Abstract
Objective
To investigate the association of cannabis use with major depression and suicidal behavior in adolescence.
Method
Data are from the National Comorbidity Survey−Adolescent Supplement (N = 10,123), a nationally representative survey of adolescents aged 13 to 18 years. Weighted logistic regression and ordinal regression analyses of major depression and suicidal behavior outcomes were conducted on cannabis variables, incorporating sociodemographic characteristics.
Results
Adolescents with lifetime cannabis use have 2.07 times higher odds of mild/moderate (adjusted odds ratio [aOR]; 95% CI = 1.69, 2.53) and 3.32 times higher odds of severe major depressive disorder (MDD; aOR; 95% CI = 2.31, 4.75). Cannabis use (aOR 6.90, 95% CI = 4.67, 10.19), mild/moderate MDD (aOR 4.10, 95% CI = 2.82, 5.98), and severe MDD (aOR 13.97, 95% CI = 7.59, 25.70) were associated with higher odds of suicide attempt. Past 12-month cannabis use (aOR 3.70, 95% CI = 2.16, 6.32), mild/moderate major depressive episodes (MDE) (aOR 7.85, 95% CI = 3.59, 17.17), and severe MDE (aOR 36.36, 95% CI = 13.68, 96.64) were associated with higher odds of suicide attempt. The frequency of past 12-month cannabis use was associated with higher odds of suicide attempt and with MDE severity, with higher odds among individuals who use cannabis 3 or more days than among individuals who use cannabis less frequently, suggesting a dose effect. Among cannabis users, older age of onset of cannabis use was associated with lower odds of suicidal behaviors.
Conclusion
Cannabis use is associated with higher odds of depression and depression severity in adolescence. Furthermore, depression and cannabis use are independently associated with higher odds of suicide attempt.
Diversity & Inclusion Statement
We worked to ensure sex and gender balance in the recruitment of human participants. We worked to ensure race, ethnic, and/or other types of diversity in the recruitment of human participants. The author list of this paper includes contributors from the location and/or community where the research was conducted who participated in the data collection, design, analysis, and/or interpretation of the work. One or more of the authors of this paper self-identifies as a member of one or more historically underrepresented racial and/or ethnic groups in science. We actively worked to promote sex and gender balance in our author group. We actively worked to promote inclusion of historically underrepresented racial and/or ethnic groups in science in our author group.
Key words: adolescence, cannabis, major depressive disorder, suicidal behavior, suicide attempt
Adolescence is characterized by a vital period of ongoing neurodevelopment,1 during which many youth first manifest symptoms of depressive and other psychiatric disorders.2 The prevalence of lifetime adolescent major depressive disorder (MDD) is 11% to 17% in the United States.2 Depression increases in prevalence among older-aged adolescents and is more prevalent in female adolescents. Adolescent depression is also associated with increased risk for morbidity and mortality, and suicide is the second leading cause of death for youth aged 10 to 19 years.3 Furthermoer, among adolescents with MDD, 1 in 4 meet criteria for severe MDD.2 As such, adolescent depression represents a significant individual and public health concern with significant adverse outcomes. These include impairment due to severe MDD and the risk of suicidal behavior. One factor that may be associated with MDD severity and suicidal behavior is cannabis use.
In addition to being a vulnerable period for the onset of mental health disorders, many individuals begin experimenting with substance use during adolescence. Furthermore, adolescent substance use problems commonly co-occur with other mental health disorders, including depression.4 Cannabis is among the most used substances during adolescence, with an estimated lifetime prevalence of 43.7% among 12th grade students in 2020.5 Moreover, adolescents aged 12 to 17 years have generally remained the largest age group to initiate cannabis use as of 2019.6,7 Although the lifetime and past 12-month prevalence of cannabis use have remained relatively steady over the past few decades, daily cannabis use has risen over the past 2 years to its highest level in 3 decades.5 Characterizing MDD and suicidal behavior in the context of comorbid factors, including substance use, is of vital importance to inform policies and interventions that mitigate adverse outcomes.
Cannabis use is twice as common among adolescents with MDD, and MDD is associated with greater risk of progressing to substance use problems, including substance use disorders.8, 9, 10 To date, studies have shown that comorbid MDD and substance use disorders are generally associated with more severe depression and substance use problems, poorer clinical outcomes, and decreased treatment adherence.11, 12, 13, 14 Drug use has also been established as a risk factor for suicidal behavior.15, 16, 17, 18 A recent meta-analysis found that onset of cannabis use before age 18 years was associated with higher odds of depression and suicidal ideation in young adulthood.19 In another study of adults aged 18 to 34 years, cannabis use and major depressive episodes (MDE) were independent risk factors for higher prevalence of suicide attempt.20 Notably, effects of cannabis use remained significant after controlling for cannabis use disorder, suggesting that associations were not due to consequences of “disordered use.” It is particularly important to understand suicidal behavior during adolescents, when it is a leading cause of morbidity and mortality. Although cannabis use and MDD are common among adolescents, their relationship with suicidal behavior during adolescence is unknown.
To address knowledge gaps in how cannabis use, suicidality, and MDD are related, we utilized the National Comorbidity Survey−Adolescent Supplement (NCS-A),21 a large, nationally representative cross-sectional study. We aimed to determine the association of cannabis use with MDD diagnosis and severity and past 12-month major depressive episode (MDE) and severity. We also examined the association of cannabis use and depression as independent risk factors for suicidal behavior, including suicide attempt. Among adolescents who used cannabis, we examined the association of age of onset of cannabis use with lifetime MDD and suicidal behavior. Finally, we investigated the association of the frequency of past 12-month cannabis use with MDE with severity and past 12-month suicidal behavior.
Method
Sample
Analyses were completed using NCS-A, a nationally representative survey of adolescents aged 13 to 18 years in the United States conducted from 2001 to 2004 (N = 10,123). The analyses presented herein include 10,100 participants for whom data on lifetime cannabis use were available. The NCS-A was designed to examine risk of and protective factors for mental health disorders in adolescents.21 Overall study design and survey procedures have been previously described.22, 23, 24 Briefly, trained interviewers administered the survey including a modified World Health Organization Composite International Diagnostic Interview (CIDI) to adolescents in household and school subsamples (82.9% response rate). A self-administered questionnaire was mailed to 1 parent or guardian of each adolescent participant (83.3% conditional response rate).2 As previously reported, recruitment, consent, and study procedures were approved by the applicable institutional human participants review committees.21 Procedures for analyses presented herein were approved by the Colorado Multiple Institutional Review Board at the University of Colorado School of Medicine.
Measures
Sociodemographic Variables
Well-established sociodemographic variables of mental health disorders were assessed, including adolescent reported age, sex/gender, race/ethnicity, region, and urbanicity.21 A poverty index ratio was calculated based on family size and the ratio of family income to poverty threshold level, with ≤1.5 defined as poor.2
Cannabis Use
We created dichotomous variables for lifetime cannabis use and past 12-month cannabis use determined by affirmative response to use of “marijuana or hashish” during those time periods. The frequency of past 12-month cannabis use was reported as an ordinal variable: none, occasional (“less than once a month”), moderate (“1-3 days per month” or “1-2 days per week”), and heavy (“3-4 days per week” or “nearly every day”). Individuals who reported never using cannabis were inferred to have not used cannabis in the past 12 months.
MDD and MDD Symptom Domains
The CIDI assesses self-report symptoms of DSM-IV lifetime MDD and past 12-month MDE, as well as dysthymia and a range of other mental health disorders. For analyses presented herein, only adolescent report was used.25,26 Participants who endorsed sadness, discouragement, or boredom lasting “several days/two weeks” were asked to think about the time when the problems were the worst. Those who endorsed either depressed mood or anhedonia were subsequently asked additional questions about other DSM-IV MDD symptoms. Per the study diagnostic algorithm, dichotomous DSM-IV MDD symptom domains were categorized as depressed mood, anhedonia, appetite change, sleep problems, psychomotor agitation or retardation, fatigue, worthlessness, impaired concentration, and suicidal behavior. Suicidal behavior in MDD was assessed specific to the depressive episode and consisted of suicidal ideation (“think a lot about death,” “think that it would be better if you were dead,” or “think about killing yourself”), suicide plan, and suicide attempt. As previously described, diagnostic hierarchy rules were applied to the diagnosis of MDD and required an endorsement of distress or impairment.2 Severe MDD required the endorsement of both high levels of distress (“severe” or “very severe”) and impairment (“a lot” or “extreme”) to be present to investigate correlates of more clinically significant manifestations of depression.2
Past 12-Month Depression Variables
Similar to MDD, diagnostic hierarchy rules were applied to the diagnosis of past 12-month MDE and severe MDE required high levels of distress or impairment.2 Adolescents with 12-month MDE were also asked about the number of MDE (“how many different episodes”) and number of days out of role (“totally unable to go to school or work or carry out your normal activity”) in the past 12 months. We created dichotomous variables for professional treatment, use of antidepressant medications, and use of any psychopharmacologic medications in the past 12 months. Use of other classes of pharmacologic agents and hospitalizations were rare and not analyzed further.
Suicidal Behavior Variables
In a separate section of the CIDI independent of any mental health diagnoses over their lifetime (“ever happen to you”) and in the past 12 months, all participants were asked about suicidal behavior in order of severity: suicidal ideation, suicide plan, and suicide attempt. If a participant answered “no” to a preceding suicidal behavior, subsequent questions were not asked. For these analyses, we inferred that those participants who reported “no” to a suicidal behavior also did not experience subsequent categories of suicidal behavior (eg, an adolescent who reported no suicidal ideation did not experience suicide plan nor suicide attempt). Similar inferences were applied to past 12-month suicidal behavior. Adolescents who attempted suicide were also asked about the intent of the most recent attempt (“serious attempt to kill myself,” “tried to kill myself, but knew that the method may not work,” and “cry for help…did not intend to die”).
Statistical Analyses
Data were analyzed in SAS version 9.4. Procedures for analyzing complex survey data such as in the NCS-A were used with appropriate specifications on the STRATA, CLUSTER, and WEIGHT statements. The unadjusted associations between lifetime cannabis use and participant characteristics and MDD symptom domains were evaluated with Rao−Scott χ2 tests, a design-adjusted version of the likelihood ratio test.27,28 Similarly, associations among past 12-month cannabis use and reported antidepressant medication use and any medication use were evaluated in the subset of participants reporting past 12-month MDE.
Weighted multiple logistic regression and ordinal regression analyses were conducted, adjusting for sociodemographic variables that were associated with lifetime cannabis use and/or MDD (age, sex, race/ethnicity, and region), to evaluate cannabis use as a predictor of MDD outcomes; similarly, past 12-month cannabis use was evaluated as a predictor of MDE in the subset of adolescents reporting lifetime depression. Initially, the cannabis by sex interaction was evaluated in these models and removed if p > .1. Weighted multiple logistic and ordinal regression analyses adjusting for the same variables were also conducted evaluating lifetime cannabis use and MDD as predictors of lifetime suicidal behavior; similarly, past 12-month cannabis use and MDE were evaluated as predictors of past 12-month suicidal behaviors. For all suicidal behavior outcomes, cannabis by depression interactions were evaluated and removed from the model if p > .1.
Finally, in the subset of those reporting past 12-month MDE, “days out of role” and “number of depressive episodes” were evaluated as frequency outcomes using weighted multiple linear regressions adjusting for the same characteristics. Analytic options are more limited in the survey design context, so SAS Procedure Surveyreg for linear regression was used even though these outcomes were not normally distributed. It has been shown that results from applying parametric procedures in these contexts approximate those from nonparametric permutation approaches very well.29
Results
The lifetime prevalence rate of any cannabis use among adolescents was 22.5%. Prevalence of cannabis use was associated with older age, race/ethnicity, and region (Table 1). The highest rates of cannabis use were reported among Hispanic (26.5%) adolescents, with the lowest prevalence among adolescents who identified race as other (17.7%). Adolescents living in the western region of the United States reported the highest rates of cannabis use (31.0%), with the lowest rates in the southern region (17.8%).
Table 1.
Sociodemographic Factors and Major Depressive Disorder (MDD) by Lifetime Cannabis Use (N = 10,100)
| Characteristic | Lifetime cannabis n = 2,281 | No cannabis n = 7,819 |
Test (df), significance (p) |
|---|---|---|---|
| Age, y | 16.0 (SE = 0.06) | 15.0 (SE = 0.07) | F1,42 = 208.2, <.0001 |
| Sex, % | χ2 (1) = 2.14, .14 | ||
| Female, n = 5,159 | 22.3 | 77.7 | |
| Male, n = 4,941 | 24.3 | 75.6 | |
| Race/ethnicity, % | χ2 (3) = 9.85, .020 | ||
| Hispanic, n = 1,907 | 26.5 | 73.5 | |
| Non-Hispanic Black, n = 1,950 | 18.4 | 81.6 | |
| Other, n = 621 | 17.7 | 82.3 | |
| Non-Hispanic White, n = 5,622 | 19.5 | 80.5 | |
| US region, % | χ2 (3)=14.34, .0025 | ||
| Northeast, n = 1,863 | 22.6 | 77.4 | |
| Midwest, n = 2,772 | 25.1 | 74.9 | |
| South, n = 3,429 | 17.8 | 82.2 | |
| West, n = 2,036 | 31.0 | 69.0 | |
| Urbanicity, % | χ2 (2) = 4.26, .12 | ||
| Metropolitan, n = 4,496 | 25.3 | 74.7 | |
| Other urban, n = 3,301 | 22.0 | 78.0 | |
| Rural, n = 2,303 | 20.5 | 79.5 | |
| Poverty index ratio, % | χ2 (3) = 0.27, .97 | ||
| ≤1.5 (poor), n = 1,713 | 22.7 | 77.3 | |
| >1.5 and ≤3, n = 2,017 | 23.1 | 76.9 | |
| >3 and ≤6, n = 3,095 | 23.7 | 76.3 | |
| >6, n = 3,275 | 23.4 | 76.6 | |
| MDD lifetime, % | χ2 (1) = 94.0, <.0001 | ||
| MDD lifetime, n = 1,125 | 41.1 | 58.9 | |
| MDD severity lifetime, % | |||
| None, n = 8,975 | 21.1 | 78.8 | χ2 (2) = 140.5, <.0001 |
| Mild/moderate, n = 828 | 37.1 | 62.9 | |
| Severe, n = 297 | 52.1 | 48.0 |
Major Depressive Disorder
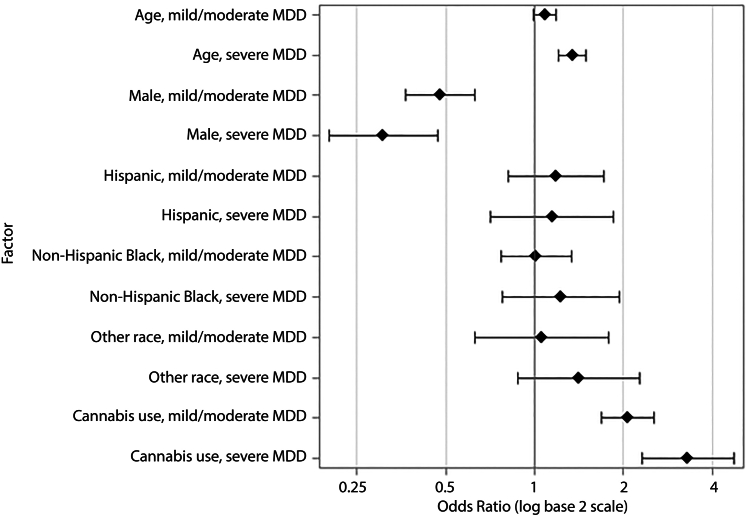
The lifetime prevalence rate of DSM-IV MDD was 11.1% among the participants, of whom 26.4% met criteria for severe MDD. Overall, lifetime cannabis use was strongly associated with having MDD, as well as with severity of MDD (Table 1). For all weighted logistic and ordinal regression models evaluating MDD, the sex by cannabis use interaction was not significant and was removed. Compared to adolescents who had never used cannabis, adolescents with lifetime cannabis use had a 2.35 times higher odds of MDD (95% CI = 1.92, 2.89) after adjusting for sociodemographic characteristics. Similarly, adolescents with lifetime cannabis had 2.07 times higher odds of mild/moderate MDD (95% CI = 1.69, 2.53) and 3.32 times higher odds of severe MDD (95% CI = 2.31, 4.75) than no depression, respectively (Figure 1). Among adolescents who reported lifetime cannabis use, age of onset of cannabis use was not significantly associated with lifetime MDD with severity after adjusting for sociodemographic factors (F = 1.70, df = 2, p = .18).
Figure 1.
Forest Plot of Odds Ratios of Lifetime Major Depressive Disorder (MDD) Severity for Lifetime Cannabis Use and Sociodemographic Factors
Note:Adjusted odds ratios (OR) and 95% CI for mild/moderate and severe major depressive disorder (MDD) are presented for cannabis use and other sociodemographic characteristics (region included in model not shown).
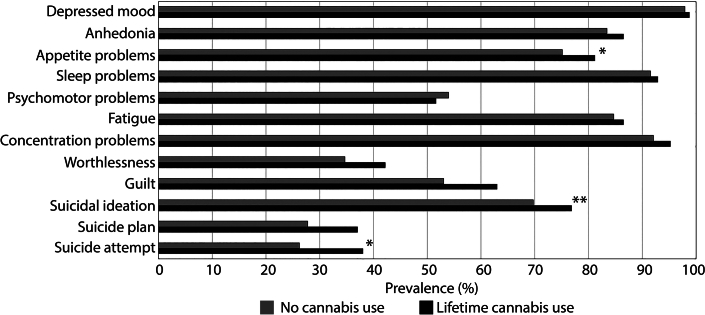
Participant age was positively associated with higher odds of MDD and severe MDD (Figure 1). Male adolescents had lower odds of MDD, mild/moderate MDD, and severe MDD (Figure 1). In those with lifetime MDD, the prevalence of each symptom of MDD and suicidal behavior during a depressive episode are shown for participants with and without lifetime cannabis use in Figure S1, available online. Lifetime cannabis users reported significantly more appetite problems (χ2 = 5.30, df = 1, p = .021), suicidal ideation (χ2 = 8.98, df = 1, p = .0027), and suicide attempt (χ2 = 4.70, df = 1, p = .030) than nonusers.
Past 12-Month MDE in Adolescents With MDD
Among adolescents with MDD, 68.7% met criteria for a MDE in the past 12 months, with 20.5% of adolescents having severe symptoms of MDE. Cannabis use in the past 12 months was associated with a higher prevalence of past 12-month MDE (76.7% vs 66.1%, χ2 = 13.18, df = 1, p = .0003) and severe past 12-month MDE (29.4% vs 17.7%, χ2 = 12.15, df = 2, p = .0023), compared to adolescents who did not use cannabis in the past 12 months. Furthermore, adolescents who used cannabis in the past 12 months had a 2.27 times higher odds of past 12-month MDE compared to those who did not use cannabis (95% CI = 1.45, 3.57), after adjusting for sociodemographic characteristics (Table S1, available online). Similarly, adolescents who used cannabis had 2.06 times higher odds of past mild/moderate MDE (95% CI = 1.30, 3.25) and 2.83 times higher odds of past severe MDE (95% CI = 1.46, 5.51), compared to no MDE. Although cannabis use was associated with MDE severity, there was no association between cannabis use and days out of role due to MDE after adjusting for sociodemographic characteristics (F1,42 = 0.67, p = .42). On average, adolescents who used cannabis in the past 12 months reported 14.6 (SE = 3.3) days out of role compared to 12.7 (SE = 2.6) days for adolescents who did not. However, after the same adjustments, there was a trend for number of depressive episodes due to MDE to be associated with cannabis use (F1,42 = 3.88, p = .055). On average, adolescents who used cannabis in the past 12 months reported 4.3 (SE = 0.48) episodes compared to 3.1 (SE= 0.30) episodes for adolescents who did not.
Table 2 shows results of multiple ordinal regression of MDE with severity on past 12-month cannabis use frequency and sociodemographic characteristics. Compared to adolescents who did not use cannabis, those who used cannabis on average 3 or more days per week had 2.24 times higher odds of mild/moderate MDE (95% CI = 1.18, 4.22) and 2.64 times higher odds of severe MDE (95% CI = 1.04, 6.70), compared to no MDE, and using cannabis 1 to 3 days per month up to 1 to 2 days per week was associated with higher odds of severe MDE. Less than monthly cannabis use was not associated with the odds of mild/moderate or severe MDE.
Table 2.
Odds Ratios of Past 12-month Major Depressive Episodes (MDE) and Suicidal Behavior by Frequency of Past 12-month Cannabis Use
| Past 12-month cannabis use frequencya | aOR point estimateb | 95% CI, upper | 95% CI, lower |
|---|---|---|---|
| Mild/moderate MDEc | |||
| Less than monthly | 1.75 | 0.78 | 3.93 |
| 1-3 days/mo to 1-2 days/wk | 1.79 | 0.69 | 4.68 |
| 3-4 days/wk or more | 2.24 | 1.18 | 4.22 |
| Severe MDEc | |||
| Less than monthly | 2.22 | 0.93 | 5.28 |
| 1-3 days/mo to 1-2 days/wk | 3.89 | 1.12 | 13.49 |
| 3-4 days/wk or more | 2.64 | 1.04 | 6.7 |
| Suicidal ideationd | |||
| Less than monthly | 2.72 | 1.46 | 5.05 |
| 1-3 days/mo to 1-2 days/wk | 5.46 | 2.81 | 10.59 |
| 3-4 days/wk or more | 5.59 | 3.56 | 8.77 |
| Suicide pland | |||
| Less than monthly | 5.65 | 2.43 | 13.12 |
| 1-3 days/mo to 1-2 days/wk | 4.44 | 1.13 | 17.48 |
| 3-4 days/wk or more | 11.16 | 3.91 | 31.88 |
| Suicide attemptd | |||
| Less than monthly | 4.91 | 1.96 | 12.26 |
| 1-3 days/mo to 1-2 days/wk | 6.77 | 1.59 | 28.90 |
| 3-4 days/wk or more | 8.67 | 1.92 | 39.15 |
Note: aOR = adjusted odds ratio.
Past 12-month cannabis use frequency was evaluated as a categorical variable, with no use as the reference group.
Adjusted OR were estimated using ordinal regression models adjusted for age, sex, race, and US region.
Past 12-month MDE severity was modeled as an ordinal outcome, with no MDE as the reference group.
Past 12-month suicidal behavior was modeled as binary outcomes of suicidal ideation, suicide plan, and suicide attempt adjusted for age, sex, race, US region, and past 12-month MDE.
Lifetime Suicidal Behavior
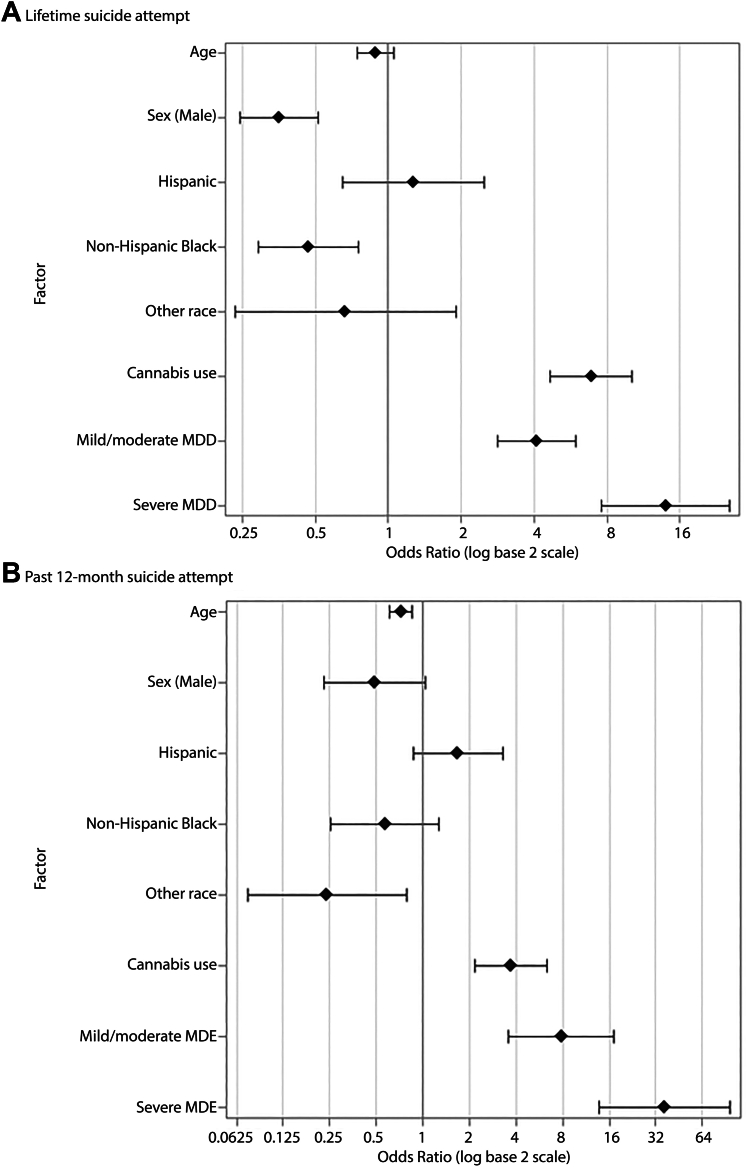
In addition to suicidal behavior queries in the context of MDD diagnosis, all survey participants were asked about lifetime suicidal behavior and past 12-month suicidal behavior. Overall, 11.1% of youth in the sample endorsed suicidal ideation, whereas 3.3% endorsed developing a suicide plan and 3.0% endorsed attempting suicide. Logistic regressions of these suicidal behaviors were conducted to evaluate lifetime cannabis use and MDD with severity as potential predictors after adjusting for sociodemographic characteristics (Table 3, Figure 2A). For each outcome, the interaction between lifetime cannabis and MDD with severity was not significant and was removed.
Table 3.
Logistic Regression Analyses of Lifetime Suicidal Behavior on Lifetime Cannabis Use, Major Depressive Disorder (MDD), and Sociodemographic Factors
| Parametera | Wald χ2 (df) | p | aOR point estimate | 95% CI, upper | 95% CI, lower |
|---|---|---|---|---|---|
| Suicidal ideation | |||||
| Age | 0.2777 (1) | .5982 | 1.02 | 0.95 | 1.08 |
| Sex (Male) | 23.6624 (1) | <.0001 | 0.65 | 0.54 | 0.78 |
| Race/ethnicity | 15.8739 (3) | .0012 | — | — | — |
| Hispanic | 0.93 | 0.68 | 1.27 | ||
| Non-Hispanic Black | 0.62 | 0.48 | 0.81 | ||
| Other race | 0.77 | 0.50 | 1.17 | ||
| US region | 10.4141 (3) | .0154 | — | — | — |
| Northeast | 1.03 | 0.77 | 1.37 | ||
| Midwest | 1.32 | 1.06 | 1.65 | ||
| West | 1.37 | 0.99 | 1.91 | ||
| Cannabis use | 94.6399 (1) | <.0001 | 3.03 | 2.41 | 3.82 |
| MDD | 218.5910 (2) | <.0001 | — | — | — |
| Mild/moderate MDD | 4.24 | 3.41 | 5.28 | ||
| Severe MDD | 10.36 | 6.75 | 15.89 | ||
| Suicide plan | |||||
| Age | 0.0589 (1) | .8083 | 1.02 | 0.87 | 1.19 |
| Sex, male | 7.6957 (1) | .0055 | 0.60 | 0.41 | 0.87 |
| Race/ethnicity | 6.2884 (3) | .0984 | — | — | — |
| Hispanic | 0.79 | 0.47 | 1.33 | ||
| Non-Hispanic Black | 0.58 | 0.34 | 0.99 | ||
| Other race | 0.49 | 0.23 | 1.03 | ||
| US region | 6.3342 (3) | .0964 | — | — | — |
| Northeast | 0.94 | 0.65 | 1.34 | ||
| Midwest | 0.86 | 0.60 | 1.25 | ||
| West | 1.70 | 1.02 | 2.85 | ||
| Cannabis use | 48.5855 (1) | <.0001 | 3.79 | 2.58 | 5.58 |
| MDD | 116.6159 (2) | <.0001 | — | — | — |
| Mild/moderate MDD | 3.58 | 2.45 | 5.22 | ||
| Severe MDD | 13.56 | 7.94 | 23.18 | ||
| Suicide attempt | |||||
| Age | 2.1360 (1) | .1439 | 0.88 | 0.75 | 1.05 |
| Sex, male | 32.3388 (1) | <.0001 | 0.35 | 0.24 | 0.51 |
| Race/ethnicity | 13.4035 (3) | .0038 | — | — | — |
| Hispanic | 1.27 | 0.65 | 2.50 | ||
| Non-Hispanic Black | 0.47 | 0.29 | 0.75 | ||
| Other race | 0.66 | 0.23 | 1.90 | ||
| US region | 2.5236 (3) | .4710 | — | — | — |
| Northeast | 1.23 | 0.78 | 1.93 | ||
| Midwest | 0.95 | 0.63 | 1.42 | ||
| West | 1.17 | 0.70 | 1.95 | ||
| Cannabis use | 99.6374 (1) | <.0001 | 6.90 | 4.67 | 10.19 |
| MDD | 97.4933 (2) | <.0001 | — | — | — |
| Mild/moderate MDD | 4.10 | 2.82 | 5.98 | ||
| Severe MDD | 13.97 | 7.59 | 25.70 |
Note: aOR = adjusted odds ratio.
Reference groups are female (sex), non-Hispanic White (race), South (region), and no MDD.
Figure 2.
Forest Plots of Odds Ratios of Suicide Attempt for Cannabis Use, Depression, and Sociodemographic Factors
Note:(A) Adjusted odds ratios (OR) and 95% CI for risk of lifetime suicide attempt are presented for lifetime cannabis use, major depressive disorder (MDD) severity, and sociodemographic characteristics. (B) Adjusted OR and 95% CI for risk of past 12-month suicide attempt are presented for past 12-month cannabis use, MDE severity, and other sociodemographic characteristics (region included in models not shown).
After adjusting for MDD and other covariates, cannabis use was significantly associated with 3.03 times higher odds of suicidal ideation (95% CI = 2.41, 3.82), 3.79 times higher odds of suicide plan (95% CI = 2.58, 5.58), and 6.90 times higher odds of suicide attempt (95% CI = 4.67, 10.19). Similarly, after adjusting for cannabis use and other covariates, mild/moderate MDD was associated with higher odds of suicidal ideation (adjusted odds ratio [aOR] = 4.24, 95% CI = 3.41, 5.28), suicide plan (aOR = 3.58, 95% CI = 2.45, 5.22), and suicide attempt (aOR = 4.10, 95% CI = 2.82, 5.98) compared to youth without MDD, and severe MDE was more strongly associated with higher odds of suicidal ideation (aOR = 10.36, 95% CI = 6.75, 15.89), suicide plan (aOR = 13.56, 95% CI = 7.94, 23.18), and suicide attempt (aOR = 13.97, 95% CI = 7.59, 25.70) compared to youth without MDD.
To further investigate the association of cannabis use with suicidal behavior, we conducted logistic regressions of suicidal behavior in the subset of participants reporting lifetime cannabis use on the age of onset of cannabis use, lifetime MDD with severity, and sociodemographic factors (Table S2, available online). After accounting for MDD with severity, age of onset of cannabis use was significantly associated with the odds of suicidal ideation (F = 9.20, df = 1, p = .004), suicide plan (F =7.94, df = 1, p = .007), and suicide attempt (F = 6.64, df = 1, p = .014). Focusing on lifetime suicide attempt, for every 1-year increase in age beginning cannabis use, the odds of reporting an attempt decreased by 15.3% (95% CI = 25.7%, 94.5%). Similar to the previous logistic regression model, among adolescents who used cannabis, MDD with severity was also significantly associated with suicidal behavior (Table S2, available online).
Past 12-Month Suicidal Behavior
Overall, 5.2% of participants reported any suicide behavior in the past 12 months, with 5.1% reporting suicidal ideation, 1.3% reporting suicide plan, and 1.2% reporting suicide attempt. There was an interaction between MDE severity and past 12-month cannabis use for past 12-month suicidal ideation (χ2 = 10.97, df = 2, p = .0042) and for suicide plan (χ2 = 11.74, df = 2, p = .0028), such that the effect of past 12-month cannabis use on suicidal behavior differed by MDE severity (Table S3, available online). For adolescents without MDE, those who used cannabis had 4.12 times higher odds of suicidal ideation (95% CI = 2.73, 6.22) compared to nonusers. Similarly, those who used cannabis had 6.38 times higher odds of endorsing a suicide plan (95% CI = 3.17, 12.85) compared to nonusers. For adolescents with mild/moderate or severe MDE, using cannabis did not result in greater odds of suicidal ideation or suicide plan.
Considering the interaction in terms of cannabis use highlights the association of MDE with suicidal behavior. Among adolescents who did not use cannabis, the odds of suicidal ideation and suicide plan were 9.01 (95% CI = 6.23, 13.03) and 13.74 (95% CI = 6.59, 28.64) times higher for mild/moderate MDE and 18.57 (95% CI = 9.38, 36.80) and 71.55 (95% CI = 28.05, 182.49) times higher for severe MDE compared to no MDE, respectively. Among adolescents with mild/moderate or severe MDE, past 12-month cannabis use was not associated with increased odds of suicidal ideation or suicide plan.
When modeling past 12-month suicide attempt, the interaction between cannabis use and MDE severity was not significant (χ2 = 3.09, df = 2, p = 0.21) and was removed. After adjusting for MDE severity and sociodemographic factors, past 12-month cannabis use was associated with 3.70 times higher odds of suicide attempt (95% CI = 2.16, 6.32) (Figure 2B, Table S4, available online). Similarly, after adjusting for cannabis use, mild/moderate MDE and severe MDE were associated with 7.85 (95% CI = 3.59, 17.17) and 36.36 (95% CI = 13.68, 96.64) times higher odds of suicide attempt compared to those in adolescents without MDE.
When modeling past 12-month suicidal behavior, the interaction between frequency of past 12-month cannabis use and MDE severity was significant (data not shown). Among adolescents without MDE, odds of suicidal behavior were highest among youth who used cannabis 3 or more days a week (Table 2). The odds of suicide attempt were 8.67 times higher for adolescents who use cannabis 3 or more days a week (95% CI = 1.92, 39.15), 6.77 times higher for adolescents who use cannabis 1 to 3 days per month to 1 to 2 days per week (95% CI = 1.59, 28.90), and 4.91 times higher for adolescents who use cannabis less than monthly (95% CI = 1.96, 12.26). Overall, for adolescents with mild/moderate or severe MDE, frequency of cannabis use was not associated with increased odds of suicidal behavior (data not shown).
Discussion
This study examined the relationship between cannabis use and MDD in a nationally representative sample of adolescents. Across several analyses, cannabis use was consistently associated with major depression, including past 12-month and lifetime use. Sociodemographic factors did not explain these associations. Furthermore, more frequent cannabis use (3 or more days a week) was associated with a higher odds of past 12-month MDE, suggesting a possible dose−response relationship. Lifetime cannabis use was also associated with specific symptoms of depression, including appetite problems, suicidal ideation, and suicide attempt. Most notable is that lifetime cannabis use was associated with suicidal ideation, having a suicide plan, and a suicide attempt, even after adjusting for lifetime MDD. Similarly, past 12-month cannabis use was associated with past 12-month suicide attempt, after adjusting for past 12-month MDE. The potential link between cannabis use and suicidal behavior is further supported by 2 additional findings. Among adolescents who used cannabis, older age of onset of cannabis use was associated with lower odds of each lifetime suicidal behavior. Finally, more frequent cannabis use (3 or more days a week) was consistently associated with higher odds of past 12-month suicidal ideation, suicide plan, and suicide attempt.
There are several proposed mechanisms by which cannabis may be associated with depression. Depression often precedes cannabis use, whereby cannabis is used as a self-medication attempt.30,31 Conversely, cannabis use in youth is also associated with increased odds of developing depression later in life.32, 33, 34 Alternatively, the association between cannabis use and depression may exist because of shared environmental and genetic risk factors.35,36 Social stressors are independently associated with cannabis use and depression, as well as their co-occurrence.30 In addition, genetic factors underlie part of the correlation between cannabis use disorder and MDD.37 Thus, multiple etiological pathways likely link cannabis use and MDD.
Research on the biological effects of cannabis may provide further insight into the etiological pathways that underlie co-occurring cannabis use and MDD. Cannabis can affect neurocircuitry and genetic predisposition related to depression.38,39 The acute and long-term effects of cannabis are attributed primarily to the exogenous cannabinoid Δ-9-tetrahydrocannabinol (THC), including in a dose-dependent manner.40 Specifically, THC binds to cannabinoid receptors, affecting the endocannabinoid, serotonin, dopamine, and other neurotransmitter systems.39,41 Trials of rimonabant, a selective cannabinoid-1 receptor antagonist developed to treat weight loss, were terminated due to serious risk of increased depression and suicide,42 further implicating the endocannabinoid system in depression. Although cannabis is related to depression and suicidality, with possible mechanisms identified, plausible alternative explanations must be ruled out to support a causal relationship.43
Family-based studies have been instrumental in controlling for important genetic and environmental confounds while testing the relationship between cannabis use and depression. For example, co-twin control studies compare twins from the same family to each other. In doing so, researchers can test whether twins who use more cannabis have, on average, higher levels of depression or suicidality. In a cotwin control study in Australia, twins who reported more frequent cannabis use were more likely to report MDD compared to less frequent users.44 Thus, cannabis may directly increase the risk for depression. Commensurate with family-based studies, research leveraging genome-wide data suggests that genetic risk for cannabis use is correlated with depression.45 Thus, genetic factors may account for some, but not all, of the association between cannabis use and depression.
Considering genetic and environmental factors is important in understanding the potential mechanism for these associations, although prior studies conducted in family samples report mixed outcomes. For instance, a twin study found that those who initiated cannabis use before 17 years of age had 3.5 times greater odds of attempting suicide but not of major depression or suicidal ideation.46 A separate twin study of Australian twins found that among monozygotic twins, only the exposed (cannabis-using) twin had higher rates of suicidal ideation, thus suggesting a more direct biological link between cannabis use and depression.44 Alternatively, the social context in which cannabis is used may include exposure to other substances, risky behaviors, and potentially adverse consequences of substance use that increase the likelihood of suicidal behavior.47 To this end, a longitudinal study conducted in Sweden found that cannabis use increased the risk of suicide among enlisted men by 62%, but the significance of the association disappeared after adjusting for covariates such as psychological or behavioral concerns.48
The findings presented herein are largely consistent with previous literature.19,46,49 A longitudinal study in Norway found that cannabis use in adolescence was selectively associated with significant increases in suicidal ideation and suicide attempts49; the authors hypothesize that increased impulsivity induced by cannabis use may set the stage for increased suicide risk. Similarly, a meta-analysis examining the association between cannabis use before the age of 18 years and subsequent depression, anxiety, and suicidal ideation during young adulthood found that those individuals who reported cannabis use had 1.4 times greater odds of depression, 1.5 times greater odds of suicidal ideation, and 3.4 times greater odds of suicide attempt later in life.19
The current study builds on this literature in several important ways. Previous reports have studied the impact of adolescent cannabis use on young adult and adult sequelae. The NCS-A is a unique resource designed to characterize epidemiologic factors associated with mental health disorders assessed with a valid diagnostic instrument, including degree of severity and impairment. The aforementioned studies did not consider the severity of depression. In addition, within this same cohort, we investigated multiple facets of the association between cannabis use and depression and suicidal behavior. These include lifetime and past−12-month reports of cannabis use and outcomes of interest; investigation of suicidal behavior individually as ideation, plan, and attempt; age of onset of cannabis use; and frequency of cannabis use. In addition, the large, nationally representative study design supports the significance and generalizability of the findings presented herein.
The findings of this study should be considered in the context of known limitations. Because of the cross-sectional study design, the temporal relationship between cannabis use and MDD is not clearly established, and we cannot determine causality in the relationships between cannabis use and MDD or suicidal behavior. Although evidence that any cannabis use increases the risk of depression and suicidal behavior is an important finding, further studies are needed to investigate the impact of problematic cannabis use and cannabis use disorder and the clinical course of adolescents with comorbid MDD. Further, the context in which data were collected should be considered. Specifically, these data were collected from 2001 to 2004, before cannabis legalization. However, as cannabis legalization has progressed, cannabis containing higher levels of THC has become increasingly potent. Thus, if cannabinoids such as THC are critical to the effects of cannabis on depression and suicidality, it may be expected that more potent products lead to more severe problems. The results presented herein that cannabis use is associated with depression severity and suicidal behavior in adolescents represent significant findings to support additional studies of the impact of these products on adolescent neurodevelopment and mental health.
In summary, the present study analyzed data from a nationally representative sample of adolescents. Findings were largely consistent with the extant literature that cannabis use is associated with depression. Notably, cannabis use was also associated with suicidal ideation, even after controlling depression. Additional studies are needed to adequately assess the temporal nature of the association between cannabis use and depression/suicidality. Finally, as recreational cannabis legalization expands, it is imperative to understand whether using higher-potency products further exacerbates this relationship.
Footnotes
The National Comorbidity Survey−Adolescent Supplement (NCS-A) and the larger program of related NCS surveys are supported by the National Institute of Mental Health (U01-MH60220) and the National Institute on Drug Abuse (R01 DA016558). Dr. Hinckley was supported by K12 DA000357. Dr. Mikulich-Gilbertson and Dr. Sakai were supported by R25 MH125758. Dr. Bhatia was supported by postdoctoral training grant T32 MH015442. Dr. Ellingson was supported by K23 AA026635 and by the Institute of Cannabis Research at Colorado State University (grant number 1100101). Dr. Merikangas and Ms. He were supported by the Intramural Research Program of the National Institute of Mental Health (ZIA MH002953-07). The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or US Government.
The research was performed with permission from the Colorado Multiple Institutional Review Board at the University of Colorado School of Medicine.
This study was presented as an abstract at the College on Problems of Drug Dependence 84th Annual Scientific Meeting; June 11-15, 2022; Minneapolis, Minnesota.
Dr. Mikulich-Gilbertson and Ms. He served as the statistical experts for this research.
Author Contributions
Conceptualization: Hinckley, Mikulich-Gilbertson, Sakai
Data curation: He, Merikangas
Formal analysis: Hinckley, Mikulich-Gilbertson
Methodology: Mikulich-Gilbertson, He, Merikangas, Sakai
Project administration: Hinckley
Writing – original draft: Hinckley, Mikulich-Gilbertson, Bhatia, Ellingson, Vu
Writing – review and editing: Hinckley, Mikulich-Gilbertson, He, Bhatia, Ellingson, Merikangas, Sakai
Disclosure: Dr. Hinckley has received research support from AACAP, NIDA, the University of Colorado Department of Psychiatry, and the Doris Duke Foundation. Dr. Mikulich-Gilbertson has received research support from the Colorado Department of Public Health and Environment, the Department of Veterans Affairs, NCI, NIDA, NIDDK, NIMH, and the University of Colorado Department of Psychiatry. Dr. Bhatia has received research support from NIMH. Dr. Ellingson has received research support from NIAAA, the Institute of Cannabis Research at Colorado State University Pueblo, and the University of Colorado Department of Psychiatry. Dr. Merikangas has received research support from NIDA and NIMH. Dr. Sakai has received research support from NIAAA, NIDA, NIMH, the Kane Family Foundation, and the Hewit Family Foundation. He received reimbursement in 2012 for completing a policy review for the WellPoint Office of Medical Policy & Technology Assessment (OMPTA), WellPoint, Inc. Dr. Vu and Ms. He have reported no biomedical financial interests or potential conflicts of interest.
Supplemental Material
Supplemental Figure 1.
References
- 1.Casey B.J., Jones R.M., Hare T.A. The adolescent brain. Ann N Y Acad Sci. 2008;1124:111–126. doi: 10.1196/annals.1440.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Avenevoli S., Swendsen J., He J.P., Burstein M., Merikangas K.R. Major depression in the National Comorbidity Survey-Adolescent Supplement: prevalence, correlates, and treatment. J Am Acad Child Adolesc Psychiatry. 2015;54(1):37–44. doi: 10.1016/j.jaac.2014.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.American Academy of Child and Adolescent Psychiatry Policy statement on suicide prevention; 2019. https://www.aacap.org/AACAP/Policy_Statements/2019/AACAP_Policy_Statement_on_Suicide_Prevention.aspx
- 4.Mason M., Mennis J., Russell M., Moore M., Brown A. Adolescent depression and substance use: the protective role of prosocial peer behavior. J Abnorm Child Psychol. 2019;47(6):1065–1074. doi: 10.1007/s10802-018-0501-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnston L.D., Meich R.A., O'Malley P.M., Bachman J.G., Schulenberg J.E., Patrick M.E. Institute for Social Research, University of Michigan; January 2021. Monitoring the Future National Survey Results on Drug Use, 1975-2020: 2020 Overview, Key Findings on Adolescent Drug Use.https://files.eric.ed.gov/fulltext/ED611736.pdf [Google Scholar]
- 6.Merikangas K.R., McClair V.L. Epidemiology of substance use disorders. Hum Genet. 2012;131(6):779–789. doi: 10.1007/s00439-012-1168-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Substance Abuse and Mental Health Services Administration (2020). Key substance use and mental health indicators in the United States: results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20-07-01-001, NSDUH Series H-55). Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/
- 8.Carrà G., Bartoli F., Crocamo C. Trends of major depressive episode among people with cannabis use: findings from the National Survey on Drug Use and Health 2006-2015. Subst Abus. 2019;40(2):178–184. doi: 10.1080/08897077.2018.1550464. [DOI] [PubMed] [Google Scholar]
- 9.Gukasyan N., Strain E.C. Relationship between cannabis use frequency and major depressive disorder in adolescents: findings from the National Survey on Drug Use and Health 2012-2017. Drug Alcohol Depend. 2020;208 doi: 10.1016/j.drugalcdep.2020.107867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Goldstein B.I., Shamseddeen W., Spirito A., et al. Substance use and the treatment of resistant depression in adolescents. J Am Acad Child Adolesc Psychiatry. 2009;48(12):1182–1192. doi: 10.1097/CHI.0b013e3181bef6e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cornelius J.R., Maisto S.A., Martin C.S., et al. Major depression associated with earlier alcohol relapse in treated teens with AUD. Addict Behav. 2004;29(5):1035–1038. doi: 10.1016/j.addbeh.2004.02.056. [DOI] [PubMed] [Google Scholar]
- 12.White A.M., Jordan J.D., Schroeder K.M., et al. Predictors of relapse during treatment and treatment completion among marijuana-dependent adolescents in an intensive outpatient substance abuse program. Subst Abus. 2004;25(1):53–59. doi: 10.1300/J465v25n01_08. [DOI] [PubMed] [Google Scholar]
- 13.Hersh J., Curry J.F., Becker S.J. The influence of comorbid depression and conduct disorder on MET/CBT treatment outcome for adolescent substance use disorders. Int J Cogn Ther. 2013;6(4):325–341. doi: 10.1521/ijct.2013.6.4.325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hinckley J.D., Riggs P. Integrated treatment of adolescents with co-occurring depression and substance use disorder. Child Adolesc Psychiatr Clin N Am. 2019;28(3):461–472. doi: 10.1016/j.chc.2019.02.006. [DOI] [PubMed] [Google Scholar]
- 15.Kandel D.B., Raveis V.H., Davies M. Suicidal ideation in adolescence: depression, substance use, and other risk factors. J Youth Adolesc. 1991;20(2):289–309. doi: 10.1007/BF01537613. [DOI] [PubMed] [Google Scholar]
- 16.Garrison C.Z., McKeown R.E., Valois R.F., Vincent M.L. Aggression, substance use, and suicidal behaviors in high school students. Am J Public Health. 1993;83(2):179–184. doi: 10.2105/ajph.83.2.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Negron R., Piacentini J., Graae F., Davies M., Shaffer D. Microanalysis of adolescent suicide attempters and ideators during the acute suicidal episode. J Am Academy Child Adolesc Psychiatry. 1997;36(11):1512–1519. doi: 10.1016/S0890-8567(09)66559-X. [DOI] [PubMed] [Google Scholar]
- 18.Gould M.S., King R., Greenwald S., et al. Psychopathology associated with suicidal ideation and attempts among children and adolescents. J Am Acad Child Adolesc Psychiatry. 1998;37(9):915–923. doi: 10.1097/00004583-199809000-00011. [DOI] [PubMed] [Google Scholar]
- 19.Gobbi G., Atkin T., Zytynski T., et al. Association of cannabis use in adolescence and risk of depression, anxiety, and suicidality in young adulthood: a systematic review and meta-analysis. JAMA Psychiatry. 2019;76(4):426–434. doi: 10.1001/jamapsychiatry.2018.4500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Han B., Compton W.M., Einstein E.B., Volkow N.D. Associations of suicidality trends with cannabis use as a function of sex and depression status. JAMA Network Open. 2021;4(6):e2113025. doi: 10.1001/jamanetworkopen.2021.13025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Merikangas K.R., Avenevoli S., Costello E.J., Koretz D., Kessler R.C. National Comorbidity Survey Replication Adolescent Supplement (NCS-A): I. Background and measures. J Am Acad Child Adolesc Psychiatry. 2009;48(4):367–379. doi: 10.1097/CHI.0b013e31819996f1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kessler R.C., Avenevoli S., Costello E.J., et al. Design and field procedures in the US National Comorbidity Survey Replication Adolescent Supplement (NCS-A) Int J Methods Psychiatr Res. 2009;18(2):69–83. doi: 10.1002/mpr.279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kessler R.C., Avenevoli S., Green J., et al. National Comorbidity Survey Replication Adolescent Supplement (NCS-A): III. Concordance of DSM-IV/CIDI diagnoses with clinical reassessments. J Am Acad Child Adolesc Psychiatry. 2009;48(4):386–399. doi: 10.1097/CHI.0b013e31819a1cbc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kessler R.C., Avenevoli S., Costello E.J., et al. National Comorbidity Survey Replication Adolescent Supplement (NCS-A): II. Overview and design. J Am Acad Child Adolesc Psychiatry. 2009;48(4):380–385. doi: 10.1097/CHI.0b013e3181999705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jensen P.S., Rubio-Stipec M., Canino G., et al. Parent and child contributions to diagnosis of mental disorder: are both informants always necessary? J Am Acad Child Adolesc Psychiatry. 1999;38(12):1569–1579. doi: 10.1097/00004583-199912000-00019. [DOI] [PubMed] [Google Scholar]
- 26.Grills A.E., Ollendick T.H. Issues in parent-child agreement: the case of structured diagnostic interviews. Clin Child Fam Psychol Rev. 2002;5(1):57–83. doi: 10.1023/a:1014573708569. [DOI] [PubMed] [Google Scholar]
- 27.Rao J.N.K., Scott A.J. On chi-squared tests for multiway contingency-tables with cell proportions estimated from survey data. Ann Stat. 1984;12(1):46–60. https://www.jstor.org/stable/2241033 [Google Scholar]
- 28.Rao J.N.K., Scott A.J. On simple adjustments to chi-square tests with sample survey data. Ann Stat. 1987;15(1):385–397. https://www.jstor.org/stable/2241089 [Google Scholar]
- 29.Mikulich-Gilbertson S.K., Wagner B.D., Grunwald G.K., Riggs P.D., Zerbe G.O. Using empirical Bayes predictors from generalized linear mixed models to test and visualize associations among longitudinal outcomes. Stat Methods Med Res. 2019;28(5):1399–1411. doi: 10.1177/0962280218758357. [DOI] [PubMed] [Google Scholar]
- 30.Hodgson K., Almasy L., Knowles E.E., et al. The genetic basis of the comorbidity between cannabis use and major depression. Addiction. 2017;112(1):113–123. doi: 10.1111/add.13558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bolton J.M., Robinson J., Sareen J. Self-medication of mood disorders with alcohol and drugs in the National Epidemiologic Survey on Alcohol and Related Conditions. J Affect Disord. 2009;115(3):367–375. doi: 10.1016/j.jad.2008.10.003. [DOI] [PubMed] [Google Scholar]
- 32.Chen C.Y., Wagner F.A., Anthony J.C. Marijuana use and the risk of major depressive episode. Epidemiological evidence from the United States National Comorbidity Survey. Soc Psychiatry Psychiatr Epidemiol. 2002;37(5):199–206. doi: 10.1007/s00127-002-0541-z. [DOI] [PubMed] [Google Scholar]
- 33.Lev-Ran S., Roerecke M., Le Foll B., George T.P., McKenzie K., Rehm J. The association between cannabis use and depression: a systematic review and meta-analysis of longitudinal studies. Psychol Med. 2014;44(4):797–810. doi: 10.1017/S0033291713001438. [DOI] [PubMed] [Google Scholar]
- 34.Moore T.H., Zammit S., Lingford-Hughes A., et al. Cannabis use and risk of psychotic or affective mental health outcomes: a systematic review. Lancet. 2007;370(9584):319–328. doi: 10.1016/S0140-6736(07)61162-3. [DOI] [PubMed] [Google Scholar]
- 35.Johnson E.C., Demontis D., Thorgeirsson T.E., et al. A large-scale genome-wide association study meta-analysis of cannabis use disorder. Lancet Psychiatry. 2020;7(12):1032–1045. doi: 10.1016/S2215-0366(20)30339-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bierhoff J., Haardorfer R., Windle M., Berg C.J. Psychological risk factors for alcohol, cannabis, and various tobacco use among young adults: a longitudinal analysis. Subst Use Misuse. 2019;54(8):1365–1375. doi: 10.1080/10826084.2019.1581220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Fu Q., Heath A.C., Bucholz K.K., et al. Shared genetic risk of major depression, alcohol dependence, and marijuana dependence: contribution of antisocial personality disorder in men. Arch Gen Psychiatry. 2002;59(12):1125–1132. doi: 10.1001/archpsyc.59.12.1125. [DOI] [PubMed] [Google Scholar]
- 38.Degenhardt L., Hall W., Lynskey M. The relationship between cannabis use, depression and anxiety among Australian adults: findings from the National Survey of Mental Health and Well-Being. Soc Psychiatry Psychiatr Epidemiol. 2001;36(5):219–227. doi: 10.1007/s001270170052. [DOI] [PubMed] [Google Scholar]
- 39.Degenhardt L., Hall W., Lynskey M. Exploring the association between cannabis use and depression. Addiction. 2003;98(11):1493–1504. doi: 10.1046/j.1360-0443.2003.00437.x. [DOI] [PubMed] [Google Scholar]
- 40.Gonzalez R. Acute and non-acute effects of cannabis on brain functioning and neuropsychological performance. Neuropsychol Rev. 2007;17(3):347–361. doi: 10.1007/s11065-007-9036-8. [DOI] [PubMed] [Google Scholar]
- 41.Chadwick B., Miller M.L., Hurd Y.L. Cannabis use during adolescent development: susceptibility to psychiatric illness. Front Psychiatry. 2013;4:129. doi: 10.3389/fpsyt.2013.00129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.King A. Prevention: neuropsychiatric adverse effects signal the end of the line for rimonabant. Nat Rev Cardiol. 2010;7(11):602. doi: 10.1038/nrcardio.2010.148. [DOI] [PubMed] [Google Scholar]
- 43.Rutter M., Pickles A., Murray R., Eaves L. Testing hypotheses on specific environmental causal effects on behavior. Psychol Bull. 2001;127(3):291–324. doi: 10.1037/0033-2909.127.3.291. [DOI] [PubMed] [Google Scholar]
- 44.Agrawal A., Nelson E.C., Bucholz K.K., et al. Major depressive disorder, suicidal thoughts and behaviours, and cannabis involvement in discordant twins: a retrospective cohort study. Lancet Psychiatry. 2017;4(9):706–714. doi: 10.1016/S2215-0366(17)30280-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Hodgson K., Coleman J.R.I., Hagenaars S.P., et al. Cannabis use, depression and self-harm: phenotypic and genetic relationships. Addiction. 2020;115(3):482–492. doi: 10.1111/add.14845. [DOI] [PubMed] [Google Scholar]
- 46.Lynskey M.T., Glowinski A.L., Todorov A.A., et al. Major depressive disorder, suicidal ideation, and suicide attempt in twins discordant for cannabis dependence and early-onset cannabis use. Arch Gen Psychiatry. 2004;61(10):1026–1032. doi: 10.1001/archpsyc.61.10.1026. [DOI] [PubMed] [Google Scholar]
- 47.Wodak A., Reinarman C., Cohen P.D., Drummond C. Cannabis control: costs outweigh the benefits. For. BMJ. 2002;324:105–106. doi: 10.1136/bmj.324.7329.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Price C., Hemmingsson T., Lewis G., Zammit S., Allebeck P. Cannabis and suicide: longitudinal study. Br J Psychiatry. 2009;195(6):492–497. doi: 10.1192/bjp.bp.109.065227. [DOI] [PubMed] [Google Scholar]
- 49.Pedersen W. Does cannabis use lead to depression and suicidal behaviours? A population-based longitudinal study. Acta Psychiatr Scand. 2008;118(5):395–403. doi: 10.1111/j.1600-0447.2008.01259.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.