Abstract
Objective
The terms critical care and the Intensive Care Unit (ICU) are often used interchangeably to describe a place of care. Defining critical care becomes challenging because of the colloquial use of the term. Using concept analysis allows for the development of definition and meaning. The aim of this concept analysis is to distinguish the use of the term critical care to develop an operational definition which describes what constitutes critical care.
Method
Walker and Avant’s eight-step approach to concept analysis guided this study. Five databases (CINAHL, Scopus, PubMed, ProQuest Dissertation Abstracts and Medline in EBSCO) were searched for studies related to critical care. The search included both qualitative and quantitative studies written in English and published between 1990 and 2022.
Results
Of the 439 papers retrieved, 47 met the inclusion criteria. The defining attributes of critical care included 1) a maladaptive response to illness/injury, 2) admission modelling criteria, 3) advanced medical technologies, and 4) specialised health professionals. Antecedents were associated with illness/injury that progressed to a level of criticality with a significant decline in both physical and psychological functioning. Consequences were identified as either death or survival with/without experiencing post-ICU syndrome.
Conclusion
Describing critical care is often challenging because of the highly technical nature of the environment. This conceptual understanding and operational definition will inform future research as to the scope of critical care and allow for the design of robust evaluative instruments to better understand the nature of care in the intensive care environment.
Keywords: Critical care, Concept analysis, Intensive care, Intensive care unit, Intensive therapy
What is known?
-
•
Critical care is often associated with the use of advanced medical technologies focused around a medical model of care.
-
•
While well known, critical care is often widely discussed in general terms, yet is poorly defined within what could be described as the essence or nature of care.
-
•
Critical care is often referred to as a ‘process’ of looking after the seriously ill or injured.
What is new?
-
•
This paper provides a detailed conceptual definition of critical care.
-
•
The formation of a model case provides information for practitioners and researchers that will support future work to better understanding of basis of critical care across the health professions.
-
•
The results of this conceptual analysis provide a different view of what constitutes care from the perspective of the different health care groups that work in the intensive care space.
1. Introduction
The terms critical care and Intensive Care Unit (ICU) are often used interchangeably to describe a place of care. Yet, one is the function of a dedicated, specialist team of health professionals to support and care for the critically ill person during a medical emergency or crisis, while the other is a dedicated location where this focused care is undertaken. As a place of critical care, it is the technology that separates it from other areas of the hospital [1]. When used, the notion of intensive care often conjures up images of a specific place in the hospital where the seriously or critically ill are cared for. In many respects, the concept of critical care may not have a different array of meanings or be elusive and this is possibly because of the normal or ordinary day language that is used to describe this concept. Yet, the term intensive or critical care has a variety of different names and perhaps meanings to signify the essence of critical care, for example, the critical care unit, the intensive care unit or the intensive therapy unit [2,3]. Moreover, the term critical care has now become a more standardised term because of the inclusion of other areas in the hospital that effectively treat and care for the seriously ill or injured such as the accident and emergency department or the coronary care unit [4]. The intensive care unit differs significantly from other areas because its major focus is on invasive mechanical ventilation. What is potentially missing is what is encompassed in ‘critical care’. For this review the term critical care will be used to exemplify and describe the ‘inter-professional care’ that is undertaken in the intensive care unit (Step 1). Therefore, the aims of this concept analysis are to 1) distinguish the use of the term in developing an operational definition, 2) to explore the concept of critical care as a possible space for care, cure and function and 3) develop a conceptual/theoretical model of critical care (Step 2). Furthermore, it may be possible to describe, define and discuss the relationship between critical illness and critical care undertaken in an intensive care unit. Using Walker and Avant's [5] eight-step approach to concept analysis may aid in seeking conceptual clarity, therefore the analysis may make it possible to promote a single vocabulary for discussion, whilst allowing an understanding of what signifies the parameters of critical care to be. It will achieve this by providing background literature in the form of a scoping review to identify uses and meanings of the concept, explore the nature of critical care in the form of fictional model cases, determine the antecedents and consequences associated with critical care and finally ascertain the empirical referents that are conducive to this concept.
2. Methods
Concept analysis, as described by Walker and Avant [5] is a strategy that allows for an examination and exploration to define and evaluate the concept of critical care. In particular, it distinguishes between those critical characteristics and attributes of critical care that allowed for clarity of meaning [5] and is therefore fundamental to the formation of nursing knowledge. The result of which is a precise operational definition that meets the requirements of construct validity.
The basis of Walker and Avant’s [5] eight-step concept analysis approach to concept analysis guided this project. It is an iterative framework, which encompasses an entity based structural analytical approach. The central focus is the identification of the wider ranges of intentions coupled with the ability to distinguish between the defining attributes and the relevant attributes, which allows for the formation of distinct analytical goals.
2.1. Search strategy
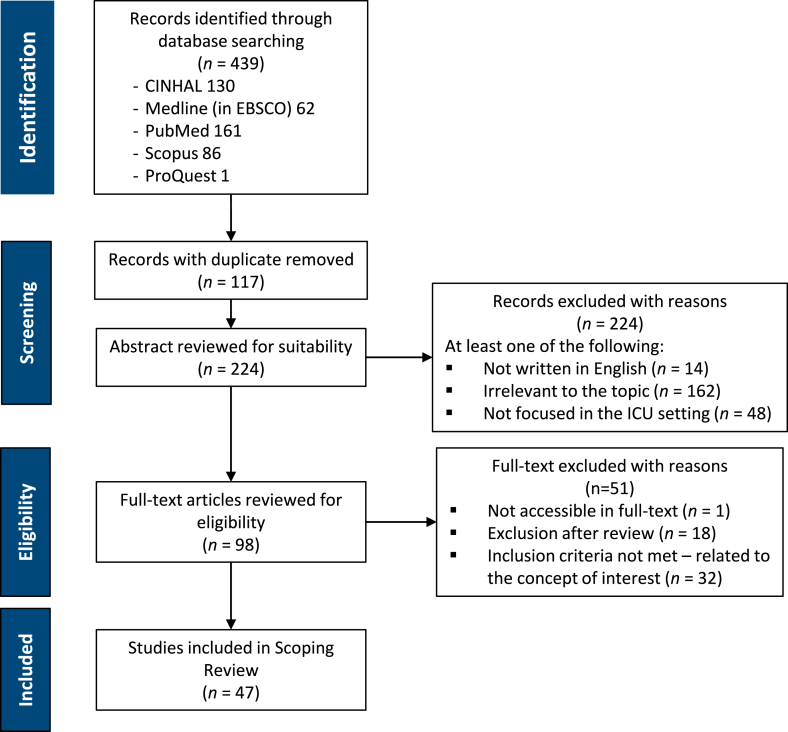
A scoping review was undertaken using the Joanna Briggs Institute (JBI) System for the Unified Management of the Assessment and Review of Information (SUMARI) and reported using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-SCR) [6]. The pneumonic PCC (population, concept and context) for scoping reviews was considered for developing the search strategy – ‘what is care in terms of critical care’ in the intensive care unit, P = critically ill, C = critical care, and C = intensive care unit. Five databases were accessed for published works which stipulated intensive care, critical care, care and caring within their title between 1990 and 2022 (CINAHL, Scopus, PubMed, ProQuest Dissertation Abstracts and Medline in EBSCO). Additional searches were undertaken within the grey literature, discursive papers, conference papers, editorials and unpublished commentaries were also included. Search terms related to definition∗, car∗ AND intensive care OR critical care were paired with intensive care unit OR ICU OR intensive therapy unit OR ITU OR cardiac ICU OR neuro ICU. Additional searches were undertaken using wild card terms using ‘?’ and truncated terms ending with ∗ to elicit further combinations associated with intensive and/or critical care. Hand searching of reference lists along with the content pages of intensive and/or critical care specific journals was also undertaken. Papers were included if they discussed the nature of care and what constituted care within an intensive care environment. Papers were excluded if they did not adequately describe the ‘essence of care’ fully. The study design was inclusive of both qualitative and quantitative methods. This resulted in 47 documents that met the criteria for identifying the concepts use (Fig. 1) [7].
Fig. 1.
Study selection flow chart.
After the search was completed, all identified citations were collated and uploaded into EndNote, and from there, all duplicates were removed. Using JBI SUMARI, all eligible titles and abstracts were screened by two independent reviewers and assessed for relevance against the inclusion criteria. Those studies that were potentially relevant were retrieved in full text. The full-text papers selected were then evaluated against the inclusion criteria by two independent reviewers. Reasons for exclusion were recorded as part of the PRISMA-ScR reporting [6]. Disagreements arising between the reviewers at each stage of the study selection process were resolved through discussion (Fig. 1).
2.2. Identify uses of the concept: critical care (Step 3)
Identifying the uses of the concept is an important first step in establishing how the concept is defined/used in everyday parlance. This may include implicit and explicit uses of the concept so that a fully rounded view of the concept is initially established. This may include a search of the relevant literature, commonly used definitions, lay language or other narrative forms that may be relevant to the concept.
The Concise Oxford Dictionary [8] defines critical care as “the continuous care and attention, often using special equipment, for people in hospital who are seriously ill or injured”. Likewise, the Cambridge Dictionary [9], describes critical care “as the continuous treatment for patients who are seriously ill, very badly injured or have just had an operation or the department of a hospital that provides this care”. The notion of critical care was first observed by Florence Nightingale, during the Crimean War of 1854, where she first used the concept of triage to identify the seriously injured and set them apart from the others to receive more critical care from a specialist team of nurses [10]. Other examples, though not typically referred to as critical care appeared in the late nineteenth century where the unstable and critically ill patients were moved to a more observable vantage point for the nurses charged with their care. An example of this is in the exert from Louisa May Alcott’s [11] Hospital Sketches where she reflects:
“My ward was now divided into three rooms … I had managed to sort out the patients in such a way that I had what I called my “duty room”, my pleasure room and my pathetic room” and worked for each in a different way. One I visited, armed with a dressing tray, full of rollers, plasters and pins; another with books, flowers, games and gossip; a third with teapots, lullabies, consolation and sometimes a shroud … wherever the sickest or most helpless man chanced to be, there I held my watch …” (p47)
It is implied in this anecdote that the duty room (perhaps the nineteenth century ICU equivalent) was where the sickest and infirm were nursed and the pathetic room was similar in some respects to a hospice or palliative care unit. The notion of increased vigilance and observation eventually became the precursor to what is now known as critical care. For example, in the mid 40’s where the physiological instability of the post-operative patient and the dangers of anaesthesia meant that collective organisation of these patients into one specific area, the recovery room, occurred. With the continued hypervigilance of patient monitoring led directly to the birth of the ICU [4,12,13]. Jackson and Cairns ([14], p2) describe critical care as the “process of looking after patients who either suffer from life threatening conditions or at risk of developing them”. Equally they describe the intensive care unit as a “distinct geographical entity in which high staffing ratios, advanced monitoring and organ support can be offered to improve patient morbidity and mortality”. This is not too dissimilar to those definitions/descriptions identified by internationally recognised intensive care societies or organisations (Table 1). However, the difference is that these definitions or more aptly descriptions of critical/intensive care are offered as lay comments specifically for patients and or families. It could be suggested, therefore, that healthcare professionals, whether they work in this environment or not, may be fully conversant with what critical care and what the intensive care unit are (Table 1). Moreover, a recent concept analysis attempted to define critical care as the “identification, monitoring and treatment of patients with critical illness through the sustained support of vital organ functions” [15, p9], yet fails to distinguish between the different health professional roles in the delivery of critical care and therefore conforms to the technical-rational medical model of care [16]. Importantly, when attributing this definition of critical care to the fictional model case, it is difficult to distinguish the actual ‘care’ involved and what is deemed critical except to identify the geographical place the patient is admitted to and the administration of oxygen along with regular monitoring. Whilst this is valuable in finding a definition of critical care, the authors also make the important distinction of what critical illness might entail in order for critical care to be implemented – “a state of ill health with vital organ dysfunction, a high risk of imminent death if care is not provided and the potential for reversibility.” ([15], p 8)
Table 1.
Consensus definitions of critical care and ICUs.
| Society/Organisation | Definitions |
|---|---|
| Intensive Care Societyhttps://ics.ac.uk/about-icu/what-is-intensive-care.html | Intensive care units (ICUs) are specialist hospital wards that provide treatment and monitoring for people who are very ill. ICUs are also sometimes called critical care units (CCUs) or intensive therapy units (ITUs). They’re staffed with specially trained healthcare professionals and contain sophisticated monitoring equipment. |
| Faculty of Intensive Care Medicinehttps://www.ficm.ac.uk/forpatients/what-is-intensive-care | Intensive Care, also known as critical care, is a place in every acute hospital that manages patients who are critically ill. |
| European Society of Intensive Care Medicinehttps://www.esicm.org/patient-and-family/what-is-intensive-care/ | Intensive care is the medical speciality that supports patients whose lives are in immediate danger – like when a vital organ such as the heart, liver, lungs, kidneys or the nervous system is affected |
| National Library of Medicinehttps://medlineplus.gov/criticalcare.html#:∼:text=What%20is%20critical%20care%3F,constantly%20monitor%20your%20vital%20signs. | Critical care is medical care for people who have life-threatening injuries and illnesses. It usually takes place in an intensive care unit (ICU). A team of specially-trained health care providers gives you 24-h care. This includes using machines to constantly monitor vital signs. It also usually involves giving specialised treatment. |
| UK National Health Servicehttps://www.nhs.uk/conditions/intensive-care/ | Intensive care units(ICUs) are specialist hospital wards that provide treatment and monitoring for people who are very ill. They’re staffed with specially trained healthcare professionals and contain sophisticated monitoring equipment. ICUs are also sometimes called critical care units (CCUs) or intensive therapy units (ITUs) |
| National Institute of Clinical Excellencehttps://www.nice.org.uk/guidance/cg83/ifp/chapter/what-critical-care-means | ‘Critical care’ is now used as the term that encompasses ‘intensive care’, ‘intensive therapy’ and ‘high dependency’ units. Critical care is needed if a patient needs specialised monitoring, treatment and attention, for example, after routine complex surgery, a life-threatening illness or an injury. If someone needs critical care, they can be said to have a ‘critical illness’. |
| American College of Physicianshttps://www.acponline.org/about-acp/about-internal-medicine/subspecialties-of-internal-medicine/critical-care-medicine | ICUs are specially equipped hospital units that provide highly specialised care, continuous observation and monitoring of critical care patients 24 h a day. Typically, patients are admitted to the ICU from an emergency room, from an operating room or from another area of the hospital. The care team for ICU patients comprises a multidisciplinary group of physicians, nurses, respiratory therapists and pharmacists who have all been trained in care of critically ill or injured patients. |
| Canadian Critical Care Societyhttps://canadiancriticalcare.org/Patients-&-Families | Critical care medicine encompasses the diagnosis and treatment of a wide variety of clinical problems representing the extreme of human disease. Critically ill patients require intensive care by a coordinated team. |
3. Results
3.1. Determining the defining attributes (Step 4)
Determining the defining attributes of the concept is attempting to identify those attributes frequently associated with the concept, in this case, critical care. Moreover, the specific phenomenon in question is reduced to those key features that differentiate the concept from other similar or related concepts, such as intensive care. To assist in this step of the concept analysis, an inductive content analysis described by Krippendorf [17] was undertaken with 47 papers identified from the literature search to ascertain uses of the concept critical care [1,12,13,[18], [19], [20], [21], [22], [23], [24], [25], [26], [27], [28], [29], [30], [31], [32], [33], [34], [35], [36], [37], [38], [39], [40], [41], [42], [43], [44], [45], [46], [47], [48], [49], [50], [51], [52], [53], [54], [55], [56], [57], [58], [59], [60], [61]]. This resulted in the development of five categories (Table 2). The defining attributes associated with critical care can be divided into three main categories – critical illness, supportive and treatment therapies, and critical care based around a technical-rational medical model of care [16]. Nursing and allied health play supportive and facilitative roles in the delivery of this care in conjunction with their individual scopes of practice. Therefore, in determining the defining attributes of critical care those distinctive features that emerged which are associated with the concept include (Table 2):
-
⁃
The patient’s maladaptive response to illness/injury that results in a systemic inflammatory reaction (critical illness);
-
⁃
The patient must present with intensive care unit admission modelling criteria that denote critical illness;
-
⁃
The application and administration of advanced medical technologies to support and treat ongoing failing organ systems;
-
⁃
The application of specialised allied health, medical and nursing care that considers the micro and macro levels of care associated with critical illness;
-
⁃
That critical care is not to be confused with the intensive care unit, which is a geographical location within the hospital setting.
Table 2.
Defining attributes of critical care.
| Defining Attributes | Sources |
|---|---|
| Critical Illness | |
|
Fletcher & Cuthbertson [24]; Garrabou et al. [25]; Trentadue et al. [26]; Quoilin et al. [27]; Van Ierssel et al. [54]; Protti et al. [35]; Kizilarslanoglu et al. [18]; McCreath et al. [38]; Bakhru et al. [19]; Liu & Li [56]; Kerckhoffs et al. [20]; McClave et al. [57]; Teblick et al. [55]; Graham & Stacy [39]; de Jager et al. [28] |
| Supportive Therapies | |
|
Kesecioglu [41]; Berthelsen & Conqvist [12]; White [13]; Wikström et al. [40]; Thompson et al. [46]; Price [47]; Christensen & Probst [1]; Elke & Heyland [59]; Reintam Blasher et al. [60]; Crilly et al. [48] |
| Critical Care | |
|
Ferreira et al. [43]; Metnitz et al. [34]; de Souza Urbanetto et al. [44]; Lee et al. [58]; de Vivanco-Allende et al. [45]; Simpson et al. [36] |
|
Lewis [62]; Williams [37]; Hanekom et al. [22]; van der Lee et al. [23] |
|
Schantz [53]; Almerud et al. [42]; Bishop et al. [49]; Ahlberg et al. [31]; Sommers et al. [22]; Clark et al. [32]; Jones et al. [50]; Jakimowicz et al. [51]; Efstathiou & Ives [52]; McLennan & Aggar [33]; Jeffs & Darbyshire [29]; Savjani et al. [30] |
Note: SAPS = Simplified Acute Physiological Score. SOFA = Sequential Organ Failure Assessment Score. TISS-28 = Therapeutic Intervention Scoring System. APACHE = Acute Physiological and Chronic Health Evaluation.
In order to identify the key components of the concept critical care, the development of a model, borderline and contrary case is useful in recognising and refining the defining attributes. It is often seen as a form of constant comparative examination so that the internal structure of the phenomenon has meaning and clarity.
3.2. Model case (Step 5)
The fictional model case contains all of the constituents identified in the defining attributes as well as the working definition of critical care from the diagnosis of critical illness and subsequent admission to an ICU along with the initiation of advanced medical technologies to support and treat the underlying condition. It also includes those activities associated with a macro level of care such as those undertaken by nursing and physiotherapy.
Mr. Melvin Jones, a 72-year-old widower who resides in a residential aged care facility, has a body mass index of 38 and was transported by ambulance to the Accident and Emergency department (A&E) after experiencing a chest infection for six days. He has a medical history of hypertension, peripheral vascular disease, insulin-controlled type 2 diabetes, and chronic bronchitis. Additionally, he smokes twenty roll-up cigarettes a day. As a result of worsening respiratory indices (oxygen saturations, arterial blood gas analysis and respiratory rate), he is electively intubated in the A&E and transferred to the ICU. Once in the ICU he is placed on continuous cardiac monitoring, a quadruple lumen right internal jugular central venous line (CVL) is placed for drug administration along with the monitoring of right atrial filling pressures (CVP). An intra-arterial line is placed in his right radial artery to continuously monitor his blood pressure while also allowing access for blood sampling in particular samples for arterial blood gas analysis (ABG). His vital signs showed marked hypotension (↓ mean arterial & central venous pressures), pyrexia, tachycardia and peripheral cyanosis. His ABG showed marked acute-on-chronic hypoxia and hypercarbia. Mr Jones is immediately given a fluid challenge as a result of his hypotension and started on an inotropic infusion. Blood samples taken in the A&E show elevated serum urea and creatinine indicative of renal insufficiency as a result of his hypotension. A sputum sample is taken for culture and sensitivity to identify the bacterium responsible for his chest infection, but in the mean while he is started on intravenous broad-spectrum antibiotics. Mr Jones’ chest x-ray reveals not only correct placement of his CVL and endotracheal tube, but increased opacity in the right lower and middle lobes consistent with pneumonia.
Once Mr. Jones is stabilised, the nursing team starts to document his baseline vital signs, ventilatory parameters, drug infusion rates, sedation score, pain assessment, and urine output hourly and often converse with the medical team as to current orders and results of blood and ABG tests, adjusting infusion rates to maintain prescribed physiological parameters. As part of their physical health assessment, Mr Jones’ nurse identifies him as a high risk of pressure injury and therefore institute positioning guidelines not only to reduce the risk of tissue injury but to also aid in secretion removal. When assessing his chest, his nurse notices decreased expansion on the right side along with coarse inspiratory crackles and bronchial breath sounds on auscultation consistent excess secretions and alveolar consolidation. In addition to positioning, they place Mr Jones on a pressure relieving mattress. They also implement other nursing activities like regular mouth, indwelling catheter, bowel and eye care. This information is documented in the nursing notes. When Mr Jones’ two daughters arrive, his nurse sits with them and explains the current situation and what they might expect to see in the ICU before showing them to their father’s bed-space. His nurse also explains what the ‘machinery’ is and how it is supporting and monitoring their father’s progress. They are invited to ask questions and stay as long as they feel able. The nurse asks the hospital chaplain assigned to the ICU to talk with them as well so as to offer another person to talk with while Mr. Jones is being cared for. As the daughters have arrived from other areas of the country, his nurse helps organise emergency accommodation.
When reviewed by the ICU physiotherapist, the nurse conveys their findings from their initial physical assessment in particular those associated with his chest infection. The physio also finds on auscultation those reported by his nurse and the findings from the chest x-ray. They implement chest physiotherapy which includes chest percussion, hyperinflation and suctioning to aide in mobilizing and removing the secretions as well as re-inflating collapsed areas of lung. The physio also starts range of movement (ROM) exercises. They also document their findings and treatment and develop a chest physiotherapy plan for the nurses to follow during out-of-hours.
3.3. Borderline case (Step 6)
The fictional borderline case in this instance possesses some of the defining attributes identified in the definition especially that of needing advanced medical technologies. In this case, Mrs. Smith required continued ventilatory support because of the failure of anaesthetic reversal and was therefore experiencing acute respiratory failure. Though potentially dangerous, Mrs. Smith was not critically ill.
Mrs. Jean Smith is a 49-year-old married woman who has undergone elective surgery for the laparoscopic removal of her gallbladder. The operation was uneventful, with very little blood loss. However, Mrs. Smith failed a reversal of anaesthesia and therefore remained intubated and ventilated whereupon she was transferred to the ICU until such time that she could be extubated. On arrival into the ICU she was placed on continuous cardiac monitoring. Her baseline vital signs were recorded which showed a systolic blood pressure (BP) of 95 mmHg, heart rate (HR) of 110 beats/min an axilla temperature of 37.6 °C, transcutaneous oxygen saturations (SaO2) of 98% on an FiO2 of 40% via the ventilator and a sedation score of −5 (unarousable to physical stimuli) on the Richmond Agitation and Sedation Scale (RASS). She was given a fluid challenge as a result of her lowered BP and rising temperature. She is receiving intravenous fluids at 120 ml/h, and regular morphine pain relief via a patient-controlled analgesia pump with a background infusion rate of 1 mg/h. Mrs. Smith is what would be affectionately known as a ‘warm, wake and wean’ patient. As the anaesthesia begins to wear off, Mrs. Smith’s RASS score improves, and she is able to respond to verbal commands. A trial of weaning is commenced where upon she is successfully extubated and placed on 6ltrs/hour of oxygen via a face mask. Mrs. Smith is monitored for 24 h and then discharged back to her admitting ward.
3.4. Contrary case (Step 6)
The fictional contrary case contains none of the defining attributes that would signify critical illness nor would require an intensive care unit admission for critical care.
Mr. Brian Koenig is a 35-year-old man with chronic gastritis and was admitted to the day case surgical unit for routine gastroscopy. Mr. Koenig, is given a mild sedative, placed on continuous cardiac monitoring (BP, HR, SaO2, RR) and receiving oxygen at 6 L/h via a face mask. The gastroscopy was uneventful, his vital signs remained stable, and Mr Koenig was transferred back to the day-case ward, monitored for 4 h and discharged home with a follow-up appointment for outpatients two weeks later.
3.5. Antecedents (Step 7)
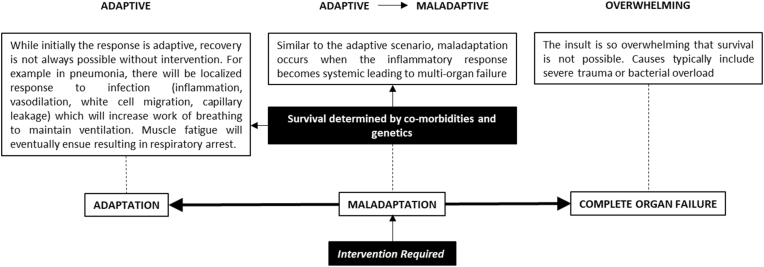
Antecedents are those factors that must occur prior to an occurrence of the concept [5]. From the perspective of critical care, the antecedents are those factors attributable to illness, which over time progresses to a level of criticality and therefore would influence an admission to an intensive care unit. In this respect, critical illness can be considered along a spectrum of adaptation to complete organ failure with maladaptation being the demarcation necessitating immediate intervention (Fig. 2). As in the example of the model case, the individual has underlying chronic disease which makes them more susceptible to illness because of a depressed or ineffective immune response. What then results is the transition from a simple chest infection (adaptive) to pneumonia (maladaptive) and then systemic inflammatory response syndrome (SIRS)/sepsis (overwhelming).
Fig. 2.
The antecedents of critical illness.
3.6. Consequences (Step 7)
Unlike antecedents, which occur before the concept, the consequences are those events that transpire as a result of the occurrence or the outcomes of the concept [5]. The consequences associated with critical care are concerned with the decline in both physical and psychological functioning, ranging from sarcopenia, depression, cognitive decline and post-traumatic stress disorder (PTSD) [[18], [19], [20]]. These result in a condition commonly known as post-ICU syndrome [62,63]. The effects are a combination of both critical illness and the treatment modalities being used. For example, positive pressure ventilation along with critical illness has been shown to cause respiratory muscle dysfunction as a result of mitochondrial dysregulation, muscle inactivity and metabolic oversupply [64,65]. Likewise, psychological impairment is related to both pre-ICU cognitive functioning and the incidence of delirious episodes each of which can lead to post-ICU PTSD, depression and worsening or new cases of dementia [[66], [67], [68]].
Moreover, while critical care is reliant on the patient being critically ill, there is also the nature of the ICU itself especially in terms of what level of critical care can be delivered. This is often dependent on the size of the hospital and the availability of resources, both human and physical. The human resource is very much dependent on patient acuity, which often necessitates an inter-professional team approach with advanced qualifications and experience to provide an immediate and critical level of care. Based on Marshall et al.’s [69] classification system of ICU’s from Level 1 to 3 denotes the level of care that can be provided safely and competently. A Level 1 ICU, for example, has many basic elements of critical care in terms of monitoring capacity and physiologic stabilisation, the level of invasive support and personnel expertise. A Level 2 ICU can provide basic support for failing organs such mechanical ventilation, inotropic support and renal dialysis, invasive monitoring and personnel often have additional critical care training and education. A Level 3 ICU provides critical care for more complex patients. This often involves more complex forms of haemodynamic monitoring and advanced modes of mechanical ventilation such as prone ventilation or extra-corporeal membrane oxygenation. It is evident that the level of medical (micro) care differs between the subsequent ICUs, the macro level care invariably remains unchanged. Both nursing and allied health practices remain relatively stable.
3.7. Empirical referents (Step 8)
The empirical referents are described as phenomenal categories that empirically demonstrate the actual occurrence of the concept in question. They are not, however, tools used to measure the concept, instead are used to measure the defining characteristics [5]. However, the difficulty with defining the empirical referents is that critical care is often associated with the ICU, which are two separate entities. One is a physical location while the other is deemed to be an advanced level of care required to support and treat a patient who is critically ill. The literature is resplendent with examples of the quality of the care experienced in the ICU [29,30], but less about measuring the actual care. Perhaps this is based on mortality and survival rates, suggesting that if the patient survived the ICU, care must have been appropriate and importantly evidenced based. As yet there are few valid tools to measure critical care apart from self-reported satisfaction scales [[31], [32], [33]], illness severity scores [34,70] or survival data [36].
3.8. Operational definition
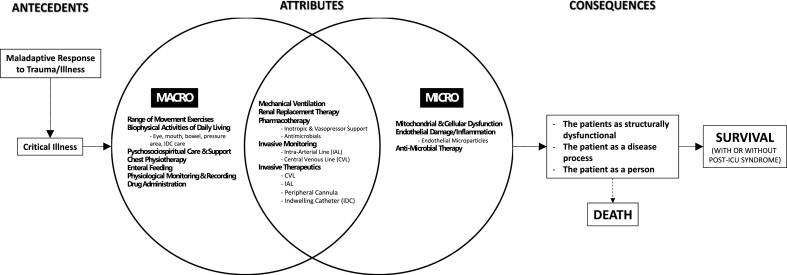
Based on these defining attributes, it might be possible to form a working theoretical definition of critical care as well as construct a possible conceptual model of critical care.
Critical care is the application of advanced medical technologies administered by specialist health care professionals to alleviate the inherent physiopsychosocial complications associated with critical illness while treating the underlying disease process.
From this definition, the characteristics of critical care encompass the three health professions based on their respective expertise in supporting critical illness (Fig. 3). Medicine as supporting and treating the underlying pathophysiology – the person as a disease process. Nursing as the administrators of care cooperating and supporting respective treatment options as well as applying their own specialised nursing care – the patient as a person. Allied health as the ‘rebuilders’– the patient as structurally dysfunctional.
Fig. 3.
Characteristics of Intensive Care incorporating the Antecedents, Attributes and Consequences.
4. Discussion
These early definitions refer to critical care as a service for those individuals with recoverable life-threatening illness or injury where more intense observation and treatment are available than on the general wards [37]. Referring to two separate criteria associated with the meaning of critical care, Lynaugh and Fairman [ [71], p20] suggest that first, the individual is at risk of dying as a result of serious physiological instability and secondly, “intensive care is usually given in the expectation or hope, however slim, of the person's survival”. More recently, Marshall et al. [69] defines critical care as:
“… a multidisciplinary and interprofessional specialty dedicated to the comprehensive management of patients having, or at risk of developing, acute, life-threatening organ dysfunction.” (p271)
However, the contemporary critical care medical and nursing literature also refers to intensive care or critical care as a physical space, geographically placed to enable easy access for patient admissions from a variety of places such as the operating theatres, the clinical wards or the emergency department [13,18,72]. Alcott’s [11] early description of an ICU room has changed considerably over time. The ICU as a space is mentioned as early as 1923 with the opening of a three-bedded ICU to monitor and treat post-operative neurosurgical patients [4]. It wasn’t until the early 1950s that the precursor to the modern ICU came into being as a result of polio epidemic [12,13]). Prior to this, what would be termed intensive care units appears to be simply recovery rooms [3]. What is significant in this initial identification of the concept in use, is that critical care is used to denote an interdisciplinary specialty [69], a critical level of illness and the congregation of the critically ill into one specialist place for care and treatment.
4.1. Critical care: a process of care, cure and function
The nature of critical care is perhaps dichotomous and symbiotic at the same time because of the inter-play between the pathology of disease processes and how care is delivered and perceived [1,40]. First, it has often been described as the application of technology to support and measure failing organ systems to determine appropriate treatment options, which would sit easily with the medical model of diagnosis, treatment and cure [12,41,42]. Second, critical care is also viewed from a psychosociospiritual aspect that is seen as the basis of holistic nursing care and practice and last, critical care is seen as the restoration of physical function which is more applicable to the work of allied health in particular physiotherapy. The centre of what is deemed critical care is the technological application associated with care. McClure [73], for example, defines technology as:
“… any means of delivering care using objects that are not part of a patient’s own body. This means that it includes not only the vast array of machinery we have come to take for granted, but also the pharmaceuticals that are prescribed and administered.” (p144)
Or more aptly, “… the substitution of machine labour in the performance of a given task ([74], p74) and “… as a collection of technological acts within the technological environment” ([75], p438), in this case the intensive care unit.
Technology in the sense of critical care involves two distinct processes – monitoring/measurement and supportive treatment. First, the monitoring/measurement capabilities are used to analyse and display indirect and/or direct physiological functions, for example electrocardiography, intra-arterial blood pressure, central venous pressure and transcutaneous oxygen saturation. Second, supportive treatment includes equipment used to support compromised or failing organ systems such as a mechanical ventilator either invasive or non-invasive, extra-corporeal membrane oxygenator, dialysis machine, intra-aortic balloon pump, all used within the context of the patient condition. Included in this array of equipment are volumetric and syringe driver pumps used for drug and/or intravenous fluid administration and an enteral feeding pump to support the nutritional needs of the patient [46]. In terms of ICU personnel, the equipment when employed in this fashion is used to primarily aide decision making regardless of the how or what equipment is being used [47]. For example, an increase in airway pressures (monitoring/measurement) would necessitate a change in ventilatory parameters (supportive treatment) to reduce these while optimising oxygenation and carbon dioxide elimination or a change in mean arterial pressure might mean a change in inotropic support or an intravenous fluid challenge.
When described in this manner, it is easy to attribute this as the technical-rationale [16] medical model of care and as mentioned earlier fits within the domain of medicine. Nursing, however, can also be ascribed this process of care because of the technological environment that is encompassed in the ICU. This has been articulated by a number of authors who have concluded that nurses can and do become unwittingly machine-like in their approach to patient care especially in this environment as a means of supporting, to a large part, medical decision-making [1,48]. However, ICU nursing is also focused on the psychosociospiritual aspect of care especially in supporting the family members in the early stages of the ICU admission and then in the latter rehabilitative stages to both the patient and family. This is a unique position for the ICU nurse when compared to medicine and allied health for one specific reason – nursing offers 24-h care whereas medicine and allied health tend to provide care as ‘snap-shots of activity’, for example, medical ward rounds or chest physiotherapy sessions. In Price’s [47] ethnographic study, she found that, in contrast to those behaviours of care which might be easily attributable to technological care (monitoring/measurement), ‘being present’ and compassionate was distinctive to nursing. Likewise, the work of Bishop et al. [49], Jones et al. [50], Jakimowicz et al. [51] and Efstathiou and Ives [52] discuss that compassionate care is a hallmark of nursing practice in the ICU. They all describe compassionate care as encompassing those elements of humanness that responds to individual suffering. For example:
“Compassion asks us to go where it hurts, to enter into places of pain, to share in brokenness, fear, confusion, and anguish. Compassion means full immersion into the condition of being human.” ([53], p52)
Structural dysfunction in critical illness can be considered both at the macro and micro levels (Fig. 2). At the micro level, this is often seen as supporting organ systems affected by mitochondrial or cellular dysfunction [54], for example, adrenal insufficiency [55], diaphragmatic ineffectiveness [56], gastro-intestinal dysfunction [57] and neurocognitive dysfunction [76]. At the macro level, restoring structural dysfunction entails reversing the effects of illness-induced sarcopenia and aiding in normal physiological processes, sometimes complicated by supportive therapies such as mechanical ventilation. These may include early enteral nutrition to reduce gut mucosal degradation, therefore reducing the incidence of bacterial translocation [59,60], ROM exercises to reduce joint contractures, early mobilisation to reduce muscle wasting [21,61] and chest physiotherapy to improve secretion removal and reduce the incidence of ventilator-induced alveolar collapse [22,23]. Medicines’ role at the micro level is focused on those supportive therapies, for example, the inception of mechanical ventilation and the prescribing of drug therapy. Their role at the macro level is minimal except perhaps the placing of invasive lines and prescribing care that will normally be undertaken by either nursing or allied health (Fig. 2). While equally conversant and responsible with the macro level of care, nursing as the administrator of the medical model will naturally adopt a supportive, facilitative and cooperative role with both medicine and allied health. Alternatively, allied health will generally provide and direct the functional recovery such as mobility and ROM exercises as well as chest physiotherapy and as such facilitates in reducing the overall effects of critical illness [22,24,61].
4.2. Critical illness
The natural progression to critical illness is seen as a fine inter-play between pathophysiological adaptation and maladaptation. This is generally seen as a result of disruption to oxygen supply and demand at the micro-circulatory level in response to a potentially life-threatening insult [[24], [25], [26], [27], [28]] (Fig. 3). During the adaptive phase, the normal processes associated with acute inflammation come into play involving both the innate immune and haemopoietic systems in an attempt to contain the injury or infection locally. However, if these systems become overwhelmed, a systemic inflammatory response then ensues causing organ dysfunction (maladaptive). If there is no reversal to the maladaptive stage multi-organ failure follows leading to death. The criteria which decides when adaptation becomes maladaptive is generally governed genetically and by co-morbid conditions present in the individual [25]. Therefore, the basis of diagnosing critical illness is often dependent on a number of pathophysiological processes [35,38,39] seen through the presenting disease symptomology for example, pyrexia, tachycardia and hypotension.
However, describing and defining critical illness based on diagnosis alone is often difficult and typically critically ill patients fall between two separate categories – too well to benefit (low risk of death) or too sick to benefit (high risk of death) [77]. Therefore, what determines critical illness is generally based on admission criteria often involving a significant decline in physiological functioning [39] in some form and the application of illness severity classification systems such as SAPS (Simplified Acute Physiological Score) [34,70] or SOFA (Sequential Organ Failure Assessment Score) [43] or TISS-28 (Therapeutic Intervention Scoring System) [44,45]. At present, there are three distinct models of ICU admission – prioritisation, diagnosis and physiological function (objective parameters) each of which serves as the basis, singularly or collectively, of defining and describing illness severity [77]. The prioritisation model determines patient characteristics based on benefit and need – those who will benefit versus those that won’t. The diagnosis model determines illness severity based on survivable outcomes, similar in some respects to the prioritisation model, but instead focused on an admission diagnosis such as myocardial infarction or traumatic brain injury. Finally, the objective parameter model uses physiological and investigative information to determine illness severity. However, there are also ethical and economic factors, which may influence an admission to ICU.
While these criteria provide some assistance for the clinician in determining who gets an ICU admission, there is perhaps a ‘loose’ connection as to defining or indeed describing critical illness. As mentioned previously illness severity classification systems such as SAPS or APACHE (Acute Physiological and Chronic Health Evaluation) scores are used to classify patients within specific groups of illness severity, the difference being that this is a mortality risk predicative tool as opposed to a decision-making tool [78]. There was an attempt to define illness severity in palliative care patients undergoing elective surgery. Using a Delphi method and a current evidence base of care, Lee et al. [58] were able to define illness severity based on ASA (American Society of Anaesthetists) risk and age (a subjective physiological based tool designed to predict perioperative risk, the higher the number the higher the risk of mortality). However, like the use of criteria modelling and severity classification scores, the definition identified here is also based on a classification system, which considers not only those mentioned above such as comorbid states, age, gender and cognitive function but also frailty. Therefore, building on the definition described by Kayambankadzanja et al. [15] it might be possible to find a single definition of critical illness which might consider the following:
Critical illness is a process in which normal or optimal physiological functioning has been severely compromised where advanced medical treatment is a necessity to preserve life.
5. Implications for practice and potential future research
Therefore, the implications for future research could encompass studies that accurately reflect the ‘care’ of the intensive care environment. In addition, describing critical care is challenging because each health professional group defines the concept based on their specific expertise. In other words, what is defined and described as critical care as opposed to the current medical model of care. As a result, nursing care associated with the critically ill, for example, can be considered universal across the spectrum of nursing, the major difference being the acuity of the patient. Therefore, further evidence of what constitutes critical care is required so that the defining attributes clearly articulate what is critical care is and is not, for example: adherence to nursing guidelines, implementation of new concepts for monitoring/documentation of wellbeing and satisfaction, and perhaps defining suitable nurse-patient ratios.
6. Limitations
The idea of concept analysis is to get a broader, deeper understanding and clarification of a concept. The limitations of this analysis lie in that it only considered published work reported in English and those from within a western context. Therefore, this may limit the depth and breadth of work reported elsewhere because of issues related to translation and interpretation. In addition, the nebulous nature of what defines and describes critical care means that the care provided in this area could equally be transposed into other clinical areas; the difficulty is that the subjectiveness of the term critical care means many different things to many different people. Yet, in saying that it is the patient acuity that may truly define what ‘critical care’ is.
7. Conclusion
When the term critical care is used, it invariably conjures up images of a physical space – ‘the patient is being transferred to intensive care’ or ‘the patient is in intensive care’ or ‘I work in intensive care’. It is often taken for granted that the patient is receiving critical care, as such describing or defining the nature of the care provided is often challenging and consumed within the medical model of care. This concept analysis of what constitutes critical care has identified key defining attributes of what comprises ‘critical care’, namely micro and macro levels of care. Additionally, in providing a working definition of critical care, it has used hypothetical clinical cases to highlight what is deemed critical care and what is not. Therefore, given that care is multi-dimensional and multi-factorial, providing a conceptual framework of what denotes critical care may give rise to more focused research in addition to that already undertaken.
Funding
Nothing to declare.
Data availability statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
CRediT authorship contribution statement
Martin Christensen: Conceptualization, Formal analysis, Writing – original draft, Writing – review & editing. Mining Liang: Conceptualization, Writing – original draft, Writing – review & editing.
Declaration of competing interest
There are no conflicts of interest.
Footnotes
Peer review under responsibility of Chinese Nursing Association.
Supplementary data to this article can be found online at https://doi.org/10.1016/j.ijnss.2023.06.020.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Christensen M., Probst B. Barbara's story: a thematic analysis of a relative's reflection of being in the intensive care unit. Nurs Crit Care. 2015;20(2):63–70. doi: 10.1111/nicc.12145. [DOI] [PubMed] [Google Scholar]
- 2.Sadove M.S., Cross J., Higgins H.G., Segall M.J. The recovery room expands its service. Mod Hosp. 1954;83(5):65–70. [PubMed] [Google Scholar]
- 3.Trubuhovich R.V. The Name of our specialty: with a historical perspective on “intensive care”. Crit Care Resusc. 2008;10(4):328–331. [PubMed] [Google Scholar]
- 4.Vincent J.L. Critical care: where have we been and where are we going? Crit Care. 2013;17(Suppl 1):S2. doi: 10.1186/cc11500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Walker L., Avant K. Pearson; New York: 2018. Strategies for theory construction in nursing. [Google Scholar]
- 6.Tricco A.C., Lillie E., Zarin W., O'Brien K.K., Colquhoun H., Levac D., et al. PRISMA extension for scoping reviews (PRISMA-ScR):Checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 7.Moher D., Liberati A., Tetzlaff J., Altman D.G. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7) doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Oxford University Press . twelfth ed. Oxford University Press Oxford; London: 2011. The Concise Oxford dictionary. [Google Scholar]
- 9.Cambridge University Press . fourth ed. Cambridge University Press; London: 2013. Cambridge English dictionary. Cambridge. [Google Scholar]
- 10.Wallace D.J., Kahn J.M. Florence nightingale and the conundrum of counting ICU beds. Crit Care Med. 2015;43(11):2517–2518. doi: 10.1097/CCM.0000000000001290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alcott L.M. James Redpath Publishing; Boston: 1863. Hospital Sketches. [Google Scholar]
- 12.Berthelsen P.G., Cronqvist M. The first intensive care unit in the world: copenhagen 1953. Acta Anaesthesiol Scand. 2003;47(10):1190–1195. doi: 10.1046/j.1399-6576.2003.00256.x. [DOI] [PubMed] [Google Scholar]
- 13.White P. Cardiff University; 2008. On producing and reproducing intensive care: the place of the patient, the place of the other (PhD thesis) [Google Scholar]
- 14.Jackson M., Cairns T. Care of the critically ill patient. Surgery. 2020;39(1):29–36. doi: 10.1016/j.mpsur.2020.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kayambankadzanja R.K., Schell C.O., Gerdin Wärnberg M., Tamras T., Mollazadegan H., Holmberg M., et al. Towards definitions of critical illness and critical care using concept analysis. BMJ Open. 2022;12(9) doi: 10.1136/bmjopen-2022-060972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kinsella E.A. Technical rationality in Schön’s reflective practice: dichotomous or non-dualistic epistemological position. Nurs Philos. 2007;8(2):102–113. doi: 10.1111/j.1466-769X.2007.00304.x. [DOI] [PubMed] [Google Scholar]
- 17.Krippendorf K. fourth ed. Sage; London: 2018. Content Analysis: an introduction to its methodology. [Google Scholar]
- 18.Kizilarslanoglu M.C., Kuyumcu M.E., Yesil Y., Halil M. Sarcopenia in critically ill patients. J Anesth. 2016;30(5):884–890. doi: 10.1007/s00540-016-2211-4. [DOI] [PubMed] [Google Scholar]
- 19.Bakhru R.N., Davidson J.F., Bookstaver R.E., Kenes M.T., Welborn K.G., Morris P.E., et al. Physical function impairment in survivors of critical illness in an ICU Recovery Clinic. J Crit Care. 2018;45:163–169. doi: 10.1016/j.jcrc.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kerckhoffs M.C., Kosasi F.F.L., Soliman I.W., van Delden Jjm, Cremer O.L., de Lange D.W., et al. Determinants of self-reported unacceptable outcome of intensive care treatment 1 year after discharge. Intensive Care Med. 2019;45(6):806–814. doi: 10.1007/s00134-019-05583-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sommers J., Engelbert R.H.H., Dettling-Ihnenfeldt D., Gosselink R., Spronk P.E., Nollet F., et al. Physiotherapy in the intensive care unit: an evidence-based, expert driven, practical statement and rehabilitation recommendations. Clin Rehabil. 2015;29(11):1051–1063. doi: 10.1177/0269215514567156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hanekom S., Louw Q.A., Coetzee A.R. Implementation of a protocol facilitates evidence-based physiotherapy practice in intensive care units. Physiotherapy. 2013;99(2):139–145. doi: 10.1016/j.physio.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 23.van der Lee L., Hill A.M., Patman S. Clinical validation of expert consensus statements for respiratory physiotherapy management of invasively ventilated adults with community-acquired pneumonia: a qualitative study. Intensive Crit Care Nurs. 2020;60 doi: 10.1016/j.iccn.2020.102854. [DOI] [PubMed] [Google Scholar]
- 24.Fletcher S.J., Cuthbertson B.H. Outreach, epistemology and the evolution of critical care. Anaesthesia. 2010;65(2):115–118. doi: 10.1111/j.1365-2044.2009.06157.x. [DOI] [PubMed] [Google Scholar]
- 25.Garrabou G., Morén C., López S., Tobías E., Cardellach F., Miró O., et al. The effects of sepsis on mitochondria. J Infect Dis. 2012;205(3):392–400. doi: 10.1093/infdis/jir764. [DOI] [PubMed] [Google Scholar]
- 26.Trentadue R., Fiore F., Massaro F., Papa F., Iuso A., Scacco S., et al. Induction of mitochondrial dysfunction and oxidative stress in human fibroblast cultures exposed to serum from septic patients. Life Sci. 2012;91(7–8):237–243. doi: 10.1016/j.lfs.2012.06.041. [DOI] [PubMed] [Google Scholar]
- 27.Quoilin C., Mouithys-Mickalad A., Lécart S., Fontaine-Aupart M.P., Hoebeke M. Evidence of oxidative stress and mitochondrial respiratory chain dysfunction in an in vitro model of sepsis-induced kidney injury. Biochim Biophys Acta. 2014;1837(10):1790–1800. doi: 10.1016/j.bbabio.2014.07.005. [DOI] [PubMed] [Google Scholar]
- 28.de Jager P., Smith O., Pool R., Bolon S., Richards G.A. Review of the pathophysiology and prognostic biomarkers of immune dysregulation after severe injury. J Trauma Acute Care Surg. 2021;90(2):e21–e30. doi: 10.1097/TA.0000000000002996. [DOI] [PubMed] [Google Scholar]
- 29.Jeffs E.L., Darbyshire J.L. Measuring sleep in the intensive care unit: a critical appraisal of the use of subjective methods. J Intensive Care Med. 2019;34(9):751–760. doi: 10.1177/0885066617712197. [DOI] [PubMed] [Google Scholar]
- 30.Savjani K., Haseeb F., Reay M. Measuring quality and outcomes in intensive care. Surg Oxf. 2018;36(4):196–200. doi: 10.1016/j.mpsur.2018.01.008. [DOI] [Google Scholar]
- 31.Ahlberg M., Bäckman C., Jones C., Walther S., Hollman Frisman G. Moving on in life after intensive care: partners' experience of group communication. Nurs Crit Care. 2015;20(5):256–263. doi: 10.1111/nicc.12192. [DOI] [PubMed] [Google Scholar]
- 32.Clark K., Milner K.A., Beck M., Mason V. Measuring family satisfaction with care delivered in the intensive care unit. Crit Care Nurse. 2016;36(6):e8–e14. doi: 10.4037/ccn2016276. [DOI] [PubMed] [Google Scholar]
- 33.McLennan M., Aggar C. Family satisfaction with care in the intensive care unit: a regional Australian perspective. Aust Crit Care. 2020;33(6):518–525. doi: 10.1016/j.aucc.2020.01.003. [DOI] [PubMed] [Google Scholar]
- 34.Metnitz P.G.H., Moreno R.P., Almeida E., Jordan B., Bauer P., Campos R.A., et al. SAPS 3:From evaluation of the patient to evaluation of the intensive care unit. Part 1:Objectives, methods and cohort description. Intensive Care Med. 2005;31(10):1336–1344. doi: 10.1007/s00134-005-2762-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Protti A., Fortunato F., Artoni A., Lecchi A., Motta G., Mistraletti G., et al. Platelet mitochondrial dysfunction in critically ill patients: comparison between sepsis and cardiogenic shock. Crit Care. 2015;19(1):39. doi: 10.1186/s13054-015-0762-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Simpson A., Puxty K., McLoone P., Quasim T., Sloan B., Morrison D.S. Comorbidity and survival after admission to the intensive care unit: a population-based study of 41, 230 patients. J Intensive Care Soc. 2021;22(2):143–151. doi: 10.1177/1751143720914229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Williams C. In: Developing expertise in critical care nursing. Scholes J., Albarran J., Williams C., editors. Wiley & Sons; London: 2006. The dynamic context of critical care provision. [Google Scholar]
- 38.McCreath G., Scullion M.M.F., Lowes D.A., Webster N.R., Galley H.F. Pharmacological activation of endogenous protective pathways against oxidative stress under conditions of sepsis. Br J Anaesth. 2016;116(1):131–139. doi: 10.1093/bja/aev400. [DOI] [PubMed] [Google Scholar]
- 39.Graham J.K., Stacy K. Mitochondrial dysregulation in sepsis. Clin Nurse Spec. 2020;34(4):170–177. doi: 10.1097/nur.0000000000000532. [DOI] [PubMed] [Google Scholar]
- 40.Wikström A.C., Cederborg A.C., Johanson M. The meaning of technology in an intensive care unit: an interview study. Intensive Crit Care Nurs. 2007;23(4):187–195. doi: 10.1016/j.iccn.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 41.Kesecioglu J. From intensive care to treatment of the critically ill. Curr Anaesth Crit Care. 2000;11(3):150–158. doi: 10.1054/cacc.2000.0261. [DOI] [Google Scholar]
- 42.Almerud S., Alapack R.J., Fridlund B., Ekebergh M. Caught in an artificial split: a phenomenological study of being a caregiver in the technologically intense environment. Intensive Crit Care Nurs. 2008;24(2):130–136. doi: 10.1016/j.iccn.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 43.Ferreira F.L., Bota D.P., Bross A., Mélot C., Vincent J.L. Serial evaluation of the SOFA score to predict outcome in critically ill patients. JAMA. 2001;286(14):1754–1758. doi: 10.1001/jama.286.14.1754. [DOI] [PubMed] [Google Scholar]
- 44.de Souza Urbanetto J., Travi Canabarro S., Prado Lima Figueiredo A.E., Weber G., Pereira dos Santos R., Stein K., et al. Correlation between the TISS-28 and NEMS indicators in an intensive care unit. Int J Nurs Pract. 2014;20(4):375–381. doi: 10.1111/ijn.12183. [DOI] [PubMed] [Google Scholar]
- 45.de Vivanco-Allende A., Rey C., Concha A., Martínez-Camblor P., Medina A., Mayordomo-Colunga J. Validation of a therapeutic intervention scoring system (TISS-28) in critically ill children. An Pediatr. 2020;92(6):339–344. doi: 10.1016/j.anpedi.2019.10.002. [DOI] [PubMed] [Google Scholar]
- 46.Thompson D.R., Hamilton D.K., Cadenhead C.D., Swoboda S.M., Schwindel S.M., Anderson D.C., et al. Guidelines for intensive care unit design. Crit Care Med. 2012;40(5):1586–1600. doi: 10.1097/CCM.0b013e3182413bb2. [DOI] [PubMed] [Google Scholar]
- 47.Price A.M. Caring and technology in an intensive care unit: an ethnographic study. Nurs Crit Care. 2013;18(6):278–288. doi: 10.1111/nicc.12032. [DOI] [PubMed] [Google Scholar]
- 48.Crilly G., Dowling M., Delaunois I., Flavin M., Biesty L. Critical care nurses' experiences of providing care for adults in a highly technological environment: a qualitative evidence synthesis. J Clin Nurs. 2019;28(23–24):4250–4263. doi: 10.1111/jocn.15043. [DOI] [PubMed] [Google Scholar]
- 49.Bishop J.P., Perry J.E., Hine A. Efficient, compassionate, and fractured: contemporary care in the ICU. Hastings Cent Rep. 2014;44(4):35–43. doi: 10.1002/hast.330. [DOI] [PubMed] [Google Scholar]
- 50.Jones J., Winch S., Strube P., Mitchell M., Henderson A. Delivering compassionate care in intensive care units: nurses' perceptions of enablers and barriers. J Adv Nurs. 2016;72(12):3137–3146. doi: 10.1111/jan.13064. [DOI] [PubMed] [Google Scholar]
- 51.Jakimowicz S., Perry L., Lewis J. Insights on compassion and patient-centred nursing in intensive care: a constructivist grounded theory. J Clin Nurs. 2018;27(7–8):1599–1611. doi: 10.1111/jocn.14231. [DOI] [PubMed] [Google Scholar]
- 52.Efstathiou N., Ives J. Compassionate care during withdrawal of treatment: a secondary analysis of ICU nurses' experiences. Nurs Ethics. 2018;25(8):1075–1086. doi: 10.1177/0969733016687159. [DOI] [PubMed] [Google Scholar]
- 53.Schantz M.L. Compassion: a concept analysis. Nurs Forum. 2007;42(2):48–55. doi: 10.1111/j.1744-6198.2007.00067.x. [DOI] [PubMed] [Google Scholar]
- 54.van Ierssel S.H., Jorens P.G., Van Craenenbroeck E.M., Conraads V.M. The endothelium, a protagonist in the pathophysiology of critical illness: focus on cellular markers. BioMed Res Int. 2014;2014 doi: 10.1155/2014/985813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Téblick A., Peeters B., Langouche L., Van den Berghe G. Adrenal function and dysfunction in critically ill patients. Nat Rev Endocrinol. 2019;15(7):417–427. doi: 10.1038/s41574-019-0185-7. [DOI] [PubMed] [Google Scholar]
- 56.Liu Y.Y., Li L.F. Ventilator-induced diaphragm dysfunction in critical illness. Exp Biol Med. 2018;243(17–18):1329–1337. doi: 10.1177/1535370218811950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.McClave S.A., Wischmeyer P.E., Miller K.R., van Zanten A.R.H. Mitochondrial dysfunction in critical illness: implications for nutritional therapy. Curr Nutr Rep. 2019;8(4):363–373. doi: 10.1007/s13668-019-00296-y. [DOI] [PubMed] [Google Scholar]
- 58.Lee K.C., Walling A.M., Senglaub S.S., Kelley A.S., Cooper Z. Defining serious illness among adult surgical patients. J Pain Symptom Manag. 2019;58(5) doi: 10.1016/j.jpainsymman.2019.08.003. 844-50.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Elke G., Heyland D.K. Enteral nutrition in critically ill septic patients-less or more? JPEN - J Parenter Enter Nutr. 2015;39(2):140–142. doi: 10.1177/0148607114532692. [DOI] [PubMed] [Google Scholar]
- 60.Reintam Blaser A., Berger M.M. Early or late feeding after ICU admission? Nutrients. 2017;9(12):1278. doi: 10.3390/nu9121278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lewis M. Intensive care unit rehabilitation within the United Kingdom. Physiotherapy. 2003;89(9):531–538. doi: 10.1016/S0031-9406(05)60179-4. [DOI] [Google Scholar]
- 62.Preiser J.C., Herridge M., Azoulay E. Springer; London: 2020. Post-intensive care syndrome. [Google Scholar]
- 63.Yuan C., Timmins F., Thompson D.R. Post-intensive care syndrome: a concept analysis. Int J Nurs Stud. 2021;114 doi: 10.1016/j.ijnurstu.2020.103814. [DOI] [PubMed] [Google Scholar]
- 64.Powers S.K., Kavazis A.N., Levine S. Prolonged mechanical ventilation alters diaphragmatic structure and function. Crit Care Med. 2009;37(10 Suppl):S347–S353. doi: 10.1097/CCM.0b013e3181b6e760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Matecki S., Dridi H., Jung B., Saint N., Reiken S.R., Scheuermann V., et al. Leaky ryanodine receptors contribute to diaphragmatic weakness during mechanical ventilation. Proc Natl Acad Sci USA. 2016;113(32):9069–9074. doi: 10.1073/pnas.1609707113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Jackson J.C., Pandharipande P.P., Girard T.D., Brummel N.E., Thompson J.L., Hughes C.G., et al. Depression, post-traumatic stress disorder, and functional disability in survivors of critical illness in the BRAIN-ICU study: a longitudinal cohort study. Lancet Respir Med. 2014;2(5):369–379. doi: 10.1016/S2213-2600(14)70051-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hopkins S.A.A., Chan D. Key emerging issues in frontotemporal dementia. J Neurol. 2016;263(2):407–413. doi: 10.1007/s00415-015-7880-7. [DOI] [PubMed] [Google Scholar]
- 68.Wade D., Page V. Long-term mental health after ICU, let's go through the looking glass. Crit Care Med. 2016;44(10):1934–1935. doi: 10.1097/CCM.0000000000002043. [DOI] [PubMed] [Google Scholar]
- 69.Marshall J.C., Bosco L., Adhikari N.K., Connolly B., Diaz J.V., Dorman T., et al. What is an intensive care unit? A report of the task force of the World Federation of Societies of Intensive and Critical Care Medicine. J Crit Care. 2017;37:270–276. doi: 10.1016/j.jcrc.2016.07.015. [DOI] [PubMed] [Google Scholar]
- 70.Vincent J.L., Marshall J.C., Namendys-Silva S.A., François B., Martin-Loeches I., Lipman J., et al. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2(5):380–386. doi: 10.1016/S2213-2600(14)70061-X. [DOI] [PubMed] [Google Scholar]
- 71.Lynaugh J.E., Fairman J. New nurses, new spaces: a preview of the AACN History Study. Am J Crit Care. 1992;1(1):19–24. [PubMed] [Google Scholar]
- 72.Vincent J.L., Singer M., Marini J.J., Moreno R., Levy M., Matthay M.A., et al. Thirty years of critical care medicine. Crit Care. 2010;14(3):311. doi: 10.1186/cc8979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.McClure M.L. Technology—a driving force for change. J Prof Nurs. 1991;7(3):144. doi: 10.1016/8755-7223(91)90041-i. [DOI] [PubMed] [Google Scholar]
- 74.Given C.W., Given B. Automation and technology: a key to professionalized care. Nurs Forum. 1969;8(1):74–81. doi: 10.1111/j.1744-6198.1969.tb00416.x. [DOI] [PubMed] [Google Scholar]
- 75.Barnard A. A critical review of the belief that technology is a neutral object and nurses are its master. J Adv Nurs. 1997;26(1):126–131. doi: 10.1046/j.1365-2648.1997.1997026126.x. [DOI] [PubMed] [Google Scholar]
- 76.Hughes C.G., Patel M.B., Brummel N.E., Thompson J.L., McNeil J.B., Pandharipande P.P., et al. Relationships between markers of neurologic and endothelial injury during critical illness and long-term cognitive impairment and disability. Intensive Care Med. 2018;44(3):345–355. doi: 10.1007/s00134-018-5120-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Egol A., Fromm R., Guntupalli K.K., Fitzpatrick M., Kaufman D., Nasraway S., et al. Guidelines for intensive care unit admission, discharge and triage. Intensive Care Med. 1999;36:545–551. [Google Scholar]
- 78.Knaus W.A., Wagner D.P., Draper E.A., Zimmerman J.E., Bergner M., Bastos P.G., et al. The Apache III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100(6):1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.