Abstract
Background:
The optimal immobilization position of the shoulder after rotator cuff repair is controversial.
Purpose:
To compare the clinical outcomes and incidence of retears after arthroscopic rotator cuff repair between patients who used an abduction brace versus a sling for postoperative shoulder immobilization.
Study Design:
Systematic review; Level of evidence, 1.
Methods:
This systematic review and meta-analysis was conducted using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. We searched the PubMed, MEDLINE, and Embase electronic databases for randomized controlled trials (RCTs) that compared abduction brace and sling immobilization after arthroscopic rotator cuff repair using single-row, double-row, or suture-bridge fixation. Clinical scores, pain severity, and retear rates were compared between patients with abduction brace versus sling immobilization.
Results:
Of 1572 retrieved studies, 4 RCTs with a total of 224 patients (112 patients with abduction brace and 112 patients with sling) were included in the qualitative analysis, and 3 of the RCTs were included in the quantitative analysis (meta-analysis). There were no significant differences between the abduction brace and sling immobilization groups in the Constant-Murley score at 3 months (weighted mean difference [WMD], 0.26 [95% CI, –1.30 to 1.83]; P = .74; I 2 = 84%), 6 months (WMD, 1.91 [95% CI, –0.17 to 4.00]; P = .07; I 2 = 85%), and 12 months (WMD, 0.55 [95% CI, –1.37 to 2.47]; P = .57; I 2 = 0%); the visual analog scale score for pain at 1 week (WMD, 0.10 [95% CI, –0.20 to 0.41]; P = .51; I 2 = 0%), 3 weeks (WMD, –0.12 [95% CI, –0.34 to 1.00]; P = .29; I 2 = 0%), 6 weeks (WMD, –0.12 [95% CI, –0.30 to 0.06]; P = .20; I 2 = 0%), and 12 weeks (WMD, –0.13 [95% CI, –0.27 to 0.02]; P = .09; I 2 = 18%); or the retear rate at 3 months (risk ratio, 0.63 [95% CI, 0.09 to 4.23]; P = .64; Z = 0.47%) postoperatively.
Conclusion:
Our systematic review demonstrated a lack of significant differences between the abduction brace and sling immobilization groups regarding postoperative clinical scores, pain severity, and tendon healing.
Keywords: rotator cuff repair, rehabilitation, abduction brace, sling, systematic review, meta-analysis
A rotator cuff tear is one of the most common shoulder disorders in older adults, with a reported incidence of 17% to 41%. 13,23 If nonoperative treatment options for symptomatic rotator cuff tears fail, surgery should be considered. Because of the advances in technology and skill in the last 2 decades, rotator cuff repair is increasingly being performed arthroscopically rather than via the open technique. 11,18 However, despite the advancement in repair techniques, a rotator cuff retear is still a common postoperative complication. 10,22 Studies have indicated that the use of a brace that immobilizes the shoulder in 30° of abduction during the postoperative rehabilitation period reduces tension on the repaired tendon, which improves tendon-bone healing. 5,17 Moreover, an abducted shoulder position is reported to achieve higher blood flow in and around the posterosuperior rotator cuff. 14 However, recent studies have found no significant difference in clinical outcomes with postoperative shoulder immobilization using an abduction brace versus a sling after rotator cuff repair. 1,3,7 Sonoda et al 20 found that using an abduction brace for immobilization after rotator cuff repair is associated with gait impairment and an increased fall risk during the early postoperative period because of visual field loss and body imbalance caused by the abduction brace. In addition, an increasing number of physicians are implementing rehabilitation protocols of early motion after rotator cuff repair to achieve greater postoperative range of motion (ROM), pain relief, and earlier return to activities, 21 which indicates that immobilization is not necessary after rotator cuff repair.
The purpose of the current systematic review and meta-analysis was to compare the clinical outcomes and rotator cuff retear rate between patients with an abduction brace versus a sling for shoulder immobilization after arthroscopic rotator cuff repair using data from randomized controlled trials (RCTs) only. We hypothesized that there would be no differences in the clinical outcomes and retear rates between patients with abduction brace versus sling immobilization.
Methods
Search Strategy
This systematic review and meta-analysis was conducted using PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. We searched the PubMed, MEDLINE, and Embase electronic databases from inception to April 2022 to identify all studies that compared abduction brace and sling immobilization after arthroscopic rotator cuff repair. The key terms were the following: (rotator cuff* OR rotator cuff) AND (arthroscop* OR endoscop*) AND (sling OR brace OR immobilization OR motion). We also manually searched the Cochrane Central Register of Controlled Trials and the Cochrane Database of Systematic Reviews to identify any additional relevant studies. There were no language restrictions. Included in the review were RCTs that used single-row, double-row, or suture-bridge techniques for arthroscopic fixation. Systematic reviews, case reports, case series, animal studies, and biomechanical studies were excluded, as were studies using open repair techniques.
Among 1572 studies retrieved in the initial search, 4 RCTs were included in the qualitative analysis, 1,3,7,14 and 3 of the RCTs were included in the quantitative analysis (meta-analysis). 3,7,14 A flowchart of the literature search is shown in Figure 1.
Figure 1.
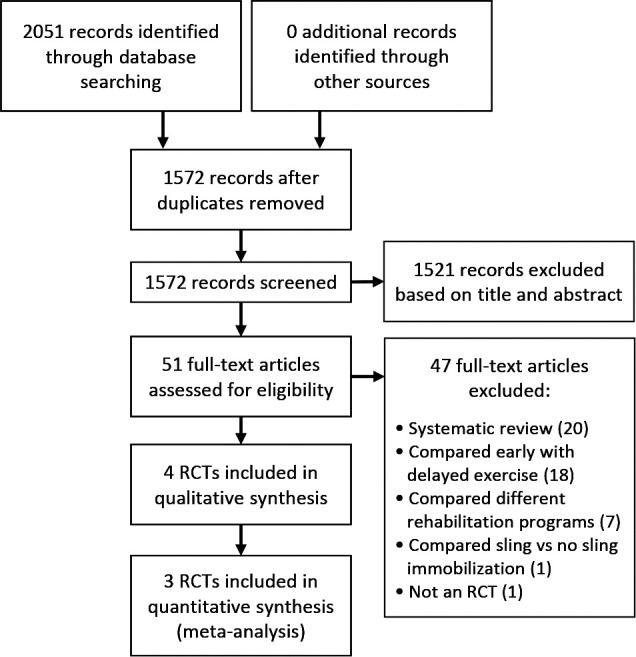
Flowchart of literature search. RCT, randomized controlled trial.
Data Extraction and Quality Assessment
There were 2 authors (J.-H.G. and J.-Y.Z.) who independently reviewed all retrieved articles and selected the studies that met the inclusion criteria. The data extracted from the selected studies included patient characteristics, arthroscopic findings, surgical procedures, rehabilitation protocols, and outcome measurements (Constant-Murley score [CMS], visual analog scale [VAS] for pain, and retear rate). Discrepancies between the 2 independent evaluators were resolved through a discussion and consensus among all authors.
The quality of the included RCTs was evaluated using the Cochrane risk-of-bias assessment tool, 2 which classifies the following items as having a low, high, or unclear risk of bias: random sequence generation; allocation concealment; blinding of participants, care providers, and outcome assessors; incomplete outcome data; selective outcome reporting; and other sources of bias.
Data Synthesis and Statistical Analysis
Continuous variables (CMS and VAS for pain) were reported as means and standard deviations. Weighted mean differences (WMDs) and 95% confidence intervals were calculated for continuous variables. For the dichotomous variable (retear rate), the risk ratio (RR) and 95% confidence interval were calculated.
Heterogeneity among studies was quantified using the I 2 statistic, with I 2 values interpreted as not important (0%), moderate (30%-60%), substantial (50%-90%), or considerable (75%-100%). 11 A random-effects model was used if I 2 was ≤50%; otherwise, a fixed-effects model was used for data synthesis. 6 Analyses were conducted using Review Manager software (Version 5.1; Cochrane).
Results
Included Studies
The 4 RCTs 1,3,7,14 included in this review involved a total of 224 patients (112 in the abduction brace immobilization group and 112 in the sling immobilization group). All RCTs had a level of evidence of 2. The characteristics of the 4 studies are summarized in Table 1.
Table 1.
Characteristics of Included Studies a
| First Author (Year) | Level of Evidence | No. of Patients | Age, b y | Male/Female Sex, n | Mean Follow-up, mo |
|---|---|---|---|---|---|
| Conti 1 (2015) | 2 | AB: 20 SL: 20 |
AB: 62.3 (45-68) SL: 59 (42-70) |
27/13 | 6 |
| Hollman 7 (2017) | 2 | AB: 20 SL: 16 |
AB: 60.2 ± 6.84 SL: 62.5 ± 9.76 |
AB: 11/9 SL: 5/11 |
12 |
| Ghandour 3 (2019) | 2 | AB: 51 SL: 55 |
AB: 50.4 ± 11.7 SL: 50.8 ± 12.0 |
AB: 25/26 SL: 28/27 |
12 |
| Pandey 14 (2020) | 2 | AB: 21 SL: 21 |
AB: 55.8 ± 7.8 (40-78) SL: 55.5 ± 10.5 (42-70) |
AB: 13/8 SL: 9/12 |
12 |
a AB, abduction brace; SL, sling.
b Data are provided as mean or mean ± SD, with ranges in parentheses.
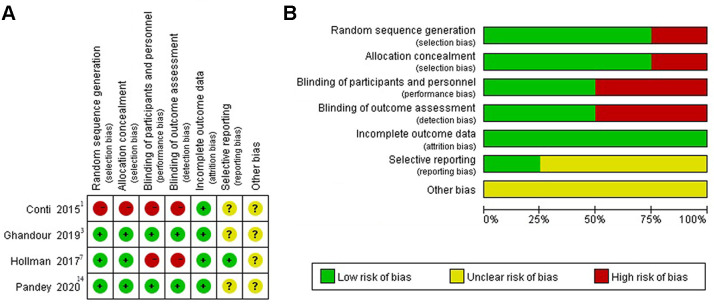
A standardized assessment of the risk of bias in the included RCTs is summarized in Figure 2. The use of randomization was mentioned in 3 studies. 3,7,14 Allocation concealment was adequate in 3 studies. 3,7,14 There were 2 studies that reported that the orthopaedic surgeons and physical medicine specialists were blinded to patient allocation. 3,14 One study discussed reporting bias, 7 while none of the studies reported incomplete outcome data or discussed any other sources of bias.
Figure 2.
(A) Risk-of-bias summary for each included study and (B) each risk-of-bias item presented as a percentage across all included studies.
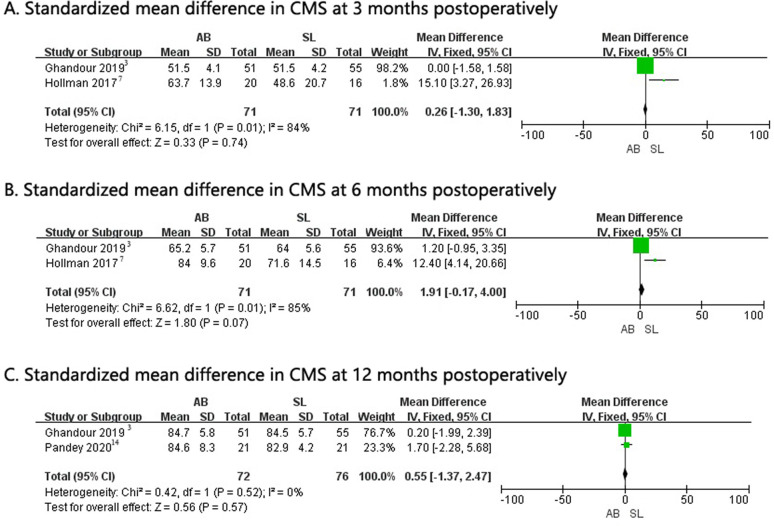
Constant-Murley Score
The CMS value from 2 of the 4 studies was pooled. 3,7 The meta-analysis revealed no significant difference in the CMS value between the abduction brace and sling immobilization groups at 3 months (WMD, 0.26 [95% CI, –1.30 to 1.83]; P = .74; I 2 = 84%), 6 months (WMD, 1.91 [95% CI, –0.17 to 4.00]; P = .07; I 2 = 85%), or 12 months (WMD, 0.55 [95% CI, –1.37 to 2.47]; P = .57; I 2 = 0%) postoperatively (Figure 3).
Figure 3.
Forest plots of standardized mean differences for the Constant-Murley score (CMS) at (A) 3 months, (B) 6 months, and (C) 12 months postoperatively. AB, abduction brace; IV, inverse variance; SL, sling.
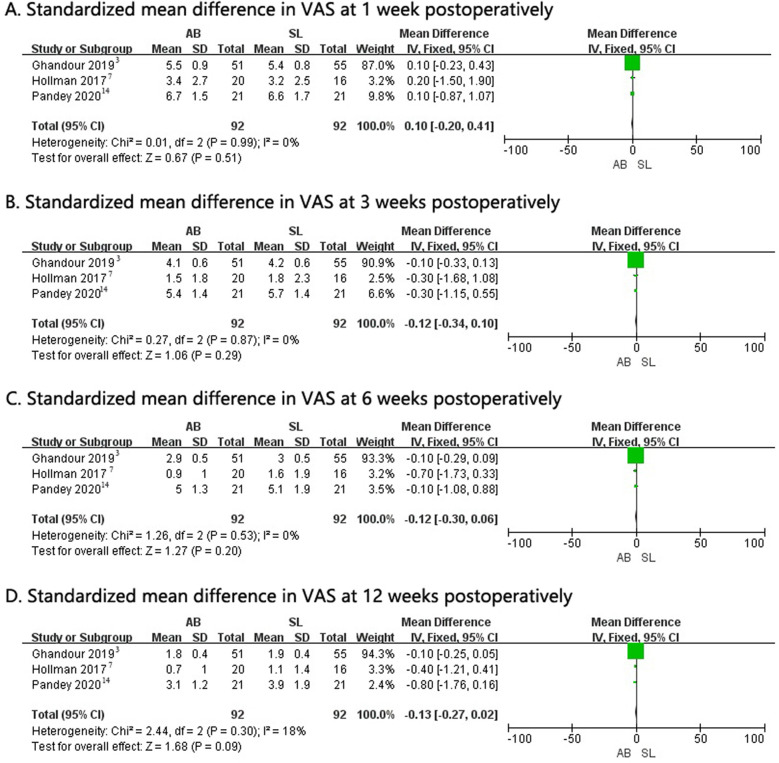
VAS Pain Score
The VAS pain score from 3 of the 4 studies was pooled. 3,7,14 The meta-analysis revealed no significant difference in the VAS pain score between the abduction brace and sling immobilization groups at 1 week (WMD, 0.10 [95% CI, –0.20 to 0.41]; P = .51; I 2 = 0%), 3 weeks (WMD, –0.12 [95% CI, –0.34 to 0.10]; P = .29; I 2 = 0%), 6 weeks (WMD, –0.12 [95% CI, –0.30 to 0.06]; P = .20; I 2 = 0%), or 12 weeks (WMD, –0.13 [95% CI, –0.27 to 0.02]; P = .09; I 2 = 18%) postoperatively (Figure 4).
Figure 4.
Forest plots of standardized mean differences for the visual analog scale (VAS) for pain score at (A) 1 week, (B) 3 weeks, (C) 6 weeks, and (D) 12 weeks postoperatively. AB, abduction brace; IV, inverse variance; SL, sling.
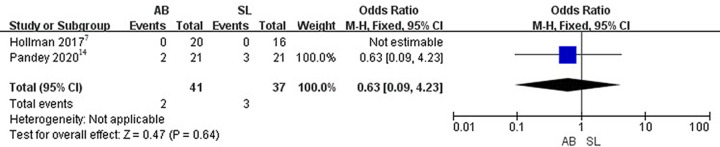
Retear Rate
The retear rate from 2 of the 4 studies was pooled. 7,14 Both studies used ultrasound to determine retears of the rotator cuff. The meta-analysis revealed no significant difference in the retear rate between the abduction brace and sling immobilization groups at 3 months postoperatively (RR, 0.63 [95% CI, 0.09-4.23]; P = .64; Z = 0.47) (Figure 5).
Figure 5.
Forest plot of the retear rate. AB, abduction brace; M-H, Mantel-Haenszel; SL, sling.
Discussion
In this study, we found that there was no significant difference between the abduction brace and sling immobilization groups in the CMS value at 3 months (WMD, 0.26 [95% CI, –1.30 to 1.83]; P = .74), 6 months (WMD, 1.91 [95% CI, –0.17 to 4.00]; P = .07), and 12 months (WMD, 0.55 [95% CI, –1.37 to 2.47]; P = .57); the VAS pain score at 1 week (WMD, 0.10 [95% CI, –0.20 to 0.41]; P = .51), 3 weeks (WMD, –0.12 [95% CI, –0.34 to 0.10]; P = .29), 6 weeks (WMD, –0.12 [95% CI, –0.30 to 0.06]; P = .20), and 12 weeks (WMD, –0.13 [95% CI, –0.27 to 0.02]; P = .09); or the retear rate at 3 months (RR, 0.63 [95% CI, 0.09 to 4.23]; P = .64) postoperatively. To our knowledge, this meta-analysis is the first to compare the differences in clinical outcomes and retear rates between patients undergoing abduction brace versus sling immobilization during rehabilitation after arthroscopic rotator cuff repair. There were no significant differences between the abduction brace and sling immobilization groups in clinical scores, pain severity, and retear rates in the first year postoperatively.
The optimal immobilization position of the shoulder after rotator cuff repair is controversial. A biomechanical study indicated that using an abducted brace reduces tension on the repaired rotator cuff. 5 Similarly, 30° of shoulder abduction reportedly reduces loading and gap formation at the repaired rotator cuff tendon, 15 and tension in the superior rotator cuff reportedly increases with the shoulder in the internal rotation position. 17 Moreover, a clinical study found that the use of an abduction brace increases blood flow in the repaired tendon at 1 day and 6 weeks postoperatively 14 ; however, this did not lead to significant differences in clinical outcomes and structural healing between the abduction brace and arm pouch groups at 12 months postoperatively. 14 In addition, recent research has suggested potential complications with the use of an abduction brace after shoulder surgery. 20 One study reported a significantly higher incidence of falls after rotator cuff repair with postoperative abduction brace shoulder immobilization than after total hip and knee replacement during the early postoperative period because of visual field loss and body imbalance caused by the abduction brace. 20 However, they did not compare the incidence of falls between the abduction brace and sling groups in their study. 20 Another study found that patients with no shoulder immobilization after rotator cuff repair have better early mobility and functional scores than those with shoulder immobilization. 21
In addition to immobilization position, an increasing number of physicians are implementing rehabilitation protocols of early motion after rotator cuff repair to achieve greater postoperative ROM, pain relief, and earlier return to activities, 21 suggesting that immobilization is not necessary after rotator cuff repair. One animal study reported that decreasing the activity level of the shoulder improves tendon-to-bone healing by increasing the organization of collagen and the mechanical properties. 4 Conversely, early passive motion after surgery has no effect on collagen organization or tendon mechanical properties in rats 15 and no effect on tendon-bone healing in rabbits. 24 Furthermore, a clinical trial showed that a progressive protocol has no adverse effects compared with the traditional protocol. 8 Adequate motion and exercises are essential for tendon healing after rotator cuff repair. Repair integrity is reported to be similar at 12 months postoperatively between early and delayed mobilization. 19 One systematic review and meta-analysis did not find that immobilization after arthroscopic rotator cuff repair is superior to early motion rehabilitation in terms of tendon healing or clinical outcomes and suggested that the early motion group recovered ROM more rapidly than the immobilization group. 18 Similarly, an overview of systematic reviews showed no difference in function, pain, ROM, or the retear rate between early and conservative rehabilitation. 12 However, another systematic review and meta-analysis concluded that early active ROM is associated with an increased risk of structural defects for small and large rotator cuff tears. 9 A systematic review of overlapping meta-analyses concluded that early motion and delayed motion after rotator cuff repair may lead to comparable functional outcomes and retear rates. 16
In the current systematic review and meta-analysis, 2 RCTs compared ROM between the abduction brace and sling immobilization groups. 1,7 Hollman et al 7 found no significant differences between the groups in external rotation or abduction at 6 weeks, 3 months, and 6 months postoperatively. Conti et al 1 found that abduction, external rotation, internal rotation, and forward flexion were significantly greater in the abduction brace immobilization group than the sling immobilization group during the early phase (within 3 months) after rotator cuff repair. However, after 3 months, no difference was found between the 2 groups. 1 Because the results were presented as medians and ranges by Conti et al, 1 ROM could not be pooled for meta-analysis.
Strengths and Limitations
The current study has some strengths. First, this is the first systematic review and meta-analysis to compare the differences in clinical outcomes and retear rates between abduction brace and sling immobilization during the rehabilitation phase after arthroscopic rotator cuff repair. Second, we included only RCTs, which increased the quality of evidence.
The current meta-analysis also has limitations. First, only 4 studies and 224 patients were included, which indicates that this field of study may require more exploration. Second, the wide variety of clinical outcome measurements and patient inclusion criteria created a heterogeneous study cohort. More high-quality studies are needed to verify the present findings. Third, when comparing the retear rate between groups, the follow-up of only 3 months was too short.
Conclusion
Our systematic review demonstrated a lack of significant differences between the abduction brace and sling immobilization groups regarding postoperative clinical scores, pain severity, and tendon healing. This may suggest that abduction brace immobilization is not necessary after arthroscopic rotator cuff repair.
Final revision submitted March 3, 2023; accepted April 13, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: This work was supported by the National Key Research and Development Program of China (grants 2019YFF030170 and 2020YFC20070405 to H.-Y.L.). AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto. The ethics approval was obtained from the ethics committee of Huashan Hospital, Fudan University.
The ethics approval was obtained from the ethics committee of Huashan Hospital, Fudan University.
References
- 1. Conti M, Garofalo R, Castagna A. Does a brace influence clinical outcomes after arthroscopic rotator cuff repair? Musculoskelet Surg. 2015;99(s uppl 1):S31–S35. [DOI] [PubMed] [Google Scholar]
- 2. Cumpston M, Li T, Page MJ, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:ED000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Ghandour TM, Ibrahim A, Abdelrahman AA, Elgammal A, Hammad MH. Does the type of shoulder brace affect postoperative pain and clinical outcome after arthroscopic rotator cuff repair? Arthroscopy. 2019;35(4):1016–1023. [DOI] [PubMed] [Google Scholar]
- 4. Gimbel JA, Van Kleunen JP, Williams GR, Thomopoulos S, Soslowsky LJ. Long durations of immobilization in the rat result in enhanced mechanical properties of the healing supraspinatus tendon insertion site. J Biomech Eng. 2007;129(3):400–404. [DOI] [PubMed] [Google Scholar]
- 5. Hatakeyama Y, Itoi E, Pradhan RL, Urayama M, Sato K. Effect of arm elevation and rotation on the strain in the repaired rotator cuff tendon: a cadaveric study. Am J Sports Med. 2001;29(6):788–794. [DOI] [PubMed] [Google Scholar]
- 6. Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hollman F, Wolterbeek N, Zijl JAC, van Egeraat SPM, Wessel RN. Abduction brace versus antirotation sling after arthroscopic cuff repair: the effects on pain and function. Arthroscopy. 2017;33(9):1618–1626. [DOI] [PubMed] [Google Scholar]
- 8. Klintberg IH, Gunnarsson AC, Svantesson U, Styf J, Karlsson J. Early loading in physiotherapy treatment after full-thickness rotator cuff repair: a prospective randomized pilot-study with a two-year follow-up. Clin Rehabil. 2009;23(7):622–638. [DOI] [PubMed] [Google Scholar]
- 9. Kluczynski MA, Isenburg MM, Marzo JM, Bisson LJ. Does early versus delayed active range of motion affect rotator cuff healing after surgical repair? A systematic review and meta-analysis. Am J Sports Med. 2016;44(3):785–791. [DOI] [PubMed] [Google Scholar]
- 10. Lapner P, Bouliane M, Pollock JW, et al. Intraoperative channeling in arthroscopic rotator cuff repair: a multicenter randomized controlled trial. Am J Sports Med. 2023;51(2):323–330. [DOI] [PubMed] [Google Scholar]
- 11. Longo UG, Ambrogioni LR, Berton A, et al. Conservative versus accelerated rehabilitation after rotator cuff repair: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2021;22(1):637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Mazuquin BF, Wright AC, Russell S, Monga P, Selfe J, Richards J. Effectiveness of early compared with conservative rehabilitation for patients having rotator cuff repair surgery: an overview of systematic reviews. Br J Sports Med. 2018;52(2):111–121. [DOI] [PubMed] [Google Scholar]
- 13. Minagawa H, Yamamoto N, Abe H, et al. Prevalence of symptomatic and asymptomatic rotator cuff tears in the general population: from mass-screening in one village. J Orthop. 2013;10(1):8–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pandey V, Madi S, Maddukuri S, Acharya K, Karegowda LH, Willems WJ. Does application of abduction brace after arthroscopic rotator cuff repair improve blood flow around posterosuperior rotator cuff and repair site, affecting pain levels and clinical and structural outcomes? A pilot randomized controlled trial. JSES Int. 2020;4(4):848–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Reilly P, Bull AM, Amis AA, et al. Passive tension and gap formation of rotator cuff repairs. J Shoulder Elbow Surg. 2004;13(6):664–667. [DOI] [PubMed] [Google Scholar]
- 16. Saltzman BM, Zuke WA, Go B, et al. Does early motion lead to a higher failure rate or better outcomes after arthroscopic rotator cuff repair? A systematic review of overlapping meta-analyses. J Shoulder Elbow Surg. 2017;26(9):1681–1691. [DOI] [PubMed] [Google Scholar]
- 17. Saul KR, Hayon S, Smith TL, Tuohy CJ, Mannava S. Postural dependence of passive tension in the supraspinatus following rotator cuff repair: a simulation analysis. Clin Biomech (Bristol, Avon). 2011;26(8):804–810. [DOI] [PubMed] [Google Scholar]
- 18. Shen C, Tang ZH, Hu JZ, Zou GY, Xiao RC, Yan DX. Does immobilization after arthroscopic rotator cuff repair increase tendon healing? A systematic review and meta-analysis. Arch Orthop Trauma Surg. 2014;134(9):1279–1285. [DOI] [PubMed] [Google Scholar]
- 19. Sheps DM, Silveira A, Beaupre L, et al. Early active motion versus sling immobilization after arthroscopic rotator cuff repair: a randomized controlled trial. Arthroscopy. 2019;35(3):749–760.e2. [DOI] [PubMed] [Google Scholar]
- 20. Sonoda Y, Nishioka T, Nakajima R, Imai S, Vigers P, Kawasaki T. Use of a shoulder abduction brace after arthroscopic rotator cuff repair: a study on gait performance and falls. Prosthet Orthot Int. 2018;42(2):136–143. [DOI] [PubMed] [Google Scholar]
- 21. Tirefort J, Schwitzguebel AJ, Collin P, Nowak A, Plomb-Holmes C, Lädermann A. Postoperative mobilization after superior rotator cuff repair: sling versus no sling. A randomized prospective study. J Bone Joint Surg Am. 2019;101(6):494–503. [DOI] [PubMed] [Google Scholar]
- 22. Turcotte JJ, Kelly M, West M, Lashgari C, Petre BM, Redziniak DE. Rates of medial and lateral row failure and risk factors for re-tear in arthroscopic double row rotator cuff repair. J Clin Orthop Trauma. 2022;36:102083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Wani Z, Abdulla M, Habeebullah A, Kalogriantis A. Rotator cuff tears: review of epidemiology, clinical assessment and operative treatment. Trauma. 2016;18(3):190–204. [Google Scholar]
- 24. Zhang S, Li H, Tao H, et al. Delayed early passive motion is harmless to shoulder rotator cuff healing in a rabbit model. Am J Sports Med. 2013;41(8):1885–1892. [DOI] [PubMed] [Google Scholar]