Abstract
Background:
Long-term follow-up for clinician–scientist training programs is sparse. We describe the outcomes of clinician–scientist scholars in the National Heart Lung and Blood Institute (NHLBI) K12 program in emergency care research up to 8.7 years after matriculation in the program.
Methods:
This was a cohort study of faculty clinician–scientist scholars enrolled in a NHLBI K12 research training program at 6 sites across the US, with median follow-up 7.7 years (range 5.7–8.7 years) from the date of matriculation. Scholars completed electronic surveys in 2017 and 2019, with the 2019 survey collecting information for their current work setting, percent time for research, and grant funding from all sources. We used NIH RePorter and online resources to verify federal grants through March 2021. The primary outcome was a funded career development award (CDA) or research project grant (RPG) where the scholar was principal investigator. We included funding from all federal sources and national foundations.
Results:
There were 43 scholars, including 16 (37%) women. Over the follow-up period, 32 (74%) received an individual CDA or RPG, with a median of 36 months (range 9–83 months) after entering the program. Of the 43 scholars, 23 (54%) received a CDA and 22 (51%) received an RPG, 7 (16%) of which were R01s. Of the 23 scholars who received a CDA, 13 (56%) subsequently had an RPG funded. Time to CDA or RPG did not differ by sex (women vs. men log-rank test p = 0.27) or specialty training (emergency medicine versus other specialties, p = 0.59).
Conclusions:
After 7 years of follow-up for this NHLBI K12 emergency care research training program, three quarters of clinician–scientist scholars had obtained CDA or RPG funding, with no notable differences by sex or clinical training.
INTRODUCTION
A 2014 Physician-Scientist Workforce Report from the National Institutes of Health (NIH) showed that the proportion of physician-scientists comprising the biomedical workforce has been declining since the 1970’s.1 The same report noted 13,700 active physician-scientists in the US, just over 1% of all American physicians.1 There have been a number of articles detailing the virtues of physician-scientists in the biomedical workforce, recommendations for increasing the pipeline, methods to decrease attrition, and unique threats to physician-scientists during the COVID-19 pandemic.2-5 These issues are particularly poignant for emergency care research, which has historically received a relatively small proportion of NIH research funding6 and has lacked a robust research workforce to translate clinical questions into high-quality and actionable research protocols.7,8
In recognition of the decline in the physician-scientist workforce, the NIH launched two career development programs targeting clinician-scientists in the 1990’s (i.e., the K08 and K23 individual mentored career development programs). The NIH also uses the K12 Clinical Scientist Institutional Career Development program as another mechanism for research training within distinct fields. Under the K12 mechanism, institutions (rather than individuals) are awarded based on the training environment, with potential scholars applying to the institutions (rather than directly to the NIH) for consideration. The K12 mechanism is often targeted by an institute for areas or specialties needing a catalyst to expand the scientific workforce. The success of these institutional awards, as evidenced by the success of individual clinician-scientists selected for the programs, are typically measured by the proportion of scholars subsequently obtaining an individual career development award (CDA) or a research project grant (RPG).9 There are limited studies tracking outcomes for K12 programs because such analyses typically require many years of follow-up. In 2018, we reported short-term scholar outcomes from the National Heart, Lung, and Blood Institute (NHLBI) K12 career development program in emergency care research.10 The NHLBI K12 program was the first large federal investment in emergency care research training, representing a $21.6 million investment in six sites across the US.11 In that report, we showed that 60% of scholars had secured independent CDA or RPG funding within 3 to 5 years of starting the K12 program,10 yet not all scholars had finished the program by the end of the follow-up period. Because successfully competing for research funding can take many years, particularly for RPG awards, longer duration follow-up would provide a better assessment of the impact of the K12 program.
In this study, we describe the outcomes of scholars from the NHLBI K12 in emergency care research up to 8.7 years after matriculation into the program, including continued participation in research, a comprehensive assessment of subsequent independent grant funding, and time to funding.
METHODS
Study design
We conducted a prospective cohort study of scholars in the NHLBI K12 program in emergency care research using a participant survey, updated scholar curriculum vitaes (CVs), publicly available databases and on-line resources for subsequent grant funding. Each participant provided consent for inclusion and the Oregon Health & Science University institutional review board approved the study.
Setting
The six sites funded in 2011 for the NHLBI K12 Program in Emergency Care Research11 included: Icahn School of Medicine at Mount Sinai (New York, NY); Oregon Health & Science University (Portland, OR); University of California, Davis School of Medicine (Sacramento, CA); University of Pennsylvania (Philadelphia, PA); University of Pittsburgh (Pittsburgh, PA); and Vanderbilt University Medical Center (Nashville, TN). While there was a separate, distinct 5-year trans-NIH K12 program starting in 2016, we report on the initial K12 program in emergency care research11 to provide a longer follow-up period.
Selection of participants
We obtained the names of K12 scholars affiliated with the six program sites throughout the duration of the program. The first scholar entered the program July 1, 2012 and the last scholar finished on November 8, 2017. The K12 program provided up to 3 years of support for each scholar, including salary support, comprehensive mentorship, formal research didactic training, and research expenses and education up to $25,000 annually. Programs guaranteed that each scholar had at least 75% protected time for research. There was also an annual meeting at the NIH for all sites, including K12 scholars, program directors, and program administrators from each site.
Methods of measurement
Scholars completed an initial electronic survey in 2017 and a subsequent survey in 2019 using REDCap®. The initial survey included demographics (age, gender, race, and ethnicity), education, clinical training, primary academic appointment, post-K12 time spent on research, and grant applications submitted as a principal investigator (PI) following entry to the K12 program. These results were supplemented by qualitative data from interviews and reported in the initial evaluation of K12 scholar outcomes.10 Scholars completed a subsequent survey in July 2019, which included two questions (current work setting [academic versus clinical] and percent time for research) and a request to upload an updated CV. We abstracted all funded grants (including their role and funding sources) since the date of matriculation into the K12 program from the CVs. We used NIH RePorter (NIH, AHRQ and VA funding), the PCORI website, Grantome (https://grantome.com/), Google, and websites at the academic programs represented by scholars to verify grants through March 2021.
Outcome measures
To measure scholar productivity, we categorized funded grants with the scholar as PI as CDAs (including K01, K08, K23, VA CDA2, and similar multi-year grants from professional or research foundations) and RPGs9 (including R01, R03, R21, R33, R34, R61, VA Merit awards, and similar multi-year grant awards from professional or research foundations). As a subset of RPGs, we also examined R01 and equivalent awards (e.g., VA Merit awards). We did not consider industry funding for scholars, given the difficulty of differentiating investigator-initiated research from industry-led research. We only considered grants with scholars listed as PI (including multiple-PI grants) to focus on a scholar's achievement of independent research grant funding and the reporting capabilities of NIH RePorter and similar online websites.
Primary data analysis
We used descriptive statistics to characterize the K12 scholars. For each scholar, we identified their first CDA or RPG in relation to the date they started the K12 program, which provided a consistent time zero for all scholars. We calculated the time interval from the date of the K12 appointment to the date of the first CDA and RPG grant and illustrated these intervals using Kaplan–Meier curves. We also compared Kaplan–Meier curves by sex and clinical specialty (emergency medicine versus other specialties) using the log-rank test. We conducted all analyses in Stata 16.1 (StataCorp, College Station, TX, USA) and considered a p value ≤0.05 to represent statistical significance.
RESULTS
The K12 emergency care research training program included 43 clinician-scientists across the 6 sites (Table 1). We obtained follow-up information directly from 41 of 43 (95%) scholars. For the two scholars who did not respond, we confirmed the presence versus absence of research grants through NIH RePorter and publicly-available on-line sources. The median follow-up period was 7.7 years from the date of matriculation into the K12 program (range 5.7–8.7 years). The demographics of scholars are shown in Table 1. The mean age was 37 years, 37% were female, 11% were Black, and 8% were Hispanic. The majority of scholars (25 of 43, 58%) continued to participate in research for at least 50% of their professional time. Eight (19%) scholars reported spending 25–50% time on research, and 5 (12%) reported spending up to 25% time performing research (one scholar reported no research activity and four provided no estimate).
TABLE 1.
Description of cohort
| All participants (N = 43) | |
|---|---|
| Age at matriculation into K12 (Median, IQR) | 37 years (34–40years) |
| Sex | 16 F (37%), 27 M (63%) |
| Race/Ethnicity | |
| White, non-Hispanic | 22 (51%) |
| Asian | 12 (27%) |
| Black | 5 (11%) |
| White, Hispanic | 3 (8%) |
| Other | 1 (3%) |
| Degrees on entry to K12 program: | |
| MD + Master's degree | 30 (70%) |
| MD | 5 (12%) |
| MD, PhD | 4 (9%) |
| PhD | 4 (9%) |
| Professional discipline: | |
| Emergency Medicine | 18 (42%) |
| Pediatric Emergency Medicine | 6 (14%) |
| Adult Critical Care* | 5 (12%) |
| Cardiology | 5 (12%) |
| Pediatric Critical Care | 2 (5%) |
| Trauma Surgery | 2 (5%) |
| Pediatric allergy and immunology | 1 (2%) |
| PhD, nursing | 1 (2%) |
| PhD, epidemiology | 1 (2%) |
| PhD, comparative pathology | 1 (2%) |
| PhD, clinical research, physiology and biophysics | 1 (2%) |
| Median scholars per institution (range) | 7 (6 to 8) |
| Median effort for research at initial assessment | 75% (IQR 30–75%) |
| Median effort for research from current assessment | 75% (IQR 25–75%, range 0–90%) |
One scholar trained in neurology and critical care.
Many of the cohort characteristics were published in the 3–5 year outcome assessment.10
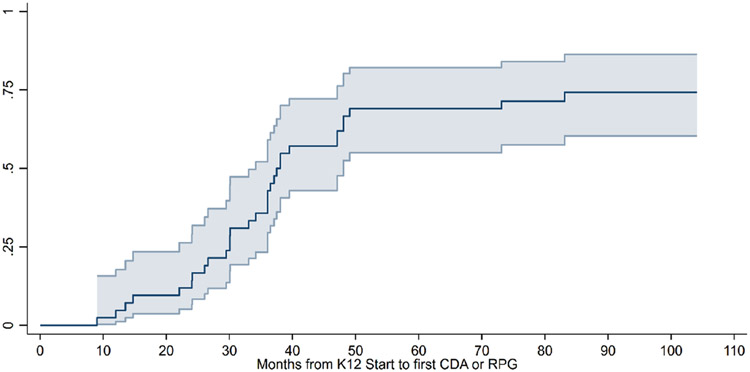
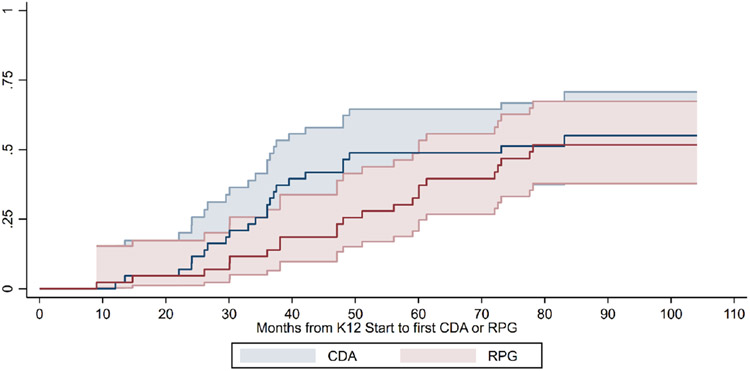
We considered the research grant outcomes (CDA or RPG) of scholars as a measure of successful funding as PI. Of the 43 scholars, 32 (74%) received a CDA or RPG as PI during the follow-up period (Table 2, Figure 1). The time to first CDA or RPG occurred a median 36 months (range 9–83 months) after entering the K12 program. During follow-up of the 43 scholars, 23 (54%) received a CDA and 22 (51%) received an RPG, 7 (16%) of which were R01s (Table 2). Table 3 shows the grant type and funding agencies for CDAs and RPGs. Of the 23 scholars who received a CDA, 13 (56%) subsequently had an RPG funded, which occurred a median of 32 months (inter-quartile range 23 to 44 months) after the award date for the CDA. In contrast, 9 of 20 (45%) scholars who did not receive a CDA obtained RPGs (median 38 months from the start of the K12 program, IQR 30–47 months). Of the 9 scholars who obtained RPGs without a CDA, two of the RPGs were R01 awards. Although the change in rate in Figure 1 begins to plateau at approximately 50 months from entry to the K12 program, there were scholars who continued to receive grant awards after 80 months. In Figure 2, we show Kaplan–Meier curves for time-to-funding, separated by CDA versus RPG grants.
TABLE 2.
Grant outcomes of the K12 cohort (n = 43)
| CDA or RPG | CDA | RPG | R01 | |
|---|---|---|---|---|
| Scholars | 32/43 (74%) | 23/43 (54%) | 22/43 (51%) | 7/43 (16%) |
| Time to award (beginning with date of matriculation into the K12 program) | Median 36 months (IQR 26–43, range 9–83) | Median 35 months (IQR 26–40, range 12–83) | Median 50 months (IQR 36–61, range 9–78) | Median 56 months (IQR 38–73, range 26–78) |
| 2 years | 5 (12%) | 3 (7%) | 2 (5%) | 0 |
| 3 years | 15 (35%) | 11 (26%) | 5 (12%) | 1 (2%) |
| 4 years | 26 (60%) | 18 (42%) | 10 (23%) | 2 (5%) |
| 5 years | 30 (70%) | 21 (49%) | 14 (33%) | 4 (9%) |
| 6 years | 30 (70%) | 21 (49%) | 17 (40%) | 4 (9%) |
| 7 years | 32 (74%) | 23 (54%) | 22 (51%) | 7 (16%) |
CDA, career development award; RPG, research project grant.
FIGURE 1. Time to receipt of first individual career development award or research project grant as principal investigator since beginning the K12 program (n = 43).
*95% CI shown. CDA, career development award; RPG, research project grant.
TABLE 3.
Funding agency and grant type for career development awards and research project grants with the scholar as principal investigator
| Career development awards (n = 23) | ||
|---|---|---|
| Type | ||
| Federal - K23 | 15 | (65%) |
| Federal - K08 | 6 | (26%) |
| National foundation | 2 | (9%) |
| Funding agency | ||
| NHLBI | 15 | (65%) |
| NINDS | 2 | (9%) |
| NICHD | 3 | (13%) |
| NIGMS | 1 | (4%) |
| Robert Wood Johnson Foundation | 1 | (4%) |
| American Heart Association | 1 | (4%) |
| Research project grants (n = 22) | ||
| Type: | ||
| R01 | 7 | (32%) |
| R21 | 3 | (14%) |
| R03 | 3 | (14%) |
| R44 | 1 | (5%) |
| Other | 8 | (36%) |
| Funding agency | ||
| NHLBI | 9 | (41%) |
| NIDDK | 2 | (9%) |
| Department of Transportation | 2 | (9%) |
| Private foundation | 2 | (9%) |
| NINDS | 1 | (5%) |
| NIMHD | 1 | (5%) |
| NIA | 1 | (5%) |
| Office of Naval Research | 1 | (5%) |
| Department of Defense | 1 | (5%) |
| Veterans Administration | 1 | (5%) |
| Clinical and Translational Science Institute | 1 | (5%) |
Abbreviations: NHLBI, National Heart, Lung, and Blood Institute; NINDS, National Institute of Neurological Disorders and Stroke; NICHD, National Institute of Child Health and Human Development; NIGMS, National Institute of General Medical Sciences; NIDDK, National Institute of Diabetes and Digestive and Kidney Diseases; NIMHD, National Institute on Minority Health and Health Disparities; NIA, National Institute on Aging.
FIGURE 2. Time to receipt of first career development award and (separately) first research project grant as principal investigator since beginning the K12 program (n = 43).
*95% CI shown. CDA, career development award; RPG, research project grant.
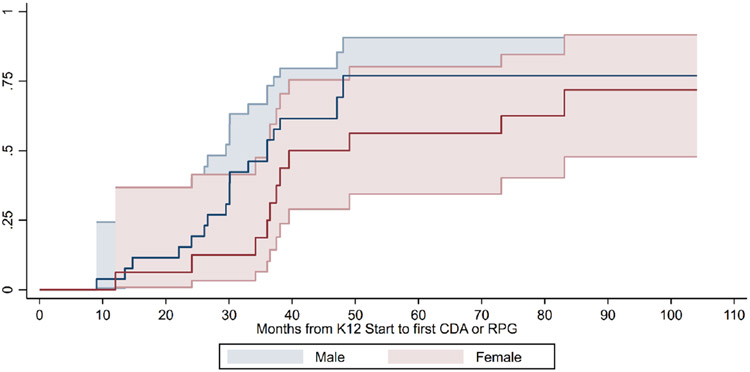
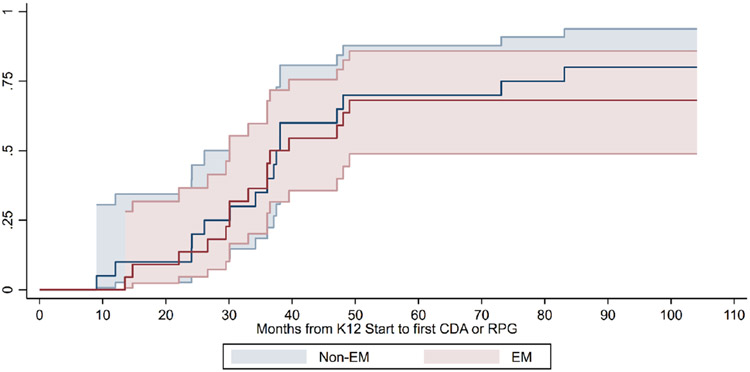
We investigated whether time to receipt of a CDA or RPG differed by scholar sex or specialty training. In Figure 3, we show that time to receipt of first CDA or RPG grant appeared longer for women (women median 37.5 months [IQR 34.1–49.1]; men median 30 months [IQR 26.1–38.1 months], p = 0.14), but the curves eventually align (log-rank test p = 0.27). When we evaluated time to grant funding by specialty training (emergency medicine versus other specialties, Figure 4), there was no difference between the groups (p = 0.59).
FIGURE 3. Time to receipt of first individual career development award or research project grant as principal investigator since beginning the K12 program, by scholar sex (n = 43).
*Log-rank test for difference in time to receipt by sex, p = 0.27. 95% CI shown.
FIGURE 4. Time to receipt of first individual career development award or research project grant as principal investigator since beginning the K12 program, by specialty training (n = 43). EM, emergency medicine.
*Log-rank test for difference in time to receipt by training, p = 0.59. 95% CI shown.
DISCUSSION
The first K12 in emergency care research resulted in a newly funded cohort of successful interdisciplinary clinician-scientists in this domain, with three quarters securing CDAs or RPGs as PI during the follow-up period. However, the duration of time required to secure such awards was well beyond a 3-year training period for many scholars, particularly for RPG awards. With over 143 million annual ED visits in the US12 and almost one in five adults12 and children13 requiring emergency care each year, there remains an urgent need to build a cadre of successful emergency care investigators to build the evidence base. This K12 program demonstrates that federal investment in such a training program helps to build the cadre of investigators, although securing subsequent funding takes many years.
The field of emergency care is inherently multidisciplinary, involving many medical specialties. It follows that clinician-scientists should similarly arise from a diverse group of specialties. This K12 training program included individuals across a variety of training backgrounds, where the orientation to NHLBI funding priorities within emergency care were defined by their research questions, rather than clinical specialty. Among the scholars, there was no difference in the success of grant funding by specialty training, illustrating that the ability to compete for subsequent funding is not dependent on the type of clinical training.
Increasing diversity within the research workforce improves innovation and impact14,15 and is a high priority for the NIH.16,17 Women are under-represented in the biomedical workforce13 and as physician scientists.1 We observed that overall success rates and times for achieving the next funding milestones were similar between men and women, yet the modest sample was likely under-powered to detect a difference. The Kaplan–Meier curves for women versus men suggested that women in the K12 cohort took longer to secure CDA or RPG funding than men, but the funding rates eventually merged. If we made the comparison at an earlier time point, the findings may have appeared different. These results are similar to those of a recent report on women in academic medicine, where a larger proportion of men had been promoted after 7 years, but this advancement gap narrowed by 10 years.18 The challenges faced by women physicians and physician scientists, such as gender-based discrimination and the impact of family responsibilities, have been described in multiple reports.1,18,19 Our results suggest that women clinician-scientists have similar grant success rates compared to their male colleagues, but may require more time, possibly due to the inequities and unique demands endured by women in healthcare and the biomedical workforce. These results provide important insights for federal funding agencies seeking to catalyze the careers and scientific discoveries of women.
Outcomes from the K12 emergency care research program compare favorably to scholar outcomes from Clinical and Translational Science Award KL2 programs across the US during the same period.20 Within the K12 program, 70% of scholars obtained a CDA or RPG within 5 years of starting the program, while 60% of KL2 scholars had secured such funding within 5 years of completing the KL2 program.20 All six institutions in the K12 cohort had an existing Clinical and Translational Science Award (CTSA) at the start of the K12 program, which provided focused education in research, instruction and infrastructure for team science, and mentorship. Similar to the KL2 program, K12 scholars represented many specialties. One unique difference in this K12 program compared to KL2 programs was the focus on a singular (if broad) content area – emergency care. This focus allowed development of an emergency care research community within and across sites, which may have enhanced career development opportunities, mentorship, and collaborations. In a previous qualitative evaluation of the K12 program, participants described collaborations and networking as primary themes in the program, with some participants noting receipt of new research funding based on such programmatic collaborations.10
Clinician-scientists are often advised to pursue institutional research training (e.g., K12 or KL2 programs), followed by an independent CDA, prior to applying for a RPG. In our cohort, a higher proportion of scholars who obtained CDAs subsequently obtained RPGs, as compared to those who did not. While the numbers were small, this finding is consistent with an analysis of National Institute of Child Health and Human Development (NICHD) K12 programs, which found that an independent CDA, whether preceded by a K12 or not, was more likely to result in a RPG compared to a K12 alone.21,22 A K12 provides a strategic boost to clinician-scientists embarking on a research path, which ideally includes a subsequent individual CDA after the K12. Scholars should be aware that it is uncommon to proceed directly to R01 funding after a K12 in the absence of an individual CDA; only two scholars in this cohort were successful in that pathway. Our findings also quantify and highlight the relatively long path for clinician-scientists to reach RPG funding, particularly for R01-level funding, which supports NIH results showing the steadily increasing age of physician scientists at the time of their first RPG.1
The NHLBI K12 program in emergency care research may eventually have a multiplier effect on the emergency care research workforce and knowledge generation, as these clinician-scientists grow as independent investigators, mentors, and leaders. The effect of participation in this K12 program endured through 7 years after matriculation, with sustained growth of these investigators and the emergency care research community. We believe that this K12 program offered a strategic opportunity to enhance the next generation of emergency care researchers across multiple disciplines. However, impact on the field of emergency care and the patients served through the emergency care system will likely take years.
There were limitations in this study. This cohort represented a single K12 program and a modest sample size of scholars. However, the scholars came from six academic sites across the US and a variety of disciplines. Although we focused on grants received as PI, most scholars had multiple grants with other roles (i.e., co-investigator or site investigator), reflecting broader success in team science. We did not include scholars from the subsequent trans-NIH K12 program in emergency care research for consistency in measuring programmatic impact and maximizing follow-up time. Although inclusion of additional scholars would have increased the sample size, their follow-up would have been much shorter and some remain in training. Our primary focus was tracking scholar grant outcomes over an extended follow-up period.
Finally, we did not have a control group for comparison to the K12 scholars. Because this K12 program included a sizable number of scholars outside of emergency medicine, it was not possible to have a pre-post study design, as identification of a similar cohort prior to the K12 was not possible. Identification of a concurrent control group was similarly not feasible due to inherent differences that would create selection bias. We recognize that these issues limit evaluation of the impact of the NHLBI K12 program. However, description of the cohort and their grant funding over an extended period of time contributes valuable information about research workforce development in a specific scientific domain.
In summary, the NHLBI K12 program in emergency care research added to and may have enhanced a competitive workforce of interdisciplinary emergency care investigators. After 7 years of follow-up, approximately three quarters of scholars successfully obtained CDA or RPG funding, with no notable differences by scholar sex or specialty training. These results compare favorably and may exceed the success of other long-standing institutional research training programs.
MEETINGS
These results have not been presented or published in any form.
Funding information
This project was supported by NIH/NHLBI K12 awards at: Icahn School of Medicine at Mount Sinai (#K12 HL109005); Oregon Health & Science University (#K12HL108974); University of California, Davis Medical Center (#K12HL108964); University of Pennsylvania (#K12 HL109009); University of Pittsburgh (#K12 HL109068); and Vanderbilt University Medical Center (#K12 HL109019). The views expressed in this manuscript are those of the authors and do not necessarily represent the views of the National Heart, Lung, and Blood Institute, the National Institutes of Health, or the U.S. Department of Health and Human Services.
Footnotes
CONFLICT OF INTEREST
No author had conflicts of interest related to this study.
REFERENCES
- 1.Physician-Scientist Workforce (PSW) Report 2014. 2014. [Google Scholar]
- 2.Salata RA, Geraci MW, Rockey DC, et al. U.S. Physician-scientist workforce in the 21st century: recommendations to attract and sustain the pipeline. Acad Med. 2018;93(4):565–573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Permar SR, Ward RA, Barrett KJ, et al. Addressing the physician-scientist pipeline: strategies to integrate research into clinical training programs. J Clin Invest. 2020;130(3):1058–1061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rao RC, Dlouhy BJ, Capell BC, Akeju O. The endangered physician-scientist and COVID-19. Cell Rep Med. 2021;2(2):100190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jain MK, Cheung VG, Utz PJ, Kobilka BK, Yamada T, Lefkowitz R. Saving the endangered physician-scientist - a plan for accelerating medical breakthroughs. N Engl J Med. 2019;381(5):399–402. [DOI] [PubMed] [Google Scholar]
- 6.Brown J. National Institutes of Health support for clinical emergency care research, 2011 to 2014. Ann Emerg Med. 2016;68(2):164–171. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine, Committee on the Future of Emergency Care in the United States Health System. Hospital-Based Emergency Care at the Breaking Point. National Academies Press; 2006. [Google Scholar]
- 8.Neumar RW, Blomkalns AL, Cairns CB, et al. Emergency medicine research: 2030 strategic goals. Acad Emerg Med. 2021;29:241–251. [DOI] [PubMed] [Google Scholar]
- 9.Definitions of Criteria and Considerations for Research Project Grant (RPG/R01/R03/R15/R21/R34) Critiques National Institutes of Health. NIH Grants & Funding, NIH Central Resource for Grants and Funding Information Web site. Accessed February 28, 2022. [Google Scholar]
- 10.Newgard CD, Morris CD, Smith L, et al. The first National Institutes of Health institutional training program in emergency care research: productivity and outcomes. Ann Emerg Med. 2018;72(6):679–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.NHLBI Research Career Development Programs in Emergency Medicine Research (K12), RFA HL-11-011. National Institutes of Health. https://grants.nih.gov/grants/guide/rfa-files/rfa-hl-11-011.html. Published 2010. Accessed March 1, 2022. [Google Scholar]
- 12.Trency Department Services, 2009–2018. Washington, DC, 2021. [Google Scholar]
- 13.Health, United States, Emergency department visits within the pasts 12 months among children under age 18. National Center for Health Statistics, https://www.cdc.gov/nchs/data/hus/2019/036-508.pdf. Published 2019. Accessed. [Google Scholar]
- 14.Woolley AW, Chabris CF, Pentland A, Hashmi N, Malone TW. Evidence for a collective intelligence factor in the performance of human groups. Science. 2010;330(6004):686–688. [DOI] [PubMed] [Google Scholar]
- 15.AlShebli BK, Rahwan T, Woon WL. The preeminence of ethnic diversity in scientific collaboration. Nat Commun. 2018;9(1):5163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Inviting Comments and Suggestions on the Draft NIH Chief Officer for Scientific Workforce Diversity Strategic Plan for FYs 2022–2026. National Institutes oh Health. https://grants.nih.gov/grants/guide/notice-files/NOT-OD-22-054.html. Published 2022. Accessed March 4, 2022. [Google Scholar]
- 17.Bernard M. NIH Chief Officer for Scientific Workforce Diversity Strategic Plan Draft. Bethesda, MD; 2022. [Google Scholar]
- 18.Lautenberger DM, Dandar VM. The State of Women in Academic Medicine 2018–2019 - Exploring Pathways to Equity. American Association of Medical Colleges; 2020. [Google Scholar]
- 19.United States Government Accountability Office Report to Congressional Committees: NIH Research - Action Needed to Ensure Workforce Diversity Strategic Goals Are Achieved. August 2018 2018. GAO-18-545. [Google Scholar]
- 20.Sorkness CA, Scholl L, Fair AM, Umans JG. KL2 mentored career development programs at clinical and translational science award hubs: practices and outcomes. J Clin Transl Sci. 2020;4(1):43–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Twombly DA, Glavin SL, Guimond J, Taymans S, Spong CY, Bianchi DW. Association of National Institute of child health and human development career development awards with subsequent research project Grant funding. JAMA Pediatr. 2018;172(3):226–231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Good M, McElroy SJ, Berger JN, Moore DJ, Wynn JL. Limited achievement of NIH research independence by pediatric K award recipients. Pediatr Res. 2018;84(4):479–480. [DOI] [PMC free article] [PubMed] [Google Scholar]