1. Introduction
Interoceptive awareness includes a noting and acknowledgment of internal body sensations, emotional states and movement, as well as a person’s appraisal of such stimuli (Farb et al., 2015; Khalsa & Lapidus, 2016). Interoceptive processes are necessary in all major body systems to support homeostasis, including pulmonary (Del Negro, Funk & Feldman, 2018), gastrointestinal (Mayer, 2013; Smith, Gudleski, Lane & Lackner, 2019; Zimmerman et al., 2019), genitourinary (de Groat, Griffiths & Yoshimura, 2015; Keller et al., 2019), neurologic (Beissner, Meissner, Bär & Napadow, 2013; Hadjikhani et al., 2013), and others. Interoception, therefore, plays a role in emotional regulation and decision making since aversive or distressing stimuli generally signal a need to return to a homeostatic state (Farb et al., 2015; Khalsa, et al., 2018a; Khoury et al., 2018). Errors in interoceptive processing, including in interoceptive expectations and accuracy, or integration with higher order cognitions, have been postulated as biomarkers of numerous affective states (Khalsa, Feinstein, Simmons & Paulus, 2018b; Price & Hooven, 2018). Specifically, individuals with psychiatric disorders, such as depression, experience abnormalities in interoceptive processes (Harshaw, 2015; Lackner & Fresco, 2016; Limmer, Kornhuber & Martin, 2015), which may contribute to illness development, symptomology or disease progression.
Depression is among the top ten causes of disability and death, worldwide, and the World Health Organization predicts that by 2030, depression will be the leading cause of disease burden (Malhi & Mann, 2018; Smith & De Torres, 2014). Importantly, rates appear similar across high-income countries and low to middle-income countries, with 5-6% of the global population experiencing depression and a lifetime prevalence rate of 20% (Malhi & Mann, 2018; Otte et al., 2016). Depression is associated with high rates of suicide and self-harm, premature morbidity, and numerous medical conditions like heart disease, stroke and metabolic consequences such as obesity (Akincigil & Matthews, 2017; Indu et al., 2017; Otte et al., 2016). Persons with depression are disproportionately represented among primary care populations (Akincigil & Matthews, 2017; Olivan-Blazquez, Rubio-Aranda, Garcia-Sanz & Magallon-Botaya, 2016). Depression is linked to homeostatic dysregulation and somatic symptoms of sleep disturbances, weight changes, alterations in appetite and sexual dysfunction, which are all common symptoms frequently seen in primary care settings (Harshaw, 2015). However, complex and diverse symptom presentation, medical comorbidity and stigma, including culturally-specific stigmas, may contribute to a lack of assessment and diagnosis (Akincigil & Matthews, 2017; Hahm, Cook, Ault-Brutus & Alegria, 2015; Malhi & Mann, 2018).
Historically, interoception in individuals with depression has been measured via physiological tests which have focused only on interoceptive accuracy, such as heartbeat detection (e.g. heartbeat-tracking, signal detection) (Garfinkel, Seth, Barrett, Suzuki & Critchley, 2015; Kleckner, Wormwood, Simmons, Barrett & Quigley, 2015). Empirical studies assessing the relationship between interoception and depression have been mixed. For example, most research indicates that as severity of depression increases, interoceptive accuracy of heartbeat detection decreases (Pollatos, Traut-Mattausch & Schandry, 2009; Herbert, Herbert & Pollatos, 2011; Limmer et al., 2015). Yet, other research shows that among individuals with depression, as severity increases, the accuracy of heartbeat detection also increases (Dunn, Dalgleish, Ogilvie & Lawrence, 2007). One recent study noted no relationship between level of depression and interoceptive accuracy of heartbeat detection (Solano-Lopez & Moore, 2018). The variability in findings may be related to the role of comorbid anxiety or panic, which varies across studies. In general, studies note substantial interaction effects (Pollatos et al., 2009; Dunn et al., 2010; Limmer et al., 2015) although some data show no significant changes to results (Dunn et al., 2007). Since over 40% of persons with depression have co-occurring anxiety disorders (Kessler et al., 2015) controlling for these comorbid symptoms is imperative. Importantly, for those with anxiety disorders, depression appears to start earlier in life and have a more chronic course (Kessler et al., 2015).
More recently, neuroimaging studies have been used to assess the relationship between interoceptive awareness and depression. These studies support the hypothesis that physical and emotional interoceptive statuses are interpreted centrally in the insula and anterior cingulate cortex (ACC) (Paulus & Stein, 2010; Farb et al., 2015). Across studies, functional magnetic resonance imaging data indicate hypoactivation of the insula during depression (Sliz & Hayley, 2012; Avery et al., 2014; DeVille et al., 2018). Specifically, hypoactivation of the insula was noted in persons with depression who were asked to become aware of interoceptive sensations (Avery et al., 2014) and during interoceptive recall of unpleasant stimuli (DeVille et al., 2018).
Physiological or neurological tests alone, however, do not represent a comprehensive assessment of interoceptive awareness (Farb et al., 2015; Garfinkel et al., 2015; Khalsa & Lapidus, 2016; Mehling et al., 2012), nor are they always feasible or cost-effective. These means of measuring interoception cannot capture all the ways in which individuals attend and respond to interoceptive stimuli (Khalsa & Lapidus, 2016; Mehling et al., 2012). Beyond the physiological accuracy and neurological activity of interoceptive stimuli, such sensations interact with higher order cognitions (e.g. beliefs, historical input, social and cultural contexts or the environment) to inform emotional status and behavior (Farb et al., 2015; Ma-Kellams, 2014). Using a broader definition of interoceptive regulation, a person’s attention to, appraisal of, and response to interoceptive stimuli are crucial to understand as it may be what underlies pathology and influences behavior, especially when considering mental illnesses such as depression (Khoury, Lutz & Schuman-Olivier, 2018).
Due to a paucity of available measures, few studies use subjective, diagnoses-independent, broad, multidimensional assessments of interoception making it difficult to compare results (Mehling et al., 2009; Khoury et al., 2018). The Multidimensional Assessment of Interoceptive Awareness (MAIA; Mehling et al., 2012) subscales are recently developed, reliable and valid measures that could help address this gap. The MAIA consists of eight self-report scales measuring different aspects of interoceptive awareness in a similar manner to what Garfinkle and colleagues describe as “interoceptive sensibility” (Garfinkle, Seth, Barrett, Suzuki & Critchley, 2015), which is an umbrella term for subjective assessment of interoceptive tendencies and skills and the extent to which people believe they focus on and detect bodily sensations (Khoury, Lutz & Schuman-Olivier, 2018). The MAIA scales include noticing, not distracting, not worrying, attention regulation, emotional awareness, self-regulation, body listening and trusting and are described further in the methods section. Importantly, interoceptive accuracy, interoceptive attention quality and interoceptive sensibility or awareness as defined by the MAIA, often do not have a high level of correlation. While others have studied physiologic or behavioral measures of interoceptive dysfunction in depression (Paulus & Stein, 2010; Sliz & Hayley, 2012; Avery et al., 2014; Farb et al., 2015; DeVille et al., 2018), the relationship of multidimensional aspects of interoceptive sensibility and the impact of the subjective, self-perceived sense of interoceptive awareness on depression are important to understand more clearly.
The noticing subscale of the MAIA, which is similar to previous measures of body awareness, may be most closely linked to physiological tests of interoceptive accuracy like heartbeat detection (Fissler, et al., 2016). Across the eight MAIA subscales, one study found that depressive symptoms were inversely associated with attention regulation, self-regulation, body listening and trusting, and positively associated with not distracting (Solano-Lopez & Moore, 2018). This positive association with not distracting likely relates to individuals with depression not ignoring uncomfortable or painful sensations (Solano-Lopez & Moore, 2018). After controlling for anxiety, only the relationships between depressive symptoms, trusting and not distracting remained significant (Solano-Lopez & Moore, 2018). Other studies have reported on the significant, longitudinal improvements in depression and MAIA scores following mind-body interventions among persons with substance use (Price, Adams Thompson, Crowell & Pike, 2019) and chronic pain with comorbid depression (de Jong et al., 2016) but do not report baseline associations. A deeper understanding of the link between interoceptive awareness and depression could help develop more effective mental health treatment.
Using the MAIA (Mehling et al., 2012), we assessed the relationship between self-reported interoceptive awareness and self-reported depression severity categories among primary care patients. We hypothesized that 1) patients with greater depression severity will have lower scores on the MAIA subscales of noticing, attention regulation, self-regulation, body listening and trusting; 2) there will be a positive relationship between greater depression severity and not distracting; and 3) when controlling for anxiety symptoms only the relationships between greater depression severity, trusting and not distracting will remain significant.
2. Method
Data for this cross-sectional analysis came from the baseline self-report measures of a randomized controlled trial (ClinicalTrials.gov Identifier: NCT02972203), which investigated the impact of mindfulness training for primary care patients on management of chronic illness and symptoms of anxiety, depression, and stress. The clinical trial was implemented within a large urban safety-net community healthcare system. Additional information on the intervention and inclusion/exclusion criteria can be found elsewhere (Gawande et al., 2018). Survey respondents consisted of adults who were 18 years and older that received primary care services within the healthcare system and had at least one diagnosis eligible for insurance reimbursement for group therapy visits (e.g. anxiety, depression, pain, insomnia). The analytic sample for this cross-sectional secondary analysis included all primary care patients that completed all four scales (demographics, PROMIS depression, PROMIS anxiety and MAIA) at baseline (N = 281) on August 8th 2019. This study was approved by the Cambridge Health Alliance Institutional Review Board in accord with the Declaration of Helsinki.
2.1. Multidimensional Assessment of Interoceptive Awareness (MAIA) Scale
Our outcomes for this study were the eight continuous subscales from the 32-item Multidimensional Assessment of Interoceptive Awareness (MAIA) scale (Mehling et al., 2012), which include noticing (e.g. “I notice where in my body I am uncomfortable”), not distracting (e.g. “When I feel pain or discomfort, I try to power through it”), not worrying (e.g. “I start to worry that something is wrong if I feel any discomfort”), attention regulation (e.g. “I can refocus my attention from thinking to sensing my body”), emotional awareness (e.g. “I notice how my body changes when I am angry”), self-regulation (e.g. “When I am caught up in thought, I can calm my mind by focusing on my body/breathing”), body listening (e.g. “I listen for information from my body about my emotional state”) and trusting (e.g. “I trust my body sensations”). We generated the eight subscale outcomes using established scoring convention (Mehling et al., 2012). The MAIA is a validated, reliable measure of interoceptive sensibility, assessing awareness of body sensations, emotional and attentional responses to these sensations, the capacity to regulate attention, awareness of the integration of body and mind connection (e.g. emotional awareness, self-regulation and body listening) and trust in bodily sensations. The MAIA evaluates a broad definition of interoception, and is a diagnosis-independent measure, allowing comparison across different illnesses (Khoury et al., 2018). The MAIA has demonstrated acceptable internal consistency and reliability (i.e., alphas for the eight scales range from 0.66 to 0.87) (Mehling et al., 2013).
2.2. Patient Reported Outcomes Measurement Information System (PROMIS®)
The independent variable of interest was categorical and based on the Patient Reported Outcomes Measurement Information System (PROMIS®) - Depression Short Form 8a (PROMIS-DSF). The PROMIS-DSF measures patient reported level of depression over the past seven days and includes items such as “I felt worthless” and “I felt that nothing could cheer me up.” Based on established scoring convention (American Psychiatric Association [APA], 2013), we categorized depression severity into the following categories using normalized T-scores: none to slight depression, mild depression, and moderate/severe depression. The accuracy of categorical T-scoring of the PROMIS-DSF has been well established (Choi, Schalet, Cook & Cella, 2014). We combined the moderate and severe categories to have a robust sample and increase estimate precision. The 8-item PROMIS-DSF is a widely used measure assessing patient reported depression (Pilkonis et al., 2014; Pilkonis et al., 2011). Validity and reliability have been well established in diverse samples (e.g. Clover et al., 2018; Sunderland, Batterham, Calear & Carragher, 2018). This scale allows for a dimensional assessment of depression (e.g. state), which may be most related to interoceptive awareness (Dunn et al., 2010) as well as categorization based on severity.
2.3. Covariates
We adjusted for age, sex, race/ethnicity (White non-Hispanic, Black, Asian, Latino, and other) marital status, education (less than high school, high school graduate, some college, college graduate), employment status, any substance use disorder diagnosis, any post-traumatic stress disorder diagnosis, any antidepressant use and anxiety severity. Clinical characteristics (e.g. substance use disorder and any antidepressant use) reflected the 12-month period prior to baseline and were obtained from patient’s Electronic Health Records. Antidepressants were classified using Medi-Span Generic Product Identifier (Kluwer, 2018) codes to identify drug group classifications. Assessment of clinical characteristics and sociodemographic variables is described elsewhere (Gawande 2018).
We defined anxiety severity using the Patient Reported Outcomes Measurement Information System (PROMIS®) - Anxiety Short Form 8a (PROMIS-ASF). The PROMIS-ASF (Pilkonis et al., 2011) is a reliable and valid measure widely used to assess patient reported anxiety (e.g. Beleckas et al., 2018; Sunderland et al., 2018) which focuses on experiences in the past seven days and consists of eight items (e.g. “I felt fearful,” “My worries overwhelmed me”). Anxiety severity was treated as a continuous variable based on normalized T scores as previously done by Gawande and colleagues (2018).
2.4. Statistical analysis
We first examined sociodemographic, service use, and clinical characteristics of the sample population by PROMIS depression severity categories, using t-test and chi-square tests for continuous and categorical variables, respectively. Next, we specified linear regression models to estimate the association between depression severity and MAIA subscales. We estimated three models, (1) unadjusted; (2) adjusting for anxiety severity; (3) adjusting for anxiety severity and all covariates. Finally, we used reverse stepwise regression to assess the relationship between highly correlated MAIA subscales (p-value removal of 0.10), separate from anxiety, on depression severity scores. As an exploratory analysis, we also ran a stepwise regression model to assess the relationship of correlated MAIA subscales (p-value removal of 0.10) on anxiety severity scores. In terms of power, we used the formula by Green (1991) for calculating sample size, N > 104 + m (where m is the number of independent variables) (VanVoorhis & Morgan, 2007). Based on Monte Carlo simulations, a minimum of two subjects per variable are needed to estimate accurate point estimates and standard errors when conducting a linear regression analysis (Austin & Steyerberg, 2015). Multicollinearity was assessed by examination of tolerance and variance inflation factors. Variables did not exceed acceptable limits of <.1 and >10, respectively. We adjusted statistical significance for the five hypothesized tests using Bonferroni correction (Abdi, 2007). All analyses were conducted using Stata version 15.1 (StataCorp, 2017).
3. Results
Table 1 shows descriptive statistics and MAIA scores. Our sample (N = 281) consisted of 63% females and about 1% nonbinary individuals. In terms of race and ethnicity, about 68% identified as White-non Hispanic, 8% as Black, 5% Asian, 10% Latino and 9% other. The majority of participants were between the ages of 25 to 54 years old and 32% were married. Our sample was well-educated with the majority having at least a college education. Most participants were employed. Individuals had Diagnostic and Statistical Manual (DSM 5) (APA, 2013) diagnoses of depressive disorders (64%), anxiety disorders (73%), post-traumatic stress disorder (9%) and substance use disorders (12%). Individuals used antidepressant medications (60%), antianxiety medications (24%) and antipsychotic medications (6%). Thirty-five percent of the sample had none to slight depression severity, 26% had mild depression and 39% had moderate to severe depression.
Table 1.
Descriptive Characteristics of Sample Populations by Depression Severity
| Depression Severity Level | ||||||
|---|---|---|---|---|---|---|
| None to Slight Depression |
Mild Depression |
P | Moderate to Severe Depression |
P | Total Population |
|
| Sample Population (n) | 99 | 73 | 109 | 281 | ||
| Multidimensional Assessment of Interceptive Awareness- Subscales (mean) | ||||||
| Overall Average | 2.67 | 2.41 | 2.45 | 2.45 | ||
| Noticing | 3.10 | 2.86 | 2.81 | 2.92 | ||
| Not-Distracting | 2.50 | 2.54 | 2.17 | * | 2.39 | |
| Not-Worrying | 2.69 | 2.37 | 2.13 | *** | 2.39 | |
| Attention Regulation | 2.22 | 2.09 | 2.09 | 2.14 | ||
| Emotional Awareness | 3.09 | 3.07 | 2.99 | 3.05 | ||
| Self-Regulation | 2.56 | 2.22 | * | 2.11 | ** | 2.29 |
| Body Listening | 1.90 | 1.76 | 1.65 | 1.76 | ||
| Trusting | 3.33 | 2.38 | *** | 2.29 | *** | 2.69 |
| PROMIS (Patient-reported Outcome Measurement Information System) (%) | ||||||
| Anxiety | ||||||
| None to slight | 28.28 | 4.11 | *** | 2.75 | *** | 12.06 |
| Mild | 27.27 | 12.33 | * | 7.34 | * | 15.60 |
| Moderate | 40.40 | 75.34 | *** | 55.05 | * | 54.96 |
| Severe | 4.04 | 8.22 | 34.86 | *** | 17.02 | |
| Demographics (Baseline Interview) | ||||||
| Sex | ||||||
| Female | 62.24 | 61.64 | 65.74 | 63.21 | ||
| Race/Ethnicity (%) | ||||||
| White | 74.75 | 64.38 | 63.3 | 67.62 | ||
| Black | 7.07 | 13.7 | 5.5 | 8.19 | ||
| Asian | 5.05 | 4.11 | 6.42 | 5.34 | ||
| Latino | 8.08 | 10.96 | 11.93 | 10.32 | ||
| Other | 5.05 | 6.85 | 12.84 | * | 8.54 | |
| Age (%) | ||||||
| 18-24 | 7.07 | 6.85 | 2.75 | 5.34 | ||
| 25-34 | 35.35 | 41.10 | 38.53 | 38.08 | ||
| 35-44 | 27.27 | 17.81 | 19.27 | 21.71 | ||
| 45-54 | 13.13 | 13.70 | 20.18 | 16.01 | ||
| 55-64 | 10.10 | 15.07 | 14.68 | 13.17 | ||
| 65+ | 7.07 | 5.48 | 4.59 | 5.69 | ||
| Marital Status (%) | ||||||
| Yes | 33.33 | 28.77 | 32.11 | 31.56 | ||
| Education Status (%) | ||||||
| Less than High School | 3.03 | 0.00 | 6.42 | 3.56 | ||
| High School | 5.05 | 2.74 | 9.17 | 6.05 | ||
| Some College | 9.09 | 16.44 | 20.18 | * | 15.30 | |
| College+ | 82.83 | 80.82 | 64.22 | ** | 75.09 | |
| Employed (%) | ||||||
| Yes | 73.74 | 69.86 | 59.63 | * | 67.02 | |
| Any Mental Health and Substance Use Disorder (%) | ||||||
| Depression Disorder | 45.45 | 64.38 | * | 80.73 | *** | 63.83 |
| Anxiety Disorder | 71.72 | 82.19 | 67.89 | 72.70 | ||
| Post-Traumatic Stress Disorder | 3.03 | 6.85 | 14.68 | ** | 8.51 | |
| Substance Use Disorder | 11.11 | 15.07 | 10.09 | 11.70 | ||
| Any Medication Use (%) | ||||||
| Antidepressant Rx | 41.00 | 46.00 | ** | 74.31 | *** | 59.57 |
| Antianxiety Rx | 19.19 | 31.51 | 22.94 | 23.76 | ||
| Antipsychotic Rx | 2.02 | 8.22 | 7.34 | 5.67 | ||
p>0.05
p<0.01
p<0.001
All comparison are versus none to slight depression; Depression is measured with PROMIS Depression 8a
Patients with mild or moderate to severe depression were more likely to have moderate or severe anxiety, a diagnosis of depression or post-traumatic stress disorder, and to have filled at least one antidepressant prescription, compared with patients with none to slight depression. Patients with moderate to severe depression were more likely to identify their race/ethnicity as “other” and were more likely to be college educated. The average MAIA score was 2.67 among persons with none to slight depression, 2.41 among persons with mild depression and 2.45 in persons with moderate to severe depression and there were no statistical significant differences by group.
Overall, patients with higher self-reported depression scores tended to have lower MAIA scores than patients with none to mild depression. Most significant was trusting score (p < .001), which was lower for patients with mild depression compared to patients with none to slight depression. Self-regulation score (p < .05) was also lower for these patients. Patients with moderate to severe depression had significantly lower scores in the subscales non-distracting (p < .05), not worrying (p < .001), self-regulation (p < .01), and trusting (p < .001) compared to those with none to slight depression.
3.1. Unadjusted Model
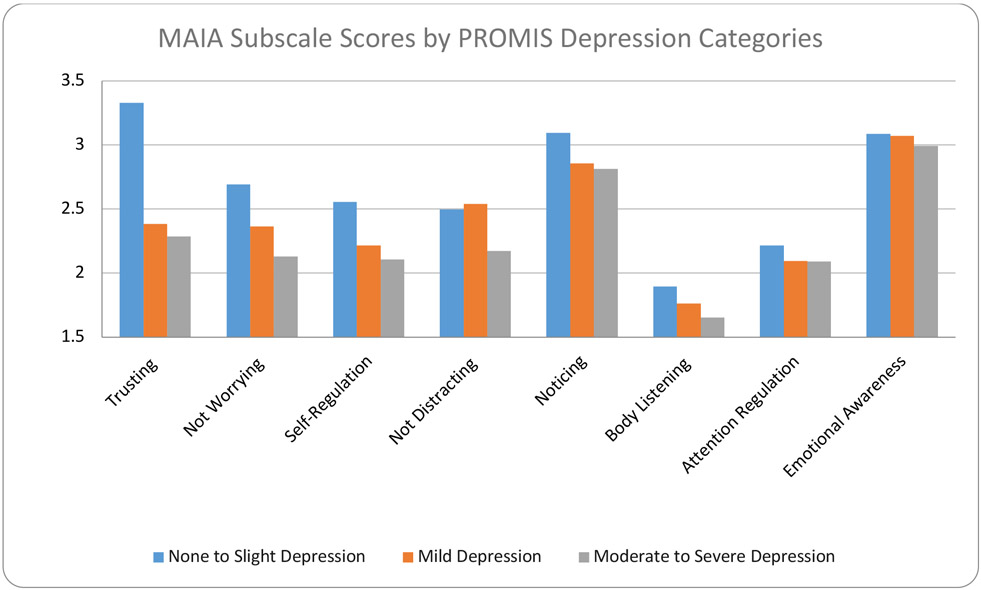
In unadjusted results (Table 2a), mild depression and moderate to severe depression were inversely associated with the MAIA sub-scales of self-regulation (p < .01) and trusting (p < .001). Moderate to severe depression was also inversely associated with not distracting (p < .05) and not worrying (p < .001). Figure 1.
Table 2a.
Unadjusted Estimates of Multidimensional Assessment of Interoceptive Awareness Subscale Scores by Depression Severity Categories
| Noticing | Not Distracting | Not Worrying | Attention Regulation | Emotional Awarenes | Self-regulation | Body Listening | Trusting | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | |
| PROMIS | ||||||||||||||||||||||||
| Depression (Reference None to slight) | ||||||||||||||||||||||||
| Mild | −0.24 | 0.16 | −0.56 to 0.08 | 0.04 | 0.17 | −0.29 to 0.37 | −0.32ⱡ | 0.17 | −0.67 to 0.01 | −0.12 | 0.15 | −0.42 to 0.18 | −0.02 | 0.17 | −0.36 to 0.32 | −0.34* | 0.15 | −0.62 to −0.05 | −0.13 | 0.18 | −0.50 to 0.23 | −0.95*** | 0.19 | −1.32 to −0.57 |
| Moderate to Severe | −0.28ⱡ | 0.15 | −0.60 to 0.02 | −0.32* | 0.14 | −0.61 to −0.04 | −0.56*** | 0.16 | −0.88 to −0.25 | −0.12 | 0.15 | −0.41 to 0.17 | −0.09 | 0.16 | −0.41 to 0.23 | −0.45** | 0.15 | −0.74 to −0.16 | −0.24 | 0.17 | −0.57 to 0.09 | −1.04*** | 0.19 | −1.41 to −0.68 |
p<0.10
p<0.05
p<0.01
p<0.001
Figure 1.
MAIA Subscales by PROMIS-DSF Categories
3.2. Adjusted Models
When adjusting for the PROMIS anxiety scale (Table 2b), similar to unadjusted results, mild depression and moderate to severe depression were inversely associated (p < .05) with the subscales self-regulation and trusting. There was also a significant inverse relationship with the noticing subscale (p < .05). Moderate to severe depression was also inversely associated with emotional awareness (p < .05) and body listening (p < .05).
Table 2b.
Adjusted Estimates of Multidimensional Assessment of Interoceptive Awareness Subscale Scores by Depression Severity Categories with Anxiety
| Noticing | Not Distracting | Not Worrying | Attention Regulation | Emotional Awarenes | Self-regulation | Body Listening | Trusting | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | |
| PROMIS | ||||||||||||||||||||||||
| Depression (Reference None to slight) | ||||||||||||||||||||||||
| Mild | −0.36* | 0.17 | −0.70 to −0.03 | 0.13 | 0.17 | −0.21 to 0.46 | 0.01 | 0.17 | −0.33 to 0.34 | −0.11 | 0.16 | −0.43 to 0.20 | −0.2 | 0.18 | −0.56 to 0.16 | −0.30* | 0.15 | −0.61 to −0.00 | −0.26 | 0.19 | −0.63 to 0.11 | −0.83*** | 0.2 | −1.22 to −0.43 |
| Moderate to Severe | −0.49** | 0.19 | −0.86 to −0.12 | −0.18 | 0.17 | −0.52 to 0.16 | 0.01 | 0.16 | −0.31 to 0.32 | −0.11 | 0.15 | −0.41 to 0.19 | −0.40* | 0.18 | −0.76 to −0.04 | −0.39* | 0.16 | −0.70 to −0.08 | −0.46* | 0.19 | −0.83 to −0.08 | −0.84*** | 0.22 | −1.27 to −0.40 |
p<0.10
p<0.05
p<0.01
p<0.001
Adjusting for PROMIS Anxiety (continuous)
In our fully adjusted regression model (Table 2c), where we include sociodemographic, service use, and clinical covariates, results were similar at the moderate to severe level of depression. In our final model, moderate to severe depression was inversely associated with trusting (p < .001), body listening (p < .01), noticing (p < .01), emotional awareness (p < .01), and self-regulation (p < .05), whereas mild depression was only inversely associated with trusting (p < .001). When accounting for multiple comparisons, moderate to severe depression was no longer significantly associated with self-regulation.
Table 2c.
Adjusted Estimates of Multidimensional Assessment of Interoceptive Awareness Subscale Scores by Depression Severity Categories with Anxiety and Other Covariates
| Noticing | Not Distracting | Not Worrying | Attention Regulation | Emotional Awarenes | Self-regulation | Body Listening | Trusting | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | Coef | SE | 95%CI | |
| PROMIS | ||||||||||||||||||||||||
| Depression (Reference None to slight) | ||||||||||||||||||||||||
| Mild | −0.30 | 0.17 | −0.64 to 0.04 | 0.17 | −0.17 | −0.17 to 0.52 | 0.13 | 0.17 | −0.21 to 0.48 | −0.07 | 0.16 | −0.39 to 0.26 | −0.21 | 0.18 | −0.57 to 0.14 | −0.31 | 0.16 | −0.63 to 0.01 | −0.33 | 0.19 | −0.70 to 0.03 | −0.74*** | 0.21 | −1.16 to −0.32 |
| Moderate to Severe | −0.47* | 0.19 | −0.86 to −0.09 | −0.08 | 0.19 | −0.45 to 0.28 | 0.13 | 0.18 | −0.22 to 0.49 | −0.11 | 0.18 | −0.46 to 0.24 | −0.52** | 0.19 | −0.89 to −0.15 | −0.40* | 0.17 | −0.74 to −0.07 | −0.57** | 0.2 | −0.96 to −0.18 | −0.75*** | 0.23 | −1.21 to −0.30 |
p<0.10
p<0.05
p<0.01 (significant after correction for multiple comparisons)
Adjusting for gender, race/ethnicity, age, education level, marriage status, employment status, PROMIS Anxiety, any PTSD diagnosis, any substance use disorder diagnosis, any antidepressent prescription
3.3. Stepwise Regression Models
Results from the reverse stepwise regression suggest that only trusting (p < 0.001) accounted for some variance in mild depression severity scores. When adding anxiety, sociodemographic, service use, and clinical covariates into the model, trusting remained significant (p < 0.01). In moderate to severe depression, trusting (p < 0.001) and not worrying (p < 0.01) accounted for some variance in the model, however only trusting (p < 0.05) remained significant when controlling for anxiety scores. Anxiety significantly contributed to depression severity scores as well (p < 0.001) (Table 3). In an exploratory analysis, when examining the relationship between the MAIA subscales on anxiety severity scores, not worrying (p < 0.001), emotional awareness (p < 0.001) and depression (p < 0.001) most significantly contributed to unique variance (Table 4).
Table 3.
Reverse Stepwise Regression Models of PROMIS Depression Scale with MAIA Subscales as Predictors
| PROMIS Depression: Mild | |||
|---|---|---|---|
| Primary Predictors | Coef | SE | 95% CI |
| Trusting | −0.57** | 0.19 | −0.94 - −0.21 |
| Not Worrying | 0.29 | 0.17 | −0.04 - 0.63 |
| Not Distracting | 0.31 | 0.20 | −0.08 - 0.70 |
| Self-regulation | 0.01 | 0.23 | −0.44 - 0.46 |
| PROMIS Anxiety | 0.17*** | 0.04 | 0.10 - 0.25 |
| PROMIS Depression: Moderate to Severe | |||
| Primary Predictors | Coef | SE | 95% CI |
| Trusting | −0.45* | 0.18 | −0.80 - −0.09 |
| Not Worrying | 0.22 | 0.17 | −0.12 - 0.56 |
| Not Distracting | −0.02 | 0.20 | −0.41 - 0.38 |
| Self-regulation | −0.14 | 0.24 | −0.61 - 0.32 |
| PROMIS Anxiety | 0.28*** | 0.05 | 0.19 - 0.37 |
p<0.05
p<0.01
p<0.001
Referent outcome level for PROMIS Depression: None to Slight
Adjusting for gender, race/ethnicity, age, education level, marriage status, employment status, any PTSD diagnosis, any substance use disorder diagnosis, any antidepressant prescription
Table 4.
Reverse Stepwise Regression Models of PROMIS Anxiety Scale with MAIA Subscales as Predictors
| Primary Predictors | Coef | SE | 95% CI |
|---|---|---|---|
| Not Worrying | −1.31*** | 0.32 | −1.95 - −0.68 |
| Trusting | −0.61* | 0.3 | −1.20 - −0.03 |
| Not Distracting | −0.46 | 0.34 | −1.12 - 0.20 |
| Emotional Awareness | 1.21*** | 0.34 | 0.54 - 1.88 |
| Self-regulation | −0.05 | 0.44 | −0.91 - 0.82 |
| PROMIS Depression | 0.51*** | 0.04 | 0.43 – 0.59 |
p<0.05
p<0.01
p<0.001
Adjusting for gender, race/ethnicity, age, education level, marriage status, employment status, any PTSD diagnosis, any substance use disorder diagnosis, any antidepressant prescription
4. Discussion
To the best of our knowledge, this is the first study to evaluate the relationship between depression severity categories and the MAIA (Mehling et al., 2012) subscales, providing a novel and useful assessment of interoceptive awareness. We hypothesized that patients with greater depression severity would have lower scores on the MAIA subscales of noticing, attention regulation, self-regulation, body listening and trusting and higher scores on the subscale of not distracting. We also hypothesized that when controlling for anxiety symptoms, the relationships between greater depression severity, trusting and not distracting would remain significant. In our final, fully adjusted model, after correcting for multiple comparisons, our hypothesis was supported for noticing, body listening and trusting. Expanding our hypothesis, individuals with greater depression severity also had lower levels of emotional awareness whereas there was no relationship with attention regulation or not distracting.
Overall, primary care patients with moderate to severe levels of depression were less self-aware of body sensations (“noticing”) and the connection between these sensations and their emotions (“emotional awareness”). They also report being less able to listen to the body for cues or insight (“body listening”) compared with individuals with less severe depressive symptoms. Interestingly, as severity of depression increased from mild to more severe, there was a progressive lack of experiencing one’s body as safe and trustworthy (“trusting”). A lack of trust in what our body sensations are telling us, therefore, appears particularly important for understanding how individuals with depression interpret or respond to interoceptive stimuli. Since there is less trust even in mild depression, it is possible that loss of trust in the meaning of body sensations precedes a reduction in other facets of interoception, such as the tendency to listen to body sensations, to notice body sensations or to be able to use interoceptive sensations to inform emotional awareness. This is a hypothesis that should be tested in future longitudinal studies.
Very little research exists examining the specific role of interoceptive trust in depression. In line with our results, in a sample of African-American women with heart disease, greater severity of depression was linked to less trust in one’s body (Solano-Lopez & Moore, 2018). Many studies report on hypoactivation, lack of feeling of body sensations associated with emotion (e.g. Nummenmaa, Glerean, Hari & Hietanend, 2014), body-dissatisfaction (e.g. Orbach, 2003; Scheffers et al., 2018) or detachment among persons with depression (e.g. Fuchs, 2013; Mitsue & Yamamoto, 2019). Our results, showing that there are reductions in interoceptive trust of one’s own body at mild, as well as increasingly at moderate to severe levels of depression, may help explain these previous findings. Specifically, in persons with depression, a lack of body trusting likely results in hypoawareness, decreased accuracy, altered prediction, misinterpretation or ineffective appraisal of interoceptive stimuli (Brewer, Cook & Bird, 2016; Farb et al., 2015; Khoury et al., 2018; Limmer et al., 2015). This may create a feedback loop and gradually decrease trust in one’s body during depressive states. These means of interoceptive processing could lead to avoidance, poor self-care, delayed treatment seeking, or difficulties interpreting the emotional or non-affective needs (e.g. hunger) of others (Brewer et al., 2016).
Mindfulness-based interventions, such as mindfulness based stress reduction (Grossman, Niemann, Schmidt & Walachcd, 2004) and mindfulness based cognitive therapy (Piet & Hougaard, 2011) may be effective in treating depression because they incorporate mindful movement, a systematic cultivation of awareness of body sensations, a focus on listening to and trusting the body, and a link between body sensations and emotions (Datko et al., 2019; Gawande et al., 2019; Loucks et al., 2019; Schuman-Olivier et al., 2020). For example, following mindfulness based cognitive therapy, persons with chronic pain and comorbid depression had improved interoceptive self-regulation and an increased tendency not to ignore bodily sensations of pain and discomfort (de Jong et al., 2016). The MAIA subscales of body listening and trusting were not examined in this study, however. More research examining the effects of mindfulness-based interventions on interoceptive awareness, specifically interoceptive trust, and subsequent emotion regulation and self-regulation, behavior change, service utilization and other health related variables in persons with depression is needed.
Anxiety is a common comorbid symptom for persons with depression (Kessler et al., 2015; Malhi & Mann, 2018). Co-occurring anxiety appears to play an impactful role in the relationship between depression and interoceptive awareness. After adjusting for anxiety, the relationship between depression and five (noticing, not distracting, not worrying, emotional awareness and body listening) out of the eight total MAIA subscales of interoceptive awareness changed. Specifically, the inverse relationships between depressive symptoms and noticing, emotion regulation and body listening became significant, while relationships observed between depressive symptoms, not distracting and not worrying were no longer significant. The inverse relationships between depression, self-regulation and trusting did not change when controlling for anxiety. Our results remained consistent after further controlling for demographic variables, substance use disorder, post-traumatic stress disorder and antidepressant use. This may be because unlike individuals with only depression, persons with panic or anxiety disorders may have hyperawareness or hyper-anticipation of specific internal states (Farb et al., 2015; Lackner & Fresco, 2016; Limmer et al., 2015). As such, a neutral or otherwise non-threatening stimuli (e.g. elevated heart rate) may cause extreme distress leading to increased and potentially unnecessary medication use or treatment seeking. Many researchers and clinicians are eager to understand why anxiety and depression are so often co-morbid. This study suggests that interoceptive dysregulation may play a unique role in those who have depression with co-occurring anxiety symptoms and MAIA subscale scores may predict some index of comorbidity. When state anxiety is high, people may develop hyperawareness and increased worrying about body sensations, but as they progress in a major depressive episode they may stop listening to their body sensations, then stop noticing what their body is telling them, ultimately losing connection with body sensations necessary for emotional awareness and self-regulation.
Although multiple MAIA subscales (e.g. not worrying, self-regulation, trusting) were associated with depression, in adjusted models using reverse stepwise regression, only trusting and anxiety account for unique variance in scores. This may be due to the high level of comorbidity between depression and anxiety, and overlapping symptoms, such that level of anxiety drives much of the way in which a person with depression relates to the internal status of their body. When using reverse stepwise regression of MAIA subscales with anxiety as an outcome variable, not worrying, emotional awareness and depression were significantly associated, further indicating some variability but a high level of overlap overall. Taken together with our regression models, the significantly lower scores on the MAIA subscale of not worrying appear to be unique to those with a presentation of anxiety separate from co-occurring depression. The specific interoceptive profile of an individual may provide a measure of where on the spectrum of depression and anxiety a person falls at a particular time.
Importantly, the relationship between depression and trusting one’s body did not change when controlling for anxiety. This particular facet of interoception, therefore, is likely important for individuals with depression, as well as those with depression and co-occurring anxiety. However, changes to other subscales or clusters of subscales of interoceptive awareness (e.g. noticing, not distracting, not worrying, emotional awareness and body listening) could indicate presence of co-morbidity between depression and anxiety. Overall, differences and similarities in interoceptive profiles could be useful as diagnostic criteria in primary care settings, where assessment is lacking. Further, interoceptive profiles could serve as research domain criteria (RDoC) to uniquely classify subtypes of depression (Khalsa & Lapidus, 2016; Khoury et al., 2018).
Our findings should be considered in the context of several limitations. First, the study uses cross-sectional data and the identified associations should not be considered causal as we cannot determine temporality of outcome and exposure. Future studies should capitalize on data over multiple time points and consider longitudinal modeling. In addition, the potential mediating role of interoceptive awareness and body trust on the effect mindfulness training has on ameliorating depression and preventing depressive relapse should be examined. Second, the study population consists of primary care patients. As such, our findings are not generalizable to patient populations receiving services in different clinical settings. Further, participants in our sample tended to be highly educated, which may impact the relationship between interoception and depression. Third, the MAIA is a subjective, self-report measure which presents potential limitations including response bias, inaccurate self-appraisal or misinterpretation of questions. Interoceptive awareness as measured by the MAIA does not necessarily relate to interoceptive accuracy. Interoceptive awareness is an emerging area of research awaiting clear characterization. It has been suggested that two main definitions of interoception exist including a narrow definition representing specifically sensory perception of interoceptive stimuli and then a broad definition which also includes interoceptive attention quality, interoceptive appraisal, and interoceptive regulation processes (Khoury et al., 2018). While the MAIA is a promising measure, more work is needed to examine the relationship between MAIA scales and other interoceptive constructs elucidated by other objective and subjective measures. However, overall our findings highlight a significant association between depression severity and different aspects of interoceptive awareness that can inform clinical practice and intervention development.
Despite these limitations, this was a novel study that examined the relationship between depression severity categories and a broad measure of interoceptive awareness among primary care patients. Our findings suggest that individuals with greater severity of depressive symptoms have lower levels of interoceptive awareness, specifically less awareness of body sensations and the connection between emotions and bodily responses and less likelihood to listen to and trust the body. Body trust, in particular, appears important for understanding how individuals with depression interpret or respond to interoceptive stimuli and may precede a reduction in other facets of interoception. These results help generate hypotheses about the mechanisms of action underlying hypoactivation, alexithymia, or detachment in persons with depression. This study supports the need for further research on interventions, such as mindfulness-based interventions, that enhance interoceptive awareness, in order to investigate the role of interoceptive awareness enhancement as a putative mechanism for enhancing depression treatment.
References
- Abdi H (2007). Bonferroni and Šidák corrections for multiple comparisons. Encyclopedia of measurement and statistics, 3, 103–107. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: American Psychiatric Publishing. [Google Scholar]
- Akincigil A, & Matthews EB (2017). National rates and patterns of depression screening in primary care: Results from 2012 and 2013. Psychiatric Services, 68(7), 660–666. [DOI] [PubMed] [Google Scholar]
- Austin PC, & Steyerberg EW (2015). The number of subjects per variable required in linear regression analyses. Journal of Clinical Epidemiology, 68(6), 627–636. [DOI] [PubMed] [Google Scholar]
- Avery JA, Drevets WC, Moseman SE, Bodurka J, Barcalow JC, & Simmons WK (2014). Major depressive disorder is associated with abnormal interoceptive activity and functional connectivity in the insula. Biological Psychiatry, 76(3), 258–266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beissner F, Meissner K, Bär KJ, & Napadow V (2013). The autonomic brain: an activation likelihood estimation meta-analysis for central processing of autonomic function. The Journal of Neuroscience: The Official Journal of the Society for Neuroscience, 33(25), 10503–10511. 10.1523/JNEUROSCI.1103-13.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beleckas CM, Prather H, Guattery J, Wright M, Kelly M, & Calfee RP (2018). Anxiety in the orthopedic patient: using PROMIS to assess mental health. Quality of Life Research, 27(9), 2275–2282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer R, Cook R, & Bird G (2016). Alexithymia: a general deficit of interoception. Royal Society Open Science, 3(10), 150664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choi SW, Schalet B, Cook KF, & Cella D (2014). Establishing a common metric for depressive symptoms: Linking the BDI-II, CES-D, and PHQ-9 to PROMIS Depression. Psychological Assessment, 26(2), 513–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clover K, Lambert SD, Oldmeadow C, Britton B, King MT, Mitchell AJ, & Carter G (2018). PROMIS depression measures perform similarly to legacy measures relative to a structured diagnostic interview for depression in cancer patients. Quality of Life Research, 27(5), 1357–1367. [DOI] [PubMed] [Google Scholar]
- Datko M, Lutz J, Gawande R, To M, Desel T, Napadow V, … & Desbordes G (2019, June). Effects of 8-week mindfulness training on BOLD fMRI response during an interoceptive attention task. Poster session presented at Organization for Human Brain Mapping (OHBM) 25th Annual Meeting, Lazio, Italy. [Google Scholar]
- de Groat WC, Griffiths D, & Yoshimura N (2015). Neural control of the lower urinary tract. Comprehensive Physiology, 5(1), 327–396. 10.1002/cphy.c130056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Jong M, Lazar SW, Hug K, Mehling WE, Hölzel BK, Sack AT, … & Gard T (2016). Effects of mindfulness-based cognitive therapy on body awareness in patients with chronic pain and comorbid depression. Frontiers in psychology, 7, 967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeVille DC, Kerr KL, Avery JA, Burrows K, Bodurka J, Feinstein JS, … & Simmons WK (2018). The neural bases of interoceptive encoding and recall in healthy adults and adults with depression. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 3(6), 546–554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Del Negro CA, Funk GD, & Feldman JL (2018). Breathing matters. Nature reviews. Neuroscience, 19(6), 351–367. 10.1038/s41583-018-0003-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn BD, Dalgleish T, Ogilvie AD, & Lawrence AD (2007). Heartbeat perception in depression. Behaviour Research and Therapy, 45(8), 1921–1930. [DOI] [PubMed] [Google Scholar]
- Dunn BD, Stefanovitch I, Evans D, Oliver C, Hawkins A, & Dalgleish T (2010). Can you feel the beat? Interoceptive awareness is an interactive function of anxiety-and depression-specific symptom dimensions. Behaviour Research and Therapy, 48(11), 1133–1138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb N, Daubenmier J, Price CJ, Gard T, Kerr C, Dunn BD, … & Mehling WE (2015). Interoception, contemplative practice, and health. Frontiers in Psychology, 6, 763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fissler M, Winnebeck E, Schroeter T, Gummersbach M, Huntenburg JM, Gaertner M, & Barnhofer T (2016). An investigation of the effects of brief mindfulness training on self-reported interoceptive awareness, the ability to decenter, and their role in the reduction of depressive symptoms. Mindfulness, 7(5), 1170–1181. [Google Scholar]
- Fuchs T (2013). Depression, intercorporeality, and interaffectivity. Journal of Consciousness Studies, 20(7-8), 219–238. [Google Scholar]
- Garfinkel SN, Seth AK, Barrett AB, Suzuki K, & Critchley HD (2015). Knowing your own heart: distinguishing interoceptive accuracy from interoceptive awareness. Biological Psychology, 104, 65–74. [DOI] [PubMed] [Google Scholar]
- Gawande R, To MN, Pine E, Griswold T, Creedon TB, Brunel A, Lozada A, Loucks EB, & Schuman-Olivier Z (2019). Mindfulness Training Enhances Self-Regulation and Facilitates Health Behavior Change for Primary Care Patients: A Randomized Controlled Trial. Journal of General Internal Medicine, 34(2), 293–302. 10.1007/s11606-018-4739-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green SB (1991). How many subjects does it take to do a regression analysis? Multivariate Behavioral Research, 26, 499–510. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, & Walach H (2004). Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research, 57(1), 35–43. [DOI] [PubMed] [Google Scholar]
- Hadjikhani N, Ward N, Boshyan J, Napadow V, Maeda Y, Truini A, Caramia F, Tinelli E, & Mainero C (2013). The missing link: enhanced functional connectivity between amygdala and visceroceptive cortex in migraine. Cephalalgia: An International Journal of Headache, 33(15), 1264–1268. 10.1177/0333102413490344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hahm HC, Cook BL, Ault-Brutus A, & Alegría M (2015). Intersection of race-ethnicity and gender in depression care: screening, access, and minimally adequate treatment. Psychiatric Services (Washington, D.C.), 66(3), 258–264. 10.1176/appi.ps.201400116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harshaw C (2015). Interoceptive dysfunction: Toward an integrated framework for understanding somatic and affective disturbance in depression. Psychological Bulletin, 141(2), 311–363. 10.1037/a0038101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herbert BM, & Pollatos O (2012). The body in the mind: on the relationship between interoception and embodiment. Topics in Cognitive Science, 4(4), 692–704. [DOI] [PubMed] [Google Scholar]
- Indu PS, Anilkumar TV, Pisharody R, Russell PSS, Raju D, Sarma PS, … & Andrade C (2017). Prevalence of depression and past suicide attempt in primary care. Asian Journal of Psychiatry, 27, 48–52. [DOI] [PubMed] [Google Scholar]
- Keller JA, Chen J, Simpson S, Wang EH, Lilascharoen V, George O, Lim BK, & Stowers L (2018). Voluntary urination control by brainstem neurons that relax the urethral sphincter. Nature Neuroscience, 21(9), 1229–1238. 10.1038/s41593-018-0204-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Sampson NA, Berglund P, Gruber MJ, Al-Hamzawi A, Andrade L, Bunting B, Demyttenaere K, Florescu S, de Girolamo G, Gureje O, He Y, Hu C, Huang Y, Karam E, Kovess-Masfety V, Lee S, Levinson D, Medina Mora ME, Moskalewicz J, … Wilcox MA (2015). Anxious and non-anxious major depressive disorder in the World Health Organization World Mental Health Surveys. Epidemiology and Psychiatric Sciences, 24, 210–226. 10.1017/S2045796015000189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalsa SS, & Lapidus RC (2016). Can interoception improve the pragmatic search for biomarkers in psychiatry? Frontiers in Psychiatry, 7, 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalsa SS, Adolphs R, Cameron OG, Critchley HD, Davenport PW, Feinstein JS, … & Meuret AE (2018). Interoception and mental health: A roadmap. Biological Psychiatry: Cognitive Neuroscience and Neuroimaging, 3(6), 501–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khalsa SS, Feinstein JS, Simmons WK, & Paulus MP (2018). Taking Aim at Interoception's Role in Mental Health. Biological psychiatry. Cognitive neuroscience and neuroimaging, 3(6), 496–498. 10.1016/j.bpsc.2018.04.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoury NM, Lutz J, & Schuman-Olivier Z (2018). Interoception in Psychiatric Disorders: A Review of Randomized Controlled Trials with Interoception-based Interventions. Harvard Review of Psychiatry, 26(5), 250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleckner IR, Wormwood JB, Simmons WK, Barrett LF, & Quigley KS (2015). Methodological recommendations for a heartbeat detection-based measure of interoceptive sensitivity. Psychophysiology, 52(11), 1432–1440. 10.1111/psyp.12503 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kluwer W (2018). Medi-Span Generic Product Identifier (GPI). Accessed from: https://www.wolterskluwercdi.com/drug-data/gpi/.
- Lackner RJ, & Fresco DM (2016). Interaction effect of brooding rumination and interoceptive awareness on depression and anxiety symptoms. Behaviour Research and Therapy, 85, 43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Limmer J, Kornhuber J, & Martin A (2015). Panic and comorbid depression and their associations with stress reactivity, interoceptive awareness and interoceptive accuracy of various bioparameters. Journal of Affective Disorders, 185, 170–179. [DOI] [PubMed] [Google Scholar]
- Loucks EB, Nardi WR, Gutman R, Kronish IM, Saadeh FB, Li Y, … & Britton WB (2019). Mindfulness-Based Blood Pressure Reduction (MB-BP): Stage 1 single-arm clinical trial. PloS one, 14(11). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma-Kellams C (2014). Cross-cultural differences in somatic awareness and interoceptive accuracy: A review of the literature and directions for future research. Frontiers in Psychology, 5, 1379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Malhi G, & Mann J (2018). Depression. The Lancet, 392(10161), 2299–2312. [DOI] [PubMed] [Google Scholar]
- Mayer E (2013). Gut sensations – Not so gut specific after all? PAIN, 154(5), 627–628. doi: 10.1016/j.pain.2013.02.014 [DOI] [PubMed] [Google Scholar]
- Mehling WE, Daubenmier J, Price CJ, Acree M, Bartmess E, & Stewart AL (2013). Self-reported interoceptive awareness in primary care patients with past or current low back pain. Journal of Pain Research, 6, 403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehling WE, Gopisetty V, Daubenmier J, Price CJ, Hecht FM, & Stewart A (2009). Body awareness: Construct and self-report measures. PloS one, 4(5), e5614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mehling WE, Price C, Daubenmier JJ, Acree M, Bartmess E, & Stewart A (2012). The Multidimensional Assessment of Interoceptive Awareness (MAIA). PLoS ONE, 7(11), Article e48230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitsue S, & Yamamoto T (2019). Relationship between depression and movement quality in normal young adults. Journal of Physical Therapy Science, 31(10), 819–822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nummenmaa L, Glerean E, Hari R, & Hietanen JK (2014). Bodily maps of emotions. Proceedings of the National Academy of Sciences of the United States of America, 111(2), 646–651. 10.1073/pnas.1321664111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olivan-Blázquez B, Rubio-Aranda E, García-Sanz O, Magallón-Botaya R (2016). Correlation between diagnosis of depression and symptoms present in primary care patients. Actas Esp Psiquiatr, 44(2), 55–63. [PubMed] [Google Scholar]
- Orbach I, Gilboa-Schechtman E, Sheffer A, Meged S, Har-Even D, & Stein D (2006). Negative bodily self in suicide attempters. Suicide and Life-Threatening Behavior, 36(2), 136–153. [DOI] [PubMed] [Google Scholar]
- Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, … & Schatzberg AF (2016). Major depressive disorder. Nature Reviews Disease Primers, 2(1), 1–20. [DOI] [PubMed] [Google Scholar]
- Paulus MP, & Stein MB (2010). Interoception in anxiety and depression. Brain structure and Function, 214(5-6), 451–463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piet J, & Hougaard E (2011). The effect of mindfulness-based cognitive therapy for prevention of relapse in recurrent major depressive disorder: a systematic review and meta-analysis. Clinical Psychology Review, 31(6), 1032–1040. [DOI] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D, & PROMIS Cooperative Group. (2011). Item banks for measuring emotional distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): depression, anxiety, and anger. Assessment, 18(3), 263–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkonis PA, Yu L, Dodds NE, Johnston KL, Maihoefer CC, & Lawrence SM (2014). Validation of the depression item bank from the Patient-Reported Outcomes Measurement Information System (PROMIS®) in a three-month observational study. Journal of Psychiatric Research, 56, 112–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollatos O, Traut-Mattausch E, & Schandry R (2009). Differential effects of anxiety and depression on interoceptive accuracy. Depression and Anxiety, 26(2), 167–173. [DOI] [PubMed] [Google Scholar]
- Price C & Hooven C (2018). Interoceptive awareness skills for emotion regulation: Theory and approach of Mindful Awareness in Body-Oriented Therapy (MABT). Frontiers in Psychology, 9, 789. https://www.frontiersin.org/article/10.3389/fpsyg.2018.00798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price CJ, Thompson EA, Crowell S, & Pike K (2019). Longitudinal effects of interoceptive awareness training through mindful awareness in body-oriented therapy (MABT) as an adjunct to women’s substance use disorder treatment: A randomized controlled trial. Drug and Alcohol Dependence, 198, 140–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scheffers M, van Duijn MAJ, Beldman M, Bosscher RJ, van Busschbach JT, & Schoevers RA (2019). Body attitude, body satisfaction and body awareness in a clinical group of depressed patients: An observational study on the associations with depression severity and the influence of treatment. Journal of Affective Disorders, 242, 22–28. [DOI] [PubMed] [Google Scholar]
- Schuman-Olivier Z, Trombka M, Lovas DA, Brewer JA, Vago DR, Gawande R, … & Fulwiler C (2020). Mindfulness and Behavior Change. Harvard review of psychiatry, 28(6), 371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sliz D, & Hayley S (2012). Major depressive disorder and alterations in insular cortical activity: A review of current functional magnetic imaging research. Frontiers in Human Neuroscience, 6, 323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith K, & De Torres IBC (2014). A world of depression. Nature, 515. [DOI] [PubMed] [Google Scholar]
- Smith Ryan & Gudleski Gregory & Lane Richard & Lackner Jeff. (2019). Higher emotional awareness is associated with reduced pain in irritable bowel syndrome patients: Preliminary results. Psychological Reports. doi: 10.1177/0033294119868778. [DOI] [PubMed] [Google Scholar]
- Solano Lopez AL, & Moore S (2019). Dimensions of Body-Awareness and Depressed Mood and Anxiety. Western Journal of Nursing Research, 41(6), 834–853. [DOI] [PubMed] [Google Scholar]
- Sunderland M, Batterham P, Calear A, & Carragher N (2018). Validity of the PROMIS depression and anxiety common metrics in an online sample of Australian adults. Quality of Life Research, 27(9), 2453–2458. [DOI] [PubMed] [Google Scholar]
- VanVoorhis CW, & Morgan BL (2007). Understanding power and rules of thumb for determining sample sizes. Tutorials in Quantitative Methods for Psychology, 3(2), 43–50. [Google Scholar]
- Walker J, Burke K, Wanat M, Fisher R, Fielding J, Mulick A, … & Frost C (2018). The prevalence of depression in general hospital inpatients: A systematic review and meta-analysis of interview-based studies. Psychological Medicine, 48(14), 2285–2298. [DOI] [PubMed] [Google Scholar]
- Zimmerman C, Huey E, Ahn J, Beutler L, Tan C, Kosar S, Bai L, Chen Y, Corpuz T, Madisen L, Zeng H & Knight Z (2019) A gut-to-brain signal of fluid osmolarity controls thirst satiation. Nature 568, 98–102 (2019). 10.1038/s41586-019-1066-x [DOI] [PMC free article] [PubMed] [Google Scholar]