Abstract
Background:
The Jobe test is commonly used to diagnose full-thickness (FT) supraspinatus (SSP) tendon tear. The original Jobe test used single-arm testing, although the double-arm Jobe test has also been used in clinical practice.
Purpose:
To evaluate the reliability, accuracy, and diagnostic value of the single-arm and double-arm Jobe test for diagnosis of FT SSP tear.
Study Design:
Cohort study (diagnosis); Level of evidence, 2.
Methods:
Patients with shoulder pain requiring magnetic resonance imaging (MRI) of the shoulder between March 1, 2021, and March 31, 2022, were enrolled. Each patient underwent both single-arm and double-arm Jobe tests by 2 orthopaedic surgeons independently, and the presence of pain, weakness, or both during the test was documented. Diagnosis of FT SSP tear on MRI scan was used as the gold standard to compare the diagnostic value of the Jobe test. The interrater reliability of the Jobe test, and the inter- and intrarater reliability of the MRI evaluation (patients with vs without FT SSP tear) was performed using the kappa (κ) coefficient.
Results:
A total of 80 patients (57 females [71%]; mean age, 61.46 ± 9.61 years) were included. MRI scans revealed FT SSP tears in 32 (40%) of the patients. Both single- and double-arm Jobe tests had low diagnostic values (accuracy, 46.25% to 60%; sensitivity, 46.9% to 84.4%; specificity, 25% to 66.7%). The single-arm test with weakness revealed the highest sensitivity (84.4%). The double-arm test with weakness plus pain revealed the highest specificity (66.7%). Double-arm testing with pain had the highest accuracy (60%), with the highest positive likelihood ratio (1.5). The interrater reliability of the Jobe test indicated substantial agreement (double-arm vs single-arm, κ = 0.771 and 0.716, respectively, agreement 85%; P < .05). The interrater reliability of MRI scan evaluation of the FT SSP tear indicated substantial agreement (κ = 0.750, agreement 85%; P < .05), while the intrarater reliability indicated almost perfect agreement (κ = 0.917, agreement 96%; P < .05).
Conclusion:
The Jobe test, either single- or double-arm, had low accuracy and diagnostic value in diagnosing FT SSP tear. The concern with a single-arm examination for weakness is that it may be an inappropriate diagnostic test for ruling out FT SSP with 84% sensitivity, while a double-arm examination provides a higher specificity.
Keywords: Jobe test, reliability, rotator cuff tear
The rotator cuff (RC) plays a fundamental role in physiological shoulder motion. RC tears may cause weakness or pain in the shoulder but may also remain completely asymptomatic. 7 Tears of the superior-posterior RC (supraspinatus [SSP] and infraspinatus) are more common compared with tears of the anterior-superior RC (subscapularis and SSP). A variety of clinical tests have been specifically developed for SSP tendon tear. With the Jobe test, as described by Jobe and Moynes in 1982, 13 the determined activity of the SSP muscle can be isolated to some degree with the arm at 90° of abduction, 30° of horizontal flexion, and full internal rotation. Electromyographic records obtained with patients in this position indicate that the SSP is the dominant RC muscle firing during the maneuver. 13
The Jobe or empty-can test is a common physical test for evaluating SSP tear or pathology. The original Jobe test used single-arm testing, with pain during the test suggestive of RC pathology. 13 The Jobe test can be performed with a single-arm or double-arm maneuver. 3,8,12,17 However, studies have no evidence comparing the diagnostic value of single-arm Jobe test and double-arm maneuvers. 3,12,17
The purpose of this study was to evaluate the reliability, accuracy, and diagnostic value of the single-arm and the double-arm Jobe test for diagnosis of full-thickness (FT) SSP tear. Our hypothesis was that the double-arm Jobe test would be more accurate, as the imbalance of the periscapular muscle during the single-arm test may result in a false-positive (FP) result.
Methods
This was a cross-sectional study of 80 consecutive shoulder pain patients prospectively enrolled from a single hospital between March 1, 2021, and March 31, 2022. The study was conducted after obtaining approval from the Human Research Ethics Committee of Thammasat University, and informed consent was obtained from all participants. Inclusion criteria included patients over 45 years of age with more than 4 weeks of symptoms (shoulder pain or weakness), positive subacromial impingement sign on examination (Neer impingement sign or Hawkins-Kennedy test), no significant shoulder stiffness (passive forward elevation >120°, external rotation >45°), and shoulder magnetic resonance imaging (MRI) scan. Excluded were patients with current fractures around the upper extremity, previous shoulder surgery, bilateral shoulder pain, calcific tendinitis of the shoulder on imaging, significant weakness or pain from cervical spine pathologies, presence of pseudoparalysis, and patients who had received shoulder or subacromial injection within 3 months.
Data Collection and Jobe Test
We collected baseline patient characteristics (age, sex, body mass index), as well as symptom duration, affected side, dominant arm, pain visual analog scale score, and Western Ontario Rotator Cuff Index score. All patients underwent axial, coronal, and sagittal T2-weighted fat-saturated imaging performed on 3-T MRI to evaluate the pathology of the affected shoulder. Finally, all patients were examined in our outpatient orthopedic clinic by 2 orthopedic surgeons (A.A. and P.B.). The 2 examiners, who were blinded to the MRI results, independently examined all patients in 5- to 10-minute intervals. During the examination, conducted with the patient in the sitting position, the SSP of the affected shoulder was evaluated using the Jobe test in a fixed pattern: first the double-arm test, followed by the single-arm test. For each test, muscle strength was measured by manual compression (Figure 1). The presence of weakness, pain, or weakness plus pain during the test was documented. The interrater reliability of the examiner findings was calculated.
Figure 1.
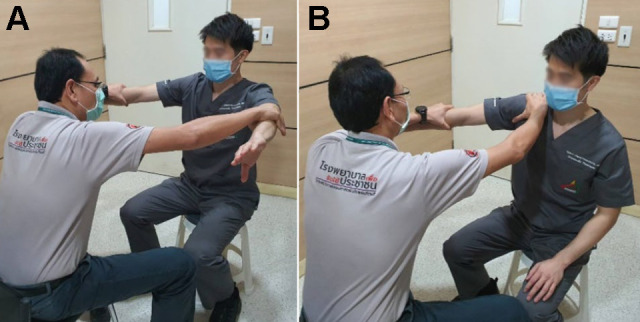
Jobe test conducted with the patient in the sitting position with the affected arm at 90° of abduction, 30° of horizontal flexion, and full internal rotation. The tests were measured by manual compression. (A) Double-arm Jobe test and (B) single-arm Jobe test of the right shoulder.
MRI Evaluation
The process of reviewing the MRI scans required a picture archiving and communication system workstation. MRI was used as the gold standard for definite diagnosis of FT SSP tear by 2 reviewers, a fellowship-trained musculoskeletal radiologist (W.S.B.) and an orthopaedic surgeon (A.A.), who independently categorized the patients into those with and those without FT SSP. The interrater and intrarater reliability of the MRI interpretations was assessed. To evaluate intrarater reliability, the orthopaedic surgeon (A.A.) re-evaluated the patients after 2 weeks.
The integrity of the RC was also evaluated on MRI scans and was categorized as RC syndrome/bursitis, partial-thickness RC tear (including low-grade tear [≤6 mm] and high-grade tear [>6 mm]), 5 and FT RC tear. 10 Some MRI scans from the study population are shown in Figure 2.
Figure 2.
Coronal T2-weighted MRI sequences of the left shoulder of different patients. (A) SSP tendinopathy with subacromial bursitis (red arrow). (B) Bursal side partial-thickness tear of SSP (yellow arrow). (C) Full-thickness tear of SSP (blue arrow). MRI, magnetic resonance imaging; SSP, supraspinatus
Statistical Analysis
The sample size was calculated a priori by assuming a sensitivity and specificity of at least 0.85 and a CI of 95%, resulting in a sample size of at least 53 patients with a power of 0.9 according to the McNemar method. An adjusted sample size with a 70% incidence of no FT SSP tear resulted in a study sample of at least 76 patients.
All statistical analyses were performed using the STATA software for Windows (Version 17; Stata Corp LP). To evaluate the diagnostic value of the Jobe test, the results of the clinical examinations were compared with the MRI scan results. Diagnostic value was evaluated in terms of test type (single-arm, double-arm, or combined single- and double-arm) and presence of weakness, pain, or weakness plus pain. The statistical analysis included the determination of the sensitivity, specificity, accuracy, positive likelihood ratio (LR+), negative likelihood ratio (LR-), positive predictive value (PPV), negative predictive value (NPV), and the area under the receiver operating characteristic (ROC) curve (AUC). 3 These parameters were calculated as follows:
Sensitivity. The sensitivity was used to describe the percentage of times in which a test was positive in patients with FT SSP tear. It was calculated by dividing the number of the true-positive (TP) tests by the sum of the false-negative (FN) and TP tests: TP/(TP + FN).
Specificity. The specificity indicated the percentage of negative tests in patients who did not have FT SSP tears (SSP tendinosis, tendinopathy, or partial thickness tear). It was determined by dividing the number of the true-negative (TN) tests by the sum of the FP and TN tests: TN/(TN + FP).
Positive Predictive Value. The PPV evaluated the probability of the positive Jobe test in patients with an MRI scan-confirmed FT SSP tear and was calculated by dividing the number of TP tests by the sum of the TP and FP tests: TP/(TP + FP).
Negative Predictive Value. The NPV evaluated the probability of a negative Jobe test in patients with no FT SSP tear on MRI and was calculated as the number of TN tests divided by the sum of the TN and FN tests: TN/(TN + FN)
Accuracy. The accuracy was defined as the proportion of correctly diagnosed patients with FT SSP tears among all the participants. The accuracy was found by dividing the number of TP and TN tests by the total number of tests: (TP + TN)/(TP + TN + FP + FN).
Likelihood Ratio. The likelihood ratio was defined as the percentage of expected test results in patients with FT SSP tear compared with the percentage of patients without FT SSP tear. It was calculated according to the following formulas: LR+ = Sensitivity/(1 - Specificity) and LR- = Specificity/(1 - Sensitivity).
Area Under the ROC Curve. ROC curves and the AUC were calculated to evaluate the accuracy of the Jobe test. The AUC has a value between 0 and 1. The closer AUC is to 1, the better the overall diagnostic performance of the test, and a test with an AUC value of 1 is perfectly accurate. 16
The interrater reliability of the Jobe tests and the inter- and intrarater reliabilities of the MRI evaluations were calculated using the kappa (κ) coefficient, 15 in which κ < 0.00 was considered poor strength of agreement; 0.00 to 0.20, slight; 0.21 to 0.40, fair; 0.41 to 0.60, moderate; 0.61 to 0.80, substantial; and 0.81 to 1.00, almost perfect. 15 The percentage agreement between the 2 raters was also calculated.
Results
A total of 80 patients were included in the study (71% female patients; mean age, 61.46 ± 9.61 years). The mean duration of shoulder pain was 9 ± 8.55 months. FT SSP tear on MRI scan was detected in 32 patients (40%). The patient characteristics are shown in Table 1.
Table 1.
Characteristics of the Study Patients (N = 80) a
| Characteristic | Value |
|---|---|
| Age, y | 61.46 ± 9.61 |
| Sex | |
| Female | 57 (71.25%) |
| Male | 23 (28.75%) |
| Body mass index | 24.64 ± 3.49 |
| Duration of symptoms, mo | 9.01 ± 8.55 |
| Affected side | |
| Left | 41 (51.25%) |
| Right | 39 (48.75%) |
| Dominant arm | |
| Left | 15 (18.75%) |
| Right | 65 (81.25%) |
| VAS pain | 6.19 ± 2.21 |
| WORC | 54.65 ± 22.06 |
| MRI diagnosis | |
| RC syndrome, subacromial bursitis | 2 (2.5%) |
| Partial-thickness RC tear | 46 (57.5%) |
| Full-thickness RC tear | |
| Small (<1 cm) | 2 (2.5%) |
| Medium (1-3 cm) | 23 (28.75%) |
| Large to massive (>3 cm) | 7 (8.75%) |
a Data are reported as mean ± SD or n (%). MRI, Magnetic resonance imaging; RC, rotator cuff; VAS, visual analog scale; WORC, Western Ontario Rotator Cuff Index.
Overall, the sensitivity of each type of Jobe test ranged from 46.9% to 84.4%, with a specificity from 25% to 66.7%. The accuracy of the Jobe test, either single-arm or double-arm, with weakness, pain, or weakness and pain, ranged from 46.25% to 60%. The single-arm test with weakness had the highest sensitivity, followed by single-arm test with pain and single-arm test with weakness plus pain (84.4%, 78.1%, and 78.1%, respectively). The double-arm test with weakness plus pain had the highest specificity, followed by the double-arm test with weakness (66.7% and 64.6, respectively). Double-arm testing with pain had the highest accuracy of 60% with the highest LR+ of 1.5. For all values, the combined single- and double-arm Jobe test showed the same results as for the double-arm test alone. The summarized diagnostic values of the Jobe tests are shown in Table 2.
Table 2.
Diagnostic Value of the Single-arm, Double-arm, and Combined Jobe Test a
| Jobe Test | Sensitivity, % | Specificity, % | Accuracy, % | AUC | LR+ | LR- | PPV, % | NPV, % |
|---|---|---|---|---|---|---|---|---|
| Weakness | ||||||||
| Single-arm | 84.4 | 35.4 | 55 | 0.60 | 1.31 | 0.44 | 46.6 | 77.3 |
| Double-arm | 50.0 | 64.6 | 58.75 | 0.57 | 1.41 | 0.77 | 48.5 | 66.0 |
| Combined | 50.0 | 64.6 | 58.75 | 0.57 | 1.41 | 0.77 | 48.5 | 66.0 |
| Pain | ||||||||
| Single-arm | 78.1 | 25.0 | 46.25 | 0.52 | 1.04 | 0.88 | 41.0 | 63.2 |
| Double-arm | 75.0 | 50.0 | 60 | 0.63 | 1.50 | 0.50 | 50.0 | 75.0 |
| Combined | 75.0 | 50.0 | 60 | 0.63 | 1.50 | 0.50 | 50.0 | 75.0 |
| Weakness and pain | ||||||||
| Single-arm | 78.1 | 41.7 | 56.25 | 0.60 | 1.34 | 0.53 | 47.2 | 74.1 |
| Double-arm | 46.9 | 66.7 | 58.75 | 0.57 | 1.41 | 0.80 | 48.4 | 65.3 |
| Combined | 46.9 | 66.7 | 58.75 | 0.57 | 1.41 | 0.80 | 48.4 | 65.3 |
a Results are based on the prevalence of full-thickness superior-posterior RC tear of 40% in the study population. AUC, area under the receiver operating characteristic curve; LR+, positive likelihood ratio; LR-, negative likelihood ratio; NPV, negative predictive value; PPV, positive predictive value; RC, rotator cuff.
The interrater reliability of the Jobe test indicated substantial agreement for both the double-arm test (κ = 0.771) and the single-arm test (κ = 0.716) (85% agreement; P < .05). The interrater reliability of MRI scan evaluation of the FT SSP tear indicated substantial agreement (κ = 0.750, 85% agreement; P < .05), while intrarater reliability was almost perfect (κ = 0.917, 96% agreement; P < .05).
Discussion
The most important finding of the present study was that single-arm Jobe test with weakness revealed the highest sensitivity of 84.4%. Double-arm Jobe test with weakness plus pain revealed the highest specificity of 66.7%. Double-arm testing with pain had the highest accuracy of 60% with the highest LR+ of 1.5. The overall accuracy of the Jobe test in the diagnosis of FT SSP tear was 46.25% to 60%.
This study revealed the low diagnostic values of the Jobe test in FT SSP tear. Physical examination, augmented by MRI or ultrasound scans, certainly plays an important role in the diagnosis of RC tears. Various clinical tests have been developed to assess the SSP tendon tear. Several studies have investigated the diagnostic value of these tests, although different symptoms, such as pain, weakness, or both, were used to interpret the results. It is still unclear which of these symptoms is more accurate. 1,2,8 –11
The diagnosis of SSP tendon tear has involved many diagnostic physical tests. The Jobe, or empty can, test is a common physical test evaluating the SSP tear or pathology. The original Jobe test used single-arm testing, while pain during the test suggested RC pathology. 13 Some reported the positive test with pain or weakness indicating SSP pathology. 4,8 The Jobe test can be performed with a single-arm or double-arm maneuver, with reported a sensitivity of 54% to 96% and a specificity of 46% to 68%. 3,8,12,17
Itoi et al 8 determined the clinical usefulness of the full can (arm in 90° of elevation in the scapular plane and 45° of external rotation) and empty can (arm in 90° of elevation in the scapular plane and full internal rotation) tests for detecting of SSP tear in 143 shoulders. The empty can test with pain, weakness, and both pain and weakness showed a sensitivity of 63%, 77%, and 89%, respectively, whereas the specificity was 55%, 68%, and 50%, respectively. The authors concluded that muscle weakness was indicative of SSP tear in the empty can test. Sgroi et al 17 analyzed the diagnostic value of 7 clinical tests for the diagnosis of SSP tears in 115 patients. The results of the empty can test with pain, weakness, and both pain and weakness showed a sensitivity of 54%, 90%, and 96%, respectively, whereas the specificity was 61%, 46%, and 31%, respectively. A systematic review revealed the pooled estimated sensitivity of the Jobe test was 0.77 (CI, 0.67-0.85) and the specificity was 0.67 (CI, 0.59-0.73) in 5 eligible studies. 14 This finding was similar to our study and was a confirmation of the low diagnostic accuracy of the Jobe test alone in the diagnosis of posterosuperior RC tears. 6,12,14,18
The detection of RC tears affects treatment strategies (ie, physical therapy, injection, surgical intervention). Due to the low diagnostic values of the Jobe test and the other clinical tests in FT SSP tear, shoulder pain patients older than 50 years without significant shoulder stiffness may require a high level of suspicion or definitive determination of an RC tear. Then, other diagnostic methods including plain radiographs, ultrasound, or MRI scan should be considered.
According to our hypothesis, the imbalance of the periscapular muscle during performance of the single-arm Jobe test may result in an FP of the test, while the double-arm Jobe test may be more accurate. The single-arm testing had higher sensitivity compared with double-arm testing in all tests (weakness, pain, or weakness and pain), while having lower specificity, accuracy, and LR+. This finding supported the view that the single-arm Jobe test may result in an FP result and may lead to overestimation of the SSP tear.
The diagnostic accuracy of the combined single- and double-arm Jobe test revealed the same results as double-arm testing alone. This finding supported our hypothesis that periscapular muscle balance in the double-arm test would lead to more accuracy than the single-arm test; thus, if the double-arm test revealed a positive result, the single-arm test would also have a positive result. The combination of single- and double-arm tests did not increase the yield of diagnosis of FT SSP tear.
The interrater reliability κ statistic was 0.716 for the single-arm test and 0.771 for the double-arm test, which was in the range of substantial agreement (0.61-0.80), thus we might require a better clinical test in the future.
Limitations
Our study has some limitations. First, selection bias must be considered because the prevalence of FT SSP tears in our investigating center (positioning of tertiary care and shoulder center in our region) was high, at up to 40%. Second, clinical examinations were not sequential random between single-arm and double-arm tests. We started with a double-arm and then a single-arm test in all participants, this may create an FP for later tests after the pain was aggravated (although we waited about 5 minutes). Third, we classified the patients into only 2 groups (FT SSP tear and no FT SSP tear) and did not differentiate among low-grade and high-grade partial-thickness SSP tear groups. The high-grade SSP tear, which has clinical meaning, was recruited in the no FT SSP tear group, which may alter the results. Fourth, the sample size in our study compared with previous studies was relatively low. Fifth, MRI scan was used as the gold standard in RC tear diagnosis with substantial interrater agreement and almost perfect agreement of intrarater reliability. Diagnostic arthroscopy is still the gold standard for making the diagnosis. Sixth, the Jobe test was conducted in a sitting rather than a standing position as in the original test. We chose the sitting position, which might have more balance and stability between the left and right upper limbs during a test in elderly patients. Seventh, we did not evaluate the intrarater reliability of the Jobe test. The patients received treatment (such as injection, physical therapy, or medications) after the test, so the results of Jobe test might be different in the subsequent weeks. Last, combining the single-arm and double-arm Jobe test did not improve diagnostic values compared with the single clinical test.
Conclusion
Jobe test, either single- or double-arm, had low accuracy and diagnostic value in diagnosing superior-posterior RC FT tear. Better clinical testing or other diagnostic methods such as ultrasound or MRI scans should be considered with a high suspicion of the RC tear. The concern with a single-arm examination for weakness is that it may be an inappropriate diagnostic test for ruling out FT SSP with 84% sensitivity, while a double-arm examination provides higher specificity.
Acknowledgment
The authors thank the Department of Orthopaedics, Faculty of Medicine, Thammasat University and Thammasat University Hospital for their kind support.
Footnotes
Final revision submitted March 16, 2023; accepted April 14, 2023.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Human Research Ethics Committee of Thammasat University (MTU-EC-OT-0-273/63).
References
- 1. Ackmann T, Schneider KN, Schorn D, Rickert C, Gosheger C, Liem D. Comparison of efficacy of supraspinatus tendon tears diagnostic tests: a prospective study on the “full-can,” the “empty-can,” and the “Whipple” tests. Musculoskelet Surg. 2021;105(2):149–153. [DOI] [PubMed] [Google Scholar]
- 2. Anauate Nicolao F, Yazigi Junior JA, Matsunaga FT, et al. Comparing shoulder maneuvers to magnetic resonance imaging and arthroscopic findings in patients with supraspinatus tears. World J Orthop. 2022;13(1):102–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Brockmeyer M, Schmitt C, Haupert A, Kohn D, Lorbach O. Limited diagnostic accuracy of magnetic resonance imaging and clinical tests for detecting partial-thickness tears of the rotator cuff. Arch Orthop Trauma Surg. 2017;137(12):1719–1724. [DOI] [PubMed] [Google Scholar]
- 4. Cotter EJ, Hannon CP, Christian D, Frank RM, Bach BR, Jr. Comprehensive examination of the athlete’s shoulder. Sports Health. 2018;10(4):366–375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ellman H. Diagnosis and treatment of incomplete rotator cuff tears. Clin Orthop Relat Res. 1990;(254):64–74. [PubMed] [Google Scholar]
- 6. Hegedus EJ, Goode AP, Cook CE, et al. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012;46(14):964–978. [DOI] [PubMed] [Google Scholar]
- 7. Hinsley H, Ganderton C, Arden NK, Carr AJ. Prevalence of rotator cuff tendon tears and symptoms in a Chingford general population cohort, and the resultant impact on UK health services: a cross-sectional observational study. BMJ Open. 2022;12(9):e059175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Itoi E, Kido T, Sano A, Urayama M, Sato K. Which is more useful, the “full can test” or the “empty can test,” in detecting the torn supraspinatus tendon? Am J Sports Med. 1999;27(1):65–68. [DOI] [PubMed] [Google Scholar]
- 9. Itoi E, Minagawa H, Yamamoto N, Seki N, Abe H. Are pain location and physical examinations useful in locating a tear site of the rotator cuff? Am J Sports Med. 2006;34(2):256–264. [DOI] [PubMed] [Google Scholar]
- 10. Jain NB, Collins J, Newman JS, Katz JN, Losina E, Higgins LD. Reliability of magnetic resonance imaging assessment of rotator cuff: the ROW study. PM R. 2015;7(3):245–254.e243; quiz 254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Jain NB, Fan R, Higgins LD, Kuhn JE, Ayers GD. Does my patient with shoulder pain have a rotator cuff tear? A predictive model from the ROW cohort. Orthop J Sports Med. 2018;6(7):2325967118784897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Jain NB, Luz J, Higgins LD, Dong Yan, Warner JPJ, Matzkin E, Katz JN. The diagnostic accuracy of special tests for rotator cuff tear: the ROW cohort study. Am J Phys Med Rehabil. 2017;96(3):176–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jobe FW, Moynes DR. Delineation of diagnostic criteria and a rehabilitation program for rotator cuff injuries. Am J Sports Med. 1982;10(6):336–339. [DOI] [PubMed] [Google Scholar]
- 14. Lädermann A, Meynard T, Denard PJ, Ibrahim M, Saffarini M, Collin P. Reliable diagnosis of posterosuperior rotator cuff tears require a combination of clinical tests. Knee Surg Sports Traumatol Arthrosc. 2021;29(7):2118–2133. [DOI] [PubMed] [Google Scholar]
- 15. McHugh ML. Interrater reliability: the kappa statistic. Biochem Med (Zagreb). 2012;22(3):276–282. [PMC free article] [PubMed] [Google Scholar]
- 16. Park SH, Goo JM, Jo CH. Receiver operating characteristic curve: practical review for radiologists. Korean J Radiol. 2004;5(1):11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sgroi M, Loitsch T, Reichel H, Kappe T. Diagnostic value of clinical tests for supraspinatus tendon tears. Arthroscopy. 2018;34(8):2326–2333. [DOI] [PubMed] [Google Scholar]
- 18. van Kampen DA, van den Berg T, van der Woude HJ, et al. The diagnostic value of the combination of patient characteristics, history, and clinical shoulder tests for the diagnosis of rotator cuff tear. J Orthop Surg Res. 2014;9:70. [DOI] [PMC free article] [PubMed] [Google Scholar]



