Highlights
-
•
This cross-sectional study involved 38 refugee families from Syria resettled in Denmark.
-
•
55% of the refugees aged ≥35 years reported less good or bad health (20% for Danes).
-
•
Wellbeing score was lower and decreased with age in refugees compared with Danes.
-
•
38% of the refugees reported to experience loneliness (6.6% among Danes).
-
•
Up to 73% of the adult refugees experienced pain and somatic symptoms.
Keywords: Refugee health, Migrant health, Health care, Wellbeing, Syria, Resettlement
Abstract
Aims
The aim was to evaluate self-reported health status and wellbeing in a well-defined group of refugee families from Syria 2–4 years after resettlement in Denmark, and, where possible, compare it with a Danish reference population. The purpose was to determine the need for specialized health care to resettled refugees.
Methods
This cross-sectional study involved 90 individuals from Syria aged 13–56 years. We used questionnaire survey to assess the general health and wellbeing in the study population in relation to a Danish reference population. Objective measurements of selected health indicators like overweight, hypertension and levels of cholesterol and blood glucose (HbA1c) were also determined for the study population.
Results
Mean wellbeing scores and the proportion of study participants rating their health as good were lower among the study participants compared with the Danish population for all age groups. The proportion of participants who reported often being alone against their will was significantly higher than among Danes, as was the proportion who had nobody to talk to when having problems. A significantly higher proportion of participants experienced various forms of pain or discomfort than in the Danish population. Overall, 23.6% and 3.4% of participants had elevated cholesterol and HbA1c levels, respectively, and the prevalence of overweight (BMI ≥ 25) was 70%. Hypertension was more frequent (16.2%) than in another refugee population in Denmark (9%).
Conclusions
The study demonstrated various mental and physical health challenges among the Syrian refugee families, and their health and wellbeing appeared to be substantially poorer as compared to the Danish reference population. The findings emphasize the need for systematic and specialized health care services at a municipality level to resettling refugees as a prerequisite for the refugees to become contributing citizens.
Introduction
The Syrian conflict in 2015 and the following situation referred to as the ‘refugee crisis’ resulted in more than 1.3 million individuals of different nationalities seeking asylum in Europe (Pew Research Center, 2016). Of these, 378,000 were refugees from Syria, accounting for 29% of all asylum seekers in Europe – the highest share of any nation. In October to December 2021, approximately 177,700 first time asylum seekers (non-EU citizens) applied for protection in EU countries (Eurostat Statistics Explained, 2022). This was a 13% increase compared to the preceding three months, and a 66% increase compared to the same period the previous year, indicating a continuous increase in the need for human protection in the European Region.
Refugees and migrants are diverse groups and have a variety of health needs, which may differ from those of the host population. Inadequate nutrition and exposure to high rates of infectious diseases, together with poor sanitary conditions and lack of access to care and medicine during migration, may affect refugees’ long-term health outcomes (Andersen et al., 2020; Maldari et al., 2019; Priebe et al., 2016). Moreover, their physical and mental health needs are closely related to experiences in the country of origin, their migration journey, entry and integration policies in the host country together with their living and working conditions (World Health Organization, 2022). The asylum process and waiting time for residence permit is further associated with long-term mental health problems (Laban et al., 2008).
A study of the health status among newly arrived refugee families from Syria resettled in Australia reported a low prevalence of infectious diseases (<10%), whereas a high prevalence of vitamin and micronutrient deficiency was observed (>60% among adults and >40% among children) (Maldari et al., 2019). Chronic diseases including cardiovascular disease, hypertension and chronic airways disease, were also high among adults (27% in women and 40% among men), as were the known risk factors smoking, overweight and obesity. Thus, 44% of the males and 8% of the females were smokers, and 72% of all adults were overweight or obese. Furthermore, 27% of the adults reported symptoms of anxiety, depressed mood and poor sleep. In a similar study of refugees resettled in Denmark, the majority reported headache (54%) or other pain (53%), and signs of posttraumatic stress disorder (PTSD) were also frequent (33%) (Andersen et al., 2020). A health evidence network synthesis report describes that PTSD is more common in refugees and asylum seekers than in host country populations, and the prevalence of depression in refugees who has been resettled for more than five years was also higher than in the host population (Priebe et al., 2016). Special attention should be paid to young individuals as traumatic experiences in childhood and youth life, such as war and parental separation, can lead to acquisition of physical, mental and behavioral problems (Hirani et al., 2016).
Despite recommendations from the World Health Organization (World Health Organization, 2023) and the European center for Disease Prevention and Control (European Centre for Disease Prevention and Control, 2018) to offer optional general health assessments to all migrants including refugees, the national guidelines in European countries presents great variation regarding how and to whom the health assessments are offered (Hvass and Weise, 2017). Previous Danish practice included voluntary general health assessments to asylum seekers as part of current integration policies, but in 2016 these were made optional for the municipalities. Today, only the two largest municipalities, Copenhagen and Aarhus, systematically continue to offer health assessments to newly resettled refugees (Andersen et al., 2020; Hvass et al., 2021). This means that a large number of refugees may encounter the Danish health care system for the first time at a point where they have an acute need for health care. This may be a stressful situation, which is likely to postpone the first contact and delay timely care, potentially leading to increased cost to the healthcare system.
The present study was nested in an intervention project involving refugee families from Syria, who resettled in Denmark in the period 2015 – 2018. The aim of this cross-sectional study was to evaluate self-reported health status and wellbeing in a well-defined group of refugee families from Syria 2–4 years after resettlement in Denmark, and, where possible, compare it with a Danish reference population. A questionnaire was developed as a tool to investigate the health status. The questionnaire was constructed to contain subsets of questions from the questionnaire that forms basis of the Danish national and regional health surveys (Rosendahl Jensen et al., 2018; Blaakilde et al., 2018), thus allowing comparisons. In addition, objective measures of cholesterol, blood glucose (HbA1c), blood pressure, and BMI were described for the study population. The study provides a perspective on refugees’ health status in relation to a host country population. Increasing evidence of refugees’ poor health several years after resettlement may accelerate appropriate future health care policies and draw attention to the need of specialized health care to refugees resettled in European countries.
Material and methods
Study participants and design
The study involved 38 refugee families from Syria resettled in a rural municipality of Denmark in the period 2015 – 2018. The families contained 169 individuals aged 0–56 years. Inclusion criteria were 1) having obtained asylum in Denmark, 2) being a resident in the municipality with age of 13 years or above, and 3) speaking and reading Arabic. The 38 families constituted more than 85% of all refugee families meeting the inclusion criteria in the municipality. Of the 169 individuals, 97 were 13 years of age or older and thereby met the inclusion criteria for participating in a health assessment, which included a questionnaire survey and measurement of blood pressure and biomarkers in venous blood samples.
Based on the questionnaire survey, 66% reported Arabic and 24% Kurdish as their mother tongue, indicating diversity in the participants’ self-perception of being Arabs or Kurds. The remaining 10% reported their mother tongue to be twofold, Arabic and Kurdish or Arabic and Turkish. Adult family members arrived in Denmark as refugees or as part of family reunification. Several adolescents had fled with one or more adults, most often male family members, whereas others had been reunified with their family in Denmark together with their mother and smaller siblings.
Questionnaire survey
The questionnaire contained themes about physical and mental health, wellbeing, stress, loneliness, and pain or discomfort. Furthermore, information on demographics, language, school attendance in the home country, duration of residence in Denmark, height, weight and smoking was collected. The questionnaire was reviewed by bilingual (Arabic and Danish) volunteers with Middle East backgrounds to assess whether the themes and questions were meaningful to the study population. Subsequently, the questionnaire was translated into Arabic by a professional interpreter from the Danish Refugee Council and reviewed by a professional proofreader. Each question appeared in both Danish and Arabic. After translation, the questionnaire was face-validated through tests and discussions with bilingual project staff who would be involved in the survey as interviewers. Thus, the survey was conducted using an interviewer-guided approach. Each participant was interviewed by a bilingual interviewer with similar cultural background as the participant, and the interviewer filled in the questionnaire. Prior to the survey, the interviewers were trained in the interview procedure to secure inter-interviewer conformity. The interviewer-guided approach with translated questions allowed the respondents to read the questions in the preferred language, and at the same time, receive an explicit explanation of each question, ensuring correct understanding of the meaning. The survey was conducted in March 2019.
Self-rated health
Self-rated health was assessed using a single item question, which asked the participants to rate their overall health (physical and mental) with five response categories: ‘excellent’, ‘very good’, ’good’, ‘less good’, or ‘bad’. The question is part of the Danish health surveys (Rosendahl Jensen et al., 2018; Blaakilde et al., 2018). For comparison reasons, self-rated health was dichotomized into good (excellent, very good, good) or bad (less good and bad) health by collapsing the first three and last two response categories.
Wellbeing score
The Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS) (© NHS Health Scotland, University of Warwick and University of Edinburgh, 2006, all rights reserved) is a validated 14-items tool for measuring mental wellbeing with a good to excellent reliability level (Chronbach's alpha 0.91 in an adult population sample (Tennant et al., 2007) and 0.89 in school students aged 13–16 years (Clarke et al., 2011)). The scale is freely available on registration. A short version of the scale (SWEMWBS) containing seven items (Stewart-Brown et al., 2009) was used to investigate the participant's wellbeing. The 7-items scale consists entirely of positively worded questions with a total score ranging from 7 to 35 (Koushede et al., 2019). The original and short version of the scale has been translated into Danish according to recommendations by the World Health Organization for the translation and adaptation of scales (Koushede et al., 2019) and used in studies among Danish children (Rasmussen et al., 2015) and adults (Nielsen et al., 2017). An overview of the questions in the original and short version of the scale with the Danish translation, together with a further validation of the questionnaire for use in a Danish context, has been published by Koushede et al. (Koushede et al., 2019). Reliability estimates displayed high internal consistency for the original (WEMWBS Chronbach's alpha 0.94) and short (SWEMWBS Chronbach's alpha 0.88) version. The study concluded that both versions of the scale are valid and appropriate instruments to measure mental wellbeing in the Danish population (Koushede et al., 2019). The 7 items of the SWEMWBS used in this study are listed in box 1.
Box 1. Items in short version of Warwick-Edinbourgh Mental Wellbeing Scale.
-
1
I've been feeling optimistic about the future
-
2
I've been feeling useful
-
3
I've been feeling relaxed
-
4
I've been dealing with problems well
-
5
I've been thinking clearly
-
6
I've been feeling close to other people
-
7
I've been able to make up my own mind about things
Alt-text: Unlabelled box
The participants were asked to describe their experience with each of the statements over the past two weeks using the 5-point Likert scale from the original WEMWBS scale. The response categories were: “none of the time”, “rarely’”, “some of the time”, “often”, or “all of the time”. In the original 14-item WEMWBS, overall scores are calculated by summing the scores for each of the 14 items, with equal weights. Thus, a higher WEMWBS score indicates a higher level of mental wellbeing (Tennant et al., 2007). The SWEMWBS is scored similarly by calculating a sum score for the 7 items with final scores transformed to enhance scaling properties using a conversion table (available online) (Stewart-Brown, 2015a, 2015b).
Stress score
A modified version of the Perceived Stress Scale (Cohen et al., 1983) covering perceived stress and coping was used to assess the participant's stress level. The original scale contains 10 items each given a score from 0 to 4. Positive items are reversed and added up into a scale ranging from 0 to 40. Higher scores indicate higher levels of perceived stress. The perceived stress scale has been translated into Danish, and a validation study found good reliability estimates (Cronbach's alpha 0.84) and assessed the translated scale to be feasible for use in research settings (Eskildsen et al., 2015). After thorough interpretation of the Arabic translation by bilingual volunteers and interviewers, we decided to exclude two questions, as their meanings were assessed to be too close to two other questions. Thus, the scale was reduced to contain the eight items listed in box 2.
Box 2. Items in the modified perceived stress scale.
In the past month,
-
1
How often have you been upset because of something that happened unexpectedly?
-
2
How often have you felt that you were unable to control the important things in your life?
-
3
How often have you felt nervous and stressed?
-
4
How often have you felt that things were going your way?
-
5
How often have you found that you could not cope with all the things that you had to do?
-
6
How often have you been able to control irritations in your life?
-
7
How often have you been angered because of things that happened that were outside of your control?
-
8
How often have you felt difficulties were piling up so high that you could not overcome them?
Alt-text: Unlabelled box
The participants answered the questions on a 5-point scale: “never”, “almost never”, “sometimes”, “fairly often”, or “very often”. Due to omission of two questions, the actual scale ranged between 0 and 32. The positively worded items (4 and 6 on our modified scale) were reversed in scoring, and overall scores were summed up. The modified 8-item scale has not been validated.
Being alone
To examine the participant's loneliness, the question “Does it happen that you are alone despite that you most feel like being together with others?” was included. The response categories were a 4-point scale: “yes, often”, “yes, sometimes”, “yes, but rarely”, or “no”. Another question was “Do you have somebody to talk to if you have problems or need support?” with the four response categories: “yes, always”, “yes, mostly”, “yes, sometimes”, or “no, never or almost never”. Both questions are part of the Danish health surveys (Rosendahl Jensen et al., 2018; Blaakilde et al., 2018).
Pain or discomfort
The participant's pain or discomfort was assessed using eight items for recent symptoms. The participants were asked: “Within the past two weeks, have you been bothered by some of the mentioned forms of pain or discomfort?” and to which degree they had been bothered:
Pain or discomfort in shoulder or neck; Pain or discomfort in arms, hands, legs, knees, hips, or joints; Pain or discomfort in back or lower back; Fatigue; Headache; Difficulties sleeping; Sadness, depressed or unhappy; Concern, nervousness, unrest, anxiety. The response options were: ‘yes, very bothered’; ‘yes, a little bothered’, or ‘no’. The questions are part of the Danish health surveys (Rosendahl Jensen et al., 2018; Blaakilde et al., 2018).
Objective health assessment
All participants were offered a health assessment including measurement of height and weight, blood glucose (HbA1c), cholesterol and blood pressure. In connection with the questionnaire survey, venous blood samples were drawn by medical laboratory technologists from Zealand University Hospital, Køge.
Body mass index (BMI)
BMI (weight in kg/height in m2) was generated from measurements of height and weight. BMI categorization in underweight (<18.5), normal weight (18.5–24.9), overweight (25.0–29.9) and obesity (≥30) was based on limits for adults (18 years and above). As adolescents aged 16–17 years approach adult limits, this age group was included, whereas participants below 16 years of age were excluded from the analyses.
Cholesterol and HbA1c
Total cholesterol was measured using the Dimension Vista 1500 Analyzer (Siemens Healthcare, Erlangen, Germany) with variation coefficients of 4.4% at 2.7 mmol/L and 4.2% at 4.4 mmol/L. HbA1c was measured using the Tosoh HPLC G11 analyzer (Tosoh Bioscience, Inc., San Francisco, CA, USA) with CVs of 3.2% at 32 mmol/mol and 2.5% at 81 mmol/mol. Measurements were performed at Zealand University Hospital, Køge.
Blood pressure
Systolic and diastolic blood pressures were measured three times, and the mean was registered as the blood pressure. Hypertension was defined as a systolic pressure ≥ 140 mmHg or a diastolic pressure ≥ 90 mmHg (Sundhed.dk, 2023a).
Danish reference populations
The Danish National Health Surveys are based on randomly selected samples of the Danish population and are conducted every fourth year. The surveys are conducted for all five regions of Denmark, and parts of the data are made available in online data sources (Danskernes Sundhed, 2023) and printed reports. In the present study, we present different self-reported health indicators of the refugee study participants in relation to the Danish Health Survey for Region Zealand 2017 (Blaakilde et al., 2018), the region which the study municipality is part of. The health survey for Region Zealand 2017 included 19,134 participants aged 16 to 80+ years, with 50.5% women and 49.5% men responding to a self-administered questionnaire (34,000 were invited; response rate 56.3%, 60.0% for women and 52.0% for men). When regional data were not available, data at national level were used as reference (Rosendahl Jensen et al., 2018; Danskernes Sundhed, 2023).
Participant's wellbeing is presented in relation to The Danish Mental Health and Wellbeing Survey 2016 (Nielsen et al., 2017). In total, 10,250 individuals (49.3% males and 50.7% females) were contacted and 1852 females and 1656 males responded to a web-based survey resulting in a response rate of 36% for females and 33% for males (Koushede et al., 2019).
Ethics
The study was conducted in accordance with the Helsinki declaration. Informed consent was obtained from all participants. To secure informed consent, all oral and written information was translated into Arabic. Adolescents received oral and written information together with their parents in an easily accessible phrasing. Parents gave consent for their children's (13–17 years) participation. Furthermore, as part of the recruitment procedure, all families were payed a home visit with the opportunity to ask questions. At the survey and sample collection, all participants were reminded that participation was voluntary. All participants received their results on biomarker levels, and individuals with elevated levels of cholesterol, HbA1c and/or hypertension were advised how to contact their own general practitioner. Ethical approval was obtained from the Region Zealand's Committee on Health Research Ethics (SJ-715).
Statistical methods
The statistical analyses were performed using Stata (Stata/MP 15.1). The χ2 test was used to test for differences in proportions, and the student's t-test was used to test for differences in means between two groups. Differences in means between multiple groups were tested using one-way ANOVA, and the Tukey post hoc test was used for pairwise comparisons. Tests for differences in proportions between the refugee study sample and the Danish reference population were performed using binomial probability test. We tested the null hypothesis that there was no difference between the two samples. Alpha level for all tests were set at p < 0.05, two-tailed.
Results
Participant characteristics
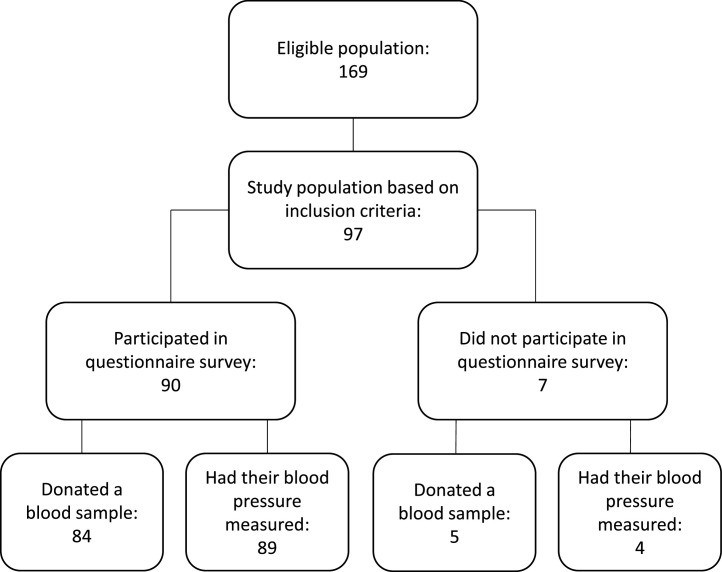
The study involved 38 refugee families from Syria resettled in a rural municipality of Denmark in the period 2015 – 2018. The families contained 169 individuals aged 0–56 years. Of the 169 individuals, 97 were 13 years of age or older and thereby met the inclusion criteria for participating in a health assessment, which included a questionnaire survey and measurement of blood pressure and biomarkers in venous blood samples. Fig. 1 shows a flowchart of the eligible population, the study population, and those who completed the questionnaire survey and measurements. Thus, 90 individuals completed the questionnaire, and data on biomarkers were available from 89 individuals, whereas blood pressure was available from 93 individuals. Characteristics of the 90 individuals participating in the questionnaire survey are given in Table 1. The median age was 32.5 years (range 13–56 years), 32 years for females and 33 years for males. Forty-six (51.1%) participants were females. The majority reported their mother tongue to be Arabic. Twenty-one (45.6%) of the females and 14 (31.8%) of the males had more than 10 years school attendance in their home country. Fourteen (30%) of the females and 23 (52%) of the males were smokers, and 29 (73%) of the females and 20 (67%) of the males aged 16 years or above were overweight or obese (BMI ≥ 25). The majority had been residents in Denmark for 2–4 years.
Fig. 1.
Flowchart showing the eligible population, the study population and completion of questionnaire and measurements.
Table 1.
Characteristics of the study participants. N = 90.
| n | % | |
|---|---|---|
| Sex | ||
| Females | 46 | 51.1 |
| Males | 44 | 48.9 |
| Age (years) | ||
| Adolecents (13–17) | 24 | 26.7 |
| Adults (18–56) | 66 | 73.3 |
| 13–15 | 19 | 21.1 |
| 16–24 | 11 | 12.2 |
| 25–34 | 22 | 24.4 |
| 35–44 | 27 | 30.0 |
| 45–56 | 11 | 12.2 |
| Mother tongue | ||
| Arabic | 59 | 65.6 |
| Kurdish | 22 | 24.4 |
| Arabic, Kurdish | 7 | 7.8 |
| Arabic, Turkish | 2 | 2.2 |
| School attendance in home country | ||
| 10 years or less | 55 | 61.1 |
| More than 10 years | 35 | 38.9 |
| Residence in Denmark | ||
| Less than 2 years | 3 | 3.3 |
| 2–4 years | 80 | 88.9 |
| More than 4 years | 7 | 7.8 |
| Smoking | 37 | 41.1 |
| BMI categorya | ||
| Underweight | 1 | 1.4 |
| Normal weight | 20 | 28.6 |
| Overweight | 26 | 37.1 |
| Obese | 23 | 32.9 |
Participants aged 16 years or above with measures on height and weight (n = 70).
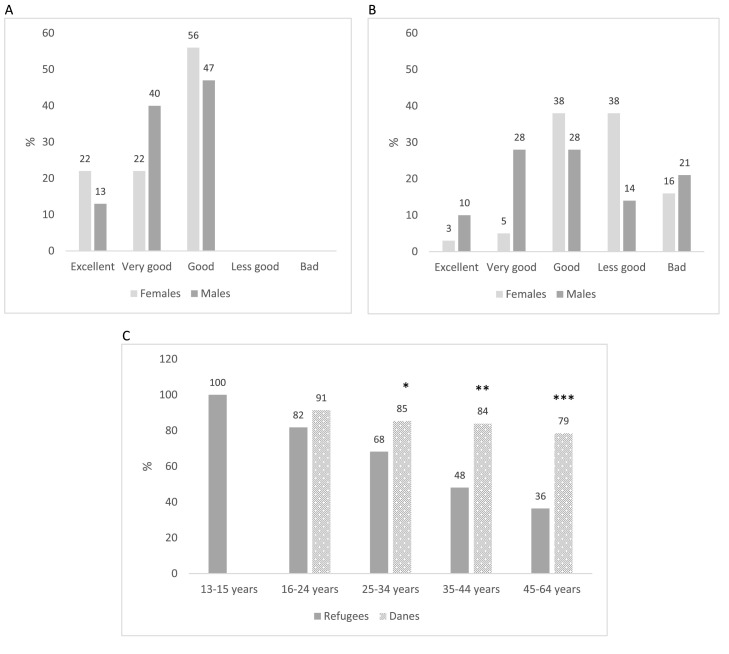
Self-rated health
Fig. 2A and B show the self-rated health among adolescent and adult study participants. No adolescents rated their health as less good or bad (Fig. 2A). More boys than girls reported their health to be very good, whereas more girls than boys reported an excellent or good health. The overall differences were, however, not statistically significant (p = 0.64). Among adult women and men there was a significant difference in self-rated health (p = 0.031). Overall, 45.5% reported their health to be less god or bad. One-third (33.3%) had rated their health as good, whereas 21.2% reported it to be very good or excellent. A higher proportion of women (54.0%) than men (34.5%) rated their health as less good or bad, and a lower proportion of women (8.1%) than men (37.9%) rated their health as very good or excellent (Fig. 2B). Thus, adult women generally reported their health as less good compared with men.
Fig. 2.
Self-rated health among adolecents aged 13–17 years (n = 24) (A) and adults aged 18 years and above (n = 66) (B). Proportion of study participants who rated their health as excellent, very good or good in relation to a Danish reference population (C).
Study participants: 13–15 years: n = 19; 16–24 years: n = 11; 25–34 years: n = 22; 35–44 years: n = 27; 45–64 years: n = 11.
Danish population: 16–24 years: n = 1870; 25–34 years: n = 1550; 35–44 years: n = 2720; 45–64 years: n = 8160. Proportions and n values reported in online data source (Danskernes Sundhed).
*P<0.05, **p<0.001, ***p<0.01 versus the Danish reference population in same age group using binomial probability test.
For comparison, the health rates good, very good and excellent were collapsed and presented in relation to a Danish reference population from Region Zealand 2017 (Fig. 2C) (Blaakilde et al., 2018). The proportion of participants reporting their health to be good, very good, or excellent was higher in the younger age groups and lower in the elder age groups (p = 0.001) and was significantly lower among the refugee study participants than in the Danish population in all age group except 16–24 years.
Wellbeing
In Table 2, mental wellbeing scores among the participants are presented together with scores from a Danish reference population reported in The Danish Mental Health and Wellbeing Survey 2016 (Koushede et al., 2019; Nielsen et al., 2017). In the refugee sample, the overall mean SWEMWBS score was 22.0 (SD 0.6) with significantly different scores across the four age groups (p < 0.001). A post hoc test showed that the eldest age group had a significantly lower mean score compared with the younger groups (45–64 years vs. 13–15 years: p < 0.001; 45–64 years vs. 16–25 years: p = 0.001, and 45–64 years vs. 26–44 years: p = 0.002). None of the other combinations were statistically significant. In contrast, the Danish study reported a mean SWEMWBS score of 26.4 (SD 4.3), and mean scores seemed to be slightly higher in elder age groups compared to younger groups.
Table 2.
Mental wellbeing scores among the study participants and a Danish reference population by sex and age groups.
| Category | n | SWEMWBSa | SD | |
|---|---|---|---|---|
| Refugees | Overall | 85 | 22.0 | 0.6 |
| Femalesb | 45 | 21.7 | 0.8 | |
| Males | 40 | 22.3 | 0.9 | |
| 13–15 yearsc | 19 | 25.4 | 1.0 | |
| 16–25 years | 11 | 24.5 | 1.1 | |
| 26–44 years | 46 | 21.0 | 0.7 | |
| 45–64 years | 9 | 16.7 | 2.2 | |
| Danesd | Overall | 3.500 | 26.4 | 4.3 |
| Femalese | 1852 | 24.1 | 3.9 | |
| Males | 1656 | 24.3 | 3.8 | |
| 13–15 years | NA | NA | NA | |
| 16–25 years | 319 | 25.8 | NA | |
| 26–44 years | 735 | 26.1 | NA | |
| 45–64 years | 1437 | 26.1 | NA |
SWEMWBS; The Short Warwick-Edinburgh Mental Well-being Scale (range 7–35). Mean and SD (standard deviation). SWEMWBS raw scores are converted to metric scores using a conversion table.
No significant difference between females and males (p = 0.615).
Significant difference in mean scores across age groups (p<0.001).
SWEMWBS scores reported in Koushede et al. (2019).
No significant difference between females and males (p = 0.164) (Koushede et al., 2019).
Stress
Mean stress scores and 95% confidence intervals (CI), based on a modification of the Perceived Stress Scale (Cohen et al., 1983), are presented in Table 3. The overall mean score was 16.1 (CI 14.6 −17.6) (on a scale ranging from 0 to 32) with higher scores among females than males. The difference was, however, not statistically significant (p = 0.155). Mean scores differed significantly across the four age groups (p < 0.001). Post hoc tests showed a lower mean score in the youngest age group compared with the two eldest groups (13–15 years vs. 26–44 years: p < 0.001; 13–15 years vs. 45–56 years: p < 0.001), whereas other combinations were not statistically significant.
Table 3.
Stress scores among the study participants by sex and age groups.
| n | Stress scorea | 95% CI | p | |
|---|---|---|---|---|
| Overall | 87 | 16.1 | 14.6 – 17.6 | |
| Sex | ||||
| Females | 44 | 17.2 | 14.8 – 19.5 | 0.155 |
| Males | 43 | 15.0 | 13.1 – 16.9 | |
| Age (years)c | <0.001 | |||
| 13–15 | 18 | 10.6 | 7.61 – 13.6 | |
| 16–25 | 12 | 15.7 | 12.0 – 19.3 | |
| 26–44 | 46 | 17.1 | 15.1 – 19.1 | |
| 45–56 | 11 | 21.4 | 17.1 – 25.6 |
Mean stress score with 95% confidence interval (CI).
Being alone
The proportion of participants who answered “yes, often” to the question of whether they happen to be alone despite wanting to be together with others was 37.8%. There was no significant sex difference (39.1% females vs. 36.4% males, p = 0.133). As shown in Table 4, the proportion being alone was lowest in the youngest age group and higher in the elder age groups (ranging between 10.5% and 52.6%, p = 0.008). The overall proportion of participants who indicated to have nobody to talk to when having problems (answering “no, never or almost never”) was 20%. The proportion was significantly higher among females than males (23.8% vs. 11.4%, p = 0.03) and highest in the age group 16–34 years (24.2%). However, the difference between the three age groups was not statistically significant. Comparison with data in the Danish Health Survey for Region Zealand 2017 indicates that being alone against one's will is more frequent among refugee participants than in the Danish population. Thus, in the age group 16–34 years, the proportion of refugee participants being alone (36.4%) was more than three times higher than in the Danish survey (10.1%) (p<0.001), and in the age group 35–64 years it was almost 10 times higher (52.6% among refugees vs. 5.5% among Danes, p<0.001). Similarly, the proportion of refugees indicating to have nobody to talk to was higher than reported in the Danish survey (16–34 years: 24.2% among refugees vs. 5.6% among Danes, p<0.001; 35–64 years: 21.1% among refugees vs. 5.2% among Danes, p<0.001) (Table 4).
Table 4.
Proportion of individuals who are often alone despite a wish to be together with others and who have nobody to talk to when having problems.
| Being alone | Nobody to talk to when having problems | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Refugees | Danesc | p | Refugees | Danesc | p | |||||
| n | % | n | % | n | % | n | % | |||
| Overall | 90 | 37.8 | 12,810d | 6.6d | <0.001 | 90 | 20.0 | 12,850d | 5.3d | <0.001 |
| Age (years) | ||||||||||
| 13–15 | 19 | 10.5a | NA | NA | – | 19 | 10.5b | NA | NA | – |
| 16–34 | 33 | 36.4 | 2860 | 10.1 | <0.001 | 33 | 24.2 | 2870 | 5.6 | <0.001 |
| 35–64 | 38 | 52.6 | 9950 | 5.5 | <0.001 | 38 | 21.1 | 9980 | 5.2 | 0.001 |
Significant difference between age groups (p = 0.008).
No significant difference between age groups (p = 0.461).
Proportions and n values reported in online data source (Region Zealand 2017) (Danskernes Sundhed).
Age-matched (age groups >64 years omitted).
NA, not available.
Pain or discomfort
Table 5 gives the proportion of participants being very bothered by different forms of pain or discomfort in relation to data from Danish surveys. It should be noted that data on overall proportions reported for the Danish population are from the Danish Health Survey for Region Zealand 2017 (Blaakilde et al., 2018), whereas proportions in age groups represents data from the Danish National Health Survey 2017 including all regions of Denmark (Rosendahl Jensen et al., 2018). Thus, the age-stratified data in the Danish sample may be less comparable, and interpretations should be made with caution. Refugee study participants’ age ranged from 13 to 56 years, whereas participants in the Danish surveys were aged 16 to 80+ years.
Table 5.
Proportion of study participants who has been very bothered (answered yes, very bothered) by different forms of pain or discomfort in relation to a Danish reference. Percent.
| Refugees | Danes | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Alla | 13–15 years | 16–34 years | 35–44 years | 45–56 years | Allb | 13–15 years | 16–34c years | 35–44c years | 45–64c years | p* | |
| n = 89–90 | n = 19 | n = 33 | n = 26–27 | n = 11 | n = 19,134 | NA | NA | NA | NA | ||
| Fatigue | 43.8 | 15.8 | 36.4 | 61.5 | 72.7 | 21.8 | NA | 22.7 | 20.1 | 18.2 | <0.001 |
| Pain or discomfort in arms, hands, legs, knees, hips or joints | 24.7 | 5.26 | 24.2 | 30.8 | 45.4 | 21.0 | NA | 8.78 | 13.8 | 21.1 | 0.365 |
| Pain or discomfort in back or lower back | 32.2 | 15.8 | 24.2 | 51.9 | 36.4 | 18.6 | NA | 12.0 | 15.1 | 17.5 | 0.002 |
| Pain or discomfort in shoulder or neck | 23.6 | 0 | 21.2 | 42.3 | 27.3 | 17.8 | NA | 12.3 | 16.0 | 18.0 | 0.165 |
| Difficulty sleeping | 28.1 | 10.5 | 27.3 | 30.8 | 54.6 | 15.6 | NA | 13.6 | 12.2 | 15.3 | 0.003 |
| Headache | 28.1 | 10.5 | 18.2 | 50.0 | 36.4 | 8.90 | NA | 9.58 | 9.65 | 7.60 | <0.001 |
| Sadness, depressed, unhappy | 25.8 | 5.3 | 21.2 | 26.9 | 72.7 | 8.20 | NA | 9.45 | 7.20 | 6.80 | <0.001 |
| Concern, nervousness, unrest, anxiety | 27.0 | 10.5 | 24.2 | 30.8 | 54.6 | 7.40 | NA | 8.68 | 6.25 | 6.60 | <0.001 |
Data represents the entire study sample of refugees 2019 (n = 90; 13–56 years).
Data are reported in Blaakilde et al. (2018) and represents the entire survey sample (16–80+ years) of the Danish health survey for Region Zealand 2017.
Data are from the Danish National Health Survey 2017 (Rosendahl Jensen et al., 2018) as age-stratified data are not available in the health survey for Region Zealand 2017. Between 174,557 and 175,506 individuals aged 16 to 80+ years answered the 8 questions, but specific numbers in age groups are not available. The numbers are means of proportions reported for men and women. NA, not available.
Difference in overall proportions in the refugee study sample and the Danish reference population from Region Zealand 2017.
Overall, fatigue (43.8%) and pain or discomfort in the back or lower back (32.2%) were the most common conditions bothering the refugee participants followed by difficulty sleeping (28.1%); headache (28.1%); concern, nervousness, unrest, anxiety (27.0%); sadness, depressed, unhappy (25.8%); pain or discomfort in arms, hands, legs, knees, hips or joints (24.7%) and pain or discomfort in shoulder or neck (23.6%).
For most forms of pain or discomfort, more females than males reported to be very bothered. Thus, 60.9% of the females and 25.0% of the males (p = 0.001) were very bothered by fatigue (data not shown). Similar differences were reported for pain or discomfort in arms, hands, legs, knees, hips, or joints (37.0% females vs. 11.6% males, p = 0.006); pain or discomfort in shoulders or neck (34.8% females vs. 11.6% males, p = 0.010); headache (43.5% females vs. 11.6% males, p = 0.001); sadness, depressed, unhappy (34.8% females vs. 16.3% males, p = 0.046); and concern, nervousness, unrest, anxiety (37.0% females vs. 16.3% males, p = 0.028). In contrast, proportions of females and males being very bothered by pain or discomfort in back or lower back (37.0% females vs. 27.3% males, p = 0.326) and difficulty sleeping (34.8% females vs. 20.9% males, p = 0.146) were not significantly different.
For most forms of pain or discomfort, the proportion of participants being very bothered was lowest in the youngest age group (13–15 years) and highest in the eldest age group (45–56 years).
The overall proportion of all forms of pain or discomfort reported in the Danish survey (Blaakilde et al., 2018) varied between 7.4% and 21.8% and was thereby generally much lower than among the refugee participants (Table 5). Thus, the occurrence of headache (28.1% vs. 8.9%, p<0.001); sadness, depressed, unhappy (25.8% vs. 8.2%, p<0.001); and concern, nervousness, unrest and anxiety (27.0% vs 7.4%, p<0.001) was more than three times higher in the refugee study population. The occurrence of fatigue (43.8% vs. 21.8%, p<0.001), difficulty sleeping (28.1% vs. 15.5%, p = 0.003) and pain or discomfort in the back or lower back (32.2% vs. 18.6%, p = 0.002) was about twice as high. Likewise, the age-stratified proportion of refugees experiencing various pain or discomfort was remarkably higher (up to four times) than among similar age groups of Danes (Rosendahl Jensen et al., 2018).
Summary of comparisons of self-reported health indicators
Table 6 presents the overall differences in proportions and means of self-rated health, wellbeing, stress, loneliness, pain and somatic symptoms between the refugee study sample and the Danish reference populations. As measured by these health indicators, refugee's health condition was observed to be significantly poorer compared to the Danish populations with respect to 9 out of 11 compared indicators.
Table 6.
Summary of overall differences in self-rated health, wellbeing, stress, loneliness, pain and somatic symptoms between the refugee study sample and the Danish reference populations.
| Refugees | Danes | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | Mean | SD/CId | n | % | Mean | SD/CId | P | |
| Good self-rated healtha | 90 | 66.7 | – | – | 14,330 | 81.8 | – | – | 0.001 |
| Wellbeing score (SWEWBS)b | 85 | – | 22.0 | 0.6 | 3500 | – | 26.4 | 4.3 | – |
| Stress | 87 | – | 16.1 | 14.6 – 17.6 | NA | NA | NA | NA | – |
| Lonelinessa | |||||||||
| Being alone | 90 | 37.8 | – | – | 12,810 | 6.6 | – | – | <0.001 |
| Nobody to talk to when having problems | 90 | 20.0 | – | – | 12,850 | 5.3 | – | – | <0.001 |
| Pain and somatic symptomsc | |||||||||
| Fatigue | 90 | 43.8 | – | – | 19,134 | 21.8 | <0.001 | ||
| Pain or discomfort in arms, hands, legs, knees, hips or joints | 90 | 24.7 | – | – | 19,134 | 21.0 | – | – | 0.365 |
| Pain or discomfort in back or lower back | 90 | 32.2 | – | – | 19,134 | 18.6 | – | – | 0.002 |
| Pain or discomfort in shoulder or neck | 90 | 23.6 | – | – | 19,134 | 17.8 | – | – | 0.165 |
| Difficulty sleeping | 90 | 28.1 | – | – | 19,134 | 15.6 | – | – | 0.003 |
| Headache | 90 | 28.1 | – | – | 19,134 | 8.90 | – | – | <0.001 |
| Sadness, depressed, unhappy | 89 | 25.8 | – | – | 19,134 | 8.20 | – | – | <0.001 |
| Concern, nervousness, unrest, anxiety | 89 | 27.0 | – | – | 19,134 | 7.40 | – | – | <0.001 |
Proportions and n values for Danes are reported in online data source (Region Zealand 2017) (Danskernes Sundhed, 2023).
SWEMWBS score reported in Koushede et al. (2019).
Proportions and n values for Danes are reported in Blaakilde et al. (2018) and represents the entire survey sample (16–80+ years) of the Danish health survey for Region Zealand 2017.
Standard deviation (SD) and 95% confidence interval (CI).
BMI
Mean BMI of participants aged 16 – 56 years (n = 70) was 28.0 (SD: 0.6) with no significant difference between females (28.6; SD: 0.8) and males (27.3; SD: 0.9) (p = 0.317). BMI categorization is shown in Table 1. Zero% females and 3.3% males were underweight, 27.5% females and 30.0% males had normal weight, 37.5% females and 36.7% males were overweight, and 35.0% females and 30.0% males were obese. Information on BMI in the Danish Health Survey for Region Zealand 2017 (Blaakilde et al., 2018) is based on self-reported height and weight and shows that 2.4% were underweight, 41.6% had normal weight, 35.4% were overweight, and 20.6% were obese in the Danish sample. Among the study participants, the prevalence of overweight (BMI ≥ 25) was 70%, whereas this prevalence was 56% in the Danish sample.
Cholesterol and HbA1c
Valid measurements of total cholesterol and HbA1c were available from 89 individuals. The overall mean cholesterol concentration was 4.5 (SD 0.9) mmol/L (Table 7). Mean concentrations were significantly higher in elder age groups (35–56 years vs. 13–15 years, p<0.001; 35–56 years vs. 16–34 years, p<0.001; and 16–34 years vs. 13–15 years, p = 0.012). Overall, 23.6% of the participants had elevated cholesterol concentration (defined as >5 mmol/L according to national guidelines (Sundhed.dk, 2023b) with most cases in the eldest age group. There was no statistically significant differences between females and males with respect to mean cholesterol (p = 0.458).
Table 7.
Total cholesterol, HbA1c and hypertension among the study participants.
| Total cholesterol (mmol/L) | n | Mean (SD) | >5 mmol/La |
|---|---|---|---|
| All | 89 | 4.5 (0.9) | 21 (23.6%) |
| Females | 47 | 4.5 (0.7) | 10 (21.3%) |
| Males | 42 | 4.4 (1.2) | 11 (26.2%) |
| 13–15 years | 15 | 3.6 (0.7) | 1 (6.7%) |
| 16–34 years | 32 | 4.4 (0.7) | 6 (18.8%) |
| 35–56 years | 42 | 4.8 (1.0) | 14 (33.3%) |
| HbA1c (mmol/mol) | n | Mean (SD) | > 44 mmol/molb |
|---|---|---|---|
| All | 89 | 35.8 (8.5) | 3 (3.4%) |
| Females | 47 | 34.5 (3.9) | 0 (0%) |
| Males | 42 | 37.1 (8.4) | 3 (7.1%) |
| 13–15 years | 15 | 34.2 (2.9) | 0 (0%) |
| 16–34 years | 32 | 34.1 (3.5) | 0 (0%) |
| 35–56 years | 42 | 37.6 (8.6) | 3 (7.0%) |
| Hypertension | n | – | Systolic ≥ 140 mmHg or diastolic ≥ 90 mmHgc |
|---|---|---|---|
| All | 93 | – | 12 (12.9%) |
| Females | 47 | – | 4 (8.5%) |
| Males | 46 | – | 8 (17.4%) |
| 13–15 years | 19 | – | 0 (0%) |
| 16–34 years | 32 | – | 0 (0%) |
| 35–56 years | 42 | – | 12 (28.6%) |
Elevated total cholesterol defined as >5 mmol/L (Sundhed.dk, 2023b). Number (prevalence).
Elevated blood glucose defined as > 44 mmol/mol (Sundhed.dk, 2023c). Number (prevalence).
Cut-off for hypertension when using home blood pressure (Sundhed.dk, 2023a). Number (prevalence).
The overall mean HbA1c concentration was 35.8 (SD 8.5) mmol/mol (Table 7). Mean concentrations were significantly higher in the eldest age group compared to the younger groups (35–56 years vs. 13–15 years, p = 0.007, and 35–56 years vs. 16–34 years, p<0.006). There was no significant difference between the two youngest groups (p = 0.888). Overall, 3.4% had elevated HbA1c concentration (defined as > 44 mmol/mol (Sundhed.dk 2023c) with all cases present in the eldest age group. Mean HbA1c concentrations tended to be higher among males than females (p = 0.062).
Hypertension
Valid measurements of blood pressure were available from 93 individuals. The overall prevalence of hypertension was 12.9% with all cases in the age group 35–56 years (Table 7). Eight males (17.4%) and 4 females (8.5%) had hypertension (p = 0.202).
Discussion
We have evaluated the mental and physical health status in a well-defined group of Syrian refugee families resettled in a rural municipality of Denmark. We found adolescents’ health to be relatively good, whereas adults’ health appeared to be substantially poorer than in an age-matched Danish population from the same geographical region.
Self-reported mental and physical health
All adolescents rated their health as good (excellent, very good or good), whereas 45.5% of the adults rated their health as less good or bad. The proportion of participants with good health decreased with increasing age group and was significantly lower compared with Danish reference values for all age groups except the youngest group aged 16–24 years. This demonstrates a generally poor health among the refugee population that seems to be strongly affected by age.
The mean wellbeing score (SWEMWBS) was also lower than observed in a Danish population (22.0 among refugees vs. 26.4 among Danes). The lower SWEMWBS scores across higher age groups was in contrast to a tendency of an increase in SWEMWBS scores with increasing age in the Danish population, indicating that age-related life factors may affect self-perceived wellbeing differently in the two populations. In the Danish population, youth-related mental health problems may affect wellbeing in the youngest age group (16–25 years) (Ottosen et al., 2018), whereas age-related physical and mental health problems are likely to account for the lower scores in the adult refugee participants. Young participants (13–15 years) had a mean SWEMWBS score quite similar to the overall mean score in the Danish population, indicating that the youngest family members thrived at a level similar to the Danish reference population.
The increase in stress scores with increasing age reveals a high stress level among the adults. This may reflect frustrations related to health challenges, language barriers, problems with understanding legislations and living up to societal expectations. Furthermore, a persistent fear of being sent back to Syria is likely to contribute to a high stress level. Neighborhood characteristics such as low socioeconomic level, limited employment opportunities, and poor knowledge of how to access primary care and other health care resources may also increase chronic stress and can lead to physical disease (Hamad et al., 2020). A previous study involving adult immigrants arriving in Denmark in 1986–1998 reported that neighborhood disadvantage was associated with increased cardiovascular risk in a relatively young population of refugees (Hamad et al., 2020). In the interpretation of the descriptive means of stress scores, the use of a modified and non-validated version of the original perceived stress scale should, however, be taken into consideration. Due to the use of a modified stress scale, no attempts were made to compare stress scores in the study population with scores in a Danish population.
The higher proportions of participants, compared to Danes, reported being alone against their will (37.8% vs. 6.57%) and having nobody to talk to when having problems (20.0% vs. 5.29%) testify that social isolation is common among the study participants. This may contribute to their generally lower wellbeing. These results corresponds with findings in the Danish Health Survey for Region Zealand 2017; the proportion of lonely citizens was around twice as high among those with a non-Danish background compared with ethnic Danes (Blaakilde et al., 2018).
The overall and age-stratified proportions of study participants being very bothered by pain or discomfort was substantially higher than in Danish surveys and applied to all forms (Blaakilde et al., 2018; Rosendahl Jensen et al., 2018). Apparently, women suffered to a larger extent than men, which corresponds with the finding that women generally reported their health as less good compared with men. The prevalence of pain or discomfort in extremities, shoulders, neck and back seemed to be similar to findings in another Danish study of refugees (Andersen et al., 2020).
BMI
The prevalence of overweight and obesity (BMI ≥ 25) was 70% with no significant difference between males and females. This is similar to findings in a study from Australia involving newly arrived Syrian refugees, which reported a prevalence of overweight and obesity of 72% (Maldari et al., 2019). The prevalence of overweight and obesity in the Danish reference population was 52%. However, due to the different data collection methods of height and weight in the samples of refugees (measured) and Danes (self-reported), interpretation of the difference should be made with caution. Thus, BMI calculations in the Danish sample may contain some inaccuracy in terms of over- or underestimation.
Cholesterol and HbA1c
Elevated levels of HbA1c were identified in three study participants aged 16–56 years (3.4%), and all three individuals were diagnosed with diabetes. This corresponds with a diabetes prevalence of 3% observed in another group of refugees resettled in Denmark (Andersen et al., 2020), but was considerably lower than the prevalence of 13% reported in the above mentioned study from Australia (Maldari et al., 2019). Cholesterol levels showed an expected increase with higher age corresponding with the age-related pattern of HbA1c.
Hypertension
The prevalence of hypertension was 16.2% among the study participants aged 16–56 years, and thereby appears to be higher than reported in the other Danish study (9%) (Andersen et al., 2020) and the Australian study (13%), which included a refugee population aged 18–81 years (Maldari et al., 2019).
Implications of poor health status
The findings show a substantial difference in health status between refugee families from Syria 2–4 years after resettlement in Denmark and a Danish reference population. For all health parameters, the study participants demonstrated poor conditions that were similar or worse than conditions reported from studies of newly arrived refugees (Andersen et al., 2020; Maldari et al., 2019). This indicates limited, if any, alleviation of their health problems while resettled in Denmark. The parameters measured reflect both mental and physical health and included self-reported health, wellbeing, stress, loneliness, pain or discomfort and objective measurements as BMI, cholesterol, HbA1c and hypertension. Thus, the findings support the conclusions of two recent Danish studies, that refugees show multiple health issues, and there is a need for systematic, specialized health assessments and services to resettled refugees (Andersen et al., 2020; Hvass et al., 2021). Self-rated health was generally lower among women than men, which is in line with a higher proportion of women reporting being very bothered by different forms of pain or discomfort. These results support previous findings of poorer health among women than men (Akhavan et al., 2004), and suggest that certain health problems among women may need special attention. The youngest family members (aged 13–15 years) seemed to thrive in their everyday lives, giving good prospects for a well-functioning adult life.
Migrants and refugees resettled in European countries are subject to the obligation of becoming self-sufficient as soon as possible. However, Akhavan et al. (2004) have pointed at a reciprocal influence between health, work, and migration. Immigration and escape from war may cause poor health, which as a selection effect, leads to unemployment and/or sick leave. Unemployment is a complex psychosocial strain, threatening the identity and self-esteem of the unemployed (Akhavan et al., 2004). Status as a migrant or refugee may also bring about an inferior position on the labor market that can affect health negatively, an influence that is more marked for women than men (Akhavan et al., 2004). Thus, migrants and refugees need support in obtaining a stable health condition as a prerequisite for mobilizing surplus and self-confidence to maintain work and contribute to the host society. Early health care initiatives may prevent prolonged poor health conditions with unemployment and/or sick leave, leading to deprived opportunities to obtain self-sufficiency.
Strengths and limitations
The study provides insight in mental and physical health in a well-defined group of Syrian refugee families in direct relation to a host country population several years after resettlement. The survey design and construction of the questionnaire allowed comparison of several health parameters with Danish norms, and the interviewer-guided approach supported a high response rate. The results of self-perceived and objective measurements may have potential to serve as reference material in future studies.
The study also has a number of limitations. First, subgroup analyses were conducted in relatively small groups, affecting the accuracy of the estimates. The results from the Danish populations represent health status among responding participants from a randomly selected sample that are likely to be more resourceful than non-responders, thereby possibly overestimating the difference between refugees participants and the Danish reference population. Data on stress could not be presented in relation to a reference population due to the modification of the Perceived Stress Scale (Cohen et al., 1983). However, we believe that our results are helpful in uncovering the overall health status, in comparison to Danish reference values, in refugees who have not been offered a general health assessment at arrival in Denmark.
Conclusion
The study demonstrates various mental and physical health challenges among refugee families 2–4 years after resettlement in Denmark. The refugee families’ health appeared to be substantially poorer as compared to a Danish reference population. These findings add to existing evidence of a high prevalence of communicable diseases, non-communicable diseases, mental health and somatic symptoms among refugees at arrival (Andersen et al., 2020; Hvass et al., 2021), and emphasize the need for general health assessments to all refugees upon arrival followed up by specialized health care.
Policy-makers should pay attention to the evidence-based need for health assessments and care to refugees, and be aware that 1) early identification of health problems and timely care are likely to reduce spread of disease and aggravation of poor health conditions, 2) proper health care and contact to the health care system may increase focus on healthy life style habits and improve health literacy, and 3) delayed health care may prevent refugees’ potentials for societal contributions and potentially lead to increased cost to the healthcare system.
In support of other researcher's suggestions, we recommend that health assessments of both communicable diseases, non-communicable diseases and mental health are offered to all resettling refugees with the aim of providing early specialized health care for the benefit of the individual and society. Clear guidelines for municipalities and clinicians should be provided.
Funding
This work was supported by the A.P. Møller Relief Foundation (grant number 12014).
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
We thank the participating refugee families for their valuable contribution to the study and the interviewers for their assistance in interviewing and filling in questionnaires.
We appreciate the opportunity to include data from the Danish National Health Survey. The Danish National Health Survey was funded by The Capital Region, Region Zealand, The South Denmark Region, The Central Denmark Region, The North Denmark Region, The Ministry of Health and the National Institute of Public Health, University of Southern Denmark.
References
- Akhavan S., Bildt C.O., Franzén E.C., Wamala S. Health in relation to unemployment and sick leave among immigrants in Sweden from a gender perspective. J. Immigr. Health. 2004;6:103–118. doi: 10.1023/b:joih.0000030226.59785.38. [DOI] [PubMed] [Google Scholar]
- Andersen M.H., Kruse A., Frederiksen H.W., Ahmadi A., Norredam M. Health status of refugees newly resettled in Denmark. Dan. Med. J. 2020;67 [PubMed] [Google Scholar]
- Blaakilde A.L., Eiriksson S.D., Hansen B.H., Olesen L.S., Wingstrand A. Danish: Sundhedsprofil 2017 For Region Sjælland Og Kommuner – ”Hvordan Har Du Det? 1st ed. Region Zealand, Production, Research and Innovation; 2018. The Danish health profile 2017 for region Zealand and municipalities.https://www.regionsjaelland.dk/Sundhed/samarbejde-og-indsatser/hvordanhardudet/Documents/052849_RESJ_Mat_Sundhedsprofil_Samlet.pdf/ 2018 (accessed 24 January 2023) [Google Scholar]
- Clarke A., Friede T., Putz R., Ashdown J., Martin S., Blake A., Adi Y., Parkinson J., Flynn P., Platt S., Stewart-Brown S. Warwick-Edinburgh Mental Well-being Scale (WEMWBS): validated for teenage school students in England and Scotland. A mixed methods assessment. BMC Public Health. 2011;11:487. doi: 10.1186/1471-2458-11-487. http://www.biomedcentral.com/1471-2458/11/487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. J. Health Soc. Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- Danskernes Sundhed. Tal fra den Nationale Sundhedsprofil 2023. http://www.danskernessundhed.dk.
- Eskildsen A., Dalgaard V.L., Nielsen K.J., Andersen J.H., Zachariae R., Olsen L.R., Jørgensen A., Christiansen D.H. Cross-cultural adaptation and validation of the Danish consensus version of the 10-item Perceived Stress Scale. Scand. J. Work Environ Health. 2015;41:486–490. doi: 10.5271/sjweh.3510. [DOI] [PubMed] [Google Scholar]
- European Centre for Disease Prevention and Control . ECDC; Stokholm: 2018. Public Health Guidance On Screening and Vaccination For Infectious Disease in Newly Arrived Migrants Within the EU/EEA. [Google Scholar]
- Eurostat Statistics Explained, Asylum quarterly report. https://ec.europa.eu/eurostat/statistics-explained/index.php?title=Asylum_quarterly_report, 2022 (accessed 25 January 2023).
- Hamad R., Öztürk B., Foverskov E., Pedersen L., Sørensen H.T., Bøtker H.E., White J.S. Association of neighborhood disadvantage with cardiovascular risk factors and events among refugees in Denmark. JAMA Netw. Open. 2020;3 doi: 10.1001/jamanetworkopen.202014.196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirani K., Payne D., Mutch R., Cherian S. Health of adolescent refugees resettling in high-income countries. Arc. Dis. Child. 2016;101:670–676. doi: 10.1136/archdischild-2014-307221. [DOI] [PubMed] [Google Scholar]
- Hvass A.M., Weise C. Systematic Health Screening of refugees after resettlement in recipient countries: a scoping review. Ann. Hum. Biol. 2017;44:475–483. doi: 10.1080/03014460.2017.1330897. [DOI] [PubMed] [Google Scholar]
- Hvass A.M.F., Norredam M., Sodemann M., Wejse C. Is there a need of health assessments for resettling refugees? A cross-sectional study of 1431 refugees who arrived in Denmark between 2014 and 2018. J. Migr. Health. 2021 doi: 10.1016/j.jmh.2021.100044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koushede V., Lasgaard M., Hinrichsen C., Meilstrup C., Nielsen L., Rayce S.B., Torres-Sahli M., Gudmundsdottir D.G., Stewart-Brown S., Santini Z.I. Measuring mental well-being in Denmark: validation of the original and short version of the Warwick-Edinburgh mental well-being scale (WEMWBS and SWEMWBS) and cross-cultural comparison across four European settings. Psychiatry Res. 2019;271:502–509. doi: 10.1016/j.psychres.2018.12.003. [DOI] [PubMed] [Google Scholar]
- Laban C.J., Komproe I.H., Gernaat H.B.P.E., de Jong J.T.V.M. The impact of a long asylum procedure on quality of life, disability and physical health in Iraqi asylum seekers in the Netherlands. Soc. Psychiatry Psychiatr. Epidemiol. 2008;43:507–515. doi: 10.1007/s00127-008-0333-1. [DOI] [PubMed] [Google Scholar]
- Maldari T., Elsley N., Rahim R.A. The health status of newly arrived Syrian refugees at the Refugess Health Service, South Australia, 2019. AJGP. 2019;48:480–486. doi: 10.31128/AJGP-09-18-4696. [DOI] [PubMed] [Google Scholar]
- Nielsen L., Hinrichsen C., Santini Z.I., Koushede V. National Institute of Public Health, University of Southern Denmark; 2017. Måling Af Mental sundhed. En baggrundsrapport For Spørgeskemaundersøgelsen Danskernes Trivsel 2016.http://maaling_af_mental_sundhed_en_baggrundsrapport_for_spoergeskeamundersoegelsen_danskernes_trivsel_2016%20(2).pdf/ accessed 20 January 2023. [Google Scholar]
- Ottosen, M.H., Andreasen, A.G., Dahl, K.M., Hestbæk, A.-D., Lausten, M., Rayce, S.B., Børn og unge i Danmark. Velfærd og trivsel 2018, VIVE – Viden til Velfærd. Det Nationale Forsknings- og Analysecenter for Velfærd. Copenhagen 2018. https://www.vive.dk/da/udgivelser/boern-og-unge-i-danmark-velfaerd-og-trivsel-2018-10762/, 2018 (accessed 15 January 2023).
- Pew Research Center, Number of refugees to Europe surges to record 1.3 million in 2015. https://www.pewresearch.org/global/2016/08/02/number-of-refugees-to-europe-surges-to-record-1-3-million-in-2015/, 2016 (accessed 24 January 2023).
- Priebe, S., Giacco, D., El-Nagib, R., 2016. Public health aspects of mental health among migrants and refugees: a review of the evidence on mental health care for refugees, Asylum seekers, and irregular migrants in the WHO European Region. Copenhagen: WHO Regional Office for Europe. https://www.euro.who.int/__data/assets/pdf_file/0003/317622/HEN-synthesis-report-47.pdf. [PubMed]
- Rasmussen M., Pedersen T.P., Due P. 2nd ed. National Institute of Public Health, University of Southern Denmark.; 2015. Skolebørnsundersøgelsen 2014.http://HBSC-Rapport-2014%20(3).pdf/ accessed 20 January 2023. [Google Scholar]
- Rosendahl Jensen H.A., Davidsen M., Ekholm O., Christensen A.I. Danish: Danskernes Sundhed - Den Nationale Sundhedsprofil 2017. 2nd ed. Danish Health Authority; 2018. The Danish national health profile 2017.https://www.sst.dk/da/udgivelser/2018/danskernes-sundhed-den-nationale-sundhedsprofil-2017/ 2018 (accessed 24 January 2023) [Google Scholar]
- Stewart-Brown S., Tennant A., Tennant R., Platt S., Parkinson J., Weich S. Internal construct validity of the Warwick-Edinburgh Mental Well-being scale (WEMWBS): a Rash analysis using data from the Scottish Health Education Population Survey. Health Qual. Life Outcomes. 2009;7:15. doi: 10.1186/1477-7525-7-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart-Brown, S., Guidance on scoring. http://www2.warwick.ac.uk/fac/med/research/platform/wemwbs/researchers/guidance/, 2015 (accessed 28 November 2022).
- Stewart-Brown, S., Warwick-Edinburgh mental wellbeing scale (WEMWBS). http://www2.warwick.ac.uk/fac/med/research/platform/wemwbs/, 2015 (accessed 28 November 2022).
- Sundhed.dk. https://www.sundhed.dk/sundhedsfaglig/laegehaandbogen/hjerte-kar/symptomer-og-tegn/hoejt-blodtryk/, 2023 (accessed 23 January 2023).
- Sundhed.dk. https://netdoktor.dk/sygdomme/fakta/kolesterolhoejt.htm, 2023 (accessed 25 January 2023).
- Sundhed.dk. https://www.sundhed.dk/borger/patienthaandbogen/undersoegelser/blod-og-urinproever/hbb-hemoglobin-a1c/, 2023 (accessed 25 January 2023).
- Tennant R., Hiller L., Fishwickal R., Platt S., Joseph S., Weich S., Parkinson J., Secker J., Stewart-Brown S. The Warwick-Edinburgh mental wellbeing scale (WEMWBS): development and UK validation, Health Qual. Life Outcomes. 2007;63 doi: 10.1186/1477-7525-5-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization, Refugee and Migrant Health. https://www.who.int/news-room/fact-sheets/detail/refugee-and-migrant-health/, 2022 (accessed 15 December 2022).
- World Health Organization, Migration and Health: key issues. https://www.euro.who.int/__data/assets/pdf_file/0005/293270/Migration-Health-Key-Issues-.pdf (accessed 23 January 2023).