Abstract
Objective
To describe older adult patients’ and care partners’ knowledge broker roles during emergency department (ED) visits.
Background
Older adult patients are vulnerable to communication and coordination challenges during an ED visit, which can be exacerbated by the time and resource constrained ED environment. Yet, as a constant throughout the patient journey, patients and care partners can act as an information conduit, or knowledge broker, between fragmented care systems to attain high-quality, safe care.
Methods
Participants included 14 older adult patients (≥ 65 years old) and their care partners (e.g., spouse, adult child) who presented to the ED after having experienced a fall. Human factors researchers collected observation data from patients, care partners and clinician interactions during the patient’s ED visit. We used an inductive content analysis to determine the role of patients and care partners as knowledge brokers.
Results
We found that patients and care partners act as knowledge brokers by providing information about diagnostic testing, medications, the patient’s health history, and care accommodations at the disposition location. Patients and care partners filled the role of knowledge broker proactively (i.e. offer information) and reactively (i.e. are asked to provide information by clinicians or staff), within-ED work system and across work systems (e.g. between the ED and hospital), and in anticipation of future knowledge brokering.
Conclusion
Patients and care partners, acting as knowledge brokers, often fill gaps in communication and participate in care coordination that assists in mitigating health care fragmentation.
Keywords: Care fragmentation, Patient-provider communication, Patient safety, Emergency medicine, Work system, Care transitions and handoffs, Patient engagement and self-care
Précis
Health care delivery is often fragmented, which may harm vulnerable older adult patients. Patients and care partners play an important role in closing communication and coordination gaps in fragmented care processes. During their visit to the ED, patients and their care partners fill these gaps by acting as knowledge brokers.
Introduction
Health care in the US is often described as fragmented as patients receive care from multiple care settings and clinicians with limited coordination and integration (Enthoven, 2009), which can adversely affect quality and safety of patient care (Kern et al., 2019). This lack of integration and continuity is apparent both within and across care settings or work systems and is influenced by multiple factors, such as different health insurance and reimbursement structures, and lack of health IT interoperability (Cebul, Rebitzer, Taylor, & Votruba, 2008; Kern et al., 2019). A pervasive characteristic of health care fragmentation is sub-optimal communication and coordination among patients and clinicians, especially when patients transition between multiple care settings and receive care from different clinicians (2018). These communication and coordination challenges can negatively affect quality and safety of care (Vincent & Amalberti, 2016) and result in unnecessary hospital visits, longer hospital stays, or readmissions to hospitals or emergency departments (Ahuja, Alvarez, & Staats, 2020). Vulnerable populations, such as older adults, are at higher risk for negative patient safety consequences that result from health care fragmentation (Long, Brown, Ames, & Vincent, 2013; Long & Vincent, 2012). In a survey of more than 11,000 older adults (>65 years old), Kern et al. (2020) found that those who reported a gap in care coordination (e.g., lack of communication among their doctors) were more likely to experience preventable adverse outcomes, such as repeat diagnostic tests, drug-drug interactions, ED visits and hospital admissions.
Older adults (≥65) comprise a large proportion of patients who present to the emergency department (ED) (over 23 million visits or 17.9% of all ED visits in 2018 in the US) (Cairns, Kang, & Santo, 2018). Surrounding an ED visit, older adults experience multiple care transitions, such as transfer from Emergency Medical Services (EMS), transitions from and back to a skilled nursing facility (SNF) or home, and admission to a hospital. For older adults, transitions of care around an ED visit are often marked by adverse events, such as functional decline, unplanned hospitalization, and repeat ED visits (Aminzadeh & Dalziel, 2002; Schnitker, Martin-Khan, Beattie, & Gray, 2011). Yet, supporting an older adult during the ED visit can be challenging as ED work environments are frequently under time and resource constraints (Perry, Wears, & Fairbanks, 2012). ED clinicians may have limited access to patient information or may not have the resources to effectively access information. The question is whether patients and their care partners could play a role in the information flow at times when ED clinicians need accurate and timely information to care for them.
As a constant in their care journey (Carayon & Wooldridge, 2019; Carayon, Wooldridge, Hoonakker, Hundt, & Kelly, 2020), patients and their care partners play a key role in the information flow across transitions and may help to close gaps in communication and coordination between care settings and clinicians resulting from misaligned work systems (Storm, Siemsen, Laugaland, Dyrstad, & Aase, 2014; Vincent & Amalberti, 2016; Werner et al., 2020; Werner et al., 2021). O’Hara et al. (2019) suggest that patients and care partners contribute to communication and coordination during the patient journey through their role as knowledge brokers. As knowledge brokers, patients fill structural holes (e.g., missing information) across health care system boundaries, contributing to patient safety (O’Hara, Canfield, & Aase, 2019; Schubert, Wears, Holden, & Hunte, 2015). O’Hara and colleagues (2019) have proposed that patients and care partners play various knowledge broker roles providing “timely information exchange”, “safety critical information” about “medical history, treatment regimens and medications”, and act as a “mechanism for information exchange between healthcare professionals”. For example, a qualitative study of hospital admissions and discharges in Norway identified several challenges for older adults, including the need for care partners to play the role of knowledge broker and provide information about the patient’s health condition (Storm et al., 2014). In a study of cardiology patients discharged from two UK hospitals, Fylan et al. (2018) found that patients acted as an information conduit after hospital discharge as they ensured information about medication changes was communicated to their primary care physician (PCP). The work of knowledge brokering is one type of knowledge work performed by patients and care partners (Papautsky & Patterson, 2021). This patient and care partner work can help to integrate information across various care settings and clinicians, especially in instances of information deficit such as during ED visits.
Patients and care partners may serve as knowledge brokers during the care journey; however, research on this topic is limited to studies on knowledge brokering during hospital admissions and discharges of older adults (Fylan et al., 2018; Storm et al., 2014). Research on knowledge brokering in health care has examined the role of clinicians as knowledge brokers (Bishop & Waring, 2017; Burgess & Currie, 2013; Waring, Currie, Crompton, & Bishop, 2013), and knowledge brokering in translating research into practice (Bornbaum, Kornas, Peirson, & Rosella, 2015; Ward, House, & Hamer, 2009). Outside of health care, a knowledge broker is defined as someone with access to knowledge from different organizations, who can integrate and share the knowledge, and enable learning (Hargadon, 2002). In the context of health care, we define a patient or care partner as a knowledge broker when they interact with a health care worker, actively share information, and act as a conduit of information with another health care worker or work system (O’Hara, Aase, et al., 2019). From our literature review, these knowledge broker roles have not been systematically identified and described for older adults and their care partners during ED visits. Thus, a critical next step is to explore the extent to which older adults and their care partners serve as knowledge brokers during ED visits. This will provide the foundation for intervention development and system redesign to support the engagement of patients and care partners throughout the patient journey.
Research objective
The objective of this study is to describe the knowledge broker roles of older adult patients and care partners during ED visits.
Methods
This study was conducted as a part of a larger project focused on the care journeys of older adults who present to the ED after having experienced a fall (https://cqpi.wisc.edu/research/health-care-and-patient-safety-seips/patient-safety-learning-lab-psll/). We collected data in the ED of a US academic medical center from August to December of 2019. This research complied with the American Psychological Association Code of Ethics and was approved by the Institutional Review Board at the University of Wisconsin-Madison.
Sample
The sample consisted of 14 older adults (female=6, age range=65–97) and their care partner(s). Older adults were accompanied in the ED by at least one care partner (range=1–4; 8 patients = 1 care partner, 5 patients = 2 care partners, 1 patient = 4 care partners), who were physically present in the ED with the patient at some point during the ED visit. Care partners included spouses, family (e.g., children, grandchildren, cousins) and friends. Out of the care partners present with the patients, 14 were female and 5 were male. Older adults arrived at the ED via ambulance (n = 7) or car (n = 7) from their home (n = 9), a skilled nursing facility (n = 2), assisted living facility (n= 2) or another hospital (n = 1). After their ED visit, older adults went to their home (n = 4), the hospital (n = 7), the skilled nursing facility where they were a resident (n = 1) or the Clinical Decision Unit (CDU) of the ED (n = 2). In the CDU located within the ED, patients are monitored by ED clinicians for up to 24 hours to aid in the final disposition decision.
Recruitment and data collection
Two human factors (HF) researchers conducted 14 patient-centered observations with the 14 participating older adults and their care partners. To qualify for the study, participants must have: presented to the ED for a primary complaint of fall occurring within the previous 48 hours; not been categorized as a Level One trauma; had their power of attorney (POA) present at the time of ED visit, if they had an activated POA; and been aged 65 years or older. The care partner(s) were also recruited to participate.
The researchers collaborated with ED research coordinators (EDRC) to recruit participants. The EDRC monitored the ED track-board for potential participants when the HF researchers were present in the ED. When a potential participant was identified, the EDRC had a discussion with an ED clinician caring for the patient to ensure the patient was appropriate to approach. Upon approval from the ED clinician, the EDRC informed the patient and/or care partner of the study, asked them to participate, and, if the patient and/or care partner agreed, obtained consent. The EDRC introduced the HF researcher to the patient and care partner, at which point the observation began. HF researchers observed the interactions among the patient, their care partners(s), and clinicians over the course of the entire ED stay, taking detailed notes using a structured observation form (https://cqpi.wisc.edu/research/health-care-and-patient-safety-seips/patient-safety-learning-lab-psll/#tools). The observation form included multiple rows to record interactions, i.e., information about who talks to whom about what using which tools or technologies. The observation concluded when the patient was physically transferred to their disposition location (e.g., hospital, home).
We collected data during weekdays and weekends across numerous clinical shifts with the earliest observation beginning at 8:49 AM and the latest observation ending at midnight. The observations lasted an average of 4.7 hours (range: 2.63–7.67) totaling 66 observation hours and yielded 121 pages of typed observation notes.
Data analysis
We analyzed the data in two phases. The first phase included an inductive content analysis (Elo & Kyngas, 2008) of eight of the 14 patient-centered observations, which led to developing a codebook that was applied in the second phase. The second phase included analyzing the remaining six observations according to the codes and refined definitions outlined in the codebook. Throughout the coding process, the researchers reviewed the coding iteratively and refined, added, and combined codes. At multiple times during phases 1 and 2, the data and resulting dimensions were presented and discussed with the entire research team, which included ED clinicians and a patient and care partner representative.
Phase 1
In phase 1, the eight observations included the patient and one care partner. With our definition of knowledge broker (see above), we identified knowledge brokering instances using the following criteria:
the patient and/or care partner interacted with a clinician or staff member,
the patient and/or care partner were actively involved in the conversation (e.g., responding to or asking questions), and
the patient and/or care partner were acting as a mechanism of information exchange between systems (e.g., ED and skilled nursing facility) or specific roles within systems (e.g., ED nurse and ED resident).
We abstracted the identified knowledge brokering instances from the observation notes into an Excel workbook where they were inductively analyzed by two researchers. The researchers individually coded observations, compared their coding, noted any discrepancies, and met to discuss their coding until consensus was reached about the assigned codes and the coding structure. During this inductive data analysis, four knowledge brokering dimensions emerged; see Table 1 for the dimensions and their definitions.
Table 1.
Dimensions and definitions of knowledge brokering
| No. | Dimensions | Definitions |
|---|---|---|
| 1 | Proactive versus reactive knowledge brokering | Proactive knowledge brokering occurs when a patient or care partner offers the information without being prompted by ED clinician or staff. |
| Reactive knowledge brokering occurs when a clinician or staff asked/prompted the patient about some information. | ||
| 2 | Content of information | Content of information is about the information being communicated during knowledge brokering instances and includes the patient’s prior health conditions, medications, care after disposition from the ED, and diagnostic testing. |
| 3 | Within-ED work system and across across-system knowledge brokering | Within-ED work system knowledge brokering occurs when a patient or care partner acts as a knowledge broker among ED clinicians and/or staff (e.g., between ED nurse and ED resident). |
| Across-system knowledge brokering occurs when a patient or care partner acts as a knowledge broker between the ED (i.e., ED clinicians and staff) and other care settings (e.g., neurology specialist, hospitalist, EMS, PCP, SNF, assisted living facility). | ||
| 4 | Anticipatory knowledge brokering | Anticipatory knowledge brokering occurs when knowledge brokering is recognized by a clinician or the patient and care partner for a future interaction (e.g., when an ED clinician or staff recommends that the patient or care partner brings up information to their PCP in a post-ED follow-up visit that will occur in the future). |
Phase 2
In phase 2, we analyzed the remaining six observations, which included a patient with more than one care partner. One researcher identified the knowledge brokering instances and coded them along the four dimensions described in Table 1. A second researcher reviewed the coding and provided feedback.
Results
Patients and care partners as knowledge brokers
We identified a total of 33 instances of patients and care partners assuming the role of knowledge broker in 12 of the 14 observations. On average, patients and care partners assumed the role of knowledge broker 2 times during their ED visit (range: 0–7). We found that care partner(s) assumed the role of knowledge broker for older adult patients in 23 of 33 instances (70%).
As described in Table 1, we characterized the knowledge brokering roles on four dimensions. An instance of knowledge brokering is illustrated in Table 2. Throughout the rest of the section, we further describe each of the four dimensions of knowledge brokering and provide examples.
Table 2.
Example of knowledge brokering
| Example | Proactive vs. reactive | Content of information | Within-ED work system vs. across-system | Anticipatory |
|---|---|---|---|---|
| EMS transported a 72-year-old male patient to the ED after he suffered a fall. While in the ED, he experienced uncontrollable shaking. The nurse asked him whether he had diabetes and if EMS had measured his blood sugar level. The patient shared his blood sugar level (taken by EMS) with the nurse. | Reactive: the nurse prompts the patient to act as a knowledge broker by asking them about the results of the blood sugar test. | Prior diagnostic testing: results of the patient’s blood sugar test | Across-system: the patient acts as a knowledge broker between EMS and the nurse in the ED | Not anticipatory |
Proactive versus reactive knowledge brokering
Patients and care partners filled the role of knowledge brokers proactively (i.e., offer information) in 17 of 33 instances (52%) and reactively (i.e., prompted by clinicians) in 16 of 33 of instances (48%). In filling the role of the knowledge broker proactively, care partners offered information to clinicians in 13 of the 17 instances (76%) and patients offered information in 4 of the 17 instances (24%). For example, in an interaction between an orthopedic surgery resident and the care partner, the orthopedic surgery resident mentioned that she will contact the hospitalist to ensure there are no additional medical problems that need to be addressed during the patient’s hospital stay. The care partner offered to contact the hospital where the patient receives treatment for her heart condition to gather additional information. The orthopedic surgery resident replied that they have access to the other hospital’s electronic health record (EHR) and asked whether the patient has any questions. The care partner replied that the patient had her pacemaker read at the other hospital two days prior. In this example, the care partner exhibits two instances of proactive knowledge brokering (1) when she offered to contact the patient’s hospital where the patient receives treatment for her heart, and (2) when she communicated that the patient’s pacemaker was read two days prior.
When filling the role of knowledge broker reactively (16 instances), patients and care partners provide information in response to questions from nurses (10 instances), ED residents (2 instances), physician assistants, patient access representatives, radiology technicians, and social workers (1 instance each). In one example, the nurse entered the room and asked the patient and care partners what the physician had told them. The patient explained that the physician told him that he would be discharged home if he could walk independently. The nurse replied that he would ask another nurse to help the patient try to walk in preparation for his discharge.
Content of information provided
In their role as knowledge brokers, patients and care partners shared information related to diagnostic testing, medications, the patient’s health history, and care accommodations at the disposition location (i.e., where the patient will be transferred to after the ED). Information about diagnostic tests included when a test is to happen, whether a test has happened, or whether the test results have been communicated. In one instance, the neurology resident asked the patient and care partner how many CT scans the patient had received; the patient replied that she had one CT scan while at a previous ED.
Patients and their care partners convey information about the patient’s medications. For example, during a conversation with the ED pharmacist, a care partner used a list on her cellphone to describe the patient’s medications and dosages. The care partner explained that the patient is taking a twice-daily medication only once per day as the patient has a hard time taking medications. She had been in contact with the patient’s primary care physician (PCP) who altered the patient’s prescription to be once daily. However, the care partner said that she had yet to transition the patient to the once-daily medication: the patient has continued to take the twice-daily medication once per day because they still had remaining pills. The pharmacist indicated that the patient was not getting the full benefit of the medication by taking only one dose per day instead of the two doses, and that the patient would likely get the new once-daily medication if he stayed in the CDU.
Patients and care partners also share knowledge about care accommodations at the next step of the patient journey, such as the ED CDU, hospital, or SNF. For example, an ED nurse asked the patient and care partner whether the patient will be receiving a physical and occupational therapy consult once admitted to the ED CDU. The care partner confirmed that the patient will receive a physical and occupational therapy consult in the CDU.
Within the ED work system and across systems
Patients and care partners acted as knowledge brokers within the ED work system and across systems (e.g., between EMS and the ED). See Figure 1 for all the roles involved within and across systems. For more details on the specific pairs of roles and care settings involved in knowledge brokering, see the table in Appendix. Within-ED work system knowledge brokering occurred in 12 of 33 instances (36%) and included situations whereby the patient or care partner filled the role of knowledge broker between ED clinicians and staff. In one example, the care partner explained to the ED nurse that the ED resident told them the patient would be discharged home, where the patient and family would care for the patient’s wounds. This represents within-system knowledge brokering because the care partner acted as a conduit of information between ED clinicians (i.e., ED nurse and ED resident). Across-system knowledge brokering occurred in 21 of 33 instances (63%), including situations whereby the patient or care partner acts as a conduit of information between the ED work system and another work system such as SNF, EMS, specialist consultant (e.g., orthopedic surgery, neurology), hospitalist, or the patient’s PCP. For example, a radiology technician asked the patient and care partner whether the patient has diabetes after noticing the patient’s medical device. The care partner responded, yes, and added that the patient has received X-rays in the past with her device. The care partner filled the role of across-system knowledge broker by reactively offering information to the ED work system (i.e., radiology technician) from another system (i.e., imaging staff at other hospital).
Figure 1.
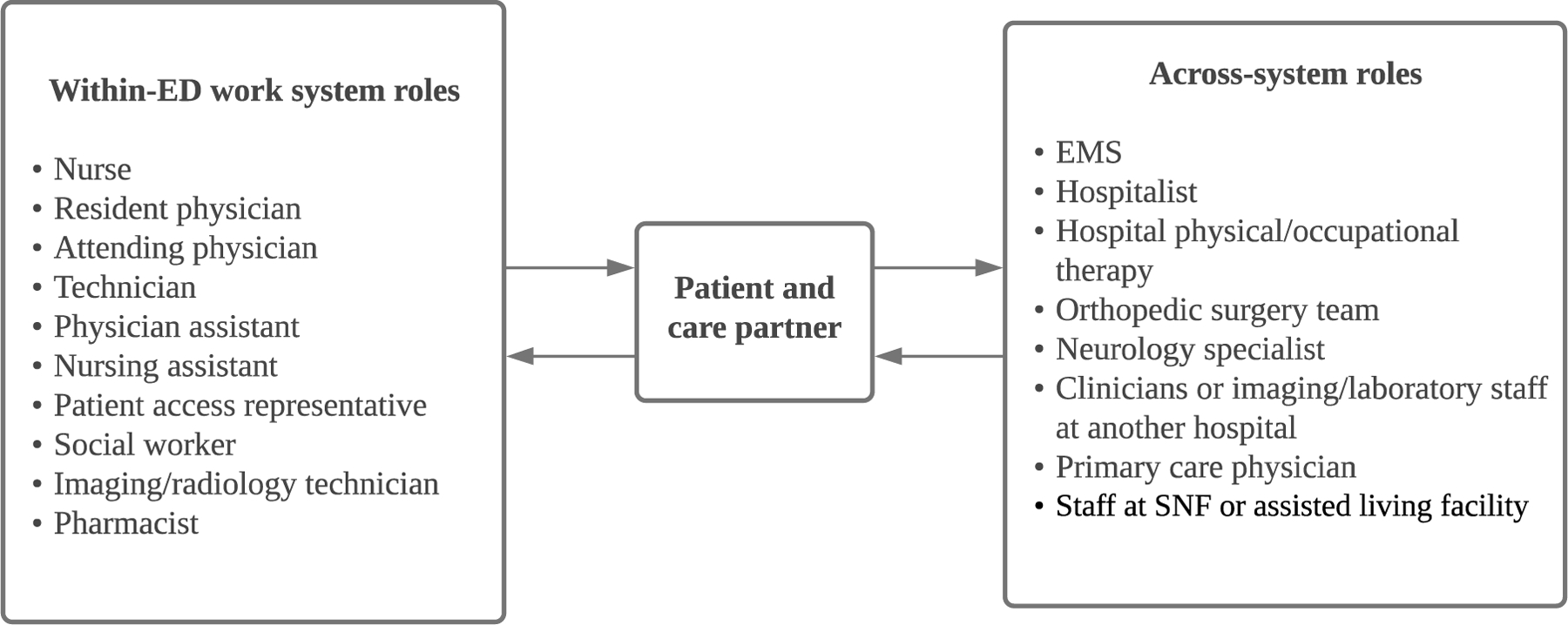
Within- and across-system roles involved in knowledge brokering
Anticipatory knowledge brokering
In five of the 33 instances (15%), patients and their care partners anticipated and acted upon the need for future knowledge brokering or a clinician or ED staff recommended the patient or care partner act as knowledge brokers in future interactions. For example, a care partner called the patient’s ALF to tell them that the patient would likely be back to the facility that night, pending consultation from the spine surgeon.
There are two instances of clinicians and ED staff recommending that the patient or care partners act as a knowledge broker in future interactions. While being discharged, the ED nurse asked the patient and care partners if they had any questions about the patient’s ED visit. The care partner asked whether the medication given to the patient during their ED visit would be documented in EHR. The ED nurse explained that the medication will be documented in the EHR and accessible to the patient’s PCP, but that they should also plan to bring the discharge instructions with them to the follow-up PCP appointment. In another instance, a social worker asked the patient and care partner about the patient’s care plan. The care partner replied that the care plan has yet to be determined but he hoped the patient would be admitted to the hospital for observation. The social worker recommended that the care partner mention this to the patient’s ED care team because they may be able to accommodate his request. In both instances, the clinician (i.e., ED nurse or social worker) anticipates and recommends that the patient or care partner act as a knowledge broker to convey information (i.e., documentation of medication in discharge instructions or preference for admission) in future health care interactions (i.e., with PCP or ED care team).
Discussion
This exploratory observational study drew on observations of 14 older adult patients and their care partners during a visit to the ED after experiencing a fall. We identified knowledge brokering in 12 of the 14 observations, highlighting the frequent and diverse ways that patients and care partners act as knowledge brokers during ED visits. Further, we found that care partners are involved in over half of knowledge brokering instances. An important contribution of this study is to define the dimensions of knowledge brokering of patients and care partners during ED visits; see Table 1.
As knowledge brokers, patients and care partners share different information on the patient’s health status, medications, care disposition after the ED visit, and the results of diagnostic tests. We add to the limited literature focused on hospital admission and discharges that found patients and care partners sharing information on the patient’s health condition and medication (Fylan et al., 2018; Storm et al., 2014). Our results expand upon these findings as patients and their care partners provide information about diagnostic testing, medications, the patient’s health history, and care accommodations at the next step in the patient journey. Further, they act as knowledge brokers through many phases of the patient journey, not only upon hospital admission and discharge. Patients’ and care partners’ role in providing information may be indicative of barriers that clinicians and staff face with access to information from elsewhere in the patient journey (Wiig et al., 2020). Thus, system factors, such as challenges in accessing information in the EHR, may contribute to ED clinicians engaging patients and care partners as an information conduit. For instance, as described in an example above, a neurology resident asks the patient about CT scans; this may result from the challenges clinicians face in timely access to information from other health care institutions.
Our findings show that both patients and their care partners initiate instances of knowledge brokering. Proactive knowledge brokering may indicate an engaged patient and care partner who can share information important to their health goals. Despite its potential role in patient engagement, proactive knowledge brokering may not be achievable by all patients and care partners. Patients with multiple comorbidities, health literacy limitations, who are not accompanied by a care partner may not be able to engage in proactive knowledge brokering. This should not preclude efforts at creating opportunities for engaging patients and their care partners in their care. Reactive knowledge brokering, where an ED clinician or staff asks for information from a patient or their care partner, may represent an invitation for patients and care partners to be engaged in their care, e.g. as a patient-centered care practice (Lor, Crooks, & Tluczek, 2016; Scholl, Zill, Harter, & Dirmaier, 2014; Snyder & Engstrom, 2016). Yet, reactive knowledge brokering may place undue burden on the patient and care partner, such as when ED clinicians use a work-around (Halbesleben, Wakefield, & Wakefield, 2008) resulting from work system barriers (Carayon, Hundt, & Hoonakker, 2019), in order to get information. For instance, updated information on the patient may not be available in a timely manner in the EHR; therefore, clinicians may instead ask the patient or care partner to provide information.
By exploring the role of patients and care partners as knowledge brokers during their ED visit, our results emphasize the unique role of patients and care partners in the patient journey where they act as within-ED work system and across-system knowledge brokers as well as anticipatory knowledge brokers. This is an important finding considering the emerging concept of patient journey in the SEIPS 3.0 model (Carayon et al., 2020). The role of patients and care partners as across-system knowledge brokers fits with findings of other studies (Fylan et al., 2018; Storm et al., 2014). The results of our study expand upon the understanding of the role of patients and care partners across systems by describing the various systems and roles that patients and care partners connect with the ED (see Figure 1 and Table in Appendix). Across-system knowledge brokering may be an outcome of the fragmented health care system that patients navigate throughout their journey. Gaps in communication and coordination across care settings in the patient journey can be the consequence of many factors, including misalignment of mental models across work systems involved in care transitions (Werner et al., 2021). The diversity of roles identified in both within- and across-system knowledge brokering emphasizes the key role of patients and care partners as the only constant surrounding an ED visit. The number of roles identified reveals that knowledge brokering is not a phenomenon isolated to certain clinicians or care settings, but rather occurs throughout the entire patient journey and across multiple work systems. Further, anticipatory knowledge brokering reveals how patients and their care partners can take steps to prepare for future activities in the patient journey.
Study limitations and future research
The findings from our study should be examined considering several limitations. First, this study was conducted with older adult patients and their care partners who presented to one ED having experienced a fall, which represent the experiences of a specific population and therefore limit the transferability of the results. Second, as demographic information about the participants and their care partners was not collected, the generalizability of the results may be limited, and future research could examine knowledge brokering in diverse populations. Third, due to the limited number of observations conducted, we may not have identified every dimension of knowledge brokering. Future work is needed to expand our understanding of the role of patients and care partners as knowledge brokers, including the factors contributing to knowledge brokering such as communication and coordination gaps. Finally, we did not evaluate the accuracy of the information that patients and care partners provided as knowledge brokers; this could be a topic for future research.
Our results identify four dimensions of the role of knowledge broker assumed by patients and care partners during ED visits; future research could build on our findings and further examine those dimensions in other settings and patient populations. In our study, we did not evaluate the impact of knowledge brokering on patients and their care partners or clinicians and staff. While filling the role of knowledge broker may positively impact the patient by facilitating their engagement in their care, it may also negatively affect them by putting undue burden on the patient and care partner. Future research should explore the outcomes of knowledge brokering by patients and care partners. For example, why do they ask questions, why do they offer information? This will further our understanding of the impact of knowledge brokering on patients, care partners, clinicians, and health care staff. Overall, there is a need for future research to investigate how to redesign work systems to support and enhance patients’ and care partners’ roles as knowledge brokers and their engagement in their care, without placing undue burden on them.
Conclusion
As the only constant in their health care journey, patients and care partners often fill gaps in communication and coordination, acting as a conduit of information or knowledge broker, to mitigate health care fragmentation and promote high-quality, safe care. Analyzing patient and care partners’ role as knowledge brokers allowed us to identify how the information transfer was initiated, who transferred the information, the content of the information, and from which system(s) the information was being transferred between. Understanding the role of patients and care partners as knowledge brokers and the content of the information they provide can help to devise solutions to close the information gaps.
Key points:
Patients and care partners often act as knowledge brokers during ED visits.
Patients and care partners are knowledge brokers within and across work systems, highlighting their unique position in the patient journey.
Patients and care partners act as both reactive (i.e., asked by clinicians) and proactive (i.e., offer information) knowledge brokers.
Various types of information (e.g., medication, care after discharge, prior health history) are communicated and shared by the patient and care partners who act as knowledge broker.
Acknowledgments
This research was supported by grant 5R18HS026624 from the Agency for Healthcare Research and Quality (AHRQ), grant UL1TR002373 from the Clinical and Translational Science Award (CTSA) program, through the NIH National Center for Advancing Translational Sciences (NCATS), and grant K24AG054560 from the National Institute on Aging. The project was also supported by the University of Wisconsin School of Medicine and Public Health through Wisconsin Partnership Program funding to the Wisconsin Institute for Healthcare Systems Engineering and the Health Innovation Program. The content is solely the responsibility of the authors and does not necessarily represent the official views of AHRQ or the NIH.
Biographies
Kathryn L. Wust is a PhD student in industrial engineering at the University of Wisconsin-Madison. She completed a M.S. in industrial engineering at the University of Wisconsin-Madison in 2020.
Pascale Carayon is the Professor Emerita in the Department of Industrial and Systems Engineering at the University of Wisconsin-Madison. She received her Ph.D. in Industrial Engineering at the University of Wisconsin-Madison in 1988.
Nicole Werner is an Associate Professor in the department of Industrial and Systems Engineering and Director of the Wisconsin Institute for Healthcare Systems Engineering at the University of Wisconsin-Madison. She received her PhD in Human Factors and Applied Cognition from George Mason University in 2014.
Peter Hoonakker is the Senior Scientist at the Wisconsin Institute for Healthcare Systems Engineering at the University of Wisconsin-Madison. He completed his Ph.D. in Psychology from the University of Vienna in 2008.
Megan E. Salwei is a NLM Postdoctoral Research Fellow in the Department of Biomedical Informatics at Vanderbilt University Medical Center. She completed her Ph.D. in Industrial Engineering at the University of Wisconsin-Madison in 2020.
Rachel A. Rutkowski is a PhD student in industrial engineering at the University of Wisconsin-Madison. She completed a M.S. in industrial engineering at the University of Wisconsin-Madison in 2020.
Hanna J. Barton (she/they) is a PhD student in Industrial and Systems Engineering at the University of Wisconsin—Madison. They hold a M.S. from the same department and a B.S. in Biomedical Engineering.
Paula vW. Dail is an emerita research professor of social welfare and public policy. She is currently a member of the University of Wisconsin-Madison Health Sciences Patient and Family Advisory Council. She earned a PhD from the University of Wisconsin-Madison in 1983.
Barbara King is an Associate Professor, Director of the Center for Aging Research and Education (CARE), and Director of Education for ICTR- CAP at the University of Wisconsin (UW)- Madison. She received her PhD in Nursing from UW- Madison in 2010.
Brian W. Patterson is an Assistant Professor in the BerbeeWalsh Department of Emergency Medicine and affiliate faculty in the Department of Industrial and Systems Engineering at the University of Wisconsin-Madison. He received his MD and MPH from Northwestern University Feinberg School of Medicine in 2009.
Michael S. Pulia is an Assistant Professor in the BerbeeWalsh Department of Emergency Medicine and affiliate faculty in the Department of Industrial and Systems Engineering at the University of Wisconsin-Madison. He earned his MD from Loyola University Chicago and MS in Clinical Investigation from University of Wisconsin-Madison.
Manish Shah is the John and Tashia Morgridge Chair of Emergency Medicine Research, Vice Chair of Research, and Professor in the BerbeeWalsh Department of Emergency Medicine. He is a clinically active emergency physician who has dedicated his academic career to improving the care of acutely ill older adults. He received his MD and MPH from the University of Rochester School of Medicine and Dentistry.
Maureen Smith is a Professor in Population Health Sciences and Family Medicine & Community Health and Director of the Health Innovation Program at the UW-Madison School of Medicine and Public Health. Dr. Smith has M.D. and M.P.H. degrees from Yale University School of Medicine, and a Ph.D. from the University of Minnesota in Health Services Research, Policy and Administration in 1999.
Appendix
Table. Pairs of roles and care settings involved, along with patients and care partners, in knowledge brokering
| Within-ED work system knowledge brokering |
| ED nurse – ED care team |
| ED nurse – ED physician assistant |
| ED nurse – ED resident |
| ED nurse – Laboratory staff |
| ED physician assistant – ED care team |
| ED physician assistant – Imaging staff |
| ED technician – Imaging staff |
| Social worker – ED care team |
| ED nursing assistant – Imaging staff |
| Across-system knowledge brokering |
| ED nurse – EMS |
| ED nurse – Hospital physical/occupational therapy |
| ED nurse – Neurology specialist |
| ED nurse – Orthopedic specialist |
| ED nurse – Primary care physician |
| ED nurse – Trauma specialist |
| ED resident – Hospitalist |
| ED resident – Orthopedic specialist |
| ED pharmacy – Primary care physician |
| ED technician – Imaging staff at another hospital |
| ED care team – Assisted living facility staff |
| ED care team – Primary care physician |
| Imaging staff – Hospitalist |
| Imaging staff – Orthopedic specialist |
| ED patient access representative – SNF |
| Clinicians at another hospital – Neurology specialist |
| Clinicians at another hospital – Orthopedic specialist |
References
- Ahuja V, Alvarez CA, & Staats BR (2020). Maintaining continuity in service: an empirical examination of primary care physicians. Manufacturing & Service Operations Management, 22(5), 1088–1106. [Google Scholar]
- Aminzadeh F, & Dalziel WB (2002). Older adults in emergency department: a systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Annals of Emergency Medicine, 39(3), 238–247. [DOI] [PubMed] [Google Scholar]
- Bishop S, & Waring J (2017). The knowledge brokering situations of care transitions. In Aase K, Waring J, & Schibevaag L (Eds.), Researching Quality in Care Transitions (pp. 159–178). Cham, Switzerland: Palgrave Macmillan. [Google Scholar]
- Bornbaum CC, Kornas K, Peirson L, & Rosella LC (2015). Exploring the function and effectiveness of knowledge brokers as facilitators of knowledge translation in health-related settings: a systematic review and thematic analysis. Implementation Science, 10. doi: 10.1186/s13012-015-0351-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgess N, & Currie G (2013). The knowledge brokering role of the hybrid middle level manager: the case of healthcare. British Journal of Management, 24, S132–S142. doi: 10.1111/1467-8551.12028 [DOI] [Google Scholar]
- Cairns C, Kang K, & Santo L (2018). National Hospital Ambulatory Medical Care Survey: 2018 Emergency Department Summary Tables Retrieved from https://www.cdc.gov/nchs/data/nhamcs/web_tables/2018_ed_web_tables-508.pdf
- Carayon P, Hundt AS, & Hoonakker P (2019). Technology barriers and strategies in coordinating care for chronically ill patients. Applied Ergonomics, 78, 240–247. doi: 10.1016/j.apergo.2019.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, & Wooldridge A (2019). Improving patient safety in the patient journey: contributions from human factors engineering. In Smith AE (Ed.), Women in Industrial and Systems Engineering: Key Advances and Perspectives on Emerging Topics (pp. 275–299). Cham, Switzerland: Springer Nature. [Google Scholar]
- Carayon P, Wooldridge A, Hoonakker P, Hundt AS, & Kelly MM (2020). SEIPS 3.0: Human-centered design of the patient journey for patient safety. Applied Ergonomics, 84. doi: 10.1016/j.apergo.2019.103033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cebul RD, Rebitzer JB, Taylor LJ, & Votruba ME (2008). Organizational fragmentation and care quality in the U.S. healthcare system. Journal of Economic Perspectives, 22(4), 93–113. [DOI] [PubMed] [Google Scholar]
- Elo S, & Kyngas H (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. doi: 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Enthoven AC (2009). Integrated delivery systems: the cure for fragmentation. American Journal of Managed Care, 15, S284–S290. [PubMed] [Google Scholar]
- Fylan B, Armitage G, Naylor D, & Blenkinsopp A (2018). A qualitative study of patient involvement in medicines managment after hospital discharge: an under-recognised source of system resilience. BMJ Qual Saf, 27, 539–546. doi: 10.1136/bmjqs-2017-006813 [DOI] [PubMed] [Google Scholar]
- Halbesleben JRB, Wakefield DS, & Wakefield BJ (2008). Work-arounds in health care settings: Literature review and research agenda. Health Care Manag. Rev, 33, 2–12. [DOI] [PubMed] [Google Scholar]
- Hargadon A (2002). Brokering knowledge: Linking learning and innovation. Research in Organizational Behavior, 24, 41–85. [Google Scholar]
- Kern LM, Reshetnyak E, Colantonio LD, Muntner PM, Rhodes JD, Casalino LP, … Safford MM (2020). Association between patients’ self-reported gaps in care coordination and preventable adverse outcomes: A cross-sectional survey. Journal of General Internal Medicine, 35(12), 3517–3524. doi: 10.1007/s11606-020-06047-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kern LM, Safford MM, Slavin MJ, Makovkina E, Fudl A, Carrillo JE, & Abramson EL (2019). Patients’ and providers’ views on causes and consequences of healthcare fragmentation in the ambulatory setting: a qualitative study. Journal of General Internal Medicine, 34(6), 899–907. doi: 10.1007/s11606-019-04859-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long SJ, Brown KF, Ames D, & Vincent C (2013). What is known about adverse events in older medical hospital inpatients? A systematic review of the literature. International Journal for Quality in Health Care, 25(5), 542–554. [DOI] [PubMed] [Google Scholar]
- Long SJ, & Vincent C (2012). Patient Safety. In Sinclair AJ, Morley JE, & Vellas D (Eds.), Principals and Practices of Geriatric Medicine (pp. 153–170): John Wiley & Sons, Ltd. [Google Scholar]
- Lor M, Crooks N, & Tluczek A (2016). A proposed model of person-, family-, and culture-centered nursing care. Nursing Outlook, 64, 352–366. [DOI] [PubMed] [Google Scholar]
- National Academies of Sciences, E., and Medicine, . (2018). Crossing the Global Quality Chasm: Improving Health Care Worldwide Retrieved from Washington, DC: [PubMed] [Google Scholar]
- O’Hara JK, Aase K, & Waring J (2019). Scaffolding our systems? Patients and families ‘reaching in’ as a source of healthcare resilience. BMJ Qual Saf, 28, 3–6. doi: 10.1136/bmjqs-2017-008216 [DOI] [PubMed] [Google Scholar]
- O’Hara JK, Canfield C, & Aase K (2019). Patient and family perspectives in healthcare studies: A question of morality or logic? Safety Science, 120, 99–106. doi: 10.1016/j.ssci.2019.06.024 [DOI] [Google Scholar]
- Papautsky EL, & Patterson ES (2021). Patients are knowledge workers in the clinical information space. Applied Clinical Information, 12, 133–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perry SJ, Wears RL, & Fairbanks RJ (2012). Human factors and ergonomics in the emergency department. In Carayon P (Ed.), Handbook of Human Factors and Ergonomics in Health Care and Patient Safety (Second ed., pp. 709–722). Boca Raton, FL: Taylor & Francis Group. [Google Scholar]
- Schnitker L, Martin-Khan M, Beattie E, & Gray L (2011). Negative health outcomes and adverse events in older people attending emergency departments: a systematic review. Australian Emergency Nursing Journal, 14, 141–162. doi: 10.1016/j.aenj.2011.04.001 [DOI] [Google Scholar]
- Scholl I, Zill JM, Harter M, & Dirmaier J (2014). An integrative model of patient-centeredness - A systematic review and concept analysis. PLoS ONE, 9(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert CC, Wears RL, Holden RJ, & Hunte GS (2015). Patients as a Source of Resilience. In Braithwaite J (Ed.), Resilient Healthcare : The Resilience of Everyday Clinical Work (Vol. 2, pp. 207–223): Taylor & Francis Group. [Google Scholar]
- Snyder J, & Engstrom J (2016). The antecedents, forms and consequences of patient involvement: A narrative review of the literature. International Journal of Nursing Studies, 53, 351–378. [DOI] [PubMed] [Google Scholar]
- Storm M, Siemsen IMD, Laugaland K, Dyrstad DN, & Aase K (2014). Quality in transitional care of the elderly: Key challenges and relevant improvement measures. International Journal of Integrated Care, 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vincent C, & Amalberti R (2016). Safer Healthcare: Strategies for the Real World: Springer Open. [PubMed] [Google Scholar]
- Ward V, House A, & Hamer S (2009). Knowledge brokering: the missing link in the evidence to action chain? Evidence & Policy, 5(3), 267–279. doi: 10.1332/174426409X463811 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waring J, Currie G, Crompton A, & Bishop S (2013). An exploratory study of knowledge brokering in hospital settings: Facilitating knowledge sharing and learning for patient safety? Social Sciences & Medicine, 98, 79–86. [DOI] [PubMed] [Google Scholar]
- Werner NE, Rutkowski RA, Graske A, Finta MK, Sellers CR, Seshadri S, & Shah MN (2020). Exploring SEIPS 2.0 as a model for analyzing care transitions across work systems. Applied Ergonomics(88). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner NE, Rutkowski RA, Krause S, Barton HJ, Wust K, Hoonakker P, … Cararyon P (2021). Disparate perspectives: Exploring healthcare professionals’ misaligned mental models of older adults’ transitions of care between the emergency department and skilled nursing facility. Applied Ergonomics, 96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiig S, Aase K, Billett S, Canfield C, Nja O, Guise V, … Macrae C (2020). Defining the boundaries and operational concepts of resilience in the resilience in healthcare research program. Health Services Research, 20. [DOI] [PMC free article] [PubMed] [Google Scholar]


