Abstract
BACKGROUND:
Prediabetes is a high-risk factor for progression to diabetes. Without lifestyle changes, such as weight loss and moderate physical activity, 15%-30% of people with prediabetes are projected to develop type 2 diabetes within 5 years. Progression to diabetes increases the financial burden significantly for patients and health care systems. Populations with low socioeconomic status are associated with a higher risk of diabetes. However, knowledge is limited about the effect of transition to diabetes on future costs incurred in low-income populations.
OBJECTIVES:
To (a) describe the characteristics of low-income and insured patients with prediabetes and (b) examine the effect of progression to type 2 diabetes on health care utilization and costs.
METHODS:
This study used South Carolina Medicaid claims data (2009-2014) to identify patients (aged ≥18 years) with newly diagnosed prediabetes. All patients were enrolled in Medicaid continuously for at least 1 year before and after the diagnosis of prediabetes and were followed for at least 1 year and up to 6 years. The time to progression to type 2 diabetes was measured by a Kaplan Meier curve, and risk factors associated with onset of type 2 diabetes were identified by Cox regression. Generalized linear models were applied to assess the effect of progression to type 2 diabetes on total health care costs during the first 3-year period.
RESULTS:
A total of 7,650 patients with prediabetes met the study criteria. During the follow-up period, 30.3% of the study population developed type 2 diabetes within 3 years. Older age, African-American race, fee-for-service plan, comorbid hypertension, obesity, and dyslipidemia were associated with higher risk for onset of type 2 diabetes. Compared with patients who did not progress to type 2 diabetes, the progression to type 2 diabetes increased total health care costs by 22.1% (P < 0.001), 39.1% (P < 0.001), and 47.6% (P < 0.001) during the first 3 years after adjusting for demographic and comorbid conditions.
CONCLUSIONS:
Age, race, type of Medicaid plan, and diabetes-related comorbidities were associated with risk for progression of prediabetes. Progression to type 2 diabetes significantly increased total health care costs in the first 3 years. Early detection and intervention to prevent or delay onset of type 2 diabetes are needed to control health care utilization and costs.
What is already known about this subject
An estimated 86 million American adults had prediabetes in 2012, but only approximately 11% of those with prediabetes were aware of their condition.
Without lifestyle changes, including weight loss and moderate physical activity, 15%-30% of people with prediabetes will develop type 2 diabetes within 5 years.
Socioeconomic status is associated with prevalence of diabetes and success of diabetes management.
What this study adds
More than one third of patients with prediabetes developed type 2 diabetes within 3 years in the Medicaid population.
Age, race, type of Medicaid plan, and diabetes-related comorbidities were associated with risk for progression of prediabetes in low-income patients with prediabetes.
Total health care costs increased over the first 3 years (22.1%-47.6%) in those who progressed to type 2 diabetes compared with patients who did not progress.
An estimated 86 million American adults had prediabetes in 2012, which is characterized by an elevated blood glucose level confirmed through a fasting plasma glucose test (100 mg/dL-125 mg/dL), an oral glucose tolerance test (140 mg/dL-200 mg/dL), or a hemoglobin A1c test (5.7%-6.4%).1,2 However, only approximately 11% of those with prediabetes were aware of their condition.3 Prediabetes is a high-risk factor for progression to diabetes.4 Progression from prediabetes to diabetes depends on a number of variable factors, including lifestyle changes, genetics, and pharmacological treatments.5,6 However, without weight loss and moderate physical activity, 15%-30% of people with prediabetes will develop type 2 diabetes within 5 years.1 Additionally, patients with prediabetes have an increased risk for developing heart disease and stroke.7-10 Therefore, early detection of and intervention for prediabetes are critical for diabetes prevention.
In 2007, the estimated national average annual cost per case was $443 for prediabetes, $2,864 for undiagnosed diabetes, and $9,975 for diagnosed type 2 diabetes.11 Prediabetes is associated with excessive use of ambulatory care services for comorbidities associated with diabetes,11 and the national annual medical costs of prediabetes were estimated to be more than $25 billion in 2007.11 However, the estimated direct medical costs related to diabetes in the Unites States in 2012 were $176 billion.12 Thus, it is conceivable that progression to diabetes increases the financial burden significantly for patients and health care systems. A previous study reported that progression to type 2 diabetes increased health care expenditures by $1,429 during the first year following diagnosis and by $3,621 during the first 3 years in privately insured patients with prediabetes.13 However, little is known how the transition from prediabetes to diabetes influences future costs incurred in low-income populations.
Socioeconomic status is associated with prevalence of diabetes and success of diabetes management.14-17 Low levels of income, education, and occupation were associated with 40%, 31%, and 41% higher risk of type 2 diabetes than higher levels of these determinants, respectively.16 Understanding characteristics of the low-income population with prediabetes and associated patterns of health care utilization can help providers identify high-risk patients with prediabetes, recognize barriers to diabetes care, and tailor diabetes self-management strategies. Gaining insights into the economic effect of progression to diabetes on the health care system may help prompt cost-effective interventions for disadvantaged populations and produce cost savings for Medicaid. The objectives of the following study were to describe the characteristics of low-income and insured patients with prediabetes and examine the effect of progression to type 2 diabetes on health care costs.
Methods
Data Source
The South Carolina Medicaid claims data were used to identify and follow patients diagnosed with prediabetes between 2009 and 2014. The Medicaid program is a joint federal and state program that shares the cost of providing medical care for persons with limited resources and income. The Medicaid claims data contain inpatient and outpatient medical services and prescription drug records of beneficiaries. Over 1 million South Carolinians are enrolled in Medicaid each fiscal year, with the number of enrollees increasing on an annual basis. In 2008, there were 944,835 enrollees, and by 2014, there were 1,207,253.18 All study data files were de-identified and provided by the South Carolina Revenue and Fiscal Affairs Office. This study was approved by the Presbyterian College Institutional Review Board.
Patient Selection
Patients (aged ≥ 18 years) with a diagnosis of prediabetes between January 2009 and December 2013 were identified by using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes indicating impaired fasting glucose (790.21), impaired glucose tolerance test (790.22), or other abnormal glucose (790.29).13 The index date was the first date of diagnosis of prediabetes. Each patient was required to be enrolled in Medicaid continuously for at least 1 year before (pre-index period) and at least 1 year after the index date (follow-up period). The follow-up period ended at death, the end of continuous enrollment, or the end of the study period (December 31, 2014), whichever occurred first. Patients with a diagnosis of diabetes (type 1 or type 2) before or on index date or with prediabetes or use of oral antidiabetic medications or insulin during the 1 year before the index date were excluded from the study population. In addition, patients with dual eligibility (Medicaid and Medicare) were also excluded from the study population because the complete medical and pharmacy claims of those patients were not available from the Medicaid database (Figure 1). Two groups were created based on whether progression to type 2 diabetes occurred during the follow-up period.
FIGURE 1.
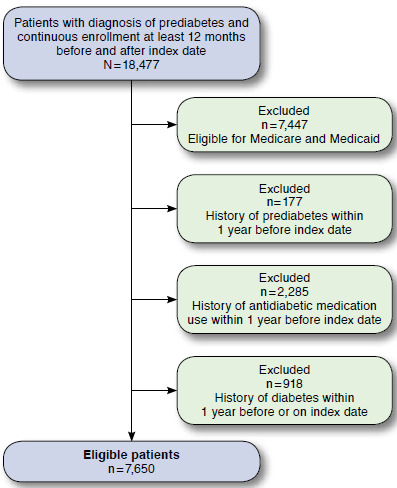
Patient Selection
Demographic Characteristics and Comorbidities
Demographic characteristics were measured on the index date, including age at diagnosis of prediabetes, gender, and race. Three categories were created for the type of Medicaid plan in which the patients enrolled, including fee for service only, managed care only, and both if they changed from one to the other during the study period. Charlson Comorbidity Index, based on ICD-9-CM codes, served as a measure of comorbidity. This index assigned weights for a number of major conditions (ranging from 1 to 6).19 The comorbidity score was calculated for each patient by totaling the assigned weights for each patient’s comorbidities within 1 year before the index date. The higher index score suggests more severe comorbidity. In addition, existing medical conditions that are associated with the risk of developing diabetes, such as hypertension, obesity, and dyslipidemia, were assessed if these conditions were identified during the 1 year before the index date.
Outcome Measures
Time to progression of type 2 diabetes was measured as the number of days from index date to the date of the first diagnosis code of type 2 diabetes. Cumulative incidence was calculated for all eligible patients at various follow-up intervals.
Annual health care costs (per person) were measured over the first 3 years in patient subsets with continuous enrollment for 1, 2, or 3 years after diagnosis of prediabetes. The total number of patients in each interval (year 1, year 2, and year 3) varied because of differences in the enrollment eligibility. Total health care costs included medical and prescription drug costs associated with any medical conditions during the previously mentioned intervals. Medical costs included inpatient, outpatient (physician office and other outpatient visits), and emergency department (ED) use identified from medical claims. Prescription drug use was identified from pharmacy claims. The amounts paid by Medicaid were used to calculate these costs.
Data Analysis
Descriptive statistics summarized the baseline characteristics of the study population. T-tests for continuous variables and chi-square tests for categorical variables compared the characteristics between patients who progressed to type 2 diabetes and patients who did not. A Kaplan-Meier curve was used to report the proportion of patients with progression to type 2 diabetes and time to progression for patients with prediabetes. A Cox regression model identified risk factors associated with progression to type 2 diabetes. In patient subsets with continuous enrollment for 1, 2, or 3 years after diagnosis of prediabetes, t-tests also compared unadjusted health care costs between patients who progressed to type 2 diabetes and patients who did not over the first 3 years following prediabetes diagnosis. Generalized linear models with log link and gamma distribution assessed the effect of progression to diabetes on total health care costs during the first 3-year period after adjusting for demographic characteristics and baseline comorbidities for each previously mentioned subset. The statistical significance was set at P < 0.05. All statistical analyses were performed by using SAS 9.4 (SAS Institute, Cary, NC).
Results
A total of 7,650 patients with prediabetes met the study criteria. Table 1 summarizes the baseline demographic characteristics and comorbidities of the study population with at least 1 year Medicaid enrollment. Compared with those who did not progress to diabetes, patients who progressed to diabetes showed greater proportions among the age group 46-64 years (43.3% vs. 28.8%); fee-for-service plan (16.2% vs. 12.5%); and those with comorbid hypertension (56.8% vs. 36.7%), obesity (23.3% vs. 15.4%), and dyslipidemia (35.2 vs. 21.8%). The characteristics of the population with 2 or 3 years enrollment are presented in Appendices A and B (available in online article).
TABLE 1.
Baseline Characteristics by Diabetes Progression in Medicaid Insured Patients with Prediabetes and Continuous Enrollment ≥ 12 Months
| All Patients with Prediabetes (N = 7,650) | Diabetes Progression (n = 2,406) | No Diabetes Progression (n = 5,244) | P Value | |
|---|---|---|---|---|
| Age (years), mean (SD) | 38.8 (12.6) | 42.6 (11.6) | 37.0 (12.7) | < 0.001 |
| 18-45, % (n) | 66.7 (5,101) | 56.7 (1,365) | 71.2 (3,736) | < 0.001 |
| 46-64, % (n) | 33.3 (2,549) | 43.3 (1,041) | 28.8 (1,508) | |
| Sex, % (n) | ||||
| Female | 77.3 (5,910) | 75.6 (1,818) | 78.0 (4,092) | 0.017 |
| Male | 22.7 (1,740) | 24.2 (588) | 22.0 (1,152) | |
| Medicaid plan, % (n) | ||||
| Fee for service | 13.7 (1,045) | 16.2 (389) | 12.5 (656) | < 0.001 |
| Managed care | 49.7 (3,805) | 47.3 (1,138) | 50.9 (2,667) | |
| Both | 36.6 (2,800) | 36.5 (879) | 36.6 (1,921) | |
| Race, % (n) | ||||
| White | 44.9 (3,432) | 41.9 (1,007) | 46.2 (2,425) | 0.002 |
| African American | 47.1 (3,603) | 49.8 (1,199) | 45.8 (2,404) | |
| Other | 8.0 (615) | 8.3 (200) | 7.9 (415) | |
| Charlson Comorbidity Index, % (n) | ||||
| 0 | 95.9 (7,334) | 94.3 (2,268) | 96.6 (5,066) | < 0.001 |
| 1 | 1.8 (141) | 2.9 (70) | 1.4 (71) | |
| > 1 | 2.3 (175) | 2.8 (68) | 2.0 (107) | |
| Other comorbid conditions, % (n) | ||||
| Hypertension | 57.0 (3,228) | 56.8 (1,366) | 36.7 (1,922) | < 0.001 |
| Obesity | 18.0 (1,380) | 23.3 (573) | 15.4 (807) | < 0.001 |
| Dyslipidemia | 26.0 (1,989) | 35.1 (844) | 21.8 (1,145) | < 0.001 |
SD = standard deviation.
The Kaplan-Meier curve in Figure 2 shows that during the entire study period 31.5% (n = 2,406) of patients developed type 2 diabetes. We found that 18.2% (n = 1,392), 23.2% (n = 1,775), and 30.3% (n = 2,318) of the prediabetes patients progressed to diabetes within 6 months, 1 year, and 3 years, respectively. As seen in Table 2, age, race, Medicaid plan, and comorbid hypertension, obesity, and dyslipidemia were significant risk factors associated with progression from prediabetes to diabetes. Patients aged 46-64 years had 27% higher risk of developing diabetes than those aged 18-45 years after diagnosis of prediabetes (hazard ratio [HR] = 1.27, 95% confidence interval [CI] = 1.14-1.42). The risk of progression to diabetes was 12% higher in African Americans than in whites (HR = 1.12, 95% CI = 1.03-1.22). Patients who were enrolled in a Medicaid managed care plan were 22% less likely to develop diabetes than those in the fee-for-service plan (HR = 0.78, 95% CI = 0.69-0.88). Comorbid hypertension, dyslipidemia, and obesity increased the risk of progression to diabetes by 53% (HR = 1.53, 95% CI = 1.39-1.67), 23% (HR = 1.23, 95% CI = 1.12-1.35), and 48% (HR = 1.48, 95% CI = 1.34-1.63), respectively.
FIGURE 2.
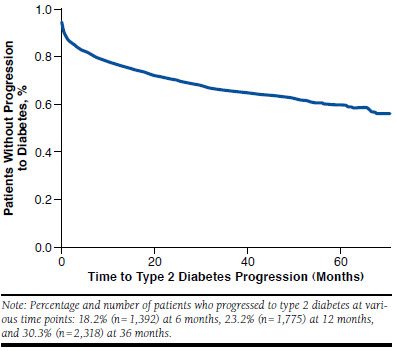
Kaplan-Meier Curve on Progression to Type 2 Diabetes After Diagnosis of Prediabetes (N=7,650)
TABLE 2.
Risk Factors Associated with Progression to Type 2 Diabetes (N = 7,650)
| HR (95% CI) | P Value | |
|---|---|---|
| Age, years | ||
| 18-45 | 1.00 | |
| 46-64 | 1.27 (1.14-1.42) | < 0.001 |
| Sex | ||
| Female | 1.00 | |
| Male | 0.96 (0.88-1.06) | 0.450 |
| Race | ||
| White | 1.00 | |
| African American | 1.12 (1.03-1.22) | 0.009 |
| Other | 1.01 (0.87-1.18) | 0.899 |
| Medicaid plan | ||
| Fee for service | 1.00 | |
| Managed care | 0.78 (0.69-0.88) | < 0.001 |
| Both | 0.86 (0.76-0.97) | 0.012 |
| Hypertension | ||
| No | 1.00 | |
| Yes | 1.53 (1.39-1.67) | < 0.001 |
| Dyslipidemia | ||
| No | 1.00 | |
| Yes | 1.23 (1.12-1.35) | < 0.001 |
| Obesity | ||
| No | 1.00 | |
| Yes | 1.48 (1.34-1.63) | < 0.001 |
| Charlson Comorbidity Index | ||
| 0 | 1.00 | |
| 1 | 1.05 (0.83-1.34) | 0.677 |
| ≥ 2 | 1.37 (1.08-1.74) | 0.011 |
CI = confidence interval; HR = hazard ratio.
Compared with patients who did not progress to diabetes, patients who developed diabetes had more outpatient and ED visits and higher prescription drug utilization over the first 3 years (Table 3). This higher health care utilization pattern resulted in higher medical and total health care costs for the patients who progressed to diabetes. As shown in Table 3, the annual medical costs for patients who progressed to diabetes versus those who did not were $14,744 versus $10,715 for year 1 (P < 0.001), $10,708 versus $7,181 for year 2 (P < 0.001), and $12,438 versus $7,657 for year 3 (P < 0.001). The annual total health care costs including medical and prescription drug costs for patients who progressed to diabetes versus those who did not were $17,506 versus $12,650 for year 1 (P < 0.001), $13,428 versus $9,258 for year 2 (P < 0.001), and $15,151 versus $9,935 for year 3 (P < 0.001). Costs associated with outpatient services accounted for 36%-45% of the total costs over 3 years for all patients. After adjusting for demographic and comorbid conditions, the annual total health care costs in patients who developed diabetes were 22.1% (P < 0.001), 39.1% (P < 0.001), and 47.6% (P < 0.001) higher than those who did not develop diabetes, respectively (Table 4). The gap of adjusted total health care costs between the 2 groups became larger gradually over the first 3 years.
TABLE 3.
Health Care Utilization and Unadjusted Annual Health Care Cost (per Person per Year) by Progression to Type 2 Diabetes for First 3 Years
| Progression to Diabetes | No Progression to Diabetes | P Value | |
|---|---|---|---|
| Utilization | |||
| Year 1 | n = 2,406 | n = 5,244 | |
| Number of outpatient visits, mean (SD) | 25.6 (36.9) | 20.4 (34.3) | < 0.001 |
| Hospitalization per 1,000 person months | 49.7 | 47.9 | 0.453 |
| ED per 1,000 person months | 196.2 | 140.1 | < 0.001 |
| Number of prescriptions, mean (SD) | 25.4 (16.1) | 17.7 (14.5) | <0.001 |
| Year 2 | n = 1,767 | n = 3,035 | |
| Number of outpatient visits, mean (SD) | 23.9 (42.4) | 17.4 (37.5) | < 0.001 |
| Hospitalization per 1,000 person months | 34.9 | 25.4 | 0.001 |
| ED per 1,000 person months | 190.8 | 130.8 | < 0.001 |
| Number of prescriptions mean (SD) | 24.5 (16.6) | 16.9 (14.9) | < 0.001 |
| Year 3 | n = 1,212 | n = 1,686 | |
| Number of outpatient visits, mean (SD) | 24.0 (44.2) | 17.4 (38.7) | < 0.001 |
| Hospitalization per 1,000 person months | 35.6 | 24.6 | 0.001 |
| ED per 1,000 person months | 174.3 | 135.8 | 0.024 |
| Number of prescriptions, mean (SD) | 24.9 (16.5) | 17.4 (15.7) | < 0.001 |
| Costs ($), mean (SD) | |||
| Year 1 | n = 2,406 | n = 5,244 | |
| Medical | 14,744 (34,922) | 10,715 (22,501) | < 0.001 |
| Outpatient | 6,312 (9,372) | 4,798 (12,355) | < 0.001 |
| Inpatient | 6,091 (21,649) | 4,402 (13,610) | < 0.001 |
| ED | 2,413 (10,248) | 1,515 (6,461) | < 0.001 |
| Prescription drug | 2,761 (5,267) | 1,935 (5,446) | < 0.001 |
| Total | 17,506 (36,225) | 12,650 (23,819) | < 0.001 |
| Year 2 | n = 1,767 | n = 3,035 | |
| Medical | 10,708 (24,481) | 7,181 (18,180) | < 0.001 |
| Outpatient | 5,231 (16,344) | 3,880 (8,305) | < 0.001 |
| Inpatient | 3,644 (14,273) | 2,253 (10,434) | < 0.001 |
| ED | 1,834 (8,054) | 1,048 (4,419) | < 0.001 |
| Prescription drug | 2,720 (5,023) | 2,077 (5,787) | < 0.001 |
| Total | 13,428 (25,892) | 9,258 (20,106) | < 0.001 |
| Year 3 | n = 1,212 | n = 1,686 | |
| Medical | 12,438 (29,634) | 7,657 (16,994) | < 0.001 |
| Outpatient | 6,619 (17,530) | 4,540 (9,845) | < 0.001 |
| Inpatient | 3,846 (14,272) | 2,110 (8,843) | < 0.001 |
| ED | 1,973 (8,008) | 1,007 (4,242) | < 0.001 |
| Prescription drug | 2,713 (5,305) | 2,278 (6,468) | 0.038 |
| Total | 15,151 (31,096) | 9,935 (19,357) | < 0.001 |
ED = emergency department; SD = standard deviation.
TABLE 4.
Effect of Progression to Type 2 Diabetes on Total Health Care Costs (per Person per Year) for First 3 Years
| Log Coefficient (SE)a (Progression vs. Nonprogression) | Change in %b | P Value | |
|---|---|---|---|
| Year 1 (n = 7,650) | 0.18 (0.03) | +19.7 | < 0.001 |
| Year 2 (n = 4,802) | 0.31 (0.04) | +36.3 | < 0.001 |
| Year 3 (n = 2,898) | 0.39 (0.05) | +47.6 | < 0.001 |
aGeneralized linear models with log link and gamma distribution were performed to assess the association between total health care costs and progression to diabetes, adjusting for age, sex, race, Medicaid plan, and comorbidities (hypertension, obesity, and dyslipidemia).
bThe estimated log coefficients were interpreted as a percent change in costs in patients who progressed to diabetes vs. patients who did not.
SE = standard error.
Discussion
This study identified the demographic and comorbid characteristics associated with progression to diabetes and assessed the effect of progression to type 2 diabetes on health care costs in low-income and Medicaid insured patients with prediabetes. It was found that more than one third of study patients developed type 2 diabetes within 3 years after diagnosis of prediabetes. Age, race, Medicaid plan, and comorbid hypertension, dyslipidemia, and obesity were associated with risk of diabetes progression. Moreover, progression to diabetes increased total health care costs during first 3 years significantly.
The annual incidence of type 2 diabetes is 5%-10% in people with prediabetes in the United States20; however, this study showed that approximately 25% of low-income patients developed type 2 diabetes within 1 year after diagnosis of prediabetes, which is much higher than the general population. This raises a significant concern for health care providers and Medicaid policymakers. The cumulative incidence of type 2 diabetes at 3 years (30.3%) in Medicaid patients with prediabetes was higher than in people with prediabetes who do not change their lifestyle (28.9%), as reported by the Diabetes Prevention Program Research Group.20 Considering low awareness of their condition (11%) in people with prediabetes and the association between type 2 diabetes and socioeconomic position,3,16,17 our results suggest the importance of delivering intervention programs to low-income populations to prevent or delay type 2 diabetes.
Among the risk factors associated with progression to diabetes in this study, patients who had comorbid hypertension, dyslipidemia, or obesity were more likely to develop type 2 diabetes. These results confirmed findings reported by previous studies and suggest that evaluating diabetes-related comorbidities plays an important role in early identification of high-risk patients.13,21 In addition to comorbidities, patients enrolled in Medicaid managed care plans were 22% less likely to develop diabetes than those in a fee-for-service plan for the entire study period. Patients enrolled in a Medicaid managed care plan for the partial study period were also less likely (14%) to develop diabetes. South Carolina Medicaid offers 7 managed care plans that provide diabetes disease management programs and accessible, comprehensive, and family-centered medical care coordination. These benefits are not routinely offered in the traditional fee-for-service Medicaid plan.22,23 Therefore, our results suggest that services available through managed care plans, but not fee-for-service plans, may help reduce the progression to diabetes.
Study results showed that total health care costs increased significantly in patients who progressed to diabetes during the first 3 years. Since outpatient costs accounted for a large proportion of total health costs in this study population, the increased outpatient service use in patients who progressed to diabetes contributed to the significant differences in the medical and total health care costs. Outpatient providers are in a position well suited for prediabetes screening in order to provide the most timely delivery of necessary patient education, especially since only 11% of the people with prediabetes are aware of their condition.3 Outpatient visits are often used to conduct screenings and deliver patient education to prevent the development of diabetes complications and additional related costs.
A previous study indicated that excessive health care utilization in patients with prediabetes was associated with diabetes-related comorbidities such as hypertension; endocrine, metabolic, and renal complications; and general medical conditions.11 Although individuals with diabetes learn their diabetes care from various sources, including licensed medical providers, diabetes education classes, and the internet,24-26 health care providers (e.g., primary care providers and medical specialists) are the most common primary source for individuals to learn how to manage diabetes. This further demonstrates the importance of screening patients with prediabetes, monitoring diabetes development, and delivering patient education during routine outpatient visits for those with prediabetes to potentially delay the development of diabetes and the need for additional costly outpatient visits for the management of diabetes and associated complications.
Economic considerations are important for policymakers, insurers, health care providers, and patients. Once onset of diabetes occurs, total health care costs increase significantly.13 From 2007 to 2012, the total economic costs of diagnosed diabetes increased by 41% in the United States.12 Francis et al. (2011) reported that total adjusted health expenditures (including payer reimbursed amount and patient out-of-pocket payment) increased by 26.7%, 24.2%, and 23.4% for the first 1, 2, and 3 years after progression from prediabetes to type 2 diabetes.13 Our study confirmed the effect of progression to diabetes on total health care costs from the payer’s perspective in the Medicaid population and showed that the differences in total health care costs between the 2 groups became larger gradually during the first 3 years following diagnosis of prediabetes. These findings imply potential cost savings for payers if early detection of prediabetes and intervention to prevent and delay diabetes are implemented for high-risk, low-income patients. Many intervention programs have been developed and have consistently shown that lifestyle changes with or without pharmacological treatment prevent or delay the diabetes onset successfully.27-29 Based on cost-effectiveness of diabetes prevention programs,29-31 the American Diabetes Association (ADA) recommends that such programs be covered by third-party payers.4 In fact, the National Diabetes Prevention Program is covered by Medicare, some private insurance, and Medicaid in some states.32,33
Although lifestyle changes with or without pharmacological treatment have been proven to effectively reduce progression to diabetes, the generalizability of the effect of the intervention programs in low-income populations is still limited.27,28 The long-term cost of lifestyle modification and medication use is still a major issue for low-income patients who have higher incidences of prediabetes and diabetes.16,17 A previous epidemiologic study indicated that many Americans with prediabetes meet ADA criteria for consideration of metformin34; however, a recent study showed that only less than 4% of patients with prediabetes were prescribed metformin to prevent diabetes onset.21 The ADA recommends that patients with prediabetes who are aged younger than 60 years receive metformin t herapy.2 More than 90% of the patients with prediabetes in the described study were younger than 60 years, representing a candidate population to use metformin treatment. Because of the high percentage of progression to diabetes in this study, additional research is needed to examine the metformin use patterns in low-income patients with prediabetes.
Limitations
Findings in this study should be interpreted in light of some limitations. First, ICD-9-CM codes were used to identify patients with prediabetes. It is possible that the conditions of hyperglycemia, impaired glucose tolerance, and impaired fasting glucose were screened by providers and discussed with patients, but the ICD-9-CM codes were not entered into claims thereby resulting in uncaptured data. The lab test information including fasting plasma glucose values, oral glucose tolerance test results, and hemoglobin A1c levels were not available from Medicaid claims, which prevented the use of clinical information to confirm patients with prediabetes. However, use of ICD-9-CM codes to identify patients with prediabetes from private insurance claims data has been performed in previous studies, and 99% of eligible patients had a qualifying ICD-9-CM prediabetes code.13,21 Second, the Medicaid claims data did not provide patient body mass index, family history of diabetes, cholesterol test values, and lifestyle interventions in the study population. These factors associated with prediabetes and progression from prediabetes to diabetes could not be identified and adjusted in multivariate regression models. Thus, the regression estimates could be biased, leading to omitted variable or residual confounding. Finally, the findings in this study were based on patients enrolled in South Carolina Medicaid. Thus, the results may not be generalized to all Medicaid patients with prediabetes in the United States. Additionally, these results cannot be extrapolated to those covered by Medicare or private insurance because of differences in benefits and services offered by the various plans.
Conclusions
The differences in demographic and comorbid characteristics between patients who progressed to diabetes and those who did not may help clinicians better identify patients at high risk for progression to diabetes. Consequently, diabetes prevention strategies may be tailored for low-income populations. Furthermore, understanding characteristics of low-income populations with prediabetes may provide guidance when enrolling patients in a plan most beneficial for their health. Differences in health care costs between patients who progressed to diabetes and those who did not imply an opportunity for primary care providers to enhance screening for prediabetes and diabetes in low-income population, which may ultimately produce cost savings for Medicaid if early interventions are implemented. More evidence is needed to help Medicaid provide affordable intervention programs to low-income insurers to reduce health care expenditures.
ACKNOWLEDGMENTS
The authors thank Heather Kirby and Joe Magagnoli at the South Carolina Revenue and Fiscal Affairs Office for technical assistance with data management.
APPENDIX A. Baseline Characteristics by Diabetes Progression in Medicaid Insured Patients with Prediabetes and Continuous Enrollment ≥ 24 Months
| All Patients with Prediabetes (N = 4,802) | Diabetes Progression (n = 1,767) | No Diabetes Progression (n = 3,035) | P Value | |
|---|---|---|---|---|
| Age (years), mean (SD) | 39.1 (12.4) | 42.7 (11.3) | 37.0 (12.5) | < 0.001 |
| 18-45, % (n) | 65.8 (3,160) | 56.4 (997) | 71.3 (2,136) | < 0.001 |
| 46-64, % (n) | 34.2 (1,642) | 44.6 (770) | 28.7 (872) | |
| Sex, % (n) | ||||
| Female | 77.1 (3,703) | 76.1 (1,345) | 77.7 (2,358) | 0.210 |
| Male | 22.9 (1,099) | 23.8 (422) | 22.3 (677) | |
| Medicaid plan, % (n) | ||||
| Fee for service | 15.1 (726) | 17.3 (306) | 13.8 (420) | 0.004 |
| Managed care | 44.0 (2,113) | 43.3 (765) | 44.4 (1,348) | |
| Both | 40.9 (1,963) | 39.4 (696) | 41.8 (1,267) | |
| Race, % (n) | ||||
| White | 44.4 (2,134) | 41.7 (736) | 46.1 (1,398) | 0.009 |
| African American | 48.0 (2,308) | 50.1 (886) | 46.9 (1,422) | |
| Other | 7.5 (360) | 8.2 (145) | 7.1 (215) | |
| Charlson Comorbidity Index, % (n) | ||||
| 0 | 95.8 (4,600) | 94.3 (1,666) | 96.7 (2,934) | < 0.001 |
| 1 | 1.9 (93) | 3.1 (55) | 1.3 (38) | |
| > 1 | 2.3 (109) | 2.6 (46) | 2.1 (63) | |
| Other comorbid conditions, % (n) | ||||
| Hypertension | 44.0 (2,114) | 57.3 (1,013) | 36.3 (1,101) | < 0.001 |
| Obesity | 17.9 (859) | 23.6 (417) | 14.6 (442) | < 0.001 |
| Dyslipidemia | 27.3 (1,309) | 36.3 (641) | 22.0 (668) | < 0.001 |
SD = standard deviation.
APPENDIX B. Baseline Characteristics by Diabetes Progression in Medicaid Insured Patients with Prediabetes and Continuous Enrollment ≥ 36 Months
| All Patients with Prediabetes (N = 2,898) | Diabetes Progression (n = 1,212) | No Diabetes Progression (n = 1,686) | P Value | |
|---|---|---|---|---|
| Age (years), mean (SD) | 39.4 (12.1) | 42.6 (11.1) | 37.1 (12.3) | < 0.001 |
| 18-45, % (n) | 65.2 (1,890) | 56.4 (683) | 71.6 (1,207) | < 0.001 |
| 46-64, % (n) | 34.8 (1,008) | 43.7 (529) | 28.4 (479) | |
| Sex, % (n) | ||||
| Female | 78.1 (2,263) | 78.0 (945) | 78.2 (1,318) | 0.896 |
| Male | 21.9 (635) | 22.0 (267) | 21.8 (368) | |
| Medicaid plan, % (n) | ||||
| Fee for service | 18.5 (536) | 20.2 (245) | 17.3 (291) | 0.099 |
| Managed care | 40.7 (1,178) | 40.5 (491) | 40.7 (687) | |
| Both | 40.9 (1,184) | 39.3 (476) | 42.0 (708) | |
| Race, % (n) | ||||
| White | 44.7 (1,294) | 42.2 (512) | 46.4 (782) | 0.078 |
| African American | 47.7 (1,382) | 49.5 (600) | 46.4 (782) | |
| Other | 7.7 (222) | 8.3 (100) | 7.2 (122) | |
| Charlson Comorbidity Index, % (n) | ||||
| 0 | 95.7 (2,772) | 94.2 (1,142) | 96.7 (1,630) | < 0.001 |
| 1 | 2.2 (63) | 3.6 (43) | 1.2 (20) | |
| > 1 | 2.2 (63) | 2.2 (27) | 2.1 (36) | |
| Other comorbid conditions, % (n) | ||||
| Hypertension | 45.1 (1,308) | 57.9 (702) | 35.9 (606) | < 0.001 |
| Obesity | 17.9 (519) | 23.7 (287) | 13.7 (232) | < 0.001 |
| Dyslipidemia | 27.9 (807) | 36.8 (446) | 21.4 (361) | < 0.001 |
SD = standard deviation.
REFERENCES
- 1.Centers for Disease Control and Prevention.. National diabetes statistics report, 2014. Estimates of diabetes and its burden in the United States. U.S. Department of Health and Human Services. Atlanta, GA. 2014. Available at http://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. Accessed January 22, 2017. [Google Scholar]
- 2.American Diabetes Association.. 4. Prevention or delay of type 2 diabetes. Diabetes Care. 2016;39(Suppl 1):S36-38. [DOI] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention.. Awareness of prediabetes— United States, 2005-2010. MMWR Morb Mortal Wkly Rep. 2013;62(11):209-12. Available at: https://www.cdc.gov/mmwr/preview/mmwrhtml/mm6211a4.htm. Accessed January 22, 2017. [PMC free article] [PubMed] [Google Scholar]
- 4.American Diabetes Association.. 5. Prevention or delay of type 2 diabetes. Diabetes Care. 2015;38(Suppl 1):S31-32. [DOI] [PubMed] [Google Scholar]
- 5.Tabak AG, Herder C, Rathmann W, Brunner EJ, Kivimäki M.. Prediabetes: a high-risk state for diabetes development. Lancet. 2012;379(9833):2279-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nathan DM, Davidson MB, DeFronzo RA, et al.. Impaired fasting glucose and impaired glucose tolerance implications for care. Diabetes Care. 2007;30(3):753-59. [DOI] [PubMed] [Google Scholar]
- 7.Balkau B, Hu G, Qiao Q, et al.. Prediction of the risk of cardiovascular mortality using a score that includes glucose as a risk factor. The DECODE study. Diabetologia. 2004;47(12):2118-28. [DOI] [PubMed] [Google Scholar]
- 8.Barzilay JI, Spiekerman CF, Wahl PW, et al.. Cardiovascular disease in older adults with glucose disorders: comparison of American Diabetes Association criteria for diabetes mellitus with WHO criteria. Lancet. 1999;354(9179):622-25. [DOI] [PubMed] [Google Scholar]
- 9.Levitan EB, Song Y, Ford ES, Liu S.. Is nondiabetic hyperglycemia a risk factor for cardiovascular disease? A meta-analysis of prospective studies. Arch Intern Med. 2004;164(19):2147-55. [DOI] [PubMed] [Google Scholar]
- 10.American Diabetes Association.. Standards of medical care in diabetes— 2013. Diabetes Care. 2013;36(Suppl 1):S11-66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zhang Y, Dall TM, Chen Y, et al.. Medical cost associated with prediabetes. Popul Health Manag. 2009;12(3):157-63. [DOI] [PubMed] [Google Scholar]
- 12.American Diabetes Association.. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013;36(4):1033-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Francis BH, Song X, Andrews L, et al.. Progression to type 2 diabetes, healthcare utilization, and cost among pre-diabetic patients with or without comorbid hypertension. Curr Med Res Opin. 2011;27(4):809-19. [DOI] [PubMed] [Google Scholar]
- 14.Smith J. Diabetes and the rise of the SES health gradient. NBER Working Paper No. 12905. February 2007. Available at: http://www.nber.org/papers/w12905. Accessed January 22, 2017.
- 15.Díaz-Redondo A, Giráldez-García C, Carrillo L, et al.. Modifiable risk factors associated with prediabetes in men and women: a cross-sectional analysis of the cohort study in primary health care on the evolution of patients with prediabetes (PREDAPS-study). BMC Fam Prac. 2015;16(1):5. Available at: http://bmcfampract.biomedcentral.com/articles/10.1186/s12875-014-0216-3. Accessed January 22, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Agardh E, Allebeck P, Hallqvist J, Moradi T, Sidorchuk A.. Type 2 diabetes incidence and socio-economic position: a systematic review and meta-analysis. Int J Epidemiol. 2011;40(3):804-18. [DOI] [PubMed] [Google Scholar]
- 17.Rabi DM, Edwards AL, Southern DA, et al.. Association of socio-economic status with diabetes prevalence and utilization of diabetes care services. BMC Health Serv Res. 2006;6(1):124. Available at: http://www.bmchealth-servres.biomedcentral.com/articles/10.1186/1472-6963-6-124. Accessed January 22, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.South Carolina eHealth Medicaid Statistics.. Medicaid enrollment. July 3, 2016. Available at: http://www.schealthviz.sc.edu/medicaid-enroll-ment. Accessed January 22, 2017.
- 19.Deyo RA, Cherkin DC, Ciol MA.. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-19. [DOI] [PubMed] [Google Scholar]
- 20.Diabetes Prevention Program Research Group.. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002(346):393-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moin T, Li J, Duru OK, et al.. Metformin prescription for insured adults with prediabetes from 2010 to 2012: a retrospective cohort study. Ann Intern Med. 2015;162(8):542-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.South Carolina Healthy Connections Choices.. Compare health plans. 2014. Available at: https://www.scchoices.com/Member/Step3PBECompare.aspx?frommenu=true. Accessed January 22, 2017.
- 23.National Academy for State Health Policy.. South Carolina - medical homes. January 1, 2014. Available at: http://www.nashp.org/south-caroli-na-422/. Accessed January 22, 2017.
- 24.Wilson V. Patient use of the internet for diabetes information. Nurs Times. 2013;109(23):18-20. [PubMed] [Google Scholar]
- 25.Forkner-Dunn J. Internet-based patient self-care: the next generation of health care delivery. J Med Internet Res. 2003;5(2):e8. Available at: http://www.jmir.org/2003/2/e8/. Accessed January 22, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mensing CR, Norris SL.. Group education in diabetes: effectiveness and implementation. Diabetes Spectr. 2003;16(2):96-103. [Google Scholar]
- 27.Albright AL, Gregg EW.. Preventing type 2 diabetes in communities across the US: the national diabetes prevention program. Am J Prev Med. 2013;44(4 Suppl 4):S346-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bansal N. Prediabetes diagnosis and treatment: a review. World J Diabetes. 2015;6(2):296-303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Shin JA, Lee JH, Kim HS, et al.. Prevention of diabetes: a strategic approach for individual patients. Diabetes Metab Res. 2012;28(Suppl 2):79-84. [DOI] [PubMed] [Google Scholar]
- 30.Diabetes Prevention Program Research Group.. 10-year follow-up of diabetes incidence and weight loss in the diabetes prevention program outcomes study. Lancet. 2009;374(9702):1677-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Diabetes Prevention Program Research Group.. The 10-year cost-effectiveness of lifestyle intervention or metformin for diabetes prevention: an intent-to-treat analysis of the DPP/DPPOS. Diabetes Care. 2012;35(4):723-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.National Association of Chronic Disease Directors.. Preventing type 2 diabetes: health insurance coverage. August 2015. Available at: http://www.chronicdisease.org/?NDPP_insure. Accessed January 22, 2017.
- 33.American Diabetes Association.. Press release. National Diabetes Prevention Program named the first preventive health initiative eligible for Medicare coverage via CMMI expansion. March 23, 2016. Available at: http://www.diabetes.org/newsroom/press-releases/2016/national-dpp-named-first-preventive-health-initiative-eligible-for-medicare.html. Accessed January 22, 2017.
- 34.Rhee MK, Herrick K, Ziemer DC, et al.. Many Americans have pre-diabetes and should be considered for metformin therapy. Diabetes Care. 2010;33(1):49-54. [DOI] [PMC free article] [PubMed] [Google Scholar]


