Abstract
Objectives
Technological advancements that use global positioning system (GPS), such as geofencing, provide the opportunity to examine place-based context in population health research. This review aimed to systematically identify, assess and synthesise the existing evidence on geofencing intervention design, acceptability, feasibility and/or impact.
Design
Scoping review, using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews guidance for reporting.
Data sources
PubMed, CINAHL, EMBASE, Web of Science, Cochrane and PsycINFO for articles in English published up to 31 December 2021.
Eligibility criteria
Articles were included if geofencing was used as a mechanism for intervention delivery. Exclusion criteria: (1) a component or combination of GPS, geographical information system or ecological momentary assessment was used without delivery of an intervention; (2) did not include a health or health-related outcome from the geofencing intervention; or (3) was not a peer-reviewed study.
Data extraction and synthesis
Several researchers independently reviewed all abstracts and full-text articles for final inclusion.
Results
A total of 2171 articles were found; after exclusions, nine studies were included in the review. The majority were published in 5 years preceding the search (89%). Geofences in most studies (n=5) were fixed and programmed in the mobile application carried by participants without their input. Mechanisms of geofencing interventions were classified as direct or indirect, with five studies (56%) using direct interventions. There were several different health outcomes (from smoking to problematic alcohol use) across the five studies that used a direct geofencing intervention.
Conclusions
This scoping review found geofencing to be an emerging technology that is an acceptable and feasible intervention applied to several different populations and health outcomes. Future studies should specify the rationale for the locations that are geofenced and user input. Moreover, attention to mechanisms of actions will enable scientists to understand not only whether geofencing is an appropriate and effective intervention but why it works to achieve the outcomes observed.
Keywords: epidemiology, HIV & AIDS, mental health, public health
STRENGTHS AND LIMITATIONS OF THIS STUDY.
The scoping review was comprehensive, using rigorous searches of six databases.
The review used the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews checklist to guide reporting.
Most of the eligible studies were conducted in the USA, limiting generalisability to other international settings.
The review was conducted through the published literature through 2021 and therefore does not include more recent publications.
Introduction
Population health outcomes and health disparities result from multilevel factors beyond the individual. For example, poverty can lead to a lack of access to healthy food1 and medical care2; unstable housing can lead to inability to adhere to medications3 and exposures to unhealthy environments4; homophobia and racism leads to stigma and discrimination, and mistrust and avoidance of medical systems.5–7
Often in behavioural research, theories or frameworks do not consider the place-based context of behaviour despite literature on the consistent and enduring impact of places such as neighbourhoods and communities on population health outcomes and disparities.8–10 Place-based context can be conceptualised as both geographical areas defined by boundaries or as socially constructed out of symbolic meanings and social relations.11 12 In both cases, place-based context operates to perpetuate hierarchical social structures, facilitate and constrain resources and protect or hinder health. Moreover, place-based context may facilitate specific health-related interactions such as drug or alcohol use, experiences of violence or engagement in healthcare. Yet behavioural interventions often conceptualise place-based context as static (eg, place of risky sex) and do not consider how place-based contexts vary over time. Real-time geospatial methods, including the use of global positioning system (GPS) technology, are the cutting-edge, best-suited methods to overcome limitations of most neighbourhoods and other environments health research because they better capture place-based contexts corresponding to individuals’ lived experiences, referred to as ‘activity space’.13
There are numerous types of GPS-based methods that collect data from individuals and in some cases deliver intervention content. For example, ecological momentary assessment (EMA) has been shown to be an acceptable method of data collection.14 Ecological momentary interventions (EMI) allow researchers to deliver intervention content through mobile devices.15 Just-in-time adaptive interventions (JITAI) attempt to address the changing needs of an individual where the intervention algorithm is programmed to determine if and what intervention content should be delivered to participants at set times throughout the day, whenever a participant requests one or based on the participant’s current state (eg, stress) or environmental changes (eg, weather).16 17 Finally, geofences are virtual boundaries drawn around a location and allow for monitoring and messaging when individuals enter or exits the geofenced parameter.18 Geofencing interventions are a subset of JITAI where there is continuous monitoring of the participant’s location using GPS and delivery of an intervention such as text messages or links to health information or information about health services that are in the area based on a spatial context trigger. A geofence involves creating a virtual predefined set of boundaries or ‘fences’ around a geographical location, including using GPS technology. Geofencing methodology can be used in public health research—both in observational and intervention studies. Thus, geofencing can be a valuable tool in intervention research, enabling researchers to study and implement interventions in specific geographical areas. For example, geofencing allows researchers to precisely target specific areas for intervention. In addition, geofencing allows researchers to send location-based notifications (an intervention) to participants, including on their mobile devices. One example of this in the public health setting is the use of geofencing to monitor movements of individuals who tested positive for COVID-19 virus.19
Reviews of JITAI and EMI show the promising potential of this evolving technology,20–22 yet, such reviews are noted to lack the inclusion of geofencing, representing a major gap in the literature. This gap is vital to address as geofencing has the capability to address an array of different health issues ranging from tobacco cessation to HIV medication adherence. The lack of a clear and systematic understanding of the scope of geofencing interventions undermines its potential to impact population health. The purpose of this scoping review is to describe the state of the evidence on geofencing intervention design, acceptability, feasibility and impact. In addition, we examine what behavioural mechanisms were targeted across the interventions assessed.
Conceptualising mechanisms of action
Another limitation in the literature of EMA and JITAI interventions is the lack of attention to specific mechanisms of action that operate to achieve outcomes.23 Therefore, we sought to develop a framework based on several complementary theories and frameworks (eg, Turan’s HIV Stigma Framework and Social Cognitive Theory24–26) to evaluate geofencing interventions included in this review. The framework posits three key mechanisms for place-based context to influence health outcomes (figure 1). Each mechanism has both a protective and risk dimension. The Cognitive mechanism includes cognitive processes such as sense of control, knowledge, attitudes, self-efficacy, maladaptive thoughts, risk perceptions and internalised stigma.27–32 The Behavioural mechanism refers to both protective behaviours such as adaptive coping as well as risky behaviours such substance use, condomless sex and non-adherence to medication and care.33–35 The Social mechanism refers to interactions with others in the personal social networks and broader community such as emotional or instrumental support or enacted stigma and conflict which have been shown to exacerbate or mitigate health outcomes.36–38 The framework can be applied to multiple spatial scales from a micro-level (eg, a room in one’s residence) to community-level (eg, a neighbourhood activity space or census tract) to macro-level (eg, state, region).
Figure 1.
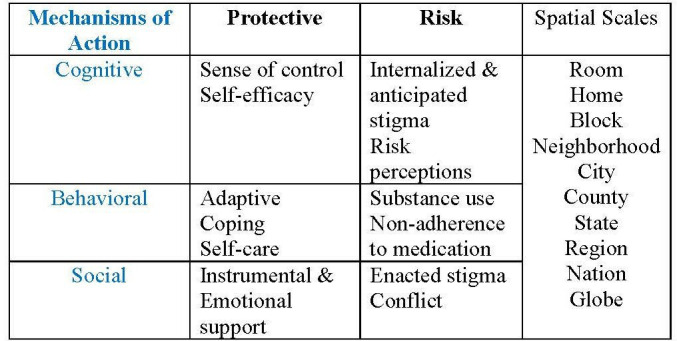
Types and mechanisms of action, protective and risk factors as well as spatial scales in geofencing interventions in population health research.
Methods
Study design
This scoping review is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews checklist.39
Inclusion criteria
Articles were only included if they used geofencing as a mechanism for intervention delivery. Articles were excluded if (1) a component or combination of GPS, geographical information system (GIS) or EMA was used without delivery of an intervention; (2) did not include a health or health-related outcome from the geofencing intervention; or (3) was not a peer-reviewed study.
Search strategy
Authors first met to develop the list of potential search terms and refined after initial searchers were conducted. Then searches were conducted in PubMed, CINAHL, EMBASE, Web of Science, Cochrane and PsycINFO for articles published through the end of 2021 (online supplemental appendix 1, detailed search strategy across n=6 databases). Search terms were for broad concepts regarding mobile delivery of a geofencing intervention: ‘Geographic Information Systems’; ‘Georeferencing’; ‘Global Positioning System’; or ‘Geofenc*’ combined with ‘Smartphone’ or ‘Mobile Applications’. The search was conducted on 12 January 2021 and was not registered. A protocol was not prepared.
bmjopen-2022-069374supp001.pdf (142.7KB, pdf)
Study selection
Screening of article titles and abstracts was conducted with two reviewers (SS and CV) to maximise scrutiny of all records. Each reviewer independently screened all articles identified from the initial search for relevance to the predefined inclusion criteria that was highlighted during a training session where it was emphasised that the reviewers should apply a liberal approach. Next, the same two reviewers independently reviewed each of the full texts for inclusion in the data extraction phase. Any disagreements in both phases were adjudicated by a third reviewer (OH). In all phases reviewers were not blinded to authors, funding or information regarding publication of all the records.
Data extraction
Two reviewers (OH and KT) extracted data for details of study design, target population, sample size, duration of follow-up, theoretical framework, software or mobile application use, goal and mechanism of geofenced intervention, and impact of the intervention of outcomes. Place-based mechanisms associated with the intervention included: (1) Behavioural, (2) Social support: Emotional, instrumental, informational and social monitoring and (3) cognitive. Finally, established guidance for reporting health intervention using mobile phone was used to evaluate the quality of each article.40
Patient and public involvement
None.
Results
Included studies
Using the search strategy in six identified databases, a total of 2171 articles were found after removing duplicates. Among them, 2039 (94%) studies were irrelevant and 132 (6%) full-text studies were assessed for eligibility. Reasons for exclusion of the 123 articles in the full-text phase included the article not being peer reviewed (n=46, 37%), review articles (n=19, 16%), was not the correct study design or intervention (n=14, 11%), or used a combination of GPS, GIS and or EMA, but was not a geofencing intervention (n=44, 36%). Nine eligible studies were ultimately included in this scoping review (figure 2; online supplemental appendix 2, details of nine studies that met inclusion for the scoping review).
Figure 2.
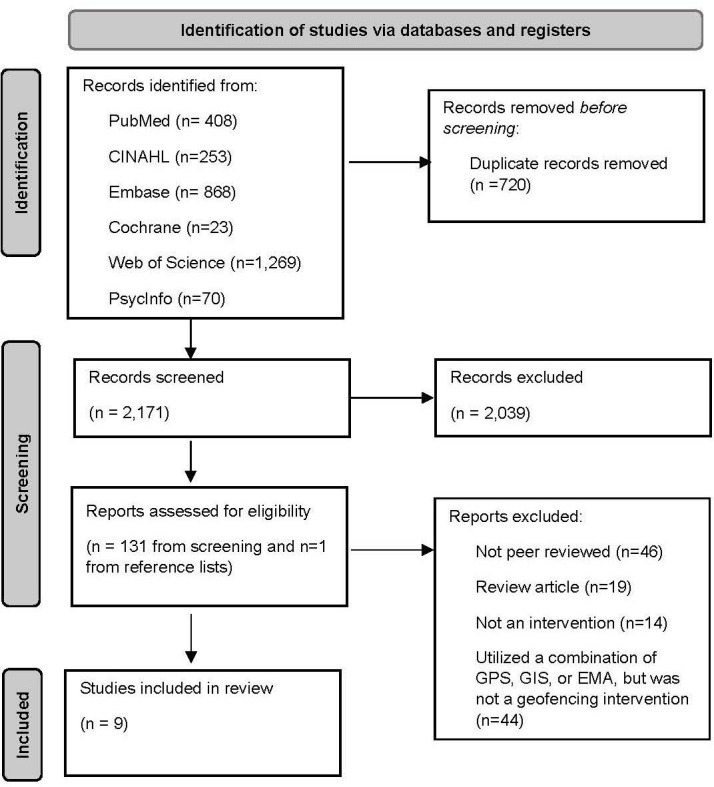
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram. EMA, ecological momentary assessment; GIS, geographical information system; GPS, global positioning system.
Study characteristics
The majority were published in 5 years preceding the search (n=8; 89%). Most employed a pre/post study design to assess changes in measured outcome or feasibility and acceptability of the geofencing intervention (n=7; 78%) with two unblinded randomised control trials. Sample sizes ranged from 4 to 3443; one study’s intervention quantified its reach with the geofencing intervention displaying on 516 073 mobile phones, though these impressions do not represent unique individuals receiving the intervention.41 Most studies (n=7; 78%) were conducted in the USA, one in the UK42 and one in Spain.23 A description of studies, including the names of the mobile applications used, study design and characteristics and place-based mechanisms are detailed in online supplemental appendix 2. The design of the geofencing interventions varied based on user input and content delivery (online supplemental appendix 3, components of mobile health evidence reporting and assessment).
Geofencing methods: user input
Geofences in most studies (n=5) were fixed and programmed in the mobile application without participant input. These included hospital emergency departments,18 43 hospitals where participants worked44 45 and a specific rural dental clinic.41 Two studies used participants input in determining where to geofence related to smoking42 or problematic alcohol use.46 Two studies used a mix of fixed and user input. Dorsch et al used user input to geofence locations where foods were consumed or purchased as well as a cloud-based web service to predict when participants entered grocery stores or restaurants. Besoain et al, used a moderated system where participants suggested locations to geofence that were venues for high-risk sexual encounters, but these venues were moderated by the study team and locations could be added or removed.
Intervention content delivery: direct versus indirect
Intervention content was delivered in direct or indirect methods. Five studies (56%) sent participants intervention content directly to their phones based on triggering the geofence boundary. These interventions included informing individuals living in a rural area of a dental clinic41 or sending behavioural messages regarding problematic alcohol use when near a bar,46 smoking cessation in areas detected as high likelihood of smoking,42 making low-sodium diet choices in grocery stores, restaurants or at home, or HIV and sexually transmitted infection prevention messages when in venues associated with high-risk sexual activity.23 The remaining four studies were categorised as indirect as they collected data when participants triggered geofence boundaries and in some cases delivered content at a later time from when the fence was triggered.
Impact of the interventions
There was not a consistent health outcome across the five studies that used a direct intervention. Both studies that used a randomised control design showed improved outcomes in the group randomised to geofencing. Addiction-Comprehensive Health Enhancement Support System (A-CHESS) sent context and place-based messages and included multiple other services such as a phone and data plan, access to a virtual counsellor and other interactive features.46 LowSalt4Life contained features including low sodium options and alternatives at grocery stores or restaurants, and the ability to scan product barcodes to find similar low-sodium options. Q Sense intervention participants decreased from 60% of pre-quit smoking days to 39% post-quit. UBeSafe intervention reported that all participants were able to trigger a hot zone where sexual contacts often took place and received a place-based prevention message.22 Finally, Wright et al,41 used a pre/post design, and found increases in community knowledge about the dental clinic (p=0.045) and increased number of dental visits post intervention.
Indirect intervention outcomes
Two studies used the geofence to track time working from medical practitioners or surgical residents. Owei et al, found the mean number of working hour violations for surgical residents’ post-intervention significantly decreased (p=0.04) compared with pre-intervention and compared with the previous year (p<0.01).44 Connor and Herzig, showed a significant correlation of early departures from operating room duties following late departures the previous day (p<0.01) and better dispersion of working hours (p=0.002) compared with the previous year.45 Two other studies geofenced major hospitals to detect hospitalisation of high priority patients. Nguyen et al, found the geofenced mobile application detected 800 unique participants who triggered a geofence, with a predictive value of true hospitalisation between 65% and 78%.18 Similarly, from a sample size of 21, four of the participants activated the alert system for patients with a ventricular assist device to their on-call care team when they triggered an emergency room geofence.43
Acceptability measures
Five studies reported data regarding acceptability of the geofencing mobile application in which all participants were positive regarding the value of the intervention. Participants in two studies with indirect intervention found the application useful and described knowledge of being monitored provided a sense of security.43 44 Additionally, participants in two studies did not have concerns regarding the continuous geolocation tracking for intervention purpose,42 44 but did stress the importance of transparency regarding the use of this data.42 Finally, in one interactive study, participants contributed to the creation and curation of geofenced hot zones as well as the prevention messages received when hot zones were triggered, accounting for 67% of hot zones created and used by the study.23
Place-based mechanisms
Four studies used a behavioural mechanism in their geofencing intervention.23 42 46 47 Four studies used a social mechanism which included informational support such as existence of a rural dental clinic41 and availability of menu grocery store items that were low in sodium.23 41 46 47 Additionally, participants were able to interact with counsellors though the application and review their data concerning visiting high-risk locations for further intervention46 or sharing context specific messages with other users on the application.23 Finally, five studies used a cognitive mechanism that provided the participant a sense of safety, security or knowing that their information was captured.45 46 These included reporting to care teams when the participants were hospitalised,18 43 capture of time and effort spent working in a clinical environment,44 45 and participants counsellor viewing their location and interacting with their place-based data of proximity and time spent in high-risk areas for binge drinking.46
Reporting and quality measures
All included studies reported on at least six items (online supplemental appendix 3). Position Health,43 Stat!45 and ResQ44 reported on how the intervention and data collected integrated into an existing health information system and described some data security procedures. CHESS46 and the Wright et al41 intervention conducted some cost assessment regarding the delivery of the intervention or cost to the participant to use the participant. No study reported on compliance of the intervention or data collection mechanism compliance with national guidelines or federal statutes. We did not assess confidence in the body of evidence or risk of bias.
Discussion
The purpose of this scoping review was to describe the use of geofencing as an intervention and mechanisms that were targeted to achieve various health outcomes. A geofence involves creating a virtual predefined set of boundaries or ‘fences’ around a geographical location, including using GPS technology. Geofencing methodology can be used in public health research—both in observational and intervention studies. Thus, geofencing can be a valuable tool in intervention research, enabling researchers to study and implement interventions in specific geographical areas. For example, geofencing allows researchers to precisely target specific areas for intervention. In addition, geofencing allows researchers to send location-based notifications (an intervention) to participants, including on their mobile devices. We identified only nine studies that fitted the criteria and, as expected, most publications were relatively recent. We found that the design of the geofencing intervention varied yet acceptability was good among study participants and impact was not assessed in all studies.
Of the studies included, only one was focused on a sexual and gender minority sample and only one with majority black, Indigenous people of colour (BIPOC), who experience disparities on a vast number of health outcomes due to social and structural factors such as racism and homophobia.23 Lack of inclusion of these populations is a significant gap that should be monitored as more studies are conducted. In addition, most studies were conducted in the USA, with no studies in developing countries, South America, Africa or Asia, which could represent an important opportunity.
The included studies described a range of user input of the geofenced locations from researcher only selection to user selection. This characteristic of an intervention merits consideration. User selection of geofenced locations may be prone to bias and recall issues.48 Researcher selected locations may not consider the variability of their sample’s place-based contexts and may under count locations that should be geofenced. The hybrid approach has the potential to address both limitations. Future studies using geofencing technology may warrant comparative studies of the user input approaches and be specific about the rationale for the type of locations that are geofenced and the user input of these so that studies can be comparable and be conducted in non-Western contexts.
Some of the interventions explicitly identified a theoretical model or foundation, and all the studies described targeting at least one of the mechanisms of action from our proposed framework. The studies in which the geofencing intervention targeted the cognitive mechanism were primarily addressing surveillance of the participants and messages to cue cognitions about their location. Cueing is a significant component of many effective interventions as they serve as reminders to engage in behaviours of interest.49–51 For example, wearing a bracelet that has a phrase as a reminder to take medication. Cues can focus on both the protective and risk dimensions of the mechanism. For example, if an individual triggers a geofence of a place they have identified as associated with a sense of control, a geofencing intervention could sent a text message that reminds the individual to engage in self-care. In places where stigma is anticipated a geofencing intervention can send a text message that reminds the individual about adaptive coping behaviours.
Studies using the behavioural mechanism described very specific behavioural targets such as buying lower sodium food, avoiding places of alcohol use, condom use and smoking cessation. As building self-efficacy is a well-established theoretical construct necessary for behavioural change,24 future studies should include opportunities to watch the desired behaviours be role-modelled and practiced to enhance the efficacy of the geofencing intervention.52
Studies that used the social mechanism were focused on the provision of both informational and emotional support. One study included a component in which the participants could create messages for other users of the geofencing application. As there are different types of social support (eg, emotional, appraisal, economic and informational) future studies should be specific and transparent about the types being targeted. With additional geofencing studies, a future review can be conducted using meta-analytical methods to determine the quantitative effectiveness of geofencing interventions in population health research.
Limitations
The search strategy was limited to English articles in PubMed, CINAHL, EMBASE, Web of Science, Cochrane and PsycINFO and we acknowledge other publications may not have been captured with these. There was heterogeneity in how studies reported intervention development, theoretical frameworks and feasibility and acceptability of the intervention. This reduced the ability to properly assess the extent of behavioural mechanism used for the given outcome. Additionally, as geofencing is a new technology, not many peer-reviewed articles have been published and this scoping review chose to exclude conference abstracts.
Conclusions
This scoping review found geofencing to be an emerging technology, that is, an acceptable and feasible intervention applied to several different populations and health outcomes.23 Attention to the mechanisms of actions will enable the field to understand not only whether geofencing is an appropriate and effective intervention but why it works to achieve the outcomes we observe. There is a need for future research that includes sexual and gender minority and BIPOC populations and populations from non-Western contexts to achieve the Health People Framework objectives given the persistent findings that BIPOC and sexual and gender minorities (SGM) populations. These studies could address those health outcomes where disparities are stark such as HIV/AIDS, cardiovascular, diabetes, COVID-19-related and monkey pox (mpox). Finally, future research can reveal place-based contexts that have not been considered which can inform resource allocation and targets for health-promoting policies.
Supplementary Material
Footnotes
Contributors: KT is the guarantor of the manuscript. KT and OH contributed equally to this manuscript. KT, OH and DD planned the study. KT, OH, CV and SS acquired data and conducted the analysis for this study. KT, OH and DD equally contributed to writing and finalising the manuscript.
Funding: This work was supported by a grant from the National Institute of Mental Health (R34MH118178). This work was supported by a grant from the National Institute of Mental Health (R34MH118178).
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
References
- 1.Larson NI, Story MT, Nelson MC. Neighborhood environments: disparities in access to healthy foods in the U.S. Am J Prev Med 2009;36:74–81. 10.1016/j.amepre.2008.09.025 [DOI] [PubMed] [Google Scholar]
- 2.Lazar M, Davenport L. Barriers to health care access for low income families: a review of literature. J Community Health Nurs 2018;35:28–37. 10.1080/07370016.2018.1404832 [DOI] [PubMed] [Google Scholar]
- 3.Kalichman SC, Kalichman MO. HIV-related stress and life chaos mediate the association between poverty and medication adherence among people living with HIV/AIDS. J Clin Psychol Med Settings 2016;23:420–30. 10.1007/s10880-016-9481-8 [DOI] [PubMed] [Google Scholar]
- 4.Taylor SE, Repetti RL, Seeman T. Health psychology: what is an unhealthy environment and how does it get under the skin? annual review of psychology Annu Rev Psychol 1997;48:411–47. 10.1146/annurev.psych.48.1.411 [DOI] [PubMed] [Google Scholar]
- 5.Earnshaw VA, Bogart LM, Dovidio JF, et al. Stigma and racial/ethnic HIV disparities: moving toward resilience. Stigma and Health 2015;1:60–74. 10.1037/2376-6972.1.S.60 [DOI] [Google Scholar]
- 6.Lutete P, Matthews DW, Sabounchi NS, et al. Intersectional stigma and prevention among gay, Bisexual, and same gender–loving men in New York city, 2020: system Dynamics models. Am J Public Health 2022;112:S444–51. 10.2105/AJPH.2022.306725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Quinn K, Dickson-Gomez J, Zarwell M, et al. A gay man and a doctor are just like, a recipe for destruction”: how racism and Homonegativity in Healthcare settings influence prep uptake among young black MSM. AIDS Behav 2019;23:1951–63. 10.1007/s10461-018-2375-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Arcaya MC, Tucker-Seeley RD, Kim R, et al. Research on neighborhood effects on health in the United States: a systematic review of study characteristics. Social Science & Medicine 2016;168:16–29. 10.1016/j.socscimed.2016.08.047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Duncan DT, Kawachi I. Neighborhoods and health, vol 10. Oxford University Press New York, 2018. [Google Scholar]
- 10.Rifkin SB. Examining the links between community participation and health outcomes: a review of the literature. Health Policy Plan 2014;29:ii98–106. 10.1093/heapol/czu076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gesler WM. Therapeutic landscapes: medical issues in light of the new cultural geography. Soc Sci Med 1992;34:735–46. 10.1016/0277-9536(92)90360-3 [DOI] [PubMed] [Google Scholar]
- 12.Keene DE, Padilla MB. Spatial stigma and health inequality. Critical Public Health 2014;24:392–404. 10.1080/09581596.2013.873532 [DOI] [Google Scholar]
- 13.Duncan DT, Kawachi I, Subramanian SV, et al. Examination of how neighborhood definition influences measurements of youths' access to tobacco retailers: a methodological note on spatial Misclassification. Am J Epidemiol 2014;179:373–81. 10.1093/aje/kwt251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Palmer JRB, Espenshade TJ, Bartumeus F, et al. New approaches to human mobility: using mobile phones for demographic research. Demography 2013;50:1105–28. 10.1007/s13524-012-0175-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heron KE, Smyth JM. Ecological momentary interventions: incorporating mobile technology into Psychosocial and health behaviour treatments. Br J Health Psychol 2010;15:1–39. 10.1348/135910709X466063 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Wang L, Miller LC. Just-in-the-moment adaptive interventions (JITAI): A meta-Analytical review. Health Commun 2020;35:1531–44. 10.1080/10410236.2019.1652388 [DOI] [PubMed] [Google Scholar]
- 17.Nahum-Shani I, Smith SN, Spring BJ, et al. Just-in-time adaptive interventions (Jitais) in mobile health: key components and design principles for ongoing health behavior support. Ann Behav Med 2018;52:446–62. 10.1007/s12160-016-9830-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nguyen KT, Olgin JE, Pletcher MJ, et al. Smartphone-based Geofencing to ascertain hospitalizations. Circ Cardiovasc Qual Outcomes 2017;10:e003326. 10.1161/CIRCOUTCOMES.116.003326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ahmed N, Michelin RA, Xue W, et al. A survey of COVID-19 contact tracing Apps. IEEE Access 2020;8:134577–601. 10.1109/ACCESS.2020.3010226 [DOI] [Google Scholar]
- 20.Carpenter SM, Menictas M, Nahum-Shani I, et al. Developments in mobile health just-in-time adaptive interventions for addiction science. Curr Addict Rep 2020;7:280–90. 10.1007/s40429-020-00322-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Naughton F. “Delivering “just-in-time” smoking cessation support via mobile phones: Current knowledge and future directions”. Nicotine & Tobacco Research 2017;19:379–83. [DOI] [PubMed] [Google Scholar]
- 22.Thomas JG, Bond DS. Review of innovations in digital health technology to promote weight control. Curr Diab Rep 2014;14:485. 10.1007/s11892-014-0485-1 [DOI] [PubMed] [Google Scholar]
- 23.Besoain F, Perez-Navarro A, Jacques Aviñó C, et al. Prevention of HIV and other sexually transmitted infections by Geofencing and Contextualized messages with a Gamified App, UBESAFE: design and creation study. JMIR Mhealth Uhealth 2020;8:e14568. 10.2196/14568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Bandura A. Social cognitive theory: an Agentic perspective. Asian J Soc Psychol 1999;2:21–41. 10.1111/1467-839X.00024 Available: http://doi.wiley.com/10.1111/ajsp.1999.2.issue-1 [DOI] [PubMed] [Google Scholar]
- 25.Turan B, Hatcher AM, Weiser SD, et al. Framing mechanisms linking HIV-related stigma, adherence to treatment, and health outcomes. Am J Public Health 2017;107:863–9. 10.2105/AJPH.2017.303744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Macintyre S, Ellaway A, Cummins S. Place effects on health: how can we Conceptualise, Operationalise and measure them Social Science & Medicine 2002;55:125–39. 10.1016/S0277-9536(01)00214-3 [DOI] [PubMed] [Google Scholar]
- 27.Khawcharoenporn T, Mongkolkaewsub S, Naijitra C, et al. HIV risk, risk perception and uptake of HIV testing and counseling among youth men who have sex with men attending a gay Sauna. AIDS Res Ther 2019;16:13. 10.1186/s12981-019-0229-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Machowska A, Bamboria BL, Bercan C, et al. Impact of ‘HIV-related stigma-reduction workshops’ on knowledge and attitude of Healthcare providers and students in central India: a pre-test and post-test intervention study. BMJ Open 2020;10:e033612. 10.1136/bmjopen-2019-033612 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Mi T, Li X, Zhou G, et al. HIV disclosure to family members and medication adherence: role of social support and self-efficacy. AIDS Behav 2020;24:45–54. 10.1007/s10461-019-02456-1 [DOI] [PubMed] [Google Scholar]
- 30.SeyedAlinaghi S, MohsseniPour M, Aghaei E, et al. The relationships between early maladaptive Schemas, quality of life and self-care behaviors in a sample of persons living with HIV: the potential mediating role of cognitive emotion regulation strategies. TOAIDJ 2020;14:100–7. 10.2174/1874613602014010100 [DOI] [Google Scholar]
- 31.Steptoe A, Jackson SE. The life skills of older Americans: association with economic, psychological, social, and health outcomes. Sci Rep 2018;8:9669. 10.1038/s41598-018-27909-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yigit I, Bayramoglu Y, Weiser SD, et al. Changes in internalized stigma and HIV health outcomes in individuals new to HIV care: the mediating roles of depression and treatment self-efficacy. AIDS Patient Care STDS 2020;34:491–7. 10.1089/apc.2020.0114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gonzalez A, Barinas J, O’Cleirigh C. Substance use: impact on adherence and HIV medical treatment. Curr HIV/AIDS Rep 2011;8:223–34. 10.1007/s11904-011-0093-5 [DOI] [PubMed] [Google Scholar]
- 34.Logie CH, Williams CC, Wang Y, et al. Adapting stigma mechanism frameworks to explore complex pathways between Intersectional stigma and HIV-related health outcomes among women living with HIV in Canada. Soc Sci Med 2019;232:129–38. 10.1016/j.socscimed.2019.04.044 [DOI] [PubMed] [Google Scholar]
- 35.Safren SA, Blashill AJ, Lee JS, et al. Condom-use self-efficacy as a mediator between Syndemics and Condomless sex in men who have sex with men (MSM). Health Psychol 2018;37:820–7. 10.1037/hea0000617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bekele T, Rourke SB, Tucker R, et al. Direct and indirect effects of perceived social support on health-related quality of life in persons living with HIV/AIDS. AIDS Care 2013;25:337–46. 10.1080/09540121.2012.701716 [DOI] [PubMed] [Google Scholar]
- 37.Koegler E, Kennedy CE. A Scoping review of the associations between mental health and factors related to HIV acquisition and disease progression in conflict-affected populations. Confl Health 2018;12:20. 10.1186/s13031-018-0156-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Vaughan E, Power M, Sixsmith J. Experiences of stigma in Healthcare settings by people living with HIV in Ireland: a qualitative study. AIDS Care 2020;32:1162–7. 10.1080/09540121.2020.1781761 [DOI] [PubMed] [Google Scholar]
- 39.Tricco AC, Lillie E, Zarin W, et al. PRISMA extension for Scoping reviews (PRISMA-SCR): checklist and explanation. Ann Intern Med 2018;169:467–73. 10.7326/M18-0850 [DOI] [PubMed] [Google Scholar]
- 40.Agarwal S, LeFevre AE, Lee J, et al. Guidelines for reporting of health interventions using mobile phones: mobile health (mHealth) evidence reporting and assessment (mERA) checklist. BMJ 2016;352:i1174. 10.1136/bmj.i1174 [DOI] [PubMed] [Google Scholar]
- 41.Wright WG, Rafferty AP, Winterbauer N, et al. Geofencing: mobile technology as a health promotion tool to raise awareness of a dental clinic in rural North Carolina. J Rural Health 2021;37:667–74. 10.1111/jrh.12501 [DOI] [PubMed] [Google Scholar]
- 42.Naughton F, Hopewell S, Lathia N, et al. A context-sensing mobile phone App (Q sense) for smoking cessation: a mixed-methods study. JMIR Mhealth Uhealth 2016;4:e106. 10.2196/mhealth.5787 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.DeFilippis EM, Safavi K, Reyes J, et al. Mobile Geolocation technology to improve Multidisciplinary care of patients with ventricular assist devices: A feasibility study. Journal of Cardiac Failure 2017;23:S84. 10.1016/j.cardfail.2017.07.243 [DOI] [PubMed] [Google Scholar]
- 44.Owei L, Luks VL, Brooks KD, et al. Smart-phone based Geofencing: A novel approach to monitoring clinical work hours in surgery Residency. J Surg Educ 2021;78:e210–7. 10.1016/j.jsurg.2021.06.024 [DOI] [PubMed] [Google Scholar]
- 45.Connor CW, Herzig M. Monitoring the location of staff via mobile devices in a large Multifacility practice group. A & A case reports. A A Case Rep 2016;6:320–8. 10.1213/XAA.0000000000000288 [DOI] [PubMed] [Google Scholar]
- 46.Gustafson DH, McTavish FM, Chih M-Y, et al. A Smartphone application to support recovery from alcoholism: a randomized clinical trial. JAMA Psychiatry 2014;71:566–72. 10.1001/jamapsychiatry.2013.4642 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Dorsch MP, Cornellier ML, Poggi AD, et al. Effects of a novel Contextual just-in-time mobile App intervention (Lowsalt4Life) on sodium intake in adults with hypertension: pilot randomized controlled trial. JMIR Mhealth Uhealth 2020;8:e16696. 10.2196/16696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wray TB, Pérez AE, Celio MA, et al. Exploring the use of Smartphone Geofencing to study characteristics of alcohol drinking locations in High‐Risk gay and Bisexual men. Alcohol Clin Exp Res 2019;43:900–6. 10.1111/acer.13991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Latkin CA, Hua W, Tobin K. Social network correlates of self-reported non-fatal overdose. Drug Alcohol Depend 2004;73:61–7. 10.1016/j.drugalcdep.2003.09.005 [DOI] [PubMed] [Google Scholar]
- 50.Tobin KE, Davey MA, Latkin CA. Calling emergency medical services during drug overdose: an examination of individual, social and setting correlates. Addiction 2005;100:397–404. 10.1111/j.1360-0443.2005.00975.x [DOI] [PubMed] [Google Scholar]
- 51.Tobin KE, Latkin CA. n.d. Social networks of HIV positive gay men: their role and importance in HIV prevention, understanding prevention for HIV positive gay men. Springer;2017:349–66. 10.1007/978-1-4419-0203-0 [DOI] [Google Scholar]
- 52.Tobin KE, Heidari O, Winiker A, et al. Peer approaches to improve HIV care Cascade outcomes: a Scoping review focused on peer behavioral mechanisms. Curr HIV/AIDS Rep 2022;19:251–64. 10.1007/s11904-022-00611-3 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2022-069374supp001.pdf (142.7KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.


