Abstract
BACKGROUND:
The prevalence and cost of subsequent fractures among patients with an incident fracture are not well defined.
OBJECTIVE:
To assess the prevalence of, and costs associated with, subsequent fractures in the year after an incident fracture.
METHODS:
This was a retrospective claims database analysis using data from Humana Medicare Advantage claims (Medicare group) and Optum Insight Clinformatics Data Mart commercial claims (commercial group). Patients included in the study had a claim for a qualifying fracture occurring between January 2008 and December 2013 (index fracture), were continuously enrolled in the health plan for ≥ 1 year before and after the index fracture, and were aged ≥ 65 years in the Medicare group or ≥ 50 years in the commercial group at the time of the index fracture. Subsequent fractures were identified by ICD-9-CM codes and were defined as the second fracture occurring ≥ 3 to ≤ 12 months after the index fracture (≥ 6 to ≤ 12 months for fractures at the same site as the index fracture). Rates of subsequent fractures were calculated as the number of patients who had a subsequent fracture divided by the total sample size. After propensity matching of demographic and clinical variables, we determined the total medical and pharmacy costs accrued within 1 year of the index fracture by patients with and without a subsequent fracture. Health care costs were compared between patients with and without a subsequent fracture using McNemar’s test.
RESULTS:
A total of 45,603 patients were included in the Medicare group, and 54,145 patients were included in the commercial group. In the Medicare group, 7,604 (16.7%) patients experienced a subsequent fracture. The proportion of patients with a subsequent fracture was highest among patients with multiple index fractures (26.2%, n = 905), followed by those with hip (25.5%, n = 1,280) and vertebral (20.2%, n = 1,908) index fractures. In the commercial group, 6,256 (11.6%) patients experienced a subsequent fracture. The proportion of patients with a subsequent fracture paralleled those observed in the Medicare group: 24.5% (n = 808) in patients with multiple index fractures, 22.0% (n = 525) in those with hip fracture, and 14.5% (n = 841) in those with vertebral fracture. For vertebral, hip, and nonhip nonvertebral fractures, subsequent fractures were most frequently of the same type as the index fracture. The mean total health care cost (sum of medical and pharmacy costs) in the year following the incident fracture for the Medicare group was $27,844 and differed significantly between patients with and without a subsequent fracture ($34,897 vs. $20,790; P < 0.001). The mean total health care cost in the year following the incident fracture for the commercial group was $29,316 and also differed significantly between patients with and without a subsequent fracture ($39,501 vs. $19,131; P < 0.001).
CONCLUSIONS:
Among patients with an incident fracture, those who experienced a subsequent fracture in the following year had significantly higher health care costs than those who did not. A subsequent fracture is most likely to be of the same type as the initial fracture.
What is already known about this subject
A history of osteoporotic fracture confers a heightened risk of experiencing a subsequent fracture.
The risk of a subsequent fracture varies according to the initial fracture type.
What this study adds
In the year following an incident fracture, a subsequent fracture is most likely to be of the same type as the initial fracture.
Among patients with an incident fracture, those who experienced a subsequent fracture in the following year had significantly higher health care costs than those who did not experience a subsequent fracture.
Osteoporosis represents a major health and economic issue in the United States. In 2010, the estimated prevalence of osteoporosis among U.S. men and women aged 50 years and older, based on bone mineral density of the lumbar spine and femoral neck, was 10.3%.1 Osteoporosis is characterized by low bone mass, deterioration of bone tissue, disruption of bone architecture, and compromised bone strength, all of which increase the risk of fracture. An estimated 50% of women and 20% of men in the United States will sustain an osteoporotic fracture in their lifetime.2 These fractures are accompanied by increased morbidity and mortality.3-5
A history of osteoporotic fracture confers a heightened risk of experiencing a subsequent fracture beyond that conferred by low bone mineral density (BMD). A 2004 meta-analysis reported that patients with a previous fracture had an 86% greater risk of experiencing a subsequent fracture than patients who had not experienced an incident fracture; the risk was 77% greater when BMD was taken into account.6 In the ongoing Dubbo Osteoporosis Epidemiology Study, the relative risk of subsequent fracture in Australian men and women with an incident low-trauma fracture was > 2.0 at all levels of BMD.7 In the Tromso Study in Norway, the age-adjusted relative risk of subsequent fracture was 1.3 in women and 2.0 in men (N = 27,000) with incident nonvertebral fractures.8 In a U.S. study of 30,000 Medicare beneficiaries who entered a nursing home in 2000, patients previously hospitalized with a hip fracture were at 3 times the risk of subsequent fractures (hazard ratio = 2.99), and those previously hospitalized with nonhip fractures were at nearly 2 times the risk (hazard ratio = 1.84).9 In U.S. studies of subsequent fracture, the incidence of subsequent fractures within a year of an incident fracture ranged from 4.0% to 35.2%, depending on index fracture type.10,11 The incidence of subsequent fracture within 2 years of an incident fracture was 11%, while 16.6%-41.7% of patients experienced a subsequent fracture within 5 years of an incident fracture.9,12 While the incidence of subsequent fractures has been previously studied, these results have only been reported through the year 2008.
The economic burden of osteoporotic fractures is well studied. A 2012 systematic review of U.S. studies published between 1990 and 2011 reported that, in the year following an osteoporotic fracture, medical costs were 1.6-6.2 times higher in patients with versus without a fracture, totaling up to $71,000 for a hip fracture and up to $68,000 for a vertebral fracture.13 However, the cost of a subsequent fracture occurring shortly after an initial fracture has only been reported in a few previous studies and only through the year 2008.10,11 Therefore, this study was carried out to determine the current prevalence and costs of osteoporotic fracture in Medicare and commercially insured U.S. men and women in the year after an initial fracture.
Methods
Data Source and Study Design
This was a retrospective claims analysis using data from 2 large U.S. administrative claims databases, both of which contain medical and pharmacy claims and laboratory test results. The Humana database includes patients with Medicare Advantage plans. The Optum Insight Clinformatics Data Mart is a nationwide database containing demographic, medical, and pharmacy data on commercially insured patients. All data were de-identified; therefore, patient informed consent and institutional review were not required.
The study period began on January 1, 2007, and ended on December 31, 2014. The index date was defined as the date of the first claim for a qualifying fracture between January 1, 2008, and December 31, 2013 (the index period). The 12 months immediately preceding the index date were defined as the pre-index period, and the 12 months following the index date were defined as the post-index period.
Study Sample
Patients in the Humana database constituted the Medicare group, and those in the Optum database were the commercial group. Eligible patients in the Medicare and commercial groups were aged ≥ 65 years and ≥ 50 years, respectively, with a fracture during the index period. Patients were required to be continuously enrolled in a health plan during the pre- and post-index periods.
Patients with a fracture in the pre-index period at the same site as the index fracture were excluded. Patients were also excluded if they had a diagnosis of metastatic cancer, bone cancer, multiple myeloma, osteomalacia, hypophosphatasia, osteogenesis imperfecta, benign bone tumors, primary or secondary hyperparathyroidism, vitamin D deficiency, Paget’s disease, or drug-induced osteoporosis in the pre-index period.
Study Variables and Outcomes
Qualifying index fractures were classified as vertebral, hip, nonhip nonvertebral (NHNV), or multiple and were identified by International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes (Appendix, available in online article). All fractures were closed. Vertebral fractures were defined as fractures of the spine, and hip fractures were defined as fractures of the upper femur. NHNV fractures were those of the ankle or foot; clavicle; femur; tibia or fibula; wrist, hand, or forearm (radius and ulna); humerus; patella; pelvis; scapula; or ribs. Multiple fractures were defined as fractures that occurred on the same date at more than 1 of the qualifying fracture sites.
Demographic characteristics assessed on the index date were age, sex, and geographic region of residence. Clinical characteristics assessed over the pre-index period were osteoporosis diagnosis (ICD-9-CM code 733.0x); use of osteoporosis medications (oral or injectable bisphosphonates [alendronate, risedronate, ibandronate, or zoledronic acid] or nonbisphosphonates [denosumab, raloxifene, or teriparatide]); fracture-related medications (i.e., analgesics including acetaminophen, nonsteroidal anti-inflammatory agents [NSAIDs], and opioids); gastroprotective agents (proton pump inhibitors, H2 receptor antagonists, or cytoprotectants); NSAIDs, glucocorticoids, or estrogen; history of falls (ICD-9-CM code V15.88); and gastrointestinal events. Gastrointestinal events were identified by ICD-9-CM and Current Procedural Terminology codes and included nausea/vomiting, dysphagia, and esophagitis; gastroesophageal reflux disease; ulcer, stricture, perforation, or hemorrhage of the esophagus; gastric, duodenal, or peptic ulcers; acute gastritis; duodenitis; and gastrointestinal hemorrhage. Pre-index comorbidities commonly observed in osteoporosis patients were identified by ICD-9-CM codes and included hypertension, arthritis, musculoskeletal pain, respiratory diseases, Alzheimer’s disease, dementia, depression, anxiety, sleep disorders, diabetes, cardiovascular diseases, and hypothyroidism. The Charlson Comorbidity Index score was calculated using a subset of 17 comorbidities as described by Deyo et al. (1992).14
A subsequent fracture was defined as any of the previously listed fracture codes occurring in the post-index period. A 3-month wash-out period (6 months if the subsequent fracture was at the same site as the index fracture) was imposed to ensure that the post-index fracture was not associated with follow-up treatment for the index fracture. The length of time used for the wash-out period was based on the assumption that most fractures heal in about 6 weeks. Therefore, doubling that time to 3 months would accommodate care related to slowly healing fractures. The 3-month duration was doubled again to 6 months for claims for the same skeletal site as the index fracture to provide assurance that the same fracture was not counted as a new one. Similar wash-out periods were reported in previous studies.10,11
Total annual health care costs were assessed during the post-index year and compared between patients with and without a subsequent fracture. Health care costs were determined for all causes (i.e., not limited to osteoporosis-specific resource use) and classified as medical or pharmacy. Medical costs were further subcategorized as outpatient services, emergency department visits, inpatient admissions, long-term care services, and “other” types of resource use. Outpatient services included claims for radiology, primary care, outpatient hospital visits, orthopedic specialist visits, and rehabilitation services. Long-term care services were defined as at least 1 long-term care stay in a rehabilitation or skilled nursing facility. Pharmacy costs included all prescription drug usage, with separate assessments of osteoporosis-related and fracture-related medications (as previously defined).
Statistical Analyses
Separate analyses were performed for the Medicare and commercial groups, with no comparisons between them. All analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC). Descriptive statistics (numbers and percentages or means and standard deviations [SDs]), were calculated for index and pre-index demographic and clinical characteristics. The proportion of patients experiencing a post-index fracture was defined as the number of patients who had a subsequent fracture divided by the total sample size and were calculated for the total study population, as well for patients with vertebral, hip, NHNV, and multiple index fractures. Chi-square analysis was used to test the hypothesis that, for vertebral, hip, and NHNV fractures, there was no relationship between the type of index fracture and the type of subsequent fracture. A P value < 0.05 was considered to be sufficient to prove the null hypothesis.
Because health care costs vary significantly across geographic regions of the United States, and also by medication use and comorbidities,15 1:1 propensity score matching was used to balance the clinical and demographic characteristics of subgroups of patients with and without post-index fractures. Patients with and without subsequent fractures were matched by their index fracture site, index date (± 1 year), age (± 3 years), gender, region, employment status (only available for the commercial group), race, and Charlson comorbidity score.
First, the association of index demographics and pre-index clinical characteristics with post-index fracture was determined using logistic regression. The regression coefficients were then used to generate propensity scores to match patients without a subsequent fracture to those with a subsequent fracture. Post-index health care costs were determined in the propensity-matched subgroups, and the costs of patients with versus without a subsequent fracture were compared using Wilcoxon signed-rank tests. Costs are reported in 2014 U.S. dollars, with costs from earlier years adjusted to 2014 using the Consumer Price Index for medical care.16
Results
Characteristics of the Study Population
The Medicare group consisted of 45,603 patients with a mean age of 78.1 years, and 28.1% were male (Table 1). Approximately one fifth of the Medicare group (18.2%) had used fracture-related medications in the pre-index period, and 11.7% were on osteoporosis medications. The mean age of the 54,145 patients in the commercial group was 61.8 years, and 37.9% were male (Table 2). Fracture-related medications and osteoporosis medications were used, respectively, by 19.8% and 8.5% of patients in this group.
TABLE 1.
Characteristics of Patients in the Medicare Groupa
| Overall (N = 45,603) | With Subsequent Fracture (n = 7,604) | Without Subsequent Fracture (n = 37,999) | P Value | |
|---|---|---|---|---|
| Index age (mean, SD) | 78.1 (10.6) | 80.1 (11.3) | 77.7 (10.4) | < 0.001 |
| Age group, years | < 0.001 | |||
| 65-69 | 10,292 (22.6) | 1,404 (18.5) | 8,888 (23.4) | |
| 70-79 | 19,498 (42.8) | 2,928 (38.5) | 16,570 (43.6) | |
| 80-89 | 9,281 (20.4) | 1,800 (23.7) | 7,481 (19.7) | |
| ≥ 90 | 6,532 (14.3) | 1,472 (19.4) | 5,060 (13.3) | |
| Sex | < 0.001 | |||
| Male | 12,828 (28.1) | 1,700 (22.4) | 11,128 (29.3) | |
| Female | 32,775 (71.9) | 5,904 (77.6) | 26,871 (70.7) | |
| Geographic region | < 0.001 | |||
| Midwest | 15,396 (33.8) | 2,240 (29.5) | 13,156 (34.6) | |
| Northeast | 1,252 (2.8) | 211 (2.8) | 1,041 (2.7) | |
| South | 23,390 (51.3) | 4,193 (55.1) | 19,197 (50.5) | |
| West | 5,565 (12.2) | 960 (12.6) | 4,605 (12.1) | |
| Osteoporosis diagnosis | 6,536 (14.3) | 1,421 (18.7) | 5,115 (13.5) | < 0.001 |
| Pre-index medication use | ||||
| Osteoporosis medications | 5,350 (11.7) | 1,100 (14.5) | 4,250 (11.2) | < 0.001 |
| Fracture-related medications | 8,317 (18.2) | 1,538 (20.2) | 6,779 (17.8) | < 0.001 |
| Gastroprotective agents | ||||
| PPI | 9,603 (21.1) | 1,784 (23.5) | 7,819 (20.6) | < 0.001 |
| H2 receptor antagonist | 2,179 (4.8) | 450 (5.9) | 1,729 (4.6) | < 0.001 |
| Cytoprotectant | 523 (1.2) | 121 (1.6) | 402 (1.1) | < 0.001 |
| NSAIDs | 9,931 (21.8) | 1,802 (23.7) | 8,129 (21.4) | < 0.001 |
| Glucocorticoids | 9,300 (20.4) | 1,714 (22.5) | 7,586 (20.0) | < 0.001 |
| Estrogens | 939 (2.1) | 143 (1.9) | 796 (2.1) | < 0.001 |
| Gastrointestinal events | 15,868 (34.8) | 2,904 (38.2) | 12,964 (34.1) | < 0.001 |
| History of falls | 3,493 (7.7) | 693 (9.1) | 2,800 (7.4) | < 0.001 |
| Charlson Comorbidity Index (mean, SD) | 0.64 (1.21) | 0.76 (1.32) | 0.62 (1.19) | < 0.001 |
| Common osteoporosis-related comorbiditiesb | ||||
| Hypertension | 32,751 (71.8) | 5,584 (73.4) | 27,167 (71.5) | 0.003 |
| Arthritis | 22,816 (50.0) | 4,192 (55.1) | 18,624 (49.0) | < 0.001 |
| Musculoskeletal pain | 16,867 (37.0) | 3,180 (41.8) | 13,687 (36.0) | < 0.001 |
| Respiratory diseases | 14,801 (32.5) | 2,665 (35.1) | 12,136 (31.9) | < 0.001 |
| Alzheimer’s disease, dementia, depression, anxiety, sleep disorders | 13,742 (30.1) | 2,758 (36.3) | 10,984 (28.9) | < 0.001 |
| Diabetes | 12,958 (28.4) | 2,249 (29.6) | 10,709 (28.2) | 0.048 |
| Cardiovascular diseases | 10,661 (23.4) | 1,956 (25.7) | 8,705 (22.9) | < 0.001 |
| Hypothyroidism | 9,388 (20.6) | 1,682 (22.1) | 7,706 (20.3) | < 0.001 |
aValues are presented as n (%) unless indicated otherwise.
bOnly comorbidities present in > 20% of patients are listed.
NSAID = nonsteroidal anti-inflammatory drug; PPI = proton pump inhibitor; SD = standard deviation.
TABLE 2.
Characteristics of Patients in the Commercial Groupa
| Overall (N = 54,145) | With Subsequent Fracture (n = 6,256) | Without Subsequent Fracture (n = 47,889) | P Value | |
|---|---|---|---|---|
| Index age (mean, SD) | 61.8 (8.9) | 64.1 (10.3) | 61.5 (8.6) | < 0.001 |
| Age groups, years | < 0.001 | |||
| 50-59 | 26,968 (49.8) | 2,653 (42.4) | 24,315 (50.8) | |
| 60-64 | 14,077 (26.0) | 1,495 (23.9) | 12,582 (26.3) | |
| 65-69 | 4,258 (7.9) | 523 (8.4) | 3,735 (7.8) | |
| 70-79 | 4,212 (7.8) | 636 (10.2) | 3,576 (7.5) | |
| 80-89 | 4,630 (8.6) | 949 (15.2) | 3,681 (7.7) | |
| ≥ 90 | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| Sex | < 0.001 | |||
| Male | 20,496 (37.9) | 2,040 (32.6) | 18,456 (38.5) | |
| Female | 33,647 (62.1) | 4,216 (67.4) | 29,431 (61.5) | |
| Geographic region | < 0.001 | |||
| Midwest | 17,436 (32.2) | 1,783 (28.5) | 15,653 (32.7) | |
| Northeast | 4,928 (9.1) | 618 (9.9) | 4,310 (9.0) | |
| South | 22,615 (41.8) | 2,696 (43.2) | 19,919 (41.6) | |
| West | 9,111 (16.8) | 1,150 (18.4) | 7,961 (16.6) | |
| Osteoporosis diagnosis | 3,412 (6.3) | 594 (9.5) | 2,818 (5.9) | < 0.001 |
| Pre-index medication use | ||||
| Osteoporosis medications | 4,581 (8.5) | 749 (12.0) | 3,832 (8.0) | < 0.001 |
| Fracture-related medications | 10,709 (19.8) | 1,365 (21.8) | 9,344 (19.5) | < 0.001 |
| Gastroprotective agents | ||||
| PPI | 7,875 (14.5) | 1,065 (17.0) | 6,810 (14.2) | < 0.001 |
| H2 receptor antagonist | 360 (0.7) | 54 (0.9) | 306 (0.6) | 0.122 |
| Cytoprotectant | 566 (1.1) | 86 (1.4) | 480 (1.0) | 0.025 |
| NSAIDs | 12,531 (23.1) | 1,601 (25.6) | 10,930 (22.8) | <0.001 |
| Glucocorticoids | 9,602 (17.7) | 1,284 (20.5) | 8,318 (17.4) | <0.001 |
| Estrogens | 2,569 (4.7) | 313 (5.0) | 2,256 (4.7) | 0.593 |
| Gastrointestinal events | 13,238 (24.5) | 1,768 (28.3) | 11,470 (24.0) | <0.001 |
| History of falls | 2,402 (4.4) | 344 (5.5) | 2,058 (4.3) | <0.001 |
| Charlson Comorbidity Index (mean, SD) | 0.71 (1.26) | 0.96 (1.50) | 0.67 (1.2) | <0.001 |
| Common osteoporosis-related comorbiditiesb | ||||
| Hypertension | 24,592 (45.4) | 3,221 (51.5) | 21,371 (44.6) | <0.001 |
| Arthritis | 20,026 (37.0) | 2,669 (42.7) | 17,357 (36.2) | <0.001 |
| Musculoskeletal pain | 15,434 (28.5) | 2,147 (34.3) | 13,287 (27.8) | <0.001 |
| Respiratory diseases | 12,505 (23.1) | 1,632 (26.1) | 10,873 (22.7) | <0.001 |
| Alzheimer’s disease, dementia, depression, anxiety, sleep disorders | 11,139 (20.6) | 1,601 (25.6) | 9,538 (19.9) | <0.001 |
aValues are presented as n (%) unless indicated otherwise.
bOnly comorbidities present in > 20% of patients are listed.
NSAID = nonsteroidal anti-inflammatory drug; PPI = proton pump inhibitor; SD = standard deviation.
In both groups, patients with a subsequent fracture were slightly older (80.1 years vs. 77.7 years in Medicare; 64.1 years vs. 61.5 years in commercial); were more frequently female (77.6% vs. 70.7% in Medicare; 67.4% vs. 61.5% in commercial); and were more often from the South (55.1% vs. 50.5% in Medicare; 43.2% vs. 41.6% in commercial; Tables 1-2; P < 0.001 for all comparisons). Patients with a subsequent fracture had higher rates of osteoporosis diagnosis (18.7% vs. 13.5% in Medicare; 9.5% vs. 5.9% in commercial) and of all types of medication use (Tables 1-2). The Charlson Comorbidity Index score was higher in patients with a subsequent fracture (0.76 vs. 0.62 in Medicare; 0.96 vs. 0.67 in commercial; P < 0.001 for both comparisons), and all reported comorbidities were more prevalent in patients with subsequent fractures (Tables 1-2).
Prevalence of Subsequent Fractures
In the Medicare group, 16.7% of patients (7,604 of 45,603) experienced a subsequent fracture (Table 3). Subsequent fractures were most common among patients with multiple index fractures (26.2%), followed by those with hip (25.5%) and vertebral (20.2%) index fractures. However, NHNV fractures were the most frequent type of fracture as both the index fracture (27,657 of 45,603 patients; 60.6%) and subsequent fractures (3,511 of 7,604 patients; 46.2%). Among patients with vertebral, hip, and NHNV fractures, the subsequent fracture was more frequently of the same type as the index fracture than of another type (P < 0.001; Table 3). Patients with multiple index fractures were more likely to have an NHNV fracture in the post-index period than any other fracture type (Table 3).
TABLE 3.
Subsequent Fracture Rates, by Type of Index Fracturea
| Subsequent Fractureb | ||||||
|---|---|---|---|---|---|---|
| Overall | Vertebral | Hip | NHNV | Multiple | ||
| Index fracture | Medicare, n (%) | |||||
| Overall (N = 45,603) | 7,604 (16.7) | 1,746 (3.8) | 1,256 (2.8) | 3,260 (7.2) | 1,342 (2.9) | |
| Vertebral (n = 9,465) | 1,908 (20.2) | 1,235 (13.1) | 101 (1.1) | 315 (3.3) | 257 (2.7) | |
| Hip (n = 5,024) | 1,280 (25.5) | 84 (1.7) | 719 (14.3) | 257 (5.1) | 220 (4.4) | |
| NHNV (n = 27,657) | 3,511 (12.7) | 354 (1.3) | 228 (0.8) | 2,351 (8.5) | 578 (2.1) | |
| Multiple (n = 3,457) | 905 (26.2) | 73 (2.1) | 208 (6.0) | 337 (9.8) | 287 (8.3) | |
| Commercial, n (%) | ||||||
| Overall (N = 54,145) | 6,256 (11.6) | 838 (1.6) | 502 (0.9) | 4,080 (7.5) | 836 (1.5) | |
| Vertebral (n = 5,799) | 841 (14.5) | 576 (9.9) | 29 (0.5) | 136 (2.4) | 100 (1.7) | |
| Hip (n = 2,385) | 525 (22.0) | 18 (0.8) | 292 (12.2) | 114 (4.8) | 101 (4.2) | |
| NHNV (n = 42,666) | 4,082 (9.6) | 192 (0.5) | 96 (0.2) | 3,405 (8.0) | 389 (0.9) | |
| Multiple (n = 3,295) | 808 (24.5) | 52 (1.6) | 85 (2.6) | 425 (12.9) | 246 (7.5) | |
aBold font highlights the propensity of the subsequent fracture to be the same type as the index fracture.
bAccording to chi-square analysis, the probability that there is not a relationship between the type of index fracture and the type of subsequent fracture is < 0.001 (for vertebral, hip, and NHNV fractures types only).
NHNV = nonhip nonvertebral.
In the commercial group, 11.6% of patients (6,256 of 54,145) experienced a subsequent fracture (Table 3). Subsequent fractures were most common among patients with multiple index fractures (24.5%) and hip index fractures (22.0%). Other results showed the same trends as in the Medicare group (i.e., NHNV was the most common fracture type, and subsequent fractures tended to be the same type as the index fracture; Table 3).
Cost of Subsequent Fractures
Propensity matching of demographic and clinical characteristics between patients with and without a subsequent fracture produced a well-matched subset of patients in the Medicare and commercial groups (Table 4). With these characteristics equalized, health care resource use and its associated costs in the year following the incident fracture were assessed.
TABLE 4.
Matched Characteristics of Patients with and Without Subsequent Fracturesa
| Medicare Groupb | Commercial Groupc | |||||
|---|---|---|---|---|---|---|
| With Subsequent Fracture (n = 7,604) | Without Subsequent Fracture (n = 7,604) | P Value | With Subsequent Fracture (n = 4,549) | Without Subsequent Fracture (n = 4,549) | P Value | |
| Index age (mean, SD) | 80.07 (11.25) | 80.09 (11.34) | 0.940 | 61.84 (8.73) | 61.65 (8.74) | 0.310 |
| Age group, years | ||||||
| 50-59 | - | - | 2,238 (49.2) | 2,284 (50.2) | 0.997 | |
| 60-64 | - | - | 1,219 (26.8) | 1,181 (26.0) | ||
| 65-69 | 1,404 (18.5) | 1,406 (18.5) | 0.995 | 362 (8.0) | 355 (7.8) | |
| 70-79 | 2,928 (38.5) | 2,883 (37.9) | 362 (8.0) | 362 (8.0) | ||
| 80-89 | 1,800 (23.7) | 1,833 (24.1) | 368 (8.1) | 367 (8.1) | ||
| ≥ 90 | 1,472 (19) | 1,482 (19.5) | - | - | ||
| Sex | ||||||
| Male | 1,700 (22.4) | 1,709 (22.5) | 0.985 | 1,606 (35.3) | 1,642 (36.1) | 0.733 |
| Female | 5,904 (77.6) | 5,895 (77.5) | 2,943 (64.7) | 2,907 (63.9) | ||
| Geographic region | ||||||
| Midwest | 2,240 (29.5) | 2,256 (29.7) | 0.986 | 1,356 (29.8) | 1,302 (28.6) | 0.677 |
| Northeast | 211 (2.8) | 200 (2.6) | 442 (9.7) | 436 (9.6) | ||
| South | 4,193 (55.1) | 4,157 (54.7) | 1,952 (42.9) | 2,045 (45.0) | ||
| West | 960 (12.6) | 991 (13.0) | 799 (17.6) | 766 (16.8) | ||
| Index fracture type | ||||||
| Vertebral | 1,908 (25.1) | 1,972 (25.9) | 0.492 | 527 (11.6) | 546 (12.0) | 0.826 |
| Hip | 1,280 (16.8) | 1,267 (16.7) | 0.961 | 162 (3.5) | 167 (3.7) | 0.961 |
| NHNV | 35,11 (46.2) | 3,484 (45.8) | 0.908 | 3,647 (80.2) | 3,622 (79.6) | 0.807 |
| Multiple | 905 (11.9) | 881 (11.6) | 0.833 | 213 (4.7) | 214 (4.7) | 0.999 |
| Osteoporosis diagnosis | 1,421 (18.7) | 1,460 (19.2) | 0.722 | 311 (6.8) | 285 (6.3) | 0.545 |
| Pre-index medication use | ||||||
| Osteoporosis medications | 1,100 (14.5) | 1,120 (14.7) | 0.900 | 400 (8.8) | 395 (8.7) | 0.983 |
| Fracture-related medications | 1,538 (20.2) | 1,547 (20.3) | 0.984 | 983 (21.6) | 977 (21.5) | 0.988 |
| Gastroprotective agents | ||||||
| PPI | 1,784 (23.5) | 1,768 (23.3) | 0.954 | 686 (15.1) | 701 (15.4) | 0.909 |
| H2 receptor antagonist | 450 (5.9) | 428 (5.6) | 0.746 | 38 (0.8) | 27 (0.6) | 0.392 |
| Cytoprotectant | 121 (1.6) | 98 (1.3) | 0.294 | 47 (1.0) | 43 (1.0) | 0.914 |
| NSAIDs | 1,802 (23.7) | 1,799 (23.7) | 0.998 | 1,149 (25.3) | 1,154 (25.4) | 0.993 |
| Glucocorticoids | 1,714 (22.5) | 1,750 (23.0) | 0.785 | 859 (18.9) | 859 (18.9) | 1.000 |
| Estrogens | 143 (1.9) | 147 (1.9) | 0.972 | 232 (5.1) | 218 (4.8) | 0.795 |
| Gastrointestinal events | 2,904 (38.2) | 2,854 (37.5) | 0.705 | 1,141 (25.1) | 1,115 (24.5) | 0.819 |
| History of falls | 693 (9.1) | 678 (8.9) | 0.914 | 205 (4.5) | 189 (4.2) | 0.712 |
| Charlson Comorbidity Index score | ||||||
| 0 | 4,814 (63.3) | 4,846 (63.7) | 0.986 | 2,770 (60.9) | 2,810 (61.8) | 0.914 |
| 1 | 1,360 (17.9) | 1,353 (17.8) | 1,046 (23.0) | 1,006 (22.1) | ||
| 2 | 669 (8.8) | 636 (8.4) | 340 (7.5) | 321 (7.1) | ||
| ≥ 3 | 761 (10.0) | 769 (10.1) | 393 (8.6) | 412 (9.1) | ||
| Common osteoporosis-related comorbidities | ||||||
| Hypertension | 5,584 (73.4) | 5,557 (73.1) | 0.885 | 2,123 (46.7) | 2,095 (46.1) | 0.841 |
| Arthritis | 4,192 (55.1) | 4,178 (54.9) | 0.974 | 1,770 (38.9) | 1,748 (38.4) | 0.894 |
| Musculoskeletal pain | 3,180 (41.8) | 3,217 (42.3) | 0.831 | 1,365 (30.0) | 1,420 (31.2) | 0.457 |
| Alzheimer’s disease, dementia, depression, anxiety, sleep disorders | 2,758 (36.3) | 2,722 (35.8) | 0.831 | 1,012 (22.3) | 993 (21.8) | 0.891 |
| Respiratory diseases | 2,665 (35.0) | 2,650 (34.9) | 0.968 | 1,093 (24.0) | 1,082 (23.8) | 0.964 |
| Diabetes | 2,249 (29.6) | 2,202 (29.0) | 0.704 | 824 (18.1) | 793 (17.4) | 0.697 |
| Cardiovascular diseases | 1,956 (25.7) | 1,958 (25.8) | 0.999 | 474 (10.4) | 454 (10.0) | 0.787 |
| Hypothyroidism | 1,682 (22.1) | 1,692 (22.3) | 0.981 | 580 (12.8) | 551 (12.1) | 0.654 |
| All health care costs, mean (SD), $ | 10,577 (18,566) | 10,287 (17,041) | 0.316 | 13,185 (28,070) | 12,079 (27,105) | 0.056 |
aValues are presented as n (%) unless indicated otherwise.
bThe Medicare group was also matched on race (white, black, or other).
cThe commercial group was also matched on health plan type (EPO, HMO, IND, OTH, POS, or PPO).
EPO = exclusive provider organization; HMO = health maintenance organization; IND = individual; NSAID = nonsteroidal anti-inflammatory drug; OTH = other; POS = point of service; PPI = proton pump inhibitor; PPO = preferred provider organization; SD = standard deviation.
During the post-index period, Medicare patients with a subsequent fracture had a greater median number of outpatient visits than patients without a subsequent fracture (21 vs. 15). The percentages of patients with emergency department visits (83.5% vs. 69.6%), inpatient admissions (72.5% vs. 53.4%), and long-term care (45.6% vs. 28.4%) were significantly greater in patients with versus without subsequent fractures (P < 0.001 for all comparisons). Similarly, patients in the commercial group who had subsequent fractures had a higher median number of outpatient visits during the post-index period (29 vs. 16 in those without subsequent fractures). Emergency department visits (13.7% vs. 11.6%; P = 0.014), inpatient admissions (38.3% vs. 20.7%; P < 0.001), and long-term care (12.4% vs. 6.1%; P < 0.001) were more common among commercial patients with versus without subsequent fractures.
The mean (SD) total cost (the sum of all medical and pharmacy costs) for Medicare patients in the year after an incident fracture was $27,844 ($16,827) and differed significantly between patients with and without subsequent fractures ($34,897 [$36,181] vs. $20,790 [$28,257]; P < 0.001; Figure 1A). Total (mean [SD]) medical costs differed significantly between patients with and without subsequent fractures ($32,585 [$35,623] vs. $18,770 [$27,727]; P < 0.001; data not shown). Costs for outpatient services, emergency department visits, inpatient admissions, long-term care services, and other costs were all significantly higher in patients with subsequent fractures (P < 0.001; Figure 1A) with the largest differentials observed for inpatient admissions and long-term care services. Total pharmacy costs also differed significantly, with patients with subsequent fractures incurring higher costs than patients without subsequent fractures (P < 0.001; Figure 1A).
FIGURE 1.
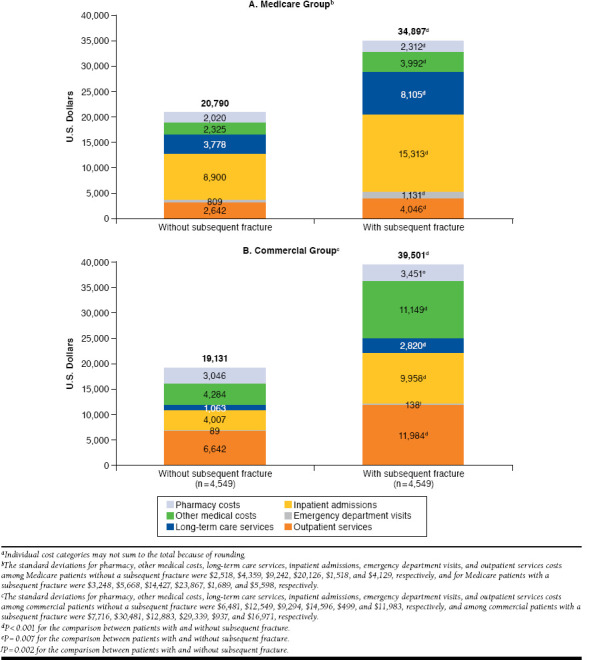
Mean Per-Patient Costs for Patients in the MedicareCommercial Groupsa
The mean (SD) total cost for patients in the commercial group in the year after an incident fracture was $29,316 ($54,552) and differed significantly between patients with and without subsequent fractures ($39,501 [$67,553] vs. $19,131 [$34,374]; P < 0.001; Figure 1B). Total (mean [SD]) medical costs were nearly $20,000 higher in patients with subsequent fractures ($36,050 [$66,484] vs. $16,085 [$33,042]; P < 0.001; data not shown), an increment attributable to significant differences in outpatient services, inpatient admissions, and other costs (Figure 1B). As with the Medicare group, pharmacy costs were slightly but significantly higher among patients with subsequent fractures (P < 0.01; Figure 1B).
Discussion
In this analysis of U.S. women and men with osteoporotic fractures, 16.7% of Medicare patients and 11.6% of commercially insured patients experienced a subsequent fracture in the following year. Subsequent fractures were most common among patients with multiple index fractures or hip index fractures. Total medical and pharmacy costs in the year following the index fracture were $14,100 higher in Medicare patients and $20,370 higher in commercially insured patients with a subsequent fracture, compared with those without a subsequent fracture.
Previous U.S. studies of subsequent fractures have assessed different patient populations and fracture types. Pike et al. (2011) determined the prevalence of subsequent fractures in Medicare and privately insured patients, similar to our study, but focused exclusively on nonvertebral fractures.11 However, the study by Pike et al. differs from our study because it included Medicare patients aged 65 years and older and privately insured patients aged 18-64 years. In that study, overall rates of nonvertebral subsequent fractures were 22.6% in the Medicare patients and 14.1% in the privately insured patients. In another U.S. study of Medicare and commercially insured patients, rates of subsequent fracture in the year following an initial hip, vertebral, or NHNV fracture were 8.0%, 5.1%, and 4.0%, respectively, in the commercially insured cohort and 8.8%, 9.2%, and 8.2%, respectively, in the Medicare cohort.10 Our findings are consistent with this study’s findings in that the Medicare cohort in our study had higher rates of subsequent fractures than the commercially insured cohort, which may be related to the higher average age of Medicare versus commercially insured patients.
Other previous analyses of Medicare patients determined subsequent fracture rates according to the type of the first fracture. Using Medicare data from 1999-2006, Curtis et al. (2010) reported the risk (i.e., cumulative incidence) of any subsequent fracture within 5 years of an incident fracture to be 33.4%-39.4% in patients with an incident vertebral fracture, 22.5%-25.5% in patients with an incident hip fracture, and 20.5%-32.6% in patients with an incident radius/ulna fracture (the ranges come from different age groups).12 Among Medicare patients aged 50 years or older admitted to a nursing home in the year 2000 with a history of hospitalization for hip or non-hip fracture in the previous 4 years, 23.9% of those with a previous hip fracture and 15.1% of those with a previous nonhip fracture were rehospitalized for a subsequent fracture within 2 years of admission.9 Our finding that subsequent fractures were more common among Medicare patients with an initial hip fracture than any other type of initial fracture (other than multiple sites) is in agreement with the latter of these 2 studies.9 Our results also show the types of subsequent fractures experienced by Medicare patients with initial vertebral, hip, and NHNV fractures.
The increased risk of subsequent fracture conferred by an incident fracture is well established.6,7 Previous studies also demonstrate that the risk of a subsequent fracture varies according to the initial fracture type.17 Our results suggest that the type of incident fracture is predictive of a subsequent fracture of the same type. Support for this finding comes from the Pike et al. study, in which a “majority of subsequent fractures occurred at the same site as the index fracture.”11 Indeed, repeat fractures at the index site constituted 69.2% of subsequent fractures in their privately insured cohort and 89.7% of subsequent fractures in their Medicare cohort.11 In contrast, in a study of 2002-2008 medical and pharmacy claims of commercially insured U.S. patients and Medicare beneficiaries aged 50 years or older, NHNV fractures were the most frequent type of subsequent fracture regardless of the type of incident fracture (i.e., even for patients with incident hip and vertebral fractures).10
The cost of osteoporosis-related fractures in the United States has been systematically reviewed.13 Based on studies published between 1990 and 2011, in the year after a fracture, medical costs (including hospitalization) were 1.6-6.2 times higher in patients with a fracture than in those without a fracture, and mean fracture costs ranged from $3,884 to $27,730.13
Studies of the costs following a subsequent fracture in the United States are comparatively few. In the Pike et al. study, mean excess costs in patients with a subsequent fracture in the year following an incident fracture were $12,527 in Medicare patients and $9,789 in privately insured patients.11 These differentials are smaller than those observed in our study ($14,100 in the Medicare group and $20,370 in the commercial group). The difference is likely due in part to inflation (our costs are in 2014 U.S. dollars, whereas costs from Pike et al. were in 2006 U.S. dollars) but perhaps more likely because of methodological differences in adjustment for covariates. Pike et al. matched patients with and without subsequent fractures on fracture type, index year, age, gender, geographic region, employment status (privately insured only), and race (Medicare only).11 Our propensity score matching accounted for these variables (except index year and employment status) plus medication and comorbidities, which may contribute greatly to the differences in cost between patients with and without osteoporotic fractures.15 Osteoporosis-related comorbidities, for example, were shown by Pike et al.11 and Song et al. (2011)10 to be more frequent among patients with a subsequent fracture, so matching for comorbidities is essential for calculating cost differences between patients with and without subsequent fractures.
Both Pike et al. and Song et al. assessed the cost of subsequent fractures according to the type of the index fracture in the year after the index fracture. In the Medicare cohort of Pike et al., “patients with index fractures of the femur had the greatest excess costs ($19,107), followed by those with fractures in multiple sites ($16,290).”11 (The privately insured cohort was not assessed due to small sample sizes.) In Song et al., excess costs due to a subsequent fracture were higher in commercially insured patients with an index hip fracture ($47,351) or vertebral fracture ($43,238) versus an NHNV fracture ($23,852) but about the same for Medicare patients with a hip ($18,645), vertebral ($19,702), or NHNV index fracture ($19,697).10 Clearly, many methodological factors, cohort matching, types of costs, and the time frame of the cost calculation influence these cost calculations. More specifically, Song et al. assessed 1-year costs associated with a subsequent fracture among patients aged 50 years and older who initially suffered a closed hip, vertebral, or NHNV fracture and did not include patients experiencing multiple fractures.10 The wash-out period in this study was only 14 days for patients experiencing fractures at different sites.10 This shorter wash-out period may have resulted in counting a post-index fracture that was associated with follow-up treatment for the index fracture.
In addition, Song et al. assessed the 2008 costs of inpatient services, emergency department visits, outpatient services (nursing home and rehabilitation services), and pharmacy costs but did not include long-term care.10 In the Pike et al. study, patients aged 18-64 years (commercially insured) or 65 years and older (Medicare) were enrolled after a nonvertebral fracture.11 This study did not include patients with other types of osteoporosis-related fractures.11 Furthermore, the study also looked at the 2006 costs associated with a subsequent fracture.11 Despite such methodological differences, however, the drivers of the excess cost were the same in our study as in the Song et al. and Pike et al. studies: hospital admissions and long-term care in the Medicare group and hospital admissions and outpatient visits in the private/commercial group.10,11
Limitations
A number of limitations should be considered when interpreting the results of our study. First, analyses of administrative claims data depend on correct diagnosis, procedure, and drug codes, and coding inaccuracies may lead to case misidentification. In addition, it is possible that patients aged 65 years and older in the commercial group were on a Medicare supplemental plan. Using an administrative claims database prohibited us from knowing this information.
Second, the definition of subsequent fractures may vary from study to study. In this case, the application of 3-month and 6-month wash-out periods before identification of subsequent fractures may have excluded some patients with a second incident fracture within those time frames. This would have led to an underestimation of the frequency of subsequent fracture but would likely not have affected the mean cost values, since all fracture types were subject to the same wash-out periods.
Third, as previously noted, the methods of cost assessment greatly influenced the cost calculations. In this regard, application of the wash-out periods meant that costs collected during the post-index year were not all necessarily related to the post-index fracture. In addition, costs may have varied across fracture types, but our cost analysis did not distinguish between patients with different fracture types. Patients with multiple fractures likely had higher costs than those with a single fracture. Although this distinction was not accounted for in the analysis, patients with multiple fractures were a small percentage of the study population (< 4% in both groups), so their influence on the mean cost values may have been offset by their small numbers. In addition, the cost results for the commercial group presented in this study are only generalizable to the roughly 70% (4,549 of 6,256) of patients who were able to be propensity-score matched to patients without a subsequent fracture.
Fourth, this study is also limited by its generalizability to patients who were continuously enrolled in a health plan for at least 2 years (1 year before and after the index fracture). In addition, census-tract level socioeconomic variables were not available in the databases, so we could not adjust the costs for these variables. However, we did adjust for geographic region and race. Finally, we did not measure patient adherence, so the effect of adherence to anti-osteoporosis medication on subsequent fractures and their associated costs was not ascertained.
Conclusions
This side-by-side analysis of Medicare beneficiaries and commercially insured adults in the United States showed that rates of refracture range up to 25% in patients with an initial osteoporotic fracture, depending on the type of initial fracture. In the year after the initial fracture, all-cause medical and pharmacy costs were significantly higher in patients with a subsequent fracture versus those without a subsequent fracture.
Acknowledgments
The authors thank Melissa Stauffer, PhD, and Anna Kaufman, MPH, in collaboration with ScribCo, for medical writing assistance.
APPENDIX. ICD-9-CM Codes for Qualifying Fractures
| Fracture Site | ICD-9-CM Code |
|---|---|
| Spine | 733.13 (pathologic), 805.2x (dorsal/thoracic, closed), 805.4x (lumbar, closed), 805.6x (sacral/coccygeal, closed), 805.8x (unspecified, closed) |
| Hip | 733.14 (pathologic), 820.0x (transcervical), 820.2x (pertrochanteric), 820.8x (unspecified), 820 (closed/open not indicated) |
| Ankle or foot | 824.0x (medial malleolus), 824.2x (lateral malleolus), 824.4x (bimalleolar), 824.6x (trimalleolar), 824.8x (unspecified), 825.25 (metatarsal), 733.94 (stress fracture: metatarsal) |
| Clavicle | 810.0x (closed), 810 (closed/open not indicated) |
| Femur | 733.15 (pathologic), 821.0x (shaft/unspecified), 821 (closed/open not indicated), 820.22 (subtrochanteric femur), 733.15 (stress fracture) |
| Tibia or fibula | 733.16 (pathologic), 733.93, 823.0x (upper end), 823.2x (shaft), 823.8x (unspecified), 823 (closed/open not indicated), 733.93 (stress fracture) |
| Wrist, hand, or forearm | 733.12 (pathologic), 813.0x (radius/ulna upper end), 813.2x (radius/ulna shaft), 813.4x (radius/ulna lower end), 813.8x (unspecified), 814.0x (carpal bones), 813 (closed/open not indicated), 815.02 (metacarpal) |
| Humerus | 733.11 (pathologic), 812.0x (upper end), 812.2x (shaft/unspecified), 812.4x (lower end), 812 (closed/open not indicated) |
| Patella | 822.0x (patella, closed) |
| Pelvis | 808.0x (acetabulum), 808.2x (pubis), 808.4x (other specified), 808.8x (unspecified), 808 (closed/open not indicated) |
| Scapula | 811.00 (closed/unspecified), 811.01 (acromial process), 811.02 (coracoid process), 811.03 (glenoid cavity and neck of scapula), 811.09 (closed fracture of scapula, other) |
| Ribs | 807.01 (one rib), 807.02 (two ribs), 807.09 (multiple ribs) |
ICD-9-CM = International Classification of Diseases, Ninth Revision, Clinical Modification.
References
- 1.Wright NC, Looker AC, Saag KG, et al. . The recent prevalence of osteoporosis and low bone mass in the United States based on bone mineral density at the femoral neck or lumbar spine. J Bone Miner Res. 2014;29(11):2520-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cosman F, de Beur SJ, LeBoff MS, et al. . Clinician’s guide to prevention and treatment of osteoporosis. Osteoporos Int. 2014;25(10):2359-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Abrahamsen B, van Staa T, Ariely R, Olson M, Cooper C. Excess mortality following hip fracture: a systematic epidemiological review. Osteoporos Int. 2009;20(10):1633-50. [DOI] [PubMed] [Google Scholar]
- 4.Bliuc D, Nguyen ND, Milch VE, et al. . Mortality risk associated with lowtrauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301(5):513-21. [DOI] [PubMed] [Google Scholar]
- 5.Nazrun AS, Tzar MN, Mokhtar SA, Mohamed IN. A systematic review of the outcomes of osteoporotic fracture patients after hospital discharge: morbidity, subsequent fractures, and mortality. Ther Clin Risk Manag. 2014;10:937-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kanis JA, Johnell O, De Laet C, et al. . A meta-analysis of previous fracture and subsequent fracture risk. Bone. 2004;35(2):375-82. [DOI] [PubMed] [Google Scholar]
- 7.Bliuc D, Alarkawi D, Nguyen TV, Eisman JA, Center JR. Risk of subsequent fractures and mortality in elderly women and men with fragility fractures with and without osteoporotic bone density: the Dubbo Osteoporosis Epidemiology Study. J Bone Miner Res. 2015;30(4):637-46. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed LA, Center JR, Bjornerem A, et al. . Progressively increasing fracture risk with advancing age after initial incident fragility fracture: the Tromso study. J Bone Miner Res. 2013;28(10):2214-21. [DOI] [PubMed] [Google Scholar]
- 9.Lyles KW, Schenck AP, Colon-Emeric CS. Hip and other osteoporotic fractures increase the risk of subsequent fractures in nursing home residents. Osteoporos Int. 2008;19(8):1225-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Song X, Shi N, Badamgarav E, et al. . Cost burden of second fracture in the U.S. health system. Bone. 2011;48(4):828-36. [DOI] [PubMed] [Google Scholar]
- 11.Pike CT, Birnbaum HG, Schiller M, et al. . Prevalence and costs of osteoporotic patients with subsequent non-vertebral fractures in the U.S. Osteoporos Int. 2011;22(10):2611-21. [DOI] [PubMed] [Google Scholar]
- 12.Curtis JR, Arora T, Matthews RS, et al. . Is withholding osteoporosis medication after fracture sometimes rational? A comparison of the risk for second fracture versus death. J Am Med Dir Assoc. 2010;11(8):584-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Budhia S, Mikyas Y, Tang M, Badamgarav E. Osteoporotic fractures: a systematic review of U.S. healthcare costs and resource utilization. Pharmacoeconomics. 2012;30(2):147-70. [DOI] [PubMed] [Google Scholar]
- 14.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613-19. [DOI] [PubMed] [Google Scholar]
- 15.Orsini LS, Rousculp MD, Long SR, Wang S. Health care utilization and expenditures in the United States: a study of osteoporosis-related fractures. Osteoporos Int. 2005;16(4):359-71. [DOI] [PubMed] [Google Scholar]
- 16.U.S. Department of Labor . Databases, tables & calculators by subject. Consumer Price Index-all urban consumers. Available at: https://www.bls.gov/data/. Accessed June 15, 2016.
- 17.Center JR, Bliuc D, Nguyen TV, Eisman JA. Risk of subsequent fracture after low-trauma fracture in men and women. JAMA. 2007;297(4):387-94. [DOI] [PubMed] [Google Scholar]


