Abstract
Retinal hemangioma has posed a therapeutic problem for ophthalmologists for almost a decade. The location of hemangioma in the retina is an important factor in determining the treatment options as well as the size of the tumor, clarity of media, and secondary features of the mass. A 22-year-old male presented to vitreoretina clinic at a tertiary eye hospital, with a history of sudden decrease of vision in the left eye for 1 year associated with mild ocular pains. Physical and systemic examination revealed no positive findings. On ocular examination, the visual acuity was 6/6 in the right eye and perception of light in the left eye, and there was no improvement with best correction. Anterior segment examination in both eyes was essentially normal. Dilated funduscopy revealed a well-circumscribed and elevated vascular orange reddish mass in the juxtapapillary area, temporal to the disc with dilated tortuous feeder blood vessels measuring 6.4 × 3.0 mm in the right eye and vitreous hemorrhage with tractional retinal detachment in the left eye. The small solitary lesion in the right eye was treated with focal laser. This was followed by intravitreal bevacizumab avastin 1.25 mg in 0.05 mL in the same eye, monthly three doses, with the aim of targeting the bigger lesion at the juxtapapillary area to reduce the risk of visual loss. Patient also had pars plana vitrectomy, endolaser photocoagulation, and silicon oil in the left eye. There was complete resolution of the tumor, which was not measurable after third dose of intravitreal avastin. Patient vision remained 6/6, and there was no recurrence at the last follow-up visit 3 years after treatment. Antivascular endothelial growth factors like avastin are effective in the treatment of retinal capillary hemangioma, thereby inducing complete tumor resolution as well as maintaining good vision in the early stages of the disease before complication occurs, as it is evident in this case study.
Keywords: Anti-vascular endothelial growth factors, focal laser photocoagulation, retinal capillary hemangioma, Von Hippel–Lindau syndrome
Introduction
Retinal capillary hemangioma is a benign vascular tumor of the retina that can occur idiopathically[1] or in association with systemic conditions like Von Hippel–Lindau (VHL) disease.[2] In addition, vascular endothelial growth factor (VEGF) is an important stimulus in the development of these retinal lesions.
The condition is a rare vascular, sight-threatening tumor that may occasionally occur in isolation, although about 50% of patients with solitary lesions and virtually all patients with multiple lesions have VHL disease.[3] The prevalence of retinal tumors in VHL is approximately 60%.
The tumor occurs in young patients between 10 and 30 years old.[4] The median age at hemangioma diagnosis in patients with VHL is earlier (18 years) than in those without VHL (31 years).
Tumors may be detected by screening of those at risk or following routine ocular examination or when patient present with painless blurring of vision due to macular exudates or retinal detachment.[3]
Early lesions appear as small red oval or round mass located between an arteriole and a venule, whereas a well-established tumor is seen as a round orange-red mass, usually located in the superior or inferior temporal periphery with dilatation and tortuosity of the supplying artery and draining vein extending from the optic disc.[3]
Lesions commonly occur in the juxtapapillary site and are often on the temporal side of the disc, rapidly threatening the fovea secondary to leakage.
Tumors can also be complicated by vitreous hemorrhage and exudate formation due to leakage, fibrotic bands with subsequent tractional or rhegmatogenous retinal detachment, secondary glaucoma, and phthisis bulbi.
Diagnosis of this condition can easily be made by fundus fluorescence angiography, which shows early hyperfluorescence and late leakage as well as systemic evaluation for VHL disease using imaging techniques that include brain magnetic resonance imaging (MRI) for central nervous system hemangioma involving the cerebellum, spinal cord, medulla, or pons, which affects about 25% of patients with retinal tumors.[3] Abdominal ultrasonographyfor renal carcinoma, pancreatic islet cell carcinoma, cysts of the testes, kidneys, ovaries, lungs, liver and pancreas as well as audiometry for any hearing or balance problems.
Laboratory investigation for polycythemia, which may be the result of factors released by a cerebellar or renal tumor, 24-h urine collection for estimation of vanillyl mandelic acid and catecholamine levels to detect pheochromocytoma.[3]
Observation may be sufficient for asymptomatic juxtapapillary hemangiomas, which may remain inactive for many years and because of the high risk of iatrogenic visual loss following treatment. Peripheral lesions can be treated early by use of laser photocoagulation, cryotheraphy, brachytheraphy, endolaser photocoagulation, or surgical excision; however, photodynamic therapy and use of anti-VEGFs may be useful in the treatment of symptomatic juxtapapillary lesion, since these treatment modalities are less likely to cause severe visual loss.[3]
In this study, we present the long-term effect of focal laser photocoagulation on mid-peripheral retinal hemangioma lesion and also the effect of intravitreal avastin injection for the treatment of juxtapapillary hemangioma.
Case Report
The study adhered to the tenant of Helsinki declaration, and ethical approval was obtained from the ethical review board of the hospital.
A 22-year-old male presented to vitreoretina clinic at a tertiary eye hospital with a history of sudden decreased vision in the left eye for 1 year duration associated with mild ocular pains. There was no preceding history of trauma, no associated history of floaters, or flashes of light. No history of headache or convulsion and no urinary symptoms.
Physical and systemic examination reveals no positive findings. On ocular examination, the visual acuity was 6/6 in the right eye and perception of light in the left eye, and there was no improvement with best correction.
Anterior segment examination in both eyes was essentially normal with an intraocular pressure of 11 mmHg in the right and left eyes, respectively, using the Goldmann applanation tonometer. Dilated funduscopy with 90D revealed a well-circumscribed and elevated vascular orange reddish mass in the juxtapapillary area, temporal to the disc with dilated tortuous feeder blood vessels measured 6.4 × 3.0 mm in the right eye and vitreous hemorrhage with tractional retinal detachment in the left eye.
Based on the above findings, provisional diagnosis of bilateral retinal capillary hemangioma was made, complicated by vitreous hemorrhage and tractional retinal detachment in the left eye.
Investigations
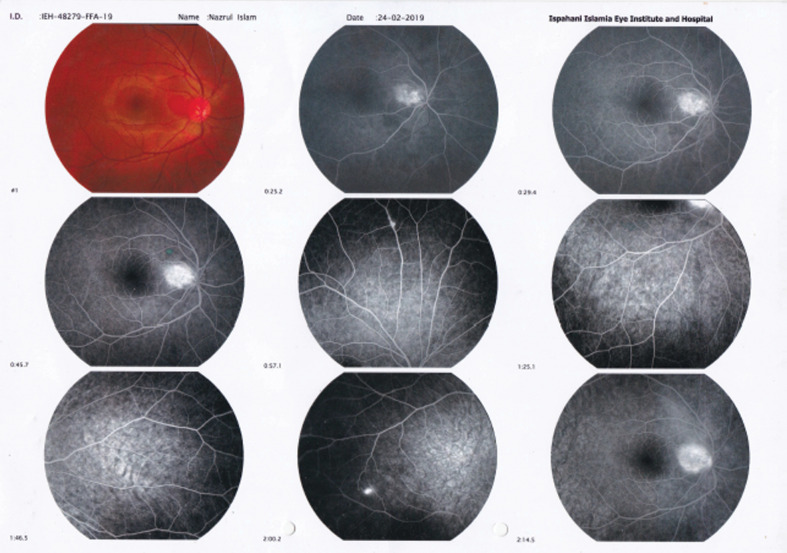
Patient was advised to do color fundal photograph of the right eye for documentation [Figure 1]. Fundus flourescein angiography of the right eye [Figure 2] showed a hyperflourescences mass in the juxtapapillary area temporal to the disc, which increases in intensity with early staining of the feeder arteriole and draining veins, a similar but smaller solitary hyperflourescence lesion in the inferior nasal quadrant of the retina was also present, this confirmed the diagnosis of retina capillary hemangioma.
Figure 1.
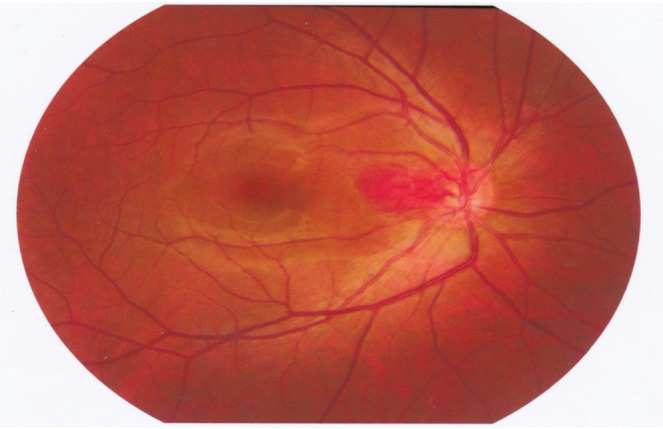
Pretreatment color fundus photograph showing tumor on the right temporal disc margin
Figure 2.
Fundus flourescein angiography (FFA) of the right eye which showed a hyperflourescences mass in the juxtapapillary area temporal to the disc, which increases in intensity with early staining of the feeder arteriole and draining veins, a similar but smaller solitary hyperflourescence lesion in the inferior nasal quadrant of the retina was also present
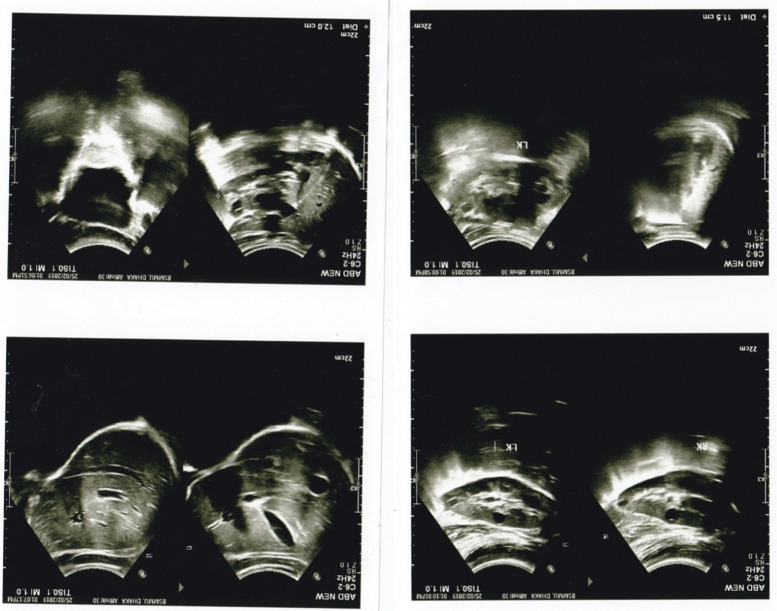
Other investigations that were carried out include abdominal ultrasound [Figure 3], which showed mild enlargement of both kidneys, bipolar length of 12.0 and 11.5 cm in the right and left kidneys, respectively, increased cortical echogenicity, and multiple cystic areas of variable size in both kidneys.
Figure 3.
Abdominal ultrasonography showed multiple cystic lesions in both kidneys, describing features of polycystic kidney disease
MRI of the brain for corticomedullary tumors, audiometry, and 24-h urine vanillylmandellic acid for phechromocytomas (4.52 mg/24 h) was essentially normal.
Treatment
The small solitary lesion in the right eye was treated with focal laser, using the argon laser photocoagulation. Laser burns were applied around and within the vascular lesions including the feeder vessels using the following settings (power = 100 mw, size = 50 µm, duration = 0.1 ms, and number of spots = 66). This was followed by monthly intravitreal injection of Bevacizumab 1.25 mg in 0.05 mL in same eye for 3 months with aim of targeting the bigger lesion at the juxtapapillary area to reduce the risk of visual loss.
Patient also had pars plana vitrectomy, endolaser photocoagulation and silicon oil in the left eye.
The tumor in the right eye reduces to 5 mm × 2.4 mm 1 week postinjection, and 1 mm × 0.5 mm at 2 months after two doses of intravitreal bevacizumab. There was complete resolution of the tumor [Figure 4] which was not measurable, 1 month after giving third dose of intravitreal bevacizumab.
Figure 4.
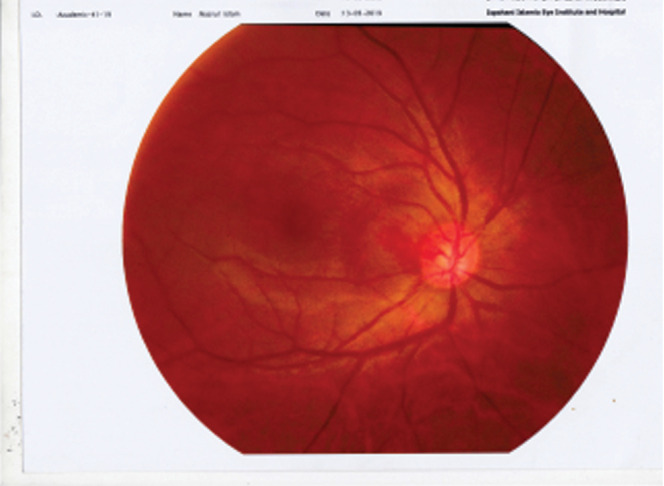
Post treatment picture after intravitreal Avastin (Right Eye) showed complete resolution of tumour mass
Patient vision still remain 6/6 and there was no recurrence as at the last follow-up visit 3 years after treatment.
Discussion
Retinal capillary hemangiomas usually occur as a clinically detectable fundus lesion between the age of 20–40 year old, as it was observed in our patient. The condition may be present at birth but are frequently not detected until this time because of the usual small size and peripheral location of the tumors.[5]
Although they may develop anywhere in the retina, they tend to be most prevalent in the temporal mid-periphery of the eye in about 66% of cases.[6] Optic disc and juxtapapillary angiomas have also been observed but less frequently, with a prevalence of 8.3%.[6]
Juxtapapillary angiomas typically have a poorer prognosis than mid-peripherally located lesions. Patients tend to manifest with bilateral, multiple tumors and often present for examination earlier due to associated visual symptom.[7] As in the case of our patient who presented at the age of 22 years with significant visual loss in left eye, following vitreous hemorrhage and tractional retinal detachment from diseased complication. And despite surgical intervention there was no visual improvement in the left eye.
Retinal angiomas are bilateral in approximately 50% of cases[8] as in this index case. The condition can occur idiopathically, however, it is more commonly found in association with VHL disease. The literature shows variable rates of association, although this is dependent on the type of angiomatosis present (single versus multiple angiomas).[5] In a study of 41 patients, Kreusel et al.[9] found 13 (32%) had a solitary angioma. Of these patients, only 38% were diagnosed with VHL disease in contrast, to all patients with multiple retinal angioma who were reported to have the disease.
VHL disease is an autosomal dominant disease cause by mutation in VHL gene, a tumor suppressor gene.[10] The main manifestation of the disease are retinal and central nervous system hemangioma. The syndrome has been known to be complicated with other neoplasm such as adrenal phechromocytoma, preganglioma, renal cell carcinoma, islet cell tumors, pancreatic cyst and neuroendocrine tumors.[10] The index case presented with multiple bilateral retinal hemangioma associated with polycystic kidney disease in the absence of other abdominal neoplasm, normal brain MRI and Audiometry, however it was not certain whether he has VHL syndrome as at the time of diagnosis and during the follow-up period because of limited facilities in genetic screening.
Retinal hemangioma has posed a therapeutic problems for ophthalmologists for almost a decade.[11] The location of hemangioma in the retina is an important factor in determining the treatment options as well as the size of the tumor, clarity of media, and secondary features of the mass.[4]
Treatment options include cryotheraphy, direct laser photocoagulation, plaque radiotheraphy, transpupillary thermotheraphy, photodynamic theraphy, extermal beam radiation and intravitreal anti-VEGF agents.[1]
The treatment of retinal hemangioblastoma varies with the clinical situation.[12,13,14] Tumors associated with VHL syndrome tend to be more aggressive; therefore, nearly all retinal hemangioblastomas must be considered for treatment. If lesions are small (<3 mm) in size, laser photocoagulation or photodynamic therapy (PDT) can be used; if medium (3–6 mm), PDT or cryotherapy can be used; and if large (>6 mm), PDT, plaque radiotherapy, or internal resection by pars plana vitrectomy route can be employed.[15]
Tumors not associated with VHL syndrome that are small and have asymptomatic lesions without subretinal fluid can be cautiously observed, particularly if they are in the macular, perimacular, or juxtapapillary region, where treatment could be detrimental to vision, unless if leakage ensues, then treatment is warranted. Criteria for treatment of these lesions include, Laser photocoagulation and PDT useful for small- to medium-sized tumors located posterior to the equator and cryotherapy, for those anterior to the equator.[15] Plaque radiotherapy is reserved for larger tumors, and surgical repair of secondary Epiretinal Membrane or tractional retinal detachment is occasionally necessary. In the case of an aggressive juxtapapillary tumor that does not respond to conventional treatment, external beam radiotherapy or plaque radiotherapy can be considered.[15]
Wong and Chew[12] reviewed the role of anti-VEGF agents and emerging therapies for retinal hemangioblastoma and reported that intravitreal anti-VEGF can be useful for reducing macular edema and occasionally subretinal fluid.[12] The expression of VEGF and the usefulness of intravitreal injection of anti-VEGF drugs was also reported in retinal vascularized tumors, including hemangioblastoma in VHL disease and astrocytic hamartoma in tuberous sclerosis.[16]
Some of the differentials diagnosis that were considered in the index patient were vasoproliferative vasoproliferative retinal tumours retinal tumors, these are benign glial and vascularized tumors of the sensory retina, commonly located at the inferotemporal periphery. However, patients with vasoproliferative retinal tumours have no systemic tumors as in VHL disease, and are not associated with large retinal feeder and tortous blood vessels, as observed in retinal hemangioblastomas.[16] Astrocytic hamartomas were another differential, these are mulberry-like yellowish lesions in the retinal peripapillary region usually associated with neurocutaneous syndromes like tuberous sclerosis,[17] these features were absent in the index patient. Optic nerve drusen was also considered as a differential in this case and were ruled out as the hemangiomas were obviously distinct from the optic nerve head with the absence of blurring of the disc margins.[17]
Conclusion
Anti-VEGF factors like Bevacizumab (avastin) were found to be effective in the treatment of retinal capillary hemangioma, thereby inducing complete tumor resolution as well as maintaining good vision in the early stages of the disease before complication occurs, as it is evident in this case study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Singh AD, Ahmad NN, Shields CL, Shields JA. Solitary retinal capillary haemangioma: Lack of genetic evidence for Von Hippel-Lindau disease. Ophthalmic Genet. 2002(23):21–7. doi: 10.1076/opge.23.1.21.2201. [DOI] [PubMed] [Google Scholar]
- 2.Niemela M, Lemeta S, Sainio M, Rauma S, Pukkala E, Kere J, et al. Haemangioblastomas of the retina: Impact of Von Hippel-Lindau disease. Invest Ophthalmol Vis Sci. 2000;41:1909–15. [PubMed] [Google Scholar]
- 3.Kanski JJ. A Systemic Approach. 8th ed. Brad Bowling; 2016. Clinical Ophthalmology; pp. 506–509. [Google Scholar]
- 4.Anand D, Razdan TB, Lal H. A case of retinal capillary haemangioma. DOS Times. 2015;20:59–62. [Google Scholar]
- 5.Paul S, Robyn T, Kevin V. Retinal angioma associated with Von Hippel Landau disease. Clin Exp Optom. 2003(86):187–91. doi: 10.1111/j.1444-0938.2003.tb03102.x. [DOI] [PubMed] [Google Scholar]
- 6.Webster AR, Maher ER, Moore AT. Clinical characteristics of ocular angiomatosis in Von Hippel-Lindau disease and correlation with germline mutation. Arch Ophthalmol. 1999(117):371–8. doi: 10.1001/archopht.117.3.371. [DOI] [PubMed] [Google Scholar]
- 7.McCabe CM, Flynn HW, Shields CL, Shields JA, Regillo CD, McDonald HR, et al. Juxtapapillary capillary haemangiomas: Clinical features and visual acuity outcomes. Ophthalmology. 2000;107:2240–8. doi: 10.1016/s0161-6420(00)00422-x. [DOI] [PubMed] [Google Scholar]
- 8.Dollfus H, Masin P, Taupin P, Nemeth C, Amara S, Giraud S, et al. Retinal haemangioblastoma in Von Hippel-Lindau disease: A clinical and molecular study. Invest Ophthalmol Vis Sci. 2002;43:3067–307. [PubMed] [Google Scholar]
- 9.Webster AR, Maher ER, Bird AC, Gregor ZG, Moore AT. A clinical and molecular genetic analysis of solitary retinal angioma. Ophthalmol. 1999(106):623–9. doi: 10.1016/S0161-6420(99)90127-6. [DOI] [PubMed] [Google Scholar]
- 10.Singh AD, Shields CL, Shields JA. Von Hippel Landau disease. Surv Ophthalmol. 2001(46):117–42. doi: 10.1016/s0039-6257(01)00245-4. [DOI] [PubMed] [Google Scholar]
- 11.Toshihiko M, Kengo H, Kouichi I, Hiroyuki Y, Soichiro N, et al. Longterm effect of external beam radiation of optic disc haemangioma in a patient with Von Hippel Landau disease. Acta Med Okayam. 2011;65:135–41. doi: 10.18926/AMO/45273. [DOI] [PubMed] [Google Scholar]
- 12.Wong WT, Chew EY. Ocular Von Hippel-Lindau disease: Clinical update and emerging treatments. Curr Opin Ophthalmol. 2008(19):213–7. doi: 10.1097/ICU.0b013e3282fb7c04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Singh AD, Nouri M, Shields CL, Shields JA, Perez N. Treatment of retinal capillary hemangioma. Ophthalmology. 2002(109):1799–806. doi: 10.1016/s0161-6420(02)01177-6. [DOI] [PubMed] [Google Scholar]
- 14.Ach T, Thiemeyer D, Hoeh AE, Schaal KB, Dithmar S. Intravitreal bevacizumab for retinal capillary hemangioma: Longterm results. Acta Ophthalmol. 2010;88:e137–8. doi: 10.1111/j.1755-3768.2009.01594.x. [DOI] [PubMed] [Google Scholar]
- 15.Carol LS, Alexzandra D, Timothy H, Wisim AS, Jerry AS. Special focus ocular oncology. Retina Today. 2015:61–7. [Google Scholar]
- 16.Saito W, Kase S, Fujiya A, Dong Z, Noda K, Ishida S. Expression of vascular endothelial growth factor and intravitreal anti-VEGF therapy with bevacizumab in vasoproliferative retinal tumors. Retina. 2013(33):1959–67. doi: 10.1097/IAE.0b013e3182923490. [DOI] [PubMed] [Google Scholar]
- 17.Babalola YO, Shah MS, Padhy SK, Behera UC. Bilateral astrocytic hamartoma with vasoproliferative tumour in retinitis pigmentosa. Niger Postgrad Med J. 2023(30):81–4. doi: 10.4103/npmj.npmj_265_22. [DOI] [PubMed] [Google Scholar]