Abstract
BACKGROUND:
Clinical pharmacy services were initiated at 7 of 11 clinics within a primary care network (PCN), which was designated as a patient-centered medical home and was affiliated with a large academic medical center in October 2014. The goal of the service was to target patients with uncontrolled chronic conditions, specifically diabetes. Patients met with a clinical pharmacist through individual clinic and telephonic appointments, in addition to usual appointments with physicians as needed. While managing patients with diabetes, many clinicians assess a patient’s hemoglobin A1c (A1c), along with blood pressure and cholesterol, as indicators of disease state control and cardiovascular risk. These 3 parameters were combined into a bundled response score (BRS) in order to assess whether the addition of the clinical pharmacy service had a positive effect on patient therapeutic goal attainment rates for these areas.
OBJECTIVES:
To assess the effect of pharmacist-led comprehensive medication management (CMM) on therapeutic goal attainment rates for glycemic, blood pressure, and dyslipidemia outcomes in PCN patients, which was represented by a BRS based on how many therapeutic goals were met.
METHODS:
This retrospective study was conducted using patients seen in clinics within the PCN between October 1, 2014, and October 31, 2015. Patients were included in the intervention group if they were actively managed by a PCN pharmacist and had a diagnosis of diabetes. A control group included patients without access to a PCN pharmacist and was matched to the intervention group by baseline A1c results. Based on current clinical practice guidelines, therapeutic goals for the BRS were set as A1c ≤ 8%, blood pressure ≤ 140/90 mmHg, and prescription of a moderate- to high-intensity statin for dyslipidemia. In addition to the primary outcome, the individual components of the BRS were assessed, as well as the average number of medications used between groups.
RESULTS:
There were 95 patients included in the intervention group, with 132 patients included in the usual care group. Patients in the intervention group had significantly higher rates of therapeutic goal attainment for the 3 endpoints (40% vs. 12%, P < 0.001). The intervention group had statistically significantly higher improvements in the individual areas of A1c, blood pressure, and statin goal attainment. There were no significant differences in the number of medications for diabetes or antihypertensive medications used between groups at the time of study termination.
CONCLUSIONS:
This study demonstrated that the addition of CMM services provided by clinical pharmacists in this PCN had a positive effect on therapeutic goal attainment rates for patients with diabetes. This finding suggests that the integration of clinical pharmacists into primary care clinics could have positive effects on the clinical outcomes of diabetic patients in glycemic control, blood pressure, and statin treatment, in accordance with current guidelines.
What is already known about this subject
The integration of pharmacists in primary care settings can have positive effects on patient outcomes relating to chronic disease state control.
Interventions by pharmacists in a variety of settings can have positive effects on patient outcomes related to diabetes, including improvements in hemoglobin A1c (A1c), blood pressure, and cholesterol management.
What this study adds
Comprehensive medication management services provided by clinical pharmacists in the primary care setting have a positive effect on patients with diabetes, based on a composite of the 3 most common clinical monitoring parameters of A1c, blood pressure, and statin treatment, in accordance with current guidelines.
Pharmacist interventions can help achieve better disease state control without significantly increasing the number of prescribed medications.
Pharmacist interventions in the primary care setting have been shown to have a positive effect on health outcomes.1-4 Study results from the primary literature has shown that the involvement of pharmacists in direct patient care can have additional average hemoglobin A1c (A1c) reductions of 0.88%-1.8%, average systolic blood pressure reductions of 5.7-7.8 mmHg, and average low-density lipoprotein (LDL) reductions of 6.3 mg/dL-18.7 mg/dL, compared with standard care.1-2
In managing patients with diabetes, many clinicians assess a patient’s A1c, blood pressure, and cholesterol as indicators of disease state control and cardiovascular risk. A report published using 2007-2010 data from the National Health and Nutrition Examination Surveys reported that 52.5% of patients achieved a target A1c of < 7.0%; 51.1% achieved a target BP of < 130/80 mmHg; and 56.2% achieved a target LDL of < 100 mg/dL.5 Another study from a managed care organization reported goal attainment rates of 37% for A1c, 41% for BP, and 23% for LDL.6
No study to date has evaluated interventions affecting the attainment of these 3 measures in individual patients with diabetes. The most recent publication of the 2013 ACC/AHA cholesterol treatment guidelines no longer includes a target LDL; instead, it recommends that patients with diabetes be prescribed a moderate- to high-intensity statin for the management of cholesterol.7 There have only been a few published studies that have addressed the prescribing rates of these recommended statins in patients with diabetes. One study reported 33% prescribing adherence to the 2013 ACC/AHA cholesterol guidelines, while another study reported that 40% of patients with diabetes have been appropriately prescribed a moderate- to high-intensity statin.8,9
The goal of this study was to evaluate the effect of clinical pharmacy services on therapeutic goal attainment for patients with diabetes, hypertension, and dyslipidemia, compared with usual care without a clinical pharmacist, as measured by post-intervention goal attainment rates.
Methods
Pilot Program and Study Design
Because of the established benefit of integrating pharmacists into the care team within the primary care setting, clinical pharmacy services were implemented at 7 of 11 clinics within a primary care network (PCN) affiliated with a large academic medical center in October 2014. These 7 clinics were selected based on geographical location and workload feasibility for 2 clinical pharmacists. The pilot program was designed to target ambulatory patients with 1 or more uncontrolled chronic conditions, such as diabetes, hypertension, or dyslipidemia, as well as medication management issues that included polypharmacy, medication access difficulties, or poor disease state or medication understanding. The goal of the clinical pharmacy service was to improve chronic disease state and medication management. The 2 clinical pharmacists provided comprehensive medication management (CMM) services, with the pharmacists assigned to their own clinics without overlap.
This single-center matched retrospective chart review evaluated outcomes of therapeutic goal attainment rates in patients who had type 2 diabetes and were managed at a PCN clinic between October 1, 2014 and October 31, 2015. Patients were stratified into 1 of 2 comparator groups based on the care they received: an intervention group that was managed by a pharmacist or a usual care group without pharmacist involvement. This study was approved by the UC Davis Institutional Review Board after expedited review.
Patient Population
The UC Davis PCN has been designated by the National Committee for Quality Assurance (NCQA) as a patient-centered medical home (PCMH). All patients included in the usual care group were identified by pulling data from the PCMH registry developed as part of the NCQA designation. The registry was built using an active list of UC Davis PCN patients who had primary care providers assigned to them and had been seen within the last 18 months. Patients with diabetes were included in the registry if they had an International Classification of Diseases, Ninth/Tenth Revision, Clinical Modification diagnosis for diabetes on their active problem list in the electronic medical record.
Patients were included in the analysis if they were aged 18 years or older, were included in the PCMH diabetes registry, were managed at a PCN clinic within the study period, and were engaged with the health care service. For the intervention group, engagement was defined as having 2 or more in-clinic pharmacy visits or 1 in-clinic pharmacy visit with at least 1 follow-up telephone encounter from a pharmacist at any time within the 13-month study period.
Because the pilot program started in October 2014, patients in the intervention group were all naive to pharmacist services in this institution. For the usual care group, engagement was defined as having at least 2 primary care provider (PCP) office visits (PCP encounters were primarily done in-clinic and not as telephone encounters) at any time within the 13-month study period. Patients were excluded from this study if they were prisoners, pregnant, or had inadequate laboratory data, which was defined as not having an A1c level drawn within 60 days before the initial clinic visit or not having an A1c level drawn within 90 days after the last clinic encounter.
Study Procedure
Patients in the intervention group were identified for the pharmacy service by 2 methods: (1) through a PCP referral for chronic disease state management, medication access assistance, or polypharmacy or (2) through the PCMH diabetes registry. The PCN pharmacy team screened the registry to identify patients who might benefit from the pharmacy service and scheduled an initial 40-minute in-clinic visit with a clinical pharmacist. At the initial clinic visit, the pharmacist performed CMM. The pharmacist services performed in the PCMH match the qualities outlined in the 2012 resource guide published by the Patient-Centered Primary Care Collaborative (PCPCC).10 Using the PCPCC approach, pharmacists performed medication reconciliation, educated the patient regarding medications and disease state, and used a collaborative practice agreement (CPA) to optimize medication regimens. The CPA allowed the pharmacist to order labs, order new medications, stop unnecessary medications, and titrate the dose of existing medications. The CPAs for diabetes, hypertension, and dyslipidemia were approved by the UC Davis Pharmacy and Therapeutics Committee. After initial CMM was performed, follow-up was then arranged as additional in-clinic visits or by telephone to ensure that initial recommendations were effective and to continually reassess for medication optimization.
Patients in the usual care group were identified retrospectively from the PCMH diabetes registry with the same parameters used for the intervention group, but for patients in the 4 PCN clinics without a pharmacist. Patients were randomly selected by a study investigator who was not part of the PCN or PCMH pilot. This investigator used a random computerized selection to match patients from the diabetes registry for inclusion in the usual care sample. This process ensured that both samples had a similar distribution of baseline A1c values. Age, gender, blood pressure, and statin medications were not considered when randomly selecting patients.
In the intervention group, patients were classified into 3 subgroups based on their baseline A1c: ≤ 8%, 8.1%-10%, and > 10%. The percentages of patients within each A1c subgroup in the intervention group were used to decide the number of patients included in the finalized usual care sample to ensure a similar distribution of baseline A1c values between the 2 groups. All patients eligible for inclusion in the usual care group were then classified into the same 3 baseline A1c subgroups (≤ 8%, 8.1%-10%, and > 10%.) Based on the percentage breakdown of subgroups in the intervention group, patients in the usual care group were then proportionately randomly selected to be distributed into the finalized usual care group to ensure that both groups were proportionately matched in all 3 A1c subgroups.
Study Outcomes
The primary objective of this study was the effect of clinical pharmacy services on achieving goal attainment rates for defined glycemic, blood pressure, and dyslipidemia parameters. To measure this effect, a bundled response score (BRS) was developed to rate these parameters from 0 to 3, in order to represent how many disease state goals (diabetes, hypertension, and moderate- to high-intensity statin prescribed) were achieved. Each patient was given a BRS at baseline and after the last encounter during the study period. The BRS was used to assess the effect of pharmacist-led interventions on the composite of therapeutic goal attainment rates for patients with diabetes. The primary outcome of this study was the comparison of the BRS between the intervention group and usual care group after the last encounter during the study period.
The 3 clinical goals within the BRS were set as A1c ≤ 8%, blood pressure ≤ 140/90 mmHg, and prescription of a moderate- to high-intensity dosed statin.7 A score of 0 indicated no disease goals were attained; a score of 1 indicated that 1 disease goal was attained; a score of 2 indicated that 2 disease state goals were attained; and a score of 3 indicated that all 3 goals were achieved. The goals were set with consideration of current clinical guidelines.7,11-13 The most recent blood pressure, A1c, and statin prescribed before the initial visit were used to determine goal attainment at baseline (within 60 days of initial visit).
Secondary outcomes included individual goal attainment rates for the 3 BRS components, BRS pre/post changes for individual patients within each group, changes in A1c, changes in blood pressure, and the number of antidiabetic and antihypertensive medications used in each treatment group.
Statistical Analysis
For all statistical analyses, a P value of 0.05 was considered significant. Baseline comparison between groups regarding proportion of gender and goal attainment rates for A1c, statin prescription, and blood pressure were assessed using the chi-square test. Baseline BRS group comparisons, pre/post differences of BRS scores, A1c, statin prescription, and blood pressure attainment rates for each group were assessed using McNemar’s test. Logistic regressions were used to test for treatment effects on postintervention goal attainment rates for A1c, blood pressure, and statin prescription, controlling for baseline values. The number of antidiabetic and antihypertensive medications used, blood pressure reductions, A1c reductions, and average age were analyzed by t-tests. Differences in post-treatment values for the BRS, A1c, blood pressure, and statin prescription were analyzed using Fisher’s exact test.
Results
Baseline Results for Patient Population
Of the 222 patients seen by a PCN pharmacist during the study period, 127 patients were excluded because of no diabetes diagnosis or inadequate laboratory data, which left 95 patients in the intervention group. Of these 95 patients, 23% (n = 22), 39% (n = 37), and 38% (n = 36) were classified into the baseline A1c subgroups of ≤ 8%, 8.1%-10%, and > 10%, respectively. Searching the PCMH diabetes registry from clinics without a pharmacist resulted in 589 patients, with 181 excluded because of inadequate laboratory data, which left 408 patients who met the inclusion criteria. Of these 408 patients, only 50 patients had a baseline A1c of > 10%. Because this A1c subgroup was the rate-limiting group, these 50 patients were set to represent 38% of the total usual care group in order to match the intervention group. This process led to 132 patients who were proportionately randomly selected within the A1c subgroups to be included in the final usual care group, which was the maximum amount of patients that could be included in order for the usual care group to be matched to the baseline A1c subgroups of the intervention group (Figure 1).
FIGURE 1.
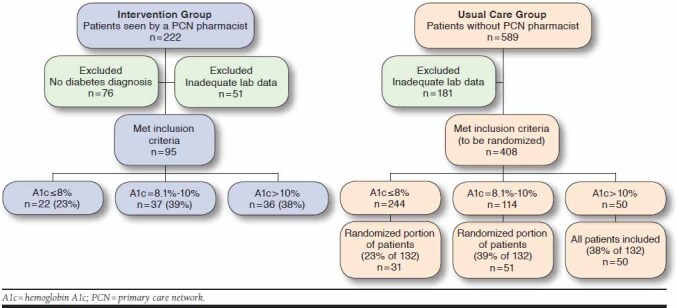
Random Selection of Patient Population
The average baseline A1c in both groups was 9.6%, and the percentage of patients with a baseline A1c at goal was 23% in both groups (P = 1.00; Table 1). In addition, the groups were found to have no statistically significant differences in any of the 3 components of the primary outcome at baseline, including the percentages of patients who had controlled blood pressure (63% vs. 73%, P = 0.10) and were already prescribed a moderate- to high-intensity statin (71% vs. 60%, P = 0.10). There were also no statistically significant differences in average age, although there were significantly more women in the intervention group. There were no significant differences between groups regarding baseline BRS (P = 0.65).
TABLE 1.
Baseline Characteristics
| Characteristics | Intervention Group n = 95 | Usual Care Group n = 132 | P Value |
|---|---|---|---|
| Average age | 62.4 | 63.6 | 0.44 a |
| Male, % | 41 | 57 | 0.02b |
| Average A1c, % | 9.6 | 9.6 | 0.96a |
| At A1c goal, n (%) | 22 (23) | 31 (23) | 1.00b |
| Number of antidiabetic medications | 2.1 | 2.1 | 0.82a |
| Average systolic blood pressure | 135.1 mmHg | 132.8 mmHg | 0.32a |
| Average diastolic blood pressure | 75.5 mmHg | 74.4 mmHg | 0.41a |
| At blood pressure goal, n (%) | 60 (63) | 97 (73) | 0.10b |
| Number of antihypertensive medications | 1.9 | 2.1 | 0.19a |
| Prescribed moderate- or high-intensity statin, n (%) | 67 (71) | 79 (60) | 0.10b |
| BRS, n (%) | 0.65c | ||
| 0 of 3 | 9 (9.5) | 9 (7) | |
| 1 of 3 | 45 (47) | 65 (49) | |
| 2 of 3 | 32 (34) | 50 (38) | |
| 3 of 3 | 9 (9.5) | 8 (6) |
aT-test.
bChi-square test.
cMcNemars test.
A1c = hemoglobin A1c; BRS = bundled response score.
Primary Outcome: Bundled Response Score
After intervention, there was a significant difference between the 2 groups regarding the BRS, with higher scores in the intervention group compared with the usual care group (P< 0.001; Figure 2). The percentage of patients with a BRS of 3 increased in both groups (40% of the intervention group and 12% of the usual care group). The percentage of patients with a BRS of 0 decreased in both groups (2% of the intervention group compared with 6% of the usual care group). A comprehensive breakdown of postintervention BRS is represented in Figure 2, which shows percentages of patients with a BRS of 0, 1, 2, and 3 in each group. This figure shows that a significantly higher percentage of patients in the intervention group achieved a higher BRS and thus had higher rates of therapeutic goal attainment.
FIGURE 2.
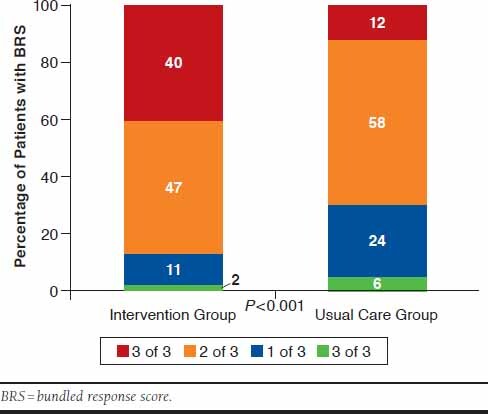
Primary Outcome: Postintervention BRS
Secondary Outcomes
Individual Disease State Goal Attainment Rates and BRS Changes.
Regarding the secondary outcome of the individual BRS components, the intervention group had significant increases from baseline in the percentage of patients achieving individual goal attainment for A1c (23% vs. 54%, P < 0.0001), blood pressure (64% vs. 93%, P =0.0001), and moderate- to high-intensity statin prescription (71% vs. 79%, P = 0.20). In the usual care group, there was also a significant increase from baseline in the percentage of patients achieving A1c goals (23% vs. 36%, P = 0.005), but no significant change was found in the blood pressure (73% vs. 77%, P = 0.640) or moderate- to high-intensity statin goal attainment (60% vs. 63%, P = 0.390). In comparing the postintervention goal attainment rates, the intervention group had a statistically significantly higher goal attainment rate for A1c (54% vs. 36%, P = 0.010), blood pressure (93% vs. 77%, P = 0.001), and statin prescription (79% vs. 63%, P = 0.010), after accounting for baseline goal attainment rates between groups (Figure 3).
FIGURE 3.
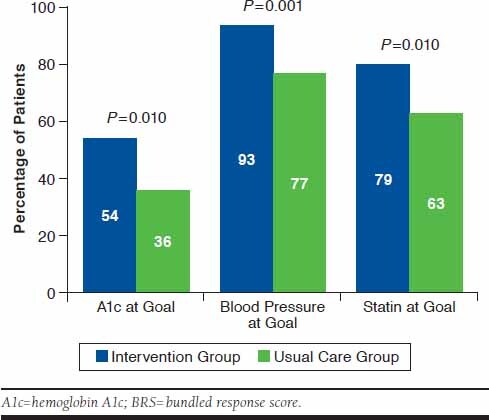
Secondary Outcomes: Postintervention Individual Components of the BRS
Changes in the BRS among the individual patients in this study showed that the majority of patients (53.7%) in the intervention group had some improvement or increase in their baseline BRS, while the majority of patients in the usual care group (53.8%) had no change in their BRS from baseline. Also, only 2.1% of patients in the intervention group had a decrease in their BRS, compared with 14.4% of patients in the usual care group.
Hemoglobin A1c and Blood Pressure Reductions.
The intervention group had an average A1c reduction of 1.4%, compared with an average reduction of 0.8% in the usual care group (P = 0.010; Table 2). In an exploratory analysis of the patient subset in each group who had an uncontrolled baseline A1c (> 8%), the intervention group had a net average A1c reduction of 2.0%, compared with an average reduction of 1.2% in the usual care group (P = 0.002). Despite the larger reduction in the intervention group, there were no significant differences found in the number of antidiabetic medications prescribed between groups at the time of the last clinic encounter during the study period (2.3 vs. 2.3, P = 0.930).
TABLE 2.
A1c and Blood Pressure T-test Results
| Intervention Group | Usual Care Group | P Value | |
|---|---|---|---|
| Change in average A1c for all patients, % | -1.4 | -0.8 | 0.010 |
| Change in average A1c for subgroup of patients with uncontrolled baseline A1c, % | -2.0 | -1.2 | 0.002 |
| Number of antidiabetic medications postintervention | 2.3 | 2.3 | 0.930 |
| Change in average systolic blood pressure | -7.4 mmHg | -1.7 mmHg | 0.030 |
| Change in average diastolic blood | -2.4 mmHg | -1.0 mmHg | 0.310 |
| Number of antihypertensive medications postintervention | 1.9 | 2.2 | 0.120 |
A1c = hemoglobin A1c.
Although there was a significantly higher percentage of patients who achieved blood pressure goals in the intervention group compared with the usual care group, there was only a statistically significant difference in average systolic blood pressure reduction (-7.4 mmHg vs. -1.7 mmHg, P = 0.030) and no statistically significant difference in the average diastolic blood pressure reduction (-2.4 mmHg vs. -1.0 mmHg, P = 0.310). There was also no significant difference in the number of antihypertensive medications prescribed between groups at the time of the last clinic encounter during the study period (1.9 vs. 2.2, P = 0.120).
Discussion
This retrospective study assessed clinical outcomes in patients with diabetes, with and without management by a PCN clinical pharmacist. Although the BRS concept is a unique outcome to measure, the components of the bundle are assessed by a majority of health care providers in primary care clinics. The 3 components of the bundle are commonly referred to as “the ABCs of diabetes,” since A1c, blood pressure, and cholesterol are the 3 main areas of concern for patients with diabetes.14
Given the clinical importance of these 3 areas, the BRS was determined to be the primary outcome for this study instead of glycemic control alone. Although current clinical practice guidelines were followed when setting the goals for the BRS, it is important to note that the A1c goal was set as ≤ 8%, since patients managed by the pharmacy service were typically more complex patients with multiple comorbidities. In addition, the 10-year atherosclerotic cardiovascular disease (ASCVD) risk estimator was not used to assess specific statin recommendations based on the 2013 ACC/AHA cholesterol guidelines. Instead, patients were considered at goal if they received a moderate- to high-intensity statin. Patient histories of ASCVD, lipid panel values, liver function, and allergies/intolerances were not assessed in this study, which is a limitation since these factors are considered when determining the appropriateness of initiating statin therapy.
In this study, it was found that 40% of patients in the pharmacist group achieved all 3 clinical goals after intervention, compared with only 12% of patients in the usual care group, which indicates that pharmacist-driven CMM had a positive effect on A1c, blood pressure, and statin prescription goal attainment in patients with diabetes based on current clinical guideline recommendations.
Two other studies published in 2013 assessed goal attainment rates of patients with diabetes but used the previous guideline recommendation targets of A1c < 7%, blood pressure < 130/80 mmHg, and LDL < 100 mg/dL.3,5 One of the studies from 2007-2010 reported that 18.8% of patients had achieved all 3 clinical goals but did not assess the types of medical interventions done for these patients, including whether there was pharmacist invovlement.5 Our study yielded higher goal attainment rates, but it is difficult to compare these findings without knowing the types of medical care the patients from the other study experienced and whether the goals used were different. The second study looked at patients who were managed in an interdisciplinary team that included a pharmacist and reported that 36.7% of patients seen had achieved all 3 clinical goals.3
The clinical goals used in these studies are different than those used in our study because of the publication of newer clinical practice guidelines that changed these goals. Although different clinical goals were targeted, these results were consistent with our findings, which adds support to the finding that the addition of a pharmacist to the interdisciplinary team can have a positive effect on goal attainment rates for this patient population.
The level of additional A1c reduction found in this study was comparable to the findings reported in a meta-analysis, which showed that the addition of a pharmacist in direct patient care had a mean additional A1c reduction of 0.88%.1 It has been demonstrated that a 1% reduction in A1c is associated with a risk reduction of 37% for microvascular complications.15
Although there was no significant difference in the diastolic blood pressure reductions between groups, there was a significantly greater reduction in systolic blood pressure and a significantly higher percentage of patients reaching their blood pressure goals in the intervention group. The nonsignificant diastolic blood pressure reduction finding may be attributable to fluctuations in blood pressure levels within the targeted goal range (i.e., increasing from 120/80 mmHg to 130/84 mmHg), which would affect the net blood pressure reduction but would not affect whether a patient is at his or her blood pressure goal.
With no significant difference in the number of medications prescribed between the 2 groups, the pharmacy service was able to achieve better outcomes without increasing the number of medications that could negatively affect adherence. Although the pharmacists followed the PCPCC approach to CMM, specific interventions made were not tracked, which may be seen as a limitation to this study. In addition, cost of medications between groups was not assessed. Although specific interventions were not tracked, it can be concluded that the interventions made did not always involve the addition of another medication based on the results of the number of medications used. Instead, interventions such as dose adjustments, medication replacements, and motivational interviewing were made by the pharmacists to achieve these improved outcomes. Future studies could track specific interventions within CMM, to identify if any specific type of intervention has a greater effect on patient outcomes.
Limitations
Although the intervention and usual care groups were only matched with regard to baseline A1c, the 2 groups were comparable in many regards. Having no statistically significant differences in baseline A1c, blood pressure, moderate- to high-intensity statin prescription, and age, the patient population of both groups appeared evenly matched. However, there are still potential confounders that were not assessed, such as difference in gender, potential differences in ethnicity, socioeconomic status, education and health literacy rates, since the clinics assessed are located in 2 counties.
Despite using the same PCMH diabetes registry for both groups, the intervention group also included patients who were referred by a PCP. It is possible that these patients may have been more engaged and proactive than those chosen from the outreach lists. In addition, patients who were referred by PCPs may have had difficulties with medication access or adherence—problems that are commonly addressed by pharmacists—which could have affected our results. Two different clinical pharmacists managed the intervention group, and patients in both groups had access to different PCPs, which could have also confounded the results. The groups were matched using only baseline A1c because of the smaller sample size that was available, since this study was a retrospective study based on a pilot service. Future studies could explore alternate matching processes, such as multiple matching points or propensity score matching.
Conclusions
The addition of a pharmacist to usual care in primary care clinics positively affected the achievement of higher A1c rates, blood pressure improvements, and the prescription of moderate- to high-intensity statins in patients with diabetes. It has been shown that clinical pharmacists have a positive effect on patient outcomes in primary care, so they should be integrated as valuable members of interdisciplinary primary care teams.
REFERENCES
- 1.Chisholm-Burns MA, Lee JK, Spivey CA, et al.. U.S. pharmacists’ effect as team members on patient care: systematic review and meta-analysis. Med Care. 2010;48(10):923-33. [DOI] [PubMed] [Google Scholar]
- 2.Tan ECK, Stewart K, Elliott RA, George J. Pharmacist services provided in general practice clinics: a systematic review and meta-analysis. Res Social Adm Pharm. 2014;10(4):608-22. [DOI] [PubMed] [Google Scholar]
- 3.Ip EJ, Shah BM, Yu J, Chan J, Nguyen LT, Bhatt DC. Enhancing diabetes care by adding a pharmacist to the primary care team. Am J Health Syst Pharm. 2013;70(10):877-86. [DOI] [PubMed] [Google Scholar]
- 4.Jacobs M, Sherry PS, Taylor LM, Amato M, Tataronis GR, Cushing G. Pharmacist Assisted Medication Program Enhancing the Regulation of Diabetes (PAMPERED) study. J Am Pharm Assoc (2003). 2012;52(5):613-21. [DOI] [PubMed] [Google Scholar]
- 5.Casagrande SS, Fradkin JE, Saydah SH, Rust KF, Cowie CC. The prevalence of meeting A1c, blood pressure, and LDL goals among people with diabetes, 1988-2010. Diabetes Care. 2013;36(8):2271-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Beaton SJ, Nag SS, Gunter MJ, Gleeson JM, Sajjan SS, Alexander CM. Adequacy of glycemic, lipid, and blood pressure management for patients with diabetes in a managed care setting. Diabetes Care. 2004;27(3):694-98. [DOI] [PubMed] [Google Scholar]
- 7.Stone NJ, Robinson JG, Lichtenstein AH, et al.. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guideline. Circulation. 2014;129 (25 Suppl 2):S1-S45. [DOI] [PubMed] [Google Scholar]
- 8.Hinds A, Lopez D, Rascati K, Jokerst J, Srinivasa M. Adherence to the 2013 blood cholesterol guidelines in patients with diabetes at a PCMH: comparison of physician only and combination physician/pharmacist visits. Diabetes Educ. 2016;42(2):228-33. [DOI] [PubMed] [Google Scholar]
- 9.Tran JN, Kao TC, Caglar T, et al.. Impact of the 2013 cholesterol guideline on patterns of lipid-lowering treatment in patients with atherosclerotic cardiovascular disease or diabetes after 1 year. J Manag Care Spec Pharm. 2016;22(8):901-08. Available at: https://www.jmcp.org/doi/10.18553/jmcp.2016.22.8.901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Nace DK, Grundy P, Nielsen M, et al.. The patient-centered medical home: integrating comprehensive medication management to optimize patient outcomes. Resource guide. Patient-Centered Primary Care Collaborative. June 2012. Available at: https://www.accp.com/docs/positions/misc/CMM%20Resource%20Guide.pdf. Accessed March 26, 2018.
- 11.American Diabetes Association . Standards of medical care in diabetes – 2016. Diabetes Care. 2016;39(Suppl 1):S4-S109. [PubMed] [Google Scholar]
- 12.American Association of Clinical Endocrinologists and American College of Endocrinology . Comprehensive type 2 diabetes management. Endocr Pract. 2016;22(1):84-13. [DOI] [PubMed] [Google Scholar]
- 13.James A, Oparil S, Carter BL, et al.. 2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311(5):507-20. [DOI] [PubMed] [Google Scholar]
- 14.National Institute of Diabetes and Digestive and Kidney Diseases . Managing diabetes. Available at: https://www.niddk.nih.gov/health-information/health-communication-programs/ndep/living-with-diabetes/know-your-abcs/pages/knowyourabcs.aspx. Accessed March 26, 2018.
- 15.Stratton IM, Adler AI, Neil HAW, et al.. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405-12. [DOI] [PMC free article] [PubMed] [Google Scholar]


