Abstract
Nurses’ contributions to stroke rehabilitation have been viewed as pivotal, but therapeutically nonspecific. This integrative review synthesized empirical literature on the roles and contributions of nurses to inpatient stroke rehabilitation to answer three research questions: (a) What specific skills or tasks have been identified as the roles and contributions of nurses to inpatient stroke rehabilitation? (b) How do nurses perform these skills/tasks to support and promote inpatient stroke rehabilitation and recovery? and (c) What factors have been identified to impact nurses’ working conditions on inpatient stroke rehabilitation units? A systematic search of multiple electronic databases retrieved seven studies which provided significant context and examples to these questions. What nurses do in practice included, for example, maximizing patients’ independence in performing daily activities, preventing harm, and preserving integrity. How nurses perform their therapeutic roles included teaching, coaching, coordination, management, advocacy, collaboration. Factors that impact nurses’ working conditions consisted of time, resources, and knowledge. This review demonstrates our current understanding of nurses’ contributions to inpatient stroke rehabilitation, highlights their significant role, identifies current barriers/challenges of implementing stroke nursing care, and suggests ways of documenting and measuring nurses’ contributions.
Keywords: Stroke rehabilitation, Nursing, Role, Competency, Identity
Stroke rehabilitation has been defined as a dynamic, goal-oriented process that aims to enable patients to achieve optimal physical, emotional, behavioral, and cognitive functioning. 1 In Ontario, direct rehabilitation costs, nursing worked hours, and nursing plus therapy worked hours have been used (as indicators) to measure the financial performance and function of stroke rehabilitation services. The indicator values for inpatient rehabilitation services are measures of the proportion of time that nurses and therapists spend providing direct nursing care, charting, performing patient education, and training healthcare professionals. 2 These human resource measures indicate that nurses are key contributors of the interprofessional rehabilitation teams and play a vital role in stroke patients’ rehabilitation. Given nurses’ extensive involvement in rehabilitation activities, their contributions to stroke rehabilitation may potentially promote physical, functional, and cognitive recovery of patients.3,4
In the research literature, stroke rehabilitation nurses’ roles have historically been considered pivotal, yet therapeutically nonspecific, 5 and rarely viewed in direct relation to rehabilitation patient outcomes. 6 Contemporary researchers disagree with this view and argue that nurses do contribute substantially to the recovery of patients after stroke. 7 In the context of interprofessional rehabilitation teams, no consensus has been demonstrated in the research literature about nurses’ specific roles in stroke rehabilitation units, how nurses perform their therapeutic roles or implement therapeutic techniques with patients, and the factors that influence nurses’ working conditions on stroke rehabilitation units. This may reflect the relative lack of focus on this area of practice within the scientific literature, with most research conducted decades ago.8,9,10,11,12
In summary, there is an obvious, longstanding gap in the literature in recognizing rehabilitation nurses as members of the interprofessional team with their clinical work often taken for granted, undervalued, and undocumented in the formal rehabilitation process.12,13,14 Thus, a formal understanding of nurses’ contributions to the stroke rehabilitation process is required. Role clarity may be beneficial in increasing awareness of the unique contributions of nurses to the interprofessional rehabilitation team; identifying barriers and challenges to integrating nursing care in stroke rehabilitation; promoting rehabilitation nursing as a specialized professional nursing entity; and advancing nursing curriculum and educating future nurses.
Purpose
An integrative review was conducted to synthesize findings from identified research literature on nurses’ roles and contributions in inpatient stroke rehabilitation units and to analyze the findings via three research questions: (a) What specific skills or tasks have been identified as the roles and contributions of nurses to inpatient stroke rehabilitation? (b) How do nurses perform these skills/tasks to support and promote inpatient stroke rehabilitation and recovery? and (c) What factors have been identified to impact the nurses’ working conditions on inpatient stroke rehabilitation units?
Methods
An integrative review of literature was chosen as the approach for this study to satisfy the study aim; a protocol was not registered or published. This approach was considered suitable for the heterogeneity of the research topic as it permits the inclusion of multiple research designs (i.e., quantitative, qualitative, non-experimental, and experimental). 15 A five-stage review methodology was used: (a) identifying the problem (i.e., introduction/objectives), (b) conducting a literature search, (c) evaluating the data, (d) analyzing the data, and (e) presenting the results. 15
Search Strategy
The literature search strategy was developed in consultation with a librarian at Western University. A search of multiple databases (i.e., MEDLINE, PsycINFO, CINAHL, EMBASE, SCOPUS, and Proquest Nursing and Allied Health) was conducted for articles that were published up to December 30, 2021. Guidelines from the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Extension for Scoping Reviews (PRISMA-ScR) 16 were used to report the review.
Search Terms/Keywords
Three primary constructs (i.e., stroke rehabilitation, geriatric rehabilitation, nursing) were searched using subject headings, keywords, and MeSH terms. As an example, Appendix A (see the online supplementary content) shows the full electronic search for MEDLINE. To identify missed citations, the reference lists of retrieved research and review articles on the topic were scanned, and leading experts in the field consulted. Two distinct groups of retrieved articles were evident: (a) rehabilitation studies for people who had sustained a stroke and were admitted to inpatient stroke rehabilitation and (b) older adults receiving inpatient care on geriatric rehabilitation units. To describe nursing care roles in stroke and geriatric rehabilitation units, which may have potentially different elements, two separate reviews were undertaken to address context-specific research questions. This review addresses the studies for people who had sustained a stroke and were admitted to inpatient stroke rehabilitation.
Inclusion and Exclusion Criteria
The following inclusion criteria were used: (a) the study setting was an inpatient stroke rehabilitation unit, where ‘inpatient’ was defined as care of patients admitted to a hospital, (b) the primary aim of the study was to explore nurses’ roles, contributions, or functions within the rehabilitation unit, (c) perspectives were sought from nurses directly, and (d) the article was available in English. All nurses working within stroke rehabilitation defined by any role, title, or designation (e.g., staff nurse, nurse manager, rehabilitation coordinator) were included. The following research documents were excluded from review: theoretical articles, continuous learning/education modules, editorials, blog posts, protocols, program descriptions or reviews, non-systematic reviews, published abstracts, textbook chapters, conference proceedings, and clinical practice guidelines.
Assessment of Methodological Quality
Each article included for review was critically appraised for methodological rigor in nine domains, as described by Hawker and colleagues. 17 Each of the nine domains include items which are rated on a four-point ordinal scale: (a) very poor, (b) poor, (c) fair, and (d) good. Total scores range from 9 to 36 with scores 28–36 considered good quality articles, 20–27 as fair, 10–19 as poor, and <10 as very poor. 17 To establish inter-rater reliability, two authors (ET, AMc) completed the appraisals separately. In the case of a discrepancy in ratings, the two authors discussed each item until consensus was achieved.
Data Extraction and Synthesis
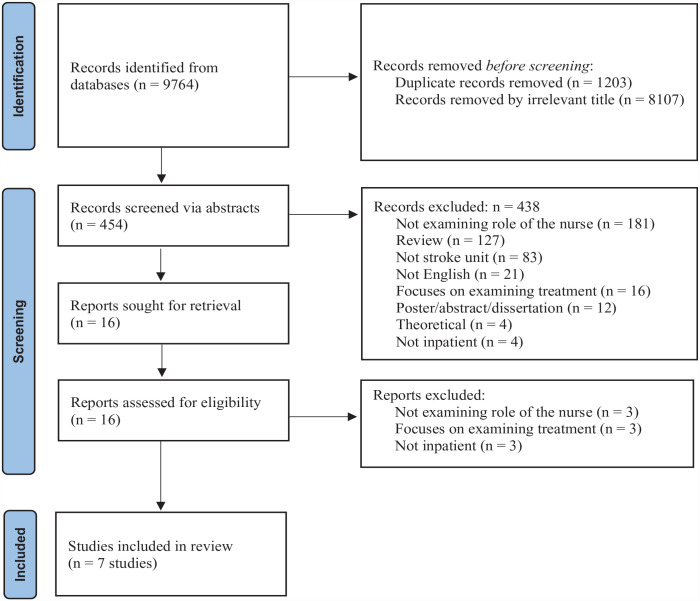
Articles retrieved from each database were first exported to Covidence software (www.covidence.org) where duplicate articles were removed. Two authors (NG, AN) screened a total of 9,764 titles followed by 454 abstracts for relevance to the review topic. Subsequently, 16 full-text articles were reviewed; disagreements were resolved through discussion. In total, seven studies met inclusion criteria (Figure 1).
Figure 1.
PRISMA flow diagram for the systematic literature search.
Two reviewers (ET, AMc) used a data extraction form to independently extract data from each of the studies included for review in the manner and language in which they were reported by the original authors (i.e., verbatim). Extracted data included author(s), country of first author’s origin, year of publication, study aim/objective, study design, method of data collection, sample size and characteristics, and reported themes/findings. In the case of missing data, individual authors were contacted and data were requested. Data were transferred from the extraction form and summarized in tabular form to prepare for data synthesis.
Whittemore and Knafl 15 describe the importance of identifying themes in the data extraction and synthesis process. Each individual study finding was reviewed line by line. Initially, brief codes were generated and applied to each finding to describe succinctly the nature of the finding. After all findings were coded, they were iteratively reviewed, compared, and contrasted for similarity of concepts. Codes were gradually grouped together and placed within three deductively determined themes. The first theme (What Nurses Do) addressed research question 1: What specific skills or tasks have been identified as the roles and contributions of nurses to inpatient stroke rehabilitation? The “what” of nursing care in rehabilitation units was defined as the episodic daily activities (related to direct patient care) that nurses perform in rehabilitation units, including administration of therapeutic interventions, management of complex health situations that change rapidly, and monitoring of therapeutic interventions. 11
The second theme (How Nurses Perform) addressed research question 2: How do nurses perform these skills/tasks to support and promote inpatient stroke rehabilitation and recovery? The “how” of nursing care in rehabilitation units was defined as nurses’ continuous actions which are woven into direct care activities described in the “what” of nursing care in rehabilitation units. 11 Continuous actions can include observation, assessment, interpretation, monitoring and ensuring quality of care, teaching and coaching, rehabilitation approach, management, advocacy, and coordination of care. 11 The third theme (Factors that Impact Nurses) addressed research question 3: What factors have been identified to impact the nurses’ working conditions on inpatient stroke rehabilitation units? Specific examples were retained from each study and used to describe the essence of the three themes.
Results
Search Results
Of the seven included studies, six were qualitative studies18,19,6,20,21,22 and one was a mixed methods study. 4 Three studies were from Denmark,18,20,22 three were from the United Kingdom,6,4,21 and one was from Canada. 19 Publication years for the studies ranged between 1999 and 2018, and sample sizes ranged from 8 to 63 (total = 145). Methodological quality was deemed to be good for all studies except for the Hill and Johnson study, 21 where quality was considered fair due to the limited description of ethics, background information, and sampling criteria.
Three themes with accompanying sub-themes were generated from the data. Table 1 demonstrates study findings that relate to Theme 1: What nurses do: skills or tasks identified as the roles and contributions of nurses in stroke rehabilitation units. Table 2 demonstrates study findings that relate to Theme 2: How nurses perform their roles to support and promote recovery of patients in stroke rehabilitation units. Table 3 demonstrates study findings that relate to Theme 3: Factors that impact nurses’ working conditions on stroke rehabilitation units.
Table 1.
Study themes which answer research question one: “What specific skills or tasks have been identified as the roles and contributions of nurses in stroke rehabilitation units?”.
| Primary Author, Year Country of Origin Method Sample Quality Rating |
Findings | |
|---|---|---|
| Assisting With Performance of Daily Living Activities | Administering and Monitoring Therapeutic Interventions | |
| Aadal et al. (2018) Denmark Hermeneutic phenomenology N=19 Nurses Good |
• Provide care for relatives in crisis • Involve relatives in goals setting. • Remain present with patient and relatives, 24×7 |
|
| Barreca & Wilkins (2008) Canada Hermeneutic phenomenology N=8 RNs, RPNs Good |
• Provide care 24×7 • Assist patients to perform daily activities |
|
| Burton (2000) United Kingdom Reflective inquiry N=13 RN, EN Good |
• With patient 24×7 • Provide basic care of physical needs (e.g., provide nutrition, hydration, elimination, hygiene) • Facilitate recovery by helping patients to translate skills learned during therapy to performing daily living activities |
• Administer medications to prevent further infarction • Perform wound dressings • Performs risk assessment to prevent harm and maintain safety |
| Clarke & Holts (2015) United Kingdom Mixed method: Q-methodological approach N=63 RNs Good |
• Facilitate and enable patients to develop confidence and skills to perform tasks independently • Initiate baths and feeding but encourages patient to perform them independently until they are unable. • Assist patients with eating, drinking, walking |
• Administers medication • Performs physiological assessments • Manages continence issues • Performs wound dressings |
| Dreyer et al. (2016) Denmark Hermeneutic phenomenology N=19 Nurses Good |
• With patient 24×7 • Meet basic needs • Manage and provide nutrition, hygiene • Assist with mobilization • Provide opportunities for sleep, rest, and stimulation • Assist patient with toileting • Assist with oral care • Develop and implement care plan • Ensure patients sleep and rest after exercise and activity • Involve relatives in patient’s care • Provide care for relatives |
• Administer medications • Monitors vital signs • Performs pain assessment • Monitors patient’s weight and height |
| Hill & Johnson (1999) United Kingdom Qualitative descriptive N=9 RNs Fair |
• Guide patients to perform tasks for themselves • Present with patient 24×7 • Continuously help patients to practice skills (e.g., mobilization) learned during therapy • Assist with bathing, and continence care • Facilitate sleep • Provide skin care • Provide nutrition • Help patients to achieve maximum independence |
• Administers medications • Dressing changes • Pain control |
| Loft et al. (2017) Qualitative descriptive Denmark N=14 RNs Good |
• Present with the patient 24×7 • Provide basic care needs and support • Assist with mobility and transfers • Help patients to repeat and practice interventions (prescribed by therapists) throughout the day • Prepare for rounds • Perform administrative tasks |
• Administer medications • Guide patients to self administer medications |
Note: EN=Enrolled Nurses; RN=Registered Nurses; RPN=Registered Practical Nurses.
Table 2.
Study themes which answer research question two: “How do nurses perform their roles to support and promote recovery of patients in stroke rehabilitation units?”.
| Primary Author, Year Method Sample Quality Rating |
Findings | ||
|---|---|---|---|
| Teaching and Coaching | Emotional and Psychosocial Support | Care coordination, Management, Advocacy, and Collaboration | |
| Aadal et al. (2018) Denmark Hermeneutic phenomenology N=19 Nurses Good |
• Teach patients and relatives about life at home after discharge • Inform, teach, and talk with both patients and relatives to facilitate mutual understanding of the patient’s condition |
• Prepare relatives to cope role as caregiver • Provide care for relatives in crisis • Create time to be with the relatives and talk to them about their feelings and how they dealt with crisis in the past • Be aware of how the relatives react to the crisis • Unable to step back from helping a patient to perform an activity |
• Facilitate communication and cooperation between relatives and the care team • Sets targets with relatives and patients • Involves relatives in care planning and decision-making • Clarify the patient’s needs through the relatives • Engage relatives to contribute their knowledge and resources toward patient care |
| Barreca & Wilkins (2008) Canada Hermeneutic phenomenology N=8 RNs, RPNs Good |
• Cue and teach patients • Help patients to relearn functional tasks |
• Unable to step back from helping the patient to perform an activity | • Offer alternative interpretations to patient circumstances • Uses humor to cope with problems • Collaborates with interprofessional teams • Clarify questions from team members because of being present with patient 24×7 |
| Burton (2000) United Kingdom Reflective inquiry N=13 RN, EN Good |
• Teach patients and families the work of other therapists • Teach patients about harm prevention |
• Provides comfort for patients • Helps patients to cope with their condition • Provide social support |
• Coordinates the multidisciplinary teams by liaising, organizing, mediating, and planning care • Inform others about patient’s progress, coping, emotional health, social support, and home circumstances • Facilitates recovery • Advocates for patients and families |
| Clarke & Holts (2015) United Kingdom Mixed method: Q-methodological approach N=63 RNs Good |
• Provides social and emotional support | • Collaborate with other members of the • Use multidisciplinary team approach to facilitate client’s independence • Coordinates patients, families, and team to provide quality care for patients |
|
| Dreyer et al. (2016) Denmark Hermeneutic phenomenology N=19 Nurses Good |
• Train patients and relatives to perform daily living activities like bathing, brushing teeth | • Knowing patient as a person (her preferences, social/family life, ways of coping with or managing illness) facilitates provision of care, implementation of rehabilitation interventions, and accomplishment of goals • Establish therapeutic relationship with patients and families to facilitate implementation of goals set by team • Create time and hope for the patient. |
• Involve patients in care planning • Integrate patient’s perspectives in goal setting • Coordinate care • Advocate for patients and families • Facilitate communication and cooperation between patients, families, and multidisciplinary team during rehabilitation • Engage relatives resource persons for support and information about patient’s condition and progress |
| Hill & Johnson (1999) United Kingdom Qualitative descriptive N=9 RNs Fair |
• Teach and inform patients about their general condition • Train patients how to self-administer medications |
• Facilitate patient’s acceptance of reality (disability) using counselling • Enable patients to take responsibility for self-care • Establish therapeutic relationship with patient |
• Coordinate care and present feedback about patient’s progress to the team |
| Loft et al. (2017) Qualitative descriptive Denmark N=14 RNs Good |
• Continuously teach patients to practice newly learned skills | • Know the patient as a person, • provide social and emotional support • Struggles to step back or perform tasks “with patient” and not of “for the patient” • Establish therapeutic relationships with patients |
• Coordinates patient care, collaboration between patients, families, and multidisciplinary team |
Note: EN=Enrolled Nurses; RN=Registered Nurses; RPN=Registered Practical Nurses.
Table 3.
Study themes which answer research question three: “What factors have been identified to impact the nurses’ working conditions on stroke rehabilitation units?”.
| Primary Author, Year Method Sample Quality Rating |
Findings | |
|---|---|---|
| Barriers and Challenges | Nurses’ Perceptions | |
| Aadal et al. (2018) Denmark Hermeneutic phenomenology N=19 Nurses Good |
• No time set aside to care for relatives • Preparing relatives to cope with unknown situation. • Non-cooperating relatives • Persistent cognitive, emotional, and behavioral changes in patients • Lack of specialty knowledge on stroke rehabilitation • Lack of organizational framework to support interventions |
• Belief that nurses have a dual role in stroke rehabilitation |
| Barreca & Wilkins (2008) Canada Hermeneutic phenomenology N=8 RNs, RPNs Good |
• Limited resources • Lack of time • Supervision of everyday practice may cause missed opportunities to care • Feeling that others devalue their role • The struggle with personal inclinations to do everything for the patient • Shortage of staff • Increased workload • Lack of recognition of nurse’s role in rehabilitation |
• Belief that nurses play a pivotal role in rehabilitation • Feeling that their role in stroke rehabilitation is devalued by others • The joy of working in stroke rehabilitation units • Belief that there is lack of recognition of nurse’s role in the rehabilitation process |
| Burton (2000) United Kingdom Reflective inquiry N=13 RN, EN Good |
• Personal beliefs about the purpose of rehabilitation | |
| Clarke & Holts (2015) United Kingdom Mixed method: Q-methodological approach N=63 RNs Good |
• Lack of specific training to integrate rehab principles with care | |
| Dreyer et al. (2016) Denmark Hermeneutic phenomenology N=19 Nurses Good |
• Lack of time | • Belief that nurses are vital members of the interprofessional team |
| Hill & Johnson (1999) United Kingdom Qualitative descriptive N=9 RNs Fair |
• Shortage of staff • Reliance on temporary staff • High turnover of physiotherapists and occupational therapists |
• Role as informal patient counselor not fully acknowledged • Nurses have a role as liaison to other team members • Nurses have a role as central communicator, reporting information to the multidisciplinary team about their patient’s progress. • Nurses have to possess a variety of the therapists’ skills to perform their role well |
| Loft et al. (2017) Qualitative descriptive Denmark N=14 RNs Good |
• Lack of specific training related to stroke rehabilitation • Lack of time to assist patients to perform tasks • Complexity of tasks or patient’s condition • Lack of time • Competing priorities • Work overload |
• Nurses believe and present themselves as manager in rehabilitation units |
Note: EN=Enrolled Nurses; RN=Registered Nurses; RPN=Registered Practical Nurses.
Theme 1: What Nurses Do
Assisting with Performance of Daily Living Activities
Data for the sub-theme assisting patients with performance of daily living activities emerged from all seven studies. This sub-theme described the provision of basic care for patients in stroke rehabilitation units. In nearly all studies, nurses reported that they spent 24 hours a day and 7 days a week (“24×7”) with patients providing basic care.18,19,6,20,21,22 Types of basic care needs included maintaining nutrition (e.g., feeding), providing hydration (e.g., drinking), assisting with elimination (e.g., toileting, continence care), and maintaining personal hygiene (e.g., bathing, dressing, grooming, oral care, skin care).6,4,20,21,22 Further, to maximize a patient’s independence in the performance of daily activities, nurses stated that they would initiate an activity (e.g., bathing, feeding), then coach and encourage the patient to perform it independently until the patient was able to continue without assistance. 4 Nurses also reported that they provided opportunities for sleep, rest, and stimulation, 20 particularly after exercise or activity.20,21 Provision of skin care was also identified as an important nurse role to prevent skin complications such as pressure ulcers. 21
In some studies, nurses reported that they facilitated stroke recovery by helping patients use the skills they learned during physiotherapy and occupational therapy to perform their daily living activities.6,21 Some of the nurses reported that throughout the day they help patients post-stroke to repeat and practice interventions prescribed or planned by these other members of the interprofessional team. 22 This constant practice of rehabilitation interventions is thought to enable patients post-stroke to further develop confidence and skills to perform tasks independently.4,21 The nurses reported that by continuously assisting patients to practice mobility and transfer skills, they help the patients integrate these skills within their daily activities and achieve maximum independence in performing them.20,21,22
Administering and Monitoring Therapeutic Interventions
Five studies reported data pertaining to the sub-theme administering and monitoring therapeutic interventions.6,4,20,21,22 Nurses reported that they administer and monitor therapeutic interventions to patients to meet their physical needs, maintain safety, and prevent harm. 6 Nurses reported administering medications to patients to prevent further cerebral infarction and treat post-stroke complications and comorbidities; some medications are also administered to control pain following pain assessment.20,21 In multiple studies, nurses identified wound dressing as another therapeutic intervention that they perform for patients with stroke who have developed pressure ulcers.6,4,21,22 Nurses also identified continence care as an intervention that they perform for patients, directed at meeting the individual needs of patients with bowel and bladder impairments. Other therapeutic interventions included monitoring vital signs (such as temperature, respiration, pulse, blood pressure) and documenting patients’ height and weight. 20 In one study, nurses reported that they perform risk assessments to prevent harm to the patient and to maintain the patient’s safety. 6
Theme 2: How Nurses Perform
Teaching and Coaching
In six studies, nurses identified teaching and coaching as one of their roles that demonstrate how nurses support and promote the rehabilitation and recovery of patients with stroke.18,19,6,20,21,22 In Hill and Johnson’s 21 study, nurses reported that they inform and educate patients about their health condition. Some of the nurses said that they teach, inform, and educate both patients and family/caregivers to facilitate a mutual understanding of the condition and prognosis of the patients. 18 Nurses also reported that they teach specific skills to patients and family/caregivers to promote patients’ independence through ‘hands-off nursing’ (taking a supervisory role and guiding patients and caregivers to perform the prescribed tasks for themselves) and to facilitate the development of an informal caregiving role. 21 In some studies, patients were taught how to self-administer medications to prevent self-harm from accidental overdose of medications.6,21 Both patients and their family/caregivers were trained to modify their basic daily activities (e.g., bathing, mouth care, and dressing) so that they could be performed independently. 20 The nurses reportedly taught patients to continually practice the skills they learned from speech and language pathologists, occupational therapists, physiotherapists, and other members of the rehabilitation team. 6 Both patients and family/caregivers were taught about life at home after discharge and how a patient’s illness may alter their routine habits and practices. 19
Emotional and Psychosocial Support
In all seven studies that were reviewed, emotional and psychosocial support emerged as an important way nurses support patients post-stroke in rehabilitation units. In one of the studies, nurses reported that they provide emotional and social support for family/caregivers of patients after stroke. 18 Family and caregivers were perceived to experience crisis when caring for a loved one after a stroke. To provide effective and quality care for family members and caregivers, nurses co-developed strategies to help family members and caregivers to cope with the situation and the needs required of them. 18 Strategies included creating time to be present, talking about their feelings, and determining how crises have been dealt with in the past. 18 Creating time for family/caregivers allowed nurses to assess and understand their needs and frustrations. Nurses reported that knowing a patient as a person (i.e., their personal preferences, ways of coping and managing stress or illness, family/social life, and social support system) was necessary to understand the needs of the patient, provide emotional and social support, and gain the patient’s cooperation and participation during rehabilitation. 20 Knowing the patient as a person also facilitated provision of care, implementation of rehabilitation interventions, and achievement of patients’ rehabilitation goals. 20
Nurses reported that establishing therapeutic relationships to facilitate the completion of rehabilitation goals was important.20,21,22 Nurses believed that establishing therapeutic relationships through counseling facilitated patients’ acceptance of reality (i.e., impairment or disability) and helped the patients to be more responsible for their self-care. 21 In some studies, nurses reported that they felt inclined to do tasks for the patient instead of “stepping back” to allow the patient to do the tasks themselves.18,19,22 This difficulty of “stepping back” was attributed to fear of criticisms for allowing a patient with impairment to struggle to complete their daily living activities. Although some nurses expressed difficulty “stepping back” and allowing the patient to perform tasks independently, the nurses acknowledged that it was part of their role to allow the patient to practice the skills that they had learned.18,19,22
Care Coordination, Management, Advocacy, and Collaboration
All seven studies addressed the nurses’ role in relation to care coordination, care management, advocacy, and collaboration. Nurses reported that they coordinate and mediate care activities and contributions of patients, family/caregivers, and the interprofessional team to promote well-being, enable smooth transitions of care, and maintain progress toward goals.6,4,20,21,22 Nurses reported that they coordinate care by liaising, organizing, mediating, and planning activities that focus on patients and family/caregiver centered care. 6 Nurses reported attending care conferences (“rounds”) to provide feedback on patient progress to the interprofessional team 21 and to clarify questions from team members. 19
In stroke rehabilitation, nurses used communication strategies to facilitate cooperation between patients, family/caregivers, and the interprofessional team.18,20 Using effective communication, nurses engage family/caregivers in care planning as resource persons for support and information about patient progress.18,20 Among patients with cognitive or communication impairments, nurses relied on the help of family/caregivers who may serve as the patient’s voice and clarify their needs.18,20 To achieve rehabilitation goals set by the rehabilitation team, nurses reported that they involve patients, families, and caregivers during care planning and decision-making, seek and integrate their perspectives in goal setting, and set rehabilitation targets according to the needs of the individual patient.18,20
Nurses reported that they collaborate with other members of the interprofessional team to implement rehabilitation interventions; provide information on patient progress; 19 inform others about coping, emotional health, social support, and home circumstances; 6 and facilitate patients’ recovery and independence in performance of daily living activities.19,4
Theme 3: Factors Identified to Impact Nurses’ Working Conditions on Stroke Rehabilitation Units
Barriers and Challenges of Nursing Rehabilitation
Six studies addressed barriers and challenges that nurses encounter in stroke rehabilitation units.18,19,4,20,21,22 These barriers and challenges related to time, staff shortages, workload, medical complexity, family/caregiver relationships, training and knowledge specific to stroke, and professional devaluation.
The lack of time to meet the basic needs of patients and family/caregivers was reported by nurses as decreasing the quality of care they provided.18,19,4,20,22 Specific timing challenges mentioned included lack of time to assist patients with performance of tasks 22 and lack of time set aside to support, inform, and educate patients and family/caregivers. 18
Staff shortages and limited resources were reported as making it difficult for nurses to attend team conferences since there were no additional nurses to replace them on the unit. 19 Frequent absences of nurses from team conferences resulted in missed opportunities for nurses to inform other interprofessional team members about their daily interactions with patients. Nurses reported that they relied on temporary staff to complete tasks, and that a high turnover of occupational therapists and physiotherapists prevented the rehabilitation nursing team from practicing to their fullest potential. 21 Nurses felt that competing priorities 22 and work overload were factors that caused burnout among experienced nurses.21,22 The nurses felt that these issues potentially discouraged new nurses from joining the profession.19,22 Nurses believed that excessive workloads contributed to greater injury, higher absenteeism, and higher stress in clinical settings. 19
Complexity of patients’ treatment, brain injury, and comorbidities heavily influenced nurses’ working conditions on stroke rehabilitation units.18,22 Patients with high post-stroke medical acuity during inpatient rehabilitation tended to have complex needs which warranted a substantial number of nursing activities to be performed. Persistent post-stroke cognitive, emotional, and behavioral impairments were cited as factors that complicated the provision and quality of care that could be provided. 18
Nurses reported that difficulties forming a positive relationship with family/caregivers impacted their working conditions on stroke rehabilitation units. Nurses attributed their inability to meaningfully form relationships to a lack of time to support, inform, and educate family/caregivers about their patient’s condition or to provide patient-centered care. 18
Nurses noted that a lack of stroke-specific knowledge and training hindered their ability to integrate stroke rehabilitation principles within their daily care.18,4,22 This lack of specialty knowledge regarding stroke rehabilitation was ascribed to a lack of time in daily practice for adequate education. 4 Another perceived reason was the lack of a professional habit of searching for specialized knowledge and/or scientific evidence during their spare time. 22
Nurses felt that they lacked recognition of their role in the rehabilitation process and this significantly influenced their working conditions on inpatient stroke rehabilitation units. 19 Nurses reported feeling that patients, family/caregivers, managers, and other interprofessional team members devalued the nursing role. 19 This undervalued rehabilitation nursing role was attributed to several factors: the lack of respect that nurses receive, minimal attention directed at what the nurses think about rehabilitation, budget cuts that affect nursing functions, lack of sufficient leadership and management positions for nurses, and nurses’ lack of control over their work environment. 19
Nurses’ Perceptions of Their Role in Stroke Rehabilitation
Nurses’ perceptions regarding their roles and contributions to stroke rehabilitation were identified as a factor that impacts their working conditions. In one study, nurses expressed personal views about rehabilitation and the relationships that they develop with other nurses, patients, family/caregivers, and other team members. 6 In all seven studies, nurses believed that they play a vital and personal role in the rehabilitation and recovery of patients with stroke.18,19,6,4,20,21,22 In another study, nurses stated that they enjoy providing care for patients after stroke. 19 Nurses referred to their role as pivotal (i.e., extensive and essential) to the rehabilitation process; they are present with the patient continuously through the day and night, teaching and cueing patients to help them relearn how to perform daily living activities. 19 Nurses also reported that they played a dual role in stroke rehabilitation, which included caring for both patients and families/caregivers. 18 This dual role was considered challenging since both patient and family/caregivers often experience personal crises at the same time, thus making it difficult for nurses to support and meet the needs of both parties. 18
Some nurses perceived their role as being a liaison to other team members and reported that they function as informal counselors to patients undergoing inpatient stroke rehabilitation. However, the nurses expressed concerns that their counselor or liaison role had not been fully acknowledged by other members of the interprofessional team.21,22 Nurses also felt that they struggled intrapersonally. For example, many spoke about having an inclination to “do everything” for patients. 19 They noted that they experienced difficulties stepping back and allowing stroke patients to perform certain tasks for themselves. There was also a concern that nurses may potentially face criticisms for allowing patients who need help to struggle. 19 Nurses viewed and presented themselves as “project managers” for stroke patients undergoing rehabilitation. This view was related to the fact that nurses in this review tended to bear the responsibility of organizing patient care, including the physical and social environment where rehabilitation occurs. 22 Regarding the care coordination role, nurses perceived themselves as being responsible for ensuring that all activities related to patient care (e.g., goal setting, preparation for scans, medication administration, discharge planning, follow-up care, and writing of report for community care) were facilitated and monitored. 3 Nurses also viewed their role in the interprofessional team as the central communicator, reporting information about patient progress, 21 advocating for patients, and coordinating all services. 22
Discussion
This integrative review synthesized the findings from seven studies in the literature on the roles and contributions of nurses in stroke rehabilitation units. According to Hawker et al.’s 2002 criteria for evaluating quality of evidence, a majority of the studies were of good quality, and were regarded as level six evidence. 17 Most studies originated from Europe; hence, the review findings are largely situated within this geo-sociocultural perspective. The greatest proportion of nurses included in the reviewed studies were Registered Nurses, suggesting that fewer studies have been conducted among other categories or designations of nurses in rehabilitation units (e.g., Registered Practical Nurses in Ontario, Canada; Enrolled Nurses in Australia, Nurse Associate in the United Kingdom). Further, the category of nurses and their subsequent differences in roles and contributions by varying levels of nursing education were inconsistently described across studies. The single Canadian study reported that the rehabilitation roles and contributions were the same between Registered Nurses and Registered Practical Nurses in Ontario, Canada. 19 This may suggest similarities and overlap in the scope and standards of practice for these two nursing designations within inpatient stroke rehabilitation settings in Canada. Significantly more research is required to better understand the distinction in contributions between nursing levels.
Consistent findings across the reviewed studies were demonstrated for each of the three research questions; this may be viewed as a reflection of the strength of the evidence that was reviewed. The first research question aimed to identify what specific skills or tasks are considered to be part of the roles and contributions of stroke rehabilitation nurses. The results showed that nurses provide direct care for patients by assisting with daily living activities (e.g., nutrition, hygiene, dressing, mobility/transfers, toileting, rest, exercise, skin care), monitoring or assessing to detect deviations (e.g., vital signs, blood glucose, input/outputs, pain assessment), and administering therapeutic interventions (e.g., medication administration, wound care) to treat complications and comorbidities, manage pain, and promote recovery. Nearly all the studies indicated that nurses spent the greatest number of hours providing basic care for patients recovering from a stroke. The findings were consistent in showcasing the nurses’ vital role in the rehabilitation and recovery of patients with stroke.
The second research question aimed to identify how nurses perform their roles to support and promote recovery of patients post-stroke. The reviewed literature is consistent with previous evidence that nurses teach and coach patients as part of their stroke rehabilitation roles, as well as provide emotional and psychosocial support. 11 Nurses were reported to educate and inform patients and families/caregivers on health conditions, promote independence in performance of daily activities, prevent harm (e.g., accidental medication overdose), and prepare the patients and families/caregivers for life after discharge from inpatient rehabilitation units. Nurses reportedly used strategies to help patients and families/caregivers promote coping via “creating time,” talking, and using effective therapeutic communication. The review also complements previous reports that nurses coordinate and manage rehabilitation care as well as advocate for patients and their families/caregivers. 11 Coordinating care activities were noted to enable smooth care transitions, promote the wellbeing of patients, and maintain progress toward rehabilitation goals. 6
The third research question aimed to identify factors that impact nurses’ working conditions on stroke rehabilitation units. The findings from this review support previous evidence that nurses experience barriers and challenges during stroke rehabilitation nursing practice 23 including time constraints, shortage of staff, increased workload, medically complex patients, family/caregiver relationships, deficiencies of stroke-specific knowledge/education, and devaluation of professional nursing roles in rehabilitation units. These factors were described in nearly all included studies and align with findings from previous research showing that these factors impact nurses’ role in stroke rehabilitation. 23 Considering that the studies had good methodological quality, their findings are relevant to clinical practice and can be used by rehabilitation clinicians and administrators to improve the nursing environment. The findings may be useful in identifying and managing challenges to rehabilitation nursing care, implementing effective rehabilitation techniques, and adequately measuring and documenting nursing activities and efforts.
There are a few limitations of this review worth noting. First, only original research articles written in the English language and published in peer-reviewed journals were included. As such, there may be other relevant articles on this topic written in other languages or in grey literature with the findings unincorporated in this paper. Second, the included studies did not always report designations of nurses (e.g., Registered Nurse versus Registered Practical Nurse). Any documentation developed without further research would need to be flexible for reporting of nursing activities across the scopes of practices of different categories of nurses. Finally, only studies reporting on the roles and contributions from the nursing perspective were included, at the exclusion of non-nursing rehabilitation professionals, as well as patients and families/caregivers; thus, critical insights from other individuals were not included in this review.
Relevance to Clinical Practice
Several important implications concerning nursing rehabilitation practice were highlighted in this review. First, the review findings have demonstrated that there is no formal or standardized documentation to report nursing contributions to inpatient stroke rehabilitation, despite the rehabilitation-focused patient care activities performed by nurses. Lack of reporting contrasts with formal documentation practices required by occupational therapists, physiotherapists, speech language pathologists, and other members of the interdisciplinary rehabilitation team. For example, in Canada, physiotherapists and occupational therapists are required to document their patient care activities, including rehabilitation intensity, for stroke inpatient rehabilitation units via an electronic National Rehabilitation Reporting System. 24 The findings from this review demonstrate that nurses are performing rehabilitation-supporting patient care in “what nurses do.” It suggests an imperative for institutions to develop formalized reporting practices to recognize nursing contributions to inpatient stroke rehabilitation.
Second, the review findings indicate that how nurses perform their care practices is aligned with other members of, and integral to, the interprofessional team. Nurses use interprofessional team approaches to facilitate clients’ independence by coordinating patients, families, and the team to provide quality care. 4 The nurses promote patient-centered care by involving patients in care planning, advocating for the patients and families, and integrating the perspectives of patients and families in goal setting. 20 Nurses further collaborate with interprofessional teams by facilitating communication and cooperation between patients, families, and the interprofessional team. 20 Nurses utilize effective leadership and management strategies (e.g., effective communication) to coordinate multidisciplinary teams by liaising, organizing, mediating, and planning the patient’s care. 6
Third, the findings of this review identified factors that impact nurses and impart challenges and barriers affecting working conditions on stroke rehabilitation units. Importantly, nurses reported that their knowledge and skills are inadequate to manage patients. The review revealed there were no mandatory requirements for specific competencies for nurses in rehabilitation units, and there may have been limited education provided. As expressed by the nurses of the included studies, there may be a significant need for nurses to have access and training in a specialist stroke rehabilitation training program. 4 Such a program would not only reinforce necessary stroke-specific nursing skills but change the focus of stroke care from acute management of stroke to provision of rehabilitation care, thereby improving the effectiveness of rehabilitation services. 25
Next, nurses felt that they lacked respect, were unsupported, and were devalued by patients, families, and the interprofessional team. This lack of respect for nurses was shown by the little attention paid to what nurses think, how their lives were controlled by budget cuts at the expense of patient care, 26 the inadequate leadership and management positions for nurses, and the lack of control over the work environment. 19 The lack of value for nursing’s role in rehabilitation may be attributed to the misconception that nurses are lower-level staff expected to assist patients whenever they need assistance; the view that nursing functions are lower level functions (e.g., toileting and cleaning of patient’s private parts); the view of nurses as a “means to an end” (e.g., moving patients to physiotherapy room on time to meet the rehabilitation goals); the disregard for suggestions from nurses; and the frequent disruption of daily work routines of nurses. 19 These perceptions all contribute to the frustrations of nurses and their relationships with management, which causes nurses to feel disenfranchised. 19 To cope with the lack of respect and value for nurses in stroke rehabilitation units, nurses utilize strategies such as humor, self-control, and walking away from stressful situations. 19 Other ways of addressing concerns of rehabilitation nurses are allowing nurses some control over their work environment, offering more respect for nursing expertise, empowering nurses to be equal partners within the stroke rehabilitation team, creating more leadership and management positions for nurses, and educating patients, families/caregivers, and the interprofessional teams about the role and contributions of nurses to stroke rehabilitation. 19 To fully understand the degree to which stroke rehabilitation nurses feel empowered in rehabilitation units, and to understand the ways that nursing contributions to rehabilitation are documented and measured, further studies are needed.
Finally, the notion of nursing invisibility, particularly in rehabilitation, has been previously noted. 27 The work of rehabilitation nurses has been critiqued as invisible to nurses, patients, families/caregivers, and other members of the interdisciplinary team. 27 This invisibility is attributed to the poorly defined nature of nurses’ rehabilitation work, the lack of clarification of role expectations and boundaries, 28 the perception that nursing voices are often excluded from formal communications during decision-making, the lack of value given to nursing care during team conferences, 20 and the view that nurses’ work occurs in invisible spaces and is taken for granted. 27 Attempts have been made to promote visibility of nursing contributions to stroke rehabilitation, but the role of nurses in interprofessional rehabilitation teams has remained unclear,29,22 misunderstood, or misinterpreted. 30 One of the attempts to increase visibility of nursing contributions to rehabilitation is the development of competencies for stroke rehabilitation nurses. 31 The lack of stroke rehabilitation competencies for nurses in the Canadian context suggests the need for further studies to develop specific competencies for stroke rehabilitation nursing in Canada.
Conclusion
This integrative review synthesized the findings from seven studies and demonstrated the rehabilitation-focused role and contributions of nurses to inpatient stroke rehabilitation. Future research should examine rehabilitation nursing in other geo-cultural contexts and among differing nurse designations. Finally, studies should explore the barriers and challenges to nurses in reporting nursing practice in the inpatient stroke rehabilitation setting, including health care team meetings, measurement of treatment intensity, and documentation, for example, as well as solutions to overcome these issues.
Supplemental Material
Supplemental material, sj-pdf-1-wjn-10.1177_01939459231178495 for The Role and Contributions of Nurses in Stroke Rehabilitation Units: An Integrative Review by Eric F. Tanlaka, Amanda McIntyre, Denise Connelly, Nicole Guitar, Angela Nguyen and Nancy Snobelen in Western Journal of Nursing Research
Supplemental material, sj-pdf-2-wjn-10.1177_01939459231178495 for The Role and Contributions of Nurses in Stroke Rehabilitation Units: An Integrative Review by Eric F. Tanlaka, Amanda McIntyre, Denise Connelly, Nicole Guitar, Angela Nguyen and Nancy Snobelen in Western Journal of Nursing Research
Footnotes
The authors declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Nancy Snobelen is employed at WeRPN (Registered Practical Nurses Association of Ontario) in Professional Practice and Research. However, Nancy Snobelen was not an investigator on the grant obtained from WeRPN as described in Funding Source.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Denise Connelly (PI), Amanda McIntyre (Co-I), and Eric Tanlaka (Co-I) are recipients of a grant from WeRPN (Registered Practical Nurses Association of Ontario) for 2021-2022.
ORCID iD: Eric F. Tanlaka  https://orcid.org/0000-0002-0897-8367
https://orcid.org/0000-0002-0897-8367
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Hebert D, Lindsay MP, McIntyre A, Kirton A, Rumney PG, Bagg S, Bayley M, Dowlatshahi D, Dukelow S, Garnhum M, Glasser E. Canadian stroke best practice recommendations: Stroke rehabilitation practice guidelines, update 2015. Int J Stroke. 2016;11(4):459-84. 10.1177/1747493016643553 [DOI] [PubMed] [Google Scholar]
- 2. Canadian Institute for Health Information. Hospital report: rehabilitation. 2007. Accessed May 22, 2023. https://secure.cihi.ca/free_products/OHA_Rehab_07_EN_final_secure.pdf
- 3. Clarke DJ. Nursing practice in stroke rehabilitation: Systematic review and meta-ethnography. J Clin Nurs. 2014;23(9-10):1201-26. 10.1111/jocn.12334 [DOI] [PubMed] [Google Scholar]
- 4. Clarke DJ, Holt J. Understanding nursing practice in stroke units: A Q-methodological study. Disabil Rehabil. 2015;37(20):1870-80. 10.3109/09638288.2014.986588 [DOI] [PubMed] [Google Scholar]
- 5. Gibbon B. Implications for nurses in approaches to the management of stroke rehabilitation: a review of the literature. Int J Nurs Stud. 1993;30(2):133-41. 10.1016/0020-7489(93)90063-z [DOI] [PubMed] [Google Scholar]
- 6. Burton CR. A description of the nursing role in stroke rehabilitation. J Adv Nurs. 2000;32(1):174-81. 10.1046/j.1365-2648.2000.01411.x [DOI] [PubMed] [Google Scholar]
- 7. Baker M, Pryor J, Fisher M. Nursing practice in inpatient rehabilitation: A narrative review (part 1). JARNA. 2019;22(2):7-21. https://search.informit.org/doi/10.3316/informit.738262658572067 [Google Scholar]
- 8. Kirkevold M. The role of nursing in the rehabilitation of stroke survivors: An extended theoretical account. ANS Adv Nurs Sci. 2010;33(1):E27-40. 10.1097/ANS.0b013e3181cd837f [DOI] [PubMed] [Google Scholar]
- 9. Hankey GJ, Langhorne P. Services for reducing the duration of hospital care for acute stroke patients. Stroke. 2006;37(1):276-7. https://eurekamag.com/research/063/507/063507137.php [Google Scholar]
- 10. Long AF, Kneafsey R, Ryan J, Berry J. The role of the nurse within the multi-professional rehabilitation team. J Adv Nurs. 2002;37(1):70-8. 10.1046/j.1365-2648.2002.02059. [DOI] [PubMed] [Google Scholar]
- 11. Pryor J, Smith C. A framework for the role of registered nurses in the specialty practice of rehabilitation nursing in Australia. J Adv Nurs. 2002;39(3):249-57. https://onlinelibrary.wiley.com/doi/abs/10.1046/j.1365-2648.2002.02271.x [DOI] [PubMed] [Google Scholar]
- 12. Pryor J. A nursing perspective on the relationship between nursing and allied health in inpatient rehabilitation. Disabil Rehabil. 2008;30(4):314-22. 10.1080/09638280701256900 [DOI] [PubMed] [Google Scholar]
- 13. De Weerdt W, Nuyens G, Feys H, Vangronsveld P, Van de Winckel A, Nieuwboer A, Osaer J, Kiekens C. Group physiotherapy improves time use by patients with stroke in rehabilitation. Aust J Physiother. 2001;47(1):53-61. 10.1016/s0004-9514(14)60298-1 [DOI] [PubMed] [Google Scholar]
- 14. MacDonell CM, Mauk KL. Where in the World Is Rehabilitation Nursing? Rehabil Nurs J. 2017;42(4):173-4. 10.1097/rnj.0000000000000105 [DOI] [PubMed] [Google Scholar]
- 15. Whittemore R, Knafl K. The integrative review: Updated methodology. J Adv Nurs. 2005;52(5):546-53. 10.1111/j.1365-2648.2005.03621.x [DOI] [PubMed] [Google Scholar]
- 16. Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MD, Horsley T, Weeks L, Hempel S. PRISMA extension for scoping reviews (PRISMA-ScR): Checklist and explanation. Ann Intern Med. 2018;169(7):467-73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 17. Hawker P, Powell Kerr H. Appraising the evidence: Re-viewing disparate data systematically. Qual Health Res. 2020;12(9):1284-99. 10.1177/1049732302238251 [DOI] [PubMed] [Google Scholar]
- 18. Aadal L, Angel S, Langhorn L, Pedersen BB, Dreyer P. Nursing roles and functions addressing relatives during in-hospital rehabilitation following stroke. Care needs and involvement. Scand J Caring Sci. 2018;32(2):871-9. 10.1111/scs.12518 [DOI] [PubMed] [Google Scholar]
- 19. Barreca S, Wilkins S. Experiences of nurses working in a stroke rehabilitation unit. J Adv Nurs. 2008;63(1):36-44. 10.1111/j.1365-2648.2008.04648.x [DOI] [PubMed] [Google Scholar]
- 20. Dreyer P, Angel S, Langhorn L, Pedersen BB, Aadal L. Nursing roles and functions in the acute and subacute rehabilitation of patients with stroke: Going all in for the patient. J Neurosurg Nurs. 2016;48(2):111-8. 10.1097/jnn.0000000000000191. [DOI] [PubMed] [Google Scholar]
- 21. Hill MC, Johnson J. An exploratory study of nurses’ perceptions of their role in neurological rehabilitation. Rehabil Nurs. 1999;24(4):152-7. 10.1002/j.2048-7940.1999.tb02163.x [DOI] [PubMed] [Google Scholar]
- 22. Loft MI, Poulsen I, Esbensen BA, Iversen HK, Mathiesen LL, Martinsen B. Nurses’ and nurse assistants’ beliefs, attitudes and actions related to role and function in an inpatient stroke rehabilitation unit—A qualitative study. J Clin Nurs. 2017;26(23-24):4905-14. 10.1111/jocn.13972 [DOI] [PubMed] [Google Scholar]
- 23. Seneviratne CC, Mather CM, Then KL. Understanding nursing on an acute stroke unit: perceptions of space, time and interprofessional practice. J Adv Nurs. 2009;65(9):1872-81. 10.1111/j.1365-2648.2009.05053. [DOI] [PubMed] [Google Scholar]
- 24. Canadian Institute for Health Information. National Rehabilitation Reporting System Metadata. 2022. Accessed May 22, 2023. https://www.cihi.ca/en/national-rehabilitation-reporting-system-metadata.
- 25. Teasell R, Hussein N, McClure A, Meyer M. Stroke: more than a ‘brain attack’. Int J Stroke. 2014;9(2):188-90. 10.1111/ijs.12233 [DOI] [PubMed] [Google Scholar]
- 26. Canadian Nursing Advisory Committee (CNAC). Our Health, our future: Creating quality workplaces for Canadian nurses. The final report of the Canadian Nursing Advisory Committee, 2002. Ottawa, ON. Accessed May 22, 2023. https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/hcs-sss/alt_formats/hpb-dgps/pdf/pubs/2002-cnac-cccsi-final/2002-cnac-cccsi-final-eng.pdf [Google Scholar]
- 27. Ehrlich C, Lewis D, New A, Jones S, Grealish L. Exploring the role of nurses in inpatient rehabilitation care teams: A scoping review. Int J Nurs Stud. 2022;128:104134. 10.1016/j.ijnurstu.2021.104134 [DOI] [PubMed] [Google Scholar]
- 28. Burke KG, Doody O. Nurses’ perceptions of their role in rehabilitation of the older person. Nurs older people. 2012;24(2). https://core.ac.uk/download/pdf/80547219.pdf [DOI] [PubMed] [Google Scholar]
- 29. Meng X, Chen X, Liu Z, Zhou L. Nursing practice in stroke rehabilitation: Perspectives from multi-disciplinary healthcare professionals. Nurs Health Sci. 2020;22(1):28-37. https://onlinelibrary.wiley.com/doi/pdfdirect/10.1111/nhs.12641 [DOI] [PubMed] [Google Scholar]
- 30. Tyrrell EF, Pryor J. Nurses as agents of change in the rehabilitation process. JARNA. 2016;19(1):13-20. https://web-p-ebscohost-com.ledproxy2.uwindsor.ca/ehost/pdfviewer/pdfviewer?vid=0&sid=181b8467-27ea-443f-b504-b83a312acb66%40redis [Google Scholar]
- 31. Vaughn S, Mauk KL, Jacelon CS, Larsen PD, Rye J, Wintersgill W, Cave CE, Dufresne D. The competency model for professional rehabilitation nursing. Rehabil Nurs. 2016;41(1):33-44. https://onlinelibrary.wiley.com/doi/pdf/10.1002/rnj.225 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-wjn-10.1177_01939459231178495 for The Role and Contributions of Nurses in Stroke Rehabilitation Units: An Integrative Review by Eric F. Tanlaka, Amanda McIntyre, Denise Connelly, Nicole Guitar, Angela Nguyen and Nancy Snobelen in Western Journal of Nursing Research
Supplemental material, sj-pdf-2-wjn-10.1177_01939459231178495 for The Role and Contributions of Nurses in Stroke Rehabilitation Units: An Integrative Review by Eric F. Tanlaka, Amanda McIntyre, Denise Connelly, Nicole Guitar, Angela Nguyen and Nancy Snobelen in Western Journal of Nursing Research