Abstract
Objective
To provide the best clinical practice guidance for surfactant use in preterm neonates with respiratory distress syndrome (RDS). The RDS-Neonatal Expert Taskforce (RDS-NExT) initiative was intended to add to existing evidence and clinical guidelines, where evidence is lacking, with input from an expert panel.
Study design
An expert panel of healthcare providers specializing in neonatal intensive care was convened and administered a survey questionnaire, followed by 3 virtual workshops. A modified Delphi method was used to obtain consensus around topics in surfactant use in neonatal RDS.
Result
Statements focused on establishing RDS diagnosis and indicators for surfactant administration, surfactant administration methods and techniques, and other considerations. After discussion and voting, consensus was achieved on 20 statements.
Conclusion
These consensus statements provide practical guidance for surfactant administration in preterm neonates with RDS, with a goal to contribute to improving the care of neonates and providing a stimulus for further investigation to bridge existing knowledge gaps.
Subject terms: Paediatrics, Respiratory tract diseases
Introduction
Respiratory distress syndrome (RDS) in neonates is often defined as respiratory distress occurring within 6 h of birth and associated with radiographic features of a reticular-granular pattern, low lung volumes, and air bronchograms and is caused by an inadequate amount of surfactant [1]. Other definitions use clinical signs and symptoms rather than radiographic data to confirm diagnosis. Although treating neonatal RDS with exogenous surfactant is lifesaving, the variability in criteria used to make the diagnosis contributes to the lack of consensus on treatment thresholds. Surfactant replacement therapy has been demonstrated to improve clinical outcomes, including reductions in mortality risk and risk of air leaks, in neonates with RDS [2, 3].
Guidelines in the US published by the American Association for Respiratory Care (AARC) and the American Academy of Pediatrics (AAP) were last updated almost 10 years ago, in 2013 and 2014, respectively [4, 5]. More recent international guidelines have been published, including the European Consensus Guidelines on the Management of RDS: 2022 Update, the Turkish Neonatal Society Guidelines in 2019, and the Canadian Paediatric Society Position Statement Guideline in 2021 [6–8]. In addition, many neonatal intensive care units (NICUs) create and adhere to their own protocols at the institutional level, for example, the Royal Children’s Hospital, Starship Children’s Hospital, and Alaska Native Medical Center [9–11]. Recent reviews summarize current research and complement existing guidelines [12–14].
Variability among these guidelines demonstrates a lack of consensus concerning surfactant use and administration in the neonatal setting. Variation exists at the institutional level in the management of neonates with RDS, including neonates born at increasingly lower gestational ages, mode of administration (as new, less-invasive, methods are being developed), timing of administration, repeat dosing, and infant positioning during administration of surfactant. Gaps in evidence and shortcomings of existing randomized clinical trials (RCTs) further complicate bedside decision-making, leaving clinicians on their own to answer important questions about the patients for whom they care in the NICU.
The objective of the Respiratory Distress Syndrome Neonatal Expert Taskforce (RDS-NExT) initiative was to define the most-effective practice strategies pertaining to neonatal surfactant use and administration, specifically in preterm neonates with RDS. We approached this by convening a panel of leading experts practicing in varying acuity level NICUs from various regions of the US, in an effort to establish consensus on best clinical surfactant practice. This was accomplished by utilizing a modified Delphi method [15]. The output of this initiative was not intended to replace existing evidence and clinical guidelines; rather, the goal was to fill in the gaps where evidence is lacking, with input from expert opinion leaders, in order to improve the care of neonates with RDS or at high-risk of developing RDS.
Methods
Independent external consultants (RB, SH, RS, and PR) worked with the committee chair (VB), to generate a list of 33 health care providers (HCPs), including physicians/neonatologists (MDs), nurse practitioners (NPs), and registered respiratory therapists (RRTs), who specialize in neonatal care and administer surfactant routinely in their NICU from published literature, known key opinion leaders, and Delphi method facilitators. The expert panel was selected from this list to include providers from academic, university-affiliated practices, as well as private practice NICUs from various regions in the US.
A targeted review of literature concerning surfactant administration in neonates with RDS was conducted. This was used to inform the development of a web-based survey led by the committee chair (VB) in collaboration with independent external consultants with expertise in Delphi methodology (RB, SH, RS, and PR). The survey consisted of 29 open-ended and 9 multiple-choice questions (Supplementary Table A) and was distributed to panelists using the Survey Monkey platform in advance of the first workshop. Results from the survey were used to develop initial proposed statements around areas of interest that lacked consensus. Statements were divided into 3 sections: Section 1: establishing RDS diagnosis and indicators for surfactant administration; Section 2: surfactant administration methods and techniques; and Section 3: other considerations.
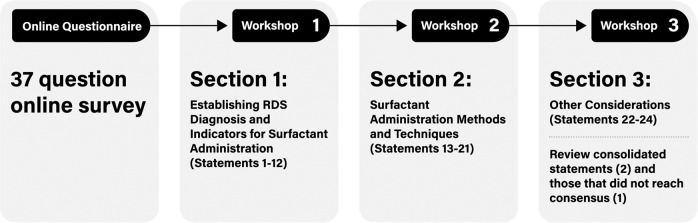
A modified Delphi method was used to obtain expert consensus over the course of 3 live, virtual workshops, during which potential consensus statements were deliberated (Fig. 1). Deliberations sometimes continued thereafter as well. During the workshops, proposed statements were reviewed and discussed. Each initial statement was presented to the group, with relevant data provided by panelists in response to the survey questionnaire. Statements were discussed and modified until panelists moved to vote, selecting their choice on a 5-point Likert scale (strongly disagree, disagree, neutral, agree, or strongly agree). Panelists anonymously submitted their vote for each statement, which was recorded. Consensus was defined a priori as 80% of panelists selecting agree or strongly agree. Section 1 statements were voted on in workshop 1 (April 7, 2022). Section 2 statements were voted on in workshop 2 (April 12, 2022). Section 3 statements were voted on in workshop 3 (May 24, 2022), along with redundant statements from workshops 1 and 2 that were consolidated and statements that did not reach consensus (Fig. 2). In advance of workshop 3, proposed statements were sent out to panelists and feedback was obtained ahead of the meeting. This feedback was incorporated into the proposed statements in advance of workshop 3.
Fig. 1. An overview of the modified Delphi process.
The figure illustrates the sequence of the initial questionnaire survey, followed by 3 workshops that covered the 3 sections of the RDS guidelines.
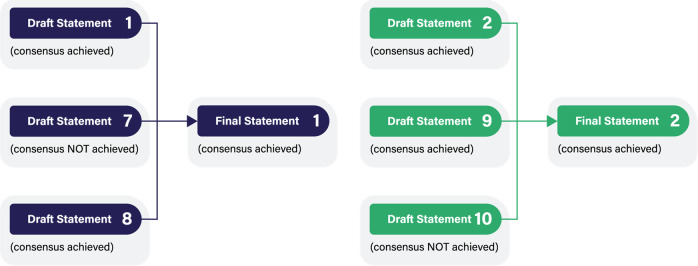
Fig. 2. An overview of the consolidation of draft statements into final statements*.
The figure illustrates the process of achieving consensus for the specific statements. *Draft Statements 1, 7, and 8 were consolidated into Final Statement 1. Draft Statements 2, 9, and 10 were consolidated into Final Statement 2.
After completion of the 3 workshops, consensus statements and voting results were compiled, and after the receipt of absentee votes, sent out to panelists. During the course of the workshops, panelists discussed the need for additional detailed information regarding the indications for surfactant use. A subcommittee of volunteers from among the workshop panelists was convened to describe parameters and clinical scenarios for which surfactant is indicated for preterm infants with RDS.
Results
Of the 15 HCPs contacted, 10 agreed to serve on the expert panel. Of these, 9 panelists completed the survey. All 11 panelists (10 plus the committee chair) participated in workshops 1 and 2. Two panelists were unable to attend workshop 3 due to scheduling conflicts, so absentee votes for these panelists were obtained via email. Names of participating panelists can be found in Supplementary Table B.
A total of 24 statements was discussed, refined, and voted on over the 3 workshops. Consensus was achieved on 20 statements. The original statements presented to the group, as well as the final statement and voting results, can be found in Supplementary Table C. The final consensus statements are listed below. They are followed by the panelists’ reasons for agreeing or disagreeing with the statements, as well as their limitations and applicability to clinical practice.
Section 1: Establishing RDS diagnosis and indicators for surfactant administration
Statement 1 (consolidated from original statements 1, 7, and 8; see Supplementary Table C): When the clinical decision has been made to administer surfactant, preterm infants with RDS should receive surfactant early (≤2 h of life), preferably within 1 h of life.
A review by Bahadue et al. concluded that early selective surfactant administration within the first 2 h of life (throughout this manuscript, life is used to denote extrauterine life) in neonates with RDS requiring assisted ventilation decreased the risk of mortality, acute pulmonary injury, and chronic lung disease compared to delayed treatment [16]. Some panelists expressed uncertainty about the 2 h limit. Variability in timing of treatment with surfactant replacement therapy and disease severity of patients included in clinical trials have left clinicians with uncertainty regarding the optimal timing of surfactant treatment [16]. Furthermore, a review that included more-recent trials demonstrating current clinical practice concluded that prophylactic use of surfactant, when compared to routine stabilization using continuous positive airway pressure (CPAP), does not improve clinical outcomes and may increase the risk of chronic lung disease or death [17].
Panelists also discussed the applicability of this statement to various patient populations, including neonates of ≥30 weeks’ gestational age (GA), extremely preterm infants (<28 weeks’ GA) and low birth weight neonates requiring CPAP.
Statement 2 (consolidated from original statements 2, 9, and 10; see Supplementary Table C): For preterm infants with RDS receiving positive pressure support, an elevated and increasing fraction of inspired oxygen (FiO2) is an important indicator of the need for surfactant treatment based on administration criteria; other clinical measures of respiratory distress and/or support, alone or in combination, may precede and preempt FiO2 as an indication of need for surfactant treatment.
There was a significant amount of discussion regarding identifying a specific FiO2 threshold for surfactant administration, as the evidence is inconsistent. The 2022 European Consensus Guidelines recommendations state that a FiO2 of >0.3 be used as a cutoff for surfactant administration for all babies with a clinical diagnosis of RDS, especially in the early phase of worsening disease [6]. Other studies have also utilized a FiO2 threshold of 0.3 [18, 19]; however, the populations included in studies supporting this cutoff are not generalizable to the entire population of neonates with RDS. The 0.3 FiO2 criterion was derived from observational studies (of CPAP failure, etc.) [18–21]. The need for a specific FiO2 threshold spurred much discussion among the group and resulted in the development of the surfactant indicator table (Table 1). Additional considerations included the type of support the infant is on, the surfactant delivery technique (invasive vs less invasive), clinical parameters, and differences in resources available, as per NICU level of care.
Table 1.
Surfactant indicator table. Considerations for Surfactant Administration for RDSa (Need to fulfill at least 3 of 4 criteria).
| Gestational age | 23 0/7–27 6/7 Weeks |
28 0/7–36 6/7 Weeks |
|---|---|---|
|
Clinical status (Downes’ Scoreb) |
4–7 | 4–7 |
| Respiratory support status |
Intubated at any timec OR NIPPV: MAP ≥ 6; CPAP ≥ 6 |
Intubated at any timec OR NIPPV: MAP ≥ 7; CPAP ≥ 7 |
| FiO2 requirementd,e |
≥0.3 if early (≤2 h of life) OR ≥0.4 if late (>2 h of life) |
≥0.3 if early (≤2 h of life) OR ≥0.4 if late (>2 h of life) |
| Blood gas statusf | pH <7.25, pCO2 > 60 | pH <7.25, pCO2 > 60 |
EARLY (≤2 h of life); LATE (>2 h of life).
CPAP continuous positive airway pressure, ETT endotracheal tube, INSURE INtubation-SURfactant-Extubation, FiO2 fraction of inspired oxygen, LISA less-invasive surfactant administration, LMA laryngeal mask airway, MAP mean airway pressure, MIST minimally invasive surfactant administration, NIPPV nasal intermittent positive pressure ventilation, pCO2 partial pressure of carbon dioxide, RDS respiratory distress syndrome, SpO2 oxygen saturations (pulse oximetry).
aHistory, signs, and symptoms consistent with surfactant deficiency.
bDetails of the Downes’ scoring system is shown in Supplementary Table D. Briefly, includes 0-2 points each for Respiratory Rate (60, 60–80, 80), Retractions (0, mild, severe), Cyanosis (no in room air, relieved by O2, yes even with O2), Air Entry (good, mildly decreased, none), Grunting (non, w/stethoscope, audible).
cIf infant is intubated for resuscitation or meets other clinical parameters for surfactant administration, consider giving surfactant before extubating.
dTo maintain a preductal SpO2 of 90–95%. Infants transitioning to extrauterine life and stable on CPAP in the delivery room may require a higher FiO2 temporarily that may not necessarily warrant surfactant administration. Severe respiratory distress, even with a lower FiO2, may warrant earlier surfactant administration.
eEvaluate the risk of the intervention for surfactant administration (via LISA-MIST/INSURE/LMA vs ETT), followed by the risk of exposure to invasive mechanical ventilation.
fArterial or capillary blood gas, only if available.
The type of support the infant is on (e.g., CPAP vs mechanical ventilation) should be considered. The use of a lower threshold negates the work from the COIN and SUPPORT trials for noninvasive ventilation (NIV) alone, as these studies suggest that a substantial number of babies can be supported on CPAP and a higher level of oxygen [22, 23]. It must be recognized that a lower FiO2 criterion results in earlier treatment in babies with true surfactant deficiency; however, it also increases exposure to risks associated with surfactant administration in the subset of babies who would have never met treatment threshold if the FiO2 criteria were set higher.
This balance of risk vs benefit is also necessarily dependent on the risk profile associated with the different modes of surfactant administration. When administered via an endotracheal tube (ETT) followed by invasive mechanical ventilation (IMV), a higher FiO2 threshold may be more appropriate. A lower threshold may be more appropriate when an infant is on NIV and surfactant is administered and not followed by IMV, such as with less-invasive surfactant administration (LISA), INtubation-SURfactant-Extubation (INSURE), minimally invasive surfactant administration (MIST), or laryngeal mask airway (LMA) surfactant delivery. When the need for surfactant administration comes with a high likelihood of prolonged mechanical ventilation if an ETT is placed or a practitioner is not comfortable with the use of LISA and/or LMA to deliver surfactant, then a higher threshold of FiO2 may be preferred [14, 24].
Clinical parameters should also be considered. However, work of breathing (WOB) is very subjective and has not been studied alone.
Differences in access to resources as per NICU level of care and how elevation (altitude) of the NICU site impacts FiO2 requirement need to be considered as well.
Statement 3. Chest x-ray (CXR) confirmation for RDS diagnosis is suggested but not required prior to surfactant administration.
CXRs can be useful to rule out pneumothorax; however, a CXR may not be available during transport or when resources are limited (e.g., night shift) and could cause delays in surfactant administration. Recent approaches with no radiation exposure, such as lung ultrasound, do not require CXR for confirmation of the diagnosis of RDS [25–31].
Statement 4. The most important predictors for determining the need for surfactant in preterm infants with RDS are GA, FiO2 requirement and clinical signs and symptoms with supporting investigations (e.g., CXR, blood gases).
The biggest predictor for RDS is GA [32–34]; however, the biggest predictor for noninvasive ventilation failure is FiO2 [18–20].
Statement 5. A second or third dose of surfactant may be necessary for ongoing RDS depending on clinical factors (e.g., lack of improvement, FiO2 requirement, increased WOB, or continued need for mechanical ventilation).
Limited data exist around indications or outcomes for repeat doses [35–37]. Findings from a review by Soll et al. suggest that infants with ongoing respiratory insufficiency who received multiple doses of surfactant had better clinical outcomes than those who received single dosing [38]. Repeat doses, in accordance with manufacturer’s guidelines, may be necessary in some situations and should not be discouraged or delayed, if clinically indicated.
Statement 6. Based on current data, GA alone should not be the sole criterion for surfactant administration.
The decision to administer surfactant should not be based on GA alone. No data exist for dosing solely based on GA; however, the younger the GA of the infant, the higher the risk for RDS and noninvasive respiratory support failure [39]. RCTs comparing initial stabilization on CPAP vs intubation in babies born at <28 weeks’ GA demonstrate that a significant majority (~50–70%) of those managed on CPAP will receive surfactant [22, 40]. Results from a German study are comparable [41].
As discussed in Statement 2, the risk-benefit profile of the mode of administration should be considered. Specifically, surfactant administered via ETT, followed by exposure to IMV potentially carries a higher risk profile than administration via LISA, MIST, INSURE, or LMA [42]. Meta-analyses suggest that LISA is superior to the INSURE technique in terms of avoidance of BPD and IVH [41]. Furthermore, the GA of the baby independently modifies the risk profile associated with mode of administration. For example, chronic lung disease affects lower GA infants at higher rates [43]. Given the relationship between IMV and chronic lung disease [44], the risk of adverse outcomes increases among lower GA infants administered surfactant via ETT followed by IMV. A recently published article showed that LISA in the delivery room is routine practice in Germany for infants <27 weeks’ GA [45]. There is an ongoing single-center study to evaluate delivery room LISA vs NICU LISA [46].
Additionally, extremely early GA should be considered, as infants at 22–23 weeks’ gestation have almost universally been shown to fail CPAP [47].
Statement 7 (originally 11; see Supplementary Table C): Additional studies are needed to assess the role of lung ultrasound and clinical respiratory scoring as adjunct tools in determining the need for surfactant administration for non-intubated infants with RDS.
Although more popular in Europe, use of lung ultrasound is becoming more commonplace in the US [48–50]. An early high lung ultrasound score correlates with the need for surfactant administration in preterm neonates with RDS [51]. Lung ultrasound score has also been correlated with oxygenation status and may help predict bronchopulmonary dysplasia (BPD) [52].
Many methods to assess the severity of respiratory distress exist, including Downes’ score [53], Silverman Anderson [54], and the Respiratory Severity Score; there is no consensus on which is the ideal scoring system [55–57]. Use of these tools should not delay therapy.
Statement 8 (originally 12; see Supplementary Table C): Barriers to the timely administration of surfactant may be due to limited availability of appropriately skilled staff and/or resources (e.g., delay in diagnosing RDS and timely transport to a regional center).
Barriers to timely surfactant administration include limited availability of appropriately skilled staff (ability to intubate, familiarity with less-invasive methods of surfactant administration) and/or resources (equipment and surfactant medication), as well as delays in diagnosing RDS (need for confirmatory radiological exams, transport to a regional center) [58].
These barriers may not be an issue for NICUs providing level III or higher care; however, it is unknown how often surfactant is delayed in other settings, as data do not exist.
Section 2: Surfactant administration methods and techniques
Statement 9 (originally 13; see Supplementary Table C): Surfactant can be administered using equipment based on the provider’s experience/skill level, preference, and institutional practice.
The type of equipment used for surfactant administration may influence procedure duration, number of attempts, accuracy of dose delivery, and need to interrupt the delivery of positive pressure during the procedure; however, no RCTs have been performed to determine the optimal delivery method. Designing such a trial would be difficult and would require consideration of the environment, the skill level of the operator, and the target patient population. Kribs et al. report findings from a non-blinded study that compared outcomes among infants who received surfactant via a thin endotracheal catheter during CPAP-assisted spontaneous breathing (LISA; intervention group) vs those who received surfactant after conventional endotracheal intubation during mechanical ventilation (control group) [59]. The primary outcome, survival without BPD, was not demonstrated; however, some of the secondary endpoints (rates of successful application and number of attempts, duration of mechanical ventilation, etc.) demonstrated important safety benefits associated with LISA administration. Infants who received surfactant via the LISA method were less frequently intubated (80 infants [74.8%] vs 103 [99.0%]; P < 0.001) and required fewer days of mechanical ventilation compared to those in the control group. The groups had a similar number of surfactant doses per infant and more than 1 attempt for successful surfactant administration was needed in 27% of the infants in both groups [59]. In a consensus guideline for LISA, Reynolds et al. concluded that LISA can be a safe method, with the potential to improve outcomes for premature neonates [60]. In a recent RCT, MIST therapy compared with sham (control) treatment did not significantly reduce the incidence of the primary composite outcome of death or BPD, though the incidence of BPD was significantly lower in the MIST group (P = 0.03) [61]. Further, a meta-analysis comparing different surfactant strategies concluded that administration of surfactant via thin catheter, compared with ETT administration, was associated with a reduced risk of BPD/death, fewer patients intubated in the first 72 h, and reduced incidence of morbidities and in-hospital mortality [62]. The above data suggest that treatment with surfactant via thin catheter may be preferable to ETT administration; however, additional studies of adequate size and power are needed to confirm these findings [62]. Furthermore, given subgroup differences observed in some of the RCTs referenced above, whether the protective effect of LISA/MIST varies across GA strata remains to be determined.
Statement 10 (originally 14; see Supplementary Table C): Routine repositioning during surfactant administration may not improve the distribution of surfactant relative to maintaining the infant supine; repositioning may increase the risk of device malposition.
There are no RCTs comparing response with repositioning of the infant during surfactant administration. Uncertainty exists around distribution of surfactant within the lungs and safety concerns arise with the repositioning of a critically ill infant. In a recent survey of US HCPs, 44% turn or reposition the infant during surfactant administration [63]. Manufacturer guidelines are available as they relate to infant positioning [64–66].
Preclinical data in a lamb model demonstrate that 1 aliquot of exogenous surfactant administered via the ETT distributes evenly without repositioning. There are data for 4 vs 2 doses, with no differences seen [67]; however, similar data in humans do not exist.
Statement 11 (originally 15; see Supplementary Table C): Surfactant can be administered as a single bolus or divided aliquots, based on provider preference, mode of administration, manufacturer recommendation, and clinical considerations.
Some centers may defer to manufacturer recommendations, which recommend using multiple aliquots [64–66]. There was an RCT comparing 2 aliquots vs 4 aliquots of Survanta®. It showed no major differences [68]; however, the studies were conducted more than 20 years ago and may not be applicable to current NICU populations. In a recent survey of US HCPs, 50% said they use 2 aliquots; 32%, a single bolus dose; 7%, >2 aliquots; and 11% reported “other” [63]. The rationale most often provided for using the single bolus dose was tolerability and maintaining the infant in a neutral position. For providers who use 2 aliquots, historical practice was most frequently noted, with tolerability being second most common rationale. HCPs who reported “other” mentioned type of surfactant used, location, GA/weight, and clinical presentation in determining how to administer surfactant. Bolus administration of surfactant is preferred when given via the ETT; using the LISA approach, surfactant administration can usually to be completed in <1 min, though it might require more time if apnea/bradycardia/surfactant reflux occur [8, 69, 70].
Statement 12 (originally 16; see Supplementary Table C): When using the INSURE technique to administer surfactant, infants should be extubated as soon as possible.
The AAP guidelines do not give a time recommendation for extubation after surfactant administration via INSURE – just that it should be rapid [5]. The experts agreed that the most likely protective effect gained through administration via INSURE is limited IMV exposure. Some centers do not specify when to extubate after surfactant administration after the INSURE procedure has been completed. If premedications were used with the INSURE technique, such as sedative and/or paralyzing agents, this may influence timing of extubation after surfactant has been administered.
Statement 13 (originally 17; see Supplementary Table C): For spontaneously breathing infants with RDS on CPAP for whom the decision to give surfactant has been made, less-invasive methods of surfactant administration may be appropriate alternatives to the INSURE technique.
In a network meta-analysis, Isayama et al. reported that the use of LISA was associated with a lower likelihood of the primary outcome of death or BPD than was mechanical ventilation or nasal CPAP alone. INSURE was associated with a lower likelihood of death or BPD than was mechanical ventilation or nasal CPAP alone. Ranking probabilities supported LISA as the best among all strategies for all outcomes assessed. INSURE tied with nasal intermittent positive pressure ventilation as the second-best strategy to prevent death or BPD [71]. However, the authors judged the quality of evidence of the meta-analysis to be low because the sample size of all included studies did not reach the optimal information size [71]. The limitations of the OPTIMIST-A trial comparing MIST vs CPAP and the LMA vs INSURE trials must be acknowledged [61, 72]. A consensus guideline from the UK has suggested that LISA has the potential to “improve outcomes” for preterm infants with RDS [60]. Although promising, these reports are not definitive and may not be applicable in certain GA categories. The consensus of this expert panel was that a single approach does not fit all NICU sites/scenarios. At the current time, the choice of delivery method should be made with careful consideration of the environment, resources available, operator experience, and patient characteristics, including GA and degree of illness. The clinician caring for the infant should choose which method of surfactant administration is most appropriate. It is likely that additional studies will further inform this practice.
Statement 14 (originally 18; see Supplementary Table C): For preterm infants with RDS with adequate respiratory effort on CPAP (not requiring IMV), LISA/MIST are appropriate less-invasive options for surfactant administration based on provider experience and institutional practice.
There is emerging evidence for LISA/MIST modes of administration of surfactant to be considered preferential [14, 45, 71, 73, 74]. It is important to note that most studies of these modes of surfactant delivery included early treatment at relatively low thresholds for administration (e.g., FiO2 of 0.3) and they have not been studied for rescue delivery in unstable neonates.
A meta-analysis of 6 RCTs comparing surfactant administration utilizing LISA vs standard endotracheal administration showed a reduction in the composite outcome of death or BPD, BPD among survivors, and need for mechanical ventilation at 72 h and at any time during the NICU course. There were no differences found in death or other neonatal morbidities. Three of the six studies included patients <28 weeks, with one including 23-week preterm infants [75].
Statement 15 (originally 19; see Supplementary Table C): Surfactant administration via supraglottic airway devices (e.g., LMA) may benefit certain populations of preterm infants and is a promising method of surfactant administration.
A study by Roberts et al. found that infants of 28 0/7–35 6/7 weeks gestational age and with birth weights ≥1250 g who received surfactant via LMA had a decreased rate of intubation and mechanical ventilation compared with controls (38% vs 64%; OR: 0.30 [95% CI, 0.13–0.70]; P = 0.006) [72]. A recent meta-analysis of 6 RCTs found that administering surfactant via LMA was associated with decreased FiO2 requirement, decreased intubation, and decreased mechanical ventilation [76]. A recent study comparing LMA to INSURE in infants of 27–36 weeks’ gestation and weighing >800 g found surfactant therapy via LMA was non-inferior to INSURE for efficacy and that LMA administration decreased early failures, possibly by avoiding adverse effects of premedication, laryngoscopy, and intubation [77]. Notably, both groups received atropine premedication while only the INSURE group received remifentanil premedication.
Statement 16 (originally 20; see Supplementary Table C): More data are required to evaluate the use of the promising technique of aerosol administration of surfactant.
Although aerosolization is the most noninvasive of all methods of surfactant administration, studies have historically been unable to show improvement in respiratory status [78–83]. A recent study was the first to show benefit, with a reduction in intubation and surfactant via endotracheal instillation of nearly one-half (26% in the aerosol group and 50% in the usual care group; P < 0.0001) [84]. There is currently no US Food and Drug Administration–approved device available.
Statement 17 (originally 21; see Supplementary Table C): Device development research and more experience with novel methods of surfactant administration (e.g., LMA, aerosol) is needed for smaller, less-mature infants.
The study by Roberts et al. included only infants of 28 0/7–35 6/7 weeks’ gestation and weighing ≥1250 g [72]. LMAs are currently available only for infants weighing ≥1250 g. Devices appropriate for smaller infants are needed.
Section 3: Other considerations
Statement 18 (originally 22; see Supplementary Table C): Premedication usage for surfactant administration depends on the method of administration. Pain management, physical discomfort, procedural success, and minimization of adverse events are all considerations around premedication usage in surfactant administration.
Discrepancies in the use of premedication prior to surfactant administration exist across clinical institutions [63, 85–88]. While early caffeine has been recommended, the exact timing of caffeine initiation has not been specified [89]; more research is needed in this area [90, 91].
Statement 19 (originally 23; see Supplementary Table C): More studies are needed to evaluate the safety and efficacy of sucrose use as a premedication prior to administration of surfactant.
Oral sucrose solution has been used as a pain medication with LISA/MIST [14] and LMA [72] administration of surfactant.
Statement 20 (originally 24; see Supplementary Table C): Intravenous (IV) atropine is not routinely used for less-invasive methods of surfactant administration.
IV atropine has been used to minimize bradycardia during nonurgent intubation and/or LISA [92, 93]. Use of atropine may mask prolonged hypoxia. This risk is related to the use of laryngoscopy. Ultimately, surfactant administration should not be delayed just for the purpose of establishing IV access for atropine administration.
Discussion
Consensus statements for the use of surfactant in infants with RDS were generated utilizing a modified Delphi method. This is a standard methodology to obtain consensus from a group of experts and has been used by neonatal specialists in the UK to generate consensus statements for surfactant replacement therapy in RDS [94]. It has also been used in other therapeutic areas [95–97]. Consensus statements are usually needed when clinical evidence, such as clinical trial data, is lacking regarding treatment decisions, when guidelines may not reflect current clinical practice, or when there are no acceptable standard practice methods. A study by Patel et al. reported the results of interviews with 54 HCPs (neonatologists, NPs, and RRTs) on how they administered surfactant therapy in infants with RDS; the authors concluded that there were no standard practices in respiratory management and surfactant administration [63]. This highlights the need for recommendations such as the consensus statements generated by the RDS-NExT panel to help clinicians better manage RDS when surfactant administration is indicated.
The consensus statements developed by the RDS-NExT panel are not meant to replace guidelines, which are usually developed based on strong clinical evidence, but instead are intended to supplement the guidelines with prevailing clinical practice standards used by experienced clinicians and researchers. Merging clinical practice with available data can help advance neonatal practice and improve patient care.
Given the variability in the criteria (clinical signs and symptoms, with or without radiographic features) used for the diagnosis of RDS, clinicians are left to use proxies to determine the need for surfactant treatment. These include FiO2 requirement and level of noninvasive pressure support needed to maintain cardiorespiratory stability. These topics generated vigorous discussion among the panelists.
Establishing a FiO2 cutoff value was a subject of much debate. Some panelists felt that using 0.3 as a minimum cutoff value was inappropriate because other important factors that should be considered might lead a clinician to treat with surfactant at a lower FiO2. These included the GA of the baby and the subsequent risk of chronic lung disease, the type and level of respiratory support the infant is receiving, the surfactant delivery technique and associated risk profile of administration, clinical parameters (including history of antenatal corticosteroid administration and cardiovascular stability), and the level of NICU care being provided at a particular site. Although a specific value was not included in a consensus statement, the surfactant indicator table (Table 1) includes a range (0.3–0.4), depending on whether the infant is within 2 h of life (early) or more than 2 h (late) after birth. The primary goal is early and appropriate treatment of infants whose respiratory distress is caused by surfactant deficiency. A similar debate was had regarding the appropriate positive pressure cutoff value. Panelists felt that too many other factors needed consideration, for example that use of a higher CPAP would decrease the FiO2 requirement. Given these complex clinical relationships, a range (6 vs 7 MAP/CPAP or higher) was ultimately included in the surfactant indicator table (Table 1).
Finally, the panel discussed surfactant administration modes at length. This issue is critically important, and any risk associated with surfactant delivery can blunt its powerful treatment effect. A recent review suggests that minimally invasive methods of surfactant administration have the potential for widespread use in the US because of the associated improved neurodevelopmental outcomes [14]. Evidence on LMA administration is emerging [72, 98]. Aerosolized surfactant is an area of active study [81, 99]. Knowledge gained in these areas through further study will likely refine our use of surfactant in the upcoming years.
The surfactant indicator table was generated with the goal of including a range of clinical presentations, with a level of detail that was not possible to include in the 20 consensus statements. It is the hope of the authors that this table can be used to provide guidance for the use of surfactant in preterm neonates with RDS at individual institutions. Developed in 1970, the Downes’ respiratory scoring system [53] is still in use; however, it has not been standardized for use in extremely preterm neonates. Despite this and consideration of other clinical scoring systems [54], the Downes’ scoring system was selected because it correlates well with blood gas analysis and degree of distress and is used in clinical practices around the world [100–105].
The goal of developing these consensus statements was to consider the general neonatal RDS patient population; therefore, clinical outliers are not discussed. It was not feasible to take into account variations in treatment for the entire spectrum of clinical presentations. It is important to highlight the fact that individual clinical parameters and resources available at a specific site should always be taken into account when considering the indication and mode of surfactant administration. How these factors apply to a particular institution may vary at community and private practices and academic centers. Furthermore, transport availability is a factor that needs to be considered when applying this guidance.
There are some limitations. The initial literature review used to develop the statements for expert review was neither exhaustive nor systematic. In addition, while many important factors regarding the administration of surfactant to neonates with RDS were discussed, other important factors, such as type and dose of surfactant, were not included due to time constraints. Key repetitive themes were identified in the recent literature and these issues were supplemented with unbiased, anonymous input from key opinion leaders, based on their expertise. These comments were collated and provided for all panelists to review. Responses to the survey were anonymous and reviewed by the entire panel, with a trained facilitator allowing all voices to be heard in the 3 live, virtual workshops. Voting at each stage of the virtual workshops was anonymous and was then discussed as a group and edited live by the panelists. This methodology allowed for frank, inclusive input and dialog among all panelists.
Consensus on some statements was difficult to achieve, given the lack of published data and variation in practice methods among the panelists and their home institutions. The panelists considered data from RCTs, review articles, manufacturer recommendations (which are from 2 to 3 decades ago and may not necessarily reflect current practice), and personal experience/preference to develop the final statements.
A key strength was the experienced group of neonatologists plus inclusion of an experienced RRT and NP. These experts, from fairly diverse geographic regions and practice parameters in a wide array of private practice and academic settings, provided information regarding the use of surfactant in preterm neonates with RDS, which we believe provides a degree of generalizability for NICUs in the US.
The goal for these consensus statements was to reach agreement on key topics identified as knowledge and clinical care gaps that have emerged since the last set of guidelines was published in the US nearly a decade ago [4, 5]. It is our hope that these statements provide practical guidance and improve the care of neonates. In addition, this report serves as a stimulus to drive further investigation around existing knowledge gaps.
Supplementary information
Author contributions
VB, RB, RH, PR, and SH conducted the targeted literature review, designed the survey, hosted the virtual workshops, analyzed the results, developed the initial outline for the manuscript, and contributed to the writing of the manuscript. VB, BG, VK, MM, FM, CP, KR, RR, and CW, along with 2 additional panelists, participated and voted in the workshops. BG, VK, MM, FM, CP, KR, RR, and CW contributed to the writing of the manuscript. All authors reviewed the manuscript at each stage of development and provided input. Ann D. Bledsoe Bollert, MA, CMPP, of Y-Axis Editorial provided editorial support.
Funding
The workshop was funded by Chiesi Farmaceutici SpA. The panelists were compensated at fair market value for their time spent preparing for the workshop (initial survey, pre-reading) and time spent participating in the workshop. The panelists were not paid for the writing or review of the manuscript. The funding body did not play a role in the collection and analysis of data, writing and editing of the manuscript, or the decision to publish the results of the workshop. They were not present at the workshop discussions.
Data availability
All data generated or analyzed during this study are included in this published article [and its supplementary information files]. Any additional information about the current study are available from the corresponding author on reasonable request.
Competing interests
RB, RH, PR, and SH are employees of AESARA Inc. All authors received consultant fees from Chiesi Farmaceutici SpA. KR receives consultant fees from ONY Biotech, has received honoraria for lectures at Bubble CPAP Institute, Controversies in Neonatal and Perinatal Care, Baylor’s Avoiding Lung Injury Conference and Margaret Handy Memorial Lectureship, and has a patent for a neonatal airway device with ONY Biotech. CW has received payment for expert testimony in Texas and in Pennsylvania and speaker payment from Chiesi Farmaceutici SpA. FM has received speaker honoraria from Chiesi Farmaceutici SpA. CP has received speaker payment from Chiesi Farmaceutici SpA.
Footnotes
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
The online version contains supplementary material available at 10.1038/s41372-023-01690-9.
References
- 1.Yadav S, Lee B, Kamity R. Neonatal respiratory distress syndrome. In StatPearls. Treasure Island, FL: StatPearls Publishing; 2022. https://www.ncbi.nlm.nih.gov/books/NBK560779/. [PubMed]
- 2.Soll RF. Synthetic surfactant for respiratory distress syndrome in preterm infants. Cochrane Database Syst Rev. 2000;1998:Cd001149. doi: 10.1002/14651858.CD001149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suresh GK, Soll RF. Overview of surfactant replacement trials. J Perinatol. 2005;25:S40–S4.. doi: 10.1038/sj.jp.7211320. [DOI] [PubMed] [Google Scholar]
- 4.Walsh BK, Daigle B, DiBlasi RM, Restrepo RD. AARC Clinical Practice Guideline. Surfactant replacement therapy: 2013. Respir Care. 2013;58:367–75. doi: 10.4187/respcare.02189. [DOI] [PubMed] [Google Scholar]
- 5.Polin RA, Carlo WA. Surfactant replacement therapy for preterm and term neonates with respiratory distress. Pediatrics. 2014;133:156–63. doi: 10.1542/peds.2013-3443. [DOI] [PubMed] [Google Scholar]
- 6.Sweet DG, Carnielli VP, Greisen G, Hallman M, Klebermass-Schrehof K, Ozek E, et al. European consensus guidelines on the management of respiratory distress syndrome: 2022 update. Neonatology. 2023;120:3–23. doi: 10.1159/000528914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ozkan H, Erdeve O, Kutman HGK. Turkish Neonatal Society guideline on the management of respiratory distress syndrome and surfactant treatment. Turk Pediatr Ars. 2018;53:S45–S54. doi: 10.5152/TurkPediatriArs.2018.01806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ng EH, Shah V. Guidelines for surfactant replacement therapy in neonates. Paediatr Child Health. 2021;26:35–49. doi: 10.1093/pch/pxaa116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Surfactant Administration in the NICU: The Royal Children’s Hospital Melbourne; 2021. https://www.rch.org.au/rchcpg/hospital_clinical_guideline_index/Surfactant_Administration_in_the_NICU/.
- 10.Surfactant Administration in NICU. Starship Children’s Hospital; 2020. https://starship.org.nz/guidelines/surfactant-administration-in-nicu/.
- 11.ANMC NICU Surfactant Administration Guideline. Alaska Native Medical Center; 2021. https://anmc.org/files/Surfactant.pdf.
- 12.Sardesai S, Biniwale M, Wertheimer F, Garingo A, Ramanathan R. Evolution of surfactant therapy for respiratory distress syndrome: past, present, and future. Pediatr Res. 2017;81:240–8. doi: 10.1038/pr.2016.203. [DOI] [PubMed] [Google Scholar]
- 13.Hentschel R, Bohlin K, van Kaam A, Fuchs H, Danhaive O. Surfactant replacement therapy: from biological basis to current clinical practice. Pediatr Res. 2020;88:176–83.. doi: 10.1038/s41390-020-0750-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kakkilaya V, Gautham KS. Should less invasive surfactant administration (LISA) become routine practice in US neonatal units? Pediatric Research. 2023;93:1188–98. [DOI] [PMC free article] [PubMed]
- 15.Hasson F, Keeney S, McKenna H. Research guidelines for the Delphi survey technique. J Adv Nurs. 2000;32:1008–15. [PubMed] [Google Scholar]
- 16.Bahadue FL, Soll R. Early versus delayed selective surfactant treatment for neonatal respiratory distress syndrome. Cochrane Database Syst Rev. 2012;11:CD001456. [DOI] [PMC free article] [PubMed]
- 17.Rojas-Reyes MX, Morley CJ, Soll R. Prophylactic versus selective use of surfactant in preventing morbidity and mortality in preterm infants. Cochrane Database Syst Rev. 2012;3:Cd000510. [DOI] [PubMed]
- 18.Dargaville PA, Aiyappan A, De Paoli AG, Dalton RGB, Kuschel CA, Kamlin CO, et al. Continuous positive airway pressure failure in preterm infants: incidence, predictors and consequences. Neonatology. 2013;104:8–14. doi: 10.1159/000346460. [DOI] [PubMed] [Google Scholar]
- 19.Gulczyńska E, Szczapa T, Hożejowski R, Maria, Rutkowska M. Fraction of inspired oxygen as a predictor of CPAP failure in preterm infants with respiratory distress syndrome: a prospective multicenter study. Neonatology. 2019;116:171–8. doi: 10.1159/000499674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kakkilaya V, Wagner S, Mangona Kate Louise M, Steven Brown L, Jubran I, He H, et al. Early predictors of continuous positive airway pressure failure in preterm neonates. J Perinatol. 2019;39:1081–8. doi: 10.1038/s41372-019-0392-z. [DOI] [PubMed] [Google Scholar]
- 21.Dell’Orto V, Nobile S, Correani A, Marchionni P, Giretti I, Rondina C, et al. Early nasal continuous positive airway pressure failure prediction in preterm infants less than 32 weeks gestational age suffering from respiratory distress syndrome. Pediatr Pulmonol. 2021;56:3879–86.. doi: 10.1002/ppul.25678. [DOI] [PubMed] [Google Scholar]
- 22.Morley CJ, Davis PG, Doyle LW, Brion LP, Hascoet J-M, Carlin JB. Nasal CPAP or intubation at birth for very preterm infants. N Engl J Med. 2008;358:700–8. doi: 10.1056/NEJMoa072788. [DOI] [PubMed] [Google Scholar]
- 23.Lantos JD. SUPPORTing premature infants. Pediatrics. 2013;132:e1661–3. doi: 10.1542/peds.2013-1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kurepa D, Perveen S, Lipener Y, Kakkilaya V. The use of less invasive surfactant administration (LISA) in the United States with review of the literature. J Perinatol. 2019;39:426–32. doi: 10.1038/s41372-018-0302-9. [DOI] [PubMed] [Google Scholar]
- 25.Bugter IAL, Janssen LCE, Dieleman J, Kramer BW, Andriessen P, Niemarkt HJ. Introduction of less invasive surfactant administration (LISA), impact on diagnostic and therapeutic procedures in early life: a historical cohort study. BMC Pediatr. 2020;20;421. [DOI] [PMC free article] [PubMed]
- 26.Conlon SM, Osborne A, Bodie J, Marasch J, Ryan RM, Glenn T. Introducing less-invasive surfactant administration into a level IV NICU: a quality improvement initiative. Children. 2021;8:580. doi: 10.3390/children8070580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Härtel C, Glaser K, Speer CP. The miracles of surfactant: less invasive surfactant administration, nebulization, and carrier of topical drugs. Neonatology. 2021;118:225–34.. doi: 10.1159/000516106. [DOI] [PubMed] [Google Scholar]
- 28.Wright CJ, Glaser K, Speer CP, Härtel C, Roehr CC. Noninvasive ventilation and exogenous surfactant in times of ever decreasing gestational age: how do we make the most of these tools? J Pediatr. 2022;247:138–46. doi: 10.1016/j.jpeds.2022.04.011. [DOI] [PubMed] [Google Scholar]
- 29.Hiles M, Culpan AM, Watts C, Munyombwe T, Wolstenhulme S. Neonatal respiratory distress syndrome: chest X-ray or lung ultrasound? A systematic review. Ultrasound. 2017;25:80–91. doi: 10.1177/1742271X16689374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bucher S. The spiral of plastic pollution: a compensatory urge from the collective unconscious for an ecological-psychological transformation of civilization. J Anal Psychol. 2022;67:1386–409.. doi: 10.1111/1468-5922.12861. [DOI] [PubMed] [Google Scholar]
- 31.Zong H, Huang Z, Zhao J, Lin B, Fu Y, Lin Y, et al. The value of lung ultrasound score in neonatology. Front Pediatr. 2022;10:791664. doi: 10.3389/fped.2022.791664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.St. Clair C, Norwitz E, Woensdregt K, Cackovic M, Shaw J, Malkus H, et al. The probability of neonatal respiratory distress syndrome as a function of gestational age and lecithin/sphingomyelin ratio. Am J Perinatol. 2008;25:473–80. doi: 10.1055/s-0028-1085066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhao Q, Zhao Z, Leung-Pineda V, Wiley CL, Nelson PJ, Grenache DG, et al. Predicting respiratory distress syndrome using gestational age and lamellar body count. Clin Biochem. 2013;46:1228–32. doi: 10.1016/j.clinbiochem.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 34.Betts KS, Kisely S, Alati R. Predicting neonatal respiratory distress syndrome and hypoglycaemia prior to discharge: Leveraging health administrative data and machine learning. J Biomed Inf. 2021;114:103651. doi: 10.1016/j.jbi.2020.103651. [DOI] [PubMed] [Google Scholar]
- 35.Cogo PE, Facco M, Simonato M, De Luca D, De Terlizi F, Rizzotti U, et al. Pharmacokinetics and clinical predictors of surfactant redosing in respiratory distress syndrome. Intensive Care Med. 2011;37:510–7. doi: 10.1007/s00134-010-2091-2. [DOI] [PubMed] [Google Scholar]
- 36.Speer CP, Robertson B, Curstedt T, Halliday HL, Compagnone D, Gefeller O, et al. Randomized European multicenter trial of surfactant replacement therapy for severe neonatal respiratory distress syndrome: single versus multiple doses of Curosurf. Pediatrics. 1992;89:13–20. doi: 10.1542/peds.89.1.13. [DOI] [PubMed] [Google Scholar]
- 37.Dunn MS, Shennan AT, Possmayer F. Single- versus multiple-dose surfactant replacement therapy in neonates of 30 to 36 weeks’ gestation with respiratory distress syndrome. Pediatrics. 1990;86:564–71. doi: 10.1542/peds.86.4.564. [DOI] [PubMed] [Google Scholar]
- 38.Soll R, Özek E. Multiple versus single doses of exogenous surfactant for the prevention or treatment of neonatal respiratory distress syndrome. Cochrane Database Syst. Rev. 2009;1:CD000141. [DOI] [PubMed]
- 39.Fernandez-Gonzalez SM, Sucasas Alonso A, Ogando Martinez A, Avila-Alvarez A. Incidence, predictors and outcomes of noninvasive ventilation failure in very preterm infants. Child. 2022;9:426. doi: 10.3390/children9030426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Finer NN, Carlo WA, Walsh MC, Rich W, Gantz MG, Laptook AR, et al. Early CPAP versus surfactant in extremely preterm infants. N Engl J Med. 2010;362:1970–9. doi: 10.1056/NEJMoa0911783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Herting E, Härtel C, Göpel W. Less invasive surfactant administration (LISA): chances and limitations. Arch Dis Child Fetal Neonatal Ed. 2019;104:F655–f9.. doi: 10.1136/archdischild-2018-316557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ge H, Qiao Y, Au F, Scrivens A, Roehr CC. Less invasive surfactant administration as a means to facilitate gentler transition for preterm infants? A narrative review. Pediatr Med. 2022;5:27. doi: 10.21037/pm-21-2. [DOI] [Google Scholar]
- 43.Stoll BJ, Hansen NI, Bell EF, Walsh MC, Carlo WA, Shankaran S, et al. Trends in care practices, morbidity, and mortality of extremely preterm neonates, 1993-2012. JAMA. 2015;314:1039–51. doi: 10.1001/jama.2015.10244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Jensen EA, DeMauro SB, Kornhauser M, Aghai ZH, Greenspan JS, Dysart KC. Effects of multiple ventilation courses and duration of mechanical ventilation on respiratory outcomes in extremely low-birth-weight infants. JAMA Pediatr. 2015;169:1011–7. doi: 10.1001/jamapediatrics.2015.2401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Härtel C, Herting E, Humberg A, Hanke K, Mehler K, Keller T, et al. Association of administration of surfactant using less invasive methods with outcomes in extremely preterm infants less than 27 weeks of gestation. JAMA Netw Open. 2022;5:e2225810. doi: 10.1001/jamanetworkopen.2022.25810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.LISA in the delivery room for extremely preterm infants. ClinicalTrials.gov identifier: NCT04715373. https://ClinicalTrials.gov/show/NCT04715373, Accessed 10 October, 2022.
- 47.Wright CJ, Sherlock LG, Sahni R, Polin RA. Preventing continuous positive airway pressure failure. Clin Perinatol. 2018;45:257–71.. doi: 10.1016/j.clp.2018.01.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Elsayed YN. Lung ultrasound as a new technique for diagnosis of neonatal respiratory diseases. Neonatal Netw. 2018;37:224–32.. doi: 10.1891/0730-0832.37.4.224. [DOI] [PubMed] [Google Scholar]
- 49.Ollier V, Loi B, Rivaud C, Fortas F, Ruetsch V, Yousef N, et al. Semi-quantitative lung ultrasound score during ground transportation of outborn neonates with respiratory failure. Eur J Pediatr. 2022;181:3085–92. [DOI] [PubMed]
- 50.Vardar G, Karadag N, Karatekin G. The role of lung ultrasound as an early diagnostic tool for need of surfactant therapy in preterm infants with respiratory distress syndrome. Am J Perinatol. 2021;38:1547–56.. doi: 10.1055/s-0040-1714207. [DOI] [PubMed] [Google Scholar]
- 51.Gregorio-Hernández R, Arriaga-Redondo M, Pérez-Pérez A, Ramos-Navarro C, Sánchez-Luna M. Lung ultrasound in preterm infants with respiratory distress: experience in a neonatal intensive care unit. Eur J Pediatr. 2020;179:81–9. doi: 10.1007/s00431-019-03470-0. [DOI] [PubMed] [Google Scholar]
- 52.Raimondi F, Migliaro F, Corsini I, Meneghin F, Dolce P, Pierri L, et al. Lung ultrasound score progress in neonatal respiratory distress syndrome. Pediatrics. 2021;147:e2020030528. doi: 10.1542/peds.2020-030528. [DOI] [PubMed] [Google Scholar]
- 53.Downes JJ, Vidyasagar D, Boggs TR, Jr., Morrow GM., 3rd Respiratory distress syndrome of newborn infants. I. New clinical scoring system (RDS score) with acid–base and blood-gas correlations. Clin Pediatr. 1970;9:325–31. doi: 10.1177/000992287000900607. [DOI] [PubMed] [Google Scholar]
- 54.Shashidhar A, Pn S, Jose J. Downes Score vs Silverman Anderson Score for assessment of respiratory distress in preterm newborns. Pediatr Oncall. 2016;13:66–8. [Google Scholar]
- 55.Vohra R. Respiratory and gastrointestinal involvement in birth asphyxia. Acad J Pediatr Neonatol. 2018;6:555751.
- 56.Hedstrom AB, Gove NE, Mayock DE, Batra M. Performance of the Silverman Andersen Respiratory Severity Score in predicting PCO2 and respiratory support in newborns: a prospective cohort study. J Perinatol. 2018;38:505–11.. doi: 10.1038/s41372-018-0049-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Rodriguez H, Hartert TV, Gebretsadik T, Carroll KN, Larkin EK. A simple respiratory severity score that may be used in evaluation of acute respiratory infection. BMC Res Notes. 2016;9:85. [DOI] [PMC free article] [PubMed]
- 58.Kim JE, Brewer M, Spinazzola R, Wallace E, Casatelli J, Beachy J, et al. A quality improvement project to standardize surfactant delivery in the era of noninvasive ventilation. Pediatr Qual Saf. 2020;5:e311. doi: 10.1097/pq9.0000000000000311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Kribs A, Roll C, Göpel W, Wieg C, Groneck P, Laux R, et al. Nonintubated surfactant application vs conventional therapy in extremely preterm infants. JAMA Pediatr. 2015;169:723. doi: 10.1001/jamapediatrics.2015.0504. [DOI] [PubMed] [Google Scholar]
- 60.Reynolds P, Bustani P, Darby C, Fernandez Alvarez JR, Fox G, Jones S, et al. Less-invasive surfactant administration for neonatal respiratory distress syndrome: a consensus guideline. Neonatology. 2021;118:586–92.. doi: 10.1159/000518396. [DOI] [PubMed] [Google Scholar]
- 61.Dargaville PA, Kamlin COF, Orsini F, Wang X, De Paoli AG, Kanmaz, et al. Effect of minimally invasive surfactant therapy vs sham treatment on death or bronchopulmonary dysplasia in preterm infants with respiratory distress syndrome: the OPTIMIST-A randomized clinical trial. JAMA. 2021;326:2478–87. doi: 10.1001/jama.2021.21892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Abdel-Latif ME, Davis PG, Wheeler KI, De Paoli AG, Dargaville PA. Surfactant therapy via thin catheter in preterm infants with or at risk of respiratory distress syndrome. Cochrane Database Syst Rev. 2021;5:Cd011672. doi: 10.1002/14651858.CD011672.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Patel P, Houck A, Fuentes D. Examining Variations in Surfactant Administration (ENVISION): a neonatology insights pilot project. Children. 2021;8:261. [DOI] [PMC free article] [PubMed]
- 64.CUROSURF (poractant alfa). Parma, Italy: Chiesi Farmaceutici, S.p.A.; 2014. https://curosurf.com/.
- 65.INFASURF ® (calfactant). Amherst, NY: ONY Biotech Inc.; 2018. https://infasurf.com/.
- 66.SURVANTA (beractant). North Chicago, IL: AbbVie Inc.; 2019. https://www.rxabbvie.com/pdf/survanta_pi.pdf.
- 67.Ueda T, Ikegami M, Rider ED, Jobe AH. Distribution of surfactant and ventilation in surfactant-treated preterm lambs. J Appl Physiol. 1994;76:45–55. doi: 10.1152/jappl.1994.76.1.45. [DOI] [PubMed] [Google Scholar]
- 68.Zola EM, Gunkel JH, Chan RK, Lim MO, Knox I, Feldman BH, et al. Comparison of three dosing procedures for administration of bovine surfactant to neonates with respiratory distress syndrome. J Pediatr. 1993;122:453–9. doi: 10.1016/S0022-3476(05)83440-7. [DOI] [PubMed] [Google Scholar]
- 69.Niemarkt HJ, Hütten MC, Kramer BW. Surfactant for respiratory distress syndrome: new ideas on a familiar drug with innovative applications. Neonatology. 2017;111:408–14.. doi: 10.1159/000458466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Herting E, Härtel C, Göpel W. Less invasive surfactant administration: best practices and unanswered questions. Curr Opin Pediatr. 2020;32:228–34.. doi: 10.1097/MOP.0000000000000878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Isayama T, Iwami H, McDonald S, Beyene J. Association of noninvasive ventilation strategies with mortality and bronchopulmonary dysplasia among preterm infants: a systematic review and meta-analysis. JAMA. 2016;316:611–24. doi: 10.1001/jama.2016.10708. [DOI] [PubMed] [Google Scholar]
- 72.Roberts KD, Brown R, Lampland AL, Leone TA, Rudser KD, Finer NN, et al. Laryngeal mask airway for surfactant administration in neonates: a randomized, controlled trial. J Pediatr. 2018;193:40–6.e1. doi: 10.1016/j.jpeds.2017.09.068. [DOI] [PubMed] [Google Scholar]
- 73.Bellos I, Fitrou G, Panza R, Pandita A. Comparative efficacy of methods for surfactant administration: a network meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2021;106:474–87.. doi: 10.1136/archdischild-2020-319763. [DOI] [PubMed] [Google Scholar]
- 74.Kleijkers LMP, Van Der Spil J, Janssen LCE, Dieleman JP, Andriessen P, van Kaam AH, et al. Short-term outcome after repeated less invasive surfactant administration: a retrospective cohort study. Neonatology. 2022;119:719–26.. doi: 10.1159/000526493. [DOI] [PubMed] [Google Scholar]
- 75.Aldana-Aguirre JC, Pinto M, Featherstone RM, Kumar M. Less invasive surfactant administration versus intubation for surfactant delivery in preterm infants with respiratory distress syndrome: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2017;102:F17–F23. doi: 10.1136/archdischild-2015-310299. [DOI] [PubMed] [Google Scholar]
- 76.Al Ali RA, Gautam B, Miller MR, Coulson S, Yuen D. Laryngeal mask airway for surfactant administration versus standard treatment methods in preterm neonates with respiratory distress syndrome: a systematic review and meta-analysis. Am J Perinatol. 2022;39:1433–40.. doi: 10.1055/s-0041-1722953. [DOI] [PubMed] [Google Scholar]
- 77.Gallup JA, Ndakor SM, Pezzano C, Pinheiro JMB. Randomized trial of surfactant therapy via laryngeal mask airway versus brief tracheal intubation in preterm neonates. J Pediatr. 2023:254:17–24.e2. [DOI] [PubMed]
- 78.Brasher M, Raffay TM, Cunningham MD, Abu Jawdeh EG. Aerosolized surfactant for preterm infants with respiratory distress syndrome. Children. 2021;8:493. doi: 10.3390/children8060493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Sood BG, Cortez J, Kolli M, Sharma A, Delaney-Black V, Chen X. Aerosolized surfactant in neonatal respiratory distress syndrome: Phase I study. Early Hum Dev. 2019;134:19–25. doi: 10.1016/j.earlhumdev.2019.05.005. [DOI] [PubMed] [Google Scholar]
- 80.Dani C, Talosi G, Piccinno A, Ginocchio VM, Balla G, Lavizzari A, et al. A randomized, controlled trial to investigate the efficacy of nebulized poractant alfa in premature babies with respiratory distress syndrome. J Pediatr. 2022;246:40–7.e5. doi: 10.1016/j.jpeds.2022.02.054. [DOI] [PubMed] [Google Scholar]
- 81.Walther FJ, Waring AJ. Aerosol delivery of lung surfactant and nasal CPAP in the treatment of neonatal respiratory distress syndrome. Front Pediatr. 2022;10:923010. doi: 10.3389/fped.2022.923010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Gaertner VD, Thomann J, Bassler D, Rüegger CM. Surfactant nebulization to prevent intubation in preterm infants: a systematic review and meta-analysis. Pediatrics. 2021;148:e2021052504. doi: 10.1542/peds.2021-052504. [DOI] [PubMed] [Google Scholar]
- 83.Sood BG, Thomas R, Delaney-Black V, Xin Y, Sharma A, Chen X. Aerosolized Beractant in neonatal respiratory distress syndrome: A randomized fixed-dose parallel-arm phase II trial. Pulm Pharm Ther. 2021;66:101986. doi: 10.1016/j.pupt.2020.101986. [DOI] [PubMed] [Google Scholar]
- 84.Cummings JJ, Gerday E, Minton S, Katheria A, Albert G, Flores-Torres J, et al. Aerosolized calfactant for newborns with respiratory distress: a randomized trial. Pediatrics. 2020;146:e20193967. doi: 10.1542/peds.2019-3967. [DOI] [PubMed] [Google Scholar]
- 85.Audil HY, Tse S, Pezzano C, Mitchell-van Steele A, Pinheiro JMB. Efficacy, safety, and usability of remifentanil as premedication for INSURE in preterm neonates. Children. 2018;5:63. [DOI] [PMC free article] [PubMed]
- 86.Pinheiro JM, Santana-Rivas Q, Pezzano C. Randomized trial of laryngeal mask airway versus endotracheal intubation for surfactant delivery. J Perinatol. 2016;36:196–201. doi: 10.1038/jp.2015.177. [DOI] [PubMed] [Google Scholar]
- 87.Peterson J, den Boer MC, Roehr CC. To sedate or not to sedate for less invasive surfactant administration: an ethical approach. Neonatology. 2021;118:639–46.. doi: 10.1159/000519283. [DOI] [PubMed] [Google Scholar]
- 88.Kumar P, Denson SE, Mancuso TJ. Premedication for nonemergency endotracheal intubation in the neonate. Pediatrics. 2010;125:608–15. doi: 10.1542/peds.2009-2863. [DOI] [PubMed] [Google Scholar]
- 89.Moschino L, Zivanovic S, Hartley C, Trevisanuto D, Baraldi E, Roehr CC. Caffeine in preterm infants: where are we in 2020? ERJ Open Res. 2020;6:00330-2019. [DOI] [PMC free article] [PubMed]
- 90.Dani C, Cecchi A, Ciarcià M, Miselli F, Luzzati M, Remaschi G, et al. Enteral and parenteral treatment with caffeine for preterm infants in the delivery room: a randomised trial. Paediatr Drugs. 2023;25:79–86. doi: 10.1007/s40272-022-00541-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gilfillan M, Bhandari V. Moving bronchopulmonary dysplasia research from the bedside to the bench. Am J Physiol Lung Cell Mol Physiol. 2022;322:L804–l21. doi: 10.1152/ajplung.00452.2021. [DOI] [PubMed] [Google Scholar]
- 92.Bourgoin L, Caeymaex L, Decobert F, Jung C, Danan C, Durrmeyer X. Administering atropine and ketamine before less invasive surfactant administration resulted in low pain scores in a prospective study of premature neonates. Acta Paediatr. 2018;107:1184–90.. doi: 10.1111/apa.14317. [DOI] [PubMed] [Google Scholar]
- 93.Brotelande C, Milési C, Combes C, Durand S, Badr M, Cambonie G. Premedication with ketamine or propofol for less invasive surfactant administration (LISA): observational study in the delivery room. Eur J Pediatr. 2021;180:3053–8. doi: 10.1007/s00431-021-04103-1. [DOI] [PubMed] [Google Scholar]
- 94.Banerjee S, Fernandez R, Fox GF, Goss KCW, Mactier H, Reynolds P, et al. Surfactant replacement therapy for respiratory distress syndrome in preterm infants: United Kingdom national consensus. Pediatr Res. 2019;86:12–4. doi: 10.1038/s41390-019-0344-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Celli BR, Fabbri LM, Aaron SD, Agusti A, Brook R, Criner GJ, et al. An updated definition and severity classification of chronic obstructive pulmonary disease exacerbations: the Rome proposal. Am J Respir Crit Care Med. 2021;204:1251–8. doi: 10.1164/rccm.202108-1819PP. [DOI] [PubMed] [Google Scholar]
- 96.Eubank BH, Mohtadi NG, Lafave MR, Wiley JP, Bois AJ, Boorman RS, et al. Using the modified Delphi method to establish clinical consensus for the diagnosis and treatment of patients with rotator cuff pathology. BMC Med Res Methodol. 2016;16:56. [DOI] [PMC free article] [PubMed]
- 97.Miller KA, Collada B, Tolliver D, Audi Z, Cohen A, Michelson C, et al. Using the modified Delphi method to develop a tool to assess pediatric residents supervising on inpatient rounds. Acad Pediatr. 2020;20:89–96. doi: 10.1016/j.acap.2019.07.012. [DOI] [PubMed] [Google Scholar]
- 98.Zapata HA, Fort P, Roberts KD, Kaluarachchi DC, Guthrie SO. Surfactant administration through laryngeal or supraglottic airways (SALSA): a viable method for low-income and middle-income countries. Front Pediatr. 2022;10:853831. doi: 10.3389/fped.2022.853831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Chahin N, Rozycki HJ. New modes of surfactant delivery. Paediatr Respir Rev. 2021;43:38–43. doi: 10.1016/j.prrv.2021.10.002. [DOI] [PubMed] [Google Scholar]
- 100.Ekhaguere OA, Okonkwo IR, Batra M, Hedstrom AB. Respiratory distress syndrome management in resource limited settings-Current evidence and opportunities in 2022. Front Pediatr. 2022;10:961509. doi: 10.3389/fped.2022.961509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Dilli D, Çakmakçı E, Akduman H, Oktem A, Aydoğan S, Çitli R, et al. Comparison of three natural surfactants according to lung ultrasonography scores in newborns with respiratory distress syndrome. J Matern Fetal Neonatal Med. 2021;34:1634–40.. doi: 10.1080/14767058.2019.1643313. [DOI] [PubMed] [Google Scholar]
- 102.Fatahi N, Dalili H, Kalani M, Niknafs N, Shariat M, Tavakkoly-Bazzaz J, et al. Association of SP-C gene codon 186 polymorphism (rs1124) and risk of RDS. J Matern Fetal Neonatal Med. 2017;30:2585–9. doi: 10.1080/14767058.2016.1256994. [DOI] [PubMed] [Google Scholar]
- 103.Koti J, Murki S, Gaddam P, Reddy A, Reddy MD. Bubble CPAP for respiratory distress syndrome in preterm infants. Indian Pediatr. 2010;47:139–43. doi: 10.1007/s13312-010-0021-6. [DOI] [PubMed] [Google Scholar]
- 104.Rusmawati A, Haksari EL, Naning R. Downes score as a clinical assessment for hypoxemia in neonates with respiratory distress. Paediatr Indones. 2016;48:342. doi: 10.14238/pi48.6.2008.342-5. [DOI] [Google Scholar]
- 105.Shrestha S, Shrestha SK, Shrestha GS, Dhakal MS. Assessment of hypoxemia using downes score in neonates with respiratory distress. Nepal Med Coll J. 2021;23:194–7. doi: 10.3126/nmcj.v23i3.40375. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated or analyzed during this study are included in this published article [and its supplementary information files]. Any additional information about the current study are available from the corresponding author on reasonable request.