Abstract
Purpose
To retrospectively determine the prevalence of multifid tendons in a population of patients who underwent iliopsoas release for painful snapping iliopsoas tendons.
Methods
Patients who underwent iliopsoas release for painful snapping iliopsoas tendons were retrospectively identified from a database of patients who had undergone arthroscopic hip surgery performed by a single surgeon between 2011 and 2020. Patients who had incomplete data or who underwent prior fracture fixation, joint arthroplasty, pelvic surgery, or other interventions for snapping hip were excluded. Magnetic resonance imaging (MRI) and operative reports were reviewed and compared with those of an age-matched control group of patients who had undergone hip or pelvic MRI examinations in the past year for different indications.
Results
This study included 91 patients (78 female and 13 male patients; mean age, 23.3 years) who were treated operatively for painful snapping hip and 78 controls (54 female and 24 male patients; mean age, 28.4 years) who received hip or pelvic MRI for other indications. Among the patients who underwent iliopsoas release, there were 5 unifid iliopsoas tendons (5.5%) compared with 86 multifid iliopsoas tendons (94.5%) when classified with MRI whereas operative examination showed 19 unifid tendons (20.9%) compared with 72 multifid tendons (79.1%, P < .001). When the MRI scans of the operative group were compared with the MRI scans of the control group, the patients who underwent surgery for painful snapping hip had a higher rate of multifid tendons (94.5% of operative hips compared with 69.2% of control right hips [P < .001] and 74.4% of control left hips [P < .001]). However, when the operative reports were used to classify the iliopsoas tendon, there was no significance between the operative and control groups (79.1% of operative hips had multifid tendons compared with 69.2% of control right hips [P = .141] and 74.4% of control left hips [P = .464]).
Conclusions
For patients with symptomatic snapping hip undergoing iliopsoas lengthening, multifid iliopsoas tendons are more prevalent than in a control population.
Level of Evidence
Level IV, prognostic case series.
Iliopsoas disorders are the primary cause of chronic groin pain in 12% to 36% of athletes.1 A common iliopsoas disorder is the internal snapping hip syndrome, in which an audible and sometimes painful click is experienced when the lower extremity is moved from a position of more than 90° of hip flexion and abduction to a position of extension and relative adduction.2 Typically, symptoms improve with nonoperative measures including stretching, physical therapy, nonsteroidal anti-inflammatory medication, activity modification, and local anesthetic injection. If the hip continues to be symptomatic despite conservative measures, surgical lengthening of the iliopsoas tendon and debridement can provide relief, with reported success rates greater than 80%.3, 4, 5, 6
In addition to its role in maintaining the position of the lumbar spine during hip flexion, the iliopsoas acts as a dynamic stabilizer to keep the femoral head reduced within the acetabulum, primarily from 0° to 15° of flexion, and acts as a flexor of the lower extremity, primarily from 45° to 60° of flexion.7 Chronic iliopsoas pathology can also contribute to atraumatic hip instability, making its evaluation part of a comprehensive treatment plan for patients with hip pathology. There is a strong association with intra-articular hip pathology in patients with painful iliopsoas tendons, given that magnetic resonance imaging (MRI) in prior studies has revealed associated chondral and labral abnormalities in 67% to 100% of these patients.1
A painful snapping iliopsoas tendon can be treated with arthroscopic release.3,4,6 Prior cadaveric anatomic studies,8 MRI studies,9 and ultrasound studies10 have reported that the iliopsoas tendon is bifid or trifid 14% to 72% of the time. Incomplete release of the iliopsoas tendon or release of only 1 slip of tendon when multiple slips are present can result in refractory pain that necessitates additional surgery.11 Therefore, knowledge of the incidence of multifid iliopsoas tendons can help individuals who treat this condition.
The purpose of this study was to retrospectively determine the prevalence of multifid tendons in a population of patients who underwent iliopsoas release for painful snapping iliopsoas tendons. We hypothesized that patients who underwent iliopsoas release for painful snapping iliopsoas tendons would have a higher prevalence of multifid iliopsoas tendons.
Methods
After institutional review board approval was obtained, patients who underwent iliopsoas release for painful snapping iliopsoas tendons were retrospectively identified from a database of patients who had undergone arthroscopic hip surgery between 2011 and 2020 performed by a single surgeon (B.G.). The exclusion criteria included patients with incomplete data such as insufficient images or missing operative notes; those who previously underwent fracture fixation, joint arthroplasty, or other interventions for snapping hip; and those who previously underwent pelvic surgery. Patients who underwent arthroscopic iliopsoas lengthening were identified by Current Procedural Terminology (CPT) billing code 29999 and were verified to have undergone an iliopsoas fractional lengthening procedure by the operative reports. Iliopsoas release was performed arthroscopically and assessed in an intracapsular manner. All operative patients were evaluated by a fellowship-trained, board-certified, sports medicine orthopaedic surgeon (B.G.) specializing in hip pathology. An age-matched control group was selected from patients who underwent MRI of the pelvis or hip at the same institution in the past year for non-orthopaedic indications. Details regarding enrollment of operative patients are presented in Figure 1.
Fig 1.
Flowchart showing exclusion of patients from study. (PACS, picture archiving and communication system.)
MRI scans of the operative hip as well as both control hips were evaluated by either an orthopaedic surgery fellow (M.M.) or resident (A.H.) to determine the number of iliopsoas tendons present at the level of the hip capsule (Figs 2 and 3). The number of tendons identified and released was recorded from the operative reports. All patients were treated with iliopsoas release between 2011 and 2020. Demographic data were gathered through retrospective chart review of enrolled subjects and included age at the time of surgery, sex, and subsequent hip operations.
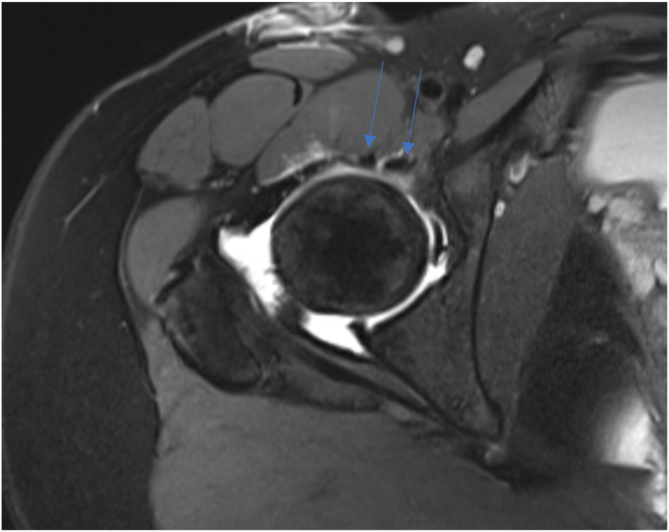
Fig 2.
Magnetic resonance imaging slice (axial intermediate fat-suppressed sequence) showing bifid iliopsoas tendon (arrows) in right hip.
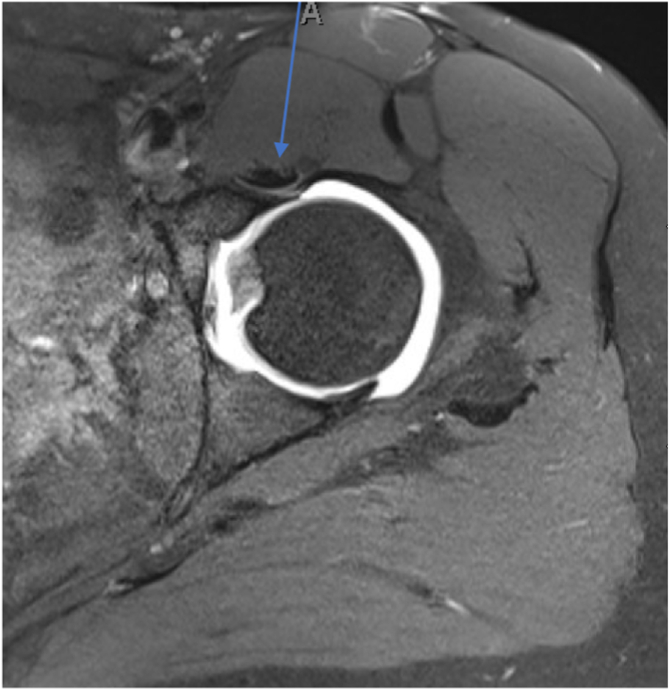
Fig 3.
Magnetic resonance imaging slice (axial intermediate fat-suppressed sequence) showing unifid iliopsoas tendon (arrow) in left hip. A, anterior.
Statistical analysis was conducted using Microsoft Excel (Redmond, WA) and SAS software (version 9.4; SAS Institute, Cary, NC) and included basic summary analysis, the Student t test, and the χ2 test as appropriate. P < .05 was considered significant. The κ statistic and the McNemar test were used to determine the level of agreement regarding whether the iliopsoas tendon was unifid or multifid between the MRI scans and the operative reports.
Results
Overall, 91 operative patients who underwent iliopsoas release and 78 controls were included in the final data set. There were 78 female patients (86%) in the operative group and 53 female patients (68%) in the control group. The average age of the operative patients was 23.3 years (range, 14-52 years; standard deviation, 8.6 years), whereas the average age of the controls was 28.4 years (range, 14-39 years; standard deviation, 6.3 years) (Table 1).
Table 1.
Demographic Data of Operative and Control Groups
| Operative Group | Control Group | |
|---|---|---|
| Total hips, n | 91 | 78 |
| Mean age (SD), yr | 23.3 (8.6) | 28.4 (6.3) |
| % Male sex | 14.3 | 32.1 |
SD, standard deviation.
Of the 91 patients who underwent iliopsoas release, 86 (95%) were noted to have multifid tendons on MRI whereas 72 (79%) were noted to have multifid tendons in the operative reports. The classification of the iliopsoas tendon was statistically significant between the MRI scans and the operative notes (P < .001). The κ statistic between the 2 diagnostic modalities was 0.27, indicating poor agreement between MRI and arthroscopic visualization of the iliopsoas tendon.
On the MRI examinations of the 78 control patients, 54 (69.2%) were noted to have multifid iliopsoas tendons on the right side whereas 58 (74.4%) were noted to have multifid iliopsoas tendons on the left side. The χ2 analysis comparing the MRI scans of the operative hips with the MRI scans of the control hips showed a significant difference between the 2 groups, for both control right and control left hips (94.5% of operative hips had multifid tendons compared with 69.2% of control right hips [P < .001] and 74.4% of control left hips [P < .001]) (Table 2).
Table 2.
Comparison Between Operative and Control Groups Based on MRI Scans
| Unifid, n (%) | Multifid, n (%) | P Value (Compared With Operative Group) | |
|---|---|---|---|
| Operative group | 5 (5.5) | 86 (94.5) | — |
| Control group | |||
| Right hip | 24 (30.8) | 54 (69.2) | <.001 |
| Left hip | 20 (25.6) | 58 (74.4) | <.001 |
MRI, magnetic resonance imaging.
However, a similar analysis comparing the iliopsoas tendons based on the operative reports rather than the MRI scans did not show any significant difference between the operative hips and control right hips (79.1% of operative hips had multifid tendons compared with 69.2% of control right hips, P = .141). This result was also not significant when the operative hips were compared with control left hips (79.1% of operative hips had multifid tendons compared with 74.4% of control left hips, P = .464) (Table 3).
Table 3.
Comparison Between Operative and Control Groups Based on Operative Reports
| Unifid, n (%) | Multifid, n (%) | P Value (Compared With Operative Group) | |
|---|---|---|---|
| Operative group | 19 (20.9) | 72 (79.1) | — |
| Control group | |||
| Right hip | 24 (30.8) | 54 (69.2) | .141 |
| Left hip | 20 (25.6) | 58 (74.4) | .464 |
Discussion
In this study, we found that the prevalence of multifid iliopsoas tendons in patients undergoing release was 79.1% as determined by arthroscopic visualization. When MRI was used as the diagnostic modality to determine whether the iliopsoas tendon was unifid or multifid, the prevalence was even higher, at 95%. These results indicate that multifid iliopsoas tendons are more prevalent than previously reported. Philippon et al.8 found the prevalence of multifid iliopsoas tendons to be 71.7% in a cadaveric study, whereas Crompton et al.9 found the prevalence of bifid iliopsoas tendons in a pediatric population to be 21% based on MRI. One reason for the higher prevalence found in our study compared with the study by Crompton et al. is that we made the classification of whether the iliopsoas tendon was unifid or multifid at the level of the hip joint whereas Crompton et al. made the determination more distally, between the femoral neck and lesser trochanter.
With these findings, this study identifies another anatomic feature that is more common in patients with symptomatic snapping hip. Multifid anatomy of the iliopsoas may predispose to symptomatic hip snapping because this adds more tendinous volume to the overall muscle-tendon unit. This potentially creates more opportunity for symptomatic contracture and abrasion of the additional tendinous portions over the anterior femur and pelvis. Previous studies have identified other predisposing factors such as lumbopelvic hyperlordosis in dancers, in which the femoral head is brought anteriorly in the acetabulum and thought to cause symptomatic snapping of the iliopsoas tendon.12 Pelvic anteversion or proximal femoral anteversion can also contribute to extra-articular snapping as the hip flexor or extrinsic muscles are placed under increased tension.13 Furthermore, bony dysmorphology of the anterior inferior iliac spine has been found to cause extra-articular snapping of the iliopsoas as well.14
Although this study suggests that multifid iliopsoas tendons are a risk factor, it is also notable that multifid tendons are not the only risk factor for a symptomatic snapping hip nor does their presence guarantee they will be symptomatic. Patients undergoing revision did not have multifid tendons at a greater frequency than the control group—a finding that supports previous works suggesting that bony pelvic anatomic measures contribute to this problem.12,15,16 It is our belief that in these patients, scar and contracture after an index surgical procedure exacerbate these anatomic variations, thus leading to the symptoms experienced.
In addition to the findings of our study, thorough knowledge of the other underlying etiologies of painful snapping hip must be considered before treating a patient with arthroscopic iliopsoas lengthening. In our experience, correcting variables such as poor exercise strategies or treating underlying bony pathology and dysmorphology will fix the painful snapping hip and preclude the need for operative intervention on the iliopsoas tendon. The release and lengthening of the iliopsoas tendon are not without risk, and prior research in patients who underwent arthroscopic treatment of femoroacetabular impingement has suggested poorer outcomes in those who underwent iliopsoas tenotomy compared with those who did not.17,18 There must be judicious selection of patients for the treatment of painful snapping hip with iliopsoas tenotomy or lengthening to prevent further instability, weakness, and continued pain.19
There was poor agreement on whether the iliopsoas tendon was unifid or multifid between the MRI scans and the operative reports, with MRI being more sensitive. One contributing reason may be the difficulty in fully visualizing the secondary or tertiary bands of the iliopsoas tendon arthroscopically, or the decision made to not further violate musculature in order to dissect out accessory tendons. Previous literature has described continued symptoms due to an unreleased second head of a bifid iliopsoas tendon, which went unrecognized during the index operative release.11 This underlies the importance of preoperative recognition of multifid tendons, and if the multiple tendon heads are not easily visible through the initial transcapsular window, further exposure should be performed for a more complete release if this is the surgeon’s intent. Although prior studies have found that a full release of the iliopsoas tendon does not fully release the entire musculotendinous unit, because there is a significant contribution from the muscle belly all the way to the insertion at the lesser trochanter,20 not every patient with multiple tendon slips requires a release of both tendons. In certain populations such as active competitive athletes, it may be best to accept some snapping—and even painful snapping—because overlengthening may lead to challenges with high-level conditioning or unacceptable loss of flexion strength.19 These considerations highlight the importance of understanding the patient’s goals for surgery, the symptoms that are most affecting the patient, and the patient’s underlying anatomic risk factors when making an operative plan for iliopsoas tendon release.
Previous studies evaluating multifid tendons using MRI and ultrasound imaging, as well as operative and cadaveric evaluations, have reported a wide range of frequencies, from 5% to 72%.2,8,9,21,22 In this study, the prevalence in the control group was nearly identical to the upper limit of this range and therefore has clinical legitimacy. Our findings suggest that in patients with hip pain and an imaging workup revealing multifid iliopsoas tendons, there must be heightened awareness of symptomatic snapping iliopsoas tendons as a source of their pain. Furthermore, understanding that there is a high frequency of multifid tendons may help prevent surgeons from performing incomplete release of the symptomatic iliopsoas tendon.
Limitations
This study is limited by its retrospective nature. However, patients were selected for arthroscopic iliopsoas release based on a constellation of symptoms and examinations performed by a fellowship-trained, board-certified, sports medicine orthopaedic surgeon specializing in hip pathology in all instances. A prospective study might offer more robust results but also might confer more bias in the way asymptomatic or mildly symptomatic snapping hips are assessed. These findings could also benefit from a matched cohort of patients with hip pathology without painful snapping, but this could not be assessed in this study. A further limitation is that the MRI scans were split between reviewers and only interpreted once, so no agreement statistic between the MRI reviewers can be calculated. Moreover, because the control group was matched on age, there was a higher proportion of male patients as the sample set of controls skewed much older and more male. This difference in sex may limit the ability to draw a direct comparison. Finally, outcome data differentiating results from patients with unifid and multifid tendons could add utility in this finding as a prognostic indicator.
Conclusions
For patients with symptomatic snapping hip undergoing iliopsoas lengthening, multifid iliopsoas tendons are more prevalent than in a control population.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: B.G. receives grant support, personal fees, and nonfinancial support from Arthrex, outside the submitted work. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
References
- 1.Anderson C.N. Iliopsoas: Pathology, diagnosis, and treatment. Clin Sports Med. 2016;35:419–433. doi: 10.1016/j.csm.2016.02.009. [DOI] [PubMed] [Google Scholar]
- 2.Ilizaliturri V.M., Suarez-Ahedo C., Acuña M. Internal snapping hip syndrome: Incidence of multiple-tendon existence and outcome after endoscopic transcapsular release. Arthroscopy. 2015;31:1991–1995. doi: 10.1016/j.arthro.2015.04.083. [DOI] [PubMed] [Google Scholar]
- 3.Flanum M.E., Keene J.S., Blankenbaker D.G., DeSmet A.A. Arthroscopic treatment of the painful “internal” snapping hip: Results of a new endoscopic technique and imaging protocol. Am J Sports Med. 2007;35:770–779. doi: 10.1177/0363546506298580. [DOI] [PubMed] [Google Scholar]
- 4.Wettstein M., Jung J., Dienst M. Arthroscopic psoas tenotomy. Arthroscopy. 2006;22:907.e1–907.e4. doi: 10.1016/j.arthro.2005.12.064. [DOI] [PubMed] [Google Scholar]
- 5.Dobbs M.B., Gordon J.E., Luhmann S.J., Szymanski D.A., Schoenecker P.L. Surgical correction of the snapping iliopsoas tendon in adolescents. J Bone Joint Surg Am. 2002;84:420–424. doi: 10.2106/00004623-200203000-00013. [DOI] [PubMed] [Google Scholar]
- 6.Hoskins J.S., Burd T.A., Allen W.C. Surgical correction of internal coxa saltans: A 20-year consecutive study. Am J Sports Med. 2004;32:998–1001. doi: 10.1177/0363546503260066. [DOI] [PubMed] [Google Scholar]
- 7.Yoshio M., Murakami G., Sato T., Sato S., Noriyasu S. The function of the psoas major muscle: Passive kinetics and morphological studies using donated cadavers. J Orthop Sci. 2002;7:199–207. doi: 10.1007/s007760200034. [DOI] [PubMed] [Google Scholar]
- 8.Philippon M.J., Devitt B.M., Campbell K.J., et al. Anatomic variance of the iliopsoas tendon. Am J Sports Med. 2014;42:807–811. doi: 10.1177/0363546513518414. [DOI] [PubMed] [Google Scholar]
- 9.Crompton T., Lloyd C., Kokkinakis M., Norman-Taylor F. The prevalence of bifid iliopsoas tendon on MRI in children. J Child Orthop. 2014;8:333–336. doi: 10.1007/s11832-014-0596-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deslandes M., Guillin R., Cardinal É., Hobden R., Bureau N.J. The snapping iliopsoas tendon: New mechanisms using dynamic sonography. AJR Am J Roentgenol. 2008;190:576–581. doi: 10.2214/AJR.07.2375. [DOI] [PubMed] [Google Scholar]
- 11.Shu B., Safran M.R. Case report: Bifid iliopsoas tendon causing refractory internal snapping hip. Clin Orthop Relat Res. 2011;469:289–293. doi: 10.1007/s11999-010-1452-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Laible C., Swanson D., Garofolo G., Rose D.J. Iliopsoas syndrome in dancers. Orthop J Sports Med. 2013;1 doi: 10.1177/2325967113500638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spina A.A. External coxa saltans (snapping hip) treated with active release techniques: A case report. J Can Chiropr Assoc. 2007;51:23–29. [PMC free article] [PubMed] [Google Scholar]
- 14.El-shaar R., Stanton M., Biehl S., Giordano B. Effect of subspine decompression on rectus femoris integrity and iliopsoas excursion: A cadaveric study. Arthroscopy. 2015;31:1903–1908. doi: 10.1016/j.arthro.2015.03.031. [DOI] [PubMed] [Google Scholar]
- 15.Jacobson T., Allen W.C. Surgical correction of the snapping iliopsoas tendon. Am J Sports Med. 1990;18:470–474. doi: 10.1177/036354659001800504. [DOI] [PubMed] [Google Scholar]
- 16.Bakhsh W., Childs S., Kenney R., Schiffman S., Giordano B. Iliopsoas snapping hip: Improving the diagnostic value of magnetic resonance imaging with a novel parameter. Skeletal Radiol. 2019;48:889–896. doi: 10.1007/s00256-018-3083-5. [DOI] [PubMed] [Google Scholar]
- 17.Matsuda D., Kivlan B.R., Nho S.J., et al. Tenotomy for iliopsoas pathology is infrequently performed and associated with poorer outcomes in hips undergoing arthroscopy for femoroacetabular impingement. Arthroscopy. 2021;37:2140–2148. doi: 10.1016/j.arthro.2021.02.018. [DOI] [PubMed] [Google Scholar]
- 18.Domb B.G., Maldonado D.R. Editorial commentary: Indiscriminate iliopsoas tenotomy may cause complications—With tight indications and transbursal lengthening, we may avoid them. Arthroscopy. 2021;37:2149–2151. doi: 10.1016/j.arthro.2021.04.065. [DOI] [PubMed] [Google Scholar]
- 19.Via A.G., Basile A., Wainer M., Musa C., Padulo J., Mardones R. Endoscopic release of internal snapping hip: A review of literature. Muscles Ligaments Tendons J. 2016;6:372–377. doi: 10.11138/mltj/2016.6.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Blomberg J.R., Zellner B.S., Keene J.S. Cross-sectional analysis of iliopsoas muscle-tendon units at the sites of arthroscopic tenotomies: An anatomic study. Am J Sports Med. 2011;39(suppl):58–63. doi: 10.1177/0363546511412162. [DOI] [PubMed] [Google Scholar]
- 21.Guillin R., Cardinal É., Bureau N.J. Sonographic anatomy and dynamic study of the normal iliopsoas musculotendinous junction. Eur Radiol. 2009;19:995–1001. doi: 10.1007/s00330-008-1212-6. [DOI] [PubMed] [Google Scholar]
- 22.Polster J.M., Elgabaly M., Lee H., Klika A., Drake R., Barsoum W. MRI and gross anatomy of the iliopsoas tendon complex. Skeletal Radiol. 2008;37:55–58. doi: 10.1007/s00256-007-0393-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.