Abstract
Introduction:
A lack of patient safety research hampers capacity to improve safety in healthcare.
Ultrasound is often considered ‘safe’ as it does not use ionising radiation, a simplistic view of patient safety. Understanding sonographers’ actions towards patient safety is crucial; however, self-reported measures cannot always predict behaviour. This study is part of a PhD exploring patient safety in medical diagnostic ultrasound. The aim of this paper is to explore sonographers’ responses to the patient safety concerns identified in Part one of this study. The ultimate aim of the study is to inform the final phase of the doctoral study which will consider the next steps in improving the quality and safety of healthcare experienced by patients.
Methods:
A qualitative study using semi-structured, one-on-one interviews. The Theory of Planned Behaviour (TPB) explained how sonographers respond to perceived patient safety risks in practice.
Results:
Thirty-one sonographers were interviewed. Based on the seven themes identified in Part one of the study, results showed that incongruences exist between identifying patient safety risks and the actions taken in practice to manage these risks.
Conclusion:
The TPB showed that behavioural, normative and control beliefs impact sonographers’ responses to perceived patient safety risks in practice and can lead to risk avoidance. Lack of regulation in ultrasound creates a challenge in dealing with Fitness to Practice issues. Collective actions are required to support sonographers in taking appropriate actions to enhance patient safety from multiple stakeholders including accreditation bodies, regulatory authorities, educational institutions and employers.
Keywords: Sonography, ultrasound, professional issues, miscellaneous, safety, physics and engineering, adverse effects
Introduction
Patient safety is fundamental to quality healthcare. 1 Various definitions and inconsistent language surrounding the concept of patient safety make it a challenging area to study. 2 A lack of patient safety research worldwide hampers the capacity to improve the safety of healthcare.1,3
Ultrasound imaging is often considered ‘safe’ as it does not use ionising radiation,4,5 a simplistic view of patient safety in medical imaging. 6 Patient safety breaches in ultrasound imaging generally relate to other safety issues in practice, as identified in Part one of this study.
While identifying areas of concern for patients’ safety is important in enhancing patient safety, 1 understanding behaviours and actions in response to identified concerns is equally important. Behaviours in practice cannot always be predicted by self-reported measures. Instead, they can be explained through the Theory of Planned Behaviour (TPB), whereby actions and behaviours in practice are guided by behavioural beliefs, normative beliefs and control beliefs. 7
Aims
This study adds to the patient safety research by exploring and describing the perceptions of Australian sonographers with regard to patient safety in ultrasound imaging. This study comprises two parts. Part one identified what sonographers believe are the most common patient safety risks during ultrasound imaging. 8 Part two of the study, reported here, analyses and describes sonographers’ responses in managing these risks, using the TPB to explain their actions in practice.
Methods
Semi-structured, one-on-one interviews were conducted by the primary investigator. Below is a précis of the methods employed in the study. 8 outlines in-depth the recruitment process, the development of the interview questions and the generation of the initial codes and themes.
Ethical considerations
Ethical approval was granted by Monash University Human Research Ethics Committee, project 19091.
Recruitment
Sonographers on the Australian Sonographer Accreditation Registry (ASAR) who agreed to participate in ASAR facilitated research were invited to participate via face-to-face, phone, or virtual online meetings.
Developing the interview questions
An interview guide, developed with input from senior academic and clinical sonographers, ensured the line of questioning addressed the aims and remained consistent across the interviews. Open-ended questions meant participants could express their views without influence, not leading respondents in their responses.
Data analysis
Data analysis followed a similar method as Part one of the study and was carried out by the primary investigator. Interviews were transcribed verbatim and transferred to NVivo data management package to support the analysis. Data analysis was aligned with Braun and Clarke’s Thematic Analysis (TA). The identifying phase of the analysis, mapping potential and final themes from the initial codes occurred in the same fashion in both parts of the study. From this point, the interpretation of the data in Part two focussed on data related to what occurs in practice. The emphasis on reflexive dialogue facilitated by TA was important when comparing the findings with those in Part one of the study. 9
According to the TPB, actions and behaviours are guided, in different measures dependent on the action, by three considerations: first, behavioural beliefs, whereby personal beliefs about the consequences of the behaviour guide the behaviour itself; second, normative beliefs, whereby beliefs about the expectations of others or society guide the behaviour; third, control beliefs, whereby beliefs about the presence of challenges and/or enablers guide the behaviour.7,10 By examining these considerations within people’s responses, and assessing the relative importance of them, we can account for peoples’ behaviours in practice. 7 The TPB has been used to explain health professionals’ actions and behaviours in several areas. 10 A literature search revealed over 100 studies using the TPB in healthcare. Within medical imaging, the TPB has been used to explain variation in the number of intra-oral radiographs acquired in different settings, 11 understand physicians’ use of contrast-enhanced ultrasound imaging, 12 explain variation in imaging referral patterns 12 and explore radiation protection practices. 13 The TPB is therefore an appropriate model to explain actions and behaviours in response to patient safety concerns in ultrasound practice.
Results and discussion
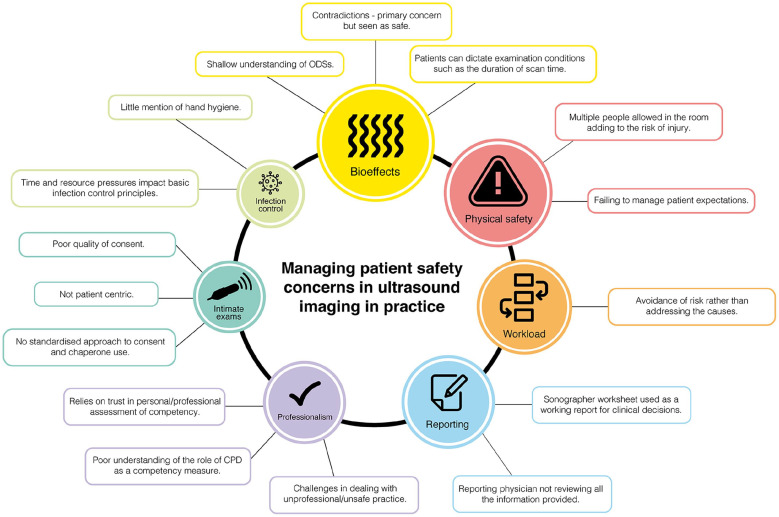
Early during data analysis, incongruences between identification of patient safety risks and the actions taken in managing these risks in practice became evident. The seven themes identified in Part one of the study supported the development of Part two. Figure 1 shows the findings across each theme and the relative strength of each theme.
Figure 1.
Major themes identified by sonographers.
Theme 1: bioeffects
Bioeffect was the most common patient safety concern that sonographers identified. 8 However, sonographers generally perceived ultrasound imaging as safe, ‘There is no debate about it. Ultrasound is [a] very safe procedure’ (PS11). This paradoxical situation has been previously reported. 5 In accordance with the TPB, sonographers’ behavioural beliefs, whereby they believe ultrasound examinations have low biological risk, lends itself to complacency around the implementation of biological safety mechanisms in practice. Sonographers were aware of the Output Display Standards (ODSs), mechanical index (MI) and thermal index (TI). However, uncertainties in dosimetry and measurement of acoustic output mean that ODSs represent approximate risk of biological effects and do not provide absolute measures of acoustic output or parameters such as the duration of the examination or dwell time on specific tissues. 14 Techniques such as spectral Doppler ultrasound require one area to be insonated for extended periods, increasing the potential for biological effects in that area. 15 Beam intensities in modern ultrasound systems are higher than superseded systems, and sonographers must be vigilant in understanding the limitations of the TI and MI during ultrasound examinations. In our study, sonographers did not consider the uncertainties and limitations of ODSs: ‘Sonographers as a whole have a poor understanding of [ODSs]’ (PS16). Instead, they relied on manufacturers’ default settings: ‘none of us have to check because it’s all done pretty much automatically’ (PS5) in implementing ODSs. Other studies raised similar concerns about sonographers’ knowledge and attitude regarding TI and MI.4,5
Theme 2: physical safety
Risk of physical harm to patients was the second most common patient safety concern; sonographers felt that additional people present during ultrasound examinations, especially children, increases the risk of physical harm. 8 Tension exists between the use of ultrasound as a diagnostic procedure and patients’ expectations for a social experience, most obvious during obstetrical ultrasound examinations.16,17 Managing these expectations plays an important part in patients’ physical safety during ultrasound examinations, and distractions should be limited to avoid physical harm.16,17 According to the TPB, it appears that sonographers’ normative beliefs can result in prioritising patient expectations over the risk of physical safety. 7
In our study, 10 (31%) respondents felt that ultrasound examinations are ‘perceived by the public as entertainment’ (PS7) rather than diagnostic tests. Sonographers felt that patients’ expectations to ‘pop the champagne, get the fireworks going’ (PS5) lead to multiple people present in the room during examinations, especially for those performing obstetrical ultrasound. However, it did not seem to stop the practice of having ‘little kids running around the room. We’ve got husbands walking around the room, grandmothers asking questions’ (PS7). Other studies have shown that up to 93.3% of sonographers believe that the potential for physical harm is increased when others, especially children, are present.16,17 However, even where policy exists to help sonographers limit the presence of others in the examination room, less than 66% of sonographers implement the policy, mostly due to fear of patient complaints. 17 Professional bodies in medical imaging have guidance on aspects of patient safety, such as bioeffects and invasive examinations, but little exists in regard to management of physical safety. In our study, it appears that sonographers allow additional people in the room to fulfil patients’ expectations, even if they believe it carries an increased risk to their physical safety. It is acknowledged that COVID safety measures often disallowed other people in the room during ultrasound examinations. This may have addressed this issue in the interim period, but as we emerge from these measures, this issue is likely to resurface.
Theme 3: workload
The number of ultrasound examinations performed across the world has risen substantially in the last 10 years, and this was reflected in our study. 8 According to those interviewed, increasing workloads mean reduced examination times: ‘ask any sonographer, scan times are being cut’ (PS10). Remuneration schemes based on numbers of examinations performed per day have proliferated: ‘people get remunerated to like knock over 30 scans’ (PS30). Sonographers reported working protracted hours to meet demands: ‘I don’t even stop for lunch or morning tea’ (PS23). In responding to increasing workload demands, sonographers cited evasive actions rather than addressing underlying issues. According to the TPB, this response could be explained by control beliefs. If a person believes that great challenges exist in implementing a behaviour in practice, they are less likely to behave in the way that might be expected.
In medical imaging, when workload demands increase, providers compensate by increasing expected productivity. 18 Ultrasound is an underfunded service on the Australian Medicare Benefits Schedule (MBS) 19 and the fee-per-service provided by the MBS favours a high-volume business model.20,21 A coronial inquest in a medical imaging setting, albeit not ultrasound, identified that high-volume patient turnover due to a bulk-billing structure contributed to poor care of the patient. 21 Compounding this, sonographer shortages in Australia have increased demand on sonographers.19,22 Decision fatigue, cognitive overload, poor processing of information, poor communication and flawed decision making can be experienced by people working prolonged shifts performing high-volume and high-complexity tasks,18,23 similar to the ultrasound imaging environment described by sonographers in our study: ‘you can be as dedicated and as good as your job, but if you are rushing through an exam, there’s so much potential for missed pathology’ (PS30).
In addressing these challenges, 10 (31%) sonographers would ‘refuse now to work anywhere that bulk-bills’ (PS24) or for imaging providers that pay by number of examinations performed. Four (8%) said they protect people they know by advising them: ‘I’m very careful with who does a member of my family and where it’s done’ (PS9). This represents a personal approach to the issue, which is limited in effectiveness in keeping patients safe and misses the opportunity for real improvement of workload issues using a system approach. Initiating a system approach to improving safety in healthcare is very challenging, and therefore, in accordance with the TPB, sonographers in our study felt powerless due to the challenges that exist, instead feeling ‘lucky’ (PS17) if they worked for an organisation that had rigorous standards over ‘a place where standards were more orientated towards productivity’ (PS29).
Theme 4: reporting
Sonographers do not generate final reports in Australia, but final reports are based on information provided by the sonographer, such as their worksheet and sonographic images. The potential for breakdown in communication in relaying findings from a dynamic ultrasound examination to a reporting clinician caused concern for patient safety. 8 Sonographers interviewed felt confident in their own worksheets, with one mentioning that ‘I’m hoping that they’re not out there changing my reports’ (PS26). However, an apparent mismatch between sonographers’ expectations around the use of the information provided for reporting and how that information is used caused concern for patient safety. According to the TPB, normative beliefs surrounding the relationship between sonographers and reporting physicians influenced sonographers’ actions in addressing safety concerns in reporting. In keeping with the TPB, people who others are most motivated to comply with, called referents, exert the greatest influence on peoples’ actions. Referents usually include those considered experts or in a position of power, such as physicians.7,24
In our study, 10 (31%) sonographers reported that ‘Radiologists don’t even look at the images . . . All they do is look at the report’ (PS25). On one level, this is what one would want to happen; sonographers are highly skilled, and the information they provide has been shown to be accurate.25,26 However, 11 (35%) sonographers reported that worksheets are used as a ‘working report’ (PS2) on which clinical decisions are made. This made sonographers feel ‘a bit uncomfortable’ (PS2), with 3 (10%) sonographers stating that ‘I find that a very dangerous practice’ (PS14). These sonographers had reservations when all the information presented is not crosschecked for accuracy and additional findings that may have been missed: ‘If they don’t look at the images, you might actually have missed something’ (PS28). One study examining litigation in ultrasound showed that, while rare (66 cases recorded from 1983 to 2002), retrospective review of images was able to correct a diagnosis when it was initially mis-reported. 27 In response to what was highlighted as a patient safety issue, sonographers seemed to accept the status quo of a final report being completed by a reporting physician without checking all the information provided. It appears that sonographers’ normative beliefs mean they may do what is expected of them by the reporting physician.
Theme 5: professionalism
The two biggest concerns for patient safety with regard to professionalism were competence and Fitness to Practice (FtP). 8 The TPB explains that when resources or opportunities are inadequate, motivation towards positive behaviour across all three beliefs can suffer. This explained sonographers’ response to the issues around competence and FtP.
With regard to competence, sonographers were concerned that ‘There’s no real assessment of competence once you’ve qualified’ (PS29). Competency hinges on ‘a personal relationship with the radiologist’ (PS5), relying on the reporting physician ‘getting a sense of how good they think you are’ (PS16). Three (10%) sonographers expressed that ‘I think some of the doctors just don’t care’ (PS6) about the standard of sonography practice. An Australian study found that sonographers training in neonatal cranial ultrasound were supervised until competency was reached with no definition of how this competency was measured. 5 It could be said that this is true for any specialised or new areas of examination for sonographers, for example, working in a paediatric setting, after initial training in adult practice.
With FtP, sonographers felt that no formal mechanism exists to manage FtP in practice. Instead, sonographers commented that ‘it’s more self-regulation’. (PS6). This was especially evident in those with experiences of unsafe practice who felt ‘we’ve got no one to talk to. It’s not regulated’ (PS23) and ‘There’s nothing to stop them doing it’ (PS2). Statutory regulation of sonography practice is being advocated for by professional bodies in Australia, 28 but currently no regulatory standard exists specifically for sonography. This leaves sonographers with little opportunity for meaningful action. 29 This was obvious in our study whereby sonographers felt that an incompetent sonographer ‘becomes another practice’s problem’ (PS6). The shortage of sonographers in Australia19,22 exacerbates this: ‘they [sonographers] go down the road and go, well I’m up to here now because I know there’s a shortage’ (PS31).
Sonographers reported personal experiences of unsafe practice and were left distressed by them and by the lack of clear mechanisms for dealing with the issues. The lack of formal FtP mechanisms and benchmarking of competence, exacerbated by workforce shortages, means that sonographers are hampered in dealing with issues of unsafe practice.
Theme 6: intimate exams
Safety in ultrasound examinations sometimes neglects the psychological safety of intimate examinations. 6 A small but significant number of women (1.6%) reported psychological distress during transvaginal ultrasound examinations. 30 Some evidence of sexual assault by sonographers during intimate examinations exists.27,31,32 Using the TPB was less obvious in explaining sonographers’ actions during intimate examinations. Their trust in consent and chaperones in keeping patients safe aligned with behavioural beliefs, and unless directly involved in an incident, sonographers reported a low perception of risk to patient safety during intimate examinations. As the interviews evolved, it was clear that issues around valid informed consent and the use of chaperones existed.
Informed consent is a protective measure for patients during intimate examinations. However, in a multicentre Australian study in medicine, it was found that 24% of intimate examinations are performed without valid consent. 33 Limited evidence exists in ultrasound, but studies have found that up to 50% of patients attending for ultrasound examinations did not have valid informed consent due to a lack of information provided to them before the study. 34 Not knowing what to expect from an imaging examination can increase patient anxiety. 35 There were similar findings in our study: “I find a lot of my patients are very stressed, because they don’t know what’s going on” (PS28) and “you get someone to sign a consent form but they still don’t really understand” (PS16). However, in each instance the examination still proceeded. Crucial to practice, two sonographers interviewed had experiences of a “critical incident” (PS27) during intimate examinations. The experience changed their perception of patient safety associated with intimate ultrasound examinations: “I never thought it was risky until . . . I was scanning his common femoral artery in the groin. He looked at me and said, “Stop touching me, how dare you touch my genitals” (PS18). Furthermore, consent was generally obtained directly prior to the examination. Studies have shown that at that point patients are committed to the ultrasound examination and undergo them systematically with inadequate opportunities for questions. 34
Gaining informed consent is not legislated for healthcare practitioners in Australia other than physicians and expectations around informed consent in the context of medical imaging is challenging. 36 Tasks associated with obtaining consent can be delegated to members of the imaging team who understand the examination, though a radiologist must be available to provide further information. 37 In our study, consent was sometimes delegated to administrative staff who may not fully understand the procedure.
Furthermore, as in most medical examinations, 33 power imbalances exist between the sonographer and patients. In our study, one sonographer mentioned that ‘Some patients feel like they have to consent because I’m in the room’ (PS23). Examining a recent conviction for sexual assault by a sonographer in Australia, the offender was able to ‘command the patients’ activities’ because of their position of authority over them. 32 The use of chaperones in ultrasound is similarly applied as a safety measure during intimate examinations. How chaperones are implemented during ultrasound examinations is inconsistent and lacks guidance. 29 Some guidelines for the use of chaperones are available through professional and government bodies, but sonographers must interpret these within the context of individual patients. 29 This manifested in a variety of actions around chaperones in our study, with local norms and personal decision-making the most common decision-making processes for the use of a chaperone in practice. In our study, out of those who raised the role of the chaperone during the interview, approximately 40% indicated that a chaperone was protocol, ‘unless the patient flatly refuses’ (PS10). The remaining 60% of the time, using a chaperone ‘would rely on how you felt for the patient’ (PS10). Male sonographers are usually ‘required to have a chaperone’ (PS26), but this itself was controversial among three (10%) interviewees. A male sonographer reported, ‘why should they have a chaperone because most females don’t’ (PS27) and a female sonographer responded, ‘I often wonder about that double standard of testicular ultrasounds’ (PS30).
Furthermore, the credentials of the chaperone are important as they could be required to testify if there are allegations of safety breaches. 38 In our study, it was noted that ‘quite often people will get the receptionist to come into the room’ (PS19). This does not provide adequate protection for patients as ‘they’re in no position to say whether I behaved inappropriately or not’ (PS19).
Theme 7: infection control
Data collection was completed 6 days before Coronavirus was detected in Australia. Infection control would likely be more dominant now, and sonographers may find themselves in a different position than pre-COVID. Overall, infection control was not prominent in the responses: ‘Sonographers are very lax in disinfection of rooms and probes’ (PS31). Seven (22%) sonographers raised infection control as a patient safety concern before probing questions and four more (35%) after further probing questions.
A striking observation from the data was the varied infection control practices during ultrasound imaging. One respondent, working at different sites, outlined that ‘At [Hospital A] we wipe the machine down, wipe the probe down, wash the bed down, clean after every single patient. Then the other hospital that I work in, we don’t do that at all’ (PS20). Other studies of infection control behaviours had similar findings, with little uniformity of hygiene practices in ultrasound imaging.39,40
Ultrasound creates multiple sources for infection, from poor hand hygiene and ultrasound coupling gel to sources such as cords and keyboards. It was clear in our study that sonographers’ focus regarding infection risk is on the probe used during endo-cavity examinations. This is similar to Westerway et al. 39 who found that while 84% of respondents disinfected the probe after endo-cavity examinations, 36% did not wipe down probes with alcohol wipes after surface ultrasound. Hand hygiene was also noticeably missing from the interviews, mentioned by only five (16%) participants. Initially surprising, the evidence points to a deeper issue. Westerway et al. 39 found that less than half of sonographers performed any form of hand hygiene between scanning patients.
Infection control is seen as time-consuming, especially when competing with workload pressures. 39 In our study, sonographers were ‘not given enough time to wipe down’ (PS20) between patients, adding to infection risk. As well as time, several sonographers also reported a lack of resources to implement infection control measures appropriately: ‘All the patients laid on the same bed, on the same sheet wearing the same gown. There’s no infection control there’ (PS12). Thus, a predicament exists in ultrasound practice that finds sonographers balancing the need to maintain infection control standards with time pressures and resource allocation.
The TPB has been used to examine hand hygiene behaviours in healthcare previously,10,24 though not in ultrasound. Our findings were consistent with these studies where healthcare workers articulated the importance of hand hygiene, but in practice showed poor hand hygiene behaviour because of perceptions of infection control as a time-consuming exercise (behavioural and control belief) and lack of access to hygiene products and training (control beliefs).10,24 In our study, sonographers were aware of the advantages of infection control in protecting the patient but acted discordantly with this.
Limitations to the study
Most studies use the TPB to look at individual practice behaviours, for example, hand hygiene. Our study explored the breadth of patient safety, which may reduce depth in individual areas.
The authors acknowledge that the study is based on perceptions rather than direct observation of practice; therefore, the findings are representative of the sample of sonographers interviewed. Previous published research, however, has relied on interviews to investigate behaviours in practice. In our study, several measures ensured that the data were robust. Data were collected in a methodical way. It was analysed using a thematic analysis well accepted in qualitative research in healthcare. Furthermore, the chief investigator was not a sonographer. Initially, there was a question that this may mean the project lacked insight of a sonographer. However, this proved a major boon to the study. With no pre-conceptions about the culture and inherent challenges of the sonography work environment, the sonographers interviewed informed each aspect of the study and the data could be interpreted without fear of insider bias.
Conclusion
The Theory of Planned Behaviour (TPB) can explain incongruences that exist between sonographers identifying patient safety risks and their actions and behaviours in practice.
Out of seven themes, physical safety and workload fell under the normative element of TPB, whereby expectations of others influenced behaviours in practice. The themes of intimate examinations and bioeffects fell under the behavioural element of the TPB, whereby sonographers’ low perception of risk to patient safety influenced how they behaved in practice. Workload fell under the control element of the TPB, whereby sonographers adopted risk avoidance strategies to manage patient safety risks due to inherent challenges present in practice. These strategies fail to address underlying patient safety issues. Infection control fell under both behavioural and control elements of the TPB. Sonographers identified infection control as a patient safety issue, but this did not always translate into expected actions. Finally, professionalism, including competency and Fitness to Practice (FtP), did not fall directly under any of the three elements of the TPB. However, the TPB also explains that a lack of resources and supporting structures for practitioners can influence their practice. This was evident in the area of professionalism whereby a lack of consistent competency benchmarking and limited mechanisms to deal with FtP issues were evident in the data.
Employers and regulatory boards are critical in addressing issues identified in this paper in providing appropriate resources, robust and consistent policies and opportunities for sonographers to reflect on their practice. Registration and regulation for sonographers should continue to be explored to provide a robust clinical practice framework to support sonographers in keeping patients safe during ultrasound imaging.
The authors hope that this article provokes reflection and discussion, and ultimately collective actions from relevant stakeholders including professional and accreditation associations, educational institutions, regulatory boards and employers to manage safety in ultrasound practice.
Footnotes
Contributors: John McInerney – Substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of data. Drafting the article or revising it critically for important intellectual content. Final approval of the version to be published.
Paul Lombardo – Drafting the article or revising it critically for important intellectual content. Final approval of the version to be published.
Cynthia Cowling – Drafting the article or revising it critically for important intellectual content. Final approval of the version to be published.
Simone Roberts – Drafting the article or revising it critically for important intellectual content.
Professor Jenny Sim – Drafting the article or revising it critically for important intellectual content. Final approval of the version to be published.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded in part by the Victorian Medical Radiation Practitioners Education Trust.
Ethics Approval: Ethical approval was granted by Monash University Human Research Ethics Committee (Project 19091, July 2019).
Guarantor: John McInerney
ORCID iDs: John McInerney  https://orcid.org/0000-0001-9668-108X
https://orcid.org/0000-0001-9668-108X
Paul Lombardo  https://orcid.org/0000-0003-2519-3358
https://orcid.org/0000-0003-2519-3358
Simone Roberts  https://orcid.org/0000-0003-0106-4500
https://orcid.org/0000-0003-0106-4500
Jenny Sim  https://orcid.org/0000-0002-0756-3848
https://orcid.org/0000-0002-0756-3848
References
- 1. World Health Organisation. Global patient safety action plan 2021–2030: towards eliminating avoidable harm in health care. Geneva: World Health Organization, 2021. [Google Scholar]
- 2. Runciman W, Hibbert P, Thomson R, et al. Towards an international classification for patient safety: key concepts and terms. Int J Qual Health Care 2009; 21: 18–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Andermann A, Ginsburg L, Norton P, et al. Core competencies for patient safety research: a cornerstone for global capacity strengthening. BMJ Qual Saf 2011; 20: 96–101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Moderiano M, McEvoy M, Childs J, et al. Safety of ultrasound exposure: knowledge, attitudes, and practices of Australasian sonographers. J Diagn Med Sonogr 2018; 34: 357–367. [Google Scholar]
- 5. Lalzad A, Wong F, Singh N, et al. Knowledge of safety, training, and practice of neonatal cranial ultrasound: a survey of operators. J Ultrasound Med 2018; 37: 1411–1421. [DOI] [PubMed] [Google Scholar]
- 6. Brady A, Loose R, Clement O, et al. Patient safety in medical imaging: a joint paper of the European Society of Radiology (ESR) and the European Federation of Radiographer Societies (EFRS). Insights Imaging 2019; 10: 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Ajzen I. Attitudes, personality and behaviour. 2nd ed. New York: McGraw-Hill Education, 2005. [Google Scholar]
- 8. McInerney J, Lombardo P, Cowling C, et al. Australian sonographers’ perceptions of patient safety in ultrasound imaging: part one – identifying the main safety concerns, a qualitative study. Ultrasound 2022; In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Clarke V, Braun V. Thematic analysis. J Posit Psychol 2017; 12: 297–298. [Google Scholar]
- 10. Jenner EA, Fletcher B, Watson P, et al. Discrepancy between self-reported and observed hand hygiene behaviour in healthcare professionals. J Hosp Infect 2006; 63: 418–422. [DOI] [PubMed] [Google Scholar]
- 11. Bonetti D, Pitts NB, Eccles M, et al. Applying psychological theory to evidence-based clinical practice: identifying factors predictive of taking intra-oral radiographs. Soc Sci Med 2006; 63: 1889–1899. [DOI] [PubMed] [Google Scholar]
- 12. Grimshaw JM, Eccles MP, Steen N, et al. Applying psychological theories to evidence-based clinical practice: identifying factors predictive of lumbar spine x-ray for low back pain in UK primary care practice. Implement Sci 2011; 6: 55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Lewis S, Downing C, Hayre CM. Using the theory of planned behaviour to determine radiation protection among South African diagnostic radiographers: a cross-sectional survey. J Med Radiat Sci 2021; 69:47–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. ter Haar G. The safe use of ultrasound in medical diagnosis. 3rd ed. London: The British Institute of Radiology, 2013. [Google Scholar]
- 15. Barnett SB. Intracranial temperature elevation from diagnostic ultrasound. Ultrasound Med Biol 2001; 27: 883–888. [DOI] [PubMed] [Google Scholar]
- 16. Najafzadeh A, Woodrow N, Thoirs K. Distractors in obstetric ultrasound: do sonographers have safety concerns? Australas J Ultrasound Med 2019; 22: 206–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Woodrow N, Najafzadeh A, Thoirs K. Distractors: do we need a policy safeguarding sonographers’ working conditions during obstetric ultrasound examinations? Sonography 2019; 6: 151–156. [Google Scholar]
- 18. Kwee TC, Kwee RM. Workload of diagnostic radiologists in the foreseeable future based on recent scientific advances: growth expectations and role of artificial intelligence. Insights Imaging 2021; 12: 88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Australasian Sonographers Association. Pre-budget submission 2019–20, 2020, https://www.sonographers.org/publicassets/f04695ab-467e-ea11-90fb-0050568796d8/ADV-2019-20_Pre-Budget-Submission.pdf
- 20. Royal Australian College of General Practice. Should bulk-billing rates be used as a measure of healthcare success? 2021, https://www1.racgp.org.au/newsgp/professional/should-bulk-billing-rates-be-used-as-a-measure-of
- 21. Coroners Court of Queensland. Inquest into the death of Maria Aurelia Willersdorf. Findings of Inquest, Contract no. 2015/1475, 24 January 2020, https://www.courts.qld.gov.au/__data/assets/pdf_file/0009/638604/cif-willersdorf-ma-20200124.pdf
- 22. McGregor R, Pollard K, Davidson R, et al. Providing a sustainable sonographer workforce in Australia: clinical training solutions. Sonography 2020; 7: 141–147. [Google Scholar]
- 23. Reiner BI, Krupinski E. The insidious problem of fatigue in medical imaging practice. J Digit Imaging 2012; 25: 3–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. White KM, Jimmieson NL, Obst PL, et al. Using a theory of planned behaviour framework to explore hand hygiene beliefs at the ‘5 critical moments’ among Australian hospital-based nurses. BMC Health Serv Res 2015; 15: 59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Necas M, Shen Y, Ong QH, et al. Do radiologists need to review abdominal ultrasound examinations reported as ‘normal’ by the sonographer? Australas J Ultrasound Med 2020; 23: 167–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Dawkins A, George N, Ganesh H, et al. Radiologist and sonographer interpretation discrepancies for biliary sonographic findings: our experience. Ultrasound Q 2017; 33: 261–264. [DOI] [PubMed] [Google Scholar]
- 27. Sanders RC. Changing patterns of ultrasound-related litigation. J Ultrasound Med 2003; 22: 1009–1015. [DOI] [PubMed] [Google Scholar]
- 28. Australasian Sonographers Association. The urgent need to regulate sonographers in Australia, 2016, https://www.asum.com.au/wp-content/uploads/MED-media-release_ISHAK-1612-v0.6.pdf
- 29. Collins K, Hamlyn T, Bruxner G, et al. Dangers in the dark: calling for a safer practice of transvaginal ultrasonography. Australas J Ultrasound Med 2021; 24: 5–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Clement S, Candy B, Heath V, et al. Transvaginal ultrasound in pregnancy: its acceptability to women and maternal psychological morbidity. Ultrasound Obstet Gynecol 2003; 22: 508–514. [DOI] [PubMed] [Google Scholar]
- 31. Siganto T. Brisbane sonographer who allegedly raped three patients during scan appointments granted bail. Australian Broadcasting Corporation News. 31 August 2021, https://www.abc.net.au/news/2021-08-31/qld-sonographer-accused-rape-three-patients-hospital-bail/100420648
- 32. Public Statement and Statement of Decision in relation to Mr Samir Ishak, https://www.hccc.nsw.gov.au/decisions-orders/public-statements-and-warnings/public-statement-and-statement-of-decision-in-relation-to-mr-samir-ishak
- 33. Rees CE, Monrouxe LV. Medical students learning intimate examinations without valid consent: a multicentre study: intimate exams without valid consent. Med Educ 2011; 45: 261–272. [DOI] [PubMed] [Google Scholar]
- 34. Favre R, Moutel G, Duchange N, et al. What about informed consent in first-trimester ultrasound screening for down syndrome? Fetal Diagn Ther 2008; 23: 173–184. [DOI] [PubMed] [Google Scholar]
- 35. Thoirs K, Deed K, Childs J. Transvaginal sonography: sonographer reflections on patient experience using a critical incident technique. Sonography 2017; 4: 55–62. [Google Scholar]
- 36. Younger CWE, Douglas C, Warren-Forward H. Medical imaging and informed consent – can radiographers and patients agree upon a realistic best practice? Radiography 2018; 24: 204–210. [DOI] [PubMed] [Google Scholar]
- 37. The Royal Australian and New Zealand College of Radiologists. Medical imaging informed consent guidelines, version 3. Sydney, NSW, Australia: The Royal Australian and New Zealand College of Radiologists, 2019. [Google Scholar]
- 38. Australasian Sonographers Association. Intimate examinations, consent and chaperones. Melbourne, VIC, Australia: Australasian Songpraphers Association, 2015. [Google Scholar]
- 39. Westerway SC, Basseal JM, Abramowicz JS. Medical ultrasound disinfection and hygiene practices: WFUMB global survey results. Ultrasound Med Biol 2019; 45: 344–352. [DOI] [PubMed] [Google Scholar]
- 40. Nyhsen CM, Humphreys H, Nicolau C, et al. Infection prevention and ultrasound probe decontamination practices in Europe: a survey of the European Society of Radiology. Insights Imaging 2016; 7: 841–847. [DOI] [PMC free article] [PubMed] [Google Scholar]