Abstract
Once considered a rare and often difficult diagnosis in the era predating routine MRI, idiopathic intracranial hypertension has become an everyday concern in ophthalmology and neurology clinics where, especially in the latter, essentially every young overweight woman with headaches is initially presumed to have IIH. Has the diagnosis of IIH become too easy, and are we over-diagnosing IIH in this period of an accelerating obesity crisis? Or are we actually missing cases of IIH because they do not fit the classic clinical profile? We think it is both: at the same time IIH is being diagnosed in excess in obese women without papilledema, often resulting in unnecessary procedures, inappropriate treatment and even iatrogenic complications, the spectrum of this disorder is expanding to include a broad array of clinical presentations that involve multiple specialists beyond just the ophthalmologist and neurologist.
Subject terms: Diseases, Eye diseases, Optic nerve diseases
Abstract
在常规核磁共振成像出现前的时代, 特发性颅内高压 (IIH) 被认为是一种罕见且通常难以诊断的疾病, 如今已经成为眼科和神经科诊所日常的关注点, 特别是在后者, 基本上每个患有头痛的年轻超重女性最初都被推定为IIH。IIH的诊断是否变得过于简单, 在这个肥胖危机加速的时期, 我们是否过度诊断了IIH? 还是我们实际上遗漏了IIH的病例, 因为他们不符合经典的临床特征? 我们认为两者都是: 同时, IIH在无视神经乳头水肿的肥胖女性中被过度诊断, 往往导致不必要的操作、不恰当的治疗甚至是医源性并发症, 这种疾病疾病诊断的范围正在扩大, 包括广泛的临床表现。IIH的诊断除了与眼科医生和神经科医生有关之外, 还涉及到了多个领域的专家。
Advancements in imaging techniques, changes in healthcare models, and evolution of awareness of various conditions are constantly altering diagnostic strategies and remodelling patient access to specialized care. Most practicing clinicians will agree that the following case scenario has become very common over the past few years: a 28-year-old obese woman presents with chronic headaches for which brain imaging is performed. An intracranial mass, hydrocephalus, and venous sinus thrombosis are excluded, but there is an expanded and empty sella, flattening of the globes, mild dilation of the optic nerve sheaths and bilateral transverse venous sinus stenoses. Her ophthalmological examination is normal with the exception of some mild optic nerve head elevation and peripapillary changes possibly suggestive of previous optic disc swelling. Lumbar puncture shows an opening pressure of 25 cm of water with normal cerebrospinal fluid (CSF) contents. A neurologist diagnoses her with idiopathic intracranial hypertension (IIH) and the patient is treated with acetazolamide and instructed to lose weight. Her headaches persist, resulting in escalation of her acetazolamide dosage, multiple visits to various healthcare providers and progressive disability. She is not able to lose weight and she becomes frustrated, losing confidence in her providers.
Once considered a rare and often difficult diagnosis in the era predating routine MRI, IIH has become an everyday concern in ophthalmology and neurology clinics where, especially in the latter, essentially every young overweight woman with headaches is initially presumed to have IIH [1]. Has the diagnosis of IIH become too easy, and are we over-diagnosing IIH in this period of an accelerating obesity crisis? Or are we actually missing cases of IIH because they do not fit the classic clinical profile? We think it is both: at the same time IIH is being diagnosed in excess in obese women without papilledema, often resulting in unnecessary procedures, inappropriate treatment and even iatrogenic complications [1, 2], the spectrum of this disorder is expanding to include a broad array of clinical presentations that involve multiple specialists beyond just the ophthalmologist and neurologist [3].
The rise in obesity rates worldwide has resulted in an increased prevalence of disorders associated with excessive body weight. This includes IIH, the incidence of which rose between 2002 and 2016 from 2.3 to 4.7 per 100,000 in the general population in the UK, with a peak incidence of 15.2 per 100,00 in women aged 25 years. This number is likely already much higher given the continuous rise in obesity [4]. Indeed, the prevalence of IIH and related syndromes has more than doubled over the past decade [5] and the dramatic projected prevalence of obesity and severe obesity, estimated at 50% of the U.S. adult population in 2030 [6], will likely parallel an epidemic of IIH-related syndromes, with an overwhelming burden on ophthalmologists, neurologists and neuro-ophthalmologists worldwide.
The exact mechanisms and causes of this syndrome of chronic isolated intracranial pressure remain largely unknown. IIH occurs most often in young overweight women, has multidisciplinary manifestations, and results in visual loss, chronic headaches, chronic tinnitus, depression and even cognitive impairment, with decreased quality of life and chronic disability associated with multiple hospital admissions [2, 7]. As such, there is a pressing need for better understanding and improved management of this disorder to limit the inevitable burden on healthcare systems around the world.
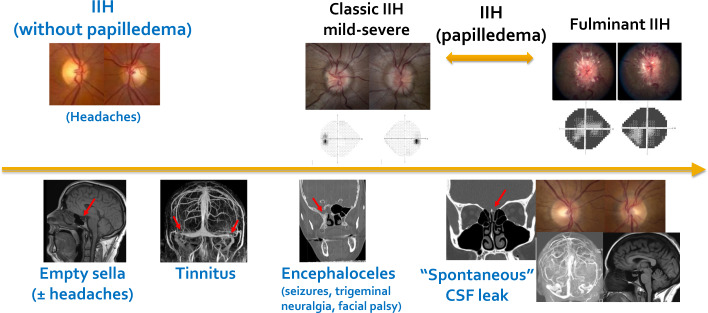
Since the last revision of the classic diagnostic criteria for IIH published by Friedman et al. [8], improved brain imaging techniques and better characterization of the multiple radiographic manifestations of elevated intracranial pressure have expanded the spectrum of symptoms and signs described in association with, or as complications of, chronic intracranial hypertension [9–11]. Beyond the classic extreme presentations of IIH with severe fulminantly-presenting papilledema and visual loss, and asymptomatic IIH with very mild papilledema and normal visual function, the spectrum of the IIH continuum now includes isolated chronic headaches without papilledema (so-called IIH without papilledema), incidentally-noted radiographic signs suggestive of intracranial hypertension (such as isolated empty sella) in a completely asymptomatic individual, compression of cranial nerves from meningoencephaloceles (causing, for example, secondary trigeminal neuralgia), seizures from temporal lobe encephaloceles, isolated tinnitus from transverse venous sinus stenosis, and spontaneous skull-base CSF leak [12–18] (Fig. 1). Although these various manifestations likely reflect a common underlying pathologic process (i.e., chronically elevated intracranial pressure), their respective morbidities, outcomes and managements are different, spanning a variety of specialists (ophthalmologists, neuro-ophthalmologists, neurologists, otolaryngologists, neurosurgeons and endocrinologists) and currently lacking in consistent appropriate management guidelines.
Fig. 1. Spectrum of idiopathic intracranial hypertension.
Classic IIH includes papilledema, which is associated with a risk of visual loss ranging from mild reversible visual field changes in very mild papilledema to profound irreversible visual loss with severe papilledema in very aggressive IIH such as fulminant IIH. Elevated intracranial hypertension without papilledema (IIH without papilledema), isolated radiologic changes suggestive of intracranial hypertension such as empty sella, tinnitus and encephaloceles, and cerebrospinal fluid leak are likely all on the spectrum of IIH, but are usually not associated with papilledema and, therefore, do not portend a risk of visual loss. IIH idiopathic intracranial hypertension.
The classic diagnostic criteria for IIH require the presence of papilledema on funduscopic examination [8]. The severity of papilledema varies tremendously and while patients with severe papilledema are at risk of irreversible visual loss with secondary optic atrophy and must be treated aggressively, a patient with mild or no papilledema can be treated medically or with weight management alone [7]. Most IIH patients have symptoms of intracranial hypertension such as headaches and pulsatile tinnitus; however, it is not uncommon for papilledema to be discovered incidentally on routine ocular examination of an asymptomatic patient, often resulting in a diagnostic dilemma for ophthalmologists [15]. Although the diagnosis and management of patients with papilledema and IIH is well codified and relatively homogeneous around the world [7, 19], deciding whether a patient with chronic headaches and radiologic signs of intracranial hypertension (but no papilledema) has IIH, and therefore may benefit from a lumbar puncture and treatments aimed at decreasing the intracranial pressure, is much less clear [3, 7, 17, 19]. Indeed, isolated signs of intracranial hypertension are often found on routine brain imaging obtained for any reason. In one series of 296 patients undergoing an outpatient brain MRI, nearly half had at least one imaging sign of intracranial hypertension, with empty sella being the most common; however, only 5 of the 296 patients (1.7%) were found to have papilledema on fundus photographs obtained at the time of the MRI and only 3 of these patients had IIH [16]. This study emphasizes the need for radiologists to be cautious when interpreting brain imaging and reporting incidental radiologic signs of IIH, as highlighted in a commentary recently published in the American Journal of Radiology [20]. This is particularly important considering the rise in neuro-ophthalmology consultations and emergency department visits for presumed IIH [2]. Our own neuro-ophthalmology service, located in a tertiary care centre in the south of the U.S. where obesity rates are particularly high, is overwhelmed daily with urgent requests to evaluate patients with presumed IIH, often based solely on incidental findings of radiologic signs suggesting possible intracranial hypertension, or, conversely, simply because they are young obese women with headaches. During a one-year period in 2019, 20% of all new patients seen in our neuro-ophthalmology outpatient clinic were referred (often urgently) because of concern for IIH, but only 27% of these patients were confirmed to have papilledema [17]. Many more patients were sent to our emergency department for immediate evaluation and were therefore not captured in this study. There is consensus among neuro-ophthalmologists worldwide that the burden of these “rule-out IIH” consultations is overwhelming and will only continue to rise with the concurrent obesity epidemic, straining the already limited neuro-ophthalmologic resources available [4, 5].
Because of the risk of vision loss if papilledema is present, we agree that it is essential to look for papilledema in all patients with symptoms suggesting intracranial hypertension such as headaches or pulsatile tinnitus, and even in those patients with incidentally found radiologic signs associated with intracranial hypertension. Ocular fundus examination can be performed by any ophthalmologist or optometrist, or via ocular fundus photography [21]. The finding of papilledema should prompt further workup with a lumbar puncture and detailed evaluation of visual function to ensure appropriate treatment and prevention of visual loss. Those patients without papilledema should be evaluated and treated by neurologists or otolaryngologists, depending on their main complaint. Although it is possible that these patients had intracranial hypertension in the past, most of these patients likely do not have active IIH at the time of evaluation, in which case they do not require further workup or treatment aimed at decreasing the intracranial pressure. Indeed, numerous recent studies have shown that chronic intracranial hypertension leads to progressive remodelling of the skull base with expansion of the sella turcica, enlargement of Meckel caves and bone thinning with development of encephaloceles [9]. These radiologic signs take years to develop and do not resolve once the intracranial pressure normalizes. Other classic radiologic signs such as flattening of the posterior globes, dilation of the optic nerve sheaths and transverse venous sinus stenoses may improve over time but may also persist despite normalization of the intracranial pressure [9, 11]. This explains why some patients present with isolated persistent tinnitus related to sigmoid venous sinus stenosis or neurologic signs secondary to herniation of cerebral contents and cranial nerves into large skull-base encephaloceles [3, 12]. Others may ultimately develop “spontaneous” skull-base CSF leak into the nasal cavity or ears [3, 13, 14]. These patients most often do not have ongoing intracranial hypertension, as their intracranial pressure likely has compensated or been “released” by the skull-base expansion or CSF leak, and they therefore do not have papilledema at the time of diagnosis [22, 23]. Symptomatic management of the specific symptoms and signs instead of treatments specifically aimed at decreasing the intracranial pressure is reasonable in many of these patients, although CSF leaks can predispose to meningitis and these patients are usually treated with leak repair, a process that at least theoretically can precipitate a rise in intracranial pressure and perhaps papilledema [13, 22]. The prevalence of chronic mixed mechanism headaches is very high in this patient population, and they would benefit greatly from multidisciplinary management in headache centres aimed at treating analgesic abuse headaches, chronic tension headaches and transformed migraines [7, 24]. Although these patients have no papilledema, and therefore are not at risk of visual loss, they likely do belong to the expanding spectrum of IIH.
It is most important to highlight that virtually all the patients along this expanded IIH spectrum are overweight or obese, sometimes morbidly so, and predominantly female. Given the major role played by obesity in the pathophysiology of IIH, it is likely that the common primary long-term treatment for all manifestations of the IIH spectrum should be weight loss. Indeed, weight loss is highly associated with a decrease in intracranial pressure, improved papilledema, improved quality of life and decreased risk of IIH recurrence [25, 26]. It remains to be shown whether weight reduction similarly improves the symptoms and signs of patients along this newly appreciated IIH spectrum, or whether the symptom-causing damage is irreversible. The increased burden of obesity and rapidly increasing prevalence of IIH make it essential that multidisciplinary IIH centres be implemented worldwide, to include ophthalmologists, neuro-ophthalmologists, neurologists, especially those with an expertise in headache, otolaryngologists, interventional neuroradiologists and neurosurgeons, as well as nutritionists and bariatric surgeons [3, 5, 27]. Such multidisciplinary centres addressing all aspects of the expanding spectrum of IIH should facilitate holistic management of these patients, targeting not only direct treatment of intracranial hypertension and papilledema, but also aggressive management of headache, CSF leak repair, symptomatic relief, improvement of patient quality of life, and sustained weight loss, preferably via a series of rapid interventions to begin as soon as diagnosis is made and before symptoms become chronic and disabling, thereby improving outcomes and preventing long-term disability [28].
Author contributions
VB and NJN have equally contributed to the preparation of the manuscript, including review and selection of relevant publications, collection of data, preparation of the first draft, review of the final draft, and preparation of the figure.
Funding
There is no funding for this manuscript. VB and NJN are supported in part by NIH/NEI core grant P30-EY06360 (Department of Ophthalmology, Emory University School of Medicine), by and by a departmental grant from Research to Prevent Blindness.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fisayo A, Bruce BB, Newman NJ, Biousse V. Overdiagnosis of idiopathic intracranial hypertension. Neurology. 2016;86:341–50. doi: 10.1212/WNL.0000000000002318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mollan SP, Mytton J, Tsermoulas G, Sinclair AJ. idiopathic intracranial hypertension: evaluation of admissions and emergency readmissions through the hospital episode statistic dataset between 2002-2020. Life. 2021;11:417. doi: 10.3390/life11050417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Urbach H, Duman IE, Altenmüller DM, Fung C, Lützen N, Elsheikh S, et al. Idiopathic intracranial hypertension - a wider spectrum than headaches and blurred vision. Neuroradiol J. 2022;35:183–92. doi: 10.1177/19714009211034480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mollan SP, Aguiar M, Evison F, Frew E, Sinclair AJ. The expanding burden of idiopathic intracranial hypertension. Eye. 2019;33:478–85. doi: 10.1038/s41433-018-0238-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miah L, Strafford H, Fonferko-Shadrach B, Hollinghurst J, Sawhney IM, Hadjikoutis S, et al. Incidence, prevalence and healthcare outcomes in idiopathic intracranial hypertension: a population study. Neurology. 2021;96:e1251–1261. doi: 10.1212/WNL.0000000000011463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ward ZJ, Bleich SN, Cradock AL, Barrett JL, Giles CM, Flax C, et al. Projected U.S. state-level prevalence of adult obesity and severe obesity. N Engl J Med. 2019;381:2440–50. doi: 10.1056/NEJMsa1909301. [DOI] [PubMed] [Google Scholar]
- 7.Ducros A, Biousse V. Headache arising from idiopathic changes in CSF pressure. Lancet Neurol. 2015;14:655–68. doi: 10.1016/S1474-4422(15)00015-0. [DOI] [PubMed] [Google Scholar]
- 8.Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults in children. Neurology. 2013;81:1159–65. doi: 10.1212/WNL.0b013e3182a55f17. [DOI] [PubMed] [Google Scholar]
- 9.Bidot S, Saindane AM, Peragallo JH, Bruce BB, Newman NJ, Biousse V. Brain imaging in idiopathic intracranial hypertension. J Neuroophthalmol. 2015;35:400–11. doi: 10.1097/WNO.0000000000000303. [DOI] [PubMed] [Google Scholar]
- 10.Mallery RM, Rehmani OF, Woo JH, Chen YJ, Reddi S, Salzman KL, et al. Utility of magnetic resonance imaging features for improving the diagnosis of idiopathic intracranial hypertension without papilledema. J Neuroophthalmol. 2019;39:299–307. doi: 10.1097/WNO.0000000000000767. [DOI] [PubMed] [Google Scholar]
- 11.Kwee RM, Kwee TC. Systematic review and meta-analysis of MRI signs for diagnosis of idiopathic intracranial hypertension. Eur J Radiol. 2019;116:106–15. doi: 10.1016/j.ejrad.2019.04.023. [DOI] [PubMed] [Google Scholar]
- 12.Chen BS, Newman NJ, Biousse V. Unusual manifestations of idiopathic intracranial hypertension. Taiwan J Ophthalmol. 2020;11:25–38. doi: 10.4103/tjo.tjo_69_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bidot S, Levy JM, Saindane AM, Oyesiku NM, Newman NJ, Biousse V. Do most patients with a spontaneous cerebrospinal fluid leak have idiopathic intracranial hypertension? J Neuroophthalmol. 2019;39:487–95. doi: 10.1097/WNO.0000000000000761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bidot S, Levy JM, Saindane AM, Narayana KM, Dattilo M, DelGaudio JM, et al. Spontaneous skull base cerebrospinal fluid leaks and their relationship to idiopathic intracranial hypertension. Am J Rhinol Allergy. 2021;35:36–43. doi: 10.1177/1945892420932490. [DOI] [PubMed] [Google Scholar]
- 15.Vosoughi AR, Margolin EA, Micieli JA. Idiopathic intracranial hypertension: incidental discovery versus symptomatic presentation. J Neuro Ophthalmol. 2022;42:187–91. doi: 10.1097/WNO.0000000000001475. [DOI] [PubMed] [Google Scholar]
- 16.Chen BS, Meyer BI, Saindane AM, Bruce BB, Newman NJ, Biousse V. Prevalence of incidentally detected signs of intracranial hypertension on magnetic resonance imaging and their association with papilledema. JAMA Neurol. 2021;78:718–25. doi: 10.1001/jamaneurol.2021.0710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Aung AB, Chen BS, Wicks J, Bruce BB, Meyer BI, Dattilo M, et al. presumptive idiopathic intracranial hypertension based on neuroimaging findings: a referral pattern study. J Neuroophthalmol. 2022. 10.1097/WNO.0000000000001660. [DOI] [PubMed]
- 18.Bouffard MA. Fulminant idiopathic intracranial hypertension. Curr Neurol Neurosci Rep. 2020;20:8. doi: 10.1007/s11910-020-1026-8. [DOI] [PubMed] [Google Scholar]
- 19.Mollan SP, Moss HE, Hamann S. Evolving evidence in idiopathic intracranial hypertension. Life. 2021;11:1225. doi: 10.3390/life11111225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuner AD, Kennedy TA. Beyond the AJR: isolated incidentally detected imaging findings associated with idiopathic intracranial hypertension are common in patients without papilledema. Am J Roentgenol. 2021. 10.2214/AJR.21.26469. [DOI] [PubMed]
- 21.Biousse V, Danesh-Meyer, HV, Saindane AM, Lamirel C, Newman NJ. Imaging of the optic nerve: technological advances and future prospects. Lancet Neurol. 2022. 10.1016/S1474-4422(22)00173-9. [DOI] [PubMed]
- 22.Aaron G, Doyle J, Vaphiades MS, Riley KO, Woodworth BA. Increased intracranial pressure in spontaneous CSF leak patients is not associated with papilledema. Otolaryngol Head Neck Surg. 2014;151:1061–6. doi: 10.1177/0194599814551122. [DOI] [PubMed] [Google Scholar]
- 23.Buchowicz B, Chen BS, Bidot S, Bruce BB, Newman NJ, Saindane AM, et al. CSF-Leak Study Group. Prediction of postoperative risk of raised intracranial pressure after spontaneous skull base cerebrospinal fluid leak repair. J Neuroophthalmol. 2021;41:e490–e497. doi: 10.1097/WNO.0000000000001118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mollan SP, Grech O, Sinclair AJ. Headache attributed to idiopathic intracranial hypertension and persistent post-idiopathic intracranial hypertension headache: a narrative review. Headache. 2021;61:808–16. doi: 10.1111/head.14125. [DOI] [PubMed] [Google Scholar]
- 25.Mollan SP, Mitchell JL, Ottridge RS, Aguiar M, Yiangou A, Alimajstorovic Z, et al. Effectiveness of bariatric surgery vs community weight management intervention for the treatment of idiopathic intracranial hypertension: a randomized clinical trial. JAMA Neurol. 2021;78:678–86. doi: 10.1001/jamaneurol.2021.0659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mollan SP, Mitchell JL, Yiangou A, Ottridge RS, Alimajstorovic Z, Cartwright DM, et al. Association of amount of weight lost after bariatric surgery with intracranial pressure in women with idiopathic intracranial hypertension. Neurology. 2022;99:e1090–e1099. doi: 10.1212/WNL.0000000000200839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Totten DJ, Schueth E, Saltagi MZ, Rabbani C, Harris AH, Tressman D, et al. Trends in spontaneous cerebrospinal fluid leak repairs in the United States, 2009-2018. Otol Neurotol Open. 2022;2:e021. doi: 10.1097/ONO.0000000000000021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Thaller M, Homer V, Hyder Y, Yiangou A, Liczkowski A, Fong AW, et al. The idiopathic intracranial hypertension prospective cohort study: evaluation of prognostic factors and outcomes. J Neurol. 10.1007/s00415-022-11402-6. [DOI] [PMC free article] [PubMed]