Abstract
Objective:
Vaginal agenesis or atresia in females suffering from MRKH syndrome is more common and management involves both surgical and non-surgical approaches. Use of prefabricated stents to maintain the patency of the canal may not fit appropriately during the initial surgical phase and are not economical. This case report discusses a series of modifications in a custom-made vaginal dilator to improve the retention for expansion after surgical management of MRKH syndrome.
Case report:
A 28-year-old female diagnosed with MRKH syndrome with characteristic Mullerian agenesis was referred for customised vaginal stent. Customised surgical stent was fabricated with loops for orientation and retention, which was later modified into interim expansion and passive stent.
Conclusion:
The customisation of the vaginal stent, provision of a retentive loop that positioned the stent in the proper orientation, and gradual increase in the size of the stent, ensured dilatation in a patient with vaginal agenesis.
Keywords: Mayer–Rokitansky–Küster–Hauser Syndrome, Neovagina, Acrylic Resin, Vaginal Aplasia, Vaginal Dilator
Introduction
Mayer-Rokitansky-Kuster-Hauser (MRKH) syndrome is a congenital anomaly of the female reproductive system that presents with primary amenorrhea, aplasia of the uterus, and the upper two-thirds of the vagina due to developmental failure of Mullerian ducts resulting in vaginal agenesis/atresia. Management of vaginal atresia or agenesis includes surgical and non-surgical approaches based on the clinical presentation. Non-surgical vaginal dilation is considered as the first line of therapy in a narrow vaginal canal, that provides an anatomical and functional success rate of more than 90% (1). A surgical approach is required in patients presenting with complete vaginal agenesis, and/or unsuccessful vaginal dilation using non-surgical vaginal dilators. Vaginoplasty fastens the achievement of vaginal patency, but the relapse occurs due to the inherent wound healing mechanisms. Hence, a long-term hard or soft vaginal stent is used to prevent stenosis, provide haemostasis, and also maintain the patency of the established neovaginal cavity. The hard vaginal stent provides a proper snug fit into the vagina that enables expansion of the tissue and also keeps the graft in close contact with the dissected space and has been largely used instead of soft vaginal stents due to the patient’s non-compliance. The duration of the wear of vaginal stent directly relates to the success of the treatment, however, the stent retention is compromised with daily activities. This case report discusses a series of modifications in a custom-made vaginal dilator to improve the retention for expansion after surgical management of MRKH syndrome.
Case report
A 28-year-old female diagnosed with MRKH syndrome with characteristic Mullerian agenesis was referred to the Department of Prosthodontics, Sri Ramachandra Institute of Higher Education and Research, Chennai for customised vaginal stent. Modified McIndoe technique was performed to enable a vaginal opening that extended 7 cm in length and 2.5 cm in width, and a vaginal stent of the determined dimensions was planned before the surgery to maintain patency and to prevent surgical failure.
Surgical Vaginal Stent:
A mold was fabricated using a PVC tube of 7 cm in length and 2.5 cm in diameter. One end of the tube was adapted with 5 mm of wax to resemble a smooth dome and the other end was closed with wax that formed the base. The base housed two lateral loops with vent holes to hold the stent in the desired position through elastics attached to the patient’s hip. The patency of the loop during processing was maintained using a putty consistency elastomeric impression material. The vaginal stent pattern was then invested in a custom-made flask using dental stone (Figure 1a). The set investment was dewaxed (Figure 1b) and processed using heat polymerizing acrylic resin.
Figure 1:
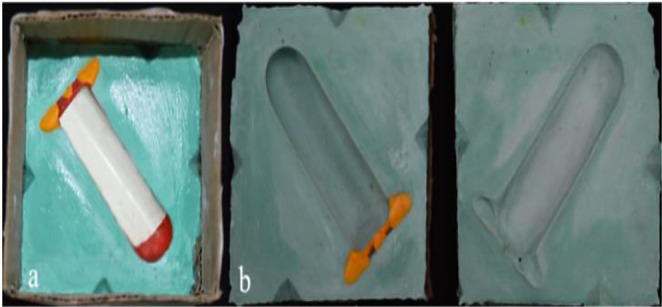
a- Wax pattern invested with dental stone, b- Mould space after dewaxing
The processed stent was retrieved, finished, polished, and cold sterilized. The 4 hip elastic chains were tied separately to the two lateral loops to prevent misposition and lateral movement of the stent in the surgical site (Figure 2a). This additional support aided in snug fit and retention of the stent during all physical activities of the patient (Figure 2b). The patient was advised to use the interim vaginal stent for 6 months to prevent surgical relapse and to maintain the patency of the canal.
Figure 2:
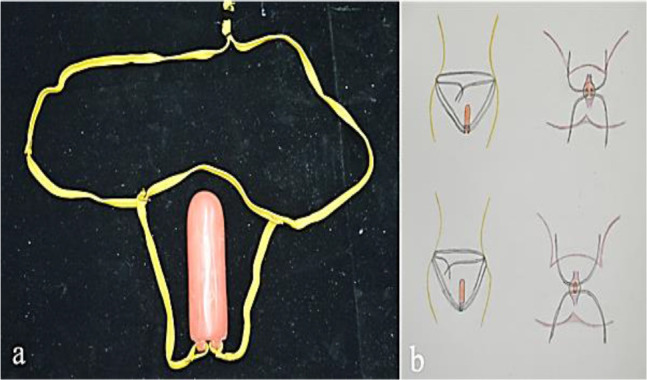
a- Processed Surgical Vaginal stent with double loops, b- Line diagram of the elastic chain and the loop
Interim expansion vaginal stent:
A 6 months follow-up visit revealed that the patient was comfortable with insertion and removal of the stent and was referred back again to the department of prosthodontics. However, the presence of 4 elastic chains and the knots caused a mild discomfort in the urethral region and the medial surface of the thigh, hence the number of loops were reduced. The increase in width for vaginal dilation was achieved by rolling a wax sheet over the existing 2.5 cm diameter surgical stent until a diameter of 3.5 cm. The stent was fabricated with a single loop in the centre that had two vent holes and a single hip elastic chain travelled through these holes to provide retention (Figure 3a). The patient was advised to use the stent regularly until she could wear the prosthesis without the exertion of pressure.
Figure 3:
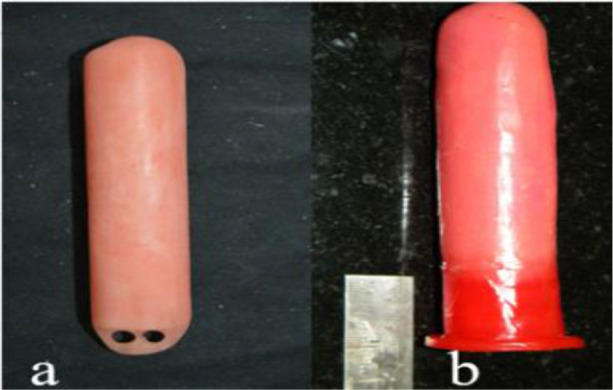
a- Modified vaginal stent with single loop, b- Modified vaginal stent without loops
Conversion of Interim expansion vaginal stent to Passive stent:
The Interim expansion stent was converted to a passive stent after achieving the desired length and width. The loops were removed since the patient felt discomfort. Wax was adapted over the base of the stent to achieve a pattern of 10 cm in length and 3.5 cm in width. Processing was completed and the patient was advised to insert the ighly polished stent for a year only during the sedentary period to achieve comfortable insertion (Figure 3b). After a period of one year, the patient was advised to wear the stent continuously as a passive appliance until she could engage in sexual activity.
Discussion
Vaginal stents of increasing diameters are required subsequent to the healing period to dilate the surgically created neovagina. Several prefabricated stents of different designs are available that sequentially increase the vaginal width by 0.25 inches, but are only available in specific sizes. The customized stent can be of specified dimension, provides adequate strength and offers a definite advantage over the prefabricated stent (2). In the present technique report we further customized the vaginal stent with retentive loops to sequentially dilate the vagina post-surgery with adequate retention. Customized vaginal stents can be soft silicone-based or rigid acrylic-based. Soft vaginal stents are more prone to fungal infections with surface deterioration when improperly maintained and hence replaced with hard vaginal stent. Customised hard acrylic vaginal stent used in the present technique was relined for sequential dilation of the vagina throughout the treatment period and, hence economical with better patient adaptation.
Lack of retention during the normal functional activity dissuades the patient from wearing the stent. The outcome of the treatment rendered by vaginal dilators is determined by the duration of the wear, retention and position of the stent. However, the technique involved in the fabrication of the retentive aids and the outcome of the retentive aids were not widely reported. Literature suggests that the wear of the stent 3 times a day for a minimum of 10 minutes increased the anatomic success rate, while prolonged wear showed better in functional success (3). Hence to prevent dislodgement during functional activity, the stent was fabricated with 2 loops to which 4 elastics were attached that were held around the hips. The loops also held the stent parallel to the vaginal axis which prevented undue pressure and subsequent meatal or urethral necrosis postoperatively.
The subsequent stents for vaginal width expansion was modified with a single loop to improve the retention of the stent, and the healed vagina reduced the chances of pressure necrosis. However, there were possibilities for lateral movement of the stent as the elastics only passed through the loop and were not tied to the base of the loop. The final vaginal dilator was given without the loops and the elastics increased the treatment duration due to lack of retention and non-compliance of the patient to wear the stent during functional activities. We observed that vaginal dilator with loops and elastics were ideal for vaginal expansion, however, the vaginal dilator without loops can be used only as a passive stent.
Conclusion
The customisation of the vaginal stent, provision of a retentive loop that positioned the stent in the proper orientation, and gradual increase in the size of the stent, ensured dilatation in a patient with vaginal agenesis. In addition, the 2-year follow-up revealed that the use of the single customised stent that was modified based on the clinical scenario was cost-effective, increased the adaptability, duration of wear, and the acceptance of the treatment by the patient.
Acknowledgments
None.
Footnotes
Conflict of Interests
There is no conflict of interests among the authors.
Notes:
Citation: Raza FB, Raju K, Babu A, Vaidyanathan AK, Mehta BS. Customised Vaginal Stent–The Phases in Management of Vaginal Agenesis in Mayer-Rokitansky-Küster-Hauser (MRKH) Syndrome. J Family Reprod Health 2023; 17(1):54-7.
References
- 1.Ogliari KCM, Rios SDS, Chen ACR, Chen JR, Resende CN, Araujo Júnior E. An alternative approach to vaginal dilation in patients with Meyer-Rokitanski-Küster-Hauser syndrome: two case reports. Gynecol Endocrinol. 2020. Aug;36(8):746–748. [DOI] [PubMed] [Google Scholar]
- 2.Patnana AK, Chugh A, Chugh VK, Shekhar S. Simple and novel technique for fabrication of prosthetic vaginal dilators. BMJ Case Rep. 2019 ;12(4):e229524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amies Oelschlager AM, Debiec K. Vaginal Dilator Therapy: A Guide for Providers for Assessing Readiness and Supporting Patients Through the Process Successfully. J Pediatr Adolesc Gynecol. 2019. Aug;32(4):354–358. [DOI] [PubMed] [Google Scholar]


