Abstract
In recent years, health partnerships have shared infection prevention and control innovations between United Kingdom hospitals and Low-Middle-Income Countries. However, none had focused on antimicrobial stewardship (AMS), a core component of tackling antimicrobial resistance (AMR). This paper documents an effective approach to developing a program to increase AMS capacity in four African countries: Ghana, Tanzania, Uganda, and Zambia as part of the Commonwealth Partnerships for Antimicrobial Stewardship (CwPAMS) program. A systematic approach was applied to assess gaps in AMS interventions and inform the development of the CwPAMS program through deskbased assessments, including National Action Plans on AMR, online focus group meetings, and expert advisory group reviews. Twelve partnerships were selected for the CwPAMS program. AMS support tools were developed based on recommendations from the scoping, including an AMS checklist tool, a healthcare worker knowledge and attitudes questionnaire, and an antimicrobial prescribing app to support clinical decision-making. Training workshops on AMS were developed and delivered to volunteers in Africa and the UK using a train-the-trainer model. The tools and workshops facilitated capacity building for AMS through the generation and strengthening of knowledge, skills, commitment, structures, systems, and leadership among stakeholders in the UK and Africa. The overall average rating assigned to the program following independent evaluation using the Organisation for Economic Cooperation and Development Assistance Committee Evaluation Criteria was very good. The evaluation also highlighted that the majority of the HPs (75%) focused on AMS and/or improved prescribing practice; all HPs have developed and implemented AMS strategies, guidelines, and tools within their hospitals; and NHS staff were able to translate the knowledge and skills they had received early on in the program into clinical practice in response to COVID-19 challenges.
Key words: CwPAMS, one health, pharmacy, multi-disciplinary working, AMS, health partnership
Introduction
Addressing antimicrobial resistance
Whilst governments, public health institutes and professional organisations have a key role in tackling antimicrobial resistance (AMR), healthcare workers and the public also need to contribute to the efforts.1 Multiple factors including poor infection prevention and control (IPC) measures lack of regulatory restrictions on antimicrobial access in the community, and overuse and misuse of antimicrobials contribute to the development of AMR.2 A crosssectoral one-health approach is important for tackling AMR as it recognizes the interconnectedness of human health, animal health, agriculture and the environment.3 There is a need for concerted efforts within and between nations to mobilize the necessary tools to tackle the threat of AMR.4 This can be achieved through the development of regulations and guided by a global action plan to tackle AMR.3
Analysis of the WHO self-assessment survey results highlighted that 79% (154/194) of WHO’s Member States had made progress during 2017-2018. More Commonwealth countries (51%) had a national action plan compared to 48% of countries globally; 25% of Commonwealth countries compared to 26% of all countries had a national action plan currently under development; lastly, 6% and 5% of Commonwealth countries and all countries had no action plan on AMR, respectively.5 The Commonwealth Pharmacists Association (CPA) has been supporting member organizations in Commonwealth countries to implement relevant aspects of the WHO Global AMR Action Plan objectives. One way is through a health partnership program in collaboration with the Tropical Health and Education Trust (THET).6
Health partnerships
Health partnerships (HPs) are a model for improving health and health services based on co-development between actors and institutions from different countries.7 The partnerships are longterm, but not permanent, and based on ideas of reciprocal learning and mutual benefits. The judicious use of institutional HPs to fortify health service delivery is gaining increasing acknowledgment.8 Partnerships are actively encouraged between low and middle-income countries (LMIC) and high-income countries because of the benefits they can confer on both health systems.9,10
Evaluation findings from the Health Partnership Scheme (HPS), funded by the UK Department for International Development and managed by THET (which supported partnerships between UK and LMIC health organizations in 32 countries), demonstrated the effectiveness of HPs.11 The impact was viewed with respect to effectiveness, value for money, relevance, volunteering, and UK health system impact, monitoring, evaluation, and learning.11 HPS projects often improved the knowledge, skills, and confidence of LMIC health workers and frequently resulted in increased quality of care or new services. Training and education capacity, accreditation, and curricula have been improved in several countries. The HPS benefited individuals volunteering their time and the UK health system by providing opportunities to learn and enhance important competencies that were brought back to the UK workplace. Overall, HPS was successful in strengthening partnerships and project approaches, increasing the chances of sustainability and wide-scale change.12
Establishment of the commonwealth partnerships for antimicrobial stewardship
Building on lessons from the HPS described above, the Commonwealth Partnerships for Antimicrobial Stewardship (CwPAMS) was created. CwPAMS (funded by the UK aid fund, the Fleming Fund, managed by the Department of Health and Social Care), aimed to build antimicrobial stewardship (AMS) capacity through sharing skills and knowledge by bringing together multidisciplinary teams from the National Health Service (NHS) and hospitals in four countries in Africa: Ghana, Tanzania, Zambia, and Uganda. It was a pioneering program run by the CPA and THET and was the first health partnership scheme to focus on AMS, including surveillance, IPC, and antimicrobial pharmacy expertise and capacity.6
How did we get started: scoping
The CwPAMS program design was informed by a desk scoping study conducted in October 2018 to assess AMS related gaps and opportunities in the four countries. Scoping studies were undertaken by CPA for each of the focus countries. The scoping studies analyzed key AMR priority areas in each country by assessing AMR National Action Plans (NAPs) to identify gaps in AMR initiatives and inform the scope of the call for applications. At the project level, all the health partnerships conducted a local and national level scoping study to inform their project aims, objectives, and activities, and as a result, all project activities and objectives were both contextually relevant and in line with NAPs.
The research and program team agreed on the information that would be required to inform the AMS-related grant call criteria described in Supplementary Table 1.
Call for and selection of projects
The call for applications for the CwPAMS program was announced in 2018.13 Following a competitive process, twelve partnerships between UK institutions and institutions in Ghana, Tanzania, Uganda and Zambia to tackle the growing challenge of AMR were selected for a 15-month program to run from February 2019 until April 2020. Multidisciplinary healthcare teams, which all included pharmacists, were awarded funding as indicated in Supplementary Table 2.
Programmatic support for the partnerships
The CPA provided technical expertise and hands-on support to HPs, and this was integral to the success achieved by the partnerships. This included the scoping of the program at the initial stages, supporting the development of evidence-based standards, guidelines and protocols, the provision of the AMS Checklist tool and other training tools and materials. This also involved training on data collection for Global Point Prevalence Surveys and the development of mentorship and networking platforms for CwPAMS with a range of learning resources to aid shared learning. Based on feedback from the scoping exercise which revealed that countryspecific antimicrobial prescribing guidelines were difficult to access in hospitals, CPA developed the CwPAMS antimicrobial prescribing smartphone app using each of the national standard treatment guidelines. Additionally, CPA in collaboration with Health Education England developed the Chief Pharmaceutical Officers’ Global Health (CPhOGH) Fellowship and took the lead in leadership training for the fellows. Supplementary Table 3 highlights support offered by the CPA and the number of partnerships that reported using the support.
THET led grant management and programmatic support for partnerships. Each HP benefited from an assigned grant officer, and THET provided support for project planning, project and financial management, reporting, and Monitoring, Evaluation and Learning (MEL), as well as support in matters related to sustainability, safeguarding, and health system strengthening. This included running (in collaboration with CPA) webinars on topics such as MEL and communications, finance and project management, providing individual assistance in finalizing baselines and MEL templates, holding regular progress meetings to identify and support areas for improvement, and helping partners to strengthen the effectiveness of their HP through partnership development plans. CPA and THET also supported the HPs through shared learning events midway and at the culmination of the projects. A range of tools and training courses developed and delivered at a programmatic level are highlighted in Figure 1.
Chief pharmaceutical officers’ global health fellowship
To complement the learning for the CwPAMS program, the CPhOGH Fellowship was developed to expand the knowledge gained by NHS pharmacists under the CwPAMS program in ways that would enhance their leadership and project management skills. Following a competitive selection process, 16 NHS pharmacists volunteering as part of the HPs in the CwPAMS program were appointed as the first CPhOGH Fellows. The fellowship spanned a period of 18 months, with each fellow leading a project in one of the partnership institutions among other responsibilities. The impact of a Global Health Fellowship on pharmacists’ leadership skills and consideration of benefits to the NHS were assessed and published and are highlighted in Figure 2.14
Evaluating the program
A logical framework was designed shortly after the call for proposals was launched. Based on the scoping assessment and grant call criteria, this included three outputs, three outcomes, and a series of fourteen cross-program indicators. Once designed, awarded HPs completed MEL plans based on the log frame. These included project-specific outputs, outcomes and indicators that could be aggregated across the 12 partnerships and fed into the log frame, at regular periods throughout implementation, to provide a quantitative and macro-assessment of the progress being made by CwPAMS.
Evaluation of the CwPAMS program and individual HPs was conducted through an independent assessment by Ingentium Limited. It was based on the three overarching evaluation questions, the Organisation for Economic Cooperation and Development Assistance Committee (OECD-DAC) Evaluation Criteria and indicators that were developed as part of the logical framework.15 In Figure 3, we highlight a summary of the methods used in evaluating the program.
Ethical approval was not required as per NHS Health Research Authority guidance because this was a service evaluation of CPA’s and THET’s program of activities to lead the CPhOGH Fellowship.16 Hospital administration/management board and senior leadership granted approval for the partnership, memorandum of understanding, and CwPAMS project proposal before the commencement of the projects. Data were anonymized and informed consent was obtained as part of the data collection.
The overarching questions included, first the Proof-of-concept: To what extent has the CwPAMS program improved AMS in LMIC partner healthcare institutions? Also, does the HP approach improve AMS in LMIC partner healthcare institutions and staff?; second: what is the value to the NHS of its volunteers participating in the CwPAMS project? How are skills and experiences absorbed within the UK healthcare institution, and is there evidence of a “skills exchange” between UK volunteers and their counterparts in the LMIC?; lastly: what is the potential for scaling up AMS in NAPs?
The results of the evaluation showed approximately 75% of HPs focused on AMS and/or improved prescribing practice; all HPs have developed and implemented AMS strategies, guidelines and tools within their hospitals; NHS staff were able to translate the knowledge and skills they had received early on in the program into clinical practice in response to COVID-19 challenges. Supplementary Table 4 shows more results on the extent to which the partnership objectives were achieved. The program’s OECDDAC Evaluation Criteria overall score was 82% and the individual scores for effectiveness, impact, sustainability, relevance and efficiency were 96%, 85%, 85%, 73%, and 58% respectively (Figure 4). Other key program achievements are explained further below.
Figure 1.
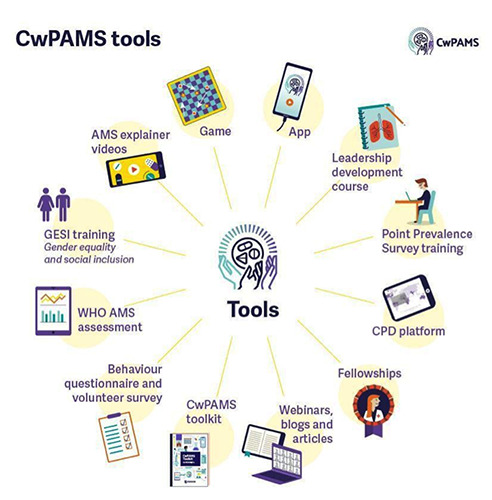
Tools developed during the Commonwealth Partnerships for Antimicrobial Stewardship Program.
Figure 2.
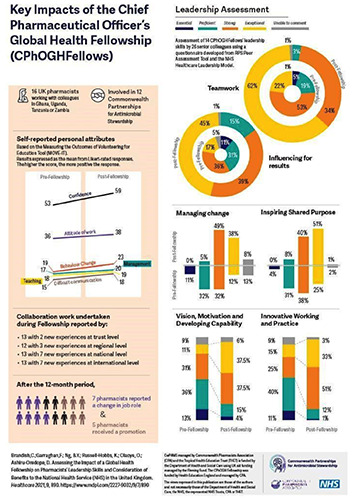
Key impacts of the Chief Pharmaceutical Officers’ Global Health Fellowship.
Extent to which commonwealth partnerships for antimicrobial stewardship has influenced antimicrobial stewardship policy
There is evidence that HPs were able to influence AMS at the policy level and gain the support of relevant stakeholders. This was achieved through the involvement of national bodies as well as representatives for the Ministries of Health (MoH) in LMICs in the partnerships. The CPA played a specific role in the engagement of national and governmental bodies as well as in influencing the AMS agenda on a national level. THET Country Directors were in constant communication with the LMIC MoH representatives, and HPs were registered in relevant committees. As a result, HPs have been able to engage important stakeholders and influence AMS policies in hospitals, as shown in Supplementary Table 5.
Benefit of the commonwealth partnerships for antimicrobial stewardship program to the National Health Service in the United Kingdom
The program contributed positively to the UK health institutions (NHS) in a few ways. Volunteers gained skills and knowledge pertinent to their careers and some earned new roles within their hospital departments (for example seven CPhOGH Fellows reported a change in job role and five received a promotion before the end of their CwPAMS project and fellowship year).14
Knowledge exchange between LMIC and UK partners was evident, both online and offline. The former was demonstrated in the webinars and conferences hosted by THET and CPA. An excellent example of the latter was a new partnership, which, at the beginning of Q4, hosted a doctor, nurse, and pharmacist from Ghana in the UK to demonstrate the process of stewardship and quality improvement programs at the respective UK NHS trust. The visit was considered successful as it also gained recognition at the NHS trust board level and was featured in the highly influential Chief Medical Officer’s Annual Report.
NHS staff were able to translate their knowledge and skills from training into clinical practice in response to COVID-19 challenges. For example, at the start of the pandemic, alcohol hand gel was in short supply in the UK and one hospital learned how to manufacture alcohol hand gel from its African partners.17
Throughout the program, HPs acknowledged increased retention and much happier staff. This had a positive impact on their work, where volunteers were referenced as good role models for their respective departments.
Due to the COVID-19 disruptions, the shift to remote working became a common occurrence in the UK; however, NHS teams involved with various partnerships were already using remote communication with their respective partners. Hence, project members were versed and comfortable with communicating with staff inside and outside the NHS, using online resources, and conducting consultations remotely.
Dissemination of findings
The CwPAMS program successfully disseminated adapted media material, participated in conferences, global events, and launched various tools and resources to publicize the relevance and achievements of CwPAMS through a range of avenues noted in Supplementary Table 6, including peer-reviewed publications listed in Supplementary Table 7.
Figure 3.
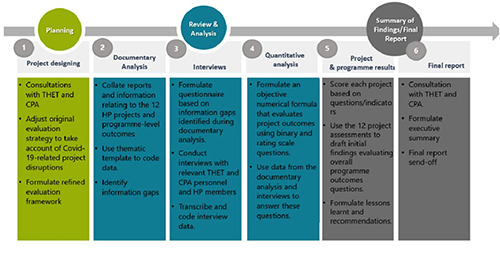
Illustration of a summary of evaluation of program activities.
Conclusions
Partnership collaboration
The partnership approach was critical for the overall success of CwPAMS and the sustainability of the projects (and their impact) once the program came to an end. Strong collaborations, not only at a high level but also in hospitals, were to some extent a key factor enabling HPs to mitigate challenges resulting from limited funding and resources. By engaging influential AMR personnel and having their activities endorsed from the outset, many HPs were able to function more efficiently and generate new opportunities within their respective settings.
Setting up partnerships and project management
Agile project management and risk mitigation played a central role in individual project success. However, many HPs were newly formed (or consisted of newly created project teams within an existing HP) and project proposals were compiled remotely, sometimes under time pressure and with poor connection. Support from THET and CPA facilitated the achievements of the HPs, although more contextually relevant support could have been provided to the HPs in-country. Additionally, more could have been done to set expectations with the HPs and clearly communicate the roles of THET and CPA and the support that they could provide.
Volunteer-based approach
Although funding is available and expected for project management of projects, the ‘volunteer-based approach’ is a key component of THET’s long standing Health Partnership Scheme. Organisations permitting their staff to volunteer with the CwPAMS Program, gained staff with increased competency around AMR and improved interpersonal, management and training skills. Several UK health institutions also actively integrated returned volunteer skills and experience, providing a platform for volunteers to share their insights, endorsing publications associated with CwPAMS and recognising/rewarding the improved competence of returning volunteers. In some cases, however, the voluntary nature of the program hindered the ability of HPs to achieve their objectives. The voluntary nature of most roles meant that CwPAMS relied on both LMIC and UK partners dividing their time between their project, personal, and professional obligations. This sometimes led to delays project activities, demotivation amongst the volunteers, and became a source of tension for some HPs.
Gender equality and social inclusion
There was a superficial prioritisation of gender equality and social inclusion (GESI) in CwPAMS from the grant call stage and throughout its duration. For example, the grant application template which HPs were to complete, only dedicated a small section to GESI. As a result, most HPs did not provide adequate GESI plans. Further analysis of reports and responses from interview participants highlighted that many felt that simply having women as a majority within teams and training sessions was enough evidence to demonstrate the empowerment and upskilling of women.
Consideration for next steps
It is advisable for THET and particularly CPA to consider more direct and clear communication with HPs explaining their roles and ways in which they may provide support. It is also important that travel policies are made clearer as part of the training sessions. Furthermore, both organizations should consider more proactive diligence of HPs, particularly during the start-up phase, to identify likely challenges projects may have (for example ethical approval delays). This hands-on approach is likely to help increase efficiency across the projects, set and manage expectations, and also equalize the sense of obligation and ownership between all partners involved within the partnership. Examples of bespoke support should include project management, development of in-country AMS technical lead roles and development of AMS training on an online continuous professional development (CPD) platform. Considerations should also be made on the extension of projects within the community, One Health, and taking into consideration new WHO tools published since CwPAMS commenced.
GESI tools should highlight in more detail the kinds of interventions that are likely to translate into meaningful change and prevent the use of a ‘silver bullet’ and transplanted approaches. In international development theory ‘silver bullets’ refer to a single solution/mechanism that is put forward as applicable and effective to all underdeveloped countries and contexts. More attention should be paid to GESI during the initial scoping and project planning phases as it is not given equal weighting in all NAPs and thus HPs must take more initiative. More emphasis should be placed on ensuring that these interventions translate into meaningful benefits and access to opportunities for women in the form of promotions and greater decision-making power. As all 12 LMIC HP Leads were male, CwPAMS might need to consider adopting gender affirmative action policies to ensure that there is equal representation of both genders, disabled persons, and other marginalized groups at the forefront of HP leadership, and have specialized HR and other personnel who have been specifically trained on issues concerning GESI.
Acknowledgments
All members of the twelve partnerships, as well as the CPA and THET teams, are acknowledged for their support, contributions and shared learning throughout the CwPAMS program. The partnerships included: North Middlesex University Hospital NHS Trust, London (NMUH)-Korle-Bu Teaching Hospital (KBTH); Healthcare Improvement Scotland–Ghana Police Hospital and Keta Municipal Hospital; Northumbria Healthcare NHS Foundation Trust– Kilimanjaro Christian Medical Centre (KCMC); Makerere University, Mulago Specialised Women and Neonatal Hospital, Kawempe Hospital and Cambridge University Hospitals (CUH); Brighton and Sussex University Hospitals NHS Trust (BSUH), Brighton and Sussex Medical School (BSMS) Brighton–University Teaching Hospital (UTH), University of Zambia (UN ZA) School of Pharmacy, Lusaka and University Hospital Ndola; Norfolk and Suffolk NHS Foundation Trust–The Assemblies of God Hospital, Saboba; UK Faculty of Public Health (FPH)–Ghana Public Health Association (GPHA); University of Heath and Allied Sciences; Ho Teaching Hospital (UHAS); University College London Hospitals NHS Foundation Trust; University of Salford–Pharmaceutical Society of Uganda and Health Education England: Manchester University NHS Foundation Trust, Gulu Regional Referral Hospital, Saint Mary’s Lacor, University of Manchester, Manchester Metropolitan University, Nottingham Trent University (NTU), Makerere University, Uganda (MakU), Buckinghamshire Healthcare NHS Trust (BHT), London School of Hygiene and Tropical Medicine (LSHTM) and University College London Hospitals NHS Foundation Trust–Makerere University College of Health Sciences and Infectious Diseases Research Collaboration (IDRC).
Funding Statement
Funding: Commonwealth Partnerships for Antimicrobial Stewardship (CwPAMS) project, is managed by the Commonwealth Pharmacists Association (CPA) and the Tropical Health and Education Trust (THET). This project is funded by the UK Department of Health and Social Care's Fleming Fund using UK aid. The views expressed in this publication are those of the author(s) and not necessarily those of the Department of Health and Social Care, the UK National Health Service, represented organizations, THET, or CPA.
References
- 1.Ho CWL, Lee TL. Global governance of anti-microbial resistance: A legal and regulatory toolkit. Ethics and drug resistance: collective responsibility for global public health. Springer, Cham: 2020:401-20. Available from: https://link.springer.com/chapter/10.1007/978-3-030-27874-8_25 (Accessed on 02 June 2022). [Google Scholar]
- 2.World Health Organization (WHO). Global Action Plan on Antimicrobial Resistance. WHO. Geneva, Switzerland, 2015. Available from: http://www.who.int/antimicrobial-resistance/publications/global-action-plan/en/ (Accessed on 10 September 2020). [Google Scholar]
- 3.UN NEWS: at UN, global leaders commit to act on antimicrobial resistance (2016). Available at: https://news.un.org/en/story/2016/09/539912-un-global-leaders-commit-act-antimicrobial-resistance (Accessed on 10 September 2020). [Google Scholar]
- 4.United Nations. World health leaders agree on action to combat antimicrobial resistance, warning of nearly 10 million deaths annually if left unchecked (2016). Available from: https://www.un.org/press/en/2016/ga11825.doc.htm (Accessed on 02 June 2022). [Google Scholar]
- 5.World Health Organization (WHO). Global Database for Antimicrobial Resistance Country Self-Assessment. Available from: https://amrcountryprogress.org/. (Accessed on 04 March 2019). [Google Scholar]
- 6.Commonwealth Pharmacists Association: Commonwealth Partnerships for Antimicrobial Stewardship. Available from: https://commonwealthpharmacy.org/cwpams/ (Accessed on 01 June 2022). [Google Scholar]
- 7.THET: Health Partnerships Scheme. Available from: https://www.thet.org/our-work/health-partnership-scheme/ (Accessed on 02 June 2022). [Google Scholar]
- 8.World Health Organisation; Partnerships for safer health service delivery: Evaluation of WHO African Partnerships for Patient Safety 2009-2014. Available from: https://www.who.int/patientsafety/implementation/apps/evaluation-report.pdf (Accessed on 11 September 2020). [Google Scholar]
- 9.Strengthening health systems in developing countries: fifth report of session 2014-15. London: House of Commons International Development Committee, 2014. Available from: http://www.publications.parliament.uk/pa/cm201415/cmselect/cmintdev/246/246.pdf [Google Scholar]
- 10.Kostyak L, Shaw DM, Elger B, Annaheim B. A means of improving public health in low- and middle-income countries? Benefits and challenges of international public-private partnerships. Pub Health 2017;149:120-9. [DOI] [PubMed] [Google Scholar]
- 11.IPE Triple Line Health Partners International. Health Partnerships Scheme Evaluation Synthesis Report, 2016. Available from: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/589736/Evaluation-of-Health-Partnership-Scheme.pdf (Accessed on 27 May 2022). [Google Scholar]
- 12.Health Partners International; building partnerships for equitable health systems (2017). Evaluation of the Health Partnership Scheme. Available from: http://healthpartnersint.co.uk/our-projects/evaluation-of-the-health-partnershipscheme/ (Accessed on 11 September 2020). [Google Scholar]
- 13.Commonwealth Pharmacists’ Association: Commonwealth Partnerships for Antimicrobial Stewardship Scheme. Available from: https://commonwealthpharmacy.org/commonwealthpartnerships-for-antimicrobial-stewardship-scheme-call-forapplications-now-open/ (Accessed on 21 September 2020). [Google Scholar]
- 14.Brandish C, Garraghan F, Ng BY, et al. Assessing the impact of a global health fellowship on pharmacists' leadership skills and consideration of benefits to the National Health Service (NHS) in the United Kingdom. Healthcare (Basel) 2021;9:890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.OECD iLibrary. Applying evaluation criteria thoughtfully. Available from: https://www.oecd-ilibrary.org/development/applying-evaluation-criteria-thoughtfully_543e84ed-en (Accessed on 28 March 2023). [Google Scholar]
- 16.NHS Health Research Authority. Is my study research decision tool. Available from: http://www.hra-decisiontools.org.uk/research/result7.html (Accessed on 16 June 2021). [Google Scholar]
- 17.Kerr F, Sefah IA, Essah DO, et al. Practical Pharmacist-Led Interventions to Improve Antimicrobial Stewardship in Ghana, Tanzania, Uganda and Zambia. Pharmacy (Basel) 2021;9:124. [DOI] [PMC free article] [PubMed] [Google Scholar]


