic procedures. However, if perforation occurs before complete removal of the lesion using ESD, immediate endoscopic closure using hemoclips may interfere with the next step of C-ESD. Therefore, the timing of endoscopic closure should be based on patient’s condition and size of the perforation. If the patient can tolerate the pain and shows stable vital signs, and the perforation is not large enough to require surgery, the initial step for managing the perforation during C-ESD is to change the patient’s position and empty the bowel contents to prevent intraperitoneal leakage. Subsequently, submucosal dissection should be continued until the hemoclips do not interfere with C-ESD.
If the perforation closes successfully, the remaining tumor should be resected. The resection modality should be decided by the physician based on patient’s clinical condition. If the patient is stable, C-ESD can be continued after the endoscopic closure. However, if additional submucosal dissection after perforation is not possible, the remaining tumor can be resected using a snare, that is a hybrid ESD technique, before endoscopic closure of the iatrogenic perforation.19
Small perforations <10 mm can be managed with conventional through-the-scope clips.17 In the case of overt perforations, a defect in the proper muscle layer may be observed (Fig. 2A). Unlike iatrogenic colon perforation caused by other reasons, the perforation area in intraprocedural perforation during C-ESD may occupy only part of the ESD ulcer. Therefore, for smaller defects, the perforated site can be closed directly using clips (Fig. 2B). Furthermore, the proper muscle adjacent to the perforation should be approximated and clips should be deployed cautiously, to avoid tearing of the proper muscle layer. Additional clipping is recommended to ensure adequate and tight closure of the defect, even when the perforation site appears closed with a single clip (Fig. 2C). Applying the first clip directly to the defect is occasionally difficult; hence, in such cases, clipping can start from the lateral side to the opposite side of the ESD ulcer to close the mucosal defect in a ziplock manner (Fig. 3). After proper deployment of the first clip, additional clips can be placed next to the previous clip. Furthermore, both arms of the clip should be deployed to the intact mucosa or submucosa of the colonic wall rather than to the deeply excavated iatrogenic ulcer base or proper muscle layers. When the perforation site is concealed by the omentum, perforation may present as intra-abdominal fat tissue on endoscopy (Fig. 4) and may be overlooked. Therefore, endoscopists should be aware of the various types of perforation.
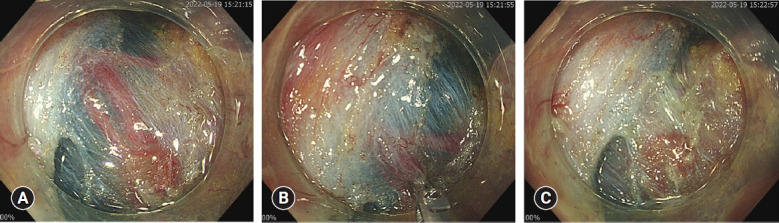
Fig. 2.
Perforation closure simply using conventional hemoclips. (A) Overt intraprocedural perforation was determined when the submucosal dissection was almost finished. (B) After completion of endoscopic submucosal dissection, the defect of the proper muscle layer was directly closed using a clip. (C) To ensure complete endoscopic closure, mucosa and submucosal layers adjacent to the perforated site were tightly closed using additional clips.
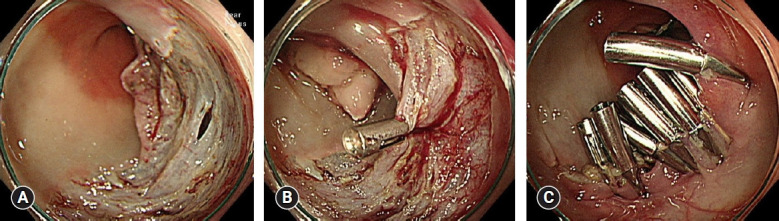
Fig. 3.
Perforation closure using the ziplock method. (A) Iatrogenic colon perforation during colonoscope insertion. (B) The first clip was placed at the lateral side of colon perforation. (C) Perforation was completely closed using additional clips. Adapted from closure of iatrogenic colon perforation during colonoscope insertion, courtesy of Prof. Yunho Jung, Soonchunhyang University College of Medicine.
Fig. 4.
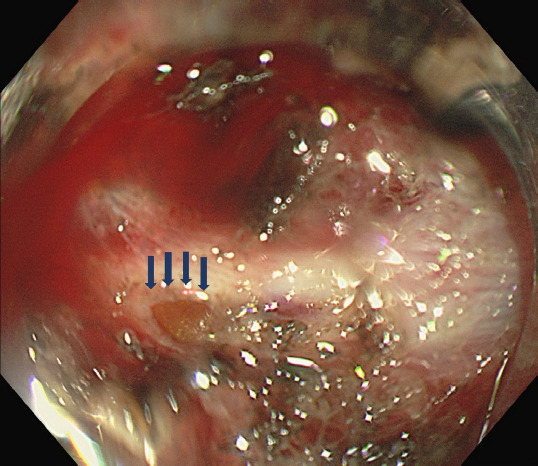
Identification of perforation concealed with the omentum. Extraluminal fat tissue was observed under a tiny proper muscle layer defect. Arrows indicate the concealed perforation site.
The first commercialized through-the-scope clip system consisted of a reusable rotatable device and a disposable clip that should be loaded manually.20 Although the cost of a reusable clip is low, reopening the clip using the reusable rotatable device is not possible. Recently, various single-use disposable clips have been made available.21 These clips can reduce the procedure time, because they are preloaded-type clips that are easy to handle.
For large perforations (>10 mm) that cannot be closed using a through-the-scope clip, additional devices or techniques are required. An over-the-scope clip (OTSC) can be applied for perforations >10 mm due to C-ESD (Fig. 5).22-24 An ex vivo animal study suggested that OTSC can be applied for perforations up to 30 mm in size.25 However, due to the tortuosity of the colon, the use of OTSC is limited for colon perforation.25 OTSC is indicated when perforations <2 to 3 cm occur at the distal colon.17,26 Endoloops and clips have been introduced to manage large perforations,27-29 and a dual-channel endoscope is required (Fig. 6). Currently, traction methods using clips and rubber bands are widely used for C-ESD.30 This method can also be used to manage perforation during C-ESD.31 Traction of one side of the colonic wall to the opposite side can approximate the post-ESD colonic defect or perforation (Fig. 7). After approximating the mural defect using the traction method, the perforation can be closed with clipping.
Fig. 5.
Over-the-scope clip (Ovesco Endoscopy AG).
Fig. 6.
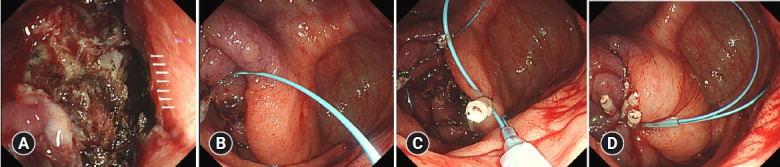
Endoloop and clip fixation for the treatment of perforation. (A) Large perforation. Arrows indicate the perforation site. (B) The first clip was fixed with an endoloop at normal colonic mucosa. (C) The second and third clips were placed to different side colon mucosa around the dissected ulcer. (D) The endoloop was tightened to close perforation.
Fig. 7.
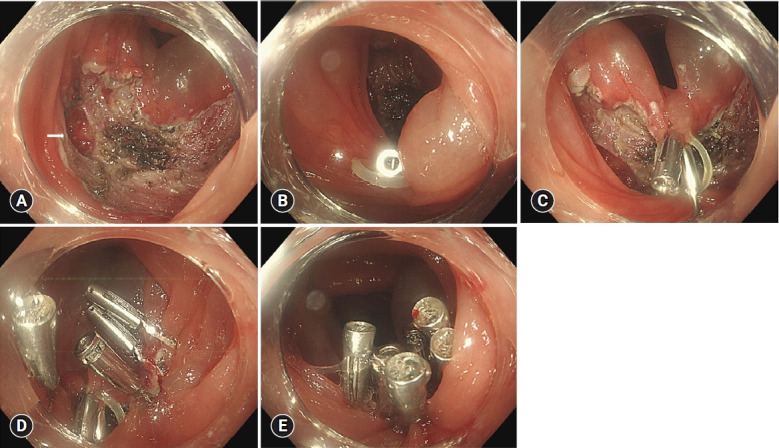
Endoscopic closure using the traction method. (A) A perforation of 6 mm in size is shown. Arrow indicates the perforation site. (B) One clip was fixed with a rubber band at the colonic mucosa. (C) Ulcer was partially approximated using the traction method (D) Additional clips were placed with ease after approximation. (E) Complete closure of the ulcer.
Endoscopic closure is usually recommended for perforations <30 mm.17,18 The suggested treatment strategies, including endoscopic and surgical treatments for intraprocedural perforations of C-ESD, are summarized in Table 1.17 The treatment strategy for intraprocedural perforation should be chosen based on the perforation size and location.
Table 1.
Treatment of intraprocedural perforation according to perforation size
| Clinical situation | Suggested treatment |
|---|---|
| Perforation size (mm) | |
| <10 | Through-the-scope clip |
| 10–30 | Endoloop fixed with clips or over-the-scope-clip |
| >30 | Surgery |
| Consideration of surgical treatment after endoscopic closure | |
| Severe peritoneal irritation sign | Surgerya) |
| Fever >1–2 days | |
| Hemodynamic instability |
Modified from Jung. Clin Endosc 2020;53:29–36.17
Decisions for surgery should be made based on patient’s condition.
The success rate of the endoscopic closure of perforations during C-ESD is not well established. In a previous study, success rate of endoscopic treatment was approximately 95.8% (23/24).7 Surgical treatment should be performed immediately when endoscopic closure is not feasible; a meta-analysis reported that 1% of all attempted C-ESD cases required surgical intervention.32
Perforations associated with C-ESD may also remain unidentifiable during the procedure. According to a multicenter study in Korea, 98 out of 135 (72.6%) C-ESD-related perforations were microperforations, which were identified radiologically only after completion of ESD.5 Therefore, post-ESD ulcers should be meticulously examined to identify muscle injury or defects in the colon wall. Once a deep mural injury is suspected or identified, prophylactic clipping is recommended. Notably, when a perforation is not managed during an endoscopic procedure, colonoscopy may be challenging.
Along with closure techniques, the use of carbon dioxide for insufflation, which is regarded as a standard technique for C-ESD, may help to reduce pain related to perforation.18,33 Despite advances in the endoscopic management of iatrogenic perforations, C-ESD-related colonic perforation may be associated with serious morbidity and rarely, mortality. Excessive air leakage after perforation can cause tension pneumoperitoneum, which manifests as severe abdominal distension, dyspnea, and hemodynamic instability. In cases of tension pneumoperitoneum, prompt percutaneous needle decompression using a 16-gauge needle should be performed.18,34,35 The lower abdomen is the recommended puncture site for decompression (Fig. 8).34 C-ESD should be performed by experienced therapeutic endoscopists in specialized centers where surgical backup is feasible.
Fig. 8.

Recommended area for needle decompression. Area in the dotted red line indicates suggested area.
POSTPROCEDURAL COMPLICATIONS
Post-ESD coagulation syndrome
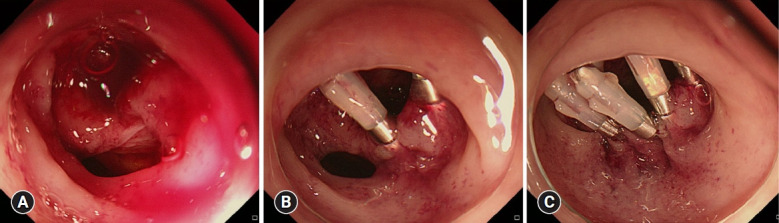
Patients may experience abdominal pain, localized tenderness, or fever after C-ESD. Although post-ESD coagulation syndrome (PECS) is not well defined, clinical diagnosis is based on the presence of localized abdominal tenderness near the ESD site, fever, or laboratory evidence of an inflammatory response, such as elevated C-reactive protein levels and leukocytosis.36,37 The pathogenesis of PECS is similar to that of postpolypectomy coagulation syndrome.38,39 The mechanism of PECS involves transmural bowel injury complicated by electrocautery (Fig. 9). Furthermore, local bacterial infections associated with mucosal defects may also lead to PECS.40 Clinically, PECS can mimic localized peritonitis caused by frank perforation. However, most PECS cases can be treated with conservative management, including a short-term fasting period, antibiotics, and adequate hydration. Hence, PECS should be differentiated from frank perforations.
Fig. 9.
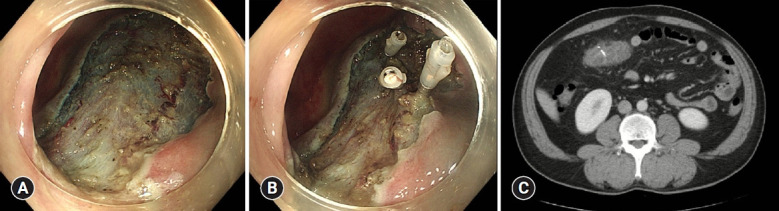
Post-endoscopic submucosal dissection coagulation syndrome. (A) After completion of submucosal dissection, neither deep proper muscle injury, nor overt perforation were suspected. (B) Clips were placed at the site of proper muscle injury. (C) Owing to abdominal pain and fever after the procedure, computed tomography was performed, revealing edematous wall thickening at the procedure site. Courtesy of Prof. Yunho Jung, Soonchunhyang University College of Medicine.
The incidence of PECS has been reported to be 4.8% to 14.2%,37,41,42 which is higher than that of postpolypectomy coagulation syndrome,38 probably because more extensive electrocautery is applied during ESD than during polypectomy. The risk factors for PECS include a longer procedure time, larger tumor size (>30 to 40 mm), submucosal fibrosis, and right-sided tumor location, such as in the ascending colon and cecum.41,42
Several strategies have been developed for the prevention of PECS. In a single-center randomized trial in Korea, administration of prophylactic antibiotics before C-ESD significantly reduced PECS occurrence (antibiotic group, 2.0% vs. non-antibiotics group, 16.0%; p=0.031).40 However, a multicenter study in Japan showed that prophylactic antibiotics did not significantly reduce the rate of PECS (antibiotics group, 4.7% vs. non-antibiotics group, 7.5%; p=0.29).43
Endoscopic closure using a hemoclip to prevent PECS has also been investigated,44 but results have been variable. A retrospective study in Japan suggested that line-assisted complete endoscopic closure of post-ESD ulcers reduced the PECS incidence (endoscopic closure, 0% [0/51] vs. non-closure, 12% [6/51]; p=0.03).45 However, in a single-center randomized study in Korea, endoscopic closure using clips did not reduce the PECS incidence (endoscopic closure, 8.2% [9/110] vs. non-closure, 10.9% [12/110]; p=0.647).46 According to a meta-analysis, endoscopic closure did not reduce the PECS incidence compared to non-closure (pooled odds ratio [OR], 0.75; 95% confidence interval [CI], 0.26–2.18).47 Hence, the efficacy of preventive strategies for PECS remains questionable.
Delayed bleeding
Delayed bleeding after C-ESD is a major adverse event that leads to unexpected hospital visits and increases in medical costs. Although the definition of delayed bleeding varies between studies, it is often defined as postprocedural bleeding that presents with hematochezia or melena and requires endoscopic hemostasis or transfusion. Large polyps, proximal location, and use of antithrombotic agents are significant risk factors for delayed bleeding in polypectomy.48 C-ESD is performed for polyps larger than 2 cm in most cases;1 hence, physicians should be cautious of delayed bleeding after C-ESD. Delayed bleeding may occur between 2 to 7 days after C-ESD.49 A multicenter study in Korea reported that the incidence of delayed bleeding after C-ESD was 2.9% among 1,604 patients, and risk factors included large tumor size (≥3 cm), use of antiplatelet agents, and location in the rectosigmoid colon.50 Furthermore, location in the rectum was a significant risk factor for delayed bleeding.51,52 In contrast, location in the cecum was a significant risk factor for delayed bleeding in terms of tumor location.53 In a meta-analysis including 22 studies, rectal location was a significant risk factor for delayed bleeding (OR, 3.55; 95% CI, 2.06–6.12).10 The rate of delayed bleeding was reported as high as 6.6%.52 In a meta-analysis for C-ESD, the incidence of major delayed bleeding requiring hemostatic intervention was 2.1% among 13,833 tumors.54 Interestingly, the incidence of delayed bleeding after C-ESD was not higher than that of postpolypectomy bleeding. Two meta-analyses reported that the risk of delayed bleeding was comparable between EMR and C-ESD.55,56 To prevent delayed bleeding after C-ESD, electrocoagulation for exposed vessels on the ulcer was recommended.57 Prophylactic clipping may prevent delayed bleeding after C-ESD. A meta-analysis reported that prophylactic clipping decreased the incidence of delayed bleeding (0.9%) compared to non-closure (5.2%, pooled ORs, 0.19; 95% CI, 0.08–0.49).47 Thus, prophylactic clipping can be considered in cases with high risk of delayed bleeding.
Delayed perforation
Delayed colorectal perforation is defined as colorectal perforation that develops or is recognized after completion of ESD without intraprocedural (endoscopic) or immediate postprocedural (radiological) evidence of perforation. Delayed perforation after C-ESD is rarer than micro- or intraprocedural perforation. According to a multicenter study conducted in Korea, the overall incidence of perforation related to C-ESD was 6.5% (134/2,046). However, the incidence of delayed perforation within this cohort was 0.1% (3/2,046).5 A prior prospective multicenter study in Japan reported that the delayed perforation rate after C-ESD was 0.4% (4/1,111), while two of these cases were surgically treated.58 In a meta-analysis, the incidence of delayed perforation was reported to be 0.22%,54 which was lower than that of PECS. However, most studies included in this meta-analysis were retrospective. A multicenter randomized controlled trial aimed to prevent PECS in Japan reported that the rate of delayed perforation was 3.9% (6/155 C-ESD cases).59 In this study, all patients who were diagnosed with PECS underwent abdominal computed tomography (CT), and delayed perforation was divided into minor (PECS with periluminal air) and major (PECS with intra-abdominal free air). All cases of delayed perforation in this study were minor PECS. The incidence of delayed perforation was overestimated if PECS with periluminal air was considered as “minor” delayed perforation. However, as none of the minor delayed perforations in this study required surgery, PECS with periluminal air should be considered as a subtype of PECS rather than delayed perforation in clinical practice. Nonetheless, severe PECS and delayed perforation may present with symptoms suggestive of peritonitis; hence, differentiating between these two adverse events may be challenging. Therefore, when delayed perforation is clinically suspected, abdominal CT should be performed immediately. CT may reveal intraperitoneal free air and intra-abdominal changes secondary to acute peritonitis. Although delayed perforations with minor symptoms can be managed with conservative treatment, including antibiotics and fasting, a considerable proportion of delayed perforations requires surgical treatment. Therefore, in cases of delayed perforation, emergency contact with the surgeon is essential for therapeutic decision making.
CONCLUSIONS
C-ESD is a technically challenging procedure. Major complications of C-ESD can be categorized as intraprocedural and postprocedural adverse events. With advancements in techniques and devices, the perforation rate has been reduced recently. To minimize perforations, C-ESD should be performed using a standardized technique. The endoscopist’s experience is the most important factor in perforation; hence, supervision by experts is essential when the procedure is performed by novices. C-ESD should be performed by physicians who can manage perforations in specialized centers where surgical treatment is possible. Furthermore, physicians should be familiar with postprocedural and intraprocedural complications. The incidence rate of PECS is higher than that of delayed perforation; however, PECS can be managed conservatively in most cases. Hence, PECS should be differentially diagnosed from delayed perforation to avoid unnecessary surgical treatment. However, to prevent delays in surgical treatment when indicated, surgical consultation is required for therapeutic decision making in patients with severe PECS and perforation.
Footnotes
Conflicts of Interest
The authors have no potential conflicts of interest.
Funding
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (MSIT) (grant number NRF-2021R1G1A1094049).
Author Contributions
Conceptualization: DHY; Data curation: TGG; Formal analysis: TGG; Investigation: TGG; Methodology: TGG; Supervision; DHY; Validation: DHY; Writing–original draft: TGG; Writing–review & editing: all authors.
REFERENCES
- 1.Saunders BP, Tsiamoulos ZP. Endoscopic mucosal resection and endoscopic submucosal dissection of large colonic polyps. Nat Rev Gastroenterol Hepatol. 2016;13:486–496. doi: 10.1038/nrgastro.2016.96. [DOI] [PubMed] [Google Scholar]
- 2.Kim ER, Chang DK. Management of complications of colorectal submucosal dissection. Clin Endosc. 2019;52:114–119. doi: 10.5946/ce.2019.063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chow CWS, Fung TLD, Chan PT, et al. Endoscopic submucosal dissection for colorectal polyps: outcome determining factors. Surg Endosc. 2023;37:1293–1302. doi: 10.1007/s00464-022-09672-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tamaru Y, Oka S, Tanaka S. Prevention and management of spouting bleeding during endoscopic submucosal dissection for large subpedunculated-type colonic tumor. Dig Endosc. 2018;30:128–129. doi: 10.1111/den.12975. [DOI] [PubMed] [Google Scholar]
- 5.Hong SN, Byeon JS, Lee BI, et al. Prediction model and risk score for perforation in patients undergoing colorectal endoscopic submucosal dissection. Gastrointest Endosc. 2016;84:98–108. doi: 10.1016/j.gie.2015.12.011. [DOI] [PubMed] [Google Scholar]
- 6.Fuccio L, Hassan C, Ponchon T, et al. Clinical outcomes after endoscopic submucosal dissection for colorectal neoplasia: a systematic review and meta-analysis. Gastrointest Endosc. 2017;86:74–86. doi: 10.1016/j.gie.2017.02.024. [DOI] [PubMed] [Google Scholar]
- 7.Takamaru H, Saito Y, Yamada M, et al. Clinical impact of endoscopic clip closure of perforations during endoscopic submucosal dissection for colorectal tumors. Gastrointest Endosc. 2016;84:494–502. doi: 10.1016/j.gie.2016.01.014. [DOI] [PubMed] [Google Scholar]
- 8.Kamigaichi Y, Oka S, Tanaka S, et al. Factors for conversion risk of colorectal endoscopic submucosal dissection: a multicenter study. Surg Endosc. 2022;36:5698–5709. doi: 10.1007/s00464-022-09250-6. [DOI] [PubMed] [Google Scholar]
- 9.Kang DU, Choi Y, Lee HS, et al. Endoscopic and clinical factors affecting the prognosis of colorectal endoscopic submucosal dissection-related perforation. Gut Liver. 2016;10:420–428. doi: 10.5009/gnl15252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Santos JB, Nobre MRC, Oliveira CZ, et al. Risk factors for adverse events of colorectal endoscopic submucosal dissection: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2021;33(1S Suppl 1):e33–e41. doi: 10.1097/MEG.0000000000001994. [DOI] [PubMed] [Google Scholar]
- 11.Kuroha M, Shiga H, Kanazawa Y, et al. Factors associated with fibrosis during colorectal endoscopic submucosal dissection: does pretreatment biopsy potentially elicit submucosal fibrosis and affect endoscopic submucosal dissection outcomes? Digestion. 2021;102:590–598. doi: 10.1159/000510145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Odagiri H, Yasunaga H. Complications following endoscopic submucosal dissection for gastric, esophageal, and colorectal cancer: a review of studies based on nationwide large-scale databases. Ann Transl Med. 2017;5:189. doi: 10.21037/atm.2017.02.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Misumi Y, Nonaka K. Prevention and management of complications and education in endoscopic submucosal dissection. J Clin Med. 2021;10:2511. doi: 10.3390/jcm10112511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hotta K, Oyama T, Shinohara T, et al. Learning curve for endoscopic submucosal dissection of large colorectal tumors. Dig Endosc. 2010;22:302–306. doi: 10.1111/j.1443-1661.2010.01005.x. [DOI] [PubMed] [Google Scholar]
- 15.Sakamoto T, Saito Y, Fukunaga S, et al. Learning curve associated with colorectal endoscopic submucosal dissection for endoscopists experienced in gastric endoscopic submucosal dissection. Dis Colon Rectum. 2011;54:1307–1312. doi: 10.1097/DCR.0b013e3182282ab0. [DOI] [PubMed] [Google Scholar]
- 16.Yang DH, Jeong GH, Song Y, et al. The feasibility of performing colorectal endoscopic submucosal dissection without previous experience in performing gastric endoscopic submucosal dissection. Dig Dis Sci. 2015;60:3431–3441. doi: 10.1007/s10620-015-3755-0. [DOI] [PubMed] [Google Scholar]
- 17.Jung Y. Endoscopic management of iatrogenic colon perforation. Clin Endosc. 2020;53:29–36. doi: 10.5946/ce.2019.061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paspatis GA, Arvanitakis M, Dumonceau JM, et al. Diagnosis and management of iatrogenic endoscopic perforations: European Society of Gastrointestinal Endoscopy (ESGE) Position Statement: update 2020. Endoscopy. 2020;52:792–810. doi: 10.1055/a-1222-3191. [DOI] [PubMed] [Google Scholar]
- 19.Okamoto Y, Oka S, Tanaka S, et al. Indications and outcomes of colorectal hybrid endoscopic submucosal dissection: a large multicenter 10-year study. Surg Endosc. 2022;36:1894–1902. doi: 10.1007/s00464-021-08471-5. [DOI] [PubMed] [Google Scholar]
- 20.Romagnuolo J. Endoscopic clips: past, present and future. Can J Gastroenterol. 2009;23:158–160. doi: 10.1155/2009/515937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galloro G, Zullo A, Luglio G, et al. Endoscopic clipping in non-variceal upper gastrointestinal bleeding treatment. Clin Endosc. 2022;55:339–346. doi: 10.5946/ce.2021.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Morgan SA, Sapci I, Hrabe JE, et al. Endoscopic submucosal dissection with closure of colonic perforation using over-the-scope clip system. Dis Colon Rectum. 2019;62:379. doi: 10.1097/DCR.0000000000001161. [DOI] [PubMed] [Google Scholar]
- 23.Kuwabara H, Chiba H, Tachikawa J, et al. Endoscopic closure using over-the-scope clip for delayed colonic perforation after hybrid endoscopic submucosal dissection. Endoscopy. 2020;52:E368–E369. doi: 10.1055/a-1134-4508. [DOI] [PubMed] [Google Scholar]
- 24.Wei MT, Ahn JY, Friedland S, et al. Over-the-Scope clip in the treatment of gastrointestinal leaks and perforations. Clin Endosc. 2021;54:798–804. doi: 10.5946/ce.2021.250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Matthes K, Jung Y, Kato M, et al. Efficacy of full-thickness GI perforation closure with a novel over-the-scope clip application device: an animal study. Gastrointest Endosc. 2011;74:1369–1375. doi: 10.1016/j.gie.2011.07.057. [DOI] [PubMed] [Google Scholar]
- 26.Lee JH, Kedia P, Stavropoulos SN, et al. AGA clinical practice update on endoscopic management of perforations in gastrointestinal tract: expert review. Clin Gastroenterol Hepatol. 2021;19:2252–2261. doi: 10.1016/j.cgh.2021.06.045. [DOI] [PubMed] [Google Scholar]
- 27.Nakagawa Y, Nagai T, Soma W, et al. Endoscopic closure of a large ERCP-related lateral duodenal perforation by using endoloops and endoclips. Gastrointest Endosc. 2010;72:216–217. doi: 10.1016/j.gie.2009.10.040. [DOI] [PubMed] [Google Scholar]
- 28.Nomura T, Kobayashi M, Morikawa T, et al. Clip-fixed endoloop: an efficacious new method for mucosal defect closure. Endoscopy. 2018;50:E126–E127. doi: 10.1055/s-0044-101025. [DOI] [PubMed] [Google Scholar]
- 29.Ryu JY, Park BK, Kim WS, et al. Endoscopic closure of iatrogenic colon perforation using dual-channel endoscope with an endoloop and clips: methods and feasibility data (with videos) Surg Endosc. 2019;33:1342–1348. doi: 10.1007/s00464-018-06616-7. [DOI] [PubMed] [Google Scholar]
- 30.Abe S, Wu SY, Ego M, et al. Efficacy of current traction techniques for endoscopic submucosal dissection. Gut Liver. 2020;14:673–684. doi: 10.5009/gnl19266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hu X, Xu QW, Liu WH. Endoscopic loop string-assisted clip suturing closure of large mucosal defects after endoscopic submucosal dissection in the sigmoid colon. Am J Gastroenterol. 2020;115:15. doi: 10.14309/ajg.0000000000000505. [DOI] [PubMed] [Google Scholar]
- 32.Repici A, Hassan C, De Paula Pessoa D, et al. Efficacy and safety of endoscopic submucosal dissection for colorectal neoplasia: a systematic review. Endoscopy. 2012;44:137–150. doi: 10.1055/s-0031-1291448. [DOI] [PubMed] [Google Scholar]
- 33.Sakamoto T, Mori G, Yamada M, et al. Endoscopic submucosal dissection for colorectal neoplasms: a review. World J Gastroenterol. 2014;20:16153–16158. doi: 10.3748/wjg.v20.i43.16153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chiapponi C, Stocker U, Körner M, et al. Emergency percutaneous needle decompression for tension pneumoperitoneum. BMC Gastroenterol. 2011;11:48. doi: 10.1186/1471-230X-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Raju GS, Saito Y, Matsuda T, et al. Endoscopic management of colonoscopic perforations (with videos) Gastrointest Endosc. 2011;74:1380–1388. doi: 10.1016/j.gie.2011.08.007. [DOI] [PubMed] [Google Scholar]
- 36.Katano T, Shimura T, Nomura S, et al. Optimal definition of coagulation syndrome after colorectal endoscopic submucosal dissection: a post hoc analysis of randomized controlled trial. Int J Colorectal Dis. 2021;36:1479–1485. doi: 10.1007/s00384-021-03921-x. [DOI] [PubMed] [Google Scholar]
- 37.Ito S, Hotta K, Imai K, et al. Risk factors of post-endoscopic submucosal dissection electrocoagulation syndrome for colorectal neoplasm. J Gastroenterol Hepatol. 2018;33:2001–2006. doi: 10.1111/jgh.14302. [DOI] [PubMed] [Google Scholar]
- 38.Cha JM, Lim KS, Lee SH, et al. Clinical outcomes and risk factors of post-polypectomy coagulation syndrome: a multicenter, retrospective, case-control study. Endoscopy. 2013;45:202–207. doi: 10.1055/s-0032-1326104. [DOI] [PubMed] [Google Scholar]
- 39.Jung D, Youn YH, Jahng J, et al. Risk of electrocoagulation syndrome after endoscopic submucosal dissection in the colon and rectum. Endoscopy. 2013;45:714–717. doi: 10.1055/s-0033-1344555. [DOI] [PubMed] [Google Scholar]
- 40.Lee SP, Sung IK, Kim JH, et al. A randomized controlled trial of prophylactic antibiotics in the prevention of electrocoagulation syndrome after colorectal endoscopic submucosal dissection. Gastrointest Endosc. 2017;86:349–357. doi: 10.1016/j.gie.2016.11.022. [DOI] [PubMed] [Google Scholar]
- 41.Kim SJ, Kim SY, Lee J. Prognosis and risk factors of electrocoagulation syndrome after endoscopic submucosal dissection in the colon and rectum. Large cohort study. Surg Endosc. 2022;36:6243–6249. doi: 10.1007/s00464-022-09060-w. [DOI] [PubMed] [Google Scholar]
- 42.Arimoto J, Higurashi T, Kato S, et al. Risk factors for post-colorectal endoscopic submucosal dissection (ESD) coagulation syndrome: a multicenter, prospective, observational study. Endosc Int Open. 2018;6:E342–E349. doi: 10.1055/s-0044-101451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Shichijo S, Takeuchi Y, Shimodate Y, et al. Performance of perioperative antibiotics against post-endoscopic submucosal dissection coagulation syndrome: a multicenter randomized controlled trial. Gastrointest Endosc. 2022;95:349–359. doi: 10.1016/j.gie.2021.08.025. [DOI] [PubMed] [Google Scholar]
- 44.Osada T, Sakamoto N, Ritsuno H, et al. Closure with clips to accelerate healing of mucosal defects caused by colorectal endoscopic submucosal dissection. Surg Endosc. 2016;30:4438–4444. doi: 10.1007/s00464-016-4763-7. [DOI] [PubMed] [Google Scholar]
- 45.Yamasaki Y, Takeuchi Y, Iwatsubo T, et al. Line-assisted complete closure for a large mucosal defect after colorectal endoscopic submucosal dissection decreased post-electrocoagulation syndrome. Dig Endosc. 2018;30:633–641. doi: 10.1111/den.13052. [DOI] [PubMed] [Google Scholar]
- 46.Lee SP, Sung IK, Kim JH, et al. Effect of prophylactic endoscopic closure for an artificial ulceration after colorectal endoscopic submucosal dissection: a randomized controlled trial. Scand J Gastroenterol. 2019;54:1291–1299. doi: 10.1080/00365521.2019.1674918. [DOI] [PubMed] [Google Scholar]
- 47.Liu M, Zhang Y, Wang Y, et al. Effect of prophylactic closure on adverse events after colorectal endoscopic submucosal dissection: a meta-analysis. J Gastroenterol Hepatol. 2020;35:1869–1877. doi: 10.1111/jgh.15148. [DOI] [PubMed] [Google Scholar]
- 48.Albéniz E, Montori S, Rodríguez de Santiago E, et al. Preventing postendoscopic mucosal resection bleeding of large nonpedunculated colorectal lesions. Am J Gastroenterol. 2022;117:1080–1088. doi: 10.14309/ajg.0000000000001819. [DOI] [PubMed] [Google Scholar]
- 49.Tanaka S, Kashida H, Saito Y, et al. Japan Gastroenterological Endoscopy Society guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2020;32:219–239. doi: 10.1111/den.13545. [DOI] [PubMed] [Google Scholar]
- 50.Seo M, Song EM, Cho JW, et al. A risk-scoring model for the prediction of delayed bleeding after colorectal endoscopic submucosal dissection. Gastrointest Endosc. 2019;89:990–998. doi: 10.1016/j.gie.2018.11.029. [DOI] [PubMed] [Google Scholar]
- 51.Chiba H, Ohata K, Tachikawa J, et al. Delayed bleeding after colorectal endoscopic submucosal dissection: when is emergency colonoscopy needed? Dig Dis Sci. 2019;64:880–887. doi: 10.1007/s10620-018-5310-2. [DOI] [PubMed] [Google Scholar]
- 52.Terasaki M, Tanaka S, Shigita K, et al. Risk factors for delayed bleeding after endoscopic submucosal dissection for colorectal neoplasms. Int J Colorectal Dis. 2014;29:877–882. doi: 10.1007/s00384-014-1901-3. [DOI] [PubMed] [Google Scholar]
- 53.Suzuki S, Chino A, Kishihara T, et al. Risk factors for bleeding after endoscopic submucosal dissection of colorectal neoplasms. World J Gastroenterol. 2014;20:1839–1845. doi: 10.3748/wjg.v20.i7.1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Akintoye E, Kumar N, Aihara H, et al. Colorectal endoscopic submucosal dissection: a systematic review and meta-analysis. Endosc Int Open. 2016;4:E1030–E1044. doi: 10.1055/s-0042-114774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Tajika M, Niwa Y, Bhatia V, et al. Comparison of endoscopic submucosal dissection and endoscopic mucosal resection for large colorectal tumors. Eur J Gastroenterol Hepatol. 2011;23:1042–1049. doi: 10.1097/MEG.0b013e32834aa47b. [DOI] [PubMed] [Google Scholar]
- 56.Lim XC, Nistala KRY, Ng CH, et al. Endoscopic submucosal dissection vs endoscopic mucosal resection for colorectal polyps: a meta-analysis and meta-regression with single arm analysis. World J Gastroenterol. 2021;27:3925–3939. doi: 10.3748/wjg.v27.i25.3925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Tanaka S, Kashida H, Saito Y, et al. JGES guidelines for colorectal endoscopic submucosal dissection/endoscopic mucosal resection. Dig Endosc. 2015;27:417–434. doi: 10.1111/den.12456. [DOI] [PubMed] [Google Scholar]
- 58.Saito Y, Uraoka T, Yamaguchi Y, et al. A prospective, multicenter study of 1111 colorectal endoscopic submucosal dissections (with video) Gastrointest Endosc. 2010;72:1217–1225. doi: 10.1016/j.gie.2010.08.004. [DOI] [PubMed] [Google Scholar]
- 59.Nomura S, Shimura T, Katano T, et al. A multicenter, single-blind randomized controlled trial of endoscopic clipping closure for preventing coagulation syndrome after colorectal endoscopic submucosal dissection. Gastrointest Endosc. 2020;91:859–867. doi: 10.1016/j.gie.2019.11.030. [DOI] [PubMed] [Google Scholar]