Abstract
Background
Recent insights suggest that remnant cholesterol (RC) plays a role in cellular senescence, yet its specific contribution to frailty remains indeterminate. Through the integration of observational and mendelian randomization (MR) studies, this research explores the impact of elevated serum RC levels on frailty susceptibility.
Methods
A dual-method approach, combining an observational study with an MR study, was employed to investigate the connection between RC and frailty. The observational study included 11,838 participants from the National Health and Nutrition Examination Survey. Multivariable logistic regression and propensity score matching were employed to control for potential confounders. The non-linear relationship was assessed using restricted cubic splines. To circumvent observational study limitations, a two-sample MR analysis was conducted using the inverse-variance weighted method, leveraging genome-wide association studies (GWAS) data.
Results
After adjusting for potential confounding variables, the observational study identified a significant association between high serum RC levels and frailty in middle-aged and older adults (odds ratio [OR] = 1.67, 95% confidence interval [CI] = 1.20 to 2.33, P = 0.003), exhibiting a non-linear dose–response correlation (non-linear P = 0.011). This association persisted after propensity score matching (OR = 1.53, 95% CI = 1.14 to 2.06, P = 0.005). The MR study echoed these results, demonstrating a causal association of RC with the frailty index (β = 0.059, 95% CI = 0.033 to 0.085, P = 1.05E-05), consistent with the observational findings (β = 0.017, 95% CI = 0.008 to 0.026, P = 4.51E-04).
Conclusion
This study provides evidence that higher RC levels amplify frailty risk in middle-aged and older adults, implying that the reduction of RC levels may present a promising strategy for frailty prevention and management.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12944-023-01882-4.
Keywords: Frailty, Remnant cholesterol, Aging, Mendelian randomization
Introduction
With advancing age, individuals tend to experience a progressive accumulation of health-related deficits, which eventually leads to cumulating in a state of frailty. This clinical condition, characterized by vulnerability, signifies severe dysregulation within a biologically complex dynamical system inherent to the aging process [1–3]. Epidemiological evidence underscores the high prevalence of frailty among the elderly demographic. For instance, a comprehensive meta-analysis incorporating 57 studies revealed that frailty affects approximately 26.8% of the aging population [4]. Given the heightened predisposition of this demographic to adverse clinical outcomes, there is a growing emphasis on the early identification and modification of risk factors related to frailty.
In the elderly population, frailty is associated with a significantly increased risk for the development of cardiovascular disease (CVD) and the occurrence of major adverse cardiovascular events [5, 6]. Evidence from a Mendelian randomization (MR) study underscores a bidirectional causal relationship between frailty and coronary heart disease (CHD) [7]. This correlation could stem from shared risk factors [8], especially the elevated serum level of cholesterol. Previous research has indicated a correlation between increased serum levels of low-density lipoprotein cholesterol (LDL-C) and the risk of frailty[9]. Numerous researches in recent years have identified remnant cholesterol (RC) as an independent risk factor that contributes to the occurrence of incident cardiovascular events [10–12]. RC is computed as the difference between total cholesterol (TC) and the aggregate of high-density lipoprotein cholesterol (HDL-C) and LDL-C, primarily representing the cholesterol content of a subset of triglyceride-rich lipoproteins (TRLs) [13]. One proposed mechanism suggests that hydrolyzed products from TRLs may expedite cellular senescence in a range of cells, including endothelial cells, vascular smooth muscle cells, macrophages, and adipose-derived mesenchymal stem cells (AMSC) [14]. While direct evidence is available for AMSC, supporting evidence for other cell types remains largely indirect [15]. Cellular senescence at the cellular level is a crucial mechanism driving frailty [16]. However, the exact mechanism through which RC is associated with the risk of frailty remains to be elucidated.
The aim of this study was to examine the potential association between RC and frailty through two distinct, yet complementary approaches. The initial phase of the investigation involved an observational study using data from the National Health and Nutrition Examination Survey (NHANES) to assess the association. However, acknowledging the limitations of observational studies, primarily the prevalence of confounding factors and potential for reverse causality, a MR study was also employed. In the MR study, genetic variants that influence serum remnant cholesterol levels were utilized as instrumental variables, simulating the conditions of a randomized experiment. This technique leverages the natural random distribution of genetic variants during gamete formation and conception, thereby effectively mitigating confounding elements and the risk of reverse causality. Such an approach provides a more robust evidence base supporting any potential causal link between RC and frailty [17].
Materials and methods
Study population for the observational epidemiological study
The present observational study leveraged data across eight NHANES cycles spanning from 2003–2004 through 2017–2018. The NHANES is a nationally representative survey dedicated to assessing the health and nutritional condition of both adult and pediatric populations in the United States [18]. The inclusion criteria for this study specified non-institutionalized individuals aged 40 years and above who had undergone lipid profiling. Subjects with triglyceride levels equal to or exceeding 400 mg/dl were excluded from the study. Protocols #98–12, #2005–06, #2011–17, and #2018–01 were granted approval by the Institutional Review Board of the National Center for Health Statistics (NCHS) [19].
Measurement of variables in the observational epidemiological study
For this observational epidemiological study, the primary exposure variables comprised of RC, RC-to-TC ratio, and TC-to-LDL-C ratio. RC was deduced by subtracting HDL-C and LDL-C from TC. As LDL-C direct measurements were not provided by NHANES, its levels for the primary analyses were calculated using the Martin-Hopkins equation [20]. A preceding study [21] demonstrated that the Martin-Hopkins equation provides more accurate estimations of LDL-C (for triglyceride levels of < 400 mg/dl) compared to the Friedewald [22] and Sampson equations [23]. For comparison, LDL-C values were also computed using the Friedewald and Sampson equations.
Frailty status, defined by the frailty index (FI), was identified as the primary outcome measure. FI was determined using 49 accessible items, based on the deficit accumulation approach proposed by Rockwood et al. (Supplementary Table 1) [24]. FI was computed by dividing the sum of deficits by the total number of items, yielding a score between 0 and 1. Participants possessing an FI greater than 0.21 were classified as frail [25, 26]. Concurrently, the Fried frailty phenotype (FP) was assessed according to a formerly published method [27]; meeting at least three criteria was deemed indicative of frailty [3].
The study accounted for various covariates, including sociodemographic attributes, socioeconomic status, lifestyle behaviors, frailty-associated risk factors, clinical comorbidities, and current medications. The sociodemographic variables included age, gender, ethnicity, education level, and marital status. Household income as a percentage of the federal poverty level (FPL) was utilized to gauge the socioeconomic status, categorized as poor (≤ 100% FPL), near poor (101–200% FPL), or non-poor (> 200% FPL). The healthy eating index—2015 (HEI-2015) was employed to evaluate dietary behaviors, which assesses adherence to the 2015–2020 Dietary Guidelines for Americans. The smoking status was segmented into three categories: never, former, or current. “Never smokers” were those who smoked fewer than 100 cigarettes throughout their lifetime. “Current smokers” referred to those who consumed more than 100 cigarettes in their lifetime and were still active smokers. “Former smokers” were those who ceased smoking after consuming more than 100 cigarettes. The study also included frailty-related risk factors such as body mass index (BMI), systolic blood pressure (SBP), diastolic blood pressure (DBP), and estimated glomerular filtration rate (eGFR), which was computed using creatinine-based eGFR (eGFRCr) via the CKD-EPI (CKD Epidemiology Collaboration) equations [28]. Self-reported histories of cardiovascular disease (CVD) and Type 2 diabetes mellitus (T2DM) were counted as clinical comorbidities. CVD was defined as self-reported instances of CHD, congestive heart failure (HF), heart attacks, strokes, or angina. The study also accounted for covariates, which included information on the current usage of specific medications, such as statins, anti-diabetic drugs, and anti-hypertensive drugs.
Data Source for mendelian randomization study
In the MR analyses, summary-level data from large-scale genome-wide association studies (GWAS) were utilized to assess the potential causal influence of RC on frailty. The GWAS summary data for RC was procured from the UK Biobank, encompassing data from 115,082 participants [29]. The quantification of remnant cholesterol was computed as the TC minus the sum of LDL-C and HDL-C. The TC, LDL-C, and HDL-C values were acquired through high-throughput nuclear magnetic resonance metabolomics conducted by Nightingale Health (biomarker quantification version 2020) [29]. The data were subsequently adjusted for variables such as age, sex, fasting status, and the genotyping array.
The GWAS summary data for the FI was derived from a meta-analysis of UK Biobank participants of European descent (N = 164,610) and Swedish TwinGene participants (N = 10,616) [30]. The UK Biobank participants were aged between 60 to 70 years, and the Swedish TwinGene participants ranged from 41 to 87 years. During the GWAS meta-analysis, covariate adjustments were made for age, sex, assessment center, and the genotyping array. The GWAS summary data for the FP was obtained from the study conducted by Ye et al., involving 386,565 individuals of European ancestry from the UK Biobank [31]. The GWAS summary statistics are compiled in Supplementary Table 2.
Selection of genetic instruments
This study entailed the selection of single nucleotide polymorphisms (SNPs) that exhibited a significant association with RC, FI, or FP (P < 5 × 10−8), and independent segregation (R2 < 0.001, within a 5000 kb window), with no evidence of linkage disequilibrium (LD). A clumping algorithm employed, referencing the 1000 genomes panel, to identify and exclude SNPs displaying LD. Furthermore, SNPs demonstrating palindrome alleles (A/T or G/C), which could potentially lead to strand ambiguity issues, were excluded from the study. The F-statistic was computed using a formula outlined in prior research, and SNPs demonstrating an F-statistic exceeding 10 were deemed as strong genetic instrumental variables (IVs) for RC level, consistent with the Staiger-Stock rule [32, 33].
Statistical analysis of observational epidemiological study
All analyses were performed using sampling weights, strata, and primary sampling units to ensure the derivation of nationally representative estimates. To circumvent the reduction in sample size attributable to missing covariate data, these gaps were filled in using the missForest method within the missForest R package. Spearman rank correlation coefficient tests were conducted to analyze the correlation between LDL-C values as calculated by different formulas.
Logistic regression analyses were employed to determine the association between RC, RC-to-TC ratio, RC-to-LDL-C ratio, and the likelihood of frailty. Further, FI, treated as a continuous outcome variable, was included in the linear regression model for subsequent re-analysis. We utilized two different methods to correct for the influence of confounding factors. The presence of multicollinearity was verified using the generalized variance inflation factor (GVIF), with variables exhibiting a GVIF > 10 excluded from the model. Three models were fitted in a stepwise manner. Model 1 adjusted for age (continuous), gender (female and male), ethnicity (white, black, or other), education level (below high school, or high school and above), family income (poor, near poor, or non-poor), and marital status (non-married or married). Model 2 accommodated the variables in model 1 and also adjusted for smoking status (never, former, or current) and HEI-2015 (quartile). Model 3 incorporated the variables from model 2 and further adjusted for BMI (continuous), SBP (continuous), DBP (continuous), eGFR level (≥ 90, 60 to 89, and < 60 mL/min per 1.73 m2), CVD (no or yes), T2DM (no or yes), statins use (no or yes), anti-diabetic drug use (no or yes), and anti-hypertensive drug use (no or yes). For RC, model 4 was created, which included TC (continuous) and LDL-C (continuous) adjustments in addition to the variables in model 3. Secondly, a 1:1 propensity score matching (PSM) method was employed to control for potential confounding variables, considering all variables in model 3 and sampling weights. The nearest-neighbor matching was conducted within a caliper of 0.05 on the propensity score scale, using the MatchIt R package. Lastly, to model a potential dose–response relationship of RC with frailty, the restricted cubic splines (RCS) with three knots were applied.
The relationship between RC, the RC-to-TC ratio, and the RC-to-LDL-C ratio with the likelihood of frailty was scrutinized in various demographic subgroups. These were divided by age (< 60 and ≥ 60 years), gender (female and male), BMI (< 30 and ≥ 30 kg/m2), eGFR level (≥ 90, 60 to 89, and < 60 mL/min per 1.73 m2), presence of CVD or T2DM (no or yes), and hypertension (no or yes) in the logistic models. Hypertension was defined as SBP ≥ 140 mmHg, DBP ≥ 90 mmHg, or current utilization of anti-hypertensive medications. The multiplicative interaction and the determination of effect size variations among different population subgroups were assessed via likelihood ratio tests.
Complementary sensitivity analyses were conducted. Firstly, the association of RC with frailty was re-evaluated excluding heart failure, coronary heart disease, angina, heart attack, stroke, and T2DM from the FI. Subsequently, differing strategies for managing missing values were employed for sensitivity analysis, encompassing direct deletion of missing values and multiple imputation. Ten complete datasets were synthesized via multiple imputation using the mice R package. Given the intricate sampling design, results were consolidated in accordance with Rubin’s rule, utilizing the survey and mitools R packages in R. Finally, the results generated using the Friedewald equation and Sampson equation were juxtaposed with the principal results.
All computations were conducted using R and RStudio software. To correct for the three tested null-hypotheses, Bonferroni adjustment was applied (Bonferroni: 0.05/3 = 0.017). A P-value < 0.017 was considered as being statistically significant.
Mendelian randomization analysis
The causal effect of RC on the FI or FP was assessed employing the multiplicative random-effects inverse-variance weighted (IVW) method, undeterred by heterogeneity statistics. Additional MR methods, including weighted median, MR-Egger, simple median, and MR Pleiotropy RESidual Sum and Outlier (MR-PRESSO) were incorporated into the data analysis process. Reverse direction MR was conducted to evaluate any pre-existing reverse-direction causal association. The MR-Steiger directionality test was employed to validate causality directionality [34]. Multivariable MR, facilitated by the IVW method, was utilized to estimate the direct causal impact of RC on the FI, incorporating adjustments for TC, LDL-C, BMI, CHD, HF, stroke, T2DM, SBP, and DBP. The execution of these methods relied on the TwoSampleMR (version 0.5.6) [35] and MRPRESSO (version 1.0) R packages [36].
Three strategies were implemented to test for potential pleiotropy. First, the intercept test from MR-Egger regression served as the principal method to identify directional pleiotropy. The PhenoScanner web tool was utilized next, aiming to identify SNPs linked to potential confounders; such SNPs were then extracted from the IVs before re-analysis of the primary results [37]. The MR-PRESSO test was subsequently employed to identify and rectify horizontal pleiotropy through the MRPRESSO (version 1.0) R package [36]. Heterogeneity was quantified using the Cochran’s Q Statistic and I2 value, supported by visual assessment via funnel plot. After removing SNPs resulting in the heterogeneity, the main results were re-analyzed. After SNPs contributing to heterogeneity were removed, the primary results were revisited. The MRlap (version 0.0.3.0) R package was used to account for and rectify potential bias induced by sample overlap [38].
Results
Observational epidemiological analysis for association of RC with frailty
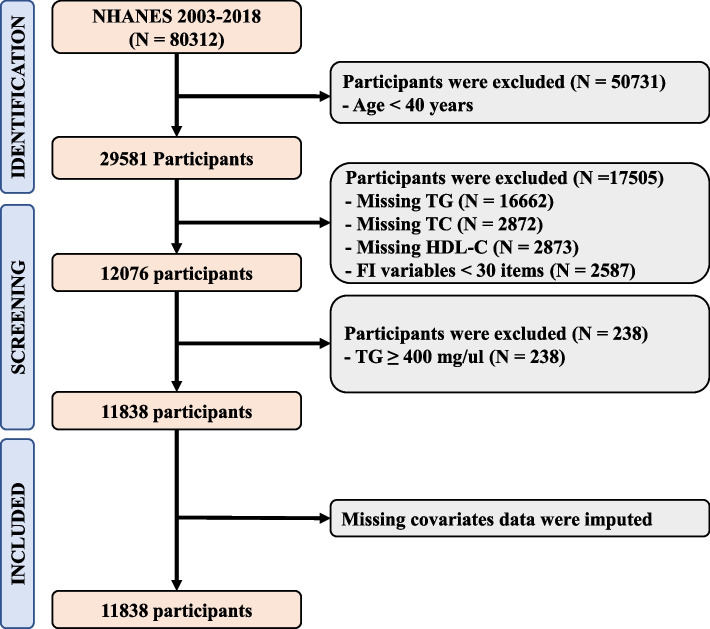
The study incorporated a total of 11,838 participants as delineated in Fig. 1. Given the sampling design, this represents a potential sampling of 58.32 million. A summary of the population characteristics is presented in Table 1. The participants’ average age was 59 (standard deviation [SD] 11.90), with 52.43% (6,059) being female. The average FI was 0.160 with a standard deviation of 0.002, and 24.88% of participants were categorized as frail according to the FI. Frail participants, in comparison to non-frail participants, were found to be older, with a higher BMI, higher SBP, lower DBP, lower eGFR, lower HEI-2015, and had a higher prevalence of CVD or T2DM. Correlation tests using Spearman method identified a significant positive correlation between LDL-C as determined by the Martin-Hopkins equation and the Friedewald equation (Spearman correlation = 0.988, P < 2.2E-16), as well as the Sampson equation (Spearman correlation = 0.998, P < 2.2E-16), as depicted in Supplementary Fig. 1.
Fig. 1.
Flowchart of Participant Inclusion and Exclusion
Table 1.
Population characteristics across frailty status
| Characteristics | Total (N = 17,052) |
Non-Frailty (N = 13,233) |
Frailty (N = 3819) |
P-value |
|---|---|---|---|---|
| Age, years | 59 (11.90) | 57 (11.46) | 63 (12.38) | 2.05E-30 |
| Gender | 1.16E-18 | |||
| Female | 6059 (52.43%) | 3973 (49.31%) | 2086 (61.84%) | |
| Male | 5779 (47.57%) | 4282 (50.69%) | 1497 (38.16%) | |
| Ethnicity | 2.63E-13 | |||
| White | 5545 (73.78%) | 3869 (75.30%) | 1676 (69.17%) | |
| Black | 2389 (9.60%) | 1520 (8.18%) | 869 (13.90%) | |
| Other | 3904 (16.62%) | 2866 (16.52%) | 1038 (16.93%) | |
| Education level | 2.66E-22 | |||
| Below High School | 3397 (17.66%) | 2043 (14.39%) | 1354 (27.54%) | |
| High School and above | 8441 (82.34%) | 6212 (85.61%) | 2229 (72.46%) | |
| Marital status | 2.49E-18 | |||
| Non-Married | 5056 (37.01%) | 3143 (33.09%) | 1913 (48.86%) | |
| Married | 6782 (62.99%) | 5112 (66.91%) | 1670 (51.14%) | |
| Family income | 8.30E-50 | |||
| Poor | 2012 (10.47%) | 1108 (7.55%) | 904 (19.27%) | |
| Near poor | 3375 (19.96%) | 2048 (16.06%) | 1327 (31.75%) | |
| Non-poor | 6451 (69.57%) | 5099 (76.39%) | 1352 (48.98%) | |
| Smoking status | 2.33E-15 | |||
| Never | 5980 (50.35%) | 4392 (53.18%) | 1588 (41.78%) | |
| Former | 3703 (31.48%) | 2495 (30.78%) | 1208 (33.61%) | |
| Current | 2155 (18.17%) | 1368 (16.04%) | 787 (24.61%) | |
| BMI, kg/m2 | 29 (6.64) | 29 (6.05) | 31 (7.86) | 1.81E-21 |
| SBP, mmHg | 126 (18.40) | 125 (17.69) | 129 (20.06) | 1.41E-15 |
| DBP, mmHg | 70 (11.69) | 71 (11.18) | 68 (12.88) | 7.33E-16 |
| HEI-2015 | 1.07E-12 | |||
| Quartile 1 | 2960 (26.04%) | 1929 (24.80%) | 1031 (29.78%) | |
| Quartile 2 | 2959 (24.67%) | 1961 (23.65%) | 998 (27.75%) | |
| Quartile 3 | 2959 (24.49%) | 2108 (24.36%) | 851 (24.89%) | |
| Quartile 4 | 2960 (24.80%) | 2257 (27.20%) | 703 (17.58%) | |
| eGFR, ml/min per 1.73 m2 | 4.68E-46 | |||
| ≥ 90 | 5104 (43.56%) | 3895 (45.87%) | 1209 (36.60%) | |
| 60 to 89 | 5106 (45.58%) | 3633 (47.14%) | 1473 (40.90%) | |
| < 60 | 1628 (10.85%) | 727 (7.00%) | 901 (22.50%) | |
| Type 2 DM | 2188 (13.96%) | 883 (8.15%) | 1305 (31.49%) | 8.66E-49 |
| CVD | 2100 (14.75%) | 692 (7.81%) | 1408 (35.69%) | 1.57E-52 |
| Statins use | 3296 (26.63%) | 1830 (21.86%) | 1466 (41.01%) | 4.36E-26 |
| Anti-diabetic drug use | 2012 (13.20%) | 837 (8.11%) | 1175 (28.56%) | 1.62E-43 |
| Anti-hypertensive drug use | 1122 (8.49%) | 680 (7.45%) | 442 (11.62%) | 2.61E-08 |
| TG, mg/dl | 109 (76, 158) | 105 (74, 153) | 121 (86, 175) | 1.54E-15 |
| TC, mg/dl | 197.94 (41.36) | 200.41 (39.95) | 190.49 (44.51) | 8.45E-16 |
| HDL-C, mg/dl | 55.64 (17.05) | 56.41 (16.85) | 53.33 (17.43) | 2.84E-10 |
| LDL-C, mg/dl | ||||
| Martin-Hopkins | 118.97 (35.72) | 121.10 (34.57) | 112.54 (38.28) | 9.28E-16 |
| Friedewald | 117.17 (36.32) | 119.70 (35.11) | 109.53 (38.77) | 3.83E-19 |
| Sampson | 119.71 (36.29) | 122.14 (35.17) | 112.38 (38.57) | 5.84E-18 |
| RC, mg/dl | ||||
| Martin-Hopkins | 23.33 (8.92) | 22.90 (8.69) | 24.62 (9.47) | 2.45E-10 |
| Friedewald | 25.13 (13.51) | 24.30 (13.08) | 27.63 (14.45) | 1.54E-15 |
| Sampson | 22.59 (11.79) | 21.86 (11.45) | 24.78 (12.49) | 3.90E-17 |
| RC to TC Ratio, % | ||||
| Martin-Hopkins | 11.15 (8.86, 14.31) | 10.71 (8.61, 13.74) | 12.47 (9.92, 15.51) | 1.91E-28 |
| Friedewald | 11.21 (7.93, 16.17) | 10.63 (7.62, 15.36) | 13.27 (9.44, 18.39) | 4.44E-28 |
| Sampson | 10.30 (7.39, 14.56) | 9.74 (7.04, 13.83) | 12.13 (8.75, 16.38) | 2.45E-29 |
| RC to LDL-C Ratio, % | ||||
| Martin-Hopkins | 18.78 (14.95, 24.31) | 17.95 (14.40, 23.27) | 21.32 (16.93, 27.39) | 1.49E-33 |
| Friedewald | 18.81 (13.15, 28.14) | 17.65 (12.50, 26.35) | 22.74 (16.06, 33.69) | 3.35E-33 |
| Sampson | 17.15 (12.16, 24.86) | 15.99 (11.51, 23.47) | 20.70 (14.80, 29.47) | 5.77E-34 |
Notes: Percentages, Mean value, and Standard deviation were weighted and accounted for the complex sampling design. Sample size was unweighted. BMI Body mass index RC Remnant cholesterol, TC Total cholesterol, LDL-C Low-density lipoprotein cholesterol, HEI-2015 Healthy Eating Index-2015, CVD Cardiovascular disease, DM Diabetes mellitus, eGFR Estimated glomerular filtration rate, SBP Systolic blood pressure, DBP Diastolic blood pressure
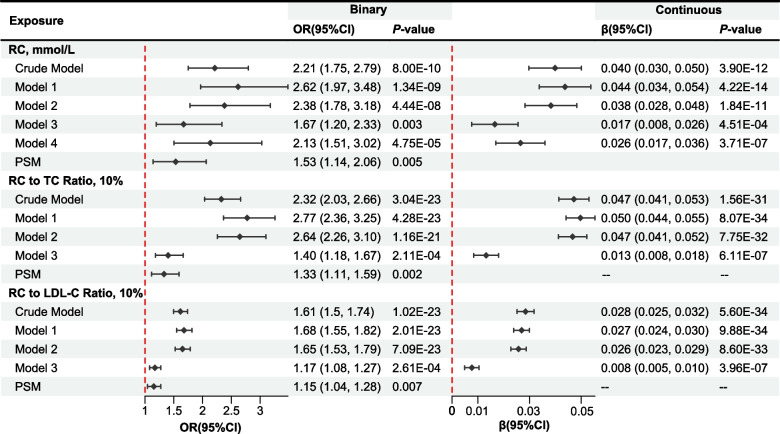
Upon adjusting for potential confounders, the study found a positive correlation between elevated serum RC levels and frailty as determined by FI (Fig. 2). In particular, the adjusted odds ratio (OR) of frailty for RC (calculated by the Martin-Hopkins equation) was determined as 1.67 (95% CI = 1.20 to 2.33, P = 0.003). A 1 mmol/L increase in serum levels of RC was associated with a 0.017 unit increase in continuous FI (β = 0.017 per 1 mmol/L increase in RC levels, 95% CI = 0.008 to 0.026, P = 4.51E-04). No multicollinearity was detected among the independent variables in model 3, as confirmed by the GVIF values (Supplementary Table 3). The relationship remained statistically significant after further adjusting for total cholesterol and LDL-C (model 4; Fig. 2). PSM achieved a satisfactory balance between the covariates in non-frail and frail groups (Supplementary Table 4), and RC maintained a significant correlation with the likelihood of frailty (OR = 1.53 per 1 mmol/L increase in RC levels, 95% CI = 1.14 to 2.06, P = 0.005). Nevertheless, there was no notable correlation detected between higher serum levels of RC and frailty as defined by FP (OR = 1.32 per 1 mmol/L increase in RC levels, 95% CI = 0.87 to 2.01, P = 0.192), as shown in Supplementary Table 5. Additionally, our study revealed a positive correlation between elevated levels of the RC-to-TC ratio, the RC-to-LDL-C ratio, and frailty as defined by both FI (Fig. 2) and FP (Supplementary Table 5).
Fig. 2.
Forest Plot for Association of RC, RC-to-TC ratio, and RC-to-LDL-C ratio with the Frailty. The value of LDL-C was calculated using the Martin-Hopkins equation. Model 1 adjusted for age (continuous), gender (female and male), ethnicity (white, black, or other), education level (below high school, or high school and above), family income (poor, near poor, or non-poor), and marital status (non-married or married). Model 2 adjusted for the variables in model 1 plus smoking status (never, former, and current) and HEI-2015 (quartile). Model 3 adjusted for the variables in model 2 plus BMI (continuous), SBP (continuous), DBP (continuous), eGFR level (≥ 90, 60 to 89, and < 60 ml/min per 1.73 m2), CVD (no or yes), DM (no or yes), statins use (no or yes), anti-Diabetic drug use (no or yes), and anti-Hypertensive drug use (no or yes). Model 4 adjusted for the variables in model 3 plus TC (continuous) and LDL-C (continuous). OR, odds ratio; CI, confidence interval; RC, remnant cholesterol; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol
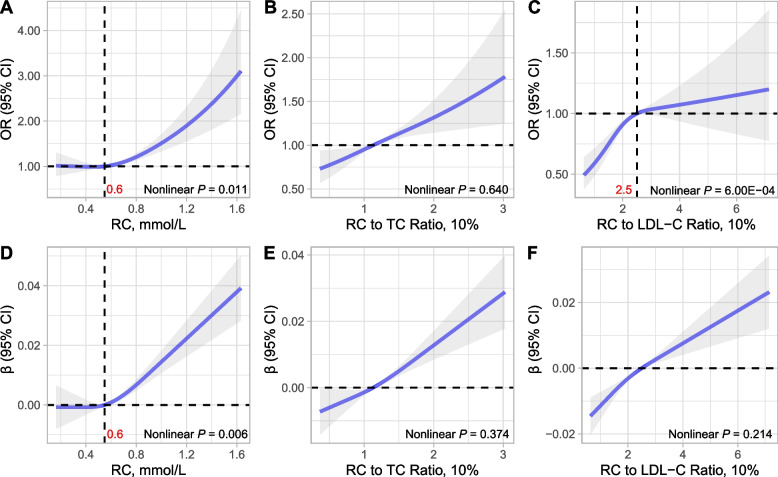
Figure 3 depicts the use of restricted cubic splines to illustrate the dose–response association between serum RC levels and the likelihood of frailty. The findings indicate that the dose–response relationship of serum RC levels (non-linear P = 0.011) and the RC-to-LDL-C ratio (non-linear P = 6.00E-04) with frailty displayed non-linearity. Conversely, the relationship between the RC-to-TC ratio and the likelihood of frailty was linear (non-linear P = 0.620). Two-segment piecewise regression models with inflection point of the curve were fitted to quantify the effect of RC above and below the inflection point. Importantly, the likelihood of frailty remained relatively constant until approximately 0.55 mmol/L of RC (OR = 1.47 per 1 mmol/L increase in RC levels, 95% CI = 0.40 to 5.43, P = 0.564) before observing a swift increase (OR = 2.83 per 1 mmol/L increase in RC levels, 95% CI = 1.54 to 5.20, P = 0.001; Supplementary Table 6). Conversely, the likelihood of frailty amplified until around 0.25 (OR = 1.38 per 1 mmol/L increase in RC levels, 95% CI = 1.17 to 1.63, P = 2.91E-04), after which the increase plateaued (OR = 1.06 per 1 mmol/L increase in RC levels, 95% CI = 0.90 to 1.25, P = 0.468), as displayed in Supplementary Table 6.
Fig. 3.
Restricted Cubic Spline Curves for Association of RC with the Frailty. (A) Association of RC with the likelihood of frailty, (B) Association of RC to TC ratio with the likelihood of frailty, (C) Association of RC to LDL-C ratio with the likelihood of frailty. (D) Association of RC with the FI, (E) Association of RC to TC ratio with the FI, (F) Association of RC to LDL-C ratio with the FI. The models adjusted for age (continuous), gender (female and male), ethnicity (white, black, or other), ethnicity (white, black, or other), education level (below high school, or high school and above), marital status (non-married or married), smoking status (never, former, and current), HEI-2015 (quartile), BMI (continuous), SBP (continuous), DBP (continuous), eGFR level (≥ 90, 60 to 89, and < 60 ml/min per 1.73 m2), CVD (no or yes), DM (no or yes), statins use (no or yes), anti-Diabetic drug use (no or yes), and anti-Hypertensive drug use (no or yes). For RC, the model additionally adjusted for TC (continuous) and LDL-C (continuous). OR, odds ratio; CI, confidence interval; RC, remnant cholesterol; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol
Subgroups and sensitivity analyses
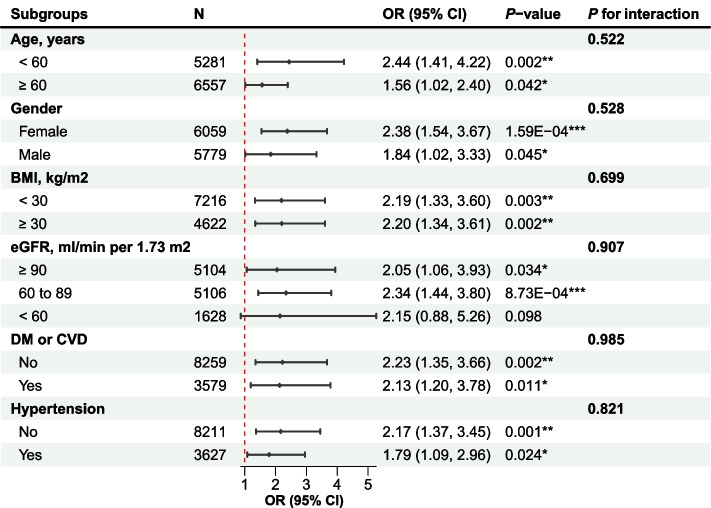
The directionality of effect estimates across all evaluated subgroups aligned with the overall outcomes (Fig. 4 and Supplementary Fig. 2). Of significance was the association between serum levels of RC and the likelihood of frailty, which demonstrated statistical significance irrespective of age subgroup: OR of 2.44 (95% CI = 1.41 to 4.22, P = 0.002) for middle-aged adults (< 60 years), and 1.56 (95% CI = 1.02 to 2.40, P = 0.042) for older adults (≥ 60 years). Corresponding trends were observed for the RC-to-TC ratio and RC-to-LDL-C ratio (Supplementary Fig. 2). No significant interactions were detected (Fig. 4 and Supplementary Fig. 2).
Fig. 4.
Forest Plot for Subgroup Analyses of the Association Between RC and Frailty. Adjusted for age (continuous), gender (female and male), ethnicity (white, black, or other), education level (below high school, or high school and above), marital status (non-married or married), smoking status (never, former, and current), HEI-2015 (quartile), BMI (continuous), SBP (continuous), DBP (continuous), eGFR level (≥ 90, 60 to 89, and < 60 ml/min per 1.73 m2), CVD (no or yes), DM (no or yes), statins use (no or yes), anti-Diabetic drug use, anti-Hypertensive drug use, TC (continuous), and LDL-C (continuous), except the subgroup variable. P-value for interaction was corrected for false discovery rate (FDR)-based multiple hypothesis testing. *, < 0.05; **, < 0.01; ***, < 0.001
Three distinct sensitivity analyses were conducted to verify the robustness of the principal findings. First, the association of RC levels with frailty, as determined by the modified FI, was verified (Supplementary Table 7). Second, missing data were addressed via two methods, direct deletion and multiple imputation, confirming that the associations of RC, RC-to-TC ratio, and RC-to-LDL-C ratio with the likelihood of frailty remained consistent irrespective of the method applied (Supplementary Table 8 and Supplementary Table 9). Lastly, the congruence between the results drawn from Friedewald and Sampson equations with the primary findings was established (Supplementary Table 10 and Supplementary Fig. 3).
Mendelian randomization analysis for causal association of RC with frailty
A total of 51 RC-related, 16 FI-related, and 36 FP-related SNPs, all with F-statistics exceeding 10, were employed as genetic instrumental variables (Supplementary Tables 11–13). The multiplicative random-effects IVW analysis illuminated a positive correlation between the genetically inferred heightened level of RC and an increase in FI (β = 0.059 per 1 mmol/L increase in RC levels, 95% CI = 0.033 to 0.085, P = 1.05E-05; Table 2). However, no causal associations between RC and FP were found (Supplementary Table 14).
Table 2.
Bidirectional MR analyses for the association between RC and FI
| Methods | β (95% CI) | P-value |
|---|---|---|
| Effect of RC on FI | ||
| IVW | 0.059 (0.033, 0.085) | 1.05E-05*** |
| MR-Egger | 0.058 (0.015, 0.100) | 0.011* |
| Weighted median | 0.063 (0.032, 0.093) | 5.18E-05*** |
| Simple median | 0.083 (0.050, 0.117) | 1.61E-06*** |
| MR-PRESSO | 0.059 (0.033, 0.085) | 5.67E-05*** |
| MRlap | 0.061 (0.036, 0.086) | 9.81E-07*** |
| Effect of FI on RC | ||
| IVW | -0.140 (-0.293, 0.014) | 0.075 |
| MR-Egger | -0.989 (-1.477, -0.502) | 0.001** |
| Weighted median | -0.137 (-0.300, 0.025) | 0.113 |
| Simple median | -0.079 (-0.235, 0.077) | 0.358 |
| MR-PRESSO | -0.140 (-0.293, 0.014) | 0.095 |
| MRlap | 0.030 (-0.170, 0.230) | 0.772 |
Notes: The effect size (β) is per 1 mmol/L increase in RC. IVW Inverse-variance-weighted, MR-PRESSO Mendelian Randomization-Pleiotropy RESidual Sum and Outlier, CI Confidence interval, RC Remnant cholesterol, FI Frailty index. *, < 0.05; **, < 0.01; ***, < 0.001
The multivariable MR analysis substantiated a direct effect of RC on FI. Following adjustment for TC and LDL-C via multivariable MR, the results maintained alignment with the principal findings (β = 0.086 per 1 mmol/L increase in RC levels, 95% CI = 0.012 to 0.161, P = 0.024; Table 3). The associations of RC with FI remained stable, irrespective of adjustment for CHD, HF, stroke, T2DM, BMI, SBP, or DBP (Table 3).
Table 3.
Multivariable MR analyses for the Causal Effect of RC on FI
| Adjustment | β (95% CI) | P-value |
|---|---|---|
| TC and LDL-C | 0.086 (0.012, 0.161) | 0.024* |
| CHD | 0.032 (0.006, 0.058) | 0.001** |
| HF | 0.043 (0.018, 0.067) | 5.67E-04*** |
| Stroke | 0.051 (0.025, 0.076) | 9.05E-05*** |
| T2DM | 0.068 (0.027, 0.108) | 0.001** |
| BMI | 0.069 (0.031, 0.107) | 2.11E-04*** |
| SBP | 0.047 (0.021, 0.073) | 4.30E-04 |
| DBP | 0.041 (0.015, 0.067) | 0.002** |
Notes: The effect size (β) is per 1 mmol/L increase in RC. LDL-C Low-density lipoprotein cholesterol, TC Total cholesterol, T2DM Type 2 diabetes mellitus, HF Heart failure, BMI Body mass index. *, < 0.05; **, < 0.01; ***, < 0.001
Furthermore, the accuracy of the inferred causal direction was verified using the MR-Steiger test for directionality. In addition, no significant causal effect of FI on RC was noted (Table 2). The MRlap analysis comparing observed and corrected effects affirmed consistency (Table 2).
High statistical heterogeneity was observed among individual SNP estimates in the analysis of FI (IVW, Cochran’s Q Statistic = 95.04, I2 = 47.39%, P = 1.27E-04; MR-Egger, Cochran’s Q Statistic = 95.03, I2 = 48.44%, P = 8.92E-05) and FP (IVW, Cochran’s Q Statistic = 88.18, I2 = 60.31%, P = 1.76E-06; MR-Egger, Cochran’s Q Statistic = 87.78, I2 = 61.27%, P = 1.22E-06). Funnel asymmetry was suggested by the visual inspection of the funnel plot (Supplementary Fig. 4). Upon removal of heterogeneity-associated SNPs (rs653178, rs9682783, rs102275, and rs6601299), heterogeneity was eliminated (IVW, Cochran’s Q Statistic = 61.26, I2 = 24.91%, P = 0.065; MR-Egger, Cochran’s Q Statistic = 0.054, I2 = 26.53%, P = 0.054), while the causal association maintained significance (Supplementary Table 15).
MR-Egger intercept test provided no evidence for directional pleiotropy in assessing the causal association of RC with FI (Egger intercept = 7.55 × 10–5, P = 0.954). Utilizing the PhenoScanner tool, three SNPs (rs12916, rs4876611, and rs653178) that had associations with potential confounders (BMI, SBP, and/or DBP) were identified in the publicly available summary-level GWAS data. An additional sensitivity analysis was conducted, excluding these SNPs and the four previously mentioned SNPs, which yielded similar results of all MR methods (Supplementary Table 16) and no significant heterogeneity was detected (IVW, Cochran’s Q Statistic = 58.05, I2 = 24.21%, P = 0.076; MR-Egger, Cochran’s Q Statistic = 57.89, I2 = 25.73%, P = 0.064; Supplementary Table 16).
Discussion
This study determined that higher establishes a correlation between elevated RC levels and an increased susceptibility to frailty among middle-aged and older adults. Both observational and MR studies corroborate this, with sensitivity analysis further strengthening the validity of the findings. Additionally, a threshold effect was observed in the relationship between RC and frailty.
The Rookwood frailty index and the Fried frailty phenotype are the two most commonly employed instruments for identifying frailty. The results of the observational analysis indicated a consistent trend in the effects of both the FI and the FP. However, the MR analysis revealed no significant association between RC and FP. These findings align with those reported in a recent study [39]. While the converging evidence for risk factors between the two measurements is regarded as indicative of validity, the two measurements should be deemed complementary but not equivalent [40, 41]. The FP primarily focuses on physical functioning, whereas the FI encompasses accumulation of health deficits, such as coronary heart disease, angina, heart attack, stroke, and T2DM. Furthermore, the sensitivity analysis of modified FI, excluding items related to cardiometabolic disease, suggested high levels of serum RC might contribute to a high burden of multimorbidity in middle-aged and older adults.
Despite a lack of direct epidemiological evidence linking serum circulating RC levels to frailty, recent MR studies have spotlighted the influential role of elevated LDL-C levels in inducing frailty [9]. Substantial increases in RC levels have been documented in adults consuming high-fat diets [42]. The same diets administered to mice resulted in a heightened frailty level [43], while simultaneously diminishing the anti-frailty benefits of intermittent fasting [44]. Consequently, this indirect evidence suggests a connection between higher RC levels and a heightened frailty risk, which this study substantiates.
Although increased serum RC levels are regarded as a potent independent risk factor for CVD [45, 46], this analysis reveals that the association between serum RC levels and frailty persists, even after adjusting for CVD and T2DM. This suggests that the contribution of RC to frailty risk is not exclusively attributed to a higher susceptibility to CVD. Furthermore, the results from our epidemiological studies and multivariable MR confirm that this association remains significant, regardless of total cholesterol or LDL-C levels.
Individuals exhibiting high RC levels, and therefore a greater frailty risk, should be promptly identified and intervened, especially those with underlying cardiometabolic conditions such as coronary heart disease and diabetes. The findings suggest that RC is a risk factor for frailty, which should urge clinicians and researchers to prioritize attention toward such individuals. This becomes particularly vital as statin therapy, commonly used to lower LDL-C and prevent cardiovascular incidents, has minimal effect on reducing RC. As such, focusing on managing elevated RC levels is critical to counteract its potential role in accelerating aging and frailty.
Strengths and limitations
This study offers multiple points of strength. This study is the first to investigate the correlation between RC and frailty among non-institutionalized middle-aged and older adults. While the cross-sectional design of the observational data inherently restricts causal interpretation, efforts have been undertaken to strengthen causal inferences through the robustness of MR analysis. Furthermore, this study has found an association of the proportion of RC to TC or LDL-C with frailty, underscoring a saturation effect.
Conversely, this research also exhibits certain limitations that warrant acknowledgment. The LDL-C levels reported in the observational study were not direct measurements but rather, estimated values, thereby introducing potential measurement bias. However, this risk has been mitigated by employing three different equations to predict LDL-C levels and subsequently comparing the results. Additionally, the study’s reliance on NHANES data that predominantly features individuals of white ancestry could potentially restrict the broader applicability of the findings to diverse populations. Another limitation pertains to the non-linear MR design, which was constrained by the unavailability of individual-level GWAS data that is publicly accessible. Lastly, the FI utilized in this research was dependent on self-reported data, a factor that could lead to potential reporting bias.
Conclusion
To summarize, this research, through a combined observational and MR study, provides compelling evidence that an elevated RC level amplifies the risk of frailty in middle-aged and older adults. Interventions aimed at decreasing RC levels and the proportion of RC to TC or LDL-C could potentially confer benefits in the prevention and management of frailty. This underscores the importance of developing innovative therapies aiming at reducing the risk of frailty.
Supplementary Information
Additional file 1: Table S1. The 49-Item Defects to Calculate Frailty Index. Table S2. Phenotype descriptions and distributions. Table S3. Generalized Variance Inflation Factor. Table S4. Population Characteristics After Propensity Score Matching (N = 5236). Table S5. Association of RC, RC-to-TC Ratio, and RC-to-LDL-C Ratio with the Fried Frailty Phenotype. Table S6. The results of the two-piecewise logistic regression model. Table S7. Association of RC, RC-to-TC Ratio, and RC-to-LDL-C Ratio with the Frailty as Defined by Modified Frailty Index. Table S8. Association of RC with frailty based on multiple imputation. Table S9. Association of RC with the risk of frailty based on direct deletion. Table 10. Association of RC with the FI (Continuous). Table S11. Instrumental Variables for RC. Table S12. Instrumental Variables for Frailty Index. Table S13. Instrumental Variables for Fried Frailty Phenotype. Table S14. Bidirectional MR Analyses for the Association between RC and Fried Frailty Phenotype. Table S15. MR Results for Effect of RC on FI Removing four SNPs. Table 16. MR Results for Effect of RC on FI Removing six SNPs. Fig. S1. Correlation of LDL-C Calculated by Different Equations. Fig. S2. Forest Plot for Subgroup Analyses. Fig. S3. Forest Plot for Association of RC, RC-to-TC ratio, and RC-to-LDL-C ratio with Frailty. Fig. S4. Funnel plot. (A) Raw; (B) Removing rs653178, rs9682783, rs102275, and rs6601299; (C) Removing rs12916, rs4876611, rs653178, rs9682783, rs102275, and rs6601299.
Acknowledgements
Not applicable.
Authors’ contributions
YLH conducted analyses and wrote the article. XJW, LL, JMH, LZ, and YL collected and assembled the data. YLH and YLL conceived the study design. All authors have contributed to the interpretation of the results and have critically revised the content of the manuscript. All authors agree to be accountable for all aspects of the work.
Funding
This work was supported by the National Natural Science Foundation of China (Grant no. 81974566) and the Jinan "University 20" Project (Grant no. 2020GXRC017).
Availability of data and materials
This data can be found at: Publicly available datasets were analyzed in this study. The summary-level GWAS data of frailty index was downloaded from the NHGRI-EBI Catalog of human genome-wide association studies (GWAS Catalog, https://www.ebi.ac.uk/gwas/home), including remnant cholesterol (ID: GCST90092943), total cholesterol (ID: GCST90092985), low-density lipoprotein cholesterol (ID: GCST90092883), frailty index (ID: GCST90020053), body mass index (ID: GCST006900), CHD (ID: GCST003116), T2DM (ID: GCST006867), HF (ID: GCST009541), stroke (ID: GCST005838), SBP (ID: GCST006624), and DBP (ID: GCST006630). The NHANES data was downloaded from the National Center for Health Statistics website (https://www.cdc.gov/nchs/nhanes/index.htm).
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Hoogendijk EO, Afilalo J, Ensrud KE, Kowal P, Onder G, Fried LP. Frailty: implications for clinical practice and public health. Lancet. 2019;394:1365–1375. doi: 10.1016/S0140-6736(19)31786-6. [DOI] [PubMed] [Google Scholar]
- 2.Fried LP, Cohen AA, Xue Q-L, Walston J, Bandeen-Roche K, Varadhan R. The physical frailty syndrome as a transition from homeostatic symphony to cacophony. Nat Aging. 2021;1:36–46. doi: 10.1038/s43587-020-00017-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–156. doi: 10.1093/gerona/56.3.M146. [DOI] [PubMed] [Google Scholar]
- 4.Veronese N, Custodero C, Cella A, Demurtas J, Zora S, Maggi S, et al. Prevalence of multidimensional frailty and pre-frailty in older people in different settings: A systematic review and meta-analysis. Ageing Res Rev. 2021;72:101498. doi: 10.1016/j.arr.2021.101498. [DOI] [PubMed] [Google Scholar]
- 5.Damluji AA, Chung S-E, Xue Q-L, Hasan RK, Moscucci M, Forman DE, et al. Frailty and cardiovascular outcomes in the national health and aging trends study. Eur Heart J. 2021;42:3856–3865. doi: 10.1093/eurheartj/ehab468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Veronese N, Cereda E, Stubbs B, Solmi M, Luchini C, Manzato E, et al. Risk of cardiovascular disease morbidity and mortality in frail and pre-frail older adults: results from a meta-analysis and exploratory meta-regression analysis. Ageing Res Rev. 2017;35:63–73. doi: 10.1016/j.arr.2017.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zhu J, Zhou D, Wang J, Yang Y, Chen D, He F, et al. Frailty and cardiometabolic diseases: a bidirectional Mendelian randomisation study. Age Ageing. 2022;51:1–6. [DOI] [PubMed]
- 8.Piotrowicz K, Gąsowski J. Risk factors for frailty and cardiovascular diseases: are they the same? Adv Exp Med Biol. 2020;1216:39–50. doi: 10.1007/978-3-030-33330-0_5. [DOI] [PubMed] [Google Scholar]
- 9.Wang Q, Wang Y, Lehto K, Pedersen NL, Williams DM, Hägg S. Genetically-predicted life-long lowering of low-density lipoprotein cholesterol is associated with decreased frailty: a Mendelian randomization study in UK biobank. EBioMedicine. 2019;45:487–494. doi: 10.1016/j.ebiom.2019.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Castañer O, Pintó X, Subirana I, Amor AJ, Ros E, Hernáez Á, et al. Remnant cholesterol, not ldl cholesterol, is associated with incident cardiovascular disease. J Am Coll Cardiol. 2020;76:2712–2724. doi: 10.1016/j.jacc.2020.10.008. [DOI] [PubMed] [Google Scholar]
- 11.Langsted A, Madsen CM, Nordestgaard BG. Contribution of remnant cholesterol to cardiovascular risk. J Intern Med. 2020;288:116–127. doi: 10.1111/joim.13059. [DOI] [PubMed] [Google Scholar]
- 12.Wadström BN, Wulff AB, Pedersen KM, Jensen GB, Nordestgaard BG. Elevated remnant cholesterol increases the risk of peripheral artery disease, myocardial infarction, and ischaemic stroke: a cohort-based study. Eur Heart J. 2022;43:3258–3269. doi: 10.1093/eurheartj/ehab705. [DOI] [PubMed] [Google Scholar]
- 13.Varbo A, Benn M, Nordestgaard BG. Remnant cholesterol as a cause of ischemic heart disease: Evidence, definition, measurement, atherogenicity, high risk patients, and present and future treatment. Pharmacol Ther. 2014;141:358–367. doi: 10.1016/j.pharmthera.2013.11.008. [DOI] [PubMed] [Google Scholar]
- 14.Xiang Q, Tian F, Xu J, Du X, Zhang S, Liu L. New insight into dyslipidemia-induced cellular senescence in atherosclerosis. Biol Rev Camb Philos Soc. 2022;97:1844–1867. doi: 10.1111/brv.12866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xiang Q-Y, Tian F, Du X, Xu J, Zhu L-Y, Guo L-L, et al. Postprandial triglyceride-rich lipoproteins-induced premature senescence of adipose-derived mesenchymal stem cells via the SIRT1/p53/Ac-p53/p21 axis through oxidative mechanism. Aging (Albany NY) 2020;12:26080–26094. doi: 10.18632/aging.202298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Liu P, Li Y, Ma L. Frailty in rodents: models, underlying mechanisms, and management. Ageing Res Rev. 2022;79:101659. doi: 10.1016/j.arr.2022.101659. [DOI] [PubMed] [Google Scholar]
- 17.Ference BA, Holmes MV, Smith GD. Using Mendelian randomization to improve the design of randomized trials. Cold Spring Harb Perspect Med. 2021;11:a040980. doi: 10.1101/cshperspect.a040980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.NHANES - About the National Health and Nutrition Examination Survey. https://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Accessed 30 Dec 2022.
- 19.National Center for Health Statistics. NHANES - NCHS Research Ethics Review Board Approval. https://www.cdc.gov/nchs/nhanes/irba98.htm. Accessed 7 May 2022.
- 20.Martin SS, Blaha MJ, Elshazly MB, Toth PP, Kwiterovich PO, Blumenthal RS, et al. Comparison of a novel method vs the Friedewald equation for estimating low-density lipoprotein cholesterol levels from the standard lipid profile. JAMA. 2013;310:2061–2068. doi: 10.1001/jama.2013.280532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sajja A, Li H-F, Spinelli KJ, Blumenthal RS, Virani SS, Martin SS, et al. Discordance between standard equations for determination of LDL cholesterol in patients with atherosclerosis. J Am Coll Cardiol. 2022;79:530–541. doi: 10.1016/j.jacc.2021.11.042. [DOI] [PubMed] [Google Scholar]
- 22.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. doi: 10.1093/clinchem/18.6.499. [DOI] [PubMed] [Google Scholar]
- 23.Sampson M, Ling C, Sun Q, Harb R, Ashmaig M, Warnick R, et al. A new equation for calculation of low-density lipoprotein cholesterol in patients with normolipidemia and/or hypertriglyceridemia. JAMA Cardiol. 2020;5:540–548. doi: 10.1001/jamacardio.2020.0013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Searle SD, Mitnitski A, Gahbauer EA, Gill TM, Rockwood K. A standard procedure for creating a frailty index. BMC Geriatr. 2008;8:24. doi: 10.1186/1471-2318-8-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Blodgett J, Theou O, Kirkland S, Andreou P, Rockwood K. Frailty in NHANES: comparing the frailty index and phenotype. Arch Gerontol Geriatr. 2015;60:464–470. doi: 10.1016/j.archger.2015.01.016. [DOI] [PubMed] [Google Scholar]
- 26.Clegg A, Bates C, Young J, Ryan R, Nichols L, Ann Teale E, et al. Development and validation of an electronic frailty index using routine primary care electronic health record data. Age Ageing. 2016;45:353–360. doi: 10.1093/ageing/afw039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fu Z, Zhou T, Dong F, Li M, Lin X, Ma W, et al. Secondhand smoke is positively associated with pre-frailty and frailty in non-smoking older adults. Front Psychiatry. 2022;13:1095254. doi: 10.3389/fpsyt.2022.1095254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Levey AS, Stevens LA, Schmid CH, Zhang Y, Castro AF, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150:604–12. doi: 10.7326/0003-4819-150-9-200905050-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Richardson TG, Leyden GM, Wang Q, Bell JA, Elsworth B, Davey Smith G, et al. Characterising metabolomic signatures of lipid-modifying therapies through drug target mendelian randomisation. PLoS Biol. 2022;20:e3001547. doi: 10.1371/journal.pbio.3001547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Atkins JL, Jylhävä J, Pedersen NL, Magnusson PK, Lu Y, Wang Y, et al. A genome-wide association study of the frailty index highlights brain pathways in ageing. Aging Cell. 2021;20:e13459. doi: 10.1111/acel.13459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ye Y, Noche RB, Szejko N, Both CP, Acosta JN, Leasure AC, et al. A genome-wide association study of frailty identifies significant genetic correlation with neuropsychiatric, cardiovascular, and inflammation pathways. GeroScience. 2023. 10.1007/s11357-023-00771-z. [DOI] [PMC free article] [PubMed]
- 32.Burgess S, Thompson SG, CRP CHD Genetics Collaboration. Avoiding bias from weak instruments in Mendelian randomization studies. Int J Epidemiol. 2011;40:755–64. [DOI] [PubMed]
- 33.Pierce BL, Ahsan H, Vanderweele TJ. Power and instrument strength requirements for Mendelian randomization studies using multiple genetic variants. Int J Epidemiol. 2011;40:740–752. doi: 10.1093/ije/dyq151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hemani G, Tilling K, Smith GD. Orienting the causal relationship between imprecisely measured traits using GWAS summary data. PLoS Genet. 2017;13:e1007081. doi: 10.1371/journal.pgen.1007081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hemani G, Zheng J, Elsworth B, Wade KH, Haberland V, Baird D, et al. The MR-Base platform supports systematic causal inference across the human phenome. Loos R, editor. eLife. 2018;7:e34408. doi: 10.7554/eLife.34408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Verbanck M, Chen C-Y, Neale B, Do R. Detection of widespread horizontal pleiotropy in causal relationships inferred from Mendelian randomization between complex traits and diseases. Nat Genet. 2018;50:693–698. doi: 10.1038/s41588-018-0099-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kamat MA, Blackshaw JA, Young R, Surendran P, Burgess S, Danesh J, et al. PhenoScanner V2: an expanded tool for searching human genotype–phenotype associations. Bioinformatics. 2019;35:4851–4853. doi: 10.1093/bioinformatics/btz469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mounier N, Kutalik Z. Bias correction for inverse variance weighting Mendelian randomization. Genet Epidemiol. 2023;47:314–331. doi: 10.1002/gepi.22522. [DOI] [PubMed] [Google Scholar]
- 39.Mak JKL, Kananen L, Qin C, Kuja-Halkola R, Tang B, Lin J, et al. Unraveling the metabolic underpinnings of frailty using multicohort observational and Mendelian randomization analyses. Aging Cell. 2023. 10.1111/acel.13868. [DOI] [PMC free article] [PubMed]
- 40.Rockwood K, Andrew M, Mitnitski A. A comparison of two approaches to measuring frailty in elderly people. J Gerontol A Biol Sci Med Sci. 2007;62:738–743. doi: 10.1093/gerona/62.7.738. [DOI] [PubMed] [Google Scholar]
- 41.Cesari M, Gambassi G, Abellan van Kan G, Vellas B. The frailty phenotype and the frailty index: different instruments for different purposes. Age Ageing. 2014;43:10–12. [DOI] [PubMed]
- 42.Xu J, Chen Y-Q, Zhao S-P, Liu L. Determination of optimal cut-off points after a high-fat meal corresponding to fasting elevations of triglyceride and remnant cholesterol in Chinese subjects. Lipids Health Dis. 2019;18:206. doi: 10.1186/s12944-019-1146-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Antoch MP, Wrobel M, Kuropatwinski KK, Gitlin I, Leonova KI, Toshkov I, et al. Physiological frailty index (PFI): quantitative in-life estimate of individual biological age in mice. Aging (Albany NY) 2017;9:615–626. doi: 10.18632/aging.101206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Henderson YO, Bithi N, Yang J, Link C, Zhang A, Baron B, et al. A long-term obesogenic high-fat diet in mice partially dampens the anti-frailty benefits of late-life intermittent fasting. Geroscience. 2022;45:1247–1262. doi: 10.1007/s11357-022-00678-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Lee SJ, Kim S-E, Go T-H, Kang DR, Jeon H-S, Kim Y-I, et al. Remnant cholesterol, LDL cholesterol and incident cardiovascular disease among Koreans: a national population-based study. Eur J Prev Cardiol. 2023. 10.1093/eurjpc/zwad036. [DOI] [PubMed]
- 46.Huh JH, Han K, Cho YK, Roh E, Kang JG, Lee SJ, et al. Remnant cholesterol and the risk of cardiovascular disease in type 2 diabetes: a nationwide longitudinal cohort study. Cardiovasc Diabetol. 2022;21:228. doi: 10.1186/s12933-022-01667-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. The 49-Item Defects to Calculate Frailty Index. Table S2. Phenotype descriptions and distributions. Table S3. Generalized Variance Inflation Factor. Table S4. Population Characteristics After Propensity Score Matching (N = 5236). Table S5. Association of RC, RC-to-TC Ratio, and RC-to-LDL-C Ratio with the Fried Frailty Phenotype. Table S6. The results of the two-piecewise logistic regression model. Table S7. Association of RC, RC-to-TC Ratio, and RC-to-LDL-C Ratio with the Frailty as Defined by Modified Frailty Index. Table S8. Association of RC with frailty based on multiple imputation. Table S9. Association of RC with the risk of frailty based on direct deletion. Table 10. Association of RC with the FI (Continuous). Table S11. Instrumental Variables for RC. Table S12. Instrumental Variables for Frailty Index. Table S13. Instrumental Variables for Fried Frailty Phenotype. Table S14. Bidirectional MR Analyses for the Association between RC and Fried Frailty Phenotype. Table S15. MR Results for Effect of RC on FI Removing four SNPs. Table 16. MR Results for Effect of RC on FI Removing six SNPs. Fig. S1. Correlation of LDL-C Calculated by Different Equations. Fig. S2. Forest Plot for Subgroup Analyses. Fig. S3. Forest Plot for Association of RC, RC-to-TC ratio, and RC-to-LDL-C ratio with Frailty. Fig. S4. Funnel plot. (A) Raw; (B) Removing rs653178, rs9682783, rs102275, and rs6601299; (C) Removing rs12916, rs4876611, rs653178, rs9682783, rs102275, and rs6601299.
Data Availability Statement
This data can be found at: Publicly available datasets were analyzed in this study. The summary-level GWAS data of frailty index was downloaded from the NHGRI-EBI Catalog of human genome-wide association studies (GWAS Catalog, https://www.ebi.ac.uk/gwas/home), including remnant cholesterol (ID: GCST90092943), total cholesterol (ID: GCST90092985), low-density lipoprotein cholesterol (ID: GCST90092883), frailty index (ID: GCST90020053), body mass index (ID: GCST006900), CHD (ID: GCST003116), T2DM (ID: GCST006867), HF (ID: GCST009541), stroke (ID: GCST005838), SBP (ID: GCST006624), and DBP (ID: GCST006630). The NHANES data was downloaded from the National Center for Health Statistics website (https://www.cdc.gov/nchs/nhanes/index.htm).