Abstract
BACKGROUND:
Prescription opioid abuse is associated with substantial economic burden, with estimates of incremental annual per-patient health care costs of diagnosed opioid abuse exceeding $10,000 in prior literature. A subset of patients diagnosed with opioid abuse has disproportionately high health care costs, but little is known about the characteristics of these patients.
OBJECTIVE:
To describe the characteristics of a subset of patients diagnosed with opioid abuse with disproportionately high health care costs to assist physicians and managed care organizations in targeting interventions at the costliest patients.
METHODS:
This retrospective claims data analysis identified patients aged 12 to 64 years diagnosed with opioid abuse/dependence in the OptumHealth Reporting and Insights medical and pharmacy claims database, Quarter 1 (Q1) 1999-Q1 2012. Inclusion criteria required that patients had a diagnosis of opioid abuse during or after Q1 2006, no prior diagnoses of opioid abuse, and continuous non-HMO coverage over an 18-month study period. The study period comprised a 12-month observation period centered on the date of the first opioid abuse diagnosis (index date) and a 6-month baseline period immediately preceding the observation period. Patients in the top 20% of total health care costs in the observation period were classified as “high-cost patients,” and the remaining patients were classified as “lower-cost patients.” Patient characteristics, comorbidities, health care resource use, and health care costs were compared between high-cost patients and lower-cost patients using chi-square tests for dichotomous variables and Wilcoxon rank-sum tests for continuous variables. In addition, multivariate regression was used to assess the relationship between patient characteristics in the baseline period and total health care costs in the observation period among all patients diagnosed with opioid abuse.
RESULTS:
9,291 patients diagnosed with opioid abuse met the inclusion criteria. The 20% of patients classified as high-cost patients accounted for approximately two thirds of the total health care costs of patients diagnosed with opioid abuse. Compared with lower-cost patients, high-cost patients were older (42.5 vs. 36.1; P < 0.001) and more likely to be female (55.9% vs. 42.9%; P < 0.001). They had a higher comorbidity burden at baseline, as reflected in the Charlson Comorbidity Index (0.8 vs. 0.2; P < 0.001), and rates of conditions such as chronic pulmonary disease (12.9% vs. 5.6%; P < 0.001) and mild/moderate diabetes (8.4% vs. 3.4%; P < 0.001). High-cost patients also had higher rates of nonopioid substance abuse diagnoses (12.4% vs. 8.9%; P < 0.001) and psychotic disorders (26.5% vs. 13.6%; P < 0.001). In the observation period, high-cost patients continued to have higher rates of nonopioid substance abuse diagnoses (53.0% vs. 47.2%; P < 0.001) and psychotic disorders (67.1% vs. 47.5%; P < 0.001). In addition, they had greater medical resource use across all places of service (i.e., inpatient, emergency department, outpatient, drug/alcohol rehabilitation facility, and other) compared with lower-cost patients. The mean observation period health care costs of high-cost patients was $89,177 compared with $11,653 for lower-cost patients (P < 0.001). High-cost patients had higher medical costs linked to claims with an opioid abuse diagnosis in absolute terms, but the share of total medical costs attributed to such claims was lower among high-cost patients than among lower-cost patients. While many baseline characteristics were found to have a statistically significant (P < 0.05) association with observation period health care costs, only 27.3% of the variation in observation period health care costs was explained by patient characteristics in the baseline period.
CONCLUSIONS:
This study found that the costliest patients diagnosed with opioid abuse had high rates of preexisting and concurrent chronic comorbidities and mental health conditions, suggesting potential indicators for targeted intervention and a need for greater awareness and screening of comorbid conditions. Opioid abuse may exacerbate existing conditions and make it difficult for patients to adhere to treatment plans for those underlying conditions. Baseline patient characteristics explained only a small share of the variation in observation period health care costs, however. Future research should explore the degree to which other factors not captured in administrative claims data (e.g., severity of abuse) can explain the wide variation in health care costs among opioid abusers.
What is already known about this subject
Prescription opioid abuse is associated with substantial health and economic burden in the United States.
The prevalence of diagnosed opioid abuse increased from 6.7 per 10,000 in 2006 to 18.6 per 10,000 in 2011 in a commercially insured population.
Existing evidence suggests that patients diagnosed with opioid abuse incur higher health care resource use and costs than patients not diagnosed with opioid abuse.
What this study adds
The 20% of patients with the highest costs accounted for approximately two thirds of the total health care costs of patients diagnosed with opioid abuse.
High-cost patients had higher rates of chronic comorbidities and mental health conditions than did lower-cost patients, highlighting the need to consider the complete medical and psychosocial history of a patient when managing underlying conditions that contribute to higher health care costs.
Much of the variation in health care costs cannot be attributed to comorbidities, however.
The abuse of prescription opioids is a major public health problem in the United States. The 2012 National Survey on Drug Use and Health (NSDUH) reported that an estimated 2.1 million Americans aged 12 years and older (or 0.8% of that population) had prescription pain reliever dependence or abuse.1 Rates of diagnosed opioid abuse/dependence (known hereafter as “opioid abuse”) have grown over time. In a recent study using commercial claims data, Rice et al. (2014) reported that the prevalence of diagnosed opioid abuse increased from 6.7 per 10,000 in 2006 to 18.6 per 10,000 in 2011.2 Other studies using administrative claims data have found increasing rates of diagnosed opioid abuse among commercially insured populations as well as among publicly insured populations such as those covered by Medicaid, Medicare, and the Veteran’s Health Administration.3-5
While a recent study using Researched Abuse, Diversion, and Addiction-Related Surveillance (RADARS) data from drug-diversion investigators, poison centers, substance abuse treatment centers, and college students reported declining rates of diversion and abuse among individuals in 5 RADARS programs starting around 2011,6 it remains to be seen whether this change in trend has also occurred in broader patient populations or whether it is specific to the types of patients who entered these RADARS programs during this time period. Nevertheless, the public health burden of opioid abuse remains substantial. The Drug Abuse Warning Network reported that there were approximately 366,000 emergency department (ED) visits in 2011 associated with nonmedical use of narcotic pain relievers, out of over 5 million ED visits that were drug related.7
In addition, prior research has identified substantial opioid abuse-related costs to payers and society. Rice et al. matched commercially insured diagnosed opioid abusers to controls (i.e., patients not diagnosed with opioid abuse) based on baseline demographics, comorbidities, and health care resource use and estimated excess annual per-patient health care costs of diagnosed opioid abuse of $10,627 ($20,343 for opioid abusers vs. $9,716 for matched controls; P < 0.01).2 A follow-up study by Rice et al. (2014) using a different and larger commercial claims database yielded similar results; excess annual per-patient health care costs of diagnosed opioid abuse were estimated to be $11,376 ($22,301 for opioid abusers vs. $10,925 for matched controls; P < 0.01).8 In a recent study of the excess medical costs of diagnosed opioid abusers based on administrative claims data during 2009-2012, Rossiter et al. (2014) estimated excess medical costs of diagnosed opioid abusers of $9,456 for commercially insured continuous users of extended-release/long-acting opioids.9 White et al. (2011), using a demographically matched sample of opioid abusers and nonabusers, estimated excess annual health care costs of diagnosed opioid abuse of $20,546 per commercially insured patient.3 At a societal level, Birnbaum et al. (2011) estimated that the total societal costs of prescription opioid abuse, including direct costs and indirect costs (i.e., work-place and criminal justice costs) were $55.7 billion in 2007.10
Many of these findings reflect average excess health care costs among patients diagnosed with opioid abuse and do not capture considerable variation in the costs of opioid abuse. Health care spending in general (i.e., across all conditions) is quite concentrated, with patients in the top 20% in terms of health care spending accounting for over three quarters of total health care spending in 2009.11 An Agency for Healthcare Research and Quality study of the U.S. civilian noninstitutionalized population found that, in 2002, 5% of the population accounted for 49% of total medical expenditures, and half the population accounted for only 3% of total medical expenditures in 2002.12 As we discuss later, health care costs among patients diagnosed with opioid abuse are concentrated as well, with the top 20% of patients in terms of health care costs accounting for a disproportionate share of total health care costs. Little is known, however, about the characteristics of these diagnosed opioid abusers with extremely high health care costs. An improved understanding of these costly patients is relevant for physicians, managed care organizations, and other stakeholders who have an interest in addressing opioid abuse and reducing the associated health care costs. To this end, the primary objective of this study was to describe the characteristics of the subset of patients with total health care costs in the top 20% of total health care costs among patients diagnosed with opioid abuse (known hereafter as “high-cost patients”).
Methods
Data Source
Patients with commercial health insurance coverage were selected from the OptumHealth Reporting and Insights (OptumHealth) medical and pharmacy claims database. The OptumHealth database currently contains approximately 18.5 million commercially insured beneficiaries (employees, spouses, children, and retirees) of 84 large self-insured companies with locations across the United States and representing a variety of industries and job types. The data include medical claims (dates of service, International Classification of Diseases, Ninth Revision, Clinical Modification [ICD-9-CM] diagnosis codes, procedures performed, places of service, and payment amounts); pharmacy claims (fill dates, National Drug Code numbers, and payment amounts); and eligibility information (patient demographics and enrollment history). The data were de-identified by the data vendor in order to be compliant with the Health Insurance Portability and Accountability Act of 1996. Therefore, institutional review board approval was not necessary for this study. Data for services provided covering the period of Quarter 1 (Q1) 1999 through Q1 2012 were used in the analyses that follow.
Study Design
A retrospective analysis of administrative claims data was conducted to examine the characteristics of high-cost patients diagnosed with opioid abuse. Patients with opioid abuse were identified as those with any medical claims with at least 1 of the following ICD-9-CM diagnosis codes for opioid abuse or dependence: 304.0x, 304.7x, 305.5x, 965.00, 965.02, or 965.09 (Appendix A, available in online article). The use of opioid abuse and dependence ICD-9-CM diagnosis codes is consistent with the combination of prescription pain reliever abuse and dependence in the NSDUH.13 It is also consistent with the Diagnostic and Statistical Manual of Mental Disorders, 5th edition, which combines substance abuse and substance dependence into a single disorder.14 Several other studies on opioid abuse have also used opioid abuse and dependence ICD-9-CM diagnosis codes.3,4,9,10,15-17 Therefore, this study uses ICD-9-CM diagnosis codes for opioid abuse and dependence.
Patient Selection
Patients from the OptumHealth database were included in the study if they had at least 1 medical claim linked to an ICD-9-CM diagnosis code for opioid abuse, with the earliest such claim occurring during the period Q1 2006-Q1 2012 (Figure 1). Patients with an opioid abuse diagnosis prior to Q1 2006 were excluded in order to focus on more recent data. The study index date was defined as the date of the first medical claim with an opioid abuse diagnosis. Each individual was observed over an 18-month study period consisting of a 12-month observation period, which was centered on the index date, and a 6-month baseline period, which immediately preceded the observation period.
FIGURE 1.
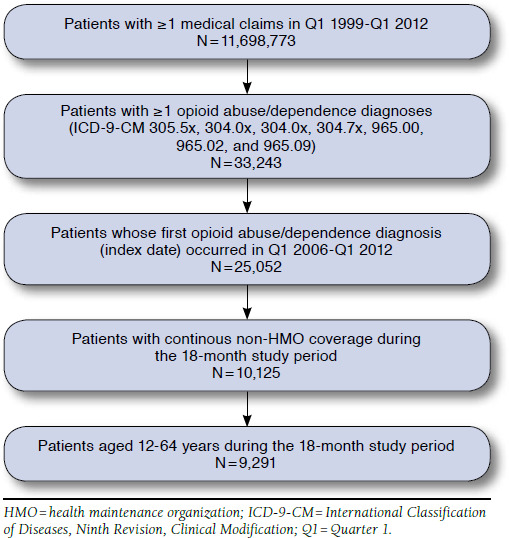
Sample Selection
Patients were required to be aged 12-64 years and to have continuous non-HMO (health maintenance organization) coverage throughout the 18-month study period (i.e., 6-month baseline period and the 12-month observation period) to ensure that all relevant medical and pharmacy claims were captured for the final sample of patients. Patients as young as aged 12 years were included because opioid abuse is a concern among youth aged 12-17 years, and they have been included in prior studies on opioid abuse.1,2,9 Patients aged 65 years and older were excluded from our study, since their Medicare eligibility would possibly have limited the ability to observe all relevant medical and pharmacy claims.
Among all patients diagnosed with opioid abuse included in the study cohort, “high-cost patients” were defined as patients with total health care costs in the top quintile (i.e., top 20%) of total health care costs among the study cohort during the 12-month observation period (Figure 2). The remaining patients were classified as “lower-cost patients.” The decision to group patients into quintiles based on total health care costs during the 12-month observation period and to compare patients in the top quintile with the rest of the patients was made a priori as a way to examine the characteristics of a subset of patients with high costs.
FIGURE 2.
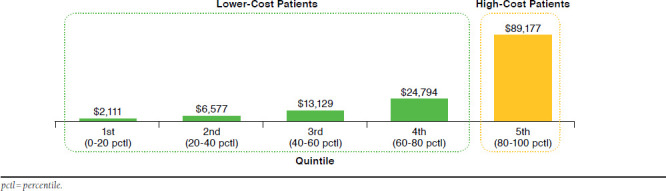
Mean Per-Patient Health Care Costs During the 12-Month Observation Period Among Patients Diagnosed with Opioid Abuse, by Quintiles
Baseline Patient Characteristics
Baseline patient characteristics were examined during the 6-month baseline period. Characteristics included demographics (age, gender, and region) and the year of the index date (i.e., date of opioid abuse diagnosis). In addition, baseline comorbidities were assessed. The Charlson Comorbidity Index was derived based on the Romano adaptation.18 The Charlson Comorbidity Index is a method of categorizing patient comorbidities based on ICD-9-CM diagnosis codes, and each comorbidity category is assigned a weight from 1 to 6 based on the adjusted risk of mortality. The sum of all the weights results in a single score for each patient, and a higher risk of mortality corresponds with a higher score. Individual categories of the Charlson Comorbidity Index, such as chronic pulmonary disease, diabetes, and rheumatologic disease, were also tabulated. In addition, given their relevance to patients diagnosed with opioid abuse, rates of nonopioid substance abuse diagnoses, psychotic disorders, and other mental disorders were calculated as well. Comorbidities were identified using ICD-9-CM diagnosis codes (Appendix A, available in online article).
Outcome Measures
The previously mentioned comorbidities were also examined during the 12-month observation period. In addition, health care resource use and health care costs were examined. Health care resource use included the rate of any health care resource use and the intensity of such use (e.g., number of visits or length of stay), and the measures were medical resource use by places of service and prescription drug use. Medical claims were classified into places of service (i.e., ED, inpatient, drug/alcohol rehabilitation facility, and outpatient) using codes for place of service, provider specialty, provider type, and type of service codes (available upon request). Claims not classified in 1 of these 4 categories were classified as “other facility.”
Health care costs were calculated as the total amount paid to service providers by the insurer for all covered services, regardless of diagnosis, as reflected on the claims. Out-of-pocket payments by patients (e.g., copay and deductibles) were not included. Measures included total health care costs, total medical costs, medical costs by places of service, and prescription drug costs. Health care costs were inflated to 2012 U.S. dollars using the medical care component of the Consumer Price Index.
The share of medical resource use directly attributed to opioid abuse (vs. other causes) was also examined. “Abuse-related medical resource use” was defined as medical resource use linked to claims with opioid abuse diagnoses. Note that this likely reflects a lower-bound estimate of opioid abuse-related medical resource use, since some medical care triggered by opioid abuse may not be coded as related to opioid abuse for insurance claims purposes. Medical resource use not linked to claims with opioid abuse diagnoses was defined as “other medical resource use.” “Abuse-related medical costs” and “other medical costs” were similarly defined.
Statistical Analysis
Dichotomous variables were summarized using frequencies and percentages. Continuous variables were summarized using means and standard deviations. Comparisons between high-cost patients and lower-cost patients diagnosed with opioid abuse were conducted using chi-square tests for dichotomous variables and Wilcoxon rank-sum tests for continuous variables.
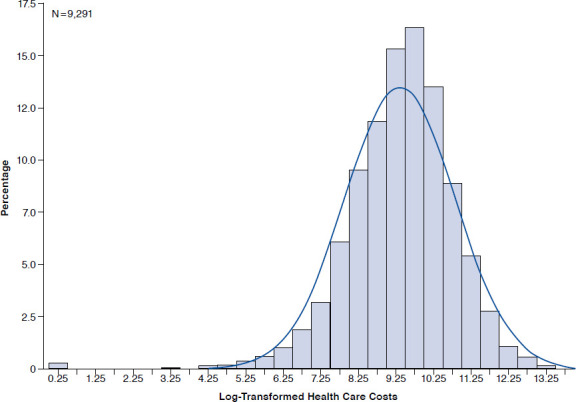
In addition, a multivariate regression analysis was conducted to examine the relationship between patient characteristics in the baseline period and health care costs in the observation period among all patients diagnosed with opioid abuse. Specifically, we estimated an ordinary least squares (OLS) regression model in which 12-month observation period health care costs (log-transformed) was the dependent variable. Health care costs were log-transformed to account for their skewed distribution; log-transformed costs were approximately normally distributed (Appendix B, available in online article). Independent variables included age; gender; geographic region; indicator variables for baseline period comorbidities (components of the Charlson Comorbidity Index, as well as nonopioid substance abuse diagnoses [e.g., abuse of hallucinogenics], psychotic disorders, and other mental disorders); log-transformed baseline health care costs; and baseline health care resource use. Data on race and socioeconomic status were not available in the OptumHealth database. All analyses were conducted using SAS software for Windows version 9.3 (SAS Institute, Cary, NC). Results were considered statistically significant at P < 0.05.
Results
The patient selection criteria resulted in a sample of 9,291 patients diagnosed with opioid abuse (Figure 1). There were 1,859 patients classified as high-cost patients, and the remaining 7,432 patients were classified as lower-cost patients.
Comparing Baseline Characteristics
Relative to lower-cost patients, high-cost patients were older (42.5 vs. 36.1; P < 0.001) and more likely to be female (55.9% vs. 42.9%; P < 0.001; Table 1). In addition, high-cost patients had increased rates of baseline comorbidities, as reflected by the Charlson Comorbidity Index (0.8 vs. 0.2; P < 0.001), as well as specific conditions such as chronic pulmonary disease (12.9% vs. 5.6%; P < 0.001), mild/moderate diabetes (8.4% vs. 3.4%; P < 0.001), rheumatologic disease (5.1% vs. 1.3%; P < 0.001), congestive heart failure (5.1% vs. 1.0%; P < 0.001), and malignancies (3.4% vs. 1.2%; P < 0.001). High-cost patients also had increased rates of nonopioid substance abuse diagnoses (12.4% vs. 8.9%; P < 0.001), psychotic disorders (26.5% vs. 13.6%; P < 0.001), and other mental disorders (36.1% vs. 25.6%; P < 0.001).
TABLE 1.
Patient Characteristics and Comorbidities in the Baseline Period
| Baseline Characteristicsa | High-Cost Patientsb (n = 1,859) | Lower-Cost Patientsb (n = 7,432) | P Valuec | ||
|---|---|---|---|---|---|
| N or Mean | % or SD | N or Mean | % or SD | ||
| Patient characteristics | |||||
| Age at index date | 42.5 | 13.9 | 36.1 | 14.4 | < 0.001 |
| Female | 819 | 55.9% | 4,244 | 42.9% | < 0.001 |
| U.S. Census divisiond | |||||
| East North Central | 368 | 19.8% | 1,427 | 19.2% | 0.561 |
| Middle Atlantic | 291 | 15.7% | 1,415 | 19.0% | < 0.001 |
| South Atlantic | 332 | 17.9% | 1,307 | 17.6% | 0.782 |
| West South Central | 230 | 12.4% | 736 | 9.9% | 0.002 |
| Mountain | 188 | 10.1% | 699 | 9.4% | 0.353 |
| Pacific | 188 | 10.1% | 575 | 7.7% | < 0.001 |
| East South Central | 89 | 4.8% | 596 | 8.0% | < 0.001 |
| West North Central | 106 | 5.7% | 344 | 4.6% | 0.054 |
| New England | 66 | 3.6% | 324 | 4.4% | 0.120 |
| Unknown | 1 | 0.1% | 9 | 0.1% | 0.698 |
| Year of index date | |||||
| 2006 | 228 | 12.3% | 860 | 11.6% | 0.406 |
| 2007 | 301 | 16.2% | 1,074 | 14.5% | 0.059 |
| 2008 | 262 | 14.1% | 1,145 | 15.4% | 0.158 |
| 2009 | 344 | 18.5% | 1,269 | 17.1% | 0.145 |
| 2010 | 413 | 22.2% | 1,669 | 22.5% | 0.824 |
| 2011 | 311 | 16.7% | 1,415 | 19.0% | 0.022 |
| Comorbidities | |||||
| Charlson Comorbidity Index | 0.8 | 1.4 | 0.2 | 0.7 | < 0.001 |
| Components of Charlson Comorbidity Index | |||||
| Chronic pulmonary disease | 240 | 12.9% | 417 | 5.6% | < 0.001 |
| Mild-to-moderate diabetes | 157 | 8.4% | 254 | 3.4% | < 0.001 |
| Rheumatologic disease | 94 | 5.1% | 93 | 1.3% | < 0.001 |
| Congestive heart failure | 95 | 5.1% | 72 | 1.0% | < 0.001 |
| Any malignancy including leukemia and lymphoma | 64 | 3.4% | 92 | 1.2% | < 0.001 |
| Cerebrovascular disease | 77 | 4.1% | 78 | 1.0% | < 0.001 |
| Diabetes with chronic complications | 62 | 3.3% | 65 | 0.9% | < 0.001 |
| Peripheral vascular disease | 54 | 2.9% | 68 | 0.9% | < 0.001 |
| Mild liver disease | 42 | 2.3% | 49 | 0.7% | < 0.001 |
| Renal disease | 50 | 2.7% | 32 | 0.4% | < 0.001 |
| Peptic ulcer disease | 26 | 1.4% | 26 | 0.3% | < 0.001 |
| Myocardial infarction | 21 | 1.1% | 17 | 0.2% | < 0.001 |
| Hemiplegia or paraplegia | 20 | 1.1% | 16 | 0.2% | < 0.001 |
| Metastatic solid tumor | 21 | 1.1% | 8 | 0.1% | < 0.001 |
| HIV/AIDS | 13 | 0.7% | 14 | 0.2% | < 0.001 |
| Moderate or severe liver disease | 8 | 0.4% | 5 | 0.1% | 0.001 |
| Dementia | 0 | 0.0% | 3 | 0.0% | 1.000 |
| Other selected comorbidities | |||||
| Nonopioid substance abuse diagnoses | 231 | 12.4% | 662 | 8.9% | < 0.001 |
| Psychotic disorders | 493 | 26.5% | 1,008 | 13.6% | < 0.001 |
| Other mental disorders | 672 | 36.1% | 1,900 | 25.6% | < 0.001 |
aThe baseline period was defined as the 6-month period prior to the 12-month observation period (which was centered on the index date).
bHigh-cost patients were defined as patients with health care costs in the top 20% of health care costs among all patients in the study cohort during the observation period.
cP values were calculated using chi-square tests for dichotomous variables and Wilcoxon rank-sum tests for continuous variables. Results were considered statistically significant at P<0.05.
dU.S. Census Bureau divisions were classified as follows: East North Central (IL, IN, MI, OH, WI); Middle Atlantic (NJ, NY, PA); South Atlantic (DC, DE, FL, GA, MD, NC, VA, SC, WV); West South Central (AR, LA, OK, TX); Mountain (AZ, CO, ID, MT, NM, NV, UT, WY); Pacific (AK, CA, HI, OR, WA); East South Central (AL, KY, MS, TN); West North Central (IA, KS, ND, MN, MO, NE, SD); and New England (CT, NH, MA, ME, RI, VT).
AIDS = acquired immune deficiency syndrome; HIV = human immunodeficiency virus; SD = standard deviation.
Comparing Observation Period Characteristics
In the observation period, high-cost patients continued to have increased rates of comorbidities, as reflected by the Charlson Comorbidity Index (1.6 vs. 0.4; P < 0.001), as well as specific conditions such as chronic pulmonary disease (24.0% vs. 10.5%; P < 0.001), mild/moderate diabetes (10.8% vs. 5.2%; P < 0.001), rheumatologic disease (8.3% vs. 2.4%; P < 0.001), congestive heart failure (12.2% vs. 2.2%; P < 0.001), and malignancies (7.4% vs. 2.4%; P < 0.001; Table 2). In fact, high-cost patients had higher rates of all components of the Charlson Comorbidity Index, and the ratios of rates of comorbidities among high-cost patients to those among lower-cost patients increased for nearly all conditions in the follow-up period. High-cost patients also had increased rates of nonopioid substance abuse diagnoses (53.0% vs. 47.2%; P < 0.001), psychotic disorders (67.1% vs. 47.5%; P < 0.001), and other mental disorders (70.2% vs. 57.5%; P < 0.001).
TABLE 2.
Comorbidities, Health Care Resource Use, and Health Care Costs in the Observation Period
| Characteristicsa | High-Cost Patientsb (n = 1,859) | Lower-Cost Patientsb (n = 7,432) | P Valuec | ||
|---|---|---|---|---|---|
| N or Mean | % or SD | N or Mean | % or SD | ||
| Comorbidities | |||||
| Charlson Comorbidity Index | 1.60 | 2.29 | 0.42 | 1.05 | < 0.001 |
| Components of Charlson Comorbidity Index | |||||
| Chronic pulmonary disease | 447 | 24.0% | 784 | 10.5% | < 0.001 |
| Mild-to-moderate diabetes | 200 | 10.8% | 387 | 5.2% | < 0.001 |
| Rheumatologic disease | 154 | 8.3% | 176 | 2.4% | < 0.001 |
| Congestive heart failure | 226 | 12.2% | 161 | 2.2% | < 0.001 |
| Any malignancy including leukemia and lymphoma | 138 | 7.4% | 180 | 2.4% | < 0.001 |
| Cerebrovascular disease | 214 | 11.5% | 197 | 2.7% | < 0.001 |
| Diabetes with chronic complications | 120 | 6.5% | 126 | 1.7% | < 0.001 |
| Peripheral vascular disease | 123 | 6.6% | 105 | 1.4% | < 0.001 |
| Mild liver disease | 92 | 4.9% | 95 | 1.3% | < 0.001 |
| Renal disease | 144 | 7.7% | 70 | 0.9% | < 0.001 |
| Peptic ulcer disease | 65 | 3.5% | 52 | 0.7% | < 0.001 |
| Myocardial infarction | 73 | 3.9% | 43 | 0.6% | < 0.001 |
| Hemiplegia or paraplegia | 49 | 2.6% | 40 | 0.5% | < 0.001 |
| Metastatic solid tumor | 44 | 2.4% | 16 | 0.2% | < 0.001 |
| HIV/AIDS | 19 | 1.0% | 25 | 0.3% | < 0.001 |
| Moderate or severe liver disease | 32 | 1.7% | 16 | 0.2% | < 0.001 |
| Dementia | 13 | 0.7% | 14 | 0.2% | < 0.001 |
| Other selected comorbidities | |||||
| Nonopioid substance abuse diagnoses | 984 | 53.0% | 3,351 | 47.2% | < 0.001 |
| Psychotic disorders | 1,244 | 67.1% | 3,374 | 47.5% | < 0.001 |
| Other mental disorders | 1,302 | 70.2% | 4,081 | 57.5% | < 0.001 |
| Annual Health Care Resource Use | |||||
| Medical resource use | |||||
| Any visit | |||||
| Inpatient | 1,529 | 82.2% | 2,702 | 36.4% | < 0.001 |
| Emergency department | 1,640 | 88.2% | 4,528 | 60.9% | < 0.001 |
| Outpatient | 1,855 | 99.8% | 7,274 | 97.9% | < 0.001 |
| Drug/alcohol rehabilitation facility | 559 | 30.1% | 1,632 | 22.0% | < 0.001 |
| Other | 1,487 | 80.0% | 4,005 | 53.9% | < 0.001 |
| Number of visits/days | |||||
| Inpatient days | 16.1 | 23.9 | 2.9 | 7.2 | < 0.001 |
| Emergency department days | 8.9 | 13.6 | 1.9 | 3.2 | < 0.001 |
| Outpatient visits | 38.2 | 24.6 | 18.7 | 15.9 | < 0.001 |
| Drug/alcohol rehabilitation facility days | 9.5 | 22.3 | 5.6 | 18.0 | < 0.001 |
| Other visits | 8.2 | 13.7 | 2.6 | 5.3 | < 0.001 |
| Abuse-related medical resource use | |||||
| Inpatient days | 4.7 | 10.7 | 1.6 | 4.7 | < 0.001 |
| Emergency department days | 1.3 | 3.0 | 0.5 | 1.1 | < 0.001 |
| Outpatient visits | 2.5 | 7.5 | 3.4 | 7.0 | < 0.001 |
| Drug/alcohol rehabilitation facility days | 4.6 | 14.9 | 4.3 | 16.4 | < 0.001 |
| Other visits | 0.6 | 2.6 | 0.7 | 2.6 | < 0.001 |
| Abuse-related share of total medical resource use | |||||
| Inpatient days | 29% | - | 56% | - | - |
| Emergency department days | 15% | - | 25% | - | - |
| Outpatient visits | 7% | - | 18% | - | - |
| Drug/alcohol rehabilitation facility days | 49% | - | 76% | - | - |
| Other visits | 8% | - | 27% | - | - |
| Prescription drug use | |||||
| Any prescription drug fill | 1,802 | 96.9% | 6,871 | 92.5% | < 0.001 |
| Number of prescriptions filled | 71.4 | 50 | 32.6 | 32 | < 0.001 |
| Number of unique NDC numbers filled | 29.0 | 20 | 12.9 | 11 | < 0.001 |
| Annual Health Care Costs | $89,177 | $87,211 | $11,653 | $9,031 | < 0.001 |
| Medical costs | $79,386 | $86,986 | $8,986 | $8,075 | < 0.001 |
| Inpatient | $34,600 | $68,531 | $1,577 | $3,752 | < 0.001 |
| Emergency department | $16,597 | $35,913 | $1,630 | $3,102 | < 0.001 |
| Outpatient | $19,513 | $25,233 | $3,696 | $4,474 | < 0.001 |
| Drug/alcohol rehabilitation facility | $4,393 | $11,696 | $1,263 | $3,666 | < 0.001 |
| Other | $4,283 | $10,949 | $821 | $2,178 | < 0.001 |
| Abuse-related medical costs | $15,706 | $31,980 | $3,429 | $4,978 | < 0.001 |
| Inpatient | $8,089 | $29,449 | $909 | $2,774 | < 0.001 |
| Emergency department | $3,320 | $10,675 | $559 | $1,774 | < 0.001 |
| Outpatient | $1,231 | $5,336 | $617 | $1,473 | 0.029 |
| Drug/alcohol rehabilitation facility | $2,336 | $7,924 | $940 | $3,106 | < 0.001 |
| Other | $730 | $3,271 | $405 | $1,537 | < 0.001 |
| Abuse-related share of total medical costs | 20% | - | 38% | - | - |
| Inpatient | 23% | - | 58% | - | - |
| Emergency department | 20% | - | 34% | - | - |
| Outpatient | 6% | - | 17% | - | - |
| Drug/alcohol rehabilitation facility | 53% | - | 74% | - | - |
| Other | 17% | - | 49% | - | - |
| Prescription drug costs | $9,791 | $16,811 | $2,667 | $3,864 | < 0.001 |
aThe observation period was defined as the 12-month period centered on the index date.
bHigh-cost patients were defined as patients with health care costs in the top 20% of health care costs among all patients in the study cohort during the observation period.
cP values were calculated using chi-square tests for dichotomous variables and Wilcoxon rank-sum tests for continuous variables. Results were considered statistically significant at P < 0.05.
AIDS = acquired immune deficiency syndrome; HIV = human immunodeficiency virus; NDC = National Drug Code; SD = standard deviation.
Compared with lower-cost patients, high-cost patients had a greater likelihood of utilizing medical resources across all places of service and did so with greater intensity. For example, high-cost patients were more likely to have at least 1 inpatient visit (82.2% vs. 36.4%; P < 0.001) and at least 1 ED visit (88.2% vs. 60.9%; P < 0.001). They also had longer inpatient stays (16.1 days vs. 2.9; P < 0.001) and spent more days in the ED (8.9 days vs. 1.9; P < 0.001). High-cost patients were more likely to have any prescription drug fill (96.9% vs. 92.5%; P < 0.001), and they filled more prescriptions (71.4 vs. 32.6; P < 0.001) and more unique prescriptions as measured by different National Drug Code numbers (29.0 vs. 12.9; P < 0.001) compared with lower-cost patients.
High-cost patients also had a greater intensity of opioid abuse-related medical resource use in the inpatient setting (4.7 days vs. 1.6; P < 0.001), ED (1.3 days vs. 0.5; P < 0.001), and drug/alcohol rehabilitation facility (4.6 days vs. 4.3; P < 0.001). However, the share of overall all-cause medical resource use that was related to opioid abuse was lower among high-cost patients than among lower-cost patients across all places of service. For example, opioid abuse-related inpatient days accounted for 29% of inpatient days for high-cost patients but accounted for 56% of inpatient days for lower-cost patients. Abuse-related ED days accounted for 15% of ED days for high-cost patients but accounted for 25% of ED days for lower-cost patients.
The mean observation period health care costs of high-cost patients was $89,177 (vs. $11,653 for lower-cost patients; P < 0.001), of which 38.8% ($34,600) was attributed to inpatient costs, 21.9% ($19,513) to outpatient costs, 18.6% ($16,597) to ED costs, 4.9% ($4,393) to drug/alcohol rehabilitation facility costs, 4.8% ($4,283) to other facility costs, and 11.0% ($9,791) to prescription drugs. In total, high-cost patients accounted for approximately two thirds of the total health care costs of patients diagnosed with opioid abuse (Figure 3).
FIGURE 3.
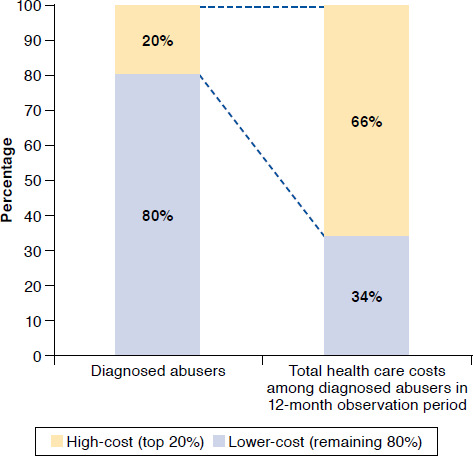
Relative Contributions of High-Cost Patients and Lower-Cost Patients to Total Health Care Costs in the Observation Period
High-cost patients had overall all-cause medical costs that were nearly 9 times higher ($79,386 vs. $8,986; P < 0.001) and opioid abuse-related medical costs that were 4.5 times higher ($15,706 vs.$3,429; P < 0.001) than lower-cost patients. Although high-cost patients had higher health care costs across all places of service, the largest differential was due to inpatient stays ($34,600 vs. $1,577; P < 0.001). In addition, high-cost patients had higher prescription drug costs compared with lower-cost patients ($9,791 vs. $2,667; P < 0.001).
However, mirroring the resource use findings, the share of medical costs directly attributable to claims with opioid abuse diagnoses was lower among high-cost patients than among lower-cost patients. For example, opioid abuse-related inpatient costs accounted for 23% of inpatient costs for high-cost patients but 58% of inpatient costs for lower-cost patients. Opioid abuse-related drug/alcohol rehabilitation facility costs accounted for 53% of drug/alcohol rehabilitation facility costs for high-cost patients but 74% of opioid abuse-related drug/alcohol rehabilitation facility costs for lower-cost patients.
A sensitivity analysis was conducted in order to examine whether the results were sensitive to the definition of the study period. The results using a 6-month post-index period (i.e., the second half of the 12-month observation period) were consistent with those using the full 12-month observation period (results available upon request).
Multivariate Regression Results
Several baseline characteristics had a statistically significant (P < 0.05) relationship with observation period health care costs when considered jointly in a multivariate regression framework (Table 3). Eight of the 17 components of the Charlson Comorbidity Index had a positive and statistically significant association with observation period health care costs. Log-transformed baseline medical costs and prescription drug costs also had a positive and statistically significant association with observation period health care costs, as did health care resource use (i.e., number of visits/days by different places of service). The R-squared value of our OLS regression on log-transformed heath care costs was 0.273, suggesting that a relatively small share of the variation in health care costs in the observation period was explained by observable baseline characteristics.
TABLE 3.
Multivariate Regression Results
| Parameter | Co-efficient | Standard Error | P Value |
|---|---|---|---|
| Intercept | 8.08 | 0.07 | < 0.001 |
| Patient characteristics | |||
| Age | 0.00 | 0.00 | 0.078 |
| Male | -0.15 | 0.03 | < 0.001 |
| U.S. Census Division: Unknown | 0.19 | 0.40 | 0.636 |
| U.S. Census Division 1: New England | -0.10 | 0.07 | 0.157 |
| U.S. Census Division 2: Middle Atlantic | -0.01 | 0.04 | 0.807 |
| U.S. Census Division 4: West North Central | 0.09 | 0.07 | 0.189 |
| U.S. Census Division 5: South Atlantic | 0.09 | 0.04 | 0.034 |
| U.S. Census Division 6: East South Central | -0.16 | 0.06 | 0.005 |
| U.S. Census Division 7: West South Central | 0.12 | 0.05 | 0.015 |
| U.S. Census Division 8: Mountain | 0.11 | 0.05 | 0.043 |
| U.S. Census Division 9: Pacific | 0.23 | 0.06 | < 0.001 |
| Year of index date: 2007 | -0.01 | 0.05 | 0.901 |
| Year of index date: 2008 | 0.07 | 0.05 | 0.159 |
| Year of index date: 2009 | 0.01 | 0.05 | 0.866 |
| Year of index date: 2010 | -0.03 | 0.05 | 0.468 |
| Year of index date: 2011 | -0.07 | 0.05 | 0.170 |
| Comorbidities | |||
| Components of Charlson Comorbidity Index | |||
| Chronic pulmonary disease | 0.14 | 0.05 | 0.011 |
| Mild-to-moderate diabetes | 0.16 | 0.07 | 0.014 |
| Rheumatologic disease | 0.25 | 0.09 | 0.008 |
| Congestive heart failure | 0.16 | 0.11 | 0.137 |
| Any malignancy including leukemia and lymphoma | 0.16 | 0.10 | 0.123 |
| Cerebrovascular disease | 0.18 | 0.11 | 0.092 |
| Diabetes with chronic complications | 0.34 | 0.12 | 0.004 |
| Peripheral vascular disease | 0.11 | 0.12 | 0.337 |
| Mild liver disease | 0.21 | 0.13 | 0.121 |
| Renal disease | 0.44 | 0.14 | 0.002 |
| Peptic ulcer disease | 0.15 | 0.18 | 0.393 |
| Myocardial infarction | 0.10 | 0.21 | 0.640 |
| Hemiplegia or paraplegia | 0.59 | 0.21 | 0.005 |
| Metastatic solid tumor | 0.63 | 0.24 | 0.008 |
| HIV/AIDS | 0.46 | 0.24 | 0.061 |
| Moderate or severe liver disease | 0.85 | 0.35 | 0.015 |
| Dementia | -0.17 | 0.73 | 0.815 |
| Other selected comorbidities | |||
| Nonopioid substance abuse diagnoses | 0.01 | 0.05 | 0.814 |
| Psychotic disorders | 0.07 | 0.04 | 0.092 |
| Other mental disorders | 0.00 | 0.03 | 0.898 |
| Baseline health care costs (log-transformed) | |||
| Medical costs | 0.09 | 0.01 | < 0.001 |
| Prescription drug costs | 0.10 | 0.10 | < 0.001 |
| Baseline health care resource use (number of visits/days) | |||
| Inpatient days | 0.01 | 0.00 | < 0.001 |
| Emergency department days | 0.02 | 0.00 | < 0.001 |
| Outpatient visits | 0.01 | 0.00 | < 0.001 |
| Drug/alcohol rehabilitation facility days | 0.01 | 0.00 | 0.050 |
| Other visits | 0.01 | 0.00 | 0.014 |
Note: An ordinary least squares (OLS) regression was performed on log-transformed health care costs. N = 9,291; R-squared value = 0.273. Results were considered statistically significant at P < 0.05.
AIDS = acquired immune deficiency syndrome; HIV = human immunodeficiency virus.
Discussion
This study provides insights into the challenges physicians and managed care organizations face in managing patients diagnosed with opioid abuse. Compared with lower-cost patients, the costliest patients diagnosed with opioid abuse were found to have higher rates of preexisting and concurrent chronic comorbidities and mental health conditions. While we focused on identifying differences within the population of diagnosed opioid abusers, these findings are consistent with prior research on opioid abuse comparing opioid abusers to nonabusers. White et al. (2005) reported that opioid abusers have higher rates of certain comorbidities than do nonabusers.19 For example, opioid abusers were 11.2 times more likely to have had at least 1 mental health outpatient visit and 12.2 times more likely to have had at least 1 hospital inpatient stay than nonabusers (P < 0.01). In addition, nonopioid poisoning and psychiatric illnesses were 78.0 and 8.5 times more prevalent among opioid abusers than among nonabusers, respectively (P < 0.01). Becker et al. (2008) also found that mental health conditions (e.g., panic and social phobic/agoraphobic symptoms, misuse of another class of prescription medication) were prevalent among opioid abusers than among nonabusers.20 Furthermore, 2 review articles also had similar observations. Jan (2010) noted that psychiatric disorders are common among patients with opioid dependence.21 Strassels (2009) noted that patients who abuse opioids may be at risk for certain conditions such as hepatitis or human immunodeficiency virus, as they may be at higher risk for hazardous routes of administration such as intravenous use.22
Reducing costs and improving quality and outcomes are important functions of managed care organizations. With nearly two thirds of the health care costs associated with patients diagnosed with opioid abuse concentrated in just one fifth of patients, being able to target the subset of patients that accounts for a disproportionate share of the economic burden of opioid use is an important step towards achieving these goals. High-cost patients had greater all-cause and opioid abuse-related medical resource use and costs in absolute terms, so addressing opioid abuse in this population could reduce the overall economic burden of opioid abuse by reducing the medical costs of the costliest opioid abuse patients. However, the finding that the share of overall all-cause medical resource use and costs that was directly related to opioid abuse was lower among high-cost patients than among lower-cost patients suggests that high-cost patients would likely continue to have high medical resource use and costs due to other conditions. High-cost patients have higher rates of nonopioid abuse-related comorbidities, so the share of total health care costs attributed to opioid abuse specifically is lower than that among lower-cost patients who have lower rates of nonopioid abuse-related comorbidities. In addition, differences in rates of comorbidities between high-cost patients and lower-cost patients widened in the observation period, suggesting that disease progression for nonopioid abuse-related comorbidities may have been more pronounced or accelerated among high-cost patients. Better understanding of the characteristics of high-cost patients diagnosed with opioid abuse could help physicians and managed care organizations target their efforts to address opioid abuse and to reduce health care costs.
This study found that high-cost patients were complicated patients with higher rates of baseline comorbidities. Opioid abuse may interact with these baseline comorbidities and make it difficult for patients to adhere to treatment plans for underlying conditions, thereby resulting in greater health care resource use and costs. This suggests that there is a need for greater awareness and screening of comorbid conditions when patients are first diagnosed with opioid abuse. Baseline comorbidities, combined with baseline health care costs and resource use, explained a relatively small share of the variation in observation period health care costs, however.
Using administrative claims data, it would be difficult to predict which opioid abusers will be the costliest patients based on characteristics prior to the first opioid abuse diagnosis. Therefore, future research should explore other reasons for the disproportionately higher health care costs among high-cost patients, such as differences in the severity of opioid abuse, which cannot be observed in administrative claims data but could potentially be observed in electronic medical records or survey data, for example. A multifaceted approach may be necessary to address opioid abuse at the societal level. In addition to treatment for patients diagnosed with opioid abuse, other efforts may include education of physicians, risk stratification tools to identify patients at higher risk of opioid abuse, prescription drug monitoring programs, and new drug formulations intended to deter opioid abuse.23
Limitations
This study has a number of limitations. First, the study did not assess the causal relationship between patient characteristics and health care costs among diagnosed opioid abusers. Moreover, no causal relationship was established between opioid abuse severity and costs, since data were not available regarding opioid abuse severity. Because much of the variation in observation period health care costs cannot be explained by observable patient characteristics, further research is necessary to understand the extent to which treating or preventing opioid abuse among the higher cost patients would reduce health care costs. Second, as with any claims-based study, this study relied on the accuracy of claims data, and any miscoding in the underlying data could affect our results. For example, opioid abusers were identified using ICD-9-CM diagnosis codes for opioid abuse, but a substantial share of opioid abusers may be undiagnosed. In addition, opioid abuse may be coded as another condition, such as depression, for reimbursement purposes. These undiagnosed opioid abusers would not be captured in this analysis. In addition, our analysis of opioid abuse-related medical resource use and opioid abuse-related medical costs relied on medical claims associated with ICD-9-CM diagnosis codes for opioid abuse. As previously noted, these claims likely reflect a lower-bound estimate of opioid abuse-related resource use and costs, since some medical care resulting from opioid abuse (e.g., repeat visits, treatment of complications) may not be coded as opioid abuse-related for insurances claims purposes. Third, the rates of comorbidities estimated in this study are likely underestimates due to the relatively short duration of the baseline period (i.e., 6 months). A longer baseline period would have allowed for the observation of more comorbidities. In addition, only the primary and secondary diagnosis codes are included in the OptumHealth claims data, so any additional diagnoses would not be captured in our analysis. Fourth, the OptumHealth claims data do not include race or socioeconomic status, which may affect opioid abuse and the costs associated with opioid abuse. Finally, this study used the OptumHealth commercial claims database. Future research should examine the characteristics of high-cost patients diagnosed with opioid abuse in Medicaid, Medicare, and uninsured populations.
Conclusions
Addressing a problem as complicated as prescription opioid abuse requires a nuanced understanding of opioid abusers. Such an understanding could help physicians and managed care organizations identify opportunities for intervention and target their efforts to address prescription opioid abuse and reduce the associated costs. This study found that high-cost patients accounted for a disproportionately large share of the total health care costs of patients diagnosed with opioid abuse. The costliest patients diagnosed with opioid abuse had high rates of preexisting and concurrent chronic comorbidities and mental health conditions. These results highlight the need to consider the complete medical and psychosocial patient history to better manage the underlying conditions contributing to high health care costs. Abuse may also exacerbate existing conditions and make it difficult for patients to adhere to treatment plans. In addition to targeting the subset of patients that accounts for a disproportionate share of the economic burden of opioid abuse, other multifaceted efforts, such as provider education, coordinated programs that address medical and social needs, prescription drug monitoring programs, and new drug formulations intended to deter opioid abuse, may be necessary to address prescription opioid abuse at the societal level.
APPENDIX A. Diagnosis Codes
| Comorbidity | ICD-9-CM Diagnosis Codes |
|---|---|
| Opioid abuse and dependence | |
| Opioid type dependence | 304.0x |
| Combinations of opioid type drug with any other drug dependence | 304.7x |
| Nondependent opioid abuse | 305.5x |
| Poisoning by opiates and related narcotics | 965.0x (excluding 965.01 for poisoning by heroin) |
| Components of the Charlson Comorbidity Index | |
| Myocardial infarction | 410.xx, 412.xx |
| Congestive heart failure | 402.01, 402.11, 402.91, 404.01, 404.03, 404.11, 404.13, 404.91, 404.93, 425.xx, 428.xx, 429.3x |
| Peripheral vascular disease | 440.xx-442.xx, 443.1x-443.9x, 447.1x, 785.4x |
| Cerebrovascular disease | 362.34, 430.xx-436.xx, 437.0x-437.1x, 437.9x, 438.xx, 781.4x, 784.3x, 997.0x |
| Dementia | 290.xx, 331.0x-331.2x |
| Chronic pulmonary disease | 415.0x, 416.8x, 416.9x, 491.xx-494.xx, 496.xx |
| Rheumatologic disease | 710.xx, 714.xx |
| Peptic ulcer disease | 531.xx-534.xx |
| Mild liver disease | 571.2x, 571.5x, 571.6x, 571.8x, 571.9x |
| Diabetes | 250.0x-250.3x |
| Diabetes with chronic complications | 250.4x-250.9x |
| Hemiplegia or paraplegia | 342.xx, 344.xx |
| Renal disease | 585.xx-586.xx, V42.0x, V45.1x, V56.xx |
| Any malignancy including leukemia and lymphoma | 140.xx-171.xx, 174.xx-195.xx, 200.xx-208.xx, 273.0x, 273.3x, V10.46 |
| Moderate or severe liver disease | 572.2x-572.4x, 456.0x-456.2x |
| Metastatic solid tumor | 196.xx-199.xx |
| AIDS | 042.xx-044.xx |
| Other selected comorbidities | |
| Nonopioid substance abuse diagnoses | 303.xx, 304.1x-304.6x, 304.8x-304.9x, 305.0x-305.4x, 305.6x-305.9x, V11.3 |
| Psychotic disorders | 290.xx-299.xx, V11.0-V11.1 |
| Other mental disorders | 300.xx-302.xx, 306.xx-319.xx, V11.2, V11.8-V11.9 |
AIDS = acquired immune deficiency syndrome; ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification.
APPENDIX B. Distribution of Log-Transformed Total Health Care Costs
References
- 1. Substance Abuse and Mental Health Services Administration. . Results from the 2012 National Survey on Drug Use and Health: summary of national findings. NSDUH Series H-46, HHS Publication No. (SMA) 13-4795. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. Available at: http://www.samhsa.gov/data/sites/default/files/NSDUHresults2012/NSDUHresults2012.pdf. Accessed August 19, 2015. [Google Scholar]
- 2. Rice JB, Kirson NY, Shei A, et al. . Estimating the costs of opioid abuse and dependence from an employer perspective: a retrospective analysis using administrative claims data. Appl Health Econ Health Policy. 2014; 12(4): 435-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. White AG, Birnbaum HG, Schiller M, Waldman T, Cleveland JM, Roland CL.. Economic impact of opioid abuse, dependence, and misuse. Am J Pharm Benefits. 2011; 3(4): e59-e70. [DOI] [PubMed] [Google Scholar]
- 4. Dufour R, Joshi AV, Pasquale MK, et al. . The prevalence of diagnosed opioid abuse in commercial and Medicare managed care populations. Pain Pract. 2014; 14(3): E106-15. [DOI] [PubMed] [Google Scholar]
- 5. Baser O, Xie L, Mardekian J, Schaaf D, Wang L, Joshi AV.. Prevalence of diagnosed opioid abuse and its economic burden in the Veterans Health Administration. Pain Pract. 2014; 14(5): 437-45. [DOI] [PubMed] [Google Scholar]
- 6. Dart RC, Surratt HL, Cicero TJ, et al. . Trends in opioid analgesic abuse and mortality in the United States. N Engl J Med. 2015; 15;372(3): 241-48. [DOI] [PubMed] [Google Scholar]
- 7. Substance Abuse and Mental Health Services Administration. . Drug Abuse Warning Network, 2011: national estimates of drug-related emergency department visits. HHS Publication No. (SMA) 13-4760, DAWN Series D-39. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013. Available at: http://www.samhsa.gov/data/sites/default/files/DAWN2k11ED/DAWN2k11ED/DAWN2k11ED.pdf. Accessed August 19, 2015. [Google Scholar]
- 8. Rice JB, Kirson NY, Shei A, et al. . The economic burden of diagnosed opioid abuse among commercially insured individuals. Postgrad Med. 2014; 126(4): 53-58. [DOI] [PubMed] [Google Scholar]
- 9. Rossiter LF, Kirson NY, Shei A, et al. . Medical cost savings associated with an extended-release opioid with abuse-deterrent technology in the U.S. J Med Econ. 2014; 17(4): 279-87. [DOI] [PubMed] [Google Scholar]
- 10. Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL.. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med. 2011; 12(4): 657-67. [DOI] [PubMed] [Google Scholar]
- 11. Henry J. Kaiser Family Foundation. Health care costs: a primer. Key information on health care costs and their impact. May 2012. Available at: http://kaiserfamilyfoundation.files.wordpress.com/2013/01/7670-03.pdf. Accessed August 19, 2015. [Google Scholar]
- 12. Conwell LJ, Cohen JW.. Characteristics of persons with high medical expenditures in the U.S. civilian noninstitutionalized population, 2002. Statistical Brief #73. March 2005. Agency for Healthcare Research and Quality, Rockville, MD. Available at: http://meps.ahrq.gov/mepsweb/data_files/publications/st73/stat73.pdf. Accessed August 19, 2015. [Google Scholar]
- 13. Substance Abuse and Mental Health Services Administration. . Results from the 2006 National Survey on Drug Use and Health: national findings. Office of Applied Studies, NSDUH Series H-32, DHHS Publication No. SMA 07-4293. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2007. Available at: https://www.asipp.org/documents/2006NSDUH.pdf. Accessed August 19, 2015. [Google Scholar]
- 14. American Psychiatric Association. . Substance-related and addictive disorders. 2013. Available at: http://www.dsm5.org/Documents/Substance%20 Use%20Disorder%20Fact%20Sheet.pdf. Accessed August 19, 2015.
- 15. Rice JB, White AG, Birnbaum HG, Schiller M, Brown DA, Roland CL.. A model to identify patients at risk for prescription opioid abuse, dependence, and misuse. Pain Med. 2012; 13(9): 1162-73. [DOI] [PubMed] [Google Scholar]
- 16. White AG, Birnbaum HG, Rothman DB, Katz N.. Development of a budget-impact model to quantify potential cost savings from prescription opioids designed to deter abuse or ease of extraction. Appl Health Econ Policy. 2009; 7(1): 61-70. [DOI] [PubMed] [Google Scholar]
- 17. Michna E, Kirson NY, Shei A, Birnbaum HG, Ben-Joseph R.. Use of prescription opioids with abuse-deterrent technology to address opioid abuse. Curr Med Res Opin. 2014; 30(8): 1589-98. [DOI] [PubMed] [Google Scholar]
- 18. Romano PS, Roos LL, Jollis JG.. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993; 46(10): 1075-79. [DOI] [PubMed] [Google Scholar]
- 19. White AG, Birnbaum HG, Mareva MN, et al. . Direct costs of opioid abuse in an insured population in the United States. J Manag Care Pharm. 2005; 11(6): 469-79. Available at: http://www.amcp.org/data/jmcp/3.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Becker WC, Sullivan LE, Tetrault JM, Desai RA, Fiellin DA.. Non-medical use, abuse and dependence on prescription opioids among U.S. adults: psychiatric, medical and substance use correlates. Drug Alcohol Depend. 2008; 94(1-3): 38-47. [DOI] [PubMed] [Google Scholar]
- 21. Jan SA. Patient perspective, complexities, and challenges in managed care. J Manag Care Pharm. 2010; 16(1 Suppl B): S22-25. Available at: http://www.amcp.org/data/jmcp/S22-S25.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Strassels SA. Economic burden of prescription opioid misuse and abuse. J Manag Care Pharm. 2009; 15(7): 556-62. Available at: http://www.amcp.org/data/jmcp/556-562.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fishbain D, Johnson S, Webster L, Greene L, Faysal J.. Review of regulatory programs and new opioid technologies in chronic pain management: balancing the risk of medication abuse with medical need. J Manag Care Pharm. 2010; 16(4): 276-87. Available at: http://www.amcp.org/data/jmcp/276-287.pdf. [DOI] [PMC free article] [PubMed] [Google Scholar]


