Abstract
Preparing lay Community Health Ambassadors (CHA) to assess, document and monitor physical activity using standardized instruments can be daunting. Administering some instruments needs specialized training. System for Observing Play and Recreation in Communities (SOPARC) is a standardized instrument requiring extensive training. The question guiding this project was: Can lay Community Health Ambassadors (CHA) be trained to administer SOPARC at Racial and Ethnic Approaches to Community Health (REACH) physical activity fitness sites? This manuscript presents the process undertaken to train Community Health Ambassadors (CHAs) and some preliminary results. Preliminary results are that fifty-six (56) Community Health Ambassadors (CHAs) representing four (4) community partner groups were certified in the SOPARC training. These CHAs successfully documented pre/post data for 20 different physical activity sites. Additionally, the results support the premise that Community Health Ambassadors are a viable liaison in community health delivery.
Keywords: Community Health Ambassadors, Physical Activity, SOPARC
Introduction
An emerging group of healthcare para-professionals with varying degrees of training working with an ever widening group of individual and community group members continues to gain notability. The para-professional’s prominence correlates directly with their success as health care liaisons. These individuals are variably called, Community Health Workers [1], Community Health Navigators [2], Community Health Ambassadors [3,4], Community Ambassadors [5], Health Worker [6], Patient Navigators [7,8,9], Nurse Navigators [10], and Mental Health Ambassadors [11]. Regardless of different roles, these health care liaisons are generally members of, or knowledgeable about communities they serve. They commonly help link community members to healthcare resources and healthcare and healthcare providers.
Our project trained Community Health Ambassadors (CHAs) to promote physical activity through policy, systems and environmental changes at their respective community sites. CHAs were members of faith-based organizations, public housing towers, a federally qualified health center and the Urban League, all of Omaha, Nebraska. The project is the Center for Promoting Health and Health Equity-Racial and Ethnic Approaches to Community Health (CPHHE-REACH), funded in a cooperative agreement with the Centers for Disease Control and Prevention (CDC). CPHHE is a community-academic partnership housed at Creighton University of Omaha, Nebraska [12].
A CPHHE-REACH assessment aim was to document physical activity through an established instrument: the System for Observing Play and Recreation in Communities (SOPARC). However, we found no description of how to train lay CHAs to administer SOPARC. We wanted CPHHE-REACH CHAs to use SOPARC to assess, document the use of and monitor physical activity in local community churches, low-income residential housing towers, a federally qualified health center, the Urban League and local after-school programs.
Literature Review: Liaison Roles and Results
To set further background for our study, we next summarize what some health liaisons do. Community Health Workers (CHWs) are one major group. The Occupational Outlook Handbook [1], states that CHWs can:
Assess health needs,
Develop program and materials,
Teach people to manage existing health conditions,
Help people find services,
Advocate for improved health services and resources,
Discuss concerns with individuals and community,
Collect data,
Provide training and
Report findings
To provide these services CHWs draw on local and cultural knowledge, among other things. Although varied, CHW work has similarities. For example, CHWs were trained to provide education, encouragement and monitoring support for family members with type-2 diabetes and cardiovascular disease [3]. Through home visits, CHW’s “followed participants’ nutrition, physical activity, blood pressure, glucose levels and BMI” (p.21). In another project, trained “Community Ambassadors” (CAs) provided “late-life acculturation” support to South Asian American families who had elders living with them or in close proximity [5]. CAs volunteers took a 40-hour training primarily addressing “information referral and counseling services” (p.1771). The CAs’ success was partly because they established polygonal (three sided)-triadic (three group) relationships with the elders and family members (p. 1773). CAs sometimes provide service to both elders, and their families. CAs also helped Asian elders negotiate a complex network of social and health-care professionals. Other factors in CAs’ success in promoting successful acculturation were their training and familiarity to community members.
In another effort, Nurse Health Workers (NHWs) improved cardiac treatment outcomes as members of multidisciplinary teams [6]. These NHWs were integral in recruiting, selection, training and compensation processes. They provided cardiovascular education, telephone pre-appointment calls, re-contact calls for patients missing appointments, and took blood pressures and pulse rates. Their work vitally linked service providers and patients promoting improved health outcomes. For example, a high percentage of patients achieved blood pressure control after 12 months of interdisciplinary team efforts [6].
Further publications demonstrate Patient Navigators’ (PNs) substantial contributions in Oncology and Diabetic care [7,9]. For diabetes, Loskutova, et al. [9] reported that PNs were “selected and trained via electronic webinars on patient-centeredness, motivational interviewing, individualized care and communication and tracking” (p.80). These PNs provided telephonic services, used motivational interviewing skills, gave regular and accurate feedback to primary care providers and helped patients access appointments.
Oncology PNs require further specialized knowledge and skills. Pratt-Chapman et al. [7] designed a set of core competencies to standardize Oncology PN training. The set employed eight (8) competency domains identified by the Association of American Medical Colleges’ (AAMC) accreditation body, the Accreditation Council for Graduate Medical Education (ACGME).
Training for such health care liaisons (CHA, CHW, PN, etc.) continues expanding. These para-professionals bridge gaps among physician, nurse and patient. The liaisons also facilitate links to resources and information. We now turn to our specific project of training CHAs to use SOPARC in assessing, observing and monitoring physical activities in the Omaha community.
Our study of African-Americans in our community
African-Americans in Douglas County, Nebraska (most of the Omaha area) experience above-average incidence of death and disability from chronic diseases, particularly cardiovascular disease [12]. Increasing physical activity (PA) can prevent and ameliorate chronic diseases [13–15]. Given PA’s potential benefits, CPHHE-REACH’s innovative coalition of university and community partners works to eliminate physical activity barriers, promoting PA opportunities for African Americans in the Douglas County community [12]. Following CDC guidelines, CPHHE created a Community Action Plan (CAP)-a contractual agreement between the CDC, CPHHE-REACH and each community partner member in the form of a Project Period Objective (PPO).
A critical sub-objective of the first PPO was to work with the Douglas County Health Department (DCHD) to institute a series of Policy, Systems and Environmental (PSE) improvements. The core strategy was to, “Identify a group of Community Health Ambassadors (CHAs) who, after professional-development training, would design site-specific ‘Implementation Plans’ to increase physical activity opportunities” ([12] p. 3). The training would introduce SOPARC. Volunteer CHAs were recommended by community partners. CPHHE-REACH compensated CHAs for their participation and training. Publications report compensation for CHAs receiving specialized training [16]. Pairing SOPARC training and compensation demonstrated their SOPARC work’s value for larger REACH goals. This emphasis helped stress the requirement for “attention to the detail” of SOPARC training.
SOPARC elements
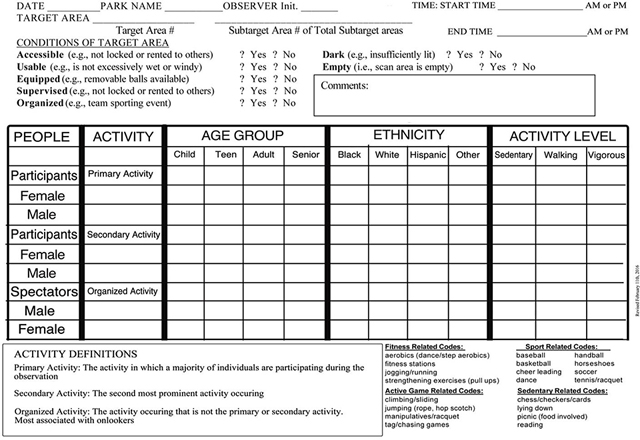
McKenzie and Cohen [17] designed SOPARC to obtain direct information on community park use…including characteristics of parks and their users…“It provides an assessment of the park users’ physical activity levels, gender, activity modes/types and estimated age and ethnicity groupings” (p.2). When administered properly, this instrument accurately captures a wealth of physical activity information about both the environment and people engaging in PA (See Appendix A). The SOPARC instrument has three (3) critical areas for documentation: a.) demographics, b.) target area conditions and c.) the coding grid.
Basic demographic information required is: date, start/end time, park name, target area and coder’s initials. Obviously, accuracy and preciseness are crucial. Target area conditions for PA is a 7-nominal data question section. The coder circles “Yes or No” for the following questions:
| • Accessible? | Yes | No |
| • Usable? | Yes | No |
| • Equipped? | Yes | No |
| • Supervised? | Yes | No |
| • Organized? | Yes | No |
| • Dark? | Yes | No |
| • Empty? | Yes | No |
Coders must visually observe the site and then review and answer each question before the coding process. A comment box just below the last of the 7-questions is to include any information not requested elsewhere in the sections of demographics or target area conditions. The last section, the 5-column coding grid documents information about the people participating in PA and their PA level (see Appendix A).
The coding grid section typically requires practice simulation before attempting to complete the 5-column section. The elements are: a.) People, b.) Activity, c.) Age Group, d.) Ethnicity and e.) Activity level. The coder scans the target area (after completing SOPARC’s top two (2) sections) to observe and code the people, their specific PA, their estimated age and their (observer judged) race/ethnicity.
Accurately observing, assessing and recording the information requires training. The SOPARC form has multiple sections requiring specific information. Thus, effectively learning the observation and coding process requires CHA skill and aptitude as well as SOPARC trainer instructional skill and patience.
SOPARC Training
The CPHHE-REACH Evaluator and Data Manager trained CHAs on the history, purpose and implementation of the SOPARC instrument. These instructors studied the instrument, conceptualized a plan of instruction, and designed and piloted the training prior to CHAs instruction. The multimodal instructional plan consisted of, a.) classroom teaching and b.) experiential practice.
Instructors determined that CHA SOPARC training should be multi-modal to best promote learning. The training combined didactic instruction with experiential learning (see Appendix B and C). The ultimate instructional aim was 90% or greater interrater agreement and accuracy in the recorded SOPARC observations and subsequent coding.
The didactic instruction included SOPARC’s origin and purpose in order to help CHAs visualize the instrument’s use in their personal settings. The instrument’s structure was next introduced. Training methodically moved through SOPARC’s sections: a.) Demographic Information, b.) Conditions of the Target Area, c.) Comment Box, d.) People/Activity Coding Area, e.) Activity Definitions/Descriptions. CHAs were provided SOPARC coding forms, a new clipboard, pencils, a copy of the power point presentation, the narrative scenarios and 12 blank SOPARC observation and coding forms. The CHA trainees would use these items to learn and practice administering the SOPARC instrument.
Trainers introduced the three sections for each the information, the rationale and “how-to.” CHAs learned that the, “Basic Demographics” section must be accurate and completed prior to any other coding section. The demographic section of the coding form explains the “who, where, when and what” of the observation coding (Appendix A). The “Conditions of Target Area” section required a composite explanation for physical activity target areas (See Appendix A). The 5-column grid section for People and Physical Activity-type required the most aptitude and observational skills during the didactic instruction. This section was where people must be accurately observed, coded and accounted for when people were engaged in physical activity, or simply “in-motion” in the play area. An enormous amount of activity and people to monitor can exist simultaneously. People may enter and exit the play area in irregular patterns; however, the coding must account for their presence, activity and exit. Explaining the needed was easy, but novice CHAs had some difficulty understanding. This training required instruction for applicability and focused attention from the CHAs.
During the training’s experiential component, CHAs began understanding the complexity and potential for both, great accuracy and subjectivity. Explaining that 90% interrater agreement and accuracy is the acceptable criteria helped them see the ultimate outcome expectation. The experiential teaching section first offered CHAs contrived, written-narrative scenarios of an indoor and outdoor park area with a full complement of physical activities (see Appendix B and C). The contrived scenarios included all information necessary to complete a blank SOPARC observation and coding sheet. The form’s opposite side provided an accurate and correctly completed SOPARC form mirroring the information in the narrative scenario. Although SOPARC was originally designed to record data in outdoor community settings, many of the physical activities planned for CPHE-REACH would be conducted indoors. The trainers provided both indoor and outdoor narrative scenarios in the training.
The trainers guided the CHAs to silently read the scenario for 5–10 minutes. After readings were completed, CHAs were asked to flip the page over to view the correct information from the scenario coded in its accurate and proper place on the SOPARC form. Next the trainers asked the CHAs to flip the paper back to the narrative scenario side, take-out a blank SOPARC form and prepare to code the blank SOPARC form from the narrative scenario without looking at the pre-coded SOPARC side. Note that the narrative scenarios were designed to provide demographic descriptors representing people of diverse in age, race, gender and levels of physical activity. In this multi-modal training, the scenarios were contrived to discern the CHAs’ ability to apply SOPARC principles.
The next training section often demonstrated how well CHAs actually understood the didactic instruction. For two reasons, we required that CHAs speak aloud as they completed their SOPARC forms. The purpose for speaking aloud was two-fold. First, it was important for the trainers to hear the process the CHAs used and the rationale for that process. Second, CHAs learned from hearing how each other coded and why they coded as they did.
The trainers monitored the discussion and comments to determine both interrater reliability and points of confusion or error. This part of the experiential process required the most time, as CHAs read and re-read, agreed and disagreed with each other. As they corrected and re-entered data according to new discovery, they began to understand not only their own individual coding process, but also their co-CHAs’ coding process.
Once everyone completed filling in the blank SOPARC form from the narrative scenario, the trainers reviewed the forms’ content and the experience process. When 90% interrater accuracy and agreement were achieved, trainers discussed the process. Some CHAs immediately understood and could execute the correct interpretation and coding of the form; however, others could not, and time was required to hear the rationale for specific coding error discussion because. The trainers welcomed the discussion because it afforded trainers the opportunity to hear and see CHAs’ thinking behind coding actions. Once there was unanimous agreement and understanding of SOPARC coding expectations, the trainers proceeded to the next experiential activity.
CHAs next had to observe and code a simulated, but real-life setting. The purpose was to apply the didactic instruction and the narrative scenario into coding a setting without cues. Trainers determined that because the CHAs had to design physical activity opportunities in their local settings, we would host the training in those settings where they lived, worked and worshipped. This setting enabled immediate application of everything taught and learned. The Community Action Plan (CAP) mandated that each community partner increase physical activity opportunities in their specific setting domain. Thus, the trainers selected three (3) possible physical activity settings inside the site for coding and observation. For example, Faith-Based CHAs’ trainings were conducted in local churches. Hence, trainers asked CHAs to identify where in the church building they expected to host physical activities (e.g. the sanctuary, fellowship hall and outdoor parking lot). When identified, the trainers selected each area as a spot for practice. The trainers accompanied the CHAs to the fellowship hall, asked them to observe the area, complete the demographic section, verbally-in unison, complete the, “Conditions of Target Area” section and stop. Then, if everyone had all information accurately completed, the two trainers would leave the CHAs and begin engaging in physical activities either separately or in tandem. The CHAs were directed to, “code what you see.” After 3–7 minutes, the trainers stopped their activities and returned to the CHAs to review and check their coding. When it was determined that 90% interrater accuracy and agreement was met as the passing criteria, the CHAs chose another physical activity setting in their respective areas. Trainers and CHAs proceeded to the 2nd physical activity area, repeated the process, and finally moved to the 3rd and final physical activity area (which often was the outdoor parking area) repeating the process of the previous 2 settings.
When working with CHAs representing local Community Health Center, the Public School Afterschool Programs or the Metropolitan Residential Towers, REACH trainers repeated this same entire process; however, the implementation process was tailored to the different community partner settings. In each instance, when the training was completed, trainers explained how when working through each observation and coding section, they listened to CHAs responses during the training to better understand the rationale for the action taken in the observation and coding process. Additionally, trainers explained the 90% agreement and accuracy criteria so CHAs would end the training and leave the setting with an understanding of the emphasis on accuracy. Incumbent on CHAs’ post-SOPARC training was that they designed an implementation plan for introducing new physical activity opportunities into their local community setting. They had to provide baseline SOPARC observation and coding prior to their implementation plan(s) and a post-implementation plan SOPARC observation and coding after instituting all of their planned physical activities.
Results
The 3-year CPHHE-REACH Physical Activity grant had numerous successes. Training CHAs to understand and administer SOPARC physical activity forms in indoor and outdoor settings was but one. The first chart below shows 56 SOPARC-trained CHAs over the 3-year grant period. The next chart depicts the results of the SOPARC-trained CHAs who administered, observed and coded forms and the increased number of people participating in physical activity. The new physical activity was due in part to CHAs’ implementation and accurate coding. CHAs designed new physical activities in their respective settings-some of which, never existed prior to CHAs’ implementation. Ultimately, over 5000 physical activities were accurately observed, documented and reported back to CPHHE-REACH administrators.
Post results decisions
Each year the CPHHE-REACH SOPARC trainers reviewed the training process, discussed field notes taken during each training and decided to amend the SOPARC training to enhance its outcome(s). After year-one, trainers decided to add an indoor narrative scenario (Appendix D) for the didactic training. Adding the indoor narrative allowed CHAs to practice SOPARC coding indoors where many of their physical activities would take place. Although SOPARC was initially designed to collect data for outdoor community settings, CPHHE-REACH trainers knew community partners would offer indoor activities during the winter months. Now, two indoor narrative scenarios were used with the accurate and correctly coded SOPARC form on the opposite side of the narrative scenario. This was done to provide maximum opportunity for training and coding success. Trainers determined that CHAs could benefit from additional opportunities to visually and mentally consider scenarios prior to the live observation and coding practice. By grant year-3, trainers designed a YouTube video to be used as a refresher course for CHAs who had been trained earlier, but had not observed and coded again after their initial SOPARC baseline observation and coding because of the protracted time to complete the implementation plan of designing the physical activity areas at their different community sites.
The SOPARC YouTube video benefitted CHAs and is still online. The YouTube address is: https://youtu.be/93CVcwyO3Jw. (Appendix D).
The video’s structure mirrors the didactic instruction of the trainers; however, there are numerous visual images and cues permitting the reviewer to pause, review or fast-forward the video to a specific section.
Limitations
The manuscript and project have a series of limitations of note. First, the CHAs were selected by the organizational leaders who committed themselves and organization members to CPHHE-REACH’s physical activity improvement. As a result, although there were CHAs volunteering of their own volition, some were compelled to acquiesce to the wish(es) of their superior(s). Second, the socio-economic and educational background of the CHAs varied which impacted CHA performance in training. Trainers designed SOPARC trainings to ensure outcome success regardless of socio-economic status (SES). Third, the 3-year grant period saw new CHAs from new organizations join CPHHE-REACH’s project. As a result, the trainings were adapted as new insights were discovered. By grant year-3, trainings improved in content, delivery and implementation. Although there was standardization in the training process, evaluation brought a limited number of changes to the SOPARC training process. Last, because all 56 CHAs were not trained at the same time, there were slight differences in both trainer implementation and CHA outcomes.
Discussion
The training of Health-care Liaisons is as diverse as the physical, psychological, emotional and other health needs of patients, clients and community members. Commensurate with these Liaisons’ growing numbers are increasing reporting of their wide ranging training. Health-care Liaisons’ value is proven. Examples are Oncology or Diabetes Nurse Navigators who conduct home visits to monitor home environments or provide post-operative education and support. Such liaisons assist nurses and physicians in providing more comprehensive care for patients, support families in transition and aid community members seeking to improve their health by smoking cessation or increased physical activity. Liaisons demonstrate continued effectiveness as intermediaries between formal health–care providers and patient/clients. These Community Health Ambassadors accept the challenges and sometimes arduous training to provide service to their local communities.
Community Health Ambassadors (CHAs) trained to administer the SOPARC instrument demonstrated similar success as other Health–care Liaisons in other health-care disciplines. This success contributes to the meta-analysis of Health-care Liaison accomplishment, but it expands the knowledge of the range of activities these Health-care Liaisons can engage.
Conclusion
Community Health Ambassadors (CHAs) by any title or name given are invaluable assets to the health-care and patient communities. Regardless of title and setting, they accept the responsibility of committing themselves to a training regime germane to the health-care field and discipline in which they work. Community Health Ambassadors (CHAs) trained to administer the System for Observing Play and Recreation in Communities (SOPARC) [18] completed an extensive training regime to learn accurately observe and code the SOPARC form for an area designed for indoor or outdoor physical activity. In this CPHHE-REACH grant period, 56 dedicated CHAs were trained, certified and successfully observed and coded SOPARC forms for spaces specifically designated for physical activity opportunities in their local communities. As a result, there was marked increase in the number of completed SOPARC forms submitted by CHAs from all community member organizations. These completed SOPARC forms represent an accurate assessment of the amount of new physical activity generated during the CPHHE-REACH grant period. The completion of this task also answered the research question, “Can lay Community Health Ambassadors be trained to administer SOPARC assessing physical activity in their respective settings?” Those 56 SOPARC-trained CHAs submitted accurate pre/post SOPARC forms delineating actual use physical activity data from their community settings. Having demonstrated the ability to use an instrument as complex as SOPARC, strengthens the case for more training in the area of physical activity monitoring for a group of Lay Community Health Ambassadors.
Acknowledgments
The authors wish to thank Creighton University, The Center for Promoting Health and Health Equity (CPHHE), Health Sciences Multicultural and Community Affairs(HS-MACA), The Department of Health and Human Services (HHS), Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Grant Number: 1U58DP005842–01, FAIN:U58DP005842, Racial Approaches to Community Health (REACH). Additionally, the authors thank all the; Community Health Ambassadors from all REACH Community Partners participating in SOPARC Training.
APPENDIX A.
System for Observing Play and Recreation in Communities (SOPARC) [18]
SOPARC Observation & Coding Form
APPENDIX B.
CPHHE-REACH
SOPARC Training for Health Ambassadors Problem Solving-SOPARC Narrative Training
Scenario:
You come to the Smith Park, a local neighborhood park to observe and code for SOPARC. You stop, take your time to scan the entire park area and notice people engaging in a baseball game on Sanders Field. It’s a sunny, clear, Fall, Wednesday midafternoon (1:30pm). You notice that the only entrance into Sanders Field is through an open gate which is kept closed and locked at night. The fenced-in field contains a baseball field, bleachers and an open concession stand where an older African American man stands inside to sell hot chocolate and cookies to guests.
As you continue to observe, you see a total of 28 (14 per team) young children ages 7–10 years. There are 6 African American boys & 5 African American girls, 6 Latin girls & 2 Latin boys, 3 Caucasian girls & 2 Caucasian boys and 4 Asian boys. There are a total of 6 African American male coaches (3 per team). There are also 6 African American females who are the wives of the coaches. The coaches and their wives seemed to be middle-aged (under 40 years) adults. The spectator section had a total of 56 grandparents who were all wrapped in their blankets. There were 4 Asian male & 4 Asian female grandparents, 8 Latin male & 8 Latin female grandparents, 4 Caucasian male & 4 Caucasian female grandparents and 12 African American male & 12 African American female grandparents.
The game lasted 2 hours. All 28 children got an equal chance to play. They all hit, ran, slid and caught the ball in the field. The wives were on the sidelines acting as cheerleaders-jumping, yelling and doing cheers to motivate their teams. During the whole
APPENDIX C.
CPHHE-REACH SOPARC Training for Health Ambassadors
Problem Solving-SOPARC Narrative Training
Scenario 2:
You are in the Mark Dean Conference Room, located on the third floor of the Charles H. Houston Community Center to observe and code for SOPARC. You stop, take your time to scan the entire conference room and notice people engaging in various exercises. It’s a cold and snowy Thursday evening (7:15pm). There are security guards and staff on patrol at the entrance and in the lobby of the community center to monitor activity, provide directions and ensure safety for all guests during the hour of 5:00pm-8:00am.
In the conference room there are exercise mats, jump-ropes, exercise balls and two senior African American male staff members, who are in the corner of the room moving tables and chairs to make space for the exercise classes.
In one section of the room, you see a total of 24 adults engaging in high-intensity jump-rope, abdominal crunches and squat activities. There are 3 African American men & 5 African American women, 4 Hispanic women & 4 Hispanic men, 2 Caucasian women 5 Asian women participating, following directions from a middle-aged female African American instructor. All the participants in this activity utilized jump-ropes, exercise balls, and some of the exercise mats. In the opposite section of the room, you see16 senior adults engaging in a separate calisthenics activity hosted by a middle-aged male Caucasian instructor. There are 4 African American men & 4 African American women, 2 Hispanic women & 1 Hispanic man, 5 Caucasian women participating in jumping jacks, push-ups and balance activities. Along the walls of the conference room, 6 children (3 African American boys, 2 Caucasian girls and 1 Hispanic girl) were sitting as they read books and completed homework assignments.
The exercise sessions in the Mark Dean Conference Room lasted for an hour and thirty minutes. All adults participated in the exercise classes for the entire period. At the end of the session, the two male staff members moved all the tables and chairs back in their appropriate places before cleaning up, turning off the lights and locking the conference room doors.
Complete your SOPARC Observation & Coding Form after reading and discussing the narrative.
APPENDIX D.
CPHHE-REACH YouTube Video
The YouTube link below allows you to access the SOPARC training video for CPHHE-REACH’s SOPARC Training: https://www.youtube.com/watch?v=93CVcwyO3Jw&t=3s
Footnotes
Disclosure
Authors are all affiliated with Creighton University’s Center for Promoting Health and Health Equality (CPHHE) and Health Sciences-Multicultural and Community Affairs (HS-MACA), Racial and Ethnic Approaches to Community Health (REACH) Grant. The CPHHE-REACH grant is funded by the Centers for Disease Control and Prevention (CDC).
References
- 1.Bureau of Labor Statistics (2018) U. S. department of labor, occupational outlook handbook, health educators and community health workers. [Google Scholar]
- 2.Koo D (n.d.). CDC Community health improvement (CHI) navigator. Adapted from Goodman RA, Bunnell R, Posner SF (2014) What is “community health”? Examining the meaning of an evolving field in public health. Prev Med 67(1): 58–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suther S, Battle AM, Battle-Jones F, et al. (2015) Utilizing health ambassadors to improve type-2 diabetes and cardiovascular disease outcomes in Gadsden County, Florida. Eval Program Plann 55: 17–26. [DOI] [PubMed] [Google Scholar]
- 4.Pullen-Smith B, Carter-Edwards L, Leathers KH (2008) Community health ambassadors: A model for engaging community leaders to promote better health in North Carolina. J Public Health Manag Pract (14): S73–S81. [DOI] [PubMed] [Google Scholar]
- 5.Blair TRW (2012) “Community ambassadors” for South Asian elder immigrants: Late-life acculturation and the roles of community health workers. Soc Sci Med 75(10): 1769–1777. [DOI] [PubMed] [Google Scholar]
- 6.Hill MN, Becker DM (1995) Roles of nurses and health workers in cardiovascular health promotion. Am J Med Sci 310(1): S123–S126. [DOI] [PubMed] [Google Scholar]
- 7.Pratt-Chapman M, Willis A, Masselink L (2015) Core competencies for oncology patient navigators. J Oncol Navigation & Survivorship 6(2): 16–21. [Google Scholar]
- 8.Morrison M (2016) Study finds patient navigators improve comprehensive cancer screening rates. Massachusetts General Hospitals. [Google Scholar]
- 9.Loskutova NY, Tsai AG, Fisher EB, et al. (2016) Patient navigators connecting patients to community resources to improve diabetes outcomes. J Am Board Fam Med 29(1): 78–91. [DOI] [PubMed] [Google Scholar]
- 10.Burbage D, Siegel S (2015) The embedded nurse navigator model: A novel approach to providing survivorship care in a community cancer center. [Google Scholar]
- 11.Lee WD, Peck D, Emmert D, et al. (2008) Mental Health Ambassador Handbook. San Jose State University, San Jose, CA. [Google Scholar]
- 12.Kosoko-Lasaki O, Stone JR, Smith J, et al. (2017) The center for promoting health and health equality’s racial and ethnic approaches to community health program. JCMHE 7(3) 1–6. [Google Scholar]
- 13.Wannamethee SG, Shaper AG (2001) Physical activity in the prevention of cardiovascular disease: An epidemiological perspective. Sports Med 31(2): 101–114. [DOI] [PubMed] [Google Scholar]
- 14.Blair SN, Kohl HW 3rd, Paffenbarger RS Jr, et al. (1989) Physical fitness and all-cause mortality: A prospective study of healthy men and women. JAMA 262(17): 2395–2401. [DOI] [PubMed] [Google Scholar]
- 15.Chave SPW, Morris JN, Moss S, et al. (1978) Vigorous exercise in leisure time and the death rate: A study of male civil servants. J Epidemiol Community Health 32(4): 239–243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Vines AI, Hunter JC, Carlisle VA, et al. (2017) Prostate cancer ambassadors: Process and outcomes of a prostate cancer informed decision-making training program. Am J Mens Health 11(1): 54–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McKenzie TL, Cohen DA (2006) SOPARC: System for observing play and recreation in communities: Description and procedure manual. Active Living Research, Coronado, CA. [Google Scholar]
- 18.McKenzie TL, Cohen DA, Sehgal A, et al. (2006) System of observing play and recreation in communities (SOPARC): Reliablility and feasibility measures. J Phys Act Health 3: 208–220. [DOI] [PubMed] [Google Scholar]


