Abstract
BACKGROUND:
The 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults emphasizes evidence-based treatment with moderate- to high-dose statins for patients at high risk for atherosclerotic cardiovascular disease (ASCVD). Whether this new guideline influenced patterns of treatment 1 year after its dissemination is unknown.
OBJECTIVE:
To compare patterns of lipid-lowering treatment before and 1 year after the release of the 2013 cholesterol guideline in 2 high-risk groups: patients with ASCVD and patients with diabetes mellitus.
METHODS:
Using pharmacy and medical claims from a large U.S. health insurance organization, 610,535 patients with ASCVD (n = 301,440) or diabetes mellitus (n = 309,095) were identified, and statin treatment rates and statin intensity were examined before and 1 year after the dissemination of the 2013 cholesterol guideline. A standardized difference of at least 10% was required to declare the effect size meaningful.
RESULTS:
Overall, there was no change in statin treatment rates for patients with ASCVD (48.0% before guideline vs. 47.3% after, standardized difference 1.4%) or diabetes (50% vs. 51.5% after, standardized difference 2.4%). Statin initiation rates among patients not on statins before the 2013 guideline were 10.1% in patients with ASCVD and 14.3% in patients with diabetes, but these gains were offset by 13.0% and 12.2% statin discontinuation rates among ASCVD and diabetes patients, respectively. Among patients taking statins 1 year after the guideline was issued, 80% of patients with ASCVD and aged ≤ 75 years were not on guideline-recommended high-intensity statin therapy, whereas most patients with ASCVD and aged > 75 years or patients with diabetes were on moderate- or high-intensity statin treatment.
CONCLUSIONS:
One year after dissemination of the 2013 cholesterol guideline, overall treatment rates with statins among patients with ASCVD and diabetes did not change appreciably, and many patients remained either untreated or undertreated.
What is already known about this subject
Clinical trials have shown that fixed doses of high-intensity statin therapy result in a more effective risk reduction in cardiovascular morbidity and mortality among primary and secondary prevention patients.
Despite efficacy trials showing superiority of intensive over conventional statin dosing, high-risk patients have been shown to be undertreated.
The 2013 American College of Cardiology and the American Heart Association cholesterol guideline recommends the use of moderate- to high-intensity statin therapy for all eligible patients at high risk for atherosclerotic cardiovascular disease (ASCVD) events.
What this study adds
This retrospective cohort study examined the impact of the 2013 cholesterol guideline on changes to statin treatment in high-risk patients.
Nearly half of patients with ASCVD and diabetes mellitus remain untreated with statin medications even at 1 year after publication of the 2013 cholesterol guideline.
Although there were modest improvements in rates of appropriate statin dosing 1 year after the 2013 guideline, statin intensification remained suboptimal, and many high-risk patients continued to be undertreated or not treated with statin therapy.
In 2013, the American College of Cardiology (ACC) and the American Heart Association (AHA) released a new guideline for cholesterol treatment.1,2 The 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults was a paradigm shift from the treat-to-target approach of low-density lipoprotein (LDL) levels of less than 70 mg per dL to a targeted treatment approach of moderate- to high-intensity statin therapy for all eligible patients at high risk for having an atherosclerotic cardiovascular disease (ASCVD) event. This shift in recommended treatment was based on a preponderance of clinical trial evidence showing that fixed doses of high-intensity statin therapy resulted in a constant relative risk reduction in cardiovascular morbidity and mortality among primary and secondary prevention patients and that the number needed to treat was inversely related to the underlying risk of the patients.3-7 Moreover, no randomized trials of a treat-to-LDL target strategy had yet been performed,8 and data supporting additional nonstatin therapy to lower LDL levels were inconsistent.9-12
A major impetus for the 2013 cholesterol guideline was documented undertreatment with effective statin therapy among patients with established ASCVD, with only 23% of acute coronary syndrome and 38% of myocardial infarction patients treated with high-intensity statins,13,14 despite efficacy trials showing superiority of intensive dosing over conventional statin dosing.3-6 However, it remains unknown if the changed cholesterol guideline affected treatment patterns in real-world practice. Little to no increase in rates of statin treatment or appropriate statin dosing would suggest that the 2013 guideline did not significantly affect care, and many patients at high risk for ASCVD have remained untreated or undertreated. Accordingly, the purpose of this study was to compare patterns of lipid-lowering treatment before and 1 year after the release of the 2013 cholesterol guideline in 2 high-risk groups: patients with ASCVD and patients with diabetes mellitus. Also, rates of statin treatment and appropriate statin dosing intensity were examined to determine if they had increased and whether use of nonstatin treatments had decreased.
Methods
Data Source and Study Population
Medical and prescription claims data were derived from OptumRx, one of the largest pharmacy benefit management companies in the United States, covering over 30 million people. Although the 2013 cholesterol guideline provided recommendations for 4 distinct patient groups, this study focused on patients with ASCVD and diabetes.1,2 Patients were categorized with a secondary prevention indication if they had an International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis or procedural code any time between May 13, 2011, and May 12, 2013, for acute coronary syndrome, myocardial infarction, unstable angina, percutaneous coronary intervention, coronary artery bypass surgery, carotid revascularization with either a stent or endarterectomy, stroke, transient ischemic attack, peripheral artery disease, or peripheral bypass surgery (Appendix A, available in online article). For patients without ASCVD, a cohort with diabetes was defined for patients that had an ICD-9-CM diagnosis code or medication treatment specific for diabetes. This cohort was restricted to patients aged between 40 and 75 years to be consistent with the recommendations for this target population in the 2013 cholesterol guideline. Patients with diabetes and ASCVD were classified as ASCVD patients.
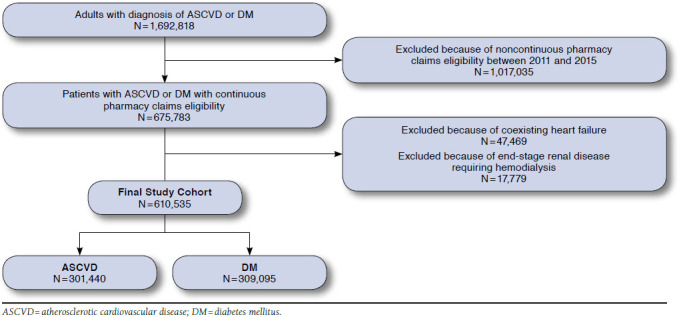
We identified 1,692,818 patients aged 18 years or older with ASCVD or aged between 40 and 75 years with diabetes based on pharmacy or medical claims codes. For this study, 1,017,035 patients were excluded who did not have continuous pharmacy claims eligibility throughout the entire study period of May 13, 2011-February 12, 2015. The rationale for this approximately 4-year period of uninterrupted pharmacy claims participation was to (a) document patterns of lipid-lowering treatment in the 6 months before the release of the 2013 cholesterol guideline (May 13, 2013-November 11, 2013); (b) ensure that study patients had at least 2 years of pharmacy claims before this period (May 13, 2011-May 12, 2013) to document their ASCVD and diabetes diagnoses and ensure stability of the cohort; and (c) reassess patterns of lipid-lowering treatment 9-15 months after the release of the 2013 cholesterol guideline (August 13, 2014-February 12, 2015).
Next, 47,469 patients with an ICD-9-CM diagnosis code for heart failure and 17,779 patients with a diagnosis or procedural code for end-stage renal failure requiring hemodialysis at any time during the 4-year study period were excluded (Appendix B, available in online article), since previous clinical trials with statins in these 2 populations have not shown benefit, and the 2013 cholesterol guideline made no recommendations for their treatment.15-18 The final study population, therefore, comprised 610,535 patients with ASCVD or diabetes.
Outcomes
The primary objective for this study was to compare the proportion of patients in each cohort treated with statins before and 1 year after release of the 2013 cholesterol guideline, with a particular focus on the intensity of statin therapy, specifically for moderate- or high-intensity statin treatment. Lipid-lowering therapy and intensity of statin therapy were measured using prescription fills during the preguideline period (May 13, 2013-November 11, 2013) and postguideline period (August 13, 2014-February 12, 2015).
Among those treated with statins, appropriate statin dosing was defined based on the 2013 cholesterol guideline.1,2 For patients with established ASCVD, an appropriate statin dose was defined as a high-dose statin in patients aged ≤ 75 years and a statin of at least moderate intensity in patients aged > 75 years. For patients with diabetes aged between 40 and 75 years, an appropriate statin dose was defined as a statin of at least moderate intensity. A patient’s age was determined based on the latest age at the end of the preguideline period, and patients were categorized into different age groups based on their ages during this period. Definitions of what constituted low-, moderate-, and high-dose statins were derived from the 2013 cholesterol guideline.1 In order to capture the actual statin daily dose in patients who may be on multiple strengths of the same statin medication, the patients’ average daily dose during the last 30 days of the preguideline or postguideline period was used to determine the statin dose intensity. Additionally, if patients had multiple statins and were on different statin intensities, they were categorized as using the higher intensity statin. As a secondary outcome, the use of the following nonstatin lipid-lowering therapies were examined before and 1 year after release of the 2013 guideline: bile acid binding resins, ezetimibe, fibrates, and niacin.
Statistical Analyses
Baseline characteristics of the ASCVD and diabetes cohorts were described using summary statistics. These included demographics, comorbid conditions, and the Charlson Comorbidity Index (CCI).
Overall treatment rates with statin and nonstatin medications in both patient groups were then examined before and 1 year after the 2013 cholesterol guideline. Because of the large sample size, standardized differences were used for the comparisons, with a significant increase or decrease in rates defined by a standardized difference (std. diff.) of greater than 10%.19 For both cohorts, each patient was grouped before the guideline into 1 of 4 lipid-lowering categories: statin only, nonstatin only, both statin and nonstatin, and no treatment, and their lipid-lowering category was compared 1 year after the guideline was issued to examine transitions in therapy, including discontinuation and de novo initiation of statins.
Next, rates of appropriate statin intensity were examined for the ASCVD and diabetes patients (as previously described) before and after the 2013 guideline. Appropriate statin intensity for ASCVD patients were reported separately for those aged ≤ 75 years and those aged > 75 years. For these analyses, patients were excluded who had discontinuation of statin therapy by 1 year to focus on those patients who remained on statins. Finally, to test the robustness of the findings, a sensitivity analysis was conducted wherein all analyses were repeated and examined as to whether statin usage patterns were different if ASCVD patients were restricted to only those patients with revascularization procedure codes for previous coronary artery bypass, percutaneous coronary intervention, carotid revascularization, peripheral bypass surgery, or other revascularization procedures (See Appendix A for ICD-9-CM procedure codes used).
All analyses were conducted using SAS version 9.2 (SAS Institute, Cary, NC). This study was approved by an external institutional review board (Ethical and Independent Review Services 14116-01).
Results
Of the 610,535 patients identified, 301,440 (49.4%) were secondary prevention patients with ASCVD, and 309,095 (50.6%) were primary prevention patients with diabetes. Table 1 summarizes characteristics of the ASCVD and diabetes cohorts. Patients with ASCVD had a mean age (standard deviation [SD]) of 70.8 (SD ±13.2); 55.5% were female; and the mean CCI was 4.4 (SD ± 2.6). Approximately 14.3% had a history of myocardial infarction; 6.8% had a history of unstable angina; 41.0% had known coronary artery disease; and 17.7% had a history of revascularization. In addition, 64.4% had a history of stroke, and 43.1% had peripheral vascular disease. More than one third had coexisting diabetes, and 77.2% had accompanying hypertensive disease. In contrast, the primary prevention diabetes cohort was younger, with a mean age of 62.8 (SD ± 9.2), and 53.3% were women. One quarter had documented complications with their diabetes, and 72.7% had hypertension. In both cohorts, less than 7% had diagnoses for mild liver disease and less than 0.5% had moderate liver disease. Dementia was uncommon, and chronic renal disease was prevalent in 16.6% of the ASCVD cohort and 10.2% of the diabetes cohort.
TABLE 1.
Baseline Characteristics of the ASCVD and Diabetes Cohorts
| ASCVD (n = 301,440) | DM (n = 309,095) | |
|---|---|---|
| Age, mean [± SD] | 70.8 [±13.2] | 62.8 [±9.2] |
| ≤ 75 years | 183,316 (60.8) | N/A |
| > 75 years | 118,124 (39.2) | N/A |
| Female | 167,253 (55.5) | 164,814 (53.3) |
| Charlson Comorbidity Index, mean [±SD] | 4.4 [±2.6] | 3.4 [±2.1] |
| Coronary artery disease | 123,492 (41.0) | N/A |
| Myocardial infarction | 42,941 (14.3) | N/A |
| History of unstable angina | 20,579 (6.8) | N/A |
| Previous revascularization | 53293 (17.7) | N/A |
| Peripheral vascular disease | 129,772 (43.1) | N/A |
| Stroke | 194,198 (64.4) | N/A |
| Transient ischemic attack | 38,011 (12.6) | N/A |
| Dementia | 16,502 (5.5) | 1,715 (0.6) |
| Chronic pulmonary disease | 80,533 (26.7) | 55,230 (17.9) |
| Liver disease | ||
| Mild | 19,439 (6.5) | 21,355 (6.9) |
| Moderate or severe | 1,208 (0.4) | 1,277 (0.4) |
| Diabetes | 109,127 (36.2) | 309,095 (100.0) |
| Diabetes with complications | 45,484 (15.1) | 75,853 (24.5) |
| Hypertension | 232,800 (77.2) | 224,740 (72.7) |
| Chronic renal disease | 49,886 (16.6) | 31,390 (10.2) |
Note: Values are represented as number (%) unless noted otherwise.
ASCVD = atherosclerotic cardiovascular disease; DM = diabetes mellitus; N/A = not applicable; SD = standard deviation.
Use of Statins and Nonstatin Medications
Table 2 summarizes aggregate use of lipid-lowering therapies before and 1 year after the 2013 cholesterol guideline. Rates of statin treatment did not change 1 year after introduction of the guideline for patients with ASCVD (48.0% before vs. 47.3% after, std. diff. = 1.4%) or diabetes (50.3% before vs. 51.5% after, std. diff. = 2.4%). Similarly, use of bile acid binding agents, ezetimibe, fibrates, and niacin did not change. Moreover, the proportion of patients taking statins only, nonstatins only, both a nonstatin and a statin, or no lipid-lowering therapy did not change before and 1 year after the guideline for either cohort (Table 2).
TABLE 2.
Aggregate Lipid-Lowering Treatment Rates Before and 1 Year After 2013 Cholesterol Guideline
| ASCVD (n = 301,440) | DM (n = 309,095) | ||||||||
| Preguideline | Postguideline | Std. Diff. (%)a | Preguideline | Postguideline | Std. Diff. (%)a | ||||
| Cholesterol-lowering agents | |||||||||
| Any statin | 144,754 (48.0) | 142,517 (47.3) | 1.4 | 155,338 (50.3) | 159,195 (51.5) | 2.4 | |||
| Low intensity | 29,489 (20.4) | 27,392 (19.2) | - | 34,112 (22.0) | 32,687 (20.5) | - | |||
| Moderate intensity | 93,022 (64.3) | 89,808 (63.0) | - | 102,047 (65.7) | 102,576 (64.4) | - | |||
| High intensity | 22,243 (15.4) | 25,317 (17.8) | - | 19,179 (12.3) | 23,932 (15.0) | - | |||
| Bile acid binding resins | 2,426 (0.8) | 2,238 (0.7) | 1.2 | 2,833 (0.9) | 2,599 (0.8) | 1.1 | |||
| Ezetimibe | 6,851 (2.3) | 6,074 (2.0) | 2.1 | 6,712 (2.2) | 6,010 (1.9) | 2.1 | |||
| Fibrates | 11,606 (3.9) | 10,812 (3.6) | 1.6 | 19,928 (6.4) | 18,892 (6.1) | 1.2 | |||
| Niacin | 3,082 (1.0) | 1,887 (0.6) | 4.5 | 3,127 (1.0) | 2,062 (0.7) | 3.3 | |||
| No lipid treatment | 149,086 (49.5) | 152,010 (50.4) | 1.8 | 142,251 (46.0) | 139,730 (45.2) | 1.6 | |||
| Treatment regimens | |||||||||
| Statin | 128,561 (42.6) | 128,379 (42.6) | 0.1 | 134,561 (43.5) | 139,791 (45.2) | 3.4 | |||
| Nonstatin | 7,600 (2.5) | 6,913 (2.3) | 1.3 | 11,506 (3.7) | 10,170 (3.3) | 2.2 | |||
| Statin and nonstatin | 16,193 (5.4) | 14,138 (4.7) | 3.2 | 20,777 (6.7) | 19,404 (6.3) | 1.6 | |||
| No lipid treatment | 149,086 (49.5) | 152,010 (50.4) | 1.8 | 142,251 (46.0) | 139,730 (45.2) | 1.6 | |||
Note: Values are represented as number (%) unless noted otherwise.
a A standardized difference of >10% was considered a significant imbalance between proportions.
ASCVD = atherosclerotic cardiovascular disease; DM = diabetes mellitus; Std. Diff. = standardized difference.
Further examination revealed that, although aggregate rates of statin treatment did not change significantly, there were modest transitions in therapy at the patient level (Table 3). For patients with ASCVD, 13.2% of patients on statins and 11.2% of patients on both statins and nonstatins before the guideline were not on any statin during the postguideline period and were considered to have discontinued their statin treatments (total discontinuation of 13.0% of ASCVD cohort on statins before the guideline). This was counterbalanced by the fact that 18.6% of patients on only nonstatins and 10.1% of patients with no treatment before the 2013 guideline were started on statins by 1 year after the guideline (total new statin initiation rate of 10.5% of ASCVD cohort not on statins before the guideline; Table 3). A similar finding was found in the diabetes cohort, in which 12.2% of the diabetes cohort on statins before the guideline were not on any statin during the postguideline period and were considered to have discontinued their statin treatments, while 14.9% of the diabetes cohort not on statins before the guideline began statin therapy 1 year after the guideline.
TABLE 3.
Patient-Level Transitions in Lipid-Lowering Therapy Before and After 2013 Cholesterol Guideline
| Postguideline | Postguideline | Statin | Statin | ||||
| No Change | To Statin | To Nonstatin | To Both | No Treatment | Discontinuationa | Initiationb | |
| ASCVD (n = 301,440) | |||||||
| Statin | 109,751 (85.4) | - | 490 (0.4) | 1,872 (1.5) | 16,448 (12.8) | 16,938 (13.2) | - |
| Nonstatin | 4,439 (58.4) | 638 (8.4) | - | 774 (10.2) | 1,749 (23.0) | - | 1,412 (18.6) |
| Statin and nonstatin | 10,913 (67.4) | 3,470 (21.4) | 715 (4.4) | - | 1,095 (6.8) | 1,810 (11.2) | - |
| No treatment | 132,718 (89.0) | 14,520 (9.7) | 1,269 (0.9) | 579 (0.4) | - | - | 15,099 (10.1) |
| Total: 18,748 (6.2) | Total: 16,511 (5.5) | ||||||
| DM (n = 309,095) | |||||||
| Statin | 115,251 (85.7) | - | 616 (0.5) | 2,573 (1.9) | 16,121 (12.0) | 16,737 (12.4) | - |
| Nonstatin | 6,679 (58.1) | 1,063 (9.2) | - | 1,432 (12.5) | 2,332 (20.3) | - | 2,495 (21.7) |
| Statin and nonstatin | 14,522 (69.9) | 3,973 (19.1) | 960 (4.6) | - | 1,322 (6.4) | 2,282 (11.0) | - |
| No treatment | 119,955 (84.3) | 19,504 (13.7) | 1,915 (1.4) | 877 (0.6) | - | - | 20,381 (14.3) |
| Total: 19,019 (6.2) | Total: 22,876 (7.4) | ||||||
Note: Values are represented as number (%) unless noted otherwise.
a Based on sum of patients transitioning to either nonstatins or no treatment at 1 year.
b Based on sum of patients transitioning to either statins only or both statins and nonstatins at 1 year.
ASCVD = atherosclerotic cardiovascular disease; DM = diabetes mellitus.
Intensification of Statin Therapy
Of the 142,517 patients with ASCVD who were on statin therapy 1 year after the 2013 cholesterol guideline, 61.4% were aged 75 years or younger. In this age group, there was a significant increase in the proportion of patients on high-dose statins postguideline (15.6% before vs. 20.4% 1 year after the guideline; std. diff. = 12.5%; Table 4). This increase was because of 7,207 patients who transitioned to high-dose statin treatment from either low- or moderate-intensity statins or who were untreated before the guideline, offset by 2,990 high-dose patients who moved to a lower-dose statin (Table 5). However, in previously untreated patients who were newly initiating statin therapy in this group, only 16.6% were started on a high-intensity statin (Table 5). Among 54,998 patients with ASCVD who were aged > 75 years and who were on a statin at 1 year, there was also a significant increase in the proportion of patients on recommended moderate- or high-intensity statins after the guideline (69.5% before vs. 77.6% after 1 year; std. diff. = 18.4%; Table 4). This increase was because of 7,492 patients who transitioned to at least moderate-dose statins from low-intensity statins or who were untreated before the guideline, offset by 3,045 moderate- and high-dose patients who moved to low-intensity statins (Table 5). In previously untreated patients newly initiating statin therapy in this group, 75.1% were started on a moderate-to high-intensity statin (Table 5).
TABLE 4.
Statin Dose Intensity Before and After 2013 Cholesterol Guidelinea
| Preguideline | Postguideline | Change | Std. Diff. (%)b | |
| ASCVD, ≥75 years (n = 87,519) | ||||
| None | 11,010 (12.6) | N/A | N/A | N/A |
| Low | 13,932 (15.9) | 15,090 (17.2) | 1,158 (1.3) | 3.5 |
| Moderate | 48,943 (55.9) | 54,578 (62.4) | 5,635 (6.4) | 13.3 |
| High | 13,634 (15.6) | 17,851 (20.4) | 4,217 (4.8) | 12.5 |
| ASCVD, > 75 years (n = 54,998) | ||||
| None | 5,501 (10.0) | N/A | N/A | N/A |
| Low | 11,248 (20.5) | 12,302 (22.4) | 1,054 (1.9) | 4.6 |
| Moderate | 32,210 (58.6) | 35,230 (64.1) | 3,020 (5.5) | 11.3 |
| High | 6,039 (11.0) | 7,466 (13.6) | 1,427 (2.6) | 7.9 |
| Moderate or high | 38,249 (69.5) | 42,696 (77.6) | 4,447 (8.1) | 18.4 |
| DM (n = 159,195) | ||||
| None | 22,876 (14.4) | N/A | N/A | N/A |
| Low | 29,451 (18.5) | 32,687 (20.5) | 3,236 (2.0) | 5.0 |
| Moderate | 89,877 (56.5) | 102,576 (64.4) | 12,699 (8.0) | 16.2 |
| High | 16,991 (10.7) | 23,932 (15.0) | 6,941 (4.4) | 12.9 |
| Moderate or high | 106,868 (67.1) | 126,508 (79.5) | 19,640 (12.3) | 28.3 |
Note: Values are represented as number (%) unless noted otherwise.
a Rates are aggregate rates and are restricted to only those patients who were on statin therapy 1 year after the 2013 cholesterol guideline.
b A standardized difference of >10% was considered a significant imbalance between proportions.
ASCVD = atherosclerotic cardiovascular disease; DM = diabetes mellitus; N/A = not applicable; Std. Diff. = standardized difference.
TABLE 5.
Patient-Level Intensification of Statin Therapy Before and After Cholesterol Guidelinea
| Statin Intensity Preguideline | Statin Intensity Postguideline | Change to Guideline Dose | Change to Nonguideline Dose | |||
| Low | Moderate | High | ||||
| ASCVD, ≤ 75 years | No statin | 2,470 (22.4) | 6,715 (61.0) | 1,825 (16.6) | 1,825 (16.6) | 2,990 |
| Low | 8,519 (61.2) | 5,011 (36.0) | 402 (2.9) | 402 (2.9) | ||
| Moderate | 3,982 (8.1) | 39,981 (81.7) | 4,980 (10.2) | 4,980 (10.2) | ||
| High | 119 (0.9) | 2,871 (21.1) | 10,644 (78.1) | 7,207 | ||
| ASCVD, > 75 years | No statin | 1,371 (24.9) | 3,409 (62.0) | 721 (13.1) | 4,130 (75.1) | 3,045 |
| Low | 7,886 (70.1) | 3,196 (28.4) | 166 (1.5) | 3,362 (29.9) | ||
| Moderate | 2,979 (9.3) | 27,243 (84.6) | 1,988 (6.2) | 7,492 | ||
| High | 66 (1.1) | 1,382 (22.9) | 4,591 (76.0) | |||
| Diabetes mellitus | No statin | 5,651 (24.7) | 14,289 (62.5) | 2,936 (12.8) | 17,225 (75.3) | 8,346 |
| Low | 18,690 (63.5) | 10,063 (34.2) | 698 (2.4) | 10,761 (36.5) | ||
| Moderate | 8,159 (9.1) | 74,398 (82.8) | 7,320 (8.1) | 27,986 | ||
| High | 187 (1.1) | 3,826 (22.5) | 12,978 (76.4) | |||
Note: Values are represented as number (%) unless noted otherwise.
a Rates are for only those patients who were on statin therapy 1 year after the 2013 cholesterol guideline.
ASCVD = atherosclerotic cardiovascular disease.
In sensitivity analyses, when the ASCVD cohort was restricted to 53,467 patients with documented procedure codes for revascularization, results were similar to those of the main ASCVD study cohort. Approximately 55% of ASCVD patients were on statin therapy after the guideline was released, compared with 56% before the guideline. For patients who were aged ≤ 75 years, only 22.3% were on high-intensity statins after the guideline, which was similar to the pattern seen in the main ASCVD cohort. Similarly, in patients aged > 75 years, 80.7% were on at least a moderate-intensity statin.
Finally, among 159,195 diabetes patients on statins 1 year after the guideline, there was a significant increase from 67.1% before the guideline to 79.5% after the guideline (std. diff. = 28.3%; Table 4) of more patients treated with a moderate- or high-intensity statin dose at 1 year. This was because of 27,986 patients who transitioned to at least moderate-dose statins from low-intensity statins or who were untreated before the guideline, offset by 8,346 moderate- and high-dose patients who moved to low-intensity statins (Table 5). In patients newly initiating statin therapy in this group, 75.3% were started on a moderate- to high-intensity statin.
Discussion
This study examined whether the 2013 ACC/AHA cholesterol guideline changed the cholesterol management of patients already at the highest risk of an ASCVD event—patients with clinical ASCVD or with diabetes and between the ages of 40 and 75 years. Using patients who were diagnosed before the guideline release, we found that 1 year after release of the guideline, overall rates of evidence-based statin treatment for these patients had not changed appreciably, with treatment rates before and after the guideline at approximately 50% for both cohorts. Patient-level data did reveal that 11% of ASCVD patients and 15% of diabetes patients who were not on statins before the 2013 cholesterol guideline were taking one at 1 year, suggesting modest improvements in initiation of statin treatment. However, overall rates of patients treated with statins did not change in the year after release of the guideline because of similar numbers of patients discontinuing statin therapy in the ASCVD and diabetes cohorts, which neutralized gains in statin initiation.
Initiating statin treatment and adequate dosing of statin treatment are priorities in the 2013 guideline. For patients with ASCVD who were aged > 75 years or with diabetes, the results were only partially encouraging. Although more than 75% of these patients on statins after the guideline were on guideline-recommended dose intensity, only about 50% of both cohorts were taking statins 1 year after the guideline, which suggests that the majority of patients remained either untreated or undertreated. Among patients with ASCVD who were aged ≤ 75 years, only 1 in 5 patients on statins after the guideline were taking recommended high-intensity statins, which represents approximately 10% of all patients in this group (since only half of this group were treated with statins at 1 year). In addition, only 17% of previously untreated patients who were newly initiated on statin therapy in this group were actually started on a high-intensity statin despite being a “new start,” as recommended by the 2013 guideline. However, the rates of patients who were newly initiating various statin intensities before the release of the guideline were not examined to determine whether this was a departure from previous rates. The findings in this younger ASCVD group is particularly concerning, since they represent the highest risk group with the most to gain. Although the 2013 cholesterol guideline represented an enormous opportunity to maximize the benefit of treatment with optimally dosed statin therapy, this finding suggests that, at 1 year after dissemination, there was room for improvement.
Previous studies have documented that physicians do not routinely intensify evidence-based treatments in the outpatient setting, while initiation of a high-dose statin during a hospitalization is associated with 8-fold odds that a patient is on a high-dose statin during follow-up.14,20 Given the inertia to intensify therapies during routine outpatient care and the modest changes in statin treatment rates and appropriate statin dosing intensities 1 year after the 2013 cholesterol guideline, there is a critical need to develop more detailed performance measures that integrate dosing intensity so that high-risk patients are adequately treated with statins.
Limitations
This study should be interpreted in the context of the following limitations. First, although data from a large pharmacy benefit management organization were used, the results may not be generalizable to other patients, especially those that do not stay enrolled in the same health plan for more than 4 years and those without insurance for whom we expect statin treatment rates to be even lower.
Second, in contrast to previous studies that reported rates of statin use of more than 75%, this study found a statin use rate of approximately 50% among ASCVD patients. This difference is a result of the examination of actual statin prescription fill and use of a broader definition of cardiovascular disease as outlined by the 2013 cholesterol guideline to additionally encompass cerebrovascular and peripheral vascular disease. Additionally, the main study cohort used a single medical or pharmacy claim to define patients with ASCVD or diabetes, which could potentially include patients who may not truly have established ASCVD or diabetes. To address this limitation, a sensitivity analysis was conducted, and it was found that the results were similar to when the ASCVD cohort was restricted to only those patients with a procedure code for a revascularization procedure.
Third, because of the medical claims data lag in the database, information was unavailable for patients’ adverse events during the postguideline period, so details could not be provided regarding reasons for statin discontinuation or what proportion of patients who remained untreated with statins had true statin intolerance. Therefore, we were unable to distinguish between statin intolerance, physician discontinuation because of LDL levels < 70, patient preference, or inability to afford medications. However, accurate documentation of statin myalgias as a diagnosis code or an adverse event is often incomplete. Regardless, it is unlikely that half of all ASCVD and diabetes patients have statin intolerance, which further underscores the study findings of missed opportunities for statin treatment in these high-risk groups.
Fourth, we were not able to determine if patients purchased their statin therapies out-of-pocket, since this information was not captured in the pharmacy claims. Fifth, 2 of the 4 groups highlighted in the 2013 cholesterol guideline were not assessed, since information was not collected on LDL values. Even if these values were available, however, it would have been difficult to define a primary hyperlipidemia cohort with LDL > 190, since LDL levels before initiation of any lipid-lowering therapy in chronically treated patients are difficult to obtain, and the cardiovascular risk calculator remains controversial for the primary prevention group, with a 10-year risk of > 7.5% for cardiovascular events.22 Additionally, there was a 3% change to a lower intensity statin after the 2013 guideline was released in patients with ASCVD and aged ≤ 75 years. It is possible that some of these patients may have been older patients who turned 76 years of age after the guideline was released; however, it was found that only 0.3% of this group actually turned 76 years of age during the evaluated year, and they did not change their statin usage patterns.
Finally, providers may be reluctant to change prescribing patterns for patients currently being treated. Because of limited medical claims availability during the postguideline period, newly diagnosed patients after the guideline was released and whether newly diagnosed patients were treated with guideline-recommended statin doses were not examined.
Conclusions
One year after dissemination of the 2013 cholesterol guideline, we found that overall treatment rates with statins among patients with ASCVD and diabetes did not change appreciably. A modest percentage of previously untreated patients were started on statins in the year after the release of the guideline, but these gains were offset by a similar number of patients discontinuing statin treatment. Moreover, for patients with ASCVD who were aged ≤ 75 years, who were previously untreated, and who were started on statin therapy, less than 20% were started on recommended doses. Additionally, there were only small to modest gains in titrating statin medications to recommended dose intensities, and many patients taking statins remained inadequately treated, including 4 in 5 patients who were aged ≤ 75 years with ASCVD. This study shows that the uptake of new guidelines by the medical community is slow, and future studies should be conducted to examine a longer follow-up period. In order for the 2013 cholesterol guideline to realize its full potential, renewed efforts are needed to further improve statin treatment rates and optimize statin dosing.
APPENDIX A. Diagnosis and Procedure Codes Used in Study
| Descriptiona | Code Type | Code |
| Unstable angina (intermediate coronary syndrome) | ICD-9-CM diagnosis | 411.1 |
| Myocardial infarction | ICD-9-CM diagnosis | 410.xx, 412 |
| Cerebrovascular disease (stroke) | ICD-9-CM diagnosis | 430.x-438.x |
| Percutaneous coronary intervention (PCI) | ICD-9-CM procedure | 36.09, 00.66 |
| Coronary artery bypass (CABG) | ICD-9-CM procedure | 36.10, 36.11, 36.12, 36.13, 36.14, 36.15, 36.16, 36.17, 36.19, 36.20 |
| Carotid revascularization | ICD-9-CM procedure | 36.2, 36.3, 36.31, 36.32, 36.33, 36.34, 36.39 |
| Transient ischemic attack (TIA) | ICD-9-CM diagnosis | 435, 435.8, 435.9 |
| Peripheral artery and vascular disease (PAD/PVD) | ICD-9-CM diagnosis | 443.89, 443.9 |
| Perphieral bypass surgery | ICD-9-CM procedure | 39.2, 39.50, 00.55, 00.63, 36.06, 39.90 |
| Revascularization procedure | CPT | 33140, 33141, 33510-33519, 33521-33523, 33533-33536, 37220-37235, 92920-92944, 92973, 92980-92984, 92995-92996 |
| Revascularization procedure | HCPCS | S2205, S2206, S2207, S2208, S2209 |
| Diabetes | ICD-9-CM diagnosis | 250.xx |
| End-stage renal disease (ESRD)/chronic kidney disease stage V/dialysis (18 yrs+) | ICD-9-CM diagnosis | 403.01, 403.11, 403.91, 404.02, 404.03, 404.12, 404.13, 404.92, 404.93, 585.5, 585.6, v45.1, v45.11, v45.12 |
| End-stage renal disease (ESRD)/chronic kidney disease stage V/dialysis (18 yrs+) | ICD-9-CM procedure | 38.95, 39.27, 39.42, 39.43, 39.53, 39.95, 54.98, |
| End-stage renal disease (ESRD)/chronic kidney disease stage V/dialysis (18 yrs+) | CPT | 36147, 36148, 36800, 36810, 36815, 36831-36833, 36838, 90935, 90937, 90940, 90945, 90947, 90957-90962, 90965, 90966, 90969, 90970, 90989, 90993, 90997, 90999, 99512 |
| End-stage renal disease (ESRD)/chronic kidney disease stage V/dialysis (18 yrs+) | HCPCS | G0257, S9339 |
| Heart failure | ICD-9-CM diagnosis | 428.xx, 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 398.91, 425.4x–425.9x |
a Coronary artery disease/atherosclerosis diagnoses were not included (ICD-9-CM 414.0x, 414, 414.2, 414.3, 414.4, 414.8, 414.9, 440.xx).
CPT = Current Procedural Terminology; HCPCS = Healthcare Common Procedure Coding System; ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification.
APPENDIX B. Derivation of the Study Cohort
References
- 1.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guideline. Circulation. 2014;129(25 Suppl 2):S1-45. [DOI] [PubMed] [Google Scholar]
- 2.Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guideline. J Am Coll Cardiol. 2014;63(25 Pt B):2889-934. [DOI] [PubMed] [Google Scholar]
- 3.Cannon CP, Braunwald E, McCabe CH, et al. Intensive versus moderate lipid lowering with statins after acute coronary syndromes. N Engl J Med. 2004;350(15):1495-504. [DOI] [PubMed] [Google Scholar]
- 4.de Lemos JA, Blazing MA, Wiviott SD, et al. Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: phase Z of the A to Z trial. JAMA. 2004;292(11):1307-16. [DOI] [PubMed] [Google Scholar]
- 5.LaRosa JC, Grundy SM, Waters DD, et al. Intensive lipid lowering with atorvastatin in patients with stable coronary disease. N Engl J Med. 2005;352(14):1425-35. [DOI] [PubMed] [Google Scholar]
- 6.Pedersen TR, Faergeman O, Kastelein JJ, et al. High-dose atorvastatin vs usual-dose simvastatin for secondary prevention after myocardial infarction: the IDEAL study: a randomized controlled trial. JAMA. 2005;294(19):2437-45. [DOI] [PubMed] [Google Scholar]
- 7.Hayward RA, Krumholz HM, Zulman DM, Timbie JW, Vijan S.. Optimizing statin treatment for primary prevention of coronary artery disease. Ann Intern Med. 2010;152(2):69-77. [DOI] [PubMed] [Google Scholar]
- 8.Hayward RA, Hofer TP, Vijan S.. Narrative review: lack of evidence for recommended low-density lipoprotein treatment targets: a solvable problem. Ann Intern Med. 2006;145(7):520-30. [DOI] [PubMed] [Google Scholar]
- 9.Landray MJ, Haynes R, Hopewell JC, et al. Effects of extended-release niacin with laropiprant in high-risk patients. N Engl J Med. 2014;371(3):203-12. [DOI] [PubMed] [Google Scholar]
- 10.Boden WE, Probstfield JL, Anderson T, et al. Niacin in patients with low HDL cholesterol levels receiving intensive statin therapy. N Engl J Med. 2011;365(24):2255-67. [DOI] [PubMed] [Google Scholar]
- 11.Rauch B, Schiele R, Schneider S, et al. OMEGA, a randomized, placebo-controlled trial to test the effect of highly purified omega-3 fatty acids on top of modern guideline-adjusted therapy after myocardial infarction. Circulation. 2010;122(21):2152-59. [DOI] [PubMed] [Google Scholar]
- 12.Ginsberg HN, Elam MB, Lovato LC, et al. Effects of combination lipid therapy in type 2 diabetes mellitus. N Engl J Med. 2010;362(17):1563-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Javed U, Deedwania PC, Bhatt DL, et al. Use of intensive lipid-lowering therapy in patients hospitalized with acute coronary syndrome: an analysis of 65,396 hospitalizations from 344 hospitals participating in Get With The Guideline (GWTG). Am Heart J. 2011;161(2):418-24. [DOI] [PubMed] [Google Scholar]
- 14.Arnold SV, Kosiborod M, Tang F, et al. Patterns of statin initiation, intensification, and maximization among patients hospitalized with an acute myocardial infarction. Circulation. 2014;129(12):1303-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fellstrom BC, Jardine AG, Schmieder RE, et al. Rosuvastatin and cardiovascular events in patients undergoing hemodialysis. N Engl J Med. 2009;360(14):1395-407. [DOI] [PubMed] [Google Scholar]
- 16.Kjekshus J, Apetrei E, Barrios V, et al. Rosuvastatin in older patients with systolic heart failure. N Engl J Med. 2007;357(22):2248-61. [DOI] [PubMed] [Google Scholar]
- 17.Tavazzi L, Maggioni AP, Marchioli R, et al. Effect of rosuvastatin in patients with chronic heart failure (the GISSI-HF trial): a randomised, double-blind, placebo-controlled trial. Lancet. 2008;372(9645):1231-39. [DOI] [PubMed] [Google Scholar]
- 18.Wanner C, Krane V, Marz W, et al. Atorvastatin in patients with type 2 diabetes mellitus undergoing hemodialysis. N Engl J Med. 2005;353(3):238-48. [DOI] [PubMed] [Google Scholar]
- 19.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38(6):1228-34. [Google Scholar]
- 20.Arnold SV, Spertus JA, Masoudi FA, et al. Beyond medication prescription as performance measures: optimal secondary prevention medication dosing after acute myocardial infarction. J Am Coll Cardiol. 2013;62(19):1791-801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ehrmann DA. Polycystic ovary syndrome. N Eng J Med. 2005;352(12):1223-36. [DOI] [PubMed] [Google Scholar]
- 22.Cook NR, Ridker PM.. Further insight into the cardiovascular risk calculator: the roles of statins, revascularizations, and underascertainment in the Women’s Health Study. JAMA Intern Med. 2014;174(12):1964-71. [DOI] [PMC free article] [PubMed] [Google Scholar]


