Abstract
Primary liver cancer is one of the most common malignant tumours worldwide; it caused approximately 830,000 deaths in 2020. Hepatocellular carcinoma (HCC) is the most common type of primary liver cancer, accounting for over 80% of all cases. Various methods, including surgery, chemotherapy, radiotherapy, and radiofrequency ablation, have been widely used in the treatment of HCC. With the advancement of technology, radiotherapy has become increasingly important in the comprehensive treatment of HCC. However, due to the insufficient sensitivity of tumour cells to radiation, there are still multiple limitation in clinical application of radiotherapy. In recent years, the role of immunotherapy in cancer has been increasingly revealed, and more researchers have turned their attention to the combined application of immunotherapy and radiotherapy in the hope of achieving better treatment outcomes. This article reviews the progress on radiation therapy in HCC and the current status of its combined application with immunotherapy, and discusses the prospects and value of radioimmunotherapy in HCC.
Keywords: Hepatocellular carcinoma, Radiotherapy, Immunotherapy, Radioimmunotherapy
Introduction
Primary liver cancer is the third leading cause of cancer-related mortality worldwide, accounting for 8.3% of total cancer deaths, following lung cancer (18.0%) and colorectal cancer (9.4%). In 2020, it accounted for a total of 830,000 deaths and 906,000 new cancer cases globally, and it has significantly higher incidence and mortality rates in males than in females [1]. Hepatocellular carcinoma (HCC) is the main type of primary liver cancer, and China is a high-risk region for HCC [2]. Chronic viral infection is the major factor leading to HCC, and other risk factors include exposure to aflatoxin, excessive alcohol consumption, obesity, etc. [3]. The treatment options for HCC vary depending on factors such as tumour stage, and location [4]. For early-stage HCC patients, local resection and liver transplantation are the preferred treatment options, with 5-year survival rates ranging from 70 to 80% [5]. Radiofrequency ablation is the preferred alternative method for unresectable early-stage HCC patients, and transarterial chemoembolization is the standard choice for intermediate-stage HCC patients [6]. However, most HCC patients are diagnosed at an advanced stage, at which point they have lost the opportunity for local curative treatment [7]. Although the combination of the anti-PD-L1 antibody atezolizumab and the anti-VEGF antibody bevacizumab has significantly improved the survival of advanced-stage patients, drug resistance remains a pressing issue that needs to be addressed [8].
With the continuous advancement of technology, the role of radiotherapy has been increasingly recognized, and it has been widely used as an integral part of comprehensive treatment for HCC [9]. Precision radiotherapy techniques, such as stereotactic body radiotherapy (SBRT), accurately deliver high doses to the target area while reducing radiation damage to surrounding normal organs and tissues; these approached, show excellent local control in early-stage HCC patients who are not eligible for surgery or ablation treatment and play an important role as bridging therapy options for liver transplantation [10–12]. Radiation sensitivity is a primary barrier that limits the efficacy of tumour treatment, and the mechanisms affecting radiation sensitivity in HCC are complex and diverse. Combination with other treatment modalities may offer more clinical benefits for patients [13]. The liver harbours the largest population of tissue-resident macrophages, known as Kupffer cells, as well as various other types of infiltrating lymphocytes, creating a unique tumour microenvironment in HCC [14]. Previous studies have also shown that radiotherapy can enhance the immunogenicity of tumours, indicating the great potential of combining radiotherapy with immunotherapy in the comprehensive treatment of HCC [15]. This review summarizes the progress on radiotherapy in HCC and the current status of radiotherapy combined with immunotherapy, and discusses the future prospects and research value of this combination treatment approach in HCC.
Current status of radiotherapy for HCC
As a common malignant tumour, primary liver cancer ranks third in global cancer mortality, following lung cancer and colorectal cancer. According to statistics, there were approximately 906,000 new cases and 830,000 deaths from primary liver cancer worldwide in 2020, and the incidence and mortality rates in males were 2–3 times higher than those in females in most regions [1]. Data from the National Cancer Center (NCC) of China show that primary liver cancer ranks fourth among malignant tumours in China in terms of incidence and second in terms of mortality rate, imposing a heavy disease burden on the country [16]. HCC accounts for approximately 80–90% of primary liver cancer cases, while intrahepatic cholangiocarcinoma (CCA) and other rare types account for 10–15%. The main risk factors for the development of HCC include infection with hepatitis B virus (HBV) or hepatitis C virus (HCV), chronic toxin exposure (such as aflatoxin), alcohol abuse, obesity, etc., with the first two being the predominant factors in China [17]. For early-stage HCC patients, surgical resection is the preferred curative treatment, but most patients are diagnosed at advanced stages, and only a few patients have the opportunity to undergo radical resection [18]. Local treatment strategies, including radiofrequency ablation or microwave ablation, are mostly used to control tumours with a diameter smaller than 4 cm, and their efficacy is limited in large tumours or tumours near major blood vessels or with vascular involvement [19]. Systemic treatments such as sorafenib, lenvatinib, and other targeted therapies have improved the prognosis of advanced HCC, but primary or acquired drug resistance still occurs in a significant proportion of patients [20].
In recent years, radiotherapy has gradually become widely used as an important local therapy for HCC and has become an essential component of its comprehensive treatment. Early limitations in technology, such as limited accuracy and wide irradiation range of radiotherapy, resulted in suboptimal treatment outcomes, high toxicity, and inadequate dosages. With the emergence of precision radiotherapy techniques, these issues have gradually been overcome [21]. With steep dose gradients and precise target coverage, SBRT is an important local treatment method for HCC, not only demonstrating excellent local control in the primary tumour, but also serving as a safe and effective therapy for bridging to liver transplantation and reducing tumour volume [22]. A study of 297 HCC patients without vascular invasion included in the research tracked overall survival (OS), liver function, alpha-fetoprotein, and other indicators within five years after SBRT. The results showed that SBRT provided high local control and long-term survival for a significant proportion of HCC patients who were not eligible for or had adverse effects with standard local regional treatment [23]. For HCC patients with microvascular invasion at the surgical margin, SBRT can also provide a safe adjuvant treatment option to prevent local recurrence and improve disease-free survival [24]. In a study comparing the local control rates and OS of SBRT and transarterial chemoembolization (TACE) in patients with medium-sized HCC tumours (diameter 3–8 cm), SBRT showed better local control rates and OS than TACE, particularly for recurrent HCC patients [25]. Another study showed that for 1–2 tumours, SBRT can be a safe alternative to TACE, but no significant difference in OS was observed between the two [26]. A retrospective cohort study found that SBRT had a lower risk of local recurrence than radiofrequency ablation (RFA); subgroup analysis also showed that SBRT was associated with better local control rates for small tumours (diameter ≤ 3 cm) irrespective of location; for tumours located below the diaphragm and tumours progressing after TACE, SBRT showed lower toxicity than RFA. Therefore, SBRT may be an effective alternative to RFA for unresectable HCC [27]. Liver transplantation is an important life-saving option for some HCC patients, but there is a risk of tumour progression or recurrence during the waiting process for a liver transplant [4]. Researchers have compared the safety and effectiveness of SBRT, TACE, and RFA as bridging therapies for liver transplantation, and the results showed that SBRT can be a good alternative to conventional bridging therapies [28]. Patients with advanced HCC with macrovascular invasion usually have a poor prognosis, and the response to sorafenib and the survival benefit are still unsatisfactory [29]. In a prospective randomized controlled trial, researchers compared the treatment outcomes of patients receiving sorafenib alone and patients receiving TACE plus SBRT. The results showed that the progression-free survival rate at week 12 was significantly higher in the TACE-SBRT group than in the sorafenib group, and the median progression-free survival and OS rates at week 24 were notably higher in the TACE-SBRT group than in the sorafenib group. Therefore, TACE plus SBRT may be a better treatment option than sorafenib alone for advanced HCC patients with macrovascular invasion [30]. In addition to SBRT, high-dose fractionated proton beam therapy (HPT) is also a treatment option for HCC. A phase II study evaluated the efficacy and safety of HPT in HCC. The results showed a 2-year local control rate of 94.8% and a 2-year overall survival rate of 63.2%, indicating that the application of HPT in HCC is safe and effective [31].
However, limited sensitivity of tumour to radiotherapy is one of the important factors that results in lower-than-expected treatment outcomes [32–34]. A study observed the survival fraction of HCC cell lines in 16 patients and classified them into sensitive, moderately sensitive, and radioresistant groups. The results showed that the radiosensitivity of the cell lines was mainly distributed in the moderately sensitive group (43.75%) and the radioresistant group (37.5%), with only approximately one-fifth of the cell lines (18.75%) classified as sensitive [35]. Although various solid tumours, including cervical cancer, have been treated with concurrent chemotherapy to enhance sensitivity to radiotherapy, the effects of traditional radiosensitizers such as mitomycin and 5-FU in HCC seem to be less satisfactory. Therefore, improving the radiosensitivity of HCC to enhance treatment outcomes has become a current research hotspot [36].
The DNA damage response (DDR) induced by radiation is key to the tumour-killing effect of radiotherapy, with DNA double-strand breaks (DSBs) being the most lethal form of damage, which is repaired mainly through homologous recombination (HR) or nonhomologous end joining (NHEJ) pathways [37]. These DNA damage repair responses confer protection to normal tissues, while providing resistance to radiation in tumour cells [38]. As one of the most prevalent RNA modifications, N7-methylguanosine (m7G) plays an important role in regulating RNA processing, function, and gene expression and is catalysed mainly by methyltransferase-like 1 (METTL1) and WD repeat domain 4 (WDR4) proteins [39]. Studies have revealed that METTL1/WDR4-mediated modification of m7G tRNA can significantly promote HCC progression, and this promotion effect is associated with cell cycle regulation and EGFR signalling pathways. Knockdown of METTL1 inhibits the translation of cell cycle protein A2, which subsequently leads to G2/M cell cycle arrest. It also reduces the mRNA translation of EGFR and VEGFA signalling pathway components, thereby inhibiting HCC proliferation and metastasis [40]. Studies have explored the interaction between tRNA modification and radiation resistance and found that the RNA methyltransferase METTL1 is closely related to the radiation resistance in HCC. The results showed that tRNA modification catalysed by METTL1 can promote DNA double-strand break repair, leading to insensitivity of HCC to radiotherapy. The molecular mechanism is that the m7G tRNA modification mediated by METTL1 is able to upregulate the translation of DNA-dependent protein kinase catalytic subunits (DNA-PKcs) or DNA ligase IV required for DNA damage repair, which improves the efficiency of DSB repair in the NHEJ pathway. In addition, clinical data have also shown that high expression of METTL1 is significantly correlated with a poor prognosis in HCC patients after radiotherapy [41]. Epidermal growth factor receptor (EGFR) is a member of the subfamily of membrane-bound receptor tyrosine kinases (RTKs), which can phosphorylate intracellular tyrosine residues, activate downstream signalling pathways (e.g., the RAS-RAF-MEK-ERK, JAK-STAT, and PI3K-AKT pathways) and regulate a wide range of biological processes [42]. EGFR mutations have been shown to promote the development and progression of various tumours [43–45]. Despite the promising results of drugs targeting EGFR in tumours, their complex drug resistance cannot be ignored [46]. Studies have shown that the activation of EGFR significantly inhibits the response of HCC to the tyrosine kinase inhibitor lenvatinib, and this resistance is overcome after inhibition of the EGFR -STAT3-ABCB1 pathway [47, 48]. In addition, mutations in EGFR are also closely associated with radiotherapy resistance, with proliferation of tumour cells, DNA damage repair, hypoxia, and tumour metastasis formation being the four mechanisms, and DNA damage repair occupying an important position [49]. DNA-PKcs is a key enzyme in the NHEJ pathway that can be used to facilitate DNA damage repair after exposure to radiation [50]. However, radiation can promote the translocation of EGFR to the nucleus or promote the activation of EGFR directly, which could increase the activity of DNA-PKcs and promote DSB repair in the NHEJ pathway, making radiation ineffective [38]. Another study found that ubiquitin-conjugating enzyme E2T (UBE2T) is upregulated in HCC, and HCC patients with higher levels of UBE2T are less sensitive to radiotherapy. This is because the presence of radiation resistance is due to monoubiquitination of H2AX/γH2AX mediated by UBE2T, which promotes activation of checkpoint kinase 1 (CHK1) and provides sufficient time for radiation-induced DNA repair [51] (Fig. 1A). As p53 is a key tumour suppressor molecule, p53 mutation occurs in various types of malignancies [52]. Mutant(mut) p53 loses the inhibitory function of wild-type(wt) p53 and promotes the proliferation, invasion, metastasis, and metabolic reprogramming of tumour cells, which are closely associated with the development of most malignancies [53]. Radiotherapy-induced DNA damage activates the p53 signalling pathway, and p53 mutations also have an impact on the biological effects of ionizing radiation, which are often associated with radiation resistance [54–56]. This mechanism was first identified in head and neck squamous cell carcinoma cell lines and subsequently confirmed in bladder tumours [57, 58]. One study compared the radiosensitivity of three HCC cell lines: MHCC97L mutp53 cells, Hep3B p53 null cells, and HepG2 wtp53 cells. The results showed that the radiosensitivity of MHCC97L cells was much lower than that of the other two cell lines, indicating that deletion or mutation of the p53 protein is closely related to the radioresistance of HCC cells [59]. Chaperone-mediated autophagy (CMA) is a type of autophagy, and previous studies have shown that CMA can reduce the level of accumulated mutant p53 protein [60]. Researchers have found that radiation-induced activation of CMA can degrade the high-mobility group box 1 (HMGB1) protein and downregulate p53, thereby conferring radiation resistance to HCC cells [61]. The phosphatidylinositol-3 kinase (PI3K)/protein kinase B (PKB, AKT)/mammalian target of rapamycin (mTOR) signalling pathway is involved in the regulation of a variety of cellular activities, such as proliferation, metabolism, apoptosis, and autophagy, and aberrant activation of this pathway occurs in approximately 50% of HCC patients [62]. One study explored the effect of phosphoinositide-dependent protein kinase-1 (PDK1) on radiosensitisation in HCC. The results showed that PDK1 could activate the PI3K/AKT/mTOR signalling pathway, thereby inhibiting DNA damage repair and making HCC radiation therapy ineffective [62]. In contrast, PKI-587, a dual PI3K/mTOR inhibitor, was able to increase the sensitivity to radiotherapy [63] (Fig. 1B).
Fig. 1.
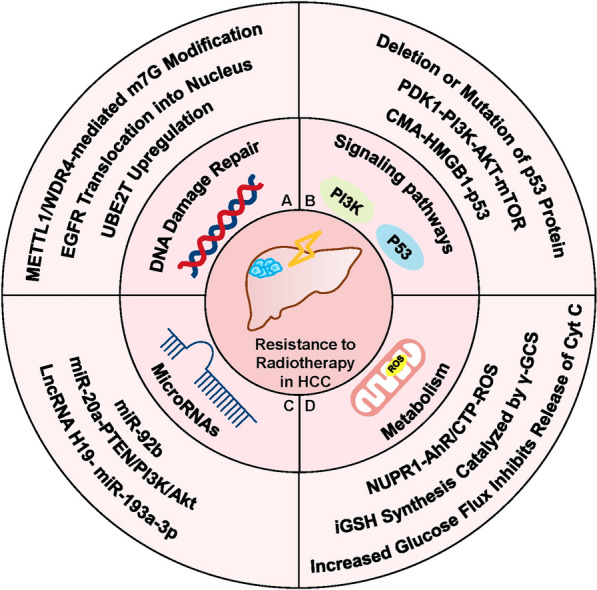
Molecular mechanisms of resistance to radiotherapy in HCC. A DNA damage repair is an important contributor to radiation resistance. Both METTL1/WDR4-mediated modification of m7G tRNA and EGFR mutations enhance the efficiency of DNA double-strand break (DSB) repair in the nonhomologous end-joining (NHEJ) pathway by augmenting the activity of the catalytic subunits of DNA-dependent protein kinases (DNA-PKcs). Upregulation of the ubiquitin-conjugating enzyme E2T (UBE2T) in HCC cells plays a similar role. B Changes in multiple signalling pathways in HCC cells affect their sensitivity to radiation. Deletion and mutation of p53 both decrease the radiosensitivity of HCC, and chaperone-mediated autophagy (CMA) impairs the efficacy of radiotherapy by downregulating p53. The effect of phosphoinositide-dependent protein kinase-1 (PDK1) on HCC radiosensitivity is mediated by activation of the PI3K/AKT/mTOR signalling pathway, which inhibits DNA damage repair. C MicroRNAs (miRNAs) are involved in the regulation of radiosensitivity in HCC by affecting cell proliferation and cell cycle. MiR-92b, mir-20a and miR-193a-3p confer radiation resistance to HCC cells in different ways. D The role of metabolism in radiosensitivity cannot be ignored. Glucose addiction in HCC cells promotes phospholipid synthesis, which inhibits cytochrome c release and reduces radiation-induced apoptosis. γ-Glutamylcysteine synthetase (γ-GCS) and nuclear protein 1 (NUPR1) inhibit cellular oxidative stress by producing GSH and modulating the AhR/CTP signalling axis, respectively, thereby enhancing cell viability after radiotherapy
MicroRNAs (miRNAs) are endogenous noncoding RNAs that play a regulatory role by inhibiting the translation of target messenger RNAs (mRNAs), and their mutation or misexpression is closely associated with a wide range of malignancies [64]. miRNA dysregulation plays an important role in the development of HCC and is involved in the regulation of radiosensitivity in HCC [65]. This regulatory role involves various mechanisms such as DNA damage repair, cell cycle regulation, and apoptosis [66]. Some miRNAs positively regulate the radiosensitivity of HCC cells. MiR-146a-5p could restrict proliferation and promote apoptosis to improve radiosensitivity by activating DNA damage repair pathways and repressing replication protein A3 (RPA3) expression [67]. The formation of γ-H2AX upon phosphorylation of histone 2AX (H2AX) is an important indicator of DSBs [68]. Overexpression of RAD21, an important protein for DNA damage repair and homologous recombination, reduces γ-H2AX levels and decreases the efficiency of radiotherapy. MiR-320b was able to inhibit RAD21 expression by targeting the RAD21 3'-UTR, thereby increasing the radiosensitivity of HCC [69]. The expression of miR-621 is significantly reduced in HCC tissues compared to normal tissues, and the SET domain bifurcated 1 (SETDB1) gene is a direct target gene of miR-621. It was found that miR-621 could inhibit the expression of SETDB1 by targeting its 3' UTR, and the miR-621/SETDB1 signalling axis further activated the p53 signaling pathway to enhance the radiosensitivity of HCC [70]. However, many miRNAs inhibit the efficacy of radiotherapy for HCC. A study exploring the effects of miR-193a-3p on HCC cell lines found that miR-193a-3p could enhance cellular resistance to radiation by promoting DNA double-strand break repair, and the long-stranded noncoding RNA (lncRNA) H19/miR-193a-3p signaling pathway is a promising therapeutic target in HCC radiotherapy [71]. MiR-92b has also been found to affect the response of HCC to radiotherapy. MiR-92b is overexpressed in both HCC tissues and cell lines, and is associated with poor patient prognosis. Overexpression of miR-92b promotes tumour cell proliferation, inhibits apoptosis, and ameliorates radiation-induced cell cycle arrest, thereby reducing the sensitivity of HCC cells to radiation [72]. Additionally, both in vivo and in vitro experiments also demonstrated that mir-20a overexpression in HCC could activate the PTEN/PI3K/Akt signalling pathway, which conferred greater radiation resistance to tumour cells [73] (Fig. 1C). Metabolism is closely associated with the sensitivity of HCC to radiation. Researchers screened these cell lines with radiation resistance and found that HCC cells with radiation resistance showed increased dependence on glucose after studying proteomics, metabolomics, and metabolic flux. Increased glucose flux promotes the synthesis of glucose into phospholipids, the accumulation of which inhibits the release of cytochrome c, reducing radiation-induced cell apoptosis. Glucose addiction in HCC cells is dependent on HIF-1α, and mTORC1 mediates the radiation resistance of HCC by enhancing the translation of HIF-1α and SREBP1 [74]. Moreover, γ-glutamylcysteine synthetase (γ-GCS) has been identified as a possible target to overcome radioresistance in HCC. Researchers have found that γ-GCS is the rate-limiting enzyme that regulates GSH biosynthesis and that γ-GCS can enhance HCC radiosensitivity by catalysing endogenous GSH synthesis [75]. Nuclear protein 1 (NUPR1) also plays a key role in regulating oxidation‒reduction reactions in vivo and is able to inhibit reactive oxygen species (ROS) production and oxidative stress through the AhR/CTP signalling axis, thereby increasing cell viability during radiotherapy [76] (Fig. 1D).
Therefore, considering the radioresistant status of HCC with multiple complex mechanisms, combining radiotherapy with other treatment modalities to enhance the body's antitumour immune response seems to be a more effective approach.
Effects of radiotherapy on immunity in HCC
The tumour microenvironment (TME) consists of noncancerous host cells and other noncellular components present in the tumour, and the continuous interaction between tumour cells and the TME plays a critical role in tumour initiation, progression, metastasis, and response to treatment [77]. In 2006, Dr. Robert Schreiber proposed the concept of "immune editing," which describes how tumour cells evade immune responses and even "reprogram" certain immune cells to promote tumour growth [78]. This process of immune editing occurs almost every time a tumour is present, resulting in a highly suppressed TME [79]. One mechanism of immune escape is achieved by tumour cells inducing and recruiting immune suppressive cells and increasing the expression of various immune inhibitory molecules [80]. The liver is an important immune organ enriched with a large number of innate immune cells, including natural killer cells (NK cells), natural killer T cells (NKT cells), and T cell receptor γδ (TCR γδ) T cells, of which NK cells in the liver can also be referred to as pit cells [81]. Studies have shown that pit cells in the liver have higher cytotoxicity against tumour cells than NK cells in the spleen and peripheral blood. This may be due to the upregulation of tumour necrosis factor-related apoptosis-inducing ligand (TRAIL) expression in pit cells [82]. In addition to an abundance of lymphocytes, the liver contains a large number of liver-specific immunoreactive cells, such as Kupffer cells, liver sinusoidal endothelial cells (LSECs), and hepatic stellate cells (HSCs) [83]. Both LSECs and HSCs can perform antigen-presenting functions in the liver. In contrast, LSECs can promote immune tolerance by secreting IL-10 and a variety of adhesion molecules to retain activated T cells in the hepatic sinusoids, including intercellular adhesion molecule-1 (ICAM-1), vascular cell adhesion molecule-1 (VCAM-1), and vascular adhesion protein-1 (VAP-1) [84]. While presenting antigens, HSCs can also inhibit T-cell activation by expressing PD-L1 [85]. Thus, the unique immune microenvironmental characteristics of the liver promote the occurrence of HCC and immune tolerance.
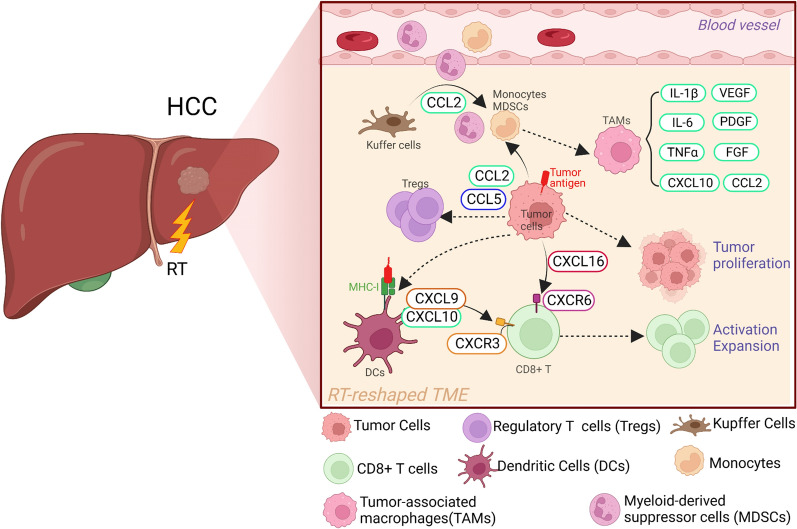
Research has revealed that major immunosuppressive cells associated with HCC immune escape include tissue-resident macrophages (mainly Kupffer cells), monocyte-derived macrophages, regulatory T cells (Tregs), and myeloid-derived suppressor cells (MDSCs) [86]. Kupffer cells are the most abundant population of tissue-resident macrophages in the liver and play a key role in immune suppression in the liver. Previous in vivo studies have shown that sustained and dysregulated chronic inflammation in the liver is carcinogenic, and Kupffer cells can drive tumour progression and metastasis in HCC, a process that is associated with their response to and activation of inflammatory signalling pathways. In the context of persistent chronic inflammation, activated Kupffer cells release C–C motif chemokine 2(CCL2) while recruiting monocytes and MDSCs from blood vessels and promoting HCC progression [87, 88]. The presence of tumour-associated macrophages (TAMs) is associated with a poor prognosis in HCC, particularly when TAMs are skewed towards the M2 polarization phenotype [89]. TAMs in HCC can secrete various cytokines and chemokines, such as IL-1β, IL-6, TNF, CCL2, and CXCL10, promoting tumour cell proliferation and NF-κB-mediated protection against cancer cell apoptosis, which is associated with a poor prognosis in HCC patients. TAMs can also produce vascular endothelial growth factor (VEGF), platelet-derived growth factor (PDGF), fibroblast growth factor (FGF), and other factors to support tumour tissue proliferation and growth [90, 91]. Treg cells, are an important subset of immunosuppressive cells, and their ratio to CD8 + T cells is an important prognostic indicator for cancer patients [92]. Compared with nontumour areas, the TME of HCC has significantly more CD4 + CD25 + FoxP3 + Treg cells and significantly fewer CD8 + T cells; and CCL2 and CCL5 produced by tumour cells play an important role in regulating this phenotype At this high level, Treg cells can impair the effector function of CD8 + T cells, significantly reducing the expression of granzyme A, granzyme B, and perforin in infiltrating CD8 + T cells, and promoting disease progression in HCC patients [93, 94]. Increasing evidence suggests that MDSCs also play an important role in the development of HCC, CCL2 and CCL5 from tumour cells and facilitate infiltration of MDSCs into the TME [95]. The level of MDSCs in the circulation of HCC patients is increased, and this high level is also associated with tumour progression and a poor prognosis in patients [96].
Radiotherapy, as one of the main modalities for the first-line treatment of multiple solid tumours, has a direct and significant impact on the tumour stroma, blood vessels, and immune cells [97]. Radiotherapy can upregulate major histocompatibility complex I (MHC-I) molecules on the surface of tumour cells, promote the maturation of dendritic cells (DCs) and presentation of tumour-associated antigens, and enhance the secretion of cytokines required for T-cell infiltration, such as chemokine (C–X–C motif) ligand 9 (CXCL9), CXCL10, and CXCL16, from DCs and tumour cells, which are beneficial for the cytotoxic activity and expansion of CD8 + T cells [98] (Fig. 2). Grassberger et al. conducted a prospective study on the levels of circulating lymphocytes in HCC patients receiving HPT. The results showed that the increase in CD8+ CD25+ T-cell levels during radiotherapy was associated with prolonged OS in HCC patients [99]. Studies have revealed that the levels of MDSCs in the body of HCC patients significantly decreased after radiotherapy, and this decrease was negatively correlated with overall survival time. In multivariate analysis, only posttreatment MDSC levels and Child‒Pugh classification were correlated with the prognosis of HCC patients, indicating that MDSC suppression achieved after radiotherapy may improve the prognosis of HCC patients [100]. Another study showed that high-dose fractionated radiation therapy of the primary site of transplanted tumours in a mouse HCC model could exert a potent abscopal effect on other sites of the same tumour. This abscopal effect may be achieved by reducing the levels of MDSCs in the body after radiotherapy [101]. Therefore, radiotherapy can have many positive effects on the immune microenvironment, reshaping the tumour microenvironment in multiple ways while killing tumour cells, providing strong support for the development of studies on radiation-immunotherapy strategies.
Fig. 2.
Changes in the TME of HCC before and after radiotherapy. TME of HCC before radiotherapy. (1) In the context of persistent chronic inflammation, activated Kupffer cells (KCs) release CCL2 while recruiting inflammatory monocytes and MDSCs and promoting HCC progression. (2) Tumour cell production of CCL5 and CCL2 promotes the infiltration of MDSCs and Tregs, which in turn inhibits the production of CD8+ T cells and immunosuppressive transforming growth factor β (TGF-β). (3) M2-like TAMs secrete interleukin 1β(IL-1β), IL-6, TNF, CCL2, and CXCL10, which promote the proliferation of tumour cells and are associated with poor patient prognosis. Radiotherapy reshapes the TME of HCC. (1) Radiotherapy induces the upregulated expression of MHC-I on the surface of tumour cells, which promotes the maturation of DCs and the presentation of tumour-associated antigens. Mature DCs release CXCL9 and CXCL10 to promote the infiltration of CD8+ T-cells in the TME. (2) Radiotherapy induces tumour cells to secrete CXCL16, which further promotes the activation and expansion of CD8+ T-cells
The current status of combined application of radiotherapy and immunotherapy in HCC
However, radiotherapy still has certain limitations in the management of advanced HCC. Local tumour control achieved by radiotherapy does not necessarily translate into long-term survival for patients, as it cannot address the risk of liver dysfunction and metastasis or progression in other organs. Therefore, the combination of local treatment and systemic treatment for HCC may provide more survival benefits for patients. With increasing evidence of the safety and efficacy of immune therapies, such as anti-PD-1/PD-L1 and anti-CTLA-4 antibodies, in the treatment of various malignant tumours, research on the combination of immunotherapy with surgery, radiotherapy, chemotherapy, targeted therapy, and other treatment modalities in HCC is ongoing. To date, the US FDA has approved the anti-PD-1 antibody pembrolizumab as monotherapy, as well as the combination of the anti-PD-1 antibody nivolumab and the anti-CTLA-4 antibody ipilimumab for the treatment of advanced HCC patients who have previously received sorafenib (as a second-line or later-line immunotherapy) [102, 103]. Moreover, in 2020, the FDA approved the combination of the anti-PD-L1 antibody atezolizumab and the VEGF antagonist bevacizumab for the treatment of unresectable or metastatic HCC patients who have not received prior systemic therapy. Compared with sorafenib, a conventional drug for treating HCC, the combination of atezolizumab and bevacizumab significantly improved patient OS and progression-free survival (PFS) [104]. Although immunotherapy has been successfully applied as a first-line treatment for HCC, the response rate and clinical benefits of treatment are still limited due to various mechanisms of intrinsic or acquired resistance. Therefore, the combination of immunotherapy with other therapies urgently needs further research in the treatment of HCC patients [105]. Previous studies have shown that anti-CTLA-4 therapy reduces the levels of Treg cells, and anti-PD-L1 antibody reverses T-cell exhaustion, thus increasing the ratio of CD8+ T cells to Treg cells [94]. Radiotherapy amplifies the diversity of the TCR repertoire of T cells within tumours and upregulates various immune checkpoints on tumour cells. This upregulation can be overcome by immune checkpoint inhibitors; thus, the combination of radiotherapy and immunotherapy holds promise for achieving better treatment outcomes in malignant tumours [106]. Based on such promising observations, an increasing number of combinations of radiotherapy with different immunotherapies have been studied in HCC, and many have entered phase III clinical trials (Fig. 3).
Fig. 3.
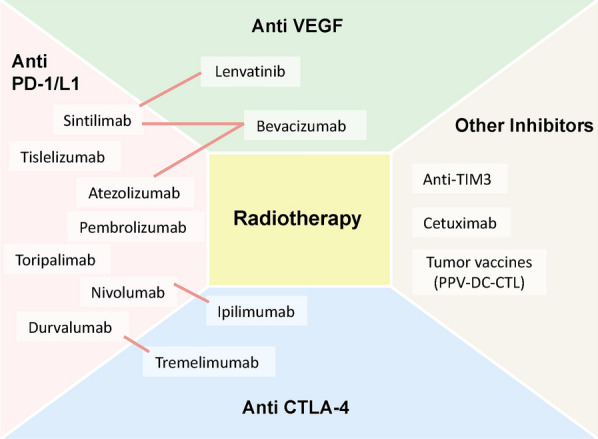
Combination treatments of radiotherapy and immunotherapy for HCC under investigation. Combination strategies reported or in ongoing investigations are presented, and lines demonstrate combinations of multiple immunotherapies. PD-1/L1 programmed cell death 1/ ligand 1; CTLA-4 cytotoxic T lymphocyte-associated antigen 4; TIM3 T-cell immunoglobulin and mucin-domain containing molecule 3; VEGF vascular endothelial growth factor
A small retrospective study analysed five unresectable HCC patients who received combined treatment with SBRT and anti-PD-1 therapy. During a median follow-up period of 14.9 months, no patients experienced tumour progression, and both local control and overall survival rates were 100% at one year, demonstrating the potential value of combined treatment [107]. The immune checkpoint T-cell immunoglobulin and mucin-domain containing molecule 3 (TIM3) was upregulated in tumour-infiltrating CD8+ and CD4+ T cells [108]. The researchers compared the effects of anti-TIM3 alone or in combination with radiation therapy in a mouse HCC model, and the results showed that the combination therapy significantly slowed tumour progression and prolonged median survival compared to monotherapy. The enhanced antitumour effect of combination therapy was associated with increased tumour cell apoptosis, decreased proliferation, and reactivation of CD8+ T cells [109]. A phase I trial investigated the combination of the CTLA-4 inhibitor ipilimumab with stereotactic ablative radiotherapy (SABR) in liver cancer patients, either concurrently or sequentially with radiotherapy. The results showed significant T-cell activation in the liver after combination treatment, characterized by an increased proportion of T cells expressing ICOS, GITR, and 4-1BB [110]. A phase I study evaluated the safety of combining pembrolizumab with multisite SBRT in patients with metastatic solid tumours, and the overall objective response rate was 13.2%, with a median overall survival of 9.6 months and a median progression-free survival of 3.1 months. This suggests that pembrolizumab given after multi-site SBRT is well-tolerated and has an acceptable toxicity profile in patients with metastatic solid tumours [111].
Previous studies have found that radiotherapy induces p53-independent transcriptional upregulation of VEGF in the serum of HCC patients, increasing VEGF secretion in a dose-, time-, and cell type-dependent manner, promoting intrahepatic and extrahepatic tumour progression outside the radiotherapy area, and offsetting the benefits of radiotherapy on overall survival [112]. Dual blockade of angiogenesis and immune checkpoints has been used in the first-line treatment of HCC, so the combination of this approach with radiotherapy has the potential to provide more clinical benefits for patients [113]. On the one hand, radiotherapy can reprogram the immunologically poor "cold" TME into a more immunologically active "hot" TME [114]. On the other hand, antiangiogenic agents can promote the transport of immune effector cells to the tumour site and partially limit hypoxia through vascular normalization, driving DC maturation, reducing MDSC and Treg levels, and transiently increasing perfusion, thereby increasing the radiosensitivity of tumour cells and improving the efficiency of radiotherapy [115]. Studies have shown that sorafenib can selectively inhibit radiation-induced upregulation of VEGFR-2, induce DNA damage, and decrease DNA repair capacity, thereby enhancing the radiosensitivity of HCC [116]. Immune checkpoint inhibitors can also enhance the efficacy of antiangiogenic therapy by recruiting immune cell subtypes with vascular regulatory functions, providing a strong rationale for the development of this combination therapy [117].
The repair of DNA damage in tumour cells partially offset the therapeutic effect of radiotherapy, and combination therapy with radiotherapy, anti-PD-L1, and DNA repair inhibitors has been studied in HCC. Researchers found that the DNA repair inhibitor AZD6738 significantly increased CD8 + T-cell infiltration and activation induced by radiotherapy, resulting in a significant improvement in the tumour immune microenvironment. The antitumour efficacy and survival rate improvement of this triple combination therapy is due to the more effective activation of the cGAS/STING signalling pathway by AZD6738, which is conducive to the synergistic effect between radiotherapy and anti-PD-L1, and this triple combination therapy can generate stronger immune memory and persistent antitumour immunity, thereby preventing tumour recurrence [118]. In addition to immune checkpoints, research has also explored the use of tumour vaccines in HCC patients. A phase I study of cell-based immunotherapy using personalized peptide vaccine (PPV-DC-CTL) combined with radiotherapy for unresectable advanced HCC patients showed a remission rate of 33% and a disease control rate of 66% after radiotherapy and one to three cycles of vaccine treatment. Most patients did not experience significant haematological side effects, and no patients had liver or kidney side effects, indicating that this combination treatment regimen can provide a new, well-tolerated, safe, and effective treatment strategy for advanced HCC patients [119]. Previous studies have demonstrated that EGFR activation subsequently increases cellular radiation resistance by promoting DNA damage repair [49]. Cetuximab is an agent targeting EGFR and is currently approved for use in head and neck squamous cell carcinoma (HNSCC) and metastatic colorectal cancer; its combination with radiotherapy continues to be studied [120, 121]. A phase III trial demonstrated that radiotherapy combined with cetuximab improved overall survival in patients with locoregionally advanced squamous cell carcinoma of the head and neck (LASCCHN) at 5 years compared to that with radiotherapy alone [122]. This combination may also play an essential role in remodelling the TME. It has been shown that the combination of radiotherapy and cetuximab can increase the infiltration of NK cells and CD8 + T cells in the TME and that the combination can activate the innate antitumour immune response, which improves the outcome of HNSCC [123]. Experiments in vivo also demonstrated the promise of cetuximab alone or in combination for the treatment of HCC [124]. Thus, cetuximab in combination with radiotherapy and immunotherapy holds promise for future breakthroughs in the treatment of HCC.
Although several clinical trials involving different types of radiotherapy and tumour stages have been conducted to investigate the efficacy of various immune therapies and radiotherapy in patients with HCC, there is still a lack of prospective clinical data on the combination of these therapies. Biomarkers that can predict patient suitability and treatment outcomes still urgently need to be identified. Studies have analysed the clinical significance of soluble PD-L1 (sPD-L1) levels in HCC patients after radiotherapy. sPD-L1 levels are significantly correlated with advanced features such as tumour stage, size, and portal vein tumour thrombosis (PVTT) and are an important adverse prognostic factor for OS. Patients with higher initial sPD-L1 levels have significantly worse overall survival, and higher sPD-L1 levels one month after radiotherapy are associated with early lung metastasis. It is evident that the combination of radiotherapy and anti-PD-L1 therapy could be a promising treatment strategy for HCC, and sPD-L1 levels may serve as a potential biomarker to predict treatment efficacy [125]. In addition, researchers have developed a model to predict the response of immune checkpoint inhibitors (ICIs) combined with radiotherapy and applied this model to study combined treatment regimens for HCC patients, based on ongoing clinical trials of radioimmunotherapy. The results showed that the constructed model successfully predicted the tumour growth patterns observed in early clinical trials of monotherapy with durvalumab (anti-PD-L1 antibody) in HCC patients. Adding radiotherapy to unirradiated tumour sites on the basis of monotherapy increased the clinical benefit from 33 to 71% for 90% of irradiated tumour cells. The results of this model are consistent with clinical data, indicating that machine learning prediction models have the potential to play a valuable role in evaluating the effectiveness and applicability of radioimmunotherapy [126].
Conclusion and perspective
The management of HCC has continually improved, particularly in the development of systemic therapies. Standard local treatments are no longer sufficient to meet clinical needs, and combination with systemic therapies is the future trend. Although radiation therapy has not yet become the standard for HCC, its excellent performance in terms of local control, overall survival, and bridging therapy as an alternative to traditional therapies has been proven. Moreover, the positive impact of radiation therapy on the immune landscape cannot be ignored. The unique immune landscape of HCC makes immunotherapy a promising treatment option for patients, and the continuous innovation of radiation therapy techniques has improved their safety and efficacy in the treatment of HCC. The combination of the two strategies could further benefit patients. However, there are currently limited studies on the combination of radiation therapy and immunotherapy in HCC, and robust prospective data are particularly lacking, which still leaves significant research gaps in this field [127]. More phase III clinical trials are needed to provide more robust evidence of efficiency and safety (Table 1). Further research is needed to clarify many key factors, such as (a) the optimal treatment sequence in combination therapy; (b) the best immunotherapy drug and the best method for degerming this; (c) strategies for determining the optimal radiation therapy dose; (d) biomarkers that can predict treatment outcomes; and (e) strategies for overcoming potential drug resistance. There are many more issues that need to be addressed, and the combination of radiation therapy and immunotherapy has shown great potential due to their synergistic effects. Therefore, conducting more research to answer these questions and promote the development of radiation-immunotherapy is of great significance.
Table 1.
Clinical trials of radiotherapy combined with immunotherapy
| Clinical trial identification(study name) | Phase | Disease | Type of radiotherapy | Type of immunotherapy | Treatment design | Estimated enrollment | Primary outcome measures |
|---|---|---|---|---|---|---|---|
| NCT04913480 | II | HCC | SBRT | Durvalumab (anti-PD-L1) | SBRT → durvalumab | 37 | Progression-free survival (PFS) |
| NCT05225116 | I | HCC | Radiotherapy | Sintilimab (anti-PD-1) | (Sintilimab + lenvatinib) → radiotherapy | 20 | Safety (number of participants with adverse events) |
| NCT05185531 | I | HCC | SBRT | Tislelizumab (anti-PD-1) | Neoadjuvant tislelizumab + SBRT | 20 | ORR, pCR (pathological complete response), pPR (pathological partial response), MPR (major pathologic response) |
| NCT04169399 | II | HCC | SBRT | Toripalimab (anti-PD-1) | Toripalimab + sBRT | 30 | PFS |
| NCT04709380 | III | Advanced HCC | Radiotherapy | Toripalimab (anti-PD-1) | (Radiotherapy + toripalimab) vs sorafenib | 85 | Time to progression (TTP) |
| NCT03482102 | II | HCC | Radiation | Durvalumab (anti-PD-L1) and Tremelimumab (anti-CTLA-4) | Tremelimumab + durvalumab + radiation | 70 | Overall response rate (ORR) |
| NCT03316872 | II | HCC | SBRT | Pembrolizumab (anti-PD-1) | Pembrolizumab + SBRT | 30 | Overall response rate (ORR) |
| NCT05530785 | II | Non-resectable HCC | Radiotherapy | Sintilimab (anti-PD-1) | radiotherapy + (sintilimab and bevacizumab biosimilar) | 35 | Overall response rate (ORR) |
| NCT04104074 | I | HCC | Radiotherapy | Sintilimab (anti-PD-1) | Radiotherapy + sintilimab | 20 | Safety (number of participants with adverse events) |
| NCT03857815 | II | HCC | SBRT | Sintilimab (anti-PD-1) | SBRT + sintilimab | 30 | PFS |
| NCT04857684 | I | HCC | SBRT | Atezolizumab (anti-PD-L1) | SBRT + atezolizumab + bevacizumab | 20 | Safety (number of participants with adverse events) |
| NCT03203304 | I | HCC | SBRT | Nivolumab (anti-PD-1) and Ipilimumab (anti-CTLA-4) | SBRT + nivolumab OR SBRT + nivolumab + ipilimumab | 14 | Safety (number of participants with adverse events) |
| NCT05096715 | I | Non-resectable HCC | SBRT | Atezolizumab (anti-PD-L1) | SBRT + atezolizumab + bevacizumab | 20 | Dose limiting toxicity rate |
| NCT04611165 | II | Advanced HCC | EBRT (External beam radiotherapy) | Nivolumab (anti-PD-1) | Nivolumab → EBRT | 50 | PFS |
| NCT04850157 | II | HCC with portal vein tumor thrombus (PVTT) | Intensity modulated radiation therapy (IMRT) | Tislelizumab (anti-PD-1) | Tislelizumab + IMRT | 30 | Relapse-free survival ( RFS) |
| NCT04167293 | II | HCC | SBRT | Sintilimab (anti-PD-1) | SBRT or SBRT + sintilimab | 116 | PFS |
| NCT05010434 | II | Recurrent HCC | Radiotherapy | Sintilimab (anti-PD-1) | Radiotherapy + sintilimab + bevacizumab | 46 | Overall response rate (ORR) |
| NCT05366829 | II | HCC | Radiotherapy | Toripalimab (anti-PD-1) | Radiotherapy + tislelizumab | 35 | Safety (number of participants with adverse events) |
| NCT04430452 | II | Advanced HCC | Hypofractionated radiotherapy (HPT) | Durvalumab (anti-PD-L1) and Tremelimumab (anti-CTLA-4) | HPT + durvalumab ± tremelimumab | 30 | Overall response rate (ORR) |
| NCT03380130 | II | HCC | Selective internal radiation therapy (SIRT) using Y-90-loaded microspheres | Nivolumab (anti-PD-1) | SIRT + nivolumab | 41 | Incidence of adverse event |
| NCT05625893 | II | HCC | proton beam therapy (PBT) | Atezolizumab (anti-PD-L1) | PBT → (atezolizumab + bevacizumab) | 63 | Incidence of adverse event, PFS |
| NCT04547452 | II | Stage IV HCC | SBRT | Sintilimab (anti-PD-1) | SBRT + sintilimab OR sintilimab | 84 | PFS |
| NCT05377034 | II | Locally Advanced HCC | SIRT | Atezolizumab (anti-PD-L1) | SIRT + atezolizumab + bevacizumab | 176 | Best overall response rate (BORR) |
| NCT05701488 | I | HCC | SIRT | Durvalumab (anti-PD-L1) and Tremelimumab (anti-CTLA-4) | Durvalumab + tremelimumab vs durvalumab + tremelimumab + SIRT | 20 | Safety (number of participants with adverse events) |
| NCT02837029 | I | Stage IIIA—IVB HCC | SIRT | Nivolumab (anti-PD-1) | SIRT + nivolumab | 27 | Maximum tolerated dose (MTD), overall response rate (ORR) |
| NCT04785287 | I/II | Metastatic liver carcinoma | SBRT | Nivolumab (anti-PD-1) and BMS986218 (anti-CTLA-4) | SBRT + BMS986218 ± nivolumab | 13 | Incidence of adverse event |
Acknowledgements
None.
Abbreviations
- HCC
Hepatocellular carcinoma
- PD-1
Programmed cell death protein 1
- PD-L1
Programmed cell death protein 1 ligand 1
- CTLA-4
Cytotoxic T-lymphocyte-associated protein 4
- VEGF
Vascular endothelial growth factor
- SBRT
Stereotactic body radiotherapy
- KCs
Kupffer cells
- CCA
Cholangiocarcinoma
- HBV
Hepatitis B virus
- HCV
Hepatitis C virus
- TACE
Transarterial chemoembolization
- RFA
Radiofrequency ablation
- OS
Overall survival
- HPT
High-dose hypofractionated proton beam therapy
- CHK1
Cell cycle checkpoint kinase 1
- HIF-1α
Hypoxia inducible factor 1α
- mTORC
Mammalian target of rapamycin complex
- SREBP
Sterol regulatory element-binding protein
- TAMs
Tumour-associated macrophages
- TME
Tumour microenvironment
- MDSCs
Myeloid-derived suppressor cells
- Tregs
Regulatory T cells
- TNF-α
Tumour necrosis factor-α
- IL-1β
Interleukin-1β
- CCL-2
Chemokine (C–C motif) ligand 2
- CXCL10
Chemokine (C–X–C motif) ligand 10
- FoxP3
Transcriptional factor P3
- NKs
Natural killer cells
- MHC-I
Major histocompatibility class I
- DCs
Dendritic cells
- TCR
T cell receptor
- ICOS
Inducible co-stimulator
- GITR
Glucocorticoid-induced TNF receptor (TNFR)-related protein
- DDR
DNA damage repair
- DSB
DNA double-strand breaks
- cGAS/STING
Cyclic GMP-AMP/stimulator of interferon genes
- NF-κB
Nuclear factor-κB
- HR
Homologous recombination
- NHEJ
Non-homologous end joining
- METTL1
Methyltransferase-like 1
- WDR4
WD repeat domain 4
- EGFR
Epidermal growth factor receptor
- RTK
Receptor tyrosine kinases
- UBE2T
Ubiquitin-conjugating enzyme E2T
- DNA-PKcs
DNA-dependent protein kinase catalytic subunits
- SETDB1
SET domain bifurcated 1
- CMA
Chaperone-mediated autophagy
- HMGB1
High-mobility group box 1
- PDK1
Phosphoinositide-dependent protein kinase-1
- NUPR1
Nuclear protein 1
- ROS
Reactive oxygen species
Author contributions
YY and LX wrote the manuscript. ML collected the materials. JW and PJ supervised the manuscript. CL designed and revised the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (82173174, 82073335), the Natural Science Foundation of Beijing Municipality (7232207), Intramural funding from the Beijing University Third Hospital (BYSY2022044), the Special Fund of the National Clinical Key Specialty Construction Program, P. R. China (2021).
Availability of data and materials
Not applicable.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yuhan Yang and Liting Xiong contributed equally to this work.
Contributor Information
Ping Jiang, Email: jiangping@bjmu.edu.cn.
Junjie Wang, Email: junjiewang_edu@sina.cn.
Chunxiao Li, Email: chunxiaoli@pku.edu.cn.
References
- 1.Sung H, et al. Global Cancer Statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660. [DOI] [PubMed] [Google Scholar]
- 2.Liu Y, Liu L. Changes in the Epidemiology of hepatocellular carcinoma in Asia. Cancers. 2022;14(18):4473. doi: 10.3390/cancers14184473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Devarbhavi H, et al. Global burden of liver disease: 2023 update. J Hepatol. 2023;79(2):516–537. doi: 10.1016/j.jhep.2023.03.017. [DOI] [PubMed] [Google Scholar]
- 4.European Association for the Study of the Liver, Electronic address, e.e.e. and L. European Association for the Study of the Liver EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2018;69(1):182–236. doi: 10.1016/j.jhep.2018.03.019. [DOI] [PubMed] [Google Scholar]
- 5.Yang JD, Heimbach JK. New advances in the diagnosis and management of hepatocellular carcinoma. BMJ. 2020;371:m3544. doi: 10.1136/bmj.m3544. [DOI] [PubMed] [Google Scholar]
- 6.Llovet JM, Kelley RK, Villanueva A, Singal AG, Pikarsky E, Roayaie S, Lencioni R, Koike K, Zucman-Rossi J, Finn RS. Hepatocellular carcinoma. Nat Rev Dis Primers. 2021;7(1):7. doi: 10.1038/s41572-020-00240-3. [DOI] [PubMed] [Google Scholar]
- 7.Wen N, et al. The clinical management of hepatocellular carcinoma worldwide: A concise review and comparison of current guidelines: 2022 update. Biosci Trends. 2022;16(1):20–30. doi: 10.5582/bst.2022.01061. [DOI] [PubMed] [Google Scholar]
- 8.Parikh ND, Pillai A. Recent advances in hepatocellular carcinoma treatment. Clin Gastroenterol Hepatol. 2021;19(10):2020–2024. doi: 10.1016/j.cgh.2021.05.045. [DOI] [PubMed] [Google Scholar]
- 9.Meyer J, Singal AG. Stereotactic ablative radiotherapy for hepatocellular carcinoma: history, current status, and opportunities. Liver Transpl. 2018;24(3):420–427. doi: 10.1002/lt.24991. [DOI] [PubMed] [Google Scholar]
- 10.Klein J, Dawson LA. Hepatocellular carcinoma radiation therapy: review of evidence and future opportunities. Int J Radiat Oncol Biol Phys. 2013;87(1):22–32. doi: 10.1016/j.ijrobp.2012.08.043. [DOI] [PubMed] [Google Scholar]
- 11.Rim CH, Kim HJ, Seong J. Clinical feasibility and efficacy of stereotactic body radiotherapy for hepatocellular carcinoma: a systematic review and meta-analysis of observational studies. Radiother Oncol. 2019;131:135–144. doi: 10.1016/j.radonc.2018.12.005. [DOI] [PubMed] [Google Scholar]
- 12.Choi SH, Seong J. Strategic application of radiotherapy for hepatocellular carcinoma. Clin Mol Hepatol. 2018;24(2):114–134. doi: 10.3350/cmh.2017.0073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ohri N, et al. Radiotherapy for hepatocellular carcinoma: new indications and directions for future study. J Natl Cancer Inst. 2016;108(9):djw133. doi: 10.1093/jnci/djw133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Giraud J, et al. Hepatocellular carcinoma immune landscape and the potential of immunotherapies. Front Immunol. 2021;12:655697. doi: 10.3389/fimmu.2021.655697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jarosz-Biej M, et al. Tumor microenvironment as a "game Changer" in Cancer Radiotherapy. Int J Mol Sci. 2019;20(13):3212. doi: 10.3390/ijms20133212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zheng R, et al. Cancer incidence and mortality in China. J Nat Cancer Center. 2016;2(1):1–9. doi: 10.1016/j.jncc.2022.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forner A, Reig M, Bruix J. Hepatocellular carcinoma. Lancet. 2018;391(10127):1301–1314. doi: 10.1016/S0140-6736(18)30010-2. [DOI] [PubMed] [Google Scholar]
- 18.European Association For The study of the liver European Organisation For Research And Treatment Of Cancer EASL-EORTC clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol. 2012;56(4):908–43. doi: 10.1016/j.jhep.2011.12.001. [DOI] [PubMed] [Google Scholar]
- 19.Peng ZW, et al. Radiofrequency ablation with or without transcatheter arterial chemoembolization in the treatment of hepatocellular carcinoma: a prospective randomized trial. J Clin Oncol. 2013;31(4):426–432. doi: 10.1200/JCO.2012.42.9936. [DOI] [PubMed] [Google Scholar]
- 20.Llovet JM, et al. Molecular therapies and precision medicine for hepatocellular carcinoma. Nat Rev Clin Oncol. 2018;15(10):599–616. doi: 10.1038/s41571-018-0073-4. [DOI] [PubMed] [Google Scholar]
- 21.Llovet JM, et al. Locoregional therapies in the era of molecular and immune treatments for hepatocellular carcinoma. Nat Rev Gastroenterol Hepatol. 2021;18(5):293–313. doi: 10.1038/s41575-020-00395-0. [DOI] [PubMed] [Google Scholar]
- 22.Bang A, Dawson LA. Radiotherapy for HCC: Ready for prime time? JHEP Rep. 2019;1(2):131–137. doi: 10.1016/j.jhepr.2019.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mathew AS, et al. Long term outcomes of stereotactic body radiation therapy for hepatocellular carcinoma without macrovascular invasion. Eur J Cancer. 2020;134:41–51. doi: 10.1016/j.ejca.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Shi C, et al. Adjuvant stereotactic body radiotherapy after marginal resection for hepatocellular carcinoma with microvascular invasion: a randomised controlled trial. Eur J Cancer. 2022;166:176–184. doi: 10.1016/j.ejca.2022.02.012. [DOI] [PubMed] [Google Scholar]
- 25.Shen PC, et al. Comparison of stereotactic body radiation therapy and transarterial chemoembolization for unresectable medium-sized hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2019;105(2):307–318. doi: 10.1016/j.ijrobp.2019.05.066. [DOI] [PubMed] [Google Scholar]
- 26.Sapir E, et al. stereotactic body radiation therapy as an alternative to transarterial chemoembolization for hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2018;100(1):122–130. doi: 10.1016/j.ijrobp.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim N, et al. Stereotactic body radiation therapy vs. Radiofrequency ablation in Asian patients with hepatocellular carcinoma. J Hepatol. 2020;73(1):121–129. doi: 10.1016/j.jhep.2020.03.005. [DOI] [PubMed] [Google Scholar]
- 28.Sapisochin G, et al. Stereotactic body radiotherapy vs. TACE or RFA as a bridge to transplant in patients with hepatocellular carcinoma. An intention-to-treat analysis. J Hepatol. 2017;67(1):92–99. doi: 10.1016/j.jhep.2017.02.022. [DOI] [PubMed] [Google Scholar]
- 29.Bruix J, et al. Prognostic factors and predictors of sorafenib benefit in patients with hepatocellular carcinoma: analysis of two phase III studies. J Hepatol. 2017;67(5):999–1008. doi: 10.1016/j.jhep.2017.06.026. [DOI] [PubMed] [Google Scholar]
- 30.Yoon SM, et al. Efficacy and safety of transarterial chemoembolization plus external beam radiotherapy vs sorafenib in hepatocellular carcinoma with macroscopic vascular invasion: a randomized clinical trial. JAMA Oncol. 2018;4(5):661–669. doi: 10.1001/jamaoncol.2017.5847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hong TS, et al. Multi-institutional phase ii study of high-dose hypofractionated proton beam therapy in patients with localized, unresectable hepatocellular carcinoma and intrahepatic cholangiocarcinoma. J Clin Oncol. 2016;34(5):460–468. doi: 10.1200/JCO.2015.64.2710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Jeggo PA, Pearl LH, Carr AM. DNA repair, genome stability and cancer: a historical perspective. Nat Rev Cancer. 2016;16(1):35–42. doi: 10.1038/nrc.2015.4. [DOI] [PubMed] [Google Scholar]
- 33.Krisnawan VE, et al. Tumor microenvironment as a regulator of radiation therapy: new insights into stromal-mediated radioresistance. Cancers (Basel). 2020;12(10):2916. doi: 10.3390/cancers12102916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lord CJ, Ashworth A. The DNA damage response and cancer therapy. Nature. 2012;481(7381):287–294. doi: 10.1038/nature10760. [DOI] [PubMed] [Google Scholar]
- 35.Yeoh KW, et al. Vinorelbine Augments Radiotherapy in Hepatocellular Carcinoma. Cancers (Basel) 2020;12(4):872. doi: 10.3390/cancers12040872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Gong L, et al. Application of radiosensitizers in cancer radiotherapy. Int J Nanomedicine. 2021;16:1083–1102. doi: 10.2147/IJN.S290438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Santivasi WL, Xia F. Ionizing radiation-induced DNA damage, response, and repair. Antioxid Redox Signal. 2014;21(2):251–259. doi: 10.1089/ars.2013.5668. [DOI] [PubMed] [Google Scholar]
- 38.Toulany M. Targeting DNA Double-Strand Break Repair Pathways to Improve Radiotherapy Response. Genes. 2019;10(1):25. doi: 10.3390/genes10010025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cheng W, et al. Novel roles of METTL1/WDR4 in tumor via m(7)G methylation. Mol Ther Oncolytics. 2022;26:27–34. doi: 10.1016/j.omto.2022.05.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen Z, et al. METTL1 promotes hepatocarcinogenesis via m(7) G tRNA modification-dependent translation control. Clin Transl Med. 2021;11(12):e661. doi: 10.1002/ctm2.661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Liao J, et al. Methyltransferase 1 is required for nonhomologous end-joining repair and renders hepatocellular carcinoma resistant to radiotherapy. Hepatology. 2022;77(6):1896–1910. doi: 10.1002/hep.32615. [DOI] [PubMed] [Google Scholar]
- 42.Yarden Y, Sliwkowski MX. Untangling the ErbB signalling network. Nat Rev Mol Cell Biol. 2001;2(2):127–137. doi: 10.1038/35052073. [DOI] [PubMed] [Google Scholar]
- 43.Loeffler-Ragg J, et al. EGFR inhibition as a therapy for head and neck squamous cell carcinoma. Expert Opin Investig Drugs. 2008;17(10):1517–1531. doi: 10.1517/13543784.17.10.1517. [DOI] [PubMed] [Google Scholar]
- 44.Tomas A, Futter CE, Eden ER. EGF receptor trafficking: consequences for signaling and cancer. Trends Cell Biol. 2014;24(1):26–34. doi: 10.1016/j.tcb.2013.11.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Zahonero C, Sanchez-Gomez P. EGFR-dependent mechanisms in glioblastoma: towards a better therapeutic strategy. Cell Mol Life Sci. 2014;71(18):3465–3488. doi: 10.1007/s00018-014-1608-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chong CR, Janne PA. The quest to overcome resistance to EGFR-targeted therapies in cancer. Nat Med. 2013;19(11):1389–1400. doi: 10.1038/nm.3388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hu B, et al. Inhibition of EGFR overcomes acquired lenvatinib resistance driven by STAT3-ABCB1 signaling in hepatocellular carcinoma. Cancer Res. 2022;82(20):3845–3857. doi: 10.1158/0008-5472.CAN-21-4140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Jin H, et al. EGFR activation limits the response of liver cancer to lenvatinib. Nature. 2021;595(7869):730–734. doi: 10.1038/s41586-021-03741-7. [DOI] [PubMed] [Google Scholar]
- 49.Nijkamp MM, et al. Interaction of EGFR with the tumour microenvironment: implications for radiation treatment. Radiother Oncol. 2013;108(1):17–23. doi: 10.1016/j.radonc.2013.05.006. [DOI] [PubMed] [Google Scholar]
- 50.Yue X, et al. DNA-PKcs: a multi-faceted player in DNA damage response. Front Genet. 2020;11:607428. doi: 10.3389/fgene.2020.607428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Sun J, et al. UBE2T-regulated H2AX monoubiquitination induces hepatocellular carcinoma radioresistance by facilitating CHK1 activation. J Exp Clin Cancer Res. 2020;39(1):222. doi: 10.1186/s13046-020-01734-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang C, et al. Gain-of-function mutant p53 in cancer progression and therapy. J Mol Cell Biol. 2020;12(9):674–687. doi: 10.1093/jmcb/mjaa040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Muller PA, Vousden KH. p53 mutations in cancer. Nat Cell Biol. 2013;15(1):2–8. doi: 10.1038/ncb2641. [DOI] [PubMed] [Google Scholar]
- 54.Kong X, et al. Relationship between p53 status and the bioeffect of ionizing radiation. Oncol Lett. 2021;22(3):661. doi: 10.3892/ol.2021.12922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Gomes AR, et al. Influence of P53 on the radiotherapy response of hepatocellular carcinoma. Clin Mol Hepatol. 2015;21(3):257–267. doi: 10.3350/cmh.2015.21.3.257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Gudkov AV, Komarova EA. The role of p53 in determining sensitivity to radiotherapy. Nat Rev Cancer. 2003;3(2):117–129. doi: 10.1038/nrc992. [DOI] [PubMed] [Google Scholar]
- 57.Pirollo KF, et al. p53 mediated sensitization of squamous cell carcinoma of the head and neck to radiotherapy. Oncogene. 1997;14(14):1735–1746. doi: 10.1038/sj.onc.1201116. [DOI] [PubMed] [Google Scholar]
- 58.Hinata N, et al. Radiation induces p53-dependent cell apoptosis in bladder cancer cells with wild-type- p53 but not in p53-mutated bladder cancer cells. Urol Res. 2003;31(6):387–396. doi: 10.1007/s00240-003-0355-9. [DOI] [PubMed] [Google Scholar]
- 59.Cun Y, et al. Silencing of APE1 enhances sensitivity of human hepatocellular carcinoma cells to radiotherapy in vitro and in a xenograft model. PLoS ONE. 2013;8(2):e55313. doi: 10.1371/journal.pone.0055313. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 60.Vakifahmetoglu-Norberg H, et al. Chaperone-mediated autophagy degrades mutant p53. Genes Dev. 2013;27(15):1718–1730. doi: 10.1101/gad.220897.113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wu JH, et al. CMA down-regulates p53 expression through degradation of HMGB1 protein to inhibit irradiation-triggered apoptosis in hepatocellular carcinoma. World J Gastroenterol. 2017;23(13):2308–2317. doi: 10.3748/wjg.v23.i13.2308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Sun EJ, et al. Targeting the PI3K/Akt/mTOR Pathway in Hepatocellular Carcinoma. Biomedicines. 2021;9(11):1639. doi: 10.3390/biomedicines9111639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Xie Y, et al. PKI-587 enhances radiosensitization of hepatocellular carcinoma by inhibiting the PI3K/AKT/mTOR pathways and DNA damage repair. PLoS ONE. 2021;16(10):e0258817. doi: 10.1371/journal.pone.0258817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Esquela-Kerscher A, Slack FJ. Oncomirs - microRNAs with a role in cancer. Nat Rev Cancer. 2006;6(4):259–269. doi: 10.1038/nrc1840. [DOI] [PubMed] [Google Scholar]
- 65.Oura K, Morishita A, Masaki T. Molecular and functional roles of micrornas in the progression of hepatocellular carcinoma-a review. Int J Mol Sci. 2020;21(21):8362. doi: 10.3390/ijms21218362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wu CH, et al. Radiosensitization of hepatocellular carcinoma through targeting radio-associated microrna. Int J Mol Sci. 2020;21(5):1859. doi: 10.3390/ijms21051859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Luo J, et al. MicroRNA-146a-5p enhances radiosensitivity in hepatocellular carcinoma through replication protein A3-induced activation of the DNA repair pathway. Am J Physiol Cell Physiol. 2019;316(3):C299–C311. doi: 10.1152/ajpcell.00189.2018. [DOI] [PubMed] [Google Scholar]
- 68.Kuo LJ, Yang LX. Gamma-H2AX—a novel biomarker for DNA double-strand breaks. In Vivo. 2008;22(3):305–309. [PubMed] [Google Scholar]
- 69.Wang J, et al. MiR-320b/RAD21 axis affects hepatocellular carcinoma radiosensitivity to ionizing radiation treatment through DNA damage repair signaling. Cancer Sci. 2021;112(2):575–588. doi: 10.1111/cas.14751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Shao Y, et al. MicroRNA-621 acts as a tumor radiosensitizer by directly targeting SETDB1 in hepatocellular carcinoma. Mol Ther. 2019;27(2):355–364. doi: 10.1016/j.ymthe.2018.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Ma H, et al. The LncRNA H19/miR-193a-3p axis modifies the radio-resistance and chemotherapeutic tolerance of hepatocellular carcinoma cells by targeting PSEN1. J Cell Biochem. 2018;119(10):8325–8335. doi: 10.1002/jcb.26883. [DOI] [PubMed] [Google Scholar]
- 72.Wang J, et al. MiR-92b targets p57kip2 to modulate the resistance of hepatocellular carcinoma (HCC) to ionizing radiation (IR) -based radiotherapy. Biomed Pharmacother. 2019;110:646–655. doi: 10.1016/j.biopha.2018.11.080. [DOI] [PubMed] [Google Scholar]
- 73.Huang CY, et al. Palbociclib enhances radiosensitivity of hepatocellular carcinoma and cholangiocarcinoma via inhibiting ataxia telangiectasia-mutated kinase-mediated DNA damage response. Eur J Cancer. 2018;102:10–22. doi: 10.1016/j.ejca.2018.07.010. [DOI] [PubMed] [Google Scholar]
- 74.Fang Y, et al. Integration of glucose and cardiolipin anabolism confers radiation resistance of HCC. Hepatology. 2022;75(6):1386–1401. doi: 10.1002/hep.32177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Lin LC, et al. gamma-Glutamylcysteine synthetase (gamma-GCS) as a target for overcoming chemo- and radio-resistance of human hepatocellular carcinoma cells. Life Sci. 2018;198:25–31. doi: 10.1016/j.lfs.2018.02.015. [DOI] [PubMed] [Google Scholar]
- 76.Zhan Y, et al. NUPR1 contributes to radiation resistance by maintaining ROS homeostasis via AhR/CYP signal axis in hepatocellular carcinoma. BMC Med. 2022;20(1):365. doi: 10.1186/s12916-022-02554-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Xiao Y, Yu D. Tumor microenvironment as a therapeutic target in cancer. Pharmacol Ther. 2021;221:107753. doi: 10.1016/j.pharmthera.2020.107753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Dunn GP, Koebel CM, Schreiber RD. Interferons, immunity and cancer immunoediting. Nat Rev Immunol. 2006;6(11):836–848. doi: 10.1038/nri1961. [DOI] [PubMed] [Google Scholar]
- 79.Dunn GP, et al. Cancer immunoediting: from immunosurveillance to tumor escape. Nat Immunol. 2002;3(11):991–998. doi: 10.1038/ni1102-991. [DOI] [PubMed] [Google Scholar]
- 80.Jiang X, et al. Role of the tumor microenvironment in PD-L1/PD-1-mediated tumor immune escape. Mol Cancer. 2019;18(1):10. doi: 10.1186/s12943-018-0928-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Gao B, Jeong WI, Tian Z. Liver: an organ with predominant innate immunity. Hepatology. 2008;47(2):729–736. doi: 10.1002/hep.22034. [DOI] [PubMed] [Google Scholar]
- 82.Ishiyama K, et al. Difference in cytotoxicity against hepatocellular carcinoma between liver and periphery natural killer cells in humans. Hepatology. 2006;43(2):362–372. doi: 10.1002/hep.21035. [DOI] [PubMed] [Google Scholar]
- 83.Oura K, et al. tumor immune microenvironment and immunosuppressive therapy in hepatocellular carcinoma: a review. Int J Mol Sci. 2021;22(11):5801. doi: 10.3390/ijms22115801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Crispe IN. The liver as a lymphoid organ. Annu Rev Immunol. 2009;27:147–163. doi: 10.1146/annurev.immunol.021908.132629. [DOI] [PubMed] [Google Scholar]
- 85.Yu MC, et al. Inhibition of T-cell responses by hepatic stellate cells via B7-H1-mediated T-cell apoptosis in mice. Hepatology. 2004;40(6):1312–1321. doi: 10.1002/hep.20488. [DOI] [PubMed] [Google Scholar]
- 86.Ringelhan M, et al. The immunology of hepatocellular carcinoma. Nat Immunol. 2018;19(3):222–232. doi: 10.1038/s41590-018-0044-z. [DOI] [PubMed] [Google Scholar]
- 87.Wu J, et al. The proinflammatory myeloid cell receptor TREM-1 controls Kupffer cell activation and development of hepatocellular carcinoma. Cancer Res. 2012;72(16):3977–3986. doi: 10.1158/0008-5472.CAN-12-0938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Karin M, Clevers H. Reparative inflammation takes charge of tissue regeneration. Nature. 2016;529(7586):307–315. doi: 10.1038/nature17039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Yeung OW, et al. Alternatively activated (M2) macrophages promote tumour growth and invasiveness in hepatocellular carcinoma. J Hepatol. 2015;62(3):607–616. doi: 10.1016/j.jhep.2014.10.029. [DOI] [PubMed] [Google Scholar]
- 90.Krenkel O, Tacke F. Liver macrophages in tissue homeostasis and disease. Nat Rev Immunol. 2017;17(5):306–321. doi: 10.1038/nri.2017.11. [DOI] [PubMed] [Google Scholar]
- 91.Li X, et al. Targeting of tumour-infiltrating macrophages via CCL2/CCR2 signalling as a therapeutic strategy against hepatocellular carcinoma. Gut. 2017;66(1):157–167. doi: 10.1136/gutjnl-2015-310514. [DOI] [PubMed] [Google Scholar]
- 92.Saleh R, Elkord E. FoxP3(+) T regulatory cells in cancer: Prognostic biomarkers and therapeutic targets. Cancer Lett. 2020;490:174–185. doi: 10.1016/j.canlet.2020.07.022. [DOI] [PubMed] [Google Scholar]
- 93.Li X, et al. The immunological and metabolic landscape in primary and metastatic liver cancer. Nat Rev Cancer. 2021;21(9):541–557. doi: 10.1038/s41568-021-00383-9. [DOI] [PubMed] [Google Scholar]
- 94.Fu J, et al. Increased regulatory T cells correlate with CD8 T-cell impairment and poor survival in hepatocellular carcinoma patients. Gastroenterology. 2007;132(7):2328–2339. doi: 10.1053/j.gastro.2007.03.102. [DOI] [PubMed] [Google Scholar]
- 95.Korbecki J, et al. CC chemokines in a tumor: a review of pro-cancer and anti-cancer properties of the ligands of receptors CCR1, CCR2, CCR3, and CCR4. Int J Mol Sci. 2020;21(21):8412. doi: 10.3390/ijms21218412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Lu C, et al. Current perspectives on the immunosuppressive tumor microenvironment in hepatocellular carcinoma: challenges and opportunities. Mol Cancer. 2019;18(1):130. doi: 10.1186/s12943-019-1047-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Barker HE, et al. The tumour microenvironment after radiotherapy: mechanisms of resistance and recurrence. Nat Rev Cancer. 2015;15(7):409–425. doi: 10.1038/nrc3958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.McLaughlin M, et al. Inflammatory microenvironment remodelling by tumour cells after radiotherapy. Nat Rev Cancer. 2020;20(4):203–217. doi: 10.1038/s41568-020-0246-1. [DOI] [PubMed] [Google Scholar]
- 99.Grassberger C, et al. Differential association between circulating lymphocyte populations with outcome after radiation therapy in subtypes of liver cancer. Int J Radiat Oncol Biol Phys. 2018;101(5):1222–1225. doi: 10.1016/j.ijrobp.2018.04.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wang D, et al. The clinical and prognostic significance of CD14(+)HLA-DR(-/low) myeloid-derived suppressor cells in hepatocellular carcinoma patients receiving radiotherapy. Tumour Biol. 2016;37(8):10427–10433. doi: 10.1007/s13277-016-4916-2. [DOI] [PubMed] [Google Scholar]
- 101.Chen J, et al. Hypofractionated irradiation suppressed the off-target mouse hepatocarcinoma growth by inhibiting myeloid-derived suppressor cell-mediated immune suppression. Front Oncol. 2020;10:4. doi: 10.3389/fonc.2020.00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Zhu AX, et al. Pembrolizumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib (KEYNOTE-224): a non-randomised, open-label phase 2 trial. Lancet Oncol. 2018;19(7):940–952. doi: 10.1016/S1470-2045(18)30351-6. [DOI] [PubMed] [Google Scholar]
- 103.Yau T, et al. Efficacy and safety of nivolumab plus ipilimumab in patients with advanced hepatocellular carcinoma previously treated with sorafenib: the checkmate 040 randomized clinical trial. JAMA Oncol. 2020;6(11):e204564. doi: 10.1001/jamaoncol.2020.4564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Finn RS, et al. Atezolizumab plus bevacizumab in unresectable hepatocellular carcinoma. N Engl J Med. 2020;382(20):1894–1905. doi: 10.1056/NEJMoa1915745. [DOI] [PubMed] [Google Scholar]
- 105.El-Khoueiry AB, et al. Nivolumab in patients with advanced hepatocellular carcinoma (checkmate 040): an open-label, non-comparative, phase 1/2 dose escalation and expansion trial. Lancet. 2017;389(10088):2492–2502. doi: 10.1016/S0140-6736(17)31046-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Twyman-Saint Victor C, et al. Radiation and dual checkpoint blockade activate non-redundant immune mechanisms in cancer. Nature. 2015;520(7547):373–377. doi: 10.1038/nature14292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chiang CL, et al. Combined stereotactic body radiotherapy and checkpoint inhibition in unresectable hepatocellular carcinoma: a potential synergistic treatment strategy. Front Oncol. 2019;9:1157. doi: 10.3389/fonc.2019.01157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Anderson AC, Joller N, Kuchroo VK. Lag-3, Tim-3, and TIGIT: co-inhibitory receptors with specialized functions in immune regulation. Immunity. 2016;44(5):989–1004. doi: 10.1016/j.immuni.2016.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Kim KJ, Lee HW, Seong J. Combination therapy with anti-T-cell immunoglobulin and mucin-domain containing molecule 3 and radiation improves antitumor efficacy in murine hepatocellular carcinoma. J Gastroenterol Hepatol. 2021;36(5):1357–1365. doi: 10.1111/jgh.15319. [DOI] [PubMed] [Google Scholar]
- 110.Tang C, et al. Ipilimumab with stereotactic ablative radiation therapy: phase i results and immunologic correlates from peripheral T cells. Clin Cancer Res. 2017;23(6):1388–1396. doi: 10.1158/1078-0432.CCR-16-1432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Luke JJ, et al. Safety and clinical activity of pembrolizumab and multisite stereotactic body radiotherapy in patients with advanced solid tumors. J Clin Oncol. 2018;36(16):1611–1618. doi: 10.1200/JCO.2017.76.2229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Chung YL, et al. Sublethal irradiation induces vascular endothelial growth factor and promotes growth of hepatoma cells: implications for radiotherapy of hepatocellular carcinoma. Clin Cancer Res. 2006;12(9):2706–2715. doi: 10.1158/1078-0432.CCR-05-2721. [DOI] [PubMed] [Google Scholar]
- 113.Zhu L, et al. Angiogenesis and immune checkpoint dual blockade in combination with radiotherapy for treatment of solid cancers: opportunities and challenges. Oncogenesis. 2021;10(7):47. doi: 10.1038/s41389-021-00335-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Herrera FG, et al. Low-dose radiotherapy reverses tumor immune desertification and resistance to immunotherapy. Cancer Discov. 2022;12(1):108–133. doi: 10.1158/2159-8290.CD-21-0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Fukumura D, et al. Enhancing cancer immunotherapy using antiangiogenics: opportunities and challenges. Nat Rev Clin Oncol. 2018;15(5):325–340. doi: 10.1038/nrclinonc.2018.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Yu W, et al. Sorafenib potentiates irradiation effect in hepatocellular carcinoma in vitro and in vivo. Cancer Lett. 2013;329(1):109–117. doi: 10.1016/j.canlet.2012.10.024. [DOI] [PubMed] [Google Scholar]
- 117.Yi M, et al. Synergistic effect of immune checkpoint blockade and anti-angiogenesis in cancer treatment. Mol Cancer. 2019;18(1):60. doi: 10.1186/s12943-019-0974-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Sheng H, et al. ATR inhibitor AZD6738 enhances the antitumor activity of radiotherapy and immune checkpoint inhibitors by potentiating the tumor immune microenvironment in hepatocellular carcinoma. J Immunother Cancer. 2020;8(1):e000340. doi: 10.1136/jitc-2019-000340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Shen J, et al. Phase I clinical study of personalized peptide vaccination combined with radiotherapy for advanced hepatocellular carcinoma. World J Gastroenterol. 2017;23(29):5395–5404. doi: 10.3748/wjg.v23.i29.5395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Fornasier G, Francescon S, Baldo P. An update of efficacy and safety of cetuximab in metastatic colorectal cancer: a narrative review. Adv Ther. 2018;35(10):1497–1509. doi: 10.1007/s12325-018-0791-0. [DOI] [PubMed] [Google Scholar]
- 121.Muraro E, et al. Cetuximab in locally advanced head and neck squamous cell carcinoma: biological mechanisms involved in efficacy, toxicity and resistance. Crit Rev Oncol Hematol. 2021;164:103424. doi: 10.1016/j.critrevonc.2021.103424. [DOI] [PubMed] [Google Scholar]
- 122.Bonner JA, et al. Radiotherapy plus cetuximab for locoregionally advanced head and neck cancer: 5-year survival data from a phase 3 randomised trial, and relation between cetuximab-induced rash and survival. Lancet Oncol. 2010;11(1):21–28. doi: 10.1016/S1470-2045(09)70311-0. [DOI] [PubMed] [Google Scholar]
- 123.Jin WJ, et al. Tumor-specific antibody, cetuximab, enhances the in situ vaccine effect of radiation in immunologically cold head and neck squamous cell carcinoma. Front Immunol. 2020;11:591139. doi: 10.3389/fimmu.2020.591139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Huether A, et al. EGFR blockade by cetuximab alone or as combination therapy for growth control of hepatocellular cancer. Biochem Pharmacol. 2005;70(11):1568–1578. doi: 10.1016/j.bcp.2005.09.007. [DOI] [PubMed] [Google Scholar]
- 125.Kim HJ, et al. Clinical significance of soluble programmed cell death ligand-1 (sPD-L1) in hepatocellular carcinoma patients treated with radiotherapy. Radiother Oncol. 2018;129(1):130–135. doi: 10.1016/j.radonc.2017.11.027. [DOI] [PubMed] [Google Scholar]
- 126.Sung W, et al. Mathematical modeling to simulate the effect of adding radiation therapy to immunotherapy and application to hepatocellular carcinoma. Int J Radiat Oncol Biol Phys. 2022;112(4):1055–1062. doi: 10.1016/j.ijrobp.2021.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Grassberger C, et al. Assessing the interactions between radiotherapy and antitumour immunity. Nat Rev Clin Oncol. 2019;16(12):729–745. doi: 10.1038/s41571-019-0238-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.