This phase Ib study of the oral, small-molecule inhibitor of MDM2, brigimadlin (BI 907828), reveals its early activity in MDM2-amplified liposarcoma and biliary tract cancers when dosed intermittently.
Abstract
Brigimadlin (BI 907828) is an oral MDM2–p53 antagonist that has shown encouraging antitumor activity in vivo. We present phase Ia results from an open-label, first-in-human, phase Ia/Ib study investigating brigimadlin in patients with advanced solid tumors (NCT03449381). Fifty-four patients received escalating doses of brigimadlin on day 1 of 21-day cycles (D1q3w) or days 1 and 8 of 28-day cycles (D1D8q4w). Based on dose-limiting toxicities during cycle 1, the maximum tolerated dose was selected as 60 mg for D1q3w and 45 mg for D1D8q4w. The most common treatment-related adverse events (TRAE) were nausea (74.1%) and vomiting (51.9%); the most common grade ≥3 TRAEs were thrombocytopenia (25.9%) and neutropenia (24.1%). As evidence of target engagement, time- and dose-dependent increases in growth differentiation factor 15 levels were seen. Preliminary efficacy was encouraging (11.1% overall response and 74.1% disease control rates), particularly in patients with well-differentiated or dedifferentiated liposarcoma (100% and 75% disease control rates, respectively).
Significance:
We report phase Ia data indicating that the oral MDM2–p53 antagonist brigimadlin has a manageable safety profile and shows encouraging signs of efficacy in patients with solid tumors, particularly those with MDM2-amplified advanced/metastatic well-differentiated or dedifferentiated liposarcoma. Further clinical investigation of brigimadlin is ongoing.
See related commentary by Italiano, p. 1765.
This article is highlighted in the In This Issue feature, p. 1749
INTRODUCTION
Evasion of cell-cycle arrest and apoptosis by inactivation of p53 is a key mechanism by which tumors promote survival and proliferation (1). The TP53 gene is frequently mutated or deleted in many cancer types, which inactivates the tumor suppression activity of the p53 protein. However, loss of p53 tumor-suppressor activity can also occur in TP53 wild-type tumors through amplification or overexpression of the key negative regulator of p53, mouse double minute 2 (MDM2) oncoprotein (2, 3). MDM2 amplification promotes p53 degradation and aids tumor proliferation (1, 3). Targeting MDM2 and disrupting the MDM2–p53 interaction has therefore been proposed as a strategy to restore wild-type p53 function (3, 4).
Overall, approximately 3.5% to 7% of tumors display MDM2 amplifications (5–7). However, these amplifications are more common in some tumor types than others; for example, the incidence is >90% in some types of advanced soft-tissue sarcoma such as well-differentiated and dedifferentiated liposarcoma (WDLPS/DDLPS; refs. 8–11). Targeting the MDM2–p53 interaction, particularly in tumor types with high incidences of MDM2 amplification, could therefore be a promising therapeutic approach. However, despite several MDM2-targeting molecules being investigated in the preclinical setting, there has been limited success in the clinic to date (3).
Brigimadlin (BI 907828) is a highly potent, oral MDM2–p53 antagonist; it has shown encouraging antitumor activity in vivo, especially in TP53 wild-type, MDM2-amplified DDLPS patient-derived xenografts and syngeneic models (12, 13). NCT03449381 is a first-in-human, phase Ia/Ib study assessing oral brigimadlin monotherapy in adult patients with advanced or metastatic solid tumors. Here, we report the results of the phase Ia dose-escalation part of the study.
RESULTS
Patients and Treatment
A total of 54 patients were enrolled to phase Ia: 29 patients received brigimadlin 10 to 80 mg on day 1 of 21-day cycles (D1q3w arm), and 25 patients received brigimadlin 5 to 60 mg on days 1 and 8 of 28-day cycles (D1D8q4w arm). Baseline demographics and disease characteristics of patients were similar in the two treatment arms (Table 1). Patients had a mean age of 57.2 years (range, 19–83), they had received a median of two (range, 0–11) prior therapies, and ∼80% of patients had stage IV disease. The most common tumor type was soft-tissue sarcoma [25 patients (46.3%), including 12 with DDLPS and seven with WDLPS]; 28 patients (51.9%), including all patients with liposarcoma, had MDM2-amplified disease by central assessment [MDM2 amplification status was not assessed/data were missing for eight patients (14.8%) due to insufficient tissue provision]. Representativeness of the study participants is summarized in Supplementary Table S1.
Table 1.
Baseline demographic and disease characteristics of patients in the D1q3w arm, the D1D8q4w arm, and overall
| Characteristic | D1q3w (n = 29) | D1D8q4w (n = 25) | All patients (N = 54) |
|---|---|---|---|
| Mean age, years (range) | 59.1 (32–83) | 55.0 (19–75) | 57.2 (19–83) |
| Gender, n (%) | |||
| Male | 16 (55.2) | 15 (60.0) | 31 (57.4) |
| Female | 13 (44.8) | 10 (40.0) | 23 (42.6) |
| Race | |||
| Caucasian | 19 (65.5) | 18 (72.0) | 37 (68.5) |
| Asian | 9 (31.0) | 5 (20.0) | 14 (25.9) |
| African American | 1 (3.4) | 1 (4.0) | 2 (3.7) |
| Missing | 0 | 1 (4.0) | 1 (1.9) |
| Clinical stage | |||
| III | 2 (6.9) | 3 (12.0) | 5 (9.3) |
| IV | 24 (82.8) | 19 (76.0) | 43 (79.6) |
| Not assessed | 3 (10.3) | 3 (12.0) | 6 (11.1) |
| ECOG PS, n (%) | |||
| 0 | 11 (37.9) | 17 (68.0) | 28 (51.2) |
| 1 | 18 (62.1) | 8 (32.0) | 26 (48.1) |
| Tumor classification | |||
| Soft-tissue sarcoma | 10 (34.5) | 15 (60.0) | 25 (46.3) |
| DDLPS | 6 (20.7) | 6 (24.0) | 12 (22.2) |
| WDLPS | 3 (10.3) | 4 (16.0) | 7 (13.0) |
| Melanoma | 2 (6.9) | 2 (8.0) | 4 (7.4) |
| Head and neck cancers | 1 (3.4) | 2 (8.0) | 3 (5.6) |
| Uterine sarcoma | 2 (6.9) | 1 (4.0) | 3 (5.6) |
| Colorectal carcinoma | 1 (3.4) | 1 (4.0) | 2 (3.7) |
| Biliary tract carcinoma | 2 (6.9) | 0 | 2 (3.7) |
| Breast cancer | 2 (6.9) | 0 | 2 (3.7) |
| Small intestine carcinoma | 2 (6.9) | 0 | 2 (3.7) |
| Other tumor typesa | 7 (24.1) | 4 (16.0) | 11 (20.4) |
| Median number of prior systemic therapies (range) | 3 (0–11) | 2 (0–8) | 2 (0–11) |
| ≥2 prior therapies | 20 (69.0) | 17 (68.0) | 37 (68.5) |
| MDM2 status (central assessment) | |||
| Amplified | 14 (48.3) | 14 (56.0) | 28 (51.9) |
| Not amplified | 11 (37.9) | 7 (28.0) | 18 (33.3) |
| Not assessed/missing | 4 (13.8) | 4 (16.0) | 8 (14.8) |
| TP53 mutation (central assessment) | |||
| Yes | 2 (6.9) | 0 | 2 (3.7) |
| No | 14 (48.3) | 18 (72.0) | 32 (59.3) |
| Not assessed/missing | 13 (44.8) | 7 (28.0) | 20 (37.0) |
Abbreviation: ECOG PS, Eastern Cooperative Oncology Group performance status.
aOther tumor types included adrenal cancer, anal cancer, cancer of the ureter, cancer of the urethra and penis, cancers of unknown primary site, endometrial carcinoma, gastrointestinal tract cancer, non–small cell lung cancer, and pancreatic cancer.
Dose-Limiting Toxicities and Maximum Tolerated Dose
During the dose-escalation part of the study, patients in the D1q3w arm received brigimadlin at seven dose levels: 10 mg (n = 1), 20 mg (n = 2), 30 mg (n = 3), 45 mg (n = 6), 50 mg (n = 4), 60 mg (n = 7), and 80 mg (n = 6). Five patients in the D1q3w arm had dose-limiting toxicities (DLT) during the maximum tolerated dose (MTD) evaluation period (cycle 1): one patient (45 mg) had grade 3 nausea that led to reduction of the brigimadlin dose; one patient (45 mg) had grade 3 thrombocytopenia that led to dose reduction; one patient (60 mg) had grade 3 enterocolitis and grade 3 nausea; one patient (80 mg) had grade 4 thrombocytopenia; and one patient (80 mg) had grade 3 febrile neutropenia, grade 3 anemia, grade 4 thrombocytopenia, and grade 4 neutropenia that led to dose reduction. No patient discontinued treatment due to a DLT in cycle 1.
Patients in the D1D8q4w arm received brigimadlin at seven dose levels: 5 mg (n = 3), 10 mg (n = 3), 15 mg (n = 3), 20 mg (n = 3), 30 mg (n = 4), 45 mg (n = 6), and 60 mg (n = 3). Three patients in the D1D8q4w arm had DLTs during the MTD evaluation period (cycle 1): one patient (45 mg) had grade 3 neutropenia and grade 4 thrombocytopenia, both of which led to dose reductions; one patient (60 mg) had grade 4 neutropenia and grade 4 thrombocytopenia that led to a dose reduction; and one patient (60 mg) had grade 2 thrombocytopenia and grade 3 neutropenia that led to a dose reduction. Again, no patient discontinued treatment due to a DLT in cycle 1.
Seven patients (six in D1q3w and one in D1D8q4w) had DLTs after the MTD evaluation period. In the D1q3w arm, these were one grade 3 nausea in cycle 2 (10 mg), one grade 4 thrombocytopenia in cycle 2 (80 mg), one grade 3 arterial embolism and grade 4 thrombocytopenia in cycle 2 (80 mg), one grade 3 fatigue in cycle 3 (50 mg), one grade 3 anemia in cycle 29 (20 mg), and one grade 2 anemia in cycle 31 (45 mg). In the D1D8q4w arm, there was only one DLT after the MTD evaluation period: one grade 4 neutropenia in cycle 4 (30 mg). Based on the DLTs reported, and the protocol-specified Bayesian logistic regression model (BLRM), the MTD was confirmed as 60 mg in the D1q3w arm and 45 mg in the D1D8q4w. The recommended dose for expansion (RDE) for the phase Ib dose expansion was selected as 45 mg q3w based on a supplementary BLRM analysis taking into account the adverse events (AE) of interest over the entire treatment period; the D1D8q4w schedule was not pursued, as no clear added benefit was seen while challenges with treatment adherence were reported.
Safety and Tolerability
All 54 enrolled patients were included in the safety population. The overall safety summary and most common treatment-related AEs (TRAE) are summarized in Table 2. All-cause AEs are summarized by grade in Supplementary Table S2. The safety profile of brigimadlin was consistent across the D1q3w and D1D8q4w arms (Table 2). Briefly, all 54 patients who received brigimadlin had an AE (data cutoff, October 24, 2022), and 33 (61.1%) patients had a grade ≥3 AE (Table 2). Fifty (92.6%) patients had investigator-reported TRAEs, of which nausea (74.1%) and vomiting (51.9%) were the most common; 25 (46.3%) had grade ≥3 TRAEs, of which thrombocytopenia (25.9%; 13.0% grade 3, 13.0% grade 4) and neutropenia (24.1%; 9.3% grade 3, 14.8% grade 4) were most common (Table 2). Eighteen patients (33.3%; nine in each arm) had a serious AE; these were mainly hematologic, including thrombocytopenia (three patients in D1q3w, three in D1D8q4w) and neutropenia (three patients in D1q3w).
Table 2.
Overall safety summary and most common investigator-reported TRAEs by highest CTCAE grade with brigimadlin monotherapy (occurring in ≥10% of patients in either arm)
| n (%) | D1q3w (n = 29) | D1D8q4w (n = 25) | All patients (N = 54) | |||
|---|---|---|---|---|---|---|
| Any AE | 29 (100.0) | 25 (100.0) | 54 (100.0) | |||
| Any grade ≥3 AE | 21 (72.4) | 12 (48.0) | 33 (61.1) | |||
| Any TRAE | 27 (93.1) | 23 (92.0) | 50 (92.6) | |||
| Any grade ≥3 TRAE | 17 (58.6) | 8 (32.0) | 25 (46.3) | |||
| DLTs (MTD evaluation period) | 5 (17.2) | 3 (12.0) | 8 (14.8) | |||
| Serious AEs (any cause) | 9 (31.0) | 9 (36.0) | 18 (33.3) | |||
| Any AE (any cause) leading to study drug dose reduction | 11 (37.9) | 8 (32.0) | 19 (35.2) | |||
| Any AE (any cause) leading to study drug discontinuation | 2 (6.9) | 1 (4.0) | 3 (5.6) | |||
| Most common TRAEs | All grades | Grade ≥3 | All grades | Grade ≥3 | All grades | Grade ≥3 |
|---|---|---|---|---|---|---|
| Nausea | 21 (72.4) | 4 (13.8) | 19 (76.0) | 0 | 40 (74.1) | 4 (7.4) |
| Vomiting | 13 (44.8) | 0 | 15 (60.0) | 1 (4.0) | 28 (51.9) | 1 (1.9) |
| Fatigue | 15 (51.7) | 1 (3.4) | 10 (40.0) | 0 | 25 (46.3) | 1 (1.9) |
| Thrombocytopenia | 15 (51.7) | 9 (31.0) | 9 (36.0) | 5 (20.0) | 24 (44.4) | 14 (25.9) |
| Decreased appetite | 10 (34.5) | 0 | 7 (28.0) | 0 | 17 (31.5) | 0 |
| Anemia | 12 (41.4) | 3 (10.3) | 4 (16.0) | 2 (8.0) | 16 (29.6) | 5 (9.3) |
| Neutropenia | 10 (34.4) | 8 (27.6) | 6 (24.0) | 5 (20.0) | 16 (29.6) | 13 (24.1) |
| Diarrhea | 8 (27.6) | 0 | 8 (32.0) | 0 | 16 (29.6) | 0 |
| Decreased white blood cell count | 9 (31.0) | 5 (17.2) | 4 (16.0) | 2 (8.0) | 13 (24.1) | 7 (13.0) |
| Alopecia | 6 (20.7) | 0 | 6 (24.0) | 0 | 12 (22.2) | 0 |
| Dysgeusia | 5 (17.2) | 0 | 5 (20.0) | 0 | 10 (18.5) | 0 |
| Decreased lymphocyte count | 5 (17.2) | 3 (10.3) | 2 (8.0) | 1 (4.0) | 7 (13.0) | 4 (7.4) |
| Gastroesophageal reflux disease | 2 (6.9) | 0 | 3 (12.0) | 0 | 5 (9.3) | 0 |
| Increased aspartate aminotransferase | 4 (13.8) | 0 | 1 (4.0) | 0 | 5 (9.3) | 0 |
| Decreased weight | 3 (10.3) | 0 | 1 (4.0) | 0 | 4 (7.4) | 0 |
| Increased alanine aminotransferase | 3 (10.3) | 0 | 0 | 0 | 3 (5.6) | 0 |
Abbreviation: CTCAE, Common Terminology Criteria for Adverse Events.
A total of 19 patients (11 in D1q3w, eight in D1D8q4w) had AEs (of any cause) leading to dose reductions, the most common being neutropenia (six in D1q3w, four in D1D8q4w), thrombocytopenia (four in D1q3w, four in D1D8q4w), and nausea (three in D1q3w, one in D1D8q4w). Of these 19 patients, nine patients did not have a DLT; the AEs leading to dose reductions in these nine patients were neutropenia, thrombocytopenia, nausea, fatigue, and diarrhea. Two patients in the D1q3w arm and one patient in the D1D8q4w arm discontinued due to AEs: in D1q3w, one patient (80 mg) had grade 3 arterial embolism and one (10 mg) had grade 3 nausea; in D1D8q4w, one patient (45 mg) had grade 1 nausea. There were no deaths due to AEs.
Pharmacokinetic Profile
Pharmacokinetic analysis showed that geometric mean plasma exposures [maximum plasma concentration (Cmax) and area under the curve from 0 to infinity (AUC0-inf)] increased with dose after the first dose in both treatment arms, with no significant deviation from linearity over the dose range 5 to 80 mg (Table 3). For both treatment arms, interpatient variability in exposure was moderate to high, with geometric coefficients of variation for AUC0-inf and Cmax geometric mean values ranging from 7.9% to 190% (Table 3).
Table 3.
Pharmacokinetic and pharmacodynamic parameters after the first dose of brigimadlin
| D1q3w (n = 29) | D1D8q4w (n = 25) | |
|---|---|---|
| C max, nmol/L | 1,160 (gCV% 7.9; 20 mg; n = 2)–4,800 (gCV% 51.0; 80 mg, n = 6) | 260 (gCV% 46.6; 5 mg; n = 3)–2,480 (gCV% 50.1; 60 mg, n = 3) |
| AUC0-inf | 113,000 (gCV% 46.8; 30 mg; n = 3)–339,000 (gCV% 77.3; 80 mg; n = 6) | 17,600 (gCV% 105; 5 mg; n = 3)–120,800 (gCV% 190; 60 mg; n = 3) |
| Median Tmax, h | 4–5.5 | 4–6 |
| Geometric mean clearance/F, mL/min | 6.7 (gCV% 77.3)–10.4 (gCV% 33.0) | 5.39 (gCV% 70.9)–13.2 (gCV% 190.0) |
| Geometric mean apparent volume of distribution/F, L | 23.5 (gCV% 31.3)–35.1 (gCV% 55.0) | 24.5 (gCV% 43.6)–49.0 (gCV% 126.0) |
| Geometric mean half-life, h | 35.5 (gCV% 10.3)–59.4 (gCV% 53.0) | 33.4 (gCV% 28.9)–55.3 (gCV% 49.6) |
| GDF-15 fold change from baseline | 18.1 (SD 4.22)–43.4 (SD 22.3) | 5.4 (SD 2.69)–35.5 (SD 32.5) |
NOTE: Geometric mean data calculated when data were available from ≥2 patients.
Abbreviations: gCV, geometric coefficient of variation; SD, standard deviation; Tmax, time to maximum drug concentration.
Pharmacodynamic Analysis
Peripheral concentration of growth differentiation factor 15 (GDF-15; a circulating protein considered a downstream marker of p53 and induced upon p53 activation) was used as a surrogate to determine target engagement of brigimadlin (14). As shown in Table 3, the fold change of GDF-15 concentrations from baseline increased 18.1- to 43.4-fold with the D1qw3 schedule, and from 5.4- to 35.5-fold with the D1D8q4w schedule. Time- and dose-dependent curves of changes in GDF-15 levels were observed across all dose-escalation cohorts in both treatment arms (Supplementary Fig. S1A and S1B).
Antitumor Activity
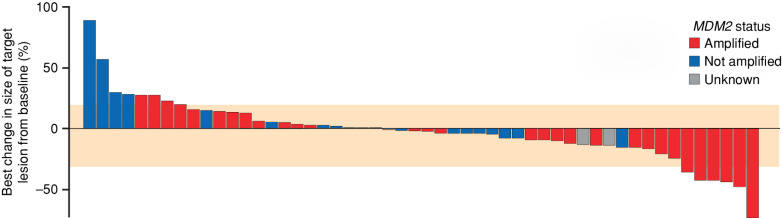
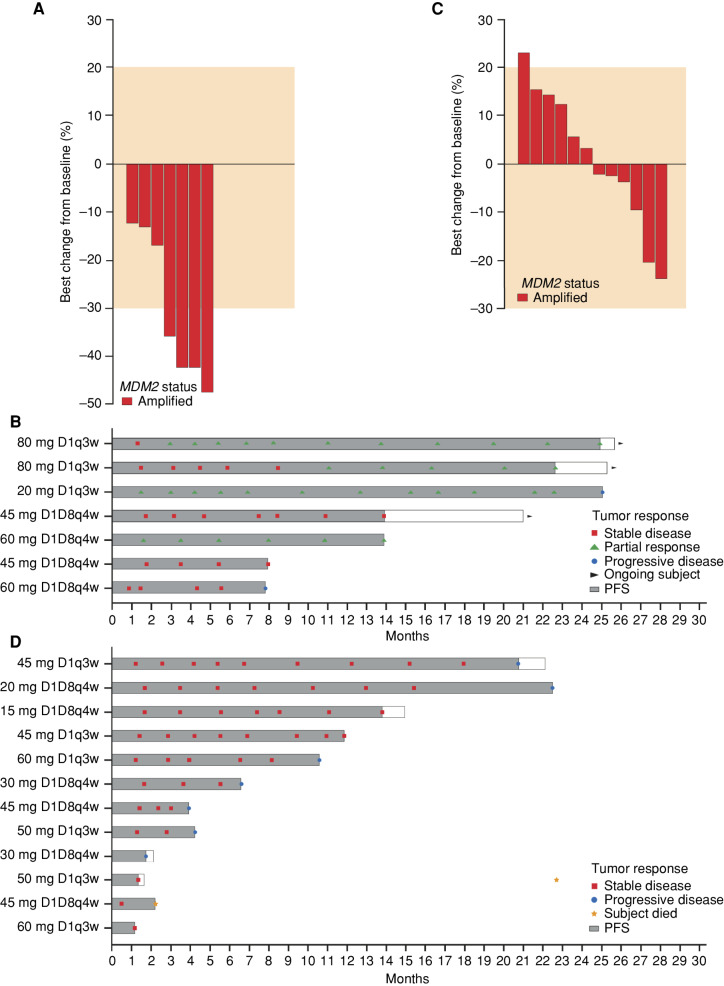
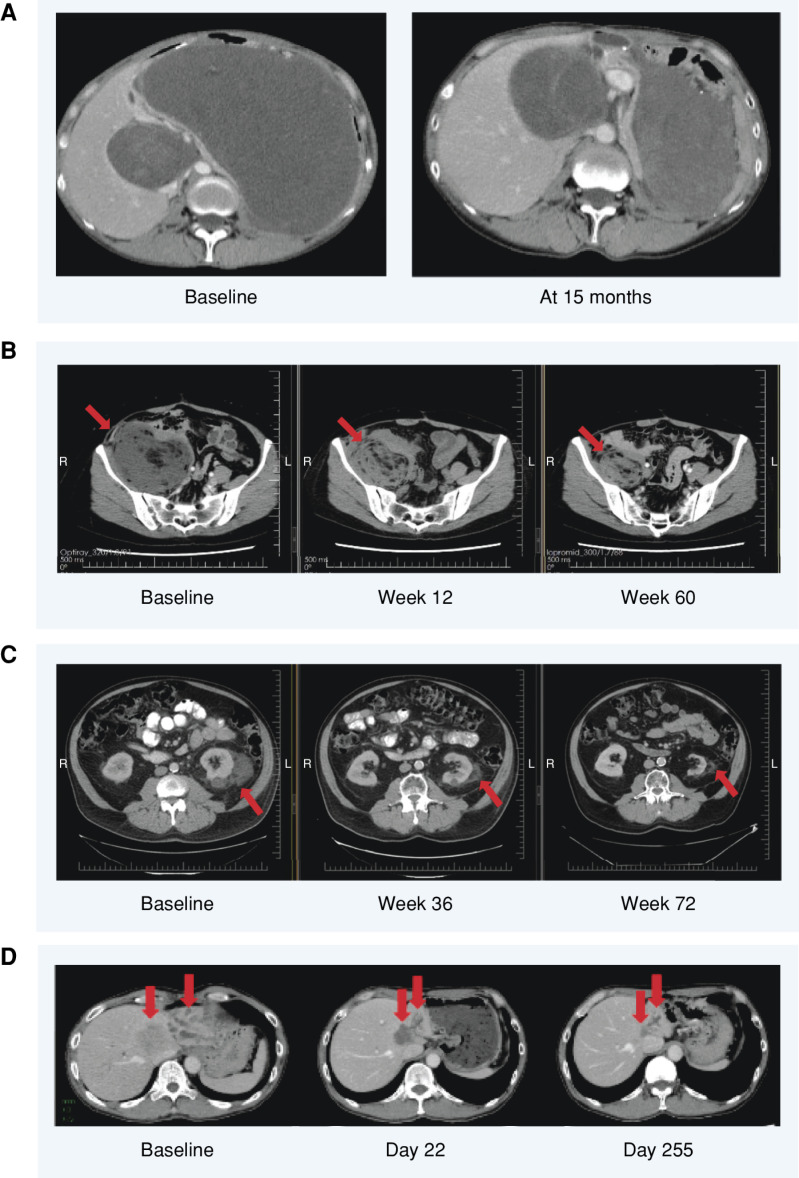
At data cutoff (October 24, 2022), six of 54 patients (four in D1q3w and two in D1D8q4w) had achieved a partial response (11.1% overall response rate; 13.8% and 8.0% in D1q3w and D1D8q4w, respectively; Table 4; Fig. 1; Supplementary Fig. S2). A further 34 patients (18 in D1q3w and 16 in D1D8q4w) achieved stable disease as best response, giving a disease control rate of 74.1% (75.9% and 72.0% in the D1q3w and D1D8q4w arms, respectively). Of seven patients with WDLPS, four achieved a partial response (all ≥12 months duration, ranging up to about 25 months; Fig. 2A and B) and three patients achieved stable disease (>14 months duration for one patient, ∼8 months for the other two patients), giving a 100% disease control rate. The other two partial responses were seen in a patient with intrahepatic cholangiocarcinoma (duration of response ∼12 months) and a patient with pancreatic cancer (duration of response >5.5 months). All patients with partial response had MDM2-amplified tumors. Of note, nine of the 12 patients with DDLPS achieved stable disease (75.0% disease control rate), with duration of stable disease ranging from ∼1.5 to 22 months (Fig. 2C and D). Example patient scans showing responses and sustained disease stabilizations are shown in Fig. 3A–D.
Table 4.
Best overall response in patients receiving brigimadlin monotherapy
| D1q3w (n = 29) | D1D8q4w (n = 25) | All patients (N = 54) | |
|---|---|---|---|
| Total treated, n | 29 | 25 | 54 |
| Confirmed objective response, n (%) | 4 (13.8) | 2 (8.0) | 6 (11.1) |
| Complete response, n (%) | 0 | 0 | 0 |
| Partial response, n (%) | 4 (13.8) | 2 (8.0) | 6 (11.1) |
| Stable disease, n (%) | 18 (62.1) | 16 (64.0) | 34 (63.0) |
| Progressive disease, n (%) | 6 (20.7) | 5 (20.0) | 11 (20.4) |
| Not evaluable, n (%) | 1 (3.4) | 2 (8.0) | 3 (5.6) |
| Disease control, n (%) | 22 (75.9) | 18 (72.0) | 40 (74.1) |
Figure 1.
Efficacy of brigimadlin in patients with advanced/metastatic solid tumors in phase Ia. Best change in size of target lesion from baseline in all patients enrolled to phase Ia.
Figure 2.
Efficacy in patients with WDLPS and DDLPS. A, Best change in the size of target lesion from baseline in patients with WDLPS. B, Time on treatment and progression-free survival (PFS) in patients with WDLPS. C, Best change in size of target lesion from baseline in patients with DDLPS. D, Time on treatment and PFS in patients with DDLPS. In C and D, the length of the bars indicates time on treatment and the shaded part of each bar indicates PFS. D, day.
Figure 3.
Example patient scans showing responses and sustained disease stabilizations with brigimadlin. A, A 54-year-old female with a retroperitoneal MDM2-amplified WDLPS. The patient was heavily pretreated before being enrolled in the present trial, in which she received brigimadlin 20 mg q3w. The patient experienced a partial response (31% tumor reduction) starting at cycle 2. At cycle 10, the dose was reduced to 10 mg due to grade 2 neutropenia not recovering within 14 days. At cycle 19, a further tumor shrinkage (47% reduction) was observed. At cycle 29, the dose was further reduced to 5 mg due to grade 3 anemia. Treatment was finally discontinued after cycle 33 due to progressive disease. B, A 53-year-old female with a retroperitoneal MDM2-amplified WDLPS first diagnosed in July 2010 who, after four surgical resections, received doxorubicin for 6 cycles starting in March 2020 before progressing and being enrolled to the present trial. The patient received brigimadlin 80 mg D1q3w and experienced a partial response at cycle 3 (32% tumor reduction). The dose was reduced to 60 mg at cycle 4 due to neutropenia, to 50 mg at cycle 5 due to neutropenia, to 45 mg at cycle 8 due to thrombocytopenia, then to 30 mg at cycle 12 (December 2021) due to neutropenia, and finally to 20 mg at cycle 20 due to neutropenia. At data cutoff, the patient was ongoing in the study with a partial response (42% best tumor reduction, more than 25 months on treatment). C, A 65-year-old male with stage IV MDM2-amplified left perirenal DDLPS. Following previous treatment with adriamycin and olaratumab, followed by radiotherapy, the patient received brigimadlin 45 mg q3w. The patient achieved stable disease and stayed on treatment for nearly 2 years before experiencing progressive disease. D, A 51-year-old male with MDM2-amplified cholangiocarcinoma. Following 3 prior lines of therapy, he received brigimadlin 80 mg q3w, which was reduced to 45 mg q3w for 38 days in cycle 2 due to grade 4 thrombocytopenia and grade 4 neutropenia. The patient achieved a partial response by day 22, which was still evident on day 360; maximum tumor shrinkage was −73%. The patient remained on treatment for 13.3 months before experiencing progressive disease. B–D, The red arrows indicate the tumor sites. L, left; R, right.
In a preliminary analysis, median progression-free survival (PFS) was 8.1 months [95% confidence interval (CI): 3.8–13.5] overall: 10.6 months (95% CI: 3.0–20.7) in the D1q3w arm and 8.0 months (95% CI: 3.7–18.5) in the D1D8q4w arm. At the data cutoff (October 24, 2022), three patients (two in D1q3w and one in D1D8q4w) remained on treatment. All seven patients with WDLPS achieved PFS >7.5 months; of these, five patients achieved PFS ≥14 months. In the 12 patients with DDLPS, PFS ranged from ∼1.5 to 22 months, and five of the 12 (41.6%) patients with DDLPS achieved PFS >10.5 months.
DISCUSSION
These results demonstrate that brigimadlin has a manageable safety profile and shows encouraging signs of efficacy in patients with advanced/metastatic solid tumors, particularly those with MDM2-amplified WDLPS or DDLPS. On the basis of DLTs during cycle 1 and the primary BLRM analysis, the MTDs were selected as 60 mg in the D1q3w arm and 45 mg in the D1D8q4w arm. Considering the AEs of interest over the entire treatment period, based on a supplementary BLRM analysis, the RDE for the phase Ib dose-expansion part was selected as 45 mg q3w; the phase Ib dose expansion is ongoing with two cohorts: one for patients with TP53 wild-type, MDM2-amplified sarcoma and one for patients with TP53 wild-type, MDM2-amplified non–small cell lung cancer, urothelial carcinoma, gastric carcinoma, biliary tract carcinoma, or pancreatic ductal adenocarcinoma.
Consistent with early-phase data for other MDM2–p53 antagonists in development (15–19), the observed AEs were typically gastrointestinal and hematologic, and no new safety signal has been observed. Across both treatment arms, the most common TRAEs were nausea (74.1%) and vomiting (51.9%), but these were manageable with antiemetic prophylaxis/treatment. Consistent with the role of MDM2 in normal hematopoiesis (4), the most common grade ≥3 TRAEs were thrombocytopenia (25.9%) and neutropenia (24.1%), but these events were manageable, and no patient discontinued treatment with brigimadlin due to a hematologic TRAE.
Pharmacokinetic analysis showed that mean plasma exposures (Cmax and AUC0-inf) increased with dose and showed no significant deviation from linearity in the dose range 10 to 60 mg. Importantly, the long half-life (30–60 hours) of brigimadlin allows for an intermittent schedule with oral administration once every 21 days. In addition to potentially increasing patient convenience and treatment adherence, this intermittent administration seems to contribute to the manageable safety profile of brigimadlin. Of note, thrombocytopenia has been a major challenge for many previous MDM2 antagonists but appears manageable with brigimadlin, possibly due to the intermittent dosing and different pharmacokinetic profile, although more data and longer follow-up are warranted. In support of the mechanism of action of brigimadlin, target engagement was demonstrated by increased levels of GDF-15, which showed a dose- and time-dependent relationship. However, the dataset is too small to conclude whether the observed interpatient variability in exposure translates into a variability of the pharmacodynamic modulation of GDF-15. As GDF-15 is a transcriptional target of p53, this demonstrates the restoration of p53 function with brigimadlin-mediated MDM2–p53 antagonism.
Consistent with previously reported preclinical evidence showing brigimadlin had antitumor activity in patient-derived xenografts (12, 13), brigimadlin showed encouraging preliminary efficacy in patients with advanced/metastatic solid tumors (overall response rate of 11.1%, disease control rate of 74.1%), particularly those with MDM2-amplified tumors. Brigimadlin is one of the most potent MDM2 antagonists, as shown by unprecedented potency in vitro (IC50 of 12 nmol/L in SJSA-1 proliferation assay; ref. 20) and has an unusually long half-life for an oral compound (up to 60 hours), which enables patients to receive a single dose in each cycle, thereby allowing enough time for the platelet and neutrophil levels to recover. This results in antitumor efficacy and long-term tolerability of brigimadlin treatment.
The efficacy data were particularly favorable in patients with liposarcoma, all of whom had MDM2-amplified disease, specifically WDLPS and DDLPS (disease control rates of 100% and 75%, respectively, and durable responses of ≥12 months to up to 2 years in four WDLPS patients). This is in line with reported preclinical evidence (12) and the high frequency of MDM2 amplification in these patients (8, 21). The preliminary efficacy in patients with advanced/metastatic MDM2-amplified WDLPS and DDLPS is particularly important given that chemotherapy remains the standard of care for these patients (22, 23), despite it being associated with generally poor tolerability, limited efficacy, and disappointing patient outcomes (22–24). For example, in patients with WDLPS and DDLPS, doxorubicin is associated with overall response rates of 9% to 11%, and median PFS and overall survival of approximately 2 to 4 months and 9 months, respectively (22, 25); however, most of the responses are seen in patients with DDLPS, while WDLPS is generally considered resistant to chemotherapy (22, 25). The durable partial responses seen in patients with WDLPS and sustained disease control in patients with DDLPS are particularly encouraging (Fig. 2).
Of note, a durable partial response (∼12 months) was also seen in a patient with MDM2-amplified intrahepatic cholangiocarcinoma. MDM2 amplification has been detected in approximately 6% of patients with biliary tract carcinomas (26), and, as treatment options are limited for these patients and survival rates remain low (27), further investigation of brigimadlin in patients with intrahepatic cholangiocarcinoma and other biliary tract carcinomas is warranted. Further, a sustained (>5.5 months) partial response was seen in a patient with MDM2-amplified pancreatic adenocarcinoma. Although phase Ia efficacy data are preliminary and further follow-up is needed, these results, together with the encouraging efficacy seen in patients with WDLPS and DDLPS, suggest that brigimadlin has antitumor activity across a range of MDM2-amplified tumors and warrants further investigation regardless of histology.
In summary, brigimadlin showed a manageable safety profile and encouraging signs of antitumor activity in patients with advanced/metastatic MDM2-amplified solid tumors, particularly in patients with DDLPS and WDLPS. Investigation of brigimadlin monotherapy is continuing with the ongoing phase Ib dose-expansion part of this study and two later-phase studies: the randomized phase II/III Brightline-1 study (NCT05218499) assessing brigimadlin versus doxorubicin as first-line treatment in patients with advanced DDLPS (28), for which the FDA has granted a Fast Track designation status, and the phase II Brightline-2 study (NCT05512377) assessing brigimadlin as second-line treatment in patients with MDM2-amplified biliary tract or pancreatic cancers.
METHODS
Brigimadlin Structure and Synthesis
The structure of brigimadlin has recently been presented (20). Synthesis of brigimadlin is outlined in patent application WO 2017/060431 (compound Ia-34).
Patients
All patients were ages ≥18 years (≥20 years in Japan) with pathologically documented advanced or metastatic solid tumors who had experienced disease progression or relapse during or after previous standard-of-care treatment, or for whom no standard-of-care treatment was available. In phase Ia, although TP53 determination was not required, all patients had TP53 wild-type status or unknown TP53 status, and patients with a TP53 mutation were not eligible. Similarly, known MDM2 amplification status was not a requirement for enrollment to phase Ia. Additional eligibility criteria included Eastern Cooperative Oncology Group performance status 0 or 1 and adequate organ function. Key exclusion criteria were previous treatment with brigimadlin or any other MDM2–p53 antagonist and active or untreated brain metastases. Full eligibility criteria are listed in the Supplementary Methods.
Study Design
This global, multicenter, open-label, phase Ia/Ib dose-escalation/dose-expansion trial (NCT03449381) assessed brigimadlin monotherapy in adult patients with advanced or metastatic solid tumors. In the phase Ia dose-escalation part, patients were recruited at six sites in Canada, Japan, and the United States between June 20, 2018, and December 3, 2020. The trial aimed to investigate the MTD based on DLTs during the first treatment cycle and the RDE, safety and tolerability, pharmacokinetics, pharmacodynamics, and preliminary efficacy of brigimadlin monotherapy in patients with advanced or metastatic solid tumors. Patients were assigned to one of the treatment arms (D1q3w and D1D8q4w) by rotation/slot allocation in order of site initiation. Participating investigators were informed of their slot assignments and provided time to identify a potential patient. In some cases, if a patient could not be identified, the slot would become competitive for all investigators to identify a potential patient and enroll.
In phase Ia, the primary endpoint was the number of patients experiencing DLTs in the first treatment cycle (21 days in the D1q3w arm or 28 days in the D1D8q4w arm) and the MTD based on the number of patients with DLTs during the first treatment cycle. The MTD was defined as the highest dose with less than 25% risk of the true DLT rate being equal to or above 33%. A BLRM based on the number of patients with DLTs during the first treatment cycle was used for the estimation of the MTD for both treatment arms. The RDE was selected based on a supplementary BLRM analysis, taking into account the AEs of interest during the entire treatment period: hematologic DLTs, hematologic AEs grade 4, hematologic AEs leading to dose delay/dose reduction/discontinuation, time for platelet count recovery (to over 100,000/mm3) longer than 21 days, and time for neutrophil count recovery (to over 1,500/mm3) longer than 21 days. Secondary endpoints in phase Ia included pharmacokinetic (Cmax and AUC) and pharmacodynamic parameters, objective response, disease control, duration of response, and the number of patients with DLTs during the entire treatment period. The study was conducted in accordance with the Declaration of Helsinki and Good Clinical Practice guidelines, it was approved by all relevant institutional review boards, and all patients provided written informed consent.
Treatment
In phase Ia dose escalation, patients received escalating doses of brigimadlin (oral administration) on day 1 of 21-day cycles (D1q3w) or days 1 and 8 of 28-day cycles (D1D8q4w). The starting dose in the D1q3w arm was 10 mg; the starting dose in the D1D8q4w arm was 50% of the dose level at which ≥2 National Cancer Institute (NCI) Common Terminology Criteria for Adverse Events (CTCAE) grade ≥2 non–dose-limiting AEs were observed in D1q3w. Dose escalation was guided by a BLRM with overdose control. Treatment continued until disease progression, unacceptable toxicity, or other reasons requiring treatment discontinuation.
Antiemetic prophylaxis (prevention of higher severity, dose reduction, or discontinuation) and treatment should be conducted in line with established international and local guidelines based on the emetogenic risk level, including, for example, serotonin receptor antagonists, metoclopramide, prochlorperazine, or thiethylperazine. Due to potential drug–drug interactions with many antiemetic agents, investigators must check frequently the occurrence of signs or symptoms that might be a consequence of a drug–drug interaction when using antiemetic regimens concomitantly with brigimadlin.
Assessments
Safety was assessed by descriptive analysis of the incidence and severity of AEs, graded per NCI CTCAE version 5.0. DLTs were defined as per the criteria in the Supplementary Methods.
Blood samples for pharmacokinetic and pharmacodynamic analyses were collected 5 minutes before and 1, 2, 3, 4, 5, 6, and 8 hours after brigimadlin administration on day 1, cycle 1, and then once on days 2, 3, 4, 5, and 8 of cycle 1. In cycles 2 and beyond, samples were collected 5 minutes before and 6 hours after brigimadlin administration on day 1, followed by once on day 2, and, in cycle 2, on days 3 and 8.
Tumor assessments were performed at screening, every 6 weeks (42 ± 7 days) in the D1q3w arm and every 8 weeks (56 ± 7 days) in the D1D8q4w arm for the first 6 months, followed by every 12 weeks (84 ± 7 days) thereafter until progressive disease or the start of subsequent anticancer treatment. Response was evaluated by the investigator per Response Evaluation Criteria in Solid Tumors v1.1 criteria.
Statistical Analysis
Sample size estimation for phase Ia was based on a simulation study using a BLRM, which relied on the assumption of a dose-toxicity correlation model as well as a number of prespecified dose levels. However, due to the exploratory and adaptive nature of this type of dose-escalation trial, the sample size estimation was approximate and the actual sample size was based on the observed safety data. Dose escalation was guided by a BLRM, with overdose control based on DLTs observed in cycle 1 (29). During the trial, the BLRM recommended dose for the next dose level was the highest level with the highest posterior probability of the DLT rate falling in the target interval (0.16, 0.33) among the doses fulfilling overdose control. The maximum allowable dose increment for the subsequent cohort could be no more than 50% from cohort to cohort after a grade ≥2 AE was observed at cycle 1. Pharmacokinetic parameters were analyzed by noncompartmental analysis. Time-to-event endpoints were analyzed using Kaplan–Meier curves; response rates were analyzed descriptively.
Data Availability
To ensure independent interpretation of clinical study results and enable authors to fulfill their role and obligations under the International Committee of Medical Journal Editors criteria, Boehringer Ingelheim grants all external authors access to clinical study data pertinent to the development of the publication. In adherence with the Boehringer Ingelheim Policy on Transparency and Publication of Clinical Study Data, scientific and medical researchers can request access to clinical study data when it becomes available on https://vivli.org/, and earliest after publication of the primary manuscript in a peer-reviewed journal, regulatory activities are complete, and other criteria are met. Please visit https://www.mystudywindow.com/msw/datasharing for further information.
Supplementary Material
Criteria for enrollment and dose-limiting toxicities
Study representativeness table
Most common any-cause adverse events by highest CTCAE grade with BI 907828 monotherapy
GDF-15 fold change from baseline for dose-escalation cohorts receiving BI 907828 D1q3w and BI 907828 D1D8q4w
Time on treatment and PFS in all patients enrolled to phase Ia
Acknowledgments
The authors thank the patients and their families, as well as the investigators and staff at the participating sites. The authors also thank Maren Rohrbacher, Rolf Grempler, Reinhard Sailer, Sara Durland-Busbice, and Yuefen Tang for their contributions to the data generation and analysis, as well as Mahmoud Ould-Kaci for his advice and contribution to study design. This study was funded by Boehringer Ingelheim. The authors were fully responsible for all content and editorial decisions, were involved at all stages of manuscript development, and have approved the final version. The authors did not receive payment related to the development of the manuscript. Medical writing support for the development of this manuscript, under the direction of the authors, was provided by Jane Saunders, of Ashfield MedComms, an Inizio Company, and funded by Boehringer Ingelheim.
The publication costs of this article were defrayed in part by the payment of publication fees. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Footnotes
Note: Supplementary data for this article are available at Cancer Discovery Online (http://cancerdiscovery.aacrjournals.org/).
Authors’ Disclosures
P. LoRusso reports personal fees from AbbVie, Agios, Five Prime, Genmab, Halozyme, CytomX, Takeda, SOTIO, Cybrexa, Agenus, Tyme, IQVIA, TRIGR, Pfizer, ImmunoMet, Black Diamond, GSK, QED Therapeutics, AstraZeneca, EMD Serono, Shattuck, Astellas, Salarius, Silverback, MacroGenics, Kyowa Kirin, Kineta, Zentalis, Molecular Templates, ABL Bio, SK Life Science, STCube, Bayer, I-Mab, Seagen, imCheck, Relay Therapeutics, Stemline, Compass BADX, Mekanist, Mersana Therapeutics, BAKX Therapeutics, Scenic Biotech, Qualigen, Roivant Sciences, NeuroTrials, Actuate Therapeutics, and Genentech and other support from Roche/Genentech outside the submitted work. N. Yamamoto reports grants from Astellas, Chugai, Eisai, Taiho, Bristol Myers Squibb, Pfizer, Novartis, Eli Lilly, AbbVie, Daiichi Sankyo, Bayer, Boehringer Ingelheim, Kyowa Kirin, Takeda, ONO, Janssen Pharma, MSD, Merck, GSK, Sumitomo Pharma, Chiome Bioscience, Otsuka, Carna Biosciences, Genmab, Shionogi, TORAY, KAKEN, AstraZeneca, Cmic, InventisBio, and Rakuten Medical, and personal fees from Eisai, Takeda, Boehringer Ingelheim, Cmic, Chugai (advisory role and speaker honoraria), Merck, Healios, ONO, Daiichi Sankyo, and Eisai outside the submitted work. M.R. Patel reports other support from Boehringer Ingelheim during the conduct of the study. S.A. Laurie reports other support from Boehringer Ingelheim during the conduct of the study, as well as personal fees from Sanofi, Bayer, and UpToDate outside the submitted work. T.M. Bauer reports grants from Boehringer Ingelheim during the conduct of the study, as well as grants and personal fees from Pfizer, Lilly, Bayer, AstraZeneca, and Bristol Myers Squibb outside the submitted work. J. Geng reports a patent for US20230058171A1 pending. M. Teufel reports personal fees from Boehringer Ingelheim during the conduct of the study. J. Li reports other support from Boehringer Ingelheim during the conduct of the study. M.M. Gounder reports grants and personal fees from Boehringer Ingelheim during the conduct of the study, as well as grants and personal fees from Ayala, Daiichi Sankyo, Bayer, Epizyme, Karyopharm, and Rain Oncology, personal fees from Aadi Biosciences, Regeneron, and TYME, and grants from Springworks outside the submitted work. No disclosures were reported by the other authors.
Authors’ Contributions
P. LoRusso: Conceptualization, resources, data curation, investigation, writing–original draft, writing–review and editing, development of the study design. N. Yamamoto: Investigation, writing–review and editing. M.R. Patel: Resources, supervision, investigation, writing–review and editing. S.A. Laurie: Investigation, writing–review and editing, enrolled patients, safety review. T.M. Bauer: Investigation, writing–review and editing. J. Geng: Conceptualization, formal analysis, investigation, writing–review and editing, development of the study design. T. Davenport: Investigation, project administration, writing–review and editing. M. Teufel: Formal analysis, investigation, writing–review and editing. J. Li: Formal analysis, investigation, writing–review and editing. M. Lahmar: Conceptualization, investigation, project administration, writing–review and editing. M.M. Gounder: Conceptualization, supervision, investigation, methodology, writing–review and editing.
References
- 1. Zhao Y, Yu H, Hu W. The regulation of MDM2 oncogene and its impact on human cancers. Acta Biochim Biophys Sin 2014;46:180–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Joerger AC, Fersht AR. The p53 pathway: origins, inactivation in cancer, and emerging therapeutic approaches. Annu Rev Biochem 2016;85:375–404. [DOI] [PubMed] [Google Scholar]
- 3. Zhu H, Gao H, Ji Y, Zhou Q, Du Z, Tian L, et al. Targeting p53-MDM2 interaction by small-molecule inhibitors: learning from MDM2 inhibitors in clinical trials. J Hematol Oncol 2022;15:91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tisato V, Voltan R, Gonelli A, Secchiero P, Zauli G. MDM2/X inhibitors under clinical evaluation: perspectives for the management of hematological malignancies and pediatric cancer. J Hematol Oncol 2017;10:133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Momand J, Jung D, Wilczynski S, Niland J. The MDM2 gene amplification database. Nucleic Acids Res 1998;26:3453–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Kato S, Ross JS, Gay L, Dayyani F, Roszik J, Subbiah V, et al. Analysis of MDM2 amplification: next-generation sequencing of patients with diverse malignancies. JCO Precis Oncol 2018;2018: PO.17.00235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Dembla V, Somaiah N, Barata P, Hess K, Fu S, Janku F, et al. Prevalence of MDM2 amplification and coalterations in 523 advanced cancer patients in the MD Anderson phase 1 clinic. Oncotarget 2018;9:33232–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Asano N, Yoshida A, Mitani S, Kobayashi E, Shiotani B, Komiyama M, et al. Frequent amplification of receptor tyrosine kinase genes in welldifferentiated/dedifferentiated liposarcoma. Oncotarget 2017;8:12941–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Pilotti S, Della Torre G, Lavarino C, Di Palma S, Sozzi G, Minoletti F, et al. Distinct MDM2/p53 expression patterns in liposarcoma subgroups: implications for different pathogenetic mechanisms. J Pathol 1997;181:14–24. [DOI] [PubMed] [Google Scholar]
- 10. Kim YJ, Kim M, Park HK, Yu DB, Jung K, Song K, et al. Co-expression of MDM2 and CDK4 in transformed human mesenchymal stem cells causes high-grade sarcoma with a dedifferentiated liposarcoma-like morphology. Lab Invest 2019;99:1309–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Thway K. Well-differentiated liposarcoma and dedifferentiated liposarcoma: an updated review. Semin Diagn Pathol 2019;36:112–21. [DOI] [PubMed] [Google Scholar]
- 12. Cornillie J, Wozniak A, Li H, Gebreyohannes YK, Wellens J, Hompes D, et al. Anti-tumor activity of the MDM2-TP53 inhibitor BI-907828 in dedifferentiated liposarcoma patient-derived xenograft models harboring MDM2 amplification. Clin Transl Oncol 2020;22:546–54. [DOI] [PubMed] [Google Scholar]
- 13. Rudolph D, Gollner A, Blake S, Rinnenthal J, Wernitznig A, Weyer-Czernilofsky U, et al. BI 907828: a novel, potent MDM2 inhibitor that is suitable for high-dose intermittent schedules [abstract]. In: Proceedings of the American Association for Cancer Research Annual Meeting 2018; 2018Apr 14–18; Chicago, IL. Philadelphia (PA): AACR; Cancer Res 2018;78(13 Suppl):Abstract nr 4868. [Google Scholar]
- 14. Bauer S, Demetri GD, Halilovic E, Dummer R, Meille C, Tan DSW, et al. Pharmacokinetic-pharmacodynamic guided optimisation of dose and schedule of CGM097, an HDM2 inhibitor, in preclinical and clinical studies. Br J Cancer 2021;125:687–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Takahashi S, Fujiwara Y, Nakano K, Shimizu T, Tomomatsu J, Koyama T, et al. Safety and pharmacokinetics of milademetan, a MDM2 inhibitor, in Japanese patients with solid tumors: a phase I study. Cancer Sci 2021;112:2361–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McKean M, Tolcher AW, Reeves JA, Chmielowski B, Shaheen MF, Beck JT, et al. Newly updated activity results of alrizomadlin (APG-115), a novel MDM2/p53 inhibitor, plus pembrolizumab: Phase 2 study in adults and children with various solid tumors. J Clin Oncol 40, 2022. (suppl 16; abstr 9517). [Google Scholar]
- 17. Italiano A, Miller WH Jr, Blay JY, Gietema JA, Bang YJ, Mileshkin LR, et al. Phase I study of daily and weekly regimens of the orally administered MDM2 antagonist idasanutlin in patients with advanced tumors. Invest New Drugs 2021;39:1587–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Ray-Coquard I, Blay JY, Italiano A, Le Cesne A, Penel N, Zhi J, et al. Effect of the MDM2 antagonist RG7112 on the P53 pathway in patients with MDM2-amplified, well-differentiated or dedifferentiated liposarcoma: an exploratory proof-of-mechanism study. Lancet Oncol 2012;13:1133–40. [DOI] [PubMed] [Google Scholar]
- 19. Gounder MM, Bauer TM, Schwartz GK, Weise AM, LoRusso P, Kumar P, et al. A first-in-human phase i study of milademetan, an MDM2 inhibitor, in patients with advanced liposarcoma, solid tumors, or lymphomas. J Clin Oncol 2023;41:1714–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Gollner A, Sini P, Rudolph D, Weinstabl H, Ramharter J, Weyer-Czernilofsky U, et al. BI 907828: a highly potent MDM2-p53 antagonist suitable for intermittent dose schedules [abstract]. In: Proceedings of the American Association for Cancer Research Annual Meeting 2023; Part 2 (Clinical Trials and Late-Breaking Research); 2023 Apr 14–19; Orlando, FL. Philadelphia (PA): AACR; Cancer Res 2023;83(8_Suppl):Abstract nr LB003. [Google Scholar]
- 21. Gounder MM, Agaram NP, Trabucco SE, Robinson V, Ferraro RA, Millis SZ, et al. Clinical genomic profiling in the management of patients with soft tissue and bone sarcoma. Nature Comm 2022;13:3406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Schöffski P. Established and experimental systemic treatment options for advanced liposarcoma. Oncol Res Treat 2022;45:525–43. [DOI] [PubMed] [Google Scholar]
- 23. Gronchi A, Miah AB, Dei Tos AP, Abecassis N, Bajpai J, Bauer S, et al. Soft tissue and visceral sarcomas: ESMO-EURACAN-GENTURIS clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 2021;32:1348–65. [DOI] [PubMed] [Google Scholar]
- 24. Gamboa AC, Gronchi A, Cardona K. Soft-tissue sarcoma in adults: an update on the current state of histiotype-specific management in an era of personalized medicine. CA Cancer J Clin 2020;70:200–29. [DOI] [PubMed] [Google Scholar]
- 25. Jones RL, Fisher C, Al-Muderis O, Judson IR. Differential sensitivity of liposarcoma subtypes to chemotherapy. Eur J Cancer 2005;41:2853–60. [DOI] [PubMed] [Google Scholar]
- 26. Kim SJ, Akita M, Sung YN, Fujikura K, Lee JH, Hwang S, et al. MDM2 amplification in intrahepatic cholangiocarcinomas: its relationship with large-duct type morphology and uncommon KRAS mutations. Am J Surg Pathol 2018;42:512–21. [DOI] [PubMed] [Google Scholar]
- 27. Koshiol J, Yu B, Kabadi SM, Baria K, Shroff RT. Epidemiologic patterns of biliary tract cancer in the United States: 2001–2015. BMC Cancer 2022;22:1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Schöffski P. Brightline-1: phase II/III trial of the MDM2–p53 antagonist BI 907828 versus doxorubicin in patients with advanced DDLPS. Future Oncol 2023;19:621–9. [DOI] [PubMed] [Google Scholar]
- 29. Neuenschwander B, Branson M, Gsponer T. Critical aspects of the Bayesian approach to phase I cancer trials. Stat Med 2008;27:2420–39. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Criteria for enrollment and dose-limiting toxicities
Study representativeness table
Most common any-cause adverse events by highest CTCAE grade with BI 907828 monotherapy
GDF-15 fold change from baseline for dose-escalation cohorts receiving BI 907828 D1q3w and BI 907828 D1D8q4w
Time on treatment and PFS in all patients enrolled to phase Ia
Data Availability Statement
To ensure independent interpretation of clinical study results and enable authors to fulfill their role and obligations under the International Committee of Medical Journal Editors criteria, Boehringer Ingelheim grants all external authors access to clinical study data pertinent to the development of the publication. In adherence with the Boehringer Ingelheim Policy on Transparency and Publication of Clinical Study Data, scientific and medical researchers can request access to clinical study data when it becomes available on https://vivli.org/, and earliest after publication of the primary manuscript in a peer-reviewed journal, regulatory activities are complete, and other criteria are met. Please visit https://www.mystudywindow.com/msw/datasharing for further information.