Abstract
Background
Producing scholarship in education is essential to the career development of a clinician-educator. Challenges to scholarly production include a lack of resources, time, expertise, and collaborators.
Objective
To develop communities of practice for education scholarship through an international society to increase community and academic productivity.
Methods
We developed multi-institutional scholarship pods within the American Thoracic Society through the creation of a working group (2017–2019). Pods met virtually, and meetings were goal focused to advance education scholarship within their area of interest. To understand the impact of these scholarship pods, we surveyed pod leaders and members in 2021 and analyzed the academic productivity of each pod via a survey of pod leaders and a review of the PubMed index.
Results
Nine pods were created, each with an assigned educational topic. The survey had a response rate of 76.6%. The perceived benefits were the opportunity to meet colleagues with similar interests at other institutions, production of scholarly work, and engagement in new experiences. The main challenges were difficulty finding times to meet because of competing clinical demands and aligning times among pod members. Regarding academic productivity, eight publications, four conference presentations, and one webinar/podcast were produced by six of the nine pods.
Conclusion
The development of communities of practice resulted in increased multi-site collaboration, with boosted academic productivity as well as an enhanced sense of belonging. Multiple challenges remain but can likely be overcome with accountability, early discussion of roles and expectations, and clear delegation of tasks and authorship.
Keywords: medical education, communities of practice, multi-institutional, education scholarship, collaboration
A “clinician-educator” is defined by their duty to care for patients and embrace educational principles, including scholarship through publication of manuscripts, presentation at national and international conferences, and/or production of webinars or podcasts (1). Over the past 40 years, the number of new faculty physicians identifying as clinician-educators has increased (2). Clinician-educator faculty are expected to produce scholarship, both to advance the field of medical education and to meet institutional merit and promotion criteria. However, medical education research across institutions remains limited, despite a clear need for multi-institutional collaborations that assess educational outcomes (3). Challenges to the production of scholarship include limitations in the following: funding opportunities, protected time for scholarship, local opportunities for collaboration, and education-focused journal outlets.
One approach to promote multi-institutional scholarship is through the development of communities of practice among researchers at different institutions. A community of practice is defined as a “persistent, sustaining social network of individuals who share and develop an overlapping knowledge base, set of beliefs, values, history, and experiences focused on a common practice and/or mutual enterprise” (4). In academic medicine, communities of practice have been implemented to promote research collaboration through established research networks that allow for multisite studies and provide scholarship opportunities for its members (5, 6). One such educational network, the Association of Pediatric Program Directors Longitudinal Educational Assessment Research Network (APPD LEARN), highlights the potential for success with this approach, which has resulted in many publications and presentations at national/international conferences since its implementation (7). Although the APPD LEARN is a robust model for development of communities of practice, to date, there has not been a similar model used through an international society.
In this article, we describe our experience with developing communities of practice for medical education scholarship through an international society. Here, we summarize our process and offer perspectives via survey analysis, which we hope can serve as a guide to others.
Methods
We developed multi-institutional communities of practice within the American Thoracic Society (ATS), with the purpose of developing education scholarship. The ATS was founded in 1905 and includes more than 16,000 members, with the mission to improve worldwide health through advancing research, clinical care, and public health in respiratory disease, critical illness, and sleep disorders (8). Within the ATS, the Section on Medical Education (SOME) is a group of approximately 3,000 clinician-educators with the goals of collaboratively developing and disseminating educational strategies, resources, and scholarship and supporting its members’ careers.
Scholarship Pods
Starting in May 2017, the ATS SOME created communities of practice, called scholarship pods, through the development of an Educational Research working group. The mission was twofold: to increase ATS scholarly activity in medical education and to advance medical education research skills among working group members.
The initial version included a total of nine pods. The pods were formed based on the scholarly interests of SOME attendees at the 2017 ATS International Conference through a web-based sign-up tool. The pod topics were simulation, interprofessional education, bedside teaching, leadership, communication, milestones, adult learning, social media, and transitions of care. On the sign-up tool, participants indicated if they were interested in serving as pod leaders. SOME leadership reviewed the prior medical education scholarship experience of these volunteers to choose leaders. The scholarship pods were expected to meet monthly through conference calls. The working group chair attended meetings as able to support the pod leader. At the annual international conference, the pods were encouraged, though not required, to meet in person. Each pod was tasked with producing a scholarly product, but the exact type was decided by the individual pods.
Pod Survey
To determine success, we surveyed pod members and analyzed the academic productivity of each pod 4 years after inception. The survey was developed through expert opinion, with further refinement based on pilot testing in a small cohort of clinician-educators with experience in scholarly production. The complete survey is included in the data supplement. The survey was online and hosted on Qualtrics (through Mayo Clinic). A 5-point Likert scale (strongly disagree to strongly agree) was used to assess benefits and perceived challenges of the pod structure, and there were optional free-text response boxes for global feedback and suggestions for improvement. The survey was disseminated via email in May 2021 to all the pod leaders and members (based on a database maintained by ATS administrative staff), with a reminder e-mail 2 weeks later. The Mayo Clinic Institutional Review Board deemed this study exempt from full review.
Academic Productivity
Academic productivity was assessed through the PubMed Index of the names of the pod leaders and group members. Only publications specific to medical education were counted. In addition, webinars, podcasts, and conference presentations were considered scholarly products and captured through a survey of pod leaders. We also asked survey respondents about scholarly output but could not compare these responses to PubMed, as the survey was anonymous.
Statistical Analysis
We performed descriptive statistics using absolute numbers and percentages of the survey results and absolute values for academic productivity. The Likert scale responses for “strongly disagree” and “disagree” were combined for analysis, as were “strongly agree” and “agree.” Summary statistics were used to analyze the Likert scale responses, and thematic analysis was performed on the free-text comments.
Results
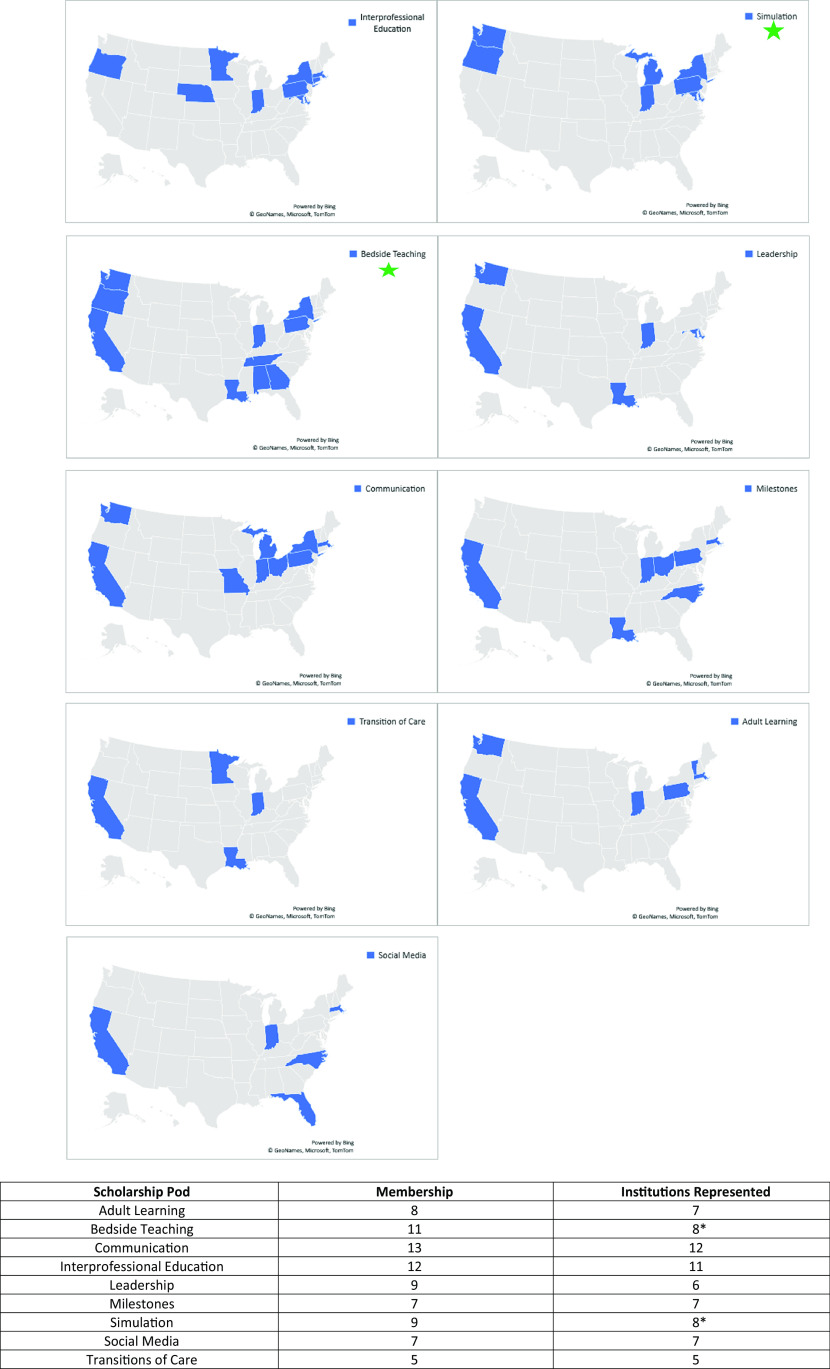
The scholarship pods ran from May 2017 to May 2019. The total membership of the nine pods was 51, with an average of 9 members per pod. A total of 33 different institutions were represented, including one international pod member (Figure 1). The survey was sent to 47 participants. Four members either dropped out of their pod or changed institutions and lacked updated e-mail addresses. Thirty-six responses were obtained, for a 76.6% response rate.
Figure 1.
Scholarship pod membership. For the Education Research working group, there were a total of nine scholarship pods. Each individual pod is shown above, with graphical representation of where members were located within the United States. There was one international member (denoted by the star).
Many of the pod members became involved in the scholarship pods through signing up at the ATS international conference (43.6%, n = 24) or being invited by a friend or colleague (21.8%, n = 12). About 42% (n = 15) were trainees during at least part of the time they were involved with the scholarship pods.
Table 1 describes the perceived benefits and challenges participants identified as part of these scholarship pods. Nearly all participants felt the benefits of being a pod member were 1) the opportunity to meet colleagues with similar interests at other institutions (94.4%, n = 34); 2) production of scholarly work (77.8%, n = 28); and 3) engagement in new experiences (75%, n = 27). Some of the specific comments included the positive networking experience, the sense of camaraderie, and the visibility for promotion. The biggest challenges identified were difficulty finding times to meet because of competing clinical demands (72.2%, n = 26) and aligning times among pod members (72.2%, n = 26). Free-text comments on the challenges faced related to unclear roles and responsibilities, lack of delegation of tasks, and productivity being dependent on the leader.
Table 1.
Benefits and challenges of the scholarship pods (Likert scale)
| Strongly Disagree/Disagree | Neither | Strongly Agree/Agree | |
|---|---|---|---|
| In your opinion, what were the benefits of being a pod member? | |||
| Met colleagues with similar interests at other institutions | 2.8 (1) | 2.8 (1) | 94.4 (34) |
| Met senior members of my field who provided mentorship/sponsorship | 11.1 (4) | 30.6 (11) | 58.3 (21) |
| Production of scholarly work | 5.6 (2) | 16.7 (6) | 77.8 (28) |
| Development of new skills | 19.4 (7) | 19.4 (7) | 61.1 (22) |
| Engagement in new experiences | 11.1 (4) | 13.9 (5) | 75 (27) |
| Pod experience led to other projects | 16.7 (6) | 13.8 (5) | 69.4 (25) |
| In your opinion, what were the biggest challenges/obstacles with the pod? | |||
| Difficulty finding times to meet because of competing clinical demands | 11.1 (4) | 16.7 (6) | 72.2 (26) |
| Difficulty aligning times to meet with pod members | 8.33 (3) | 19.4 (7) | 72.2 (26) |
| Disagreement regarding goals | 61.1 (22) | 16.7 (6) | 22.2 (8) |
| Workload unequally shared among pod members | 36.1 (13) | 27.8 (10) | 36.1 (13) |
| Unsuccessful in publishing work completed | 61.1 (22) | 13.9 (5) | 25 (9) |
| Inability to complete the work that I agreed to do | 58.3 (24) | 13.9 (5) | 19.4 (7) |
| Pod leader(s) lacked follow-through | 58.3 (21) | 16. (6) | 25 (9) |
| Members other than the leader lacked follow-through | 30.6 (11) | 30.6 (11) | 38.9 (14) |
Data are presented as % (n).
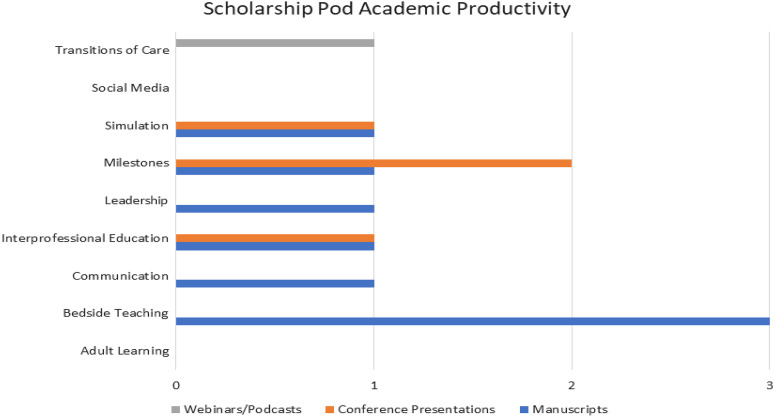
Within the survey, 88.9% (n = 32) described having produced scholarly work through the pods, which was the primary objective of the groups. Peer-reviewed publication was the most common form of academic productivity (56.6%), followed by conference abstract (20.8%), conference workshop (7.6%), webinar (9.4%), and podcasts (5.7%). On review of PubMed, out of the nine pods, six had published manuscripts (66%), for a total of eight publications (Figure 2). In addition, four conference presentations and one webinar/podcast were produced by these pods. The latter is discrepant between the survey of all pod members and the survey of the pod leaders specifically asking about scholarly output.
Figure 2.
Scholarship pod academic productivity. Each individual pod was encouraged to produce educational scholarship, including manuscripts (blue), conference presentations (orange), and webinars/podcasts (gray).
The last question of the survey asked participants for their thoughts on what can be done to improve the experience. The feedback included suggestions to use Zoom to stay connected (compared with e-mail or conference calls), prioritize early career faculty as pod leaders, have pod leaders hold members accountable for their action items, provide clearer expectations of pod membership tasks, hold in-person meetings at the ATS international conference, and provide funding support.
Discussion
We describe the creation of multi-institutional communities of educational scholarship within a pulmonary and critical care medicine international society. Participants in these scholarship pods noted several benefits to participation, including academic productivity, networking, and engagement in the international society. This highlights the benefits of building communities of practice through academic societies to enhance academic scholarship productivity and engagement.
Communities of practice are characterized by three main components: 1) domain; 2) community; and 3) practice (9). There are several elements of communities of practice visible within these scholarship pods, likely contributing to their overall success. The domain or purpose and value of the pods was to collaborate on education scholarship. The sense of community was quite clear and was one of the main benefits of the pods, as evident by the survey data. Last, the practice within these pods related to the knowledge and skills of the group, which in this case broadly involved medical education. More specifically, each pod had a narrow focus, allowing for the development of greater expertise.
There are, however, multiple challenges that make the implementation of such medical education practice-based scholarship networks difficult. Challenges identified from the survey respondents included difficulty scheduling meetings (virtually, across a variety of time zones, and at the ATS international conference) and identifying funding and statistical support, as well as lack of clarity regarding role expectations, task delegation, and agreement on authorship definitions. These challenges, when present, may have affected pod productivity. The pod leaders’ ability to overcome these challenges influenced the success of each pod, highlighting that leadership is a critical piece to the development of communities of practice. If the pod leader was engaged and held the group accountable, the pod was much more successful.
To address some of these challenges, SOME created a new ATS working group called Project Leadership in May 2020, with the focus on faculty development for pod leaders. Each member of this working group leads their own pod. During these meetings, members provide quick updates on their pods, which helps with accountability, and discuss strategies to improve accountability and enhance engagement. There is discussion of challenges/barriers, with time for collaborative brainstorming for solutions to these issues often encountered by others. In addition, with this survey feedback, this group created specific documents to help pod leaders be more successful, including criteria for pod expectations and member responsibilities, authorship guidelines based on the International Committee of Medical Journal Editors guidelines (10), a template for meeting minutes, and resources for scholarship opportunities (data supplement).
Despite these improvements to the pods, the ideal size of the scholarship pods and the best methods for continued engagement remain unknown. In our experience, we believe a group size between six and eight may be ideal to ensure accountability and motivation. We have found that larger groups have led to less accountability, especially if the roles and responsibilities are not clearly defined. Engagement varied based on clinical duties and coronavirus disease (COVID-19) surges. Many pods struggled to keep members engaged because of high clinical burdens as well as “Zoom fatigue.” As the pandemic continues, innovative ways to ensure sustainability and pod engagement will be crucial to the continued success of these pods.
As we hypothesize that improved engagement would result in improved member experiences as well as improved productivity, strategies to improve engagement and promote accountability are critical. Potential strategies to improve engagement would be to identify the deliverables of each pod member at the start of the project, set discrete deadlines, and create a standing meeting time for pod members. Importantly, the strategy for this initial iteration relied on individual pod leaders to determine any mechanisms for managing less-engaged participants. We would encourage more structured guidance from the pod leadership team, including set expectations across all pods, to minimize the burden on individual pod leaders. Finally, as the pod chair regularly attended working group meetings, a system could be implemented to encourage feedback to pod leaders about leadership effectiveness within the pods.
Strengths and Limitations
There were several strengths of our approach to fostering successful communities of practice. The scholarship pods included a diverse group of colleagues from around the country and from one international location (Figure 1). The creation of such international collaboration has potential to improve academic output for individuals (both trainees and faculty) with limited institutional resources. The pods themselves were focused on a variety of education-focused themes, which allowed members to choose their area(s) of interest and likely enhanced engagement (11). Limitations to evaluating our intervention include the potential for recall bias, as the survey data were collected after completion of the initial working group. We did complement this with objective productivity data outputs that would not be prone to bias. Similarly, the survey was completed during the COVID-19 pandemic, which may have altered the respondents’ overall perceptions of participation in their pods. Finally, we were unable to ensure accountability and/or measure the pod members’ compliance with designated meetings (both virtual and in person). Understanding how improved engagement altered the experience of pod members and ultimate scholarship output is an important area of future work.
Conclusions
Based on our experience, academic productivity can be enriched through intentional development of a community of like-minded individuals. Camaraderie and sense of belonging are important parts of our professional community and can result in a more successful (and, we hope, joyful) academic career. Challenges can be overcome with accountability, early discussion of roles and expectations, and clear delegation of tasks and authorship. Medical education research would benefit from more multi-institutional studies, and the creation of medical education communities of practice may be one way to address this need.
Acknowledgments
Acknowledgment
The authors thank Drs. Jennifer McCallister and Henry Fessler for their support of the initial Educational Research working group as well as Breana Portelli and Javier Guzman, American Thoracic Society staff, for their help in the management and coordination of the Project Leadership working group.
Footnotes
The views expressed in this article do not communicate an official position of the American Thoracic Society.
Author Contributions: All authors helped in the conception and design of this study. The analysis and interpretation were conducted by D.J.K. and W.G.C. All authors participated in the drafting of the manuscript for important intellectual content and have approved the final version.
This article has a data supplement, which is accessible from this issue’s table of contents at www.atsjournals.org.
Author disclosures are available with the text of this article at www.atsjournals.org.
References
- 1. Greenberg L. The evolution of the clinician-educator in the United States and Canada: personal reflections over the last 45 years. Acad Med . 2018;93:1764–1766. doi: 10.1097/ACM.0000000000002363. [DOI] [PubMed] [Google Scholar]
- 2. Mandel J. Career development strategies for the clinical educator. ATS Scholar . 2020;1:101–109. doi: 10.34197/ats-scholar.2020-0005PS. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Cook DA, Andriole DA, Durning SJ, Roberts NK, Triola MM. Longitudinal research databases in medical education: facilitating the study of educational outcomes over time and across institutions. Acad Med . 2010;85:1340–1346. doi: 10.1097/ACM.0b013e3181e5c050. [DOI] [PubMed] [Google Scholar]
- 4. Barab SA, Barnett M, Squire K. Developing an empirical account of a community of practice: characterizing the essential tensions. J Learn Sci . 2002;11:489–542. [Google Scholar]
- 5. Schwartz A, Young R, Hicks PJ, APPD LEARN Medical education practice-based research networks: facilitating collaborative research. Med Teach . 2016;38:64–74. doi: 10.3109/0142159X.2014.970991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Carney PA, Brandt B, Dekhtyar M, Holmboe ES. Advancing health professions education research by creating a network of networks. Acad Med . 2018;93:1110–1112. doi: 10.1097/ACM.0000000000002189. [DOI] [PubMed] [Google Scholar]
- 7. Schwartz A, King B, Mink R, Hicks PJ. The emergence and spread of practice-based medical education research networks. Acad Med . 2020;95:S12–S13. doi: 10.1097/ACM.0000000000003641. [DOI] [PubMed] [Google Scholar]
- 8.American Thoracic Society. https://www.thoracic.org/about/overview.php
- 9.Snyder WM, Wenger E. In: Social learning systems and communities of practice. Blackmore C, editor. London, UK: Springer Verlag; 2010. Our world is a learning system: a communities-of-practice approach; pp. 107–124. [Google Scholar]
- 10.International Committee of Medical Journal Editors. https://www.icmje.org/recommendations/browse/roles-and-responsibilities/defining-the-role-of-authors-and-contributors.html
- 11. Knowles MS. Andragogy: adult learning theory in perspective. Community Coll Rev . 1978;5:9–20. [Google Scholar]