Abstract
Key clinical message
The coexistence of hepatic mucinous cystic neoplasm and ovarian serous cystadenoma is rare and can only be confirmed by histological examination of the surgical specimen. Complete surgical resection is the optimal treatment.
Abstract
Mucinous cystic neoplasms (MCN) of the liver are rare premalignant lesions that account for less than 5% of all hepatic cysts. The synchronous occurrence of hepatic MCN with ovarian cystadenomas is rare. Herein, we report a case of a hepatic MCN coexistent with a serous ovarian cystadenoma.
Keywords: liver, mucinous cystic neoplasm, ovary, pathology, serous cystadenoma, surgery
We report a rare association of mucinous cystic neoplasm with ovarian serous cystadenoma in a young female patient. The diagnosis was confirmed by histopathological examination of the surgical specimen.
1. CASE DESCRIPTION
A 27‐year‐old previously healthy female patient, presented with a seven‐month history of pelvic pain. Physical examination of the patient was unremarkable. Pelvic CT scan demonstrated a unilocular cystic mass of the right ovary measuring 8 × 7 cm (Figure 1A). Axial abdominal CT scan revealed a multiloculated cystic mass with septations of segment IV measuring 11 × 7.8 cm suggestive of a hydatid cyst (Figure 1B). Laboratory tests including tumor markers (CA 125) were within normal limits. Preoperative fine needle aspiration of the liver cyst disclosed bland cuboidal epithelial cells within an inflammatory and myxoid background (Figure 1C,D). The patient underwent surgical resection of the hepatic and ovarian mass. Grossly, the hepatic cystic mass was multiloculated with a smooth glistening white‐tan lining (Figure 2A). Macroscopic examination of the ovarian mass disclosed a round cystic mass with a smooth glistening surface (Figure 2B). On the cut section, the cyst was unilocular filled with a clear fluid. Histological examination of the ovarian cyst showed a cyst wall lined by a single layer of columnar ciliated cells resembling normal tubal epithelium (Figure 2C,D). The hepatic cystic mass was lined by columnar epithelial cells overlying ovarian‐type stroma (Figure 3A–D). The final pathological diagnosis was serous cystadenoma of the right ovary and MCN of the liver. Recovery following surgery went without incident. The patient is currently being monitored on an outpatient basis with a follow‐up period of 2 months.
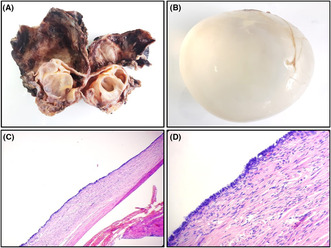
FIGURE 1.
(A) Axial pelvic CT scan revealing a unilocular cystic mass of the right ovary. (B) Axial abdominal CT scan showing a multiloculated cystic mass of segment IV measuring 11 × 7.8 cm. (C) Fine needle aspiration showing bland, degenerated cuboidal epithelial cells within an inflammatory and myxoid background (hematoxylin and eosin, magnification × 40). (D) Fine needle aspiration revealing bland, degenerated cuboidal epithelial cells within an inflammatory and myxoid background (hematoxylin and eosin, magnification × 400).
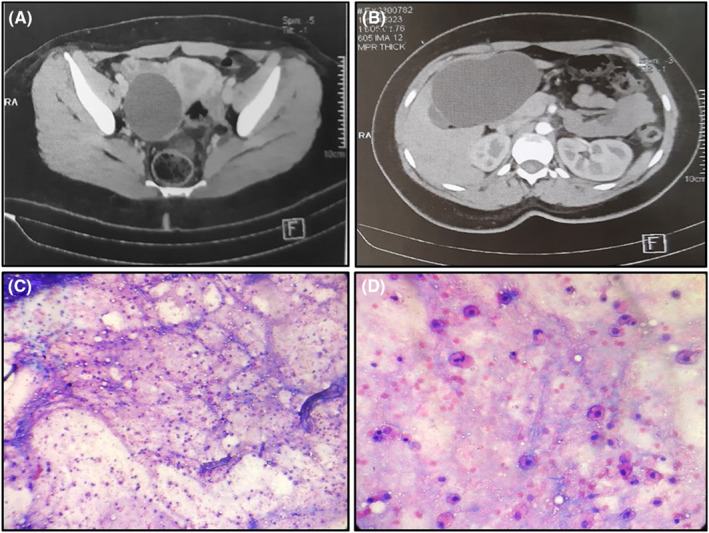
FIGURE 2.
(A) Gross appearance of a mucinous cystic neoplasm of the liver resected from hepatic segment IV. The cut section revealed a multiloculated cyst with a smooth glistening white‐tan lining. (B) Round cystic mass with a smooth glistening surface. The cyst was filled with a clear fluid. (C) Unilocular cyst lined by a single layer of tall, columnar cells. The underlying stroma contained spindle fibroblasts (hematoxylin and eosin, magnification × 40). (D) The cyst wall was lined by a single layer of tall, columnar, ciliated cells. The underlying stroma contained spindle fibroblasts (hematoxylin and eosin, magnification × 400).
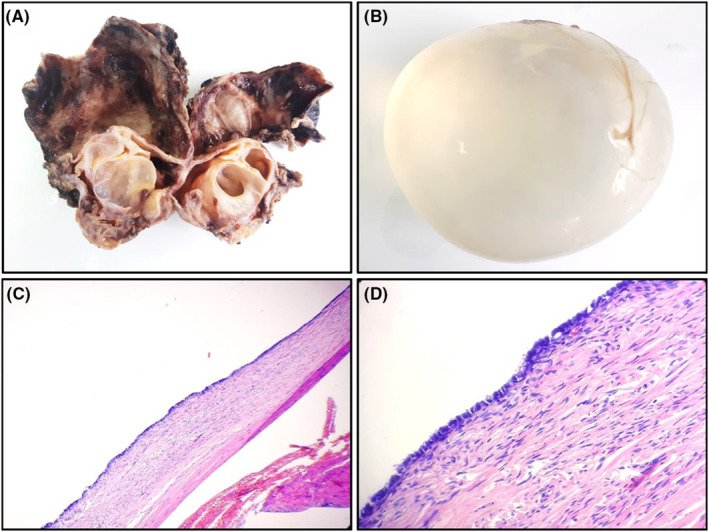
FIGURE 3.
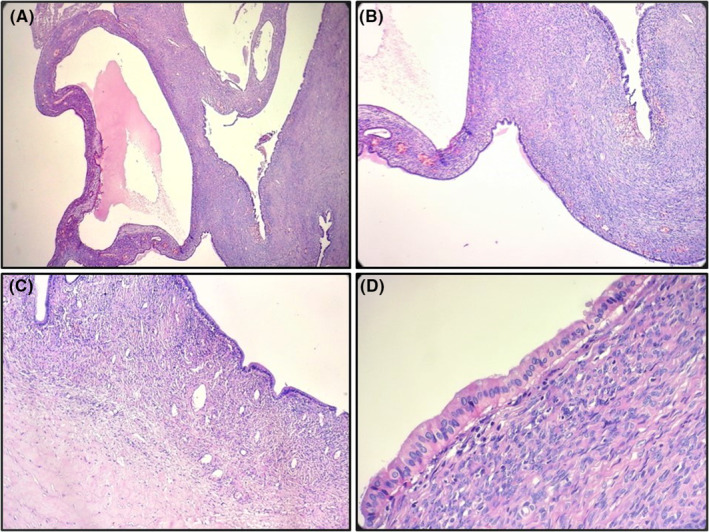
(A) Multiloculated hepatic cyst lined by columnar epithelial cells overlying ovarian‐type stroma (hematoxylin and eosin, magnification × 40). (B) Multiloculated hepatic cyst lined by columnar epithelial cells overlying ovarian‐type stroma (hematoxylin and eosin, magnification × 40). (C) Columnar biliary‐type epithelium overlying dense spindled ovarian‐type stroma (hematoxylin and eosin, magnification × 200). (D) The hepatic cyst wall is lined by a single layer of columnar bland epithelial cells overlying ovarian‐type stroma which consists of densely packed, spindle‐shaped to oval cells. (hematoxylin and eosin, magnification × 400).
2. DISCUSSION AND CONCLUSION
MCN of the liver and biliary system is a cyst‐forming epithelial neoplasm, typically showing no communication with the bile ducts, composed of cuboidal to columnar, variably mucin‐producing epithelium, associated with ovarian‐type subepithelial stroma. MCNs are categorized as MCN with either low/intermediate‐grade dysplasia or high‐grade dysplasia. In our case, MCN of the liver was incidentally discovered by CT scan. In fact, the chief complaint in our patient was pelvic pain. She did not complain of abdominal pain. MCN of the liver cannot be reliably distinguished from other cystic lesions of the liver based on imaging studies and fine needle aspiration. Only histopathological examination of the operative specimen establishes reliably the diagnosis. 1 , 2 The differential diagnoses of hepatic MCN include simple biliary cyst, endometriosis, and intraductal papillary neoplasm. Due to its potential malignant transformation, the optimal treatment for MCN is complete surgical resection whenever possible. Adequate sampling of mucinous cystic neoplasms of the liver is mandatory to rule out high‐grade dysplasia. 1 , 2 About 25% of benign ovarian tumors in women of childbearing age are serous cystadenomas. 3 Patients with serous cystadenoma frequently experience symptoms only if the lesion is twisted or has a mass effect due to its size, making diagnosis difficult due to their insidious growth. The differential diagnoses of ovarian serous cystadenoma include: cortical inclusion cyst, rete cyst, paratubal Mullerian cyst, mesonephric cyst and mucinous cystadenoma.
Our case highlights the difficulty in accurately diagnosing hepatic MCN and ovarian serous cystadenoma in the absence of histological evidence. Early discovery of hepatic MCN may allow better treatment strategies and better prognosis.
AUTHOR CONTRIBUTIONS
Faten Limaiem: Conceptualization; data curation; formal analysis; investigation; methodology; resources; software; supervision; validation; writing – original draft; writing – review and editing.
FUNDING INFORMATION
We did not receive funding for this article.
CONFLICT OF INTEREST STATEMENT
None.
ETHICS STATEMENT
All procedures performed were in accordance with the ethical standards. The examination was made in accordance with the approved principles.
CONSENT
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
ACKNOWLEDGMENT
None.
Limaiem F. Synchronous occurrence of hepatic mucinous cystic neoplasm and serous ovarian cystadenoma. Clin Case Rep. 2023;11:e7760. doi: 10.1002/ccr3.7760
DATA AVAILABILITY STATEMENT
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1. Hutchens JA, Lopez KJ, Ceppa EP. Mucinous cystic neoplasms of the liver: epidemiology, diagnosis, and management. Hepat Med. 2023;15:33‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Alzoubi MN, Alhendi RB, Eyalawwad AA, et al. Liver mucinous cystic neoplasm with obstructive jaundice. Cureus. 2022;14(11):e31970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mounir B, Anas E, Yassine E, et al. Incidental discovery of a giant ovarian cystadenoma. Ann Med Surg (Lond). 2022;82:104698. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


