Abstract
Mechanical thrombectomy is established as standard of care in the management of acute ischemic stroke due to large vessel occlusion and evidence-based guidelines for mechanical thrombectomy have been defined. As research continues to further expand the eligibility criteria for thrombectomy and the number of thrombectomy procedures increase worldwide, there is also growing focus on innovation of thrombectomy devices, procedural techniques, and related outcomes. Thrombectomy primarily involves use of stent retrievers and distal aspiration techniques, but variations and different combinations of techniques have been reported. As this is a rapidly evolving area in stroke management, there is debate as to which, if any, of these techniques leads to improved clinical outcomes over another and there is a lack of data comparing them. In this review, currently published and distinct techniques of mechanical thrombectomy are described methodically along with illustrations to aid in understanding the subtle differences between the techniques. The perceived benefits of each variation are discussed.
Keywords: Mechanical thrombectomy, techniques, recanalization, ischemic stroke
Introduction
Acute ischemic stroke (AIS) is one of the leading causes of death and disability throughout the world. 1 Evidence-based management of ischemic strokes primarily involved treatment with intravenous (IV) thrombolysis.2,3 Recently, several clinical trials have proven the safety and efficacy of mechanical thrombectomy in AIS due to large vessel occlusion (LVO).4–8 With mechanical thrombectomy now a standard of care, there is increasing focus on innovation of thrombectomy devices and techniques, and improvement in procedural and patient outcomes in stroke management. Achievement of fast and complete recanalization of the occluded large artery is fundamental for improving patient outcomes in stroke. The primary techniques of mechanical thrombectomy involve use of a stent retriever device for clot extraction or a large diameter catheter for clot aspiration. Several different techniques of thrombectomy including combinations of stent retriever and aspiration with or without a balloon guide catheter (BGC) have been reported. The objective of this study is to review all the current reported mechanical thrombectomy techniques and discuss the differences between techniques using de novo illustrations.
Methods
A comprehensive search of the published, peer-reviewed literature in the electronic database PubMed was conducted using keywords and search terms such as “thrombectomy”, “mechanical thrombectomy”, “stent retriever”, “clot retriever”, “aspiration”, “stroke”, “large vessel occlusion”, “recanalization technique”, “acute ischemic stroke treatment”. Combination search terms with Boolean operators was employed and initial search included all studies and technical reports published between January 1, 2004 and Nov 11, 2021. This search strategy and duration was used to be inclusive of all published techniques since the approval of the first mechanical thrombectomy device by the Federal Drug Administration (FDA) in 2004. A total of 1227 records were initially identified. Only the data and reports published in English were considered (n = 965). Any study describing the obsolete device technology such as the coil retrievers was eliminated. Studies were screened to include only those that discussed the current thrombectomy techniques using aspiration catheters and stent retrievers. Studies that outlined every component of the technique in a stepwise fashion were included and studies that just mentioned the technique were excluded. Bibliographies of the included papers were reviewed for relevant literature. After screening, 50 studies discussing mechanical thrombectomy techniques were identified. Of those studies, 14 were duplicate descriptions of techniques and 23 did not describe the techniques in a step wise fashion. In this review a total of 13 studies describing the standard aspiration or stent retriever technique and other minor variations were included. All techniques detailed in this review were shown as safe and effective in respective studies. Procedural steps that are common to all techniques such as arterial access, navigation in the aortic arch, catheterization of supra-aortic vessels, etc. are not included in the descriptions.
Results
Mechanical thrombectomy techniques primarily involve use of a stent retriever, a large-bore catheter for distal aspiration, or a combination of the two, with or without a balloon guide catheter (BGC). Table 1 lists the currently approved and available stent retriever devices and aspiration catheters for use to perform thrombectomy in AIS due to LVOs. The different thrombectomy techniques and variations are presented below. All technical elaborations start from post-arterial access and positioning of a guide catheter in the common carotid or the cervical internal carotid artery (ICA) for anterior circulation and in the subclavian or vertebral artery for posterior circulation occlusions.
Table 1.
Mechanical thrombectomy devices and systems.
| Aspiration Catheters | Aspiration Pumps | Stent Retriever | |
|---|---|---|---|
| Cerenovus | Large Bore Catheter | EMBOTRAP™II Revascularization Device | |
| EMBOTRAPTM III Revascularization Device | |||
| CERENOVUS NIMBUS™ geometric clot extractor | |||
| Imperative Care | Zoom 88 Large Distal PlatformTM Zoom 71, Zoom 55, Zoom 45 and Zoom 35 Catheters | Zoom Pump | |
| Medtronic | React™ 68 Catheter | Riptide™ Aspiration Pump | Solitaire™ X revascularization device |
| React™ 71 Catheter | |||
| Microvention | SOFIA™ Plus Intermediate Catheter | Gomco™ Pump | |
| Penumbra | Penumbra System® JET 7 Reperfusion Catheter | Penumbra ENGINE® aspiration source | Penumbra System® 3D Revascularization Device™ |
| Penumbra JET™ D Reperfusion Catheter | |||
| Penumbra System® ACE™ Reperfusion Catheters | |||
| Penumbra System® MAX™ Reperfusion Catheters | |||
| Penumbra RED™ 62 Reperfusion Catheter | |||
| Stryker | AXS Vecta™ Aspiration Catheter | AXS UniversalTM Aspiration Set | Trevo XP ProVue Retriever |
| Trevo NXT ProVue Retriever | |||
| Rapid Medical | Tigertriever | ||
| Tigertriever13 | |||
| TigertrieverXL |
Stent retriever alone, with or without BGC (SRBG)
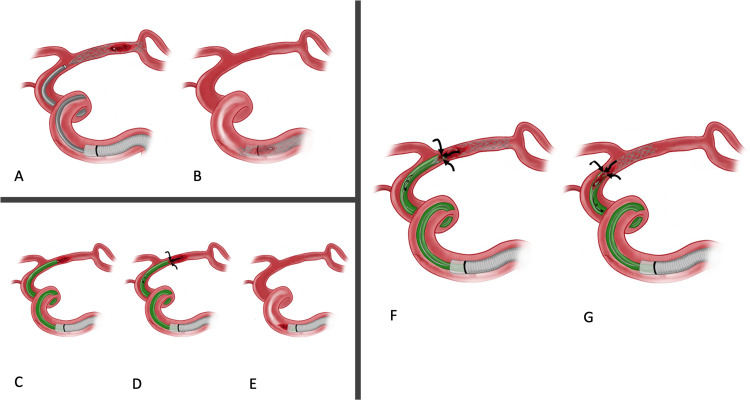
Once the guide catheter is in place, a microcatheter is advanced over a microwire and the occlusion is crossed by passing through the thrombus. The microwire is then withdrawn and a contrast injection is performed to evaluate the distal arterial segment and confirm the tip of the microcatheter is distal to the thrombus. A stent retriever is then advanced in the microcatheter and deployed across the thrombus by gradually unsheathing the microcatheter. This allows for immediate flow restoration in the previously occluded vascular territory. After a few minutes of thrombus integration in the stent retriever, the stent retriever is then slowly and carefully withdrawn into the guide catheter and removed. This technique can be combined with a BGC which is positioned in the ICA. The balloon is inflated to achieve flow arrest and prevent thrombus dislodgement and distal embolization during removal of the stent retriever (Figure 1 A, B).9,10
Figure 1.
Illustration of standard mechanical thrombectomy techniques. Stent retriever alone: Stent-retriever deployed at the site of the thrombus (A) and retrieval of stent-retriever and thrombus within the guide catheter (B). Contact aspiration: Placement of aspiration catheter at the proximal tip of the thrombus (C), aspiration initiated (D) and retrieval of both aspiration catheter and thrombus inside the guide catheter (E). Combined stent retriever and aspiration: Deployment of stent-retriever at the site of thrombus and initiation of aspiration through the aspiration catheter (F) followed by retrieval of stent-retriever, thrombus and aspiration catheter as a unit through the guide catheter (G).
Contact aspiration
A microwire and microcatheter are advanced inside an intermediate aspiration catheter and navigated distally up to or past the occlusion. The aspiration catheter is then advanced over the microcatheter to the proximal aspect of a thrombus. The aspiration pump and the tubing once primed is connected to the hub of the aspiration catheter. Under continuous aspiration, the microcatheter and microwire are then removed as the aspiration catheter is further advanced to ensure engagement of the thrombus confirmed by cessation of flow in the aspiration system. The aspiration catheter is then slowly retracted back into the guide catheter. Contact aspiration when used as the first pass treatment approach in thrombectomy, is frequently referred to as the A Direct Aspiration First Pass Technique (ADAPT) (Figure 1 C, D, E). 11
Sofia Non-wire advancement technike (SNAKE)
In this technique, the Soft torqueable catheter Optimized For Intracranial Access (Sofia) (MicroVention, Tustin, CA, USA) is used as the intermediate catheter and advanced under roadmap guidance with no additional equipment such as a guidewire or a microwire and microcatheter combination within its lumen. This technique of intermediate catheter advancement under roadmap guidance may be used to perform thrombectomy by contact aspiration or in other combined aspiration and stent retriever techniques described below. 12
Combined aspiration and stent retriever (CASPER)
A microwire and microcatheter are advanced via an intermediate aspiration catheter to cross the arterial occlusion. The microwire is removed and a microcatheter injection is performed to ensure that microcatheter tip is distal to the thrombus. A stent retriever is deployed across the thrombus and the aspiration catheter is advanced to face the proximal end of the thrombus. Under continuous suction through the aspiration catheter, the stent retriever is retracted into the aspiration catheter and the aspiration catheter is withdrawn into the guide catheter. In this technique, the microcatheter can be carefully removed to increase the aspiration force within the aspiration catheter. Also, because the aspiration catheter is essentially clogged by the clot itself, there is no active aspiration, which raises the concern of not being able to control clot fragments (Figure 1 F, G). 13
Advancing the distal aspiration catheter over the stent retriever (ADVANCE)
Microwire and microcatheter are navigated distally and placed in the MCA distal to the thrombus. After ensuring that the tip of the microcatheter is positioned distal to the thrombus, a stent retriever is deployed and five minutes are allowed for thrombus integration. Unlike in other techniques, instead of pulling back the thrombus towards the aspiration catheter or advancing the catheter only to the face of the thrombus, the large bore distal aspiration catheter is advanced and passed beyond the thrombus and over the stent retriever under manual negative suction with a 50 cc locked syringe. After the aspiration catheter reaches the distal tip of the stent retriever the stent retriever is gently withdrawn with continuous negative suction. The negative suction is continued through the aspiration catheter while slowly withdrawing it to a proximal position. At least 20 ml of blood is withdrawn until no thrombus is seen. If a blockage in blood flow is noted, the aspiration catheter is totally removed under continuous suction. 14 Advancing the aspiration catheter distally over the thrombus and stent retriever presumably causes detachment of the thrombus from the arterial wall, while passing between the stent and arterial wall and local aspiration at the thrombus site possibly promotes entrapment of the thrombus.
Continuous aspiration prior to intracranial vascular embolectomy (CAPTIVE)
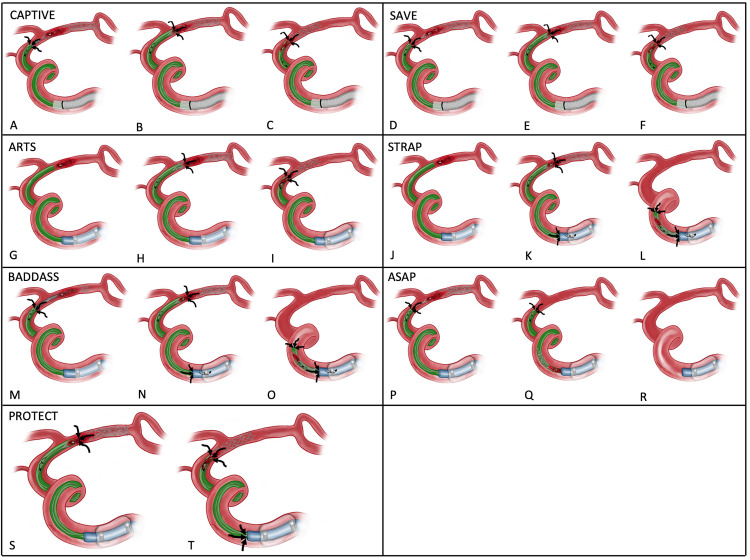
The microcatheter is advanced across the occlusion over a microwire. The local aspiration catheter is connected to a continuous aspiration pump. Aspiration starts before deploying the stent retriever to prevent dispersion of emboli during stent deployment. Stent retriever is deployed and aspiration catheter is then advanced over the stent retriever just far enough to be adjacent to the thrombus. The degree of flow return in the aspiration tubing is monitored and when rate decreases or stops, indicating the clot is engaged, the aspiration catheter is no longer advanced over the stent retriever and the microcatheter is removed to increase the aspiration force of the aspiration catheter. Next, the thrombus is retrieved by withdrawing the aspiration catheter and stent retriever as a single unit back into the guide catheter (Figure 2 A, B, C). 15
Figure 2.
CAPTIVE: continuous aspiration prior To intracranial vascular embolectomy. Deployment of stent-retriever under aspiration from catheter proximal to the thrombus (A), removal of microcatheter and advancement of aspiration catheter (B) and removal of stent-retriever, aspiration catheter and thrombus as a unit (C). SAVE: Stent-retriever Assisted Vacuum-locked Extraction technique. Deployment of stent-retriever, removal of the microcatheter and initiation of aspiration (D), advancement of the aspiration catheter to the proximal tip of the thrombus (E) and removal of stent-retriever, aspiration catheter and the thrombus as a unit under aspiration suction (F). ARTS: Aspiration-Retriever Technique for Stroke: Placement of an aspiration catheter proximally to thrombus (G), deployment of stent-retriever under constant aspiration (H), inflation of BGC and retrieval of the stent-retriever, the thrombus and the aspiration catheter as a unit through the BGC (I). STRAP: Stent Retrieval - Aspiration and Proximal Flow Arrest Placement of an aspiration catheter proximally to the thrombus (J), deployment of a stent-retriever and initiation of aspiration from aspiration catheter and BGC (K), followed by retrieval under constant suction (L). BADDASS: Balloon Guide with Large Bore Distal Access Catheter with Dual Aspiration with Stent-retriever as Standard. Partial deployment of stent-retriever with or without aspiration catheter on (M), advancement of aspiration catheter to proximal portion of thrombus, full deployment of the stent-retriever and removal of microcatheter (N), inflation of BGC and thrombus retrieval under constant suction from distal catheter and BGC (O). ASAP: A Stent-Retrieving into an Aspiration Catheter with Proximal Balloon Technique. Deployment of stent-retriever at the site of the thrombus while the aspiration catheter is under suction and BGC is inflated (P), the stent-retriever is the retrieved inside the aspiration catheter (Q) followed by removal of the aspiration catheter under continuous suction (R). PROTECT: Proximal Balloon Occlusion Together with Direct Thrombus Aspiration. Deployment of a stent-retriever at the site of the thrombus while suction is applied through the aspiration catheter and manual suction is done through the inflated BGC (S) followed by retrieval under constant suction through the aspiration catheter and through the BGC (T).
Stent-retriever assisted vacuum-locked extraction technique (SAVE)
The microwire and microcatheter are advanced past the thrombus. After removing the microwire, a stent retriever is advanced in the microcatheter and deployed using the active push deployment technique, 16 with only a third of the proximal portion interacting with the thrombus. After removal of the microcatheter, the aspiration catheter is connected to a pump for permanent aspiration, then advanced towards the thrombus while also gently retracting the stent retriever until there is no flow in the aspiration catheter and the thrombus is wedged. The permanent suction is then transferred to the guide catheter, while negative pressure is maintained in the aspiration catheter with a 60 ml vacuum pressure syringe. Both the stent retriever and the aspiration catheter are then removed slowly as a single unit into the guide catheter. The pump aspiration from the guide catheter is continued for additional 30 seconds after removal of the stent retriever/aspiration catheter unit (Figure 2 D, E, F). 17
Aspiration-Retriever technique for stroke (ARTS)
In this technique, the aspiration catheter is positioned immediately proximal to the site of occlusion. A stent retriever device is then placed across the thrombus and allowed to intercalate within the clot. The microcatheter is then removed. If being used, the BGC is inflated, and then the aspiration catheter is activated. The stent retriever is slowly retracted until resistance is felt. Then the aspiration catheter and stent retriever are both removed as a single unit through the guide catheter. Although this technique is frequently described with the use of a BGC, this only results in flow arrest within the ICA, while more distal areas may still experience retrograde or anterograde flow and can result in fragments of the clot being embolized distally (Figure 2 G, H, I). 18
Guide sheath advancement and aspiration in the distal petrocavernous ICA (GUARD)
In this technique, the guide sheath is initially placed in the cervical ICA as in a standard thrombectomy procedure. The stent retriever is deployed using a microcatheter with 50% of the stent construct distal to the thrombus. This is followed by immediate advancement of distal aspiration catheter under continuous aspiration to the proximal aspect of the thrombus, until flow arrest and engagement with thrombus and stent retriever. The delivery microcatheter is then withdrawn to maximize the aspiration force. The guide sheath is then advanced distally across the skull base in the horizontal petrous to cavernous segment of the ICA over the large-bore aspiration catheter. After 5 min allowing for thrombus integration with the stent retriever, the combined stent retriever-distal aspiration catheter unit is withdrawn under continuous aspiration, while manual aspiration is applied through the guide sheath in the distal ICA. 19 It is presumed that advancing the guide sheath over a large bore aspiration catheter further distally in the ICA could reduce antegrade flow and decrease the clot-retrieval distance allowing more efficient and complete reperfusion.
Stent retrieval - aspiration and proximal flow arrest (STRAP)
A BGC is positioned in the cervical ICA, and a microwire and microcatheter are passed across the thrombus. An aspiration catheter is then advanced to the proximal aspect of the thrombus followed by the deployment of a stent retriever across the occlusion. The balloon is inflated to achieve flow arrest, and the thrombus is wedged between the stent retriever and aspiration catheter. Continuous suction is applied to both the BGC and aspiration catheter. The stent retriever, aspiration catheter and thrombus complex are then all removed as a unit into the guide catheter (Figure 2 J, K, L). 10
Balloon guide with large bore distal access catheter with dual aspiration with stent-retriever as standard (BADDASS)
BGC is delivered to the distal cervical ICA segment. A microcatheter is advanced beyond the thrombus and the microwire is later removed. Stent retriever is then delivered to the tip of the microcatheter and before deploying the stent retriever, the distal aspiration catheter is advanced as far distally as possible but not too close to the thrombus. Aspiration can begin prior to or after deploying the stent retriever depending on the operator's preference. Once a third of the stent retriever has been deployed by unsheathing the microcatheter, the aspiration catheter can be advanced to the proximal portion of the clot, and the stent retriever deployed using active push deployment. The microcatheter is then removed. The BGC is then inflated for flow arrest, and the stent retriever/aspiration catheter/thrombus complex is removed as a unit, with aspiration both from the large bore distal access catheter and the BGC (Figure 2 M, N, O). 20
A stent-retrieving into an aspiration catheter with proximal balloon technique (ASAP)
A stent delivery microcatheter is advanced through an aspiration catheter to the point of occlusion. A proximal balloon is inflated, and the thrombus is crossed under continuous aspiration from the distal aspiration catheter to prevent distal embolization. Simultaneous angiography from both the BGC and the microcatheter is performed. A stent retriever is then deployed via the delivery microcatheter and the microcatheter is then removed using stent retriever as an anchor. The aspiration catheter is then placed immediately proximal to the stent retriever. The stent retriever is withdrawn under continuous aspiration into the aspiration catheter which remains in its initial position. The aspiration catheter is then removed under constant aspiration and proximal flow arrest In cases where the aspiration catheter is clogged, manual suction was used on the BGC (Figure 2 P, Q, R). 21
Proximal balloon occlusion together with direct thrombus aspiration (PROTECT)
A BGC is placed in the cervical ICA and the aspiration catheter is advanced over the microcatheter and microwire distally to the thrombus. The microcatheter is passed across the thrombus over the microwire. The balloon is then inflated and the stent retriever is deployed across the thrombus and continuous suction is applied to the aspiration catheter. The microcatheter is then removed. The aspiration catheter/stent retriever/thrombus complex is removed into the BGC that provides flow arrest 22 This technique when performed with both proximal flow arrest and aspiration from the BGC it is referred to PROTECTPLUS technique. 23 This technique aims at reducing thrombus fragmentation and distal embolization with both proximal balloon occlusion and contact aspiration at the thrombus (Figure 2 S, T).
Discussion
First-generation devices used in mechanical thrombectomy for stroke included snare catheters that interdigitated with the thrombus before extraction, microcatheters with a laser at the tip causing clot emulsification by photo energy, and ultrasound devices creating microfractures of thrombus for better integration of the thrombolytic agents. 24 Efficacy of these early devices was not systematically studied; however, the devices demonstrated that percutaneous thrombectomy to treat AIS was feasible. Later, the clot retrieval devices such as the mechanical embolus removal in cerebral ischemia (MERCI) and the Penumbra System for aspiration were introduced.25,26 Initial thrombectomy trials using these devices showed improved recanalization of the vessels; however, recanalization was not associated with improved clinical outcomes. 27 However, the newer generation stent retriever devices used in the landmark clinical trials of mechanical thrombectomy were proven as both safe and effective.28,29
Evidence-based guidelines have been established for mechanical thrombectomy 30 and several different devices are available and approved for thrombectomy (Table 1). Apart from the stent retrievers and aspiration catheters, BGCs are also fundamental in a thrombectomy technique. BGCs are primarily used to achieve anterograde flow arrest in the ICA and prevent distal embolism when retrieving the blood clot. Use of BGCs is associated with better procedural and patient outcomes.9,31 Of all reported techniques and variations, a BGC is used in SRBG, ARTS, STRAP, BADDASS, ASAP, PROTECT and PROTECTPLUS. Currently available BGCs for thrombectomy include products such as the FlowGate 2 TM (Stryker, Fremont, CA, USA), CelloTM (Medtronic, Irvine, CA, USA), Optimo (Tokai Medical Products, Tokyo, Japan), Walrus (Q’Apel Medical, Fremont, CA, USA), etc.
In techniques employing aspiration, an intermediate catheter is connected to a pump for continuous aspiration or a 60 cc syringe is used to provide the negative suction. Aspiration from both the intermediate or distal large bore catheter and the guide catheter is performed in the SAVE, STRAP, BADDASS, and PROTECTPLUS techniques. The size of an aspiration catheter has implications in a thrombectomy procedure. Discrepancy between aspiration catheters with smaller diameters and the diameter of ICA or MCA which usually range from 2.5–5 mm carries risk of thrombus fragmentation or partial entrapment of the aspirated clot between the aspiration catheter outer surface and the vessel wall. This may subsequently lead to re-occlusion of the vessel or embolization to a new territory. The new generation of aspiration catheters have a larger bore allowing more robust aspiration of the clot. Aspiration catheters have a relatively soft and maneuverable distal segment and these characteristics are particularly utilized in the SNAKE technique. The SNAKE technique although frequently used, it is not specific to thrombectomy and can be used in other neuroendovascular procedures. 12 Additionally, a novel aspiration technology not only provides standard continuous suction but also cyclical, pulsatile, or intermittent suction. This varying pressure cyclical aspiration system (CLEAR aspiration system) provided more aspiration force and clot clearance. 32 Compared to standard continuous aspiration, a significantly higher first-pass effect for LVO strokes was reported with the cyclical aspiration system. 33
We reviewed techniques ranging from a minimalist approach to thrombectomy involving only contact aspiration using a large bore catheter to a maximalist approach involving use of stent retriever, distal aspiration combined with proximal aspiration and flow arrest using a BGC. Some techniques aim at engulfing the clot into the aspiration catheter while others aim at trapping it between the stent retriever and the aspiration catheter. In most techniques, a large bore aspiration catheter is advanced to the face of the thrombus, but in the AVDANCE technique the catheter is passed distally over the thrombus and the stent retriever under aspiration. Systematic study comparing different thrombectomy techniques remains limited. Current randomized clinical trial data indicates no significant difference in successful recanalization or functional outcome between stent retrievers and aspiration as first line technique.34–36 Reported rates of successful reperfusion (TICI ≥ 2b) reach 100% with techniques such as CAPTIVE and SAVE. Reperfusion rates of other techniques are as follows: STRAP 92%, ADAPT 91%, SRBG 83.6%. ADVANCE 87%, GUARD 98%, ARTS 97.6%, and ASAP 95.2%. To be noted is that reperfusion rates are from studies describing the individual technique and mostly based on single center experiences.
Recently, first pass effect (FPE) has been proposed as a measure for evaluating tools and techniques in thrombectomy. 37 In a thrombectomy procedure, ‘pass’ is referred to as the attempt of clot retrieval either with aspiration using a large bore catheter at the thrombus or deployment and withdrawal of a stent retriever. Complete recanalization with a single thrombectomy device pass is referred to as FPE. 37 Hafeez et al. 10 found no difference in first-pass efficacy (FPE) between combined stent retriever and distal aspiration, ADAPT, SRBG and STRAP techniques. However, among the four evaluated techniques, only STRAP predicted successful reperfusion. In another study, addition of distal aspiration catheters to BGC and SR thrombectomy did not result in higher rates of FPE or improved clinical outcomes. 38 In refractory occlusions of large vessels, a novel double-stent retriever technique has also been proposed. In this approach, standard stent retriever-based thrombectomy techniques are used, however, a second stent retriever is deployed either within or in parallel to the first stent and thrombectomy performed to retrieve the refractory clots. 39
In posterior circulation thrombectomy involving basilar artery occlusion, ADAPT was shown to achieve a higher rate of complete reperfusion and shorter procedure duration when compared with stent retrievers. 40 In patients with CT evidence of a hyperdense vessel sign, FPE was better noted with use of stent retrievers than aspiration for thrombectomy. 41 Furthermore, novel stent retrievers specifically designed for removal of fibrin-rich clots is also reported. 42 This may imply that certain patient factors and thrombus characteristics may guide selection of a thrombectomy technique. Nevertheless, there are no large studies that affirmatively conclude which, if any, technique leads to the best clinical outcomes.
The objective of using the different combination of aspiration catheters and stent retrievers is to achieve the best reperfusion grade possible in the least amount of time while having the lowest risk of procedural complications. The role of different devices and techniques individually or in combination on patient clinical and safety outcomes, is yet to be determined. In this review, descriptions and illustrations are limited to thrombectomy techniques referable to LVOs of the anterior circulation but same techniques could be employed for posterior circulation. Only the primary thrombectomy devices and techniques are reported here and infrequently used, additional methods such as intraarterial thrombolysis or microwire manipulation techniques were not reviewed. Ongoing studies such as the ASSIST registry may provide information on procedural success and clinical outcomes of various thrombectomy techniques. 43 A deeper understanding of the tools and techniques used in mechanical thrombectomy and insight into many different factors influencing fast and complete flow restoration is fundamental in the treatment of AIS, and continues to remain the focus of future research endeavors in the field of neuroendovascular surgery.
Compliance with Ethical Standards
Author Alfredo Munoz declares that he has no conflict of interest.
Author Roland Jabre declares that he has no conflict of interest
Author Jose M Orenday-Barraza declares that he has no conflict of interest
Author Mohamed Shehab Eldin declares that he has no conflict of interest
Author Ching-Jen Chen declares that he has no conflict of interest
Author Fadi Al-Saiegh declares that he has no conflict of interest
Author Rawad Abbas declares that he has no conflict of interest
Author Kareem E Naamani declares that he has no conflict of interest
Author Michael Reid Gooch declares he is a consultant for Stryker.
Author Pascal M Jabbour declares he is a consultant to Medtronic and Microvention.
Author Stavropoula Tjoumakaris declares that she has no conflict of interest
Author Robert H Rosenwasser declares that he has no conflict of interest
Author Nabeel A Herial declares he received speaker honorarium from Penumbra and Medtronic.
Footnotes
Ethical approval: This article does not contain any studies with human participants performed by any of the authors.
Informed consent: Not applicable for this research.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Alfredo Munoz https://orcid.org/0000-0002-6209-4685
References
- 1.Krishnamurthi RV, Ikeda T, Feigin VL. Global, regional and country-specific burden of ischaemic stroke, intracerebral haemorrhage and subarachnoid haemorrhage: a systematic analysis of the global burden of disease study 2017. Neuroepidemiology 2020; 54: 171–179. 2020/02/23. DOI: 10.1159/000506396. [DOI] [PubMed] [Google Scholar]
- 2.National Institute of Neurological D and Stroke rt PASSG. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med 1995; 333: 1581–1587. 1995/12/14. DOI: 10.1056/NEJM199512143332401. [DOI] [PubMed] [Google Scholar]
- 3.group ISTc, Sandercock P, Wardlaw JM, et al. The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischaemic stroke (the third international stroke trial [IST-3]): a randomised controlled trial. Lancet (London, England) 2012; 379: 2352–2363. 2012/05/29. DOI: 10.1016/S0140-6736(12)60768-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Berkhemer OA, Fransen PS, Beumer D, et al. A randomized trial of intraarterial treatment for acute ischemic stroke. N Engl J Med 2015; 372: 11–20. 2014/12/18. DOI: 10.1056/NEJMoa1411587. [DOI] [PubMed] [Google Scholar]
- 5.Campbell BC, Mitchell PJ, Kleinig TJ, et al. Endovascular therapy for ischemic stroke with perfusion-imaging selection. N Engl J Med 2015; 372: 1009–1018. 2015/02/12. DOI: 10.1056/NEJMoa1414792. [DOI] [PubMed] [Google Scholar]
- 6.Goyal M, Demchuk AM, Menon BK, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med 2015; 372: 1019–1030. 2015/02/12. DOI: 10.1056/NEJMoa1414905. [DOI] [PubMed] [Google Scholar]
- 7.Jovin TG, Chamorro A, Cobo E, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med 2015; 372: 2296–2306. 2015/04/18. DOI: 10.1056/NEJMoa1503780. [DOI] [PubMed] [Google Scholar]
- 8.Saver JL, Goyal M, Bonafe A, et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N Engl J Med 2015; 372: 2285–2295. 2015/04/18. DOI: 10.1056/NEJMoa1415061. [DOI] [PubMed] [Google Scholar]
- 9.Nguyen TN, Malisch T, Castonguay AC, et al. Balloon guide catheter improves revascularization and clinical outcomes with the solitaire device: analysis of the North American solitaire acute stroke registry. Stroke 2014; 45: 141–145. 2013/12/05. DOI: 10.1161/STROKEAHA.113.002407. [DOI] [PubMed] [Google Scholar]
- 10.Hafeez MU, Kan P, Srivatsan A, et al. Comparison of first-pass efficacy Among four mechanical thrombectomy techniques: a single-center experience. World Neurosurg 2020; 144: e533–e540. 2020/09/07. DOI: 10.1016/j.wneu.2020.08.209. [DOI] [PubMed] [Google Scholar]
- 11.Turk AS, Spiotta A, Frei D, et al. Initial clinical experience with the ADAPT technique: a direct aspiration first pass technique for stroke thrombectomy. J Neurointerv Surg 2014; 6: 231–237. 2013/04/30. DOI: 10.1136/neurintsurg-2013-010713. [DOI] [PubMed] [Google Scholar]
- 12.Heit JJ, Wong JH, Mofaff AM, et al. Sofia Intermediate catheter and the SNAKE technique: safety and efficacy of the Sofia catheter without guidewire or microcatheter construct. J Neurointerv Surg 2018; 10: 401–406. 2017/08/05. DOI: 10.1136/neurintsurg-2017-013256. [DOI] [PubMed] [Google Scholar]
- 13.Humphries W, Hoit D, Doss VT, et al. Distal aspiration with retrievable stent assisted thrombectomy for the treatment of acute ischemic stroke. J Neurointerv Surg 2015; 7: 90–94. 2014/01/28. DOI: 10.1136/neurintsurg-2013-010986. [DOI] [PubMed] [Google Scholar]
- 14.Gurkas E, Akpinar CK, Aytac E. ADVANCE: an effective and feasible technique in acute stroke treatment. Interv Neuroradiol 2017; 23: 166–172. 2017/03/18. DOI: 10.1177/1591019916682358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McTaggart RA, Tung EL, Yaghi S, et al. Continuous aspiration prior to intracranial vascular embolectomy (CAPTIVE): a technique which improves outcomes. J Neurointerv Surg 2017; 9: 1154–1159. 2016/12/18. DOI: 10.1136/neurintsurg-2016-012838. [DOI] [PubMed] [Google Scholar]
- 16.Wiesmann M, Brockmann MA, Heringer S, et al. Active push deployment technique improves stent/vessel-wall interaction in endovascular treatment of acute stroke with stent retrievers. J Neurointerv Surg 2017; 9: 253–256. 2016/03/16. DOI: 10.1136/neurintsurg-2016-012322. [DOI] [PubMed] [Google Scholar]
- 17.Maus V, Behme D, Kabbasch C, et al. Maximizing first-pass complete reperfusion with SAVE. Clin Neuroradiol 2018; 28: 327–338. 2017/02/15. DOI: 10.1007/s00062-017-0566-z. [DOI] [PubMed] [Google Scholar]
- 18.Massari F, Henninger N, Lozano JD, et al. ARTS (Aspiration-Retriever technique for stroke): initial clinical experience. Interv Neuroradiol 2016; 22: 325–332. 2016/02/26. DOI: 10.1177/1591019916632369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ansari SA, Darwish M, Abdalla RN, et al. GUide sheath advancement and aspiRation in the distal petrocavernous internal carotid artery (GUARD) technique during thrombectomy improves reperfusion and clinical outcomes. AJNR Am J Neuroradiol 2019; 40: 1356–1362. 2019/07/28. DOI: 10.3174/ajnr.A6132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ospel JM, Volny O, Jayaraman M, et al. Optimizing fast first pass complete reperfusion in acute ischemic stroke - the BADDASS approach (BAlloon guiDe with large bore distal access catheter with dual aspiration with stent-retriever as standard approach). Expert Rev Med Devices 2019; 16: 955–963. 2019/10/28. DOI: 10.1080/17434440.2019.1684263. [DOI] [PubMed] [Google Scholar]
- 21.Goto S, Ohshima T, Ishikawa K, et al. A stent-retrieving into an aspiration catheter with proximal balloon (ASAP) technique: a technique of mechanical thrombectomy. World Neurosurg 2018; 109: e468–e475. 2017/10/19. DOI: 10.1016/j.wneu.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 22.Maegerlein C, Monch S, Boeckh-Behrens T, et al. PROTECT: PRoximal balloon occlusion TogEther with direCt thrombus aspiration during stent retriever thrombectomy - evaluation of a double embolic protection approach in endovascular stroke treatment. J Neurointerv Surg 2018; 10: 751–755. 2017/12/10. DOI: 10.1136/neurintsurg-2017-013558. [DOI] [PubMed] [Google Scholar]
- 23.Maegerlein C, Berndt MT, Monch S, et al. Further development of combined techniques using stent retrievers, aspiration catheters and BGC: the PROTECT(PLUS) technique. Clin Neuroradiol 2020; 30: 59–65. 2018/11/11. DOI: 10.1007/s00062-018-0742-9. [DOI] [PubMed] [Google Scholar]
- 24.Stead LG, Gilmore RM, Bellolio MF, et al. Percutaneous clot removal devices in acute ischemic stroke: a systematic review and meta-analysis. Arch Neurol 2008; 65: 1024–1030. 2008/08/13. DOI: 10.1001/archneur.65.8.1024. [DOI] [PubMed] [Google Scholar]
- 25.Bose A, Henkes H, Alfke K, et al. The penumbra system: a mechanical device for the treatment of acute stroke due to thromboembolism. AJNR Am J Neuroradiol 2008; 29: 1409–1413. 2008/05/24. DOI: 10.3174/ajnr.A1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Smith WS, Sung G, Starkman S, et al. Safety and efficacy of mechanical embolectomy in acute ischemic stroke: results of the MERCI trial. Stroke 2005; 36: 1432–1438. 2005/06/18. DOI: 10.1161/01.STR.0000171066.25248.1d. [DOI] [PubMed] [Google Scholar]
- 27.Broderick JP, Palesch YY, Demchuk AM, et al. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med 2013; 368: 893–903. 2013/02/09. DOI: 10.1056/NEJMoa1214300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nogueira RG, Lutsep HL, Gupta R, et al. Trevo versus merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet (London, England) 2012; 380: 1231–1240. 2012/08/31. DOI: 10.1016/S0140-6736(12)61299-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Saver JL, Jahan R, Levy EI, et al. Solitaire flow restoration device versus the merci retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet (London, England) 2012; 380: 1241–1249. 2012/08/31. DOI: 10.1016/S0140-6736(12)61384-1. [DOI] [PubMed] [Google Scholar]
- 30.Powers WJ, Rabinstein AA, Ackerson T, et al. Guidelines for the early management of patients With acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals From the American heart association/American stroke association. Stroke 2019; 50: e344–e418. 2019/10/31. DOI: 10.1161/STR.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 31.Lee DH, Sung JH, Kim SU, et al. Effective use of balloon guide catheters in reducing incidence of mechanical thrombectomy related distal embolization. Acta Neurochir (Wien) 2017; 159: 1671–1677. 2017/07/12. DOI: 10.1007/s00701-017-3256-3. [DOI] [PubMed] [Google Scholar]
- 32.Simon S, Grey CP, Massenzo T, et al. Exploring the efficacy of cyclic vs static aspiration in a cerebral thrombectomy model: an initial proof of concept study. J Neurointerv Surg 2014; 6: 677–683. 2013/11/16. DOI: 10.1136/neurintsurg-2013-010941. [DOI] [PubMed] [Google Scholar]
- 33.Kalousek V, Yoo AJ, Sheth SA, et al. Cyclical aspiration using a novel mechanical thrombectomy device is associated with a high TICI 3 first pass effect in large-vessel strokes. J Neuroimaging 2021; 31: 912–924. 2021/06/09. DOI: 10.1111/jon.12889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Turk AS , 3rd, Siddiqui A, Fifi JT, et al. Aspiration thrombectomy versus stent retriever thrombectomy as first-line approach for large vessel occlusion (COMPASS): a multicentre, randomised, open label, blinded outcome, non-inferiority trial. Lancet (London, England) 2019; 393: 998–1008. 2019/03/13. DOI: 10.1016/S0140-6736(19)30297-1. [DOI] [PubMed] [Google Scholar]
- 35.Lapergue B, Blanc R, Gory B, et al. Effect of endovascular contact aspiration vs stent retriever on revascularization in patients With acute ischemic stroke and large vessel occlusion: the ASTER randomized clinical trial. JAMA 2017; 318: 443–452. 2017/08/02. DOI: 10.1001/jama.2017.9644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lapergue B, Blanc R, Costalat V, et al. Effect of thrombectomy With combined contact aspiration and stent retriever vs stent retriever alone on revascularization in patients With acute ischemic stroke and large vessel occlusion: the ASTER2 randomized clinical trial. JAMA 2021; 326: 1158–1169. 2021/09/29. DOI: 10.1001/jama.2021.13827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zaidat OO, Castonguay AC, Linfante I, et al. First pass effect: a New measure for stroke thrombectomy devices. Stroke 2018; 49: 660–666. 2018/02/21. DOI: 10.1161/STROKEAHA.117.020315. [DOI] [PubMed] [Google Scholar]
- 38.Blasco J, Puig J, Lopez-Rueda A, et al. Addition of intracranial aspiration to balloon guide catheter does not improve outcomes in large vessel occlusion anterior circulation stent retriever based thrombectomy for acute stroke. J Neurointerv Surg 2021. 2021/08/29. DOI: 10.1136/neurintsurg-2021-017760. [DOI] [PubMed] [Google Scholar]
- 39.Imahori T, Miura S, Sugihara M, et al. Double stent retriever (SR) technique: a novel mechanical thrombectomy technique to facilitate the device-clot interaction for refractory acute cerebral large vessel occlusions. World Neurosurg 2020; 141: 175–183. 2020/06/12. DOI: 10.1016/j.wneu.2020.05.268. [DOI] [PubMed] [Google Scholar]
- 40.Gory B, Mazighi M, Blanc R, et al. Mechanical thrombectomy in basilar artery occlusion: influence of reperfusion on clinical outcome and impact of the first-line strategy (ADAPT vs stent retriever). J Neurosurg 2018; 129: 1482–1491. 2018/01/13. DOI: 10.3171/2017.7.JNS171043. [DOI] [PubMed] [Google Scholar]
- 41.Mohammaden MH, Haussen DC, Perry da Camara C, et al. Hyperdense vessel sign as a potential guide for the choice of stent retriever versus contact aspiration as first-line thrombectomy strategy. J Neurointerv Surg 2021; 13: 599–604. 2020/08/02. DOI: 10.1136/neurintsurg-2020-016005. [DOI] [PubMed] [Google Scholar]
- 42.Fennell VS, Setlur Nagesh SV, Meess KM, et al. What to do about fibrin rich ‘tough clots’? Comparing the solitaire stent retriever with a novel geometric clot extractor in an in vitro stroke model. J Neurointerv Surg 2018; 10: 907–910. 2018/01/21. DOI: 10.1136/neurintsurg-2017-013507. [DOI] [PubMed] [Google Scholar]
- 43.ASSIST Registry to Assess the Procedural Success and Clinical Outcomes Associated With Various Operator Techniques for Mechanical Thrombectomy in Large Vessel Occlusions (LVO). ClinicalTrials.gov identifier: NCT03845491. Website: https://clinicaltrials.gov/ct2/show/NCT03845491. Date Accessed: 02/04/2022.