Abstract
Background:
Flexible ligamentous fixation has increased in popularity for the treatment of ligamentous Lisfranc injury, but the optimal fixation strategy is unclear.
Purpose:
To review the biomechanical, clinical, and radiographic results of ligamentous Lisfranc injuries treated with flexible fixation.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
A systematic literature review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The PubMed/Medline and Google Scholar literature databases were queried for clinical and biomechanical (cadaveric) studies relating to flexible fixation of ligamentous Lisfranc injury. Outcomes of interest included patient-reported outcome scores, clinical/biomechanical results, radiographic alignment, and return to activity. Where appropriate, meta-analysis of the postoperative outcomes was performed.
Results:
Of the 34 initial studies, 14 articles (243 feet) were included in the analysis. In the 11 clinical studies (216 patients), the mean postoperative American Orthopaedic Foot & Ankle Society score was 90.1 (n = 150; 6 studies) and the mean visual analog scale score was 1.5 (n = 137; 5 studies). The rate of return to activity was 100% (n = 35; 5 studies), and 100% of patients maintained radiographic alignment postoperatively (n = 62; 6 studies). No complications or subsequent hardware removals were reported. Of the 3 biomechanical studies (27 feet), 1 study found significantly greater change in diastasis under axial load between intact and postfixation ligaments with suture button versus screw fixation (+1.1 vs –0.1 mm; P < .05), another found no difference in the decrease in diastasis under axial load between the injured state and screw or suture button fixation (1.2 vs 1.0 mm; P = .5), and the third found no difference in displacement between intact and either screw or suture button fixation under either axial (intact vs screw: 1.0 vs 2.0 mm, P = .1; intact vs suture button: 0.6 vs 1.8 mm, P = .1) or abduction (intact vs screw: 1.5 vs 1.1 mm, P = .5; intact vs suture button: 1.3 vs 2.1 mm, P = .1) load.
Conclusion:
Flexible fixation use in the treatment of ligamentous Lisfranc injury was found to have significant potential as a fixation option, as demonstrated by excellent clinical results. Biomechanical evidence was inconclusive but suggested a trend toward decreased diastasis in specimens fixed with screws compared with suture buttons.
Keywords: Lisfranc injury, suture button, fixation, biomechanics
Lisfranc injuries are of tremendous clinical significance, as failure to appropriately reduce and stabilize the columns of the midfoot can lead to progressive collapse and early-onset arthrosis. 2,34 The optimal fixation strategy for the subset of Lisfranc injuries without concomitant fracture, pure ligamentous, is as of yet unknown. 1,5,6,18,25,30
Traditionally, operative treatment for stabilization of the affected joint has been performed by direct or indirect reduction followed by fixation with a “home run screw,” which may range in size from 3.0 to 4.5 mm. This strategy effectively stabilizes the midfoot but has also been associated with damage to articular cartilage, hardware failure, and need for eventual hardware removal. 1,4,7,14,19,27,34 Because of the potential to alleviate some of these concerns, flexible fixation to reconstruct torn Lisfranc ligaments has become the subject of increased investigation. ∥
Potential benefits of flexible fixation compared with screws include minimized trauma to the articular cartilage of the midfoot and near elimination of the need for hardware removal after recovery. Perhaps most important is the use of a flexible fixation device across a joint that inherently experiences physiologic motion in its intact state. ¶ A similar thought process has led to increased research and ultimately intraoperative use of flexible fixation in ankle syndesmotic injuries, with overall positive results. 13,16,31,32 Currently, the clinical implications of this fixation technique for pure ligamentous Lisfranc injuries are unclear, as most publications have been able to report on only a small series of patients in a retrospective manner. 20,24,25,27,34
The aims of the present review were to report on the outcomes in the existing literature of ligamentous Lisfranc injuries treated with flexible fixation and to pool these data in a meta-analysis to arrive at more robust conclusions. Additionally, we sought to assess and summarize the relevant biomechanical data published on this topic. We hypothesized that flexible fixation for the treatment of Lisfranc injuries would be safe and effective compared with traditional screw fixation and would have fewer complications related to trauma to the adjacent articular cartilage or need for hardware removal.
Methods
Search Strategy
This systematic literature review was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The search strategy was designed to identify studies regarding flexible fixation of Lisfranc injuries including biomechanics, radiographic, and clinical outcomes. We searched the following literature databases: PubMed/Medline and Google Scholar for studies published from 2010 until February 2022. The reference lists of relevant studies were also hand-searched for additional studies. Different combinations of keywords were searched to maximize the search results. The keywords used were as follows: “Lisfranc,” “ligamentous,” “flexible,” “suture button,” “suture tape,” “biomechanics,” “outcomes,” and “radiographic.” All publication dates were included.
Eligibility Criteria
Prospective cohort and retrospective clinical studies were searched and reviewed for inclusion. Biomechanical cadaveric studies were also reviewed for inclusion. Studies were included if they were relevant to Lisfranc injury treated with flexible fixation (suture button or suture tape) and available in the English language. Studies that included ancillary fixation methods for other injuries (eg, intercuneiform screw fixation and tarsometatarsal joint [TMTJ] fixation) were included, and additional procedures were documented. Clinical studies were reviewed for patient-reported and radiographic outcomes. Studies that did not meet these inclusion criteria or clinical studies that lacked quantitative outcomes were excluded, as were published letters, comments, editorials, proceedings, and personal communications.
Study Selection and Data Extraction
Studies that were identified by the search strategy were reviewed for eligibility by first evaluating abstracts of the studies and then by examining the full texts for eligibility for data extraction. Studies were assessed by 2 reviewers (1 orthopaedic surgery resident [D.V.C.] and 1 faculty member [B.C.L.]), and any conflicts were resolved by a third, independent reviewer. Duplicates were removed. The following data were extracted from studies that met the inclusion criteria: name of first author, year of publication, study design, American Orthopaedic Foot & Ankle Society (AOFAS) score, visual analog scale (VAS) pain score, patient satisfaction score, return to activities, and radiographic outcomes.
Outcome Measures
For this meta-analysis, the primary outcome was return to activities (at the end of follow-up). Secondary outcomes were the AOFAS, VAS pain, and patient satisfaction scores, as well as radiographic alignment, revisions/failures, and complications.
Quality Assessment
The Methodological Index for Non-Randomized Studies (MINORS) instrument was used to quantify the quality of the included clinical studies. For noncomparative studies, scores <9 were considered poor quality; 9 to 12, fair quality; and >12, good quality. For comparative studies, scores <14 were considered poor quality; 14 to 18, fair quality; and >18, good quality. 29
Statistical Analysis
Weighted means were calculated for continuous variables (AOFAS and VAS), and overall percentages were calculated for categorical variables (return to activity and radiographic alignment). Because of inconsistent reporting of standard deviations and/or ranges, a weighted standard deviation could not be calculated. Calculations were performed using R Version 3.6.0 (The R Foundation for Statistical Computing).
Results
Of the 43 articles initially identified for review, 14 studies (13 articles and 1 clinical abstract) were included in the final analysis. # There were 11 clinical studies ** and 3 biomechanical studies. 1,27,28 The results of the search process are displayed in Figure 1.
Figure 1.
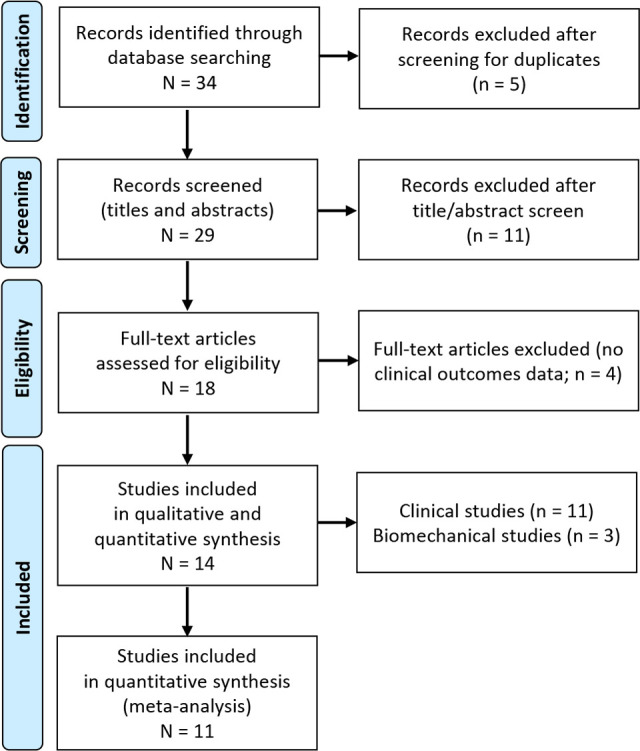
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart of study inclusion.
Clinical Studies
The included clinical studies are summarized in Tables 1 and 2. The mean MINORS score of the 11 studies was 8.9 (range, 4-19). Open reduction was performed in 8 studies, 6 –9,11,18,23,35 with 1 study 33 reporting percutaneous reduction and 2 studies 14,25 not specifying. All studies used the Mini TightRope (Arthrex) between the medial cuneiform and second metatarsal for fixation. Postoperative protocols varied, with most studies restricting patients to nonweightbearing status for 2 to 6 weeks. 6,7,14,18,23,25,33
Table 1.
Characteristics of the Clinical Studies (n = 11 studies; 216 patients) a
| Lead Author (Year) | MINORS Score | n | Mean Age, y | Patient Activity Level | Surgical Technique | Postoperative Protocol | Time to Intervention |
|---|---|---|---|---|---|---|---|
| Brin (2010) 6 | 7 | 5 | 35.4 | 2 professional athletes, 3 recreational athletes | Open reduction; suture button C1-MT2 ± C1-MT1 fusion (additional: 1st TMTJ fixation [60%]) | Wk 0-3: NWB, cast Wk 3: cast removal, PT Wk 5: WBAT |
NR |
| Charlton (2015) 7 | 9 | 7 | 24.6 | 5 professional ballet dancers, 2 D1 college soccer players | Open reduction; suture button C1-MT2 | Wk 0-2: NWB, splint Wk 2-6: boot, NWB Wk 6-8: wean crutches, supportive shoe 3 mo: Barre work (dancers), low-impact training (athletes) 6 mo: full training/participation |
Minimum 6-mo (mean, 14 mo) nonop failure |
| Cho (2021) 8 | 19 | 31 | 40.9 | NR | Open reduction; suture button C1-MT2 | Wk2: ROM, pool therapy Wk3: NWB splint, removal cast for next 3 wk Wk 6-12: PWB Wk 12-16: RTS |
6.2 days |
| Chun (2021) 9 | 7 | 12 | 31.6 | NR | Open reduction; suture button C1-MT2 | All patients returned to daily activities within median of 12.7 mo | NR |
| Cottom (2020) 11 | 4 | 84 | 39.69 | NR | Open reduction; suture button MT2-C1 (additional: C1-C2 screw | Mean time to protected FWB in CAM: 11 days | NR |
| Crates (2015) 14 | 9 | 11 | 29.6 | NR | Suture button C1-MT2 | Wk 0-3: NWB, splint Wk 3-6: boot, WBAT Wk 6-8: WBAT, orthotic, PT Mo 3-4: RTS Mo 4-6: full training/participation |
NR |
| Gee (2019) 18 | 13 | 6 | 29.7 | Active-duty military | Open reduction; suture button C1-MT2 (additional: C1-C2 screw fixation [50%]) | Mean time for NWB: 10 wk | NR |
| Jain (2017) 23 | 8 | 5 | 22.1 | Professional soccer or rugby players | Open reduction; suture button C1-MT2; targeting guide (Wright Medical) | Wk 0-2: NWB, splint Wk 2-6: boot, NWB Wk 6: boot, WBAT Wk 10: nonimpact graduated resistance program Wk 13-14: running Wk 15-17: cutting, twisting, ball work |
NR |
| Tzatzairis (2019) 33 | 5 | 1 | 13 | NR | Percutaneous reduction; suture button C1-MT2 | Wk 0-2: PWB, crutches, boot Wk 2-4: WBAT, boot |
NR |
| Yongfei (2021) 35 | 8 | 11 | 35.4 | NR | Open reduction; suture button C1-MT2 | Wk 6-8: plaster splint, PWB 3 mo: WBAT, return to activity |
4.5 days |
| Kreulen (2019) 25 | NR | 43 | NR | NR | Suture button C1-MT2 | NR | NR |
a CAM, controlled ankle movement boot; C1, medial cuneiform; C2, intermediate cuneiform; D1, Division I; FWB, full weightbearing; MINORS, Methodological Index for Non-Randomized Studies; MT1, first metatarsal; MT2, second metatarsal; nonop, nonoperative; NR, not reported; NWB, nonweightbearing; PT, physical therapy; PWB, partial weightbearing; RTS, return to sport; TMTJ, tarsometatarsal joint; WBAT, weightbearing as tolerated.
Table 2.
Summary of Outcomes for the Clinical Studies a
| Lead Author (Year) | Follow-up | Clinical Outcomes | Radiographic Outcomes | Complications |
|---|---|---|---|---|
| Brin (2010) 6 | 12 mo |
|
NR | No wound healing or any early complications |
| Charlton (2015) 7 | 25 mo |
|
100% maintained alignment | No wound healing, dehiscence, or other early complications |
| Cho (2021) 8 | 16 mo |
|
|
|
| Chun (2021) 9 | 13.2 mo |
|
Significant decrease in diastases | No reported complications |
| Cottom (2020) 11 | 3.4 y | 3 y: VAS score, 1.3 ± 1.57; AOFAS score, 90.64 ± 12.18 | Final WB XR demonstrated significant step-off of 0.43 mm |
|
| Crates (2015) 14 | 33 mo | NR | NR |
|
| Gee (2019) 18 | 12.4 mo |
|
100% maintained alignment |
|
| Jain (2017) 23 | 24 mo |
|
100% maintained alignment |
|
| Tzatzairis (2019) 33 | 3 mo | Symptom-free | Maintained alignment | No reported complications |
| Yongfei (2021) 35 | 20.5 mo | Last f/u: AOFAS score, 92.4 ± 4.3; Maryland foot score, 94.1 ± 3.5; VAS score, 1.5 ± 0.7 | Distance between MT1 and MT2 significantly shorter than preop | No wound or implant complications |
| Kreulen (2019) 25 | 9 mo | NR | Reduction accuracy (injured vs noninjured)
|
No reported complications |
a AOFAS, American Orthopaedic Foot & Ankle Society; AP, anterior-posterior; C2, intermediate cuneiform; CT, computed tomography; f/u, follow-up; MT1, first metatarsal; MT2, second metatarsal; postop, postoperative; preop, preoperative; TMTJ, tarsometatarsal joint; VAS, visual analog scale; WB, weightbearing; XR, radiograph.
Notably, some differences did exist among surgical techniques. Cottom et al 11 performed simultaneous intercuneiform screw fixation between medial and intermediate cuneiforms in all 84 of their patients, with additional Kirschner wire fixation of third and fourth metatarsals in 1 patient. Gee et al 18 reported intercuneiform screw fixation in 50% of their 6 patients. Brin et al 6 also evaluated the first TMTJ and performed fixation in 3 of their 5 patients.
Biomechanical Studies
The results of the included biomechanical studies are outlined in Table 3. Ahmed et al 1 compared fixation from the medial cuneiform to the second metatarsal with either the Mini Tightrope or a 4.0-mm partially threaded cannulated screw by measuring the distance between the first and second metatarsals. This was done in 8 matched-pair cadaveric specimens with intact, transected, and reconstructed Lisfranc ligaments. The authors applied a 600-N axial load and also performed load-to-failure testing at a rate of 50 mm/min and found that when comparing reconstructed with intact Lisfranc ligament diastases under axial load, screw fixation yielded a mean diastasis of –0.01 mm and suture button fixation of +1.1 mm, which was a statistically significant difference. Additionally, their comparisons of reconstructed specimens with and without axial load demonstrated that screw fixation resulted in +0.2-mm diastasis and suture button, +1.2 mm. This difference was statistically significant as well. Load-to-failure testing demonstrated no significant difference between the screw and suture button. The primary conclusion of the study was that fixation with a 4.0-mm partially threaded cannulated screw resulted in less displacement than the Mini Tightrope in this model of isolated Lisfranc ligament injuries. 1
Table 3.
Characteristics of the Biomechanical Studies (n = 3 studies; 27 feet) a
| Lead Author (Year) | No. of Feet | Comparison | Measurements | Load | Results | Conclusion |
|---|---|---|---|---|---|---|
| Ahmed (2010) 1 | 8 | Suture button vs 4.0-mm partially threaded cannulated screw C1-MT2 | M1-M2 distance, load to failure | Axial: 600 N; load to failure: 50 mm/min |
|
Screw resulted in less displacement than suture button in isolated Lisfranc ligament injuries |
| Panchbhavi (2009) 27 | 14 | Suture button vs 3.5-mm canulated lag screw C1-MT2 | C1-MT2 Lisfranc ligament attachment site displacement | Axial: 343 N |
|
Suture button and screw did not differ significantly in displacement in isolated Lisfranc ligament injuries |
| Pelt (2011) 28 | 5 | Suture button C1-MT2 with K-wire MT2-C2 vs 3.5-mm full threaded cortical screw ×2—C1-MT2, MT2-C2 | C1-MT2 distance | Axial: 222.4 N; abduction: 50 N; 1000 cycles, then retested |
|
|
a C1, medial cuneiform; C2, intermediate cuneiform; K-wire, Kirschner wire; M1/MT1, first metatarsal; M2/MT2, second metatarsal; postop, postoperative; preop, preoperative; TMTJ, tarsometatarsal joint.
Panchbhavi et al 27 reported on 14 matched-pair cadaveric specimens fixed with either a Mini Tightrope or a 3.5-mm cannulated lag screw from the medical cuneiform to the second metatarsal base and measured displacement at the Lisfranc ligament attachment sites under an axial load of 343 N. They reported that both screw and suture button fixation demonstrated significant improvements in diastasis compared with the unfixed injury model. Compared with intact specimens, screw fixation yielded an increase in displacement of 0.1 mm and suture button, 0.3 mm. Neither displacement was significant compared with the intact model. Additionally, the difference between the 2 fixation methods was not statistically significant. 27
Pelt et al 28 fixed 5 matched-pair cadaveric specimens with either the Mini Tightrope or a 3.5-mm fully threaded cortical screw between the medial cuneiform and second metatarsal. The suture button group also underwent fixation of the second TMTJ with 0.062-inch Kirschner wire, while the screw group underwent second TMTJ fixation with a 3.5-mm fully threaded cortical screw. The distance between the medial cuneiform and second metatarsal was measured under an axial load of 222.4 N and abduction load of 50 N. The effect of performing 1000 load cycles was then evaluated. They found that abduction stress results in greater diastasis in the injury model than axial. Under either axial or abduction loads, neither screw nor suture button demonstrated statistically significant differences in diastasis compared with the intact state, thereby suggesting that either fixation method may restore stability to a level comparable to the intact state. Additionally, cyclic loading did not have a statistically significant effect on measured diastasis. Their overall conclusions were that abduction stress results in greater displacement at the Lisfranc joint than axial and that neither suture button nor screw fixation states differ significantly from intact displacement under load. 28
Clinical Results
A total of 216 patients were included between the 11 clinical studies. †† The mean age of all included patients was 36.7 years (range, 11-57 years), and the mean time to follow-up was 25.4 months (range, 3-60 months). Data were pooled and meta-analysis was performed where possible, with results outlined in Table 4. Among the 5 clinical studies 6,7,9,18,23 that reported return-to-activity rates, all 35 patients reported full return. Two studies 6,23 reported satisfaction rates, and among their 10 combined patients, only 1 reported less than very high or excellent subjective results. AOFAS scores were pooled from 6 studies, 7 –9,11,23,35 with a mean score among 150 patients of 90.1 at a mean time of 30.7 months; this indicates an excellent result. 10 VAS scores were reported in 5 studies, 8,11,18,23,35 and among the 137 patients, the mean score was 1.5 at a time of 30.8 months; this is consistent with minimal or no pain. 17,24
Table 4.
Results of Meta-analysis of Suture Button Fixation a
| AOFAS | VAS | Return to Activity | Radiographic Results | |
|---|---|---|---|---|
| No. of studies | 6 | 5 | 5 | 6 |
| No. of patients | 150 | 137 | 35 | 62 |
| Mean age, y | 37.7 | 38.5 | 29.1 | 34.2 |
| Mean time of follow-up, mo | 30.7 | 30.8 | NR | NR |
| Mean outcome score | 90.1 | 1.5 | 100% return | 100% maintained alignment |
a AOFAS, American Orthopaedic Foot & Ankle Society Score; NR, not reported; VAS, visual analog scale.
Cho et al 8 found significantly inferior clinical outcomes associated with conventional screw fixation in comparison with suture button fixation. Interestingly, they also examined plantar foot pressure 4 to 6 months postoperatively and found significantly elevated foot pressure in the conventional screw fixation group at the great toe and first metatarsal head area compared with the contralateral foot. They proposed that inferior clinical outcomes of screw fixation could be associated with the increased metatarsal foot pressure, which may have been secondary to the increased rigidity of the Lisfranc and TMTJs. 8
Radiographic Results
Radiographically, all 62 patients in 6 studies with radiographic data were found to have maintained alignment at final radiographic follow-up. 7,13 –15,18,23 Kreulen et al 25 compared injured and uninjured feet in their 43 patients at 6 weeks postoperatively. The distance between the medial cuneiform and second metatarsal, as well as that between the first and second metatarsals, was measured and found to not differ significantly between sides. Chun et al 9 compared Lisfranc diastasis on the standing foot radiograph preoperatively and 1 year postoperatively with mean diastases of 2.91 versus 0.14 respectively, showing a significant mean difference.
Cho et al 8 also compared radiologic parameters between suture button and traditional screw fixation and found no significant difference between groups in terms of diastasis and side-to-side difference measured on weightbearing anterior-posterior radiographs. Dorsal and plantar diastasis measured on weightbearing computed tomography also showed no significant difference.
In the largest cohort of patients examined by Cottom et al 11 at a minimum 3-year follow-up, they found an increase in step-off at the final follow-up. They found that there was a 0.2-mm increase in diastasis on average; however, they indicate that this is possibly related to patient positioning for radiographs and changes in weightbearing status from initial to final radiographs. 12
Discussion
The present systematic review on flexible fixation of ligamentous Lisfranc injury (14 articles: 11 clinical retrospective series [216 patients] and 3 biomechanical studies [27 feet]) demonstrated excellent clinical and radiographic outcomes for patients undergoing suture button fixation, while biomechanical studies have yielded mixed findings when comparing suture button with traditional screw fixation in cadaveric models. This study contributes to the existing literature on flexible fixation of ligamentous Lisfranc injury by summarizing the results of biomechanical and clinical studies and meta-analyzing clinical outcomes. To our knowledge, it is the first to do so in a comprehensive manner and lays the foundation for future clinical and biomechanical studies on this topic.
The biomechanical publications report mixed results when comparing diastasis resulting from screw fixation, suture button fixation, and intact Lisfranc ligament states. 1,27,28 While Ahmed et al 1 reported a decrease in displacement in screw compared with suture button fixation in their model of ligamentous Lisfranc injury, Panchbhavi et al, 27 did not demonstrate such a difference. Of note, both of these studies used only axial load for testing purposes. Pelt et al, 28 who also reported on results of abduction load, were unable to demonstrate a statistically significant difference between specimens with intact Lisfranc ligaments and either screw or suture button fixation. However, they did not directly compare diastases of screw and suture button fixation under abduction load. Their results would appear to trend toward significance, with screw fixation yielding –0.4-mm diastasis and suture button fixation yielding +0.6-mm diastasis compared with intact specimens. However, these results may be confounded by the fact that the screw group had a 3.5-mm cortical screw stabilizing the second TMTJ, while the suture button group had only a 0.062-inch Kirschner wire. Furthermore, it is also possible that this study was underpowered with a sample size of only 5 matched pairs. Notably, neither load to failure nor effect of cyclic loading was demonstrated to cause a difference in either group. The biomechanical data, as a whole, are inconclusive, with only 1 study 1 demonstrating a statistically significant difference in diastasis between fixation types. That is, screw fixation resulted in reduced M1-M2 diastasis compared with suture button fixation, although this difference was not >1.2 mm. The clinical significance of this difference is uncertain, as biomechanical data indicate that specimens with intact Lisfranc ligaments yield nearly 3 mm of intermetatarsal diastasis and approximately 1 mm of medial cuneiform–second metatarsal diastasis under axial load. 3,28
Overall, clinical outcomes of ligamentous Lisfranc injury treated with suture button fixation have been encouraging in each of the individual studies included here. ‡‡ All these studies are retrospective case series with relatively small sample sizes. However, when considering them as a whole and combining results into meta-analysis, the same conclusion is reached, with a mean AOFAS score of 90.1 (excellent), a mean VAS score of 1.5 (minimal or no pain), and 100% return to activity with no reported hardware complication or removal. 10,17,24 This is also true of the radiographic results reported by these studies, with all studies reporting maintained alignment on final images. 7,13 –15,18,23
The overall clinical and radiographic results of suture button fixation of ligamentous Lisfranc injury suggest that it may be a reliable fixation construct and warrants direct comparison with clinical results after screw fixation. A prospective randomized study is lacking but would contribute greatly to determining a definitive answer to the question of whether suture button fixation is superior or equivalent to screw fixation when used in practice. Biomechanical data to date have provided mixed results but demonstrate that it is essential for future studies to compare the screw not only against suture button fixation but also against the intact state, as there exists some physiologic motion between the first and second metatarsals and the second metatarsal and medial cuneiform. 1,26 –28 Furthermore, based on the results of Pelt et al, 28 future studies should include abduction stress testing as part of the examination, as this was found to result in greater diastasis than axial load in the injury model (6.8 vs 2.0 mm, a statistically significant result). Further investigation has begun on the impact of varying the form of flexible fixation on postoperative results. 21,22 The use of the Arthrex Internal Brace (Arthrex), for example, has been described with the reported advantages of allowing for collagen ingrowth along the suture tape while decreasing iatrogenic bone and cartilage loss associated with suture button placement. 21,22 However, it remains to be seen to what degree such alternative methods of flexible fixation will be used in clinical practice given the difficulty of achieving an anatomic reduction, which is critical for the Lisfranc articulation.
Although the present review contributes to the existing literature, it is not without its own weaknesses. The studies included are retrospective and have small sample sizes. In addition, there is heterogeneity in surgical techniques and postoperative rehabilitation protocols (eg, weightbearing status and cast/splint immobilization) of uncertain significance among the included studies, and meta-analysis was limited by the lack of standardized reporting measures in these publications. VAS and AOFAS scores are potentially meaningful markers but were used inconsistently in outcome measurement. The nature of a systematic review and meta-analysis is such that the final outcome is limited by the preexisting literature, which in this case is primarily composed of low-quality evidence. However, this study does successfully summarize the most current knowledge on a topic of research interest and surgical relevance and, where possible, combines results from a series of small studies into a larger sample size from which more robust conclusions may be drawn.
Conclusion
The results of the present investigation demonstrate that suture button fixation is comparable to traditional screw fixation for the treatment of ligamentous Lisfranc injuries based on clinical and radiographic results. Biomechanical evidence has been inconclusive to date due in part to limited focus on abduction stress testing and in some cases small sample sizes. A prospective randomized clinical trial is lacking but is recommended based on the findings presented here.
Acknowledgment
The authors acknowledge Loretta Chou, MD, foot and ankle surgeon at Stanford University, for her contributions to this study.
Footnotes
Final revision submitted March 13, 2023; accepted April 14, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: D.V.C. has received education payments from Evolution Surgical. B.C.L. has received grant support from DJO, Evolution Surgical, and Zimmer Biomet; education payments from Smith & Nephew and Southtech Orthopedics; honoraria from Wright Medical; and hospitality payments from Crossroads Extremity Systems and Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ahmed S, Bolt B, McBryde A. Comparison of standard screw fixation versus suture button fixation in Lisfranc ligament injuries. Foot Ankle Int. 2010;31(10):892–896. [DOI] [PubMed] [Google Scholar]
- 2. Aronow MS. Treatment of the missed Lisfranc injury. Foot Ankle Clin. 2006;11(1):127–142, ix. [DOI] [PubMed] [Google Scholar]
- 3. Bansal A, Carlson DA, Owen JR, et al. Ligamentous Lisfranc injury: a biomechanical comparison of dorsal plate fixation and transarticular screws. J Orthop Trauma. 2019;33(7):e270–e275. [DOI] [PubMed] [Google Scholar]
- 4. Boffeli TJ, Pfannenstein RR, Thompson JC. Combined medial column primary arthrodesis, middle column open reduction internal fixation, and lateral column pinning for treatment of Lisfranc fracture-dislocation injuries. J Foot Ankle Surg. 2014;53(5):657–663. [DOI] [PubMed] [Google Scholar]
- 5. Briceno J, Stupay KL, Moura B, Velasco B, Kwon JY. Flexible fixation for ligamentous Lisfranc injuries. Injury. 2019;50(11):2123–2127. [DOI] [PubMed] [Google Scholar]
- 6. Brin YS, Nyska M, Kish B. Lisfranc injury repair with the TightRope device: a short-term case series. Foot Ankle Int. 2010;31(7):624–627. [DOI] [PubMed] [Google Scholar]
- 7. Charlton T, Boe C, Thordarson DB. Suture button fixation treatment of chronic Lisfranc injury in professional dancers and high-level athletes. J Dance Med Sci. 2015;19(4):135–139. [DOI] [PubMed] [Google Scholar]
- 8. Cho J, Kim J, Min TH, et al. Suture button vs conventional screw fixation for isolated Lisfranc ligament injuries. Foot Ankle Int. 2021;42(5):598–608. [DOI] [PubMed] [Google Scholar]
- 9. Chun DI, Kim J, Min TH, et al. Fixation of isolated Lisfranc ligament injury with the TightRope: a technical report. Orthop Traumatol Surg Res. 2021;107(6):102940. [DOI] [PubMed] [Google Scholar]
- 10. Cook JJ, Cook EA, Rosenblum BI, Landsman AS, Roukis TS. Validation of the American College of Foot and Ankle Surgeons scoring scales. J Foot Ankle Surg. 2011;50(4):420–429. [DOI] [PubMed] [Google Scholar]
- 11. Cottom JM, Graney CT, Sisovsky C. Treatment of Lisfranc injuries using interosseous suture button: a retrospective review of 84 cases with a minimum 3-year follow-up. J Foot Ankle Surg. 2020;59(6):1139–1143. [DOI] [PubMed] [Google Scholar]
- 12. Cottom JM, Hyer CF, Berlet GC. Treatment of Lisfranc fracture dislocations with an interosseous suture button technique: a review of 3 cases. J Foot Ankle Surg. 2008;47(3):250–258. [DOI] [PubMed] [Google Scholar]
- 13. Cottom JM, Hyer CF, Philbin TM, Berlet GC. Treatment of syndesmotic disruptions with the Arthrex Tightrope: a report of 25 cases. Foot Ankle Int. 2008;29(8):773–780. [DOI] [PubMed] [Google Scholar]
- 14. Crates JM, Barber FA, Sanders EJ. Subtle Lisfranc subluxation: results of operative and nonoperative treatment. J Foot Ankle Surg. 2015;54(3):350–355. [DOI] [PubMed] [Google Scholar]
- 15. Delman C, Patel M, Campbell M, Kreulen C, Giza E. Flexible fixation technique for Lisfranc injuries. Foot Ankle Int. 2019;40(11):1338–1345. [DOI] [PubMed] [Google Scholar]
- 16. den Daas A, van Zuuren WJ, Pelet S, van Noort A, van den Bekerom MP. Flexible stabilization of the distal tibiofibular syndesmosis: clinical and biomechanical considerations: a review of the literature. Strategies Trauma Limb Reconstr. 2012;7(3):123–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gallagher EJ, Liebman M, Bijur PE. Prospective validation of clinically important changes in pain severity measured on a visual analog scale. Ann Emerg Med. 2001;38(6):633–638. [DOI] [PubMed] [Google Scholar]
- 18. Gee S, Harris MC, Anderson C, Groth A, Ryan P. Lisfranc open reduction and internal fixation in an athletic population: screw versus suture button fixation. Curr Orthop Pract. 2019;30(4):323–326. [Google Scholar]
- 19. Granberry WM, Lipscomb PR. Dislocation of the tarsometatarsal joints. Surg Gynecol Obstet. 1962;114:467–469. [PubMed] [Google Scholar]
- 20. Heyrani N, Hopkins JN, Ngyuyen KN, Kreulen C, Giza E. Flexible fixation treatment strategies for low-energy Lisfranc injuries. Tech Foot Ankle Surg. 2019;18(1):23–28. [Google Scholar]
- 21. Hopkins J, Heyrani N, Kreulen C, Garcia T, Christiansen B, Giza E. InternalBrace has comparable stiffness and strength as Tightrope for Lisfranc fixation. Foot Ankle Orthop. 2017;2(3):2473011417S0001. [Google Scholar]
- 22. Hopkins J, Nguyen K, Heyrani N, et al. InternalBrace has biomechanical properties comparable to suture button but less rigid than screw in ligamentous Lisfranc model. J Orthop. 2020;17:7–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jain K, Drampalos E, Clough TM. Results of suture button fixation with targeting device aid for displaced ligamentous Lisfranc injuries in the elite athlete. Foot (Edinb). 2017;30:43–46. [DOI] [PubMed] [Google Scholar]
- 24. Jensen MP, Chen C, Brugger AM. Interpretation of visual analog scale ratings and change scores: a reanalysis of two clinical trials of postoperative pain. J Pain. 2003;4(7):407–414. [DOI] [PubMed] [Google Scholar]
- 25. Kreulen C, Golshani B, Nikpour A, et al. Radiographic outcomes of Lisfranc injuries treated with a suture button device. Foot Ankle Orthop. 2016;1(1):10.1177/2473011416S00258. [Google Scholar]
- 26. Nery C, Baumfeld D, Baumfeld T, et al. Comparison of suture-augmented ligamentplasty to transarticular screws in a Lisfranc cadaveric model. Foot Ankle Int. 2020;41(6):735–743. [DOI] [PubMed] [Google Scholar]
- 27. Panchbhavi VK, Vallurupalli S, Yang J, Andersen CR. Screw fixation compared with suture-button fixation of isolated Lisfranc ligament injuries. J Bone Joint Surg Am. 2009;91(5):1143–1148. [DOI] [PubMed] [Google Scholar]
- 28. Pelt CE, Bachus KN, Vance RE, Beals TC. A biomechanical analysis of a tensioned suture device in the fixation of the ligamentous Lisfranc injury. Foot Ankle Int. 2011;32(4):422–431. [DOI] [PubMed] [Google Scholar]
- 29. Slim K, Nini E, Forestier D, et al. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 30. Smith N, Stone C, Furey A. Does open reduction and internal fixation versus primary arthrodesis improve patient outcomes for Lisfranc trauma? A systematic review and meta-analysis. Clin Orthop Relat Res. 2016;474(6):1445–1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Solan MC, Davies MS, Sakellariou A. Syndesmosis stabilisation: screws versus flexible fixation. Foot Ankle Clin. 2017;22(1):35–63. [DOI] [PubMed] [Google Scholar]
- 32. Thornes B, Walsh A, Hislop M, Murray P, O’Brien M. Suture-Endobutton fixation of ankle tibio-fibular diastasis: a cadaver study. Foot Ankle Int. 2003;24(2):142–146. [DOI] [PubMed] [Google Scholar]
- 33. Tzatzairis T, Firth G, Parker L. Adolescent Lisfranc injury treated with TightRope™: a case report and review of literature. World J Orthop. 2019;10(2):115–122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Watson TS, Shurnas PS, Denker J. Treatment of Lisfranc joint injury: current concepts. J Am Acad Orthop Surg. 2010;18(12):718–728. [DOI] [PubMed] [Google Scholar]
- 35. Yongfei F, Chaoyu L, Wenqiang X, et al. Clinical outcomes of TightRope system in the treatment of purely ligamentous Lisfranc injuries. BMC Surg. 2021;21(1):395. [DOI] [PMC free article] [PubMed] [Google Scholar]


