Abstract
A series of recombinant viruses were constructed using infectious cDNA clones of the virulent J1’73 (large plaque phenotype) and the avirulent H/3’76 (small plaque phenotype) strains of swine vesicular disease virus to identify the genetic determinants of pathogenicity and plaque phenotype. Both traits could be mapped to the region between nucleotides (nt) 2233 and 3368 corresponding to the C terminus of VP3, the whole of VP1, and the N terminus of 2A. In this region, there are eight nucleotide differences leading to amino acid changes between the J1’73 and the H/3’76 strains. Site-directed mutagenesis of individual nucleotides from the virulent to the avirulent genotype and vice versa indicated that A at nt 2832, encoding glycine at VP1-132, and G at nt 3355, encoding arginine at 2APRO-20, correlated with a large-plaque phenotype and virulence in pigs, irrespective of the origin of the remainder of the genome. Of these two sites, 2APRO-20 appeared to be the dominant determinant for the large-plaque phenotype but further studies are required to elucidate their relative importance for virulence in pigs.
Swine vesicular disease (SVD) was first observed in Italy in 1966 (37). It is an infectious disease of pigs characterized by the appearance of vesicles on the coronary bands of the feet, on the legs, and less commonly on the snout and tongue. SVD is classified as a List A disease by the Office International des Epizooties (OIE) because the lesions produced by SVD virus (SVDV) are indistinguishable from those caused by foot-and-mouth disease virus. With the exception of Italy, SVD was eliminated from Europe during the 1970s and 1980s by eradication campaigns in those countries in which the disease occurred. However, during the early 1990s, the incidence of SVD increased in Europe. Outbreaks continue to occur in Italy, and the disease is thought still to be present in China, Hong Kong, and possibly other countries in Asia. Once introduced, SVD can be a difficult disease to eradicate and control is vital in countries which are free of the vesicular diseases of swine, i.e., foot-and-mouth disease, SVD and vesicular stomatitis.
SVDV, a member of the genus Enterovirus within the family Picornaviridae, contains a single-strand RNA genome of positive sense surrounded by a protein capsid comprising four proteins: VP1, VP2, VP3, and VP4. The RNA genome is composed of approximately 7,400 nucleotides (nt) (13, 14, 46) and contains 5′ and 3′ noncoding regions (5′ and 3′-NCR). SVDV is antigenically related to the human enterovirus coxsackievirus B5 (CVB5) (6, 11), but the two viruses can be distinguished by cross-neutralization and immunodiffusion tests (6, 7). Recently, the antigenic sites on the capsid proteins of SVDV were identified (19) by using monoclonal antibodies and neutralization-resistant mutant viruses. The locations of these sites on SVDV are similar to those of poliovirus (PV).
Since the first construction of an infectious clone for PV by Racaniello and Baltimore (41), several full-length infectious cDNA clones have been constructed of other picornaviruses (9, 17, 21). These infectious clones have been used as valuable tools for analyzing the genomic determinants of pathogenicity and for the development of recombinant vaccines (23, 25, 38, 44, 50, 51). In poliovirus, each of the three Sabin strains has a major site of attenuation located in the 5′-NCR within the internal ribosome entry site (IRES) (20, 31, 33, 40, 51). In addition, other major sites in the coding region of the capsid proteins were also identified as virulence determinants in three serotypes of PV (4, 45, 48, 51). In coxsackievirus, a pancreovirulent CVB4 and avirulent CVB4 strain were used to map the genetic determinants for murine pancreovirulence to Thr-129 of VP1 (8) and, to a lesser extent, Arg-16 of VP4 (42). Likewise, cardiovirulence in CVB3 is linked to nt 234 in the 5′-NCR (50).
For picornaviruses, there is some correlation between virulence and plaque size. Generally, large-plaque phenotypes are more virulent than small-plaque phenotypes. For example, small plaque size can be used to differentiate attenuated poliovirus vaccine strains from virulent strains (36), and some reports have described a correlation between virulence and plaque size for coxsackieviruses (43, 52). Likewise for SVDV, the virulent J1’73 strain shows a large plaque phenotype, while the avirulent H/3’76 strain shows a small-plaque phenotype on IBRS-2 cells (18). There are a total of 78 differences in the nucleotide sequence between the virulent and avirulent strains of SVDV (14). Of these 78 nucleotide substitutions, 10 are found in the 5′ noncoding region, 22 result in amino acid changes in the coding region, and 46 are silent. Infectious cDNA clones of the virulent J1’73 strain and the avirulent H/3’76 strain have been generated, and the characteristics of the recovered viruses have been shown to be the same as the respective parental strain (18). In the study reported here, the determinants of pathogenicity in the genome of SVDV were mapped, and their relationship to plaque size was investigated by the generation of chimeric and site-directed mutant viruses between the cDNA clones of the virulent and avirulent strains.
MATERIALS AND METHODS
Construction of recombinant viruses.
Full-length infectious cDNA clones of the avirulent SVDV H/3’76 genome, pSVLS00 (15), and the virulent SVDV J1’73 genome, pSVLSJ1, were prepared (18) and used for the construction of recombinant cDNAs. A series of recombinants were prepared by exchanging the corresponding DNA fragments digested with several restriction enzymes, SacI (nt 748), Bst1107I (nt 2233), and BssHII (nt 3368) (Fig. 1). All infectious cDNA constructs were verified by restriction endonuclease mapping. DNA transfection was performed as described by Kanno et al. (18). Cos7 cells at between 10 and 30% confluence were transfected by using the CellPhect transfection kit (Pharmacia Biotech, Uppsala, Sweden) as recommended by the manufacturer, and the culture was incubated at 37°C for 5 days. The supernatant fluid was then transferred to a monolayer of IBRS-2 cells and incubated until a distinct cytopathic effect was observed.
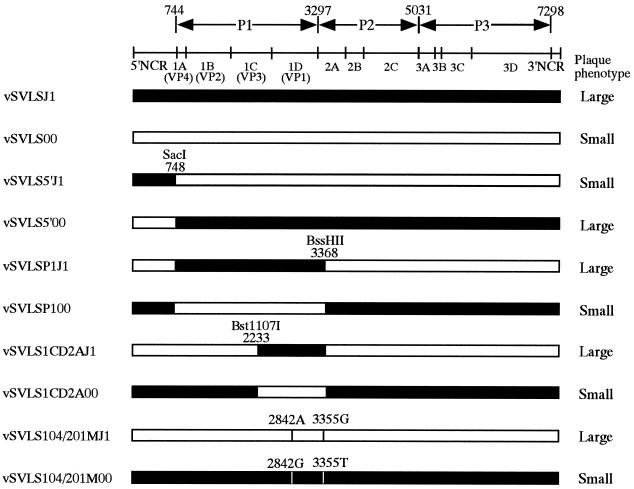
FIG. 1.
Construction and plaque phenotype of recombinant and mutant viruses. At the top of the figure is a genetic map of SVDV genomic RNA. The viruses, vSVLSJ1 (black box) and vSVLS00 (white box), were recovered from infectious cDNAs of the virulent J1’73 strain and the avirulent H/3’76 strain, respectively. Recombinant clones were constructed by using the restriction sites shown. The name of each virus is shown on the left, and its plaque phenotype is shown on the right.
Site-directed mutagenesis.
Site-directed mutagenesis in the Bst1107I (2233)-BssHII (3368) region was performed by subcloning the region into the plasmid M13 and using the Mutagene kit (Bio-Rad). After sequence analysis, mutated Bst1107I-BssHII fragments were reintegrated into infectious clones of pSVLSJ1 or pSVLS00. Viruses were recovered after transfection of Cos7 cells as described above, and mutated sites were verified by sequencing.
Plaque morphology.
The recovered viruses vSVLSJ1 and vSVLS00, 6 recombinant viruses (vSVLS5’J1, vSVLS5’00, vSVLSP1J1, vSVLSP100, vSVLS1CD2AJ1, and vSVLS1CD2A00), and 18 site-directed mutant viruses (Fig. 2) were inoculated onto IBRS-2 cell monolayers, and the cells were overlaid with agar after adsorption. After 2 days at 37°C, the monolayers were fixed with 10% formalin and stained with crystal violet to visualize plaques.
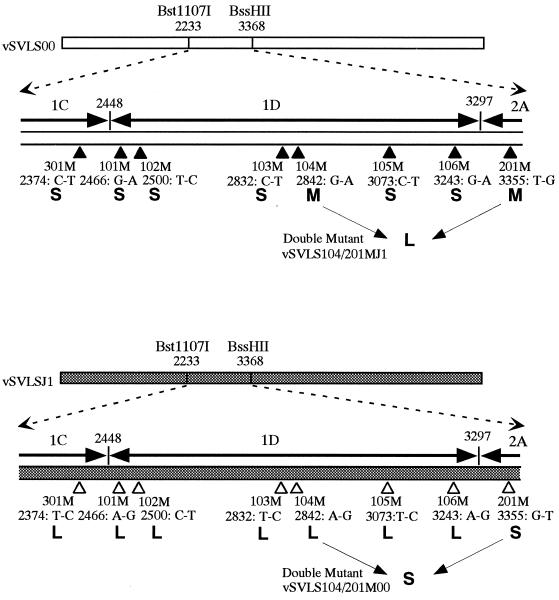
FIG. 2.
Schematic representation of site-directed mutant viruses and their respective plaque phenotypes. In the Bst1107I-BssHII (nt 2233 to 3368) region, which corresponds to the C terminus of VP3, the whole of VP1, and the N terminus of 2A, there are eight nucleotide differences leading to amino acid changes between vSVLSJ1 and vSVLS00. Site-directed mutagenesis in this region was performed by subcloning into the plasmid M13 and by using the Mutagene Kit (Bio-Rad). L, large-plaque phenotype; S, small-plaque phenotype; M, intermediate phenotype.
One-step growth.
One-step growth curves for the viruses vSVLSJ1, vSVLS00, vSVLS104/201MJ1, and vSVLS104/201M00 were performed on IBRS-2 cells with a multiplicity of infection of 10 for each virus, as previously described (18). The culture supernatant was harvested at various times after inoculation, and the virus titer was determined by standard plaque assay.
Experimental infection of pigs.
The six recombinant viruses vSVLS5’J1, vSVLS5’00, vSVLSP1J1, vSVLSP100, vSVLS1CD2AJ1, and vSVLS1CD2A00 and the site-directed mutant viruses, vSVLS104/201MJ1 and vSVLS104/201M00 were inoculated into pigs to examine the pathogenicity of each virus. For virulence controls, pigs were also inoculated with the parental viruses vSVLSJ1 and vSVLS00. A total of 50 conventionally raised pigs were used that were seronegative for antibody to SVDV prior to infection. On the first day of the experiment, pigs were inoculated with 108 50% tissue culture infective doses (TCID50) of the respective virus in 1 ml of tissue culture fluid (see Table 2 for details) by intradermal inoculation into the bulb of the heel of the right foreleg. After inoculation, pigs were observed for the appearance of clinical signs, and their rectal temperatures were measured daily. The severity of clinical signs was scored as described by Kanno et al. (18) by using the lesion scoring system of Mann (32), in which a pig with severe lesions at all predilection sites, i.e., coronary band, heel, supernumerary digit, leg, tongue, and snout, has a score of 100. Serum was collected periodically throughout the experiment and examined for SVDV-specific neutralizing antibody by the virus neutralization test as previously described (18).
TABLE 2.
Experimental infection of pigs with SVDVsa
| Virus | Dose (TCID50) | No. of pigsb | Mean lesion scorec (range) | Seroconversiond
|
|
|---|---|---|---|---|---|
| No. seropositive/no. tested | Mean titer (range)e | ||||
| vSVLSJ1 | 108.0 | 5 (TK21–25) | 12.4 (4–29) | 5/5 | 2.59 (2.11–3.16) |
| vSVLS00 | 108.3 | 5 (TK26–30) | 0 | 2/5 | 0.75 (<0.6–0.75) |
| vSVLS5’J1 | 108.0 | 5 (TC91–95) | 0.4 (0–2) | 1/5 | 1.04 (0.72–1.44) |
| vSVLS5’00 | 108.0 | 5 (TC86–90) | 30.8 (18–45) | 5/5 | 2.28 (2.17–2.53) |
| vSVLSP1J1 | 108.3 | 5 (TK65–69) | 11.6 (4–24) | 5/5 | 2.23 (2.11–2.41) |
| vSVLSP100 | 107.5 | 5 (TK70–74) | 0 | 4/5 | 1.14 (1.05–1.51) |
| vSVLS1CD2AJ1 | 108.5 | 5 (TK75–79) | 19.4 (5–27) | 5/5 | 2.59 (2.41–2.71) |
| vSVLS1CD2A00 | 108.2 | 5 (TK80–84) | 0 | 3/5 | 0.99 (0.90–1.05) |
| vSVLS104/201MJ1 | 108.3 | 5 (TK31–35) | 8.4 (7–12) | 5/5 | 1.87 (1.51–2.11) |
| vSVLS104/201M00 | 107.9 | 5 (TK36–40) | 0 | 4/5 | 2.11 (<0.6–2.26) |
All animals were inoculated intradermally with a 1-ml injection into the bulb of the heel. Each animal weighed 20 kg.
Five animals per group. The animal designations are in parentheses.
Scored at 10 days postinfection.
Seroconversion is defined as a ≥4-fold rise in the titer at any stage after infection.
Mean titer at 14 days postinfection (reciprocal log10).
Sequencing of viruses isolated from pigs.
SVDVs or viral RNA were recovered from each group of pigs. Where lesions were present, a clarified suspension of homogenized epithelium was inoculated onto IBRS-2 cell monolayers. In the case of subclinical infection, viruses were isolated from feces or tonsillar swabs by using standard techniques. Sequencing was determined for the 5′-NCR for viruses isolated from pigs infected with vSVLS5’J1 and vSVLS5’00 and for the 1D-2A region for viruses isolated from all other groups. Reverse transcriptase PCR was performed with primers appropriate to the region of interest (5), and the sequence of the PCR product was determined by using the Fmol Sequencing Kit (Promega, Madison, Wis.) kit according to the manufacturer’s instructions.
RESULTS
Construction of recombinant viruses and determination of their plaque phenotype.
Recombinant SVDVs, constructed by exchanging corresponding genomic regions between the virulent J1’73 and avirulent H/3’76 strain cDNAs (pSVLSJ1 and pSVLS00), were used to map the determinants for plaque size and virus pathogenicity (Fig. 1 and see Table 2). Substitution of the 5′-NCRs between the virulent and avirulent strains had no effect on plaque size (Fig. 1). The chimera comprising the first 748 nt, 743 nt of the 5′-NCR, and the first 5 nt of VP4 of the virulent strain attached to the remainder of the genome of avirulent strain (vSVLS5’J1) retained the small-plaque phenotype of the avirulent parental strain. Conversely, when the first 748 nt of the virulent strain were replaced with those of the avirulent strain (vSVLS5’00), no reduction in plaque size was observed compared to the parental virulent strain. Substitution of almost the entire P1 region, together with the first 71 nt of 2A, resulted in exchange of plaque phenotype. Chimera vSVLSP1J1, which was constructed by replacing the region between nt 748 and 3368 of the avirulent strain with the corresponding region of the virulent strain, changed the plaque phenotype from small to large. Correspondingly, substituting the same region of the virulent strain with that of the avirulent strain changed the plaque phenotype from large to small (vSVLSP100). It was possible to identify more precisely that the region responsible for plaque phenotype was the 1C/1D/2A region by exchanging the section of the genome spanning nt 2233 to 3368 between the virulent and avirulent strains (Fig. 1). Substitution of this region of the avirulent strain with that of the virulent strain conferred a large-plaque phenotype (vSVLS1CD2AJ1), and replacement of this region in the virulent strain by the corresponding region of the avirulent strain altered the plaque phenotype from large to small (vSVLS1CD2A00).
Identification of amino acids responsible for plaque phenotype by site-directed mutagenesis.
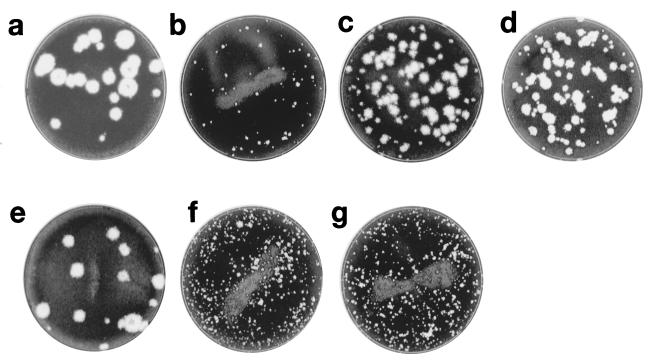
vSVLSJ1 differs from vSVLS00 by 15 nt between nt 2233 and 3368 in the 1D/1C/2A region. Of these, eight result in amino acid changes: one in VP3, six in VP1, and one in 2A (Table 1). To map more precisely the determinants of plaque size, mutant viruses were produced by site-directed mutagenesis in which single-amino-acid substitutions were made that changed the residue from that found in the virulent strain to that of the avirulent strain and vice versa (Fig. 2). For mutants derived from the avirulent strain, single changes at nt 2842, substituting A for G corresponding to Gln for Arg (vSVLS104MJ1), or at nt 3355, substituting G for T corresponding to Arg for Ile (vSVLS201MJ1), resulted in some increase in plaque size compared to the parental avirulent strain (Fig. 2 and 3). A virus mutated at both these sites, vSVLS104/201MJ1 showed the same large-plaque phenotype as the vSVLSJ1 virulent strain (Fig. 1, 2, and 3). For the corresponding single mutants derived from the virulent strain, only a substitution from G to T at nt 3355, corresponding to an Arg-to-Ile change within the 2A protease (vSVLS201M00), resulted in a change to a small-plaque phenotype (Fig. 2 and 3). The plaque phenotype was unchanged in other single-site mutants (Fig. 2). A double mutant changed at both the 104M and the 201M sites, vSVLS104/201M00, had a small-plaque phenotype similar to that of the avirulent vSVLS00 strain and of the single 201M site mutant vSVLS201M00 (Fig. 2 and 3).
TABLE 1.
Nucleotide and amino acid sequence differences in the Bst11107I-BssHII region between vSVLSJ1 and vSVLS00
| Nucleotide no. | vSVLSJ1a
|
vSVLS00a
|
Amino acid no. | Mutation siteb | ||
|---|---|---|---|---|---|---|
| nt | aa | nt | aa | |||
| 1C, 2374 | T | Val | C | Ala | 544 | 301M |
| 1D | ||||||
| 2466 | A | Met | G | Val | 575 | 101M |
| 2500 | C | Thr | T | Ile | 586 | 102M |
| 2832 | T | Ser | C | Pro | 697 | 103M |
| 2842 | A | Gln | G | Arg | 700 | 104M |
| 3073 | T | Ile | C | Thr | 777 | 105M |
| 3243 | A | Lys | G | Glu | 834 | 106M |
| 2A, 3355 | G | Arg | T | Ile | 871 | 201M |
nt, nucleotide; aa, amino acid.
Each nucleotide was termed as shown in the table for site-directed mutagenesis.
FIG. 3.
Plaque phenotype of recombinant and mutant viruses. Plates: a, vSVLSJ1; b, vSVLS00; c, vSVLS104MJ1; d, vSVLS201MJ1; e, vSVLS104/201MJ1; f, vSVLS201M00; g, vSVLS104/201M00. IBRS-2 cell monolayers were inoculated with viruses and incubated at 37°C. Cultures were fixed after 2 days and stained with crystal violet.
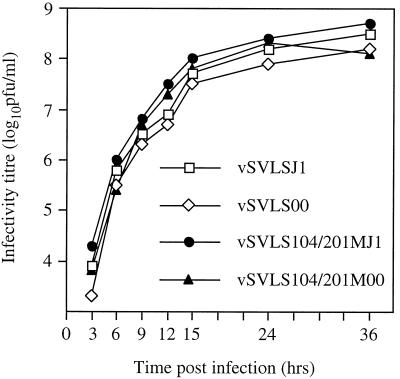
No differences were observed between the one-step growth curves of the parental strains, vSVLSJ1 and vSVLS00, and the site-directed mutants which showed an altered plaque phenotype, strains vSVLS104/201MJ1 and vSVLS104/201M00 (Fig. 4).
FIG. 4.
Single-step growth curves of vSVLSJ1, vSVLS00, vSVLS104/201MJ1, and vSVLS104/201M00. IBRS-2 cell monolayers were inoculated with the viruses shown at a multiplicity of infection of 10 and incubated at 37°C. Samples of supernatant were collected at the times shown, and the viral infectivity was determined by a standard plaque assay.
Pathogenicity in pigs.
As in previous experiments with virulent and avirulent Japanese strains (18), the clinical signs other than the appearance of vesicles at predilection sites were mild or absent. In agreement with a previous study (18), vesicles were detected on the coronary band and/or heels of all pigs inoculated with the virus vSVLSJ1, which was recovered from the infectious clone of the virulent strain, but no vesicles were observed in pigs infected with vSVLS00, which was derived from the avirulent strain.
Pathogenicity correlated well with the large-plaque phenotype. Thus, lesions were observed in all pigs inoculated with viruses containing the P1/2A region (vSVLSP1J1), the 1C/1D/2A region (vSVLS1CD2AJ1), or just the amino acids at sites 104M and 201M (vSVLS104/201MJ1), corresponding to the pathogenic J1’73 strain. Conversely, no lesions were detected in pigs if these sites or regions corresponded to the avirulent H/3’76 strain, even though the rest of the genome was derived from the virulent strain. The only exception was a single vesicle at the site of inoculation site in one pig inoculated with vSVLS5’J1.
Seroconversion was detected in all pigs which showed clinical disease (Table 2) and in the majority of those that did not. When measured at 14 days postinfection (Table 2), the mean virus-neutralizing titer of groups showing clinical disease was higher than that of groups with subclinical disease. True subclinical infection characterized by seroconversion in the absence of clinical disease was detected in between one and four of the five pigs inoculated with each of the viruses which did not cause clinical disease. Some pigs inoculated with avirulent viruses therefore showed subclinical disease, but in others the viruses did not appear to establish infection since seroconversion did not occur.
Sequencing of isolates.
For each group of pigs, live virus or viral RNA was recovered from epithelium, tonsillar swabs, or the feces of one or more animals, indicating that viral replication had taken place in some or all of the animals inoculated. To confirm the identity of the recovered viruses and to look for mutations or recombinations that might have occurred in vivo, representative isolates from each group were sequenced over the region of the genome that characterized their identity. In every case, the sequences derived from the recovered viruses over the region examined were identical to those of the clones used to infect them (data not shown).
DISCUSSION
This study examined the genetic determinants of virulence and of plaque phenotype in SVDV and the relationship between them. By exchanging genomic regions between virulent and avirulent strains, the region associated with both plaque phenotype and virulence was mapped between nt 2233 and 3368, encoding the C-terminal part of VP3, the whole of VP1, and the N-terminal part of 2A. The 5′-NCR, the P2 region other than 2A, and the P3 and 3′-NCR regions did not appear to contribute to pathogenicity since the virulence of chimeric viruses did not correlate with whether these regions originated from virulent or avirulent infectious clones. The finding that the 5′-NCR of SVDV did not affect virulence was unexpected. For other enteroviruses, this region is thought to be an important virulence determinant (20, 31, 33, 40, 51) since it contains the 5′-NCR, including the IRES, which regulates the efficiency of the initiation of translation (16, 39). The only exception was a single pig which, after inoculation with vSVLS5’J1, showed a single vesicle at the site of inoculation site. This was not a sign of an increase in the virulence of this virus, which comprised the 5′-NCR of the virulent strain attached to the remainder of the avirulent strain, but rather confirms that pigs inoculated intradermally with avirulent Japanese strains of SVDV can occasionally develop localized vesicles (22).
By site-directed mutagenesis, it was possible to map more precisely the determinants of both plaque phenotype and virulence to nt 2842, corresponding to VP1-132, and nt 3355, corresponding to 2APRO-20. All viruses which had glycine at position 132 of VP1 and arginine at position 20 of 2APRO, corresponding to the residues found in the virulent parental strain, had a large-plaque phenotype and were pathogenic for pigs. It is not clear from this study why mutations at both nt 2842 and nt 3355 were necessary to change the small-plaque phenotype of the avirulent strain to the large-plaque phenotype, while only a single mutation at nt 3355 was necessary to change the large-plaque phenotype to a small-plaque phenotype. It may be that (i) these sites contribute to plaque phenotype independently since the site-directed mutant viruses, vSVLS104MJ1 and vSVLS201MJ1, produced plaques which were intermediate in size between the two parental viruses (Fig. 3) and that (ii) 2APRO-20 is the major determinant of plaque size.
The nature of the relationship between plaque phenotype and virulence has yet to be fully elucidated. In general, strains with a large-plaque phenotype are more virulent than those which produce smaller plaques, but the genetic determinants of the two traits do not always map to the same site as, for example, in coxsackieviruses (43, 52). One hypothesis might be that virulent strains are able to replicate more rapidly in vitro to produce large plaques and in vivo to produce larger foci of cell destruction. This does not appear to be the case for the SVDV strains examined here, which all had similar one-step growth curves on IBRS-2 cells (Fig. 4). Similar results were found with CVB3, in which viruses with different plaque phenotypes showed no significant differences in one-step growth (52). Similarly for PV type 2, in which there was no difference in virus proliferation between a wild-type strain and recombinant or site-directed mutant viruses in cell culture (25). However, for CVB3 (50) and PV (1, 26) the choice of cell line on which in vitro growth was examined was important and was related to the natural tropism of the virus. Cardiovirulent strains of CVB3 can be distinguished from avirulent strains by their preferential growth on fetal murine heart fibroblasts but not on the HeLa cells (50). Likewise, neurovirulent strains of PV can be distinguished from attenuated strains by growth on a human neuroblastoma cell line (1, 26). If such a cell line could be identified for SVDV, perhaps of epithelial origin, it might be very useful for distinguishing virulent from avirulent strains in vitro.
Residue 132 of VP1 is located within the loop connecting β-strands D and E (DE loop). The three-dimensional structure of SVDV was modelled (19) by using poliovirus and HRV14 proteins data from the Protein Data Bank (PDB entry codes 2PLV and 4RHV, respectively) as templates and following a procedure termed homology modelling (3), which was implemented from the modelling software SYBYL (Tripos Associates). With this model, the loop is exposed on the external surface of the virion near the fivefold axis of symmetry. Mutations at VP1-132 might alter the conformation of the virus and thus its ability to interact with host cells. Residues within the DE loop are major determinants of pathogenicity in other enteroviruses. Threonine at position VP1-129 and isoleucine at position VP1-143 have been shown to be important for virulence in CVB4 (8) and PV type 2 (45), respectively. Alterations at the DE loop may affect virus characteristics directly or may indirectly alter the conformation of the structurally adjacent BC loop. This indirect influence of changes in the DE loop affecting the BC loop has been suggested as a means by which host range specificity is determined in PV through receptor-mediated interactions (35, 45).
The 2A protease of enteroviruses contributes to several of the processes involved in replication: initial cleavage of the viral polyprotein at the junction of 1D and 2A (49); inhibition of host cell protein synthesis (24, 27); transactivation of translation (12, 30); and RNA replication (34). The structure of the 2A protease has been well studied in PV (2, 47). From these studies, 2APRO can be classified as a cysteine protease, based on the catalytic triad His-21, Asp-39, and Cys-110 (positions refer to the deduced amino acid sequence of SVDV J1’73) (14), and their secondary structure is assumed to be conserved among all members of the genus enterovirus (53). Residue 2APRO-20 in SVDV is the amino acid adjacent to His-21. Substitutions at this site may therefore influence 2A protease activity, resulting in altered plaque phenotype and pathogenicity for pigs. In a similar manner, alterations in the nonstructural proteins of other picornaviruses are thought to affect virulence through their effect on host cell-regulated processes (10, 28) and, more specifically, neurovirulence of PV type 1 in mice has recently been mapped to the 2A coding region (29).
Identification of the genetic determinants of virulence for SVDV will improve our understanding of how some strains of the virus can exist subclinically in the field and, possibly, lead to the rational design of attenuated vaccine strains. Residues VP1-132 and 2APRO-20 are important determinants of both plaque phenotype and virulence. Further studies are in progress to determine their relative importance in virulence in vivo. But whether the virulence determinants in other strains could map to the same sites is unknown. Further work is also required to examine whether or not the two residues responsible for virulence in the Japanese strain J1’73 are equally important in other virulent strains of the virus.
ACKNOWLEDGMENTS
We are grateful to F. Lin for his assistance and discussion and to G. Hutchings for excellent technical assistance in virus isolation. We also thank the staff of the isolation units at the Institute for Animal Health, Pirbright, for their skilled handling of the animals.
REFERENCES
- 1.Agol V I, Drozdov S G, Ivannikova T A, Kolesnikova M S, Korolev M B, Tolskaya E A. Restricted growth of attenuated poliovirus strains in cultured cells of a human neuroblastoma. J Virol. 1989;63:4034–4038. doi: 10.1128/jvi.63.9.4034-4038.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bazan J F, Fletterick R J. Viral cysteine proteases are homologous to the trypsin-like family of serine proteases: structural and functional implications. Proc Natl Acad Sci USA. 1988;85:7872–7876. doi: 10.1073/pnas.85.21.7872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Blundell T, Carney D, Gardner S, Hayes F, Howlin B, Hubbard T, Overington J, Singh D A, Sibanda B L, Sutcliffe M. 18th Sir Hans Krebs Lecture: knowledge-based protein modelling and design. Eur J Biochem. 1988;172:513–520. doi: 10.1111/j.1432-1033.1988.tb13917.x. [DOI] [PubMed] [Google Scholar]
- 4.Bouchard M J, Lam D H, Racaniello V R. Determinants of attenuation and temperature sensitivity in the type 1 poliovirus Sabin vaccine. J Virol. 1995;69:4972–4978. doi: 10.1128/jvi.69.8.4972-4978.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Brocchi E, Zhang G, Knowles N J, Wilsden G, McCauley J W, Marquardt O, Ohlinger V F, De Simone F. Molecular epidemiology of recent outbreaks of swine vesicular disease: two genetically and antigenically distinct variants in Europe 1987–94. Epidemiol Infect. 1997;118:51–61. doi: 10.1017/s0950268896007170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Brown F, Talbot P, Burrows R. Antigenic differences between isolates of swine vesicular disease virus and their relationship to coxsackie B5 virus. Nature (London) 1973;245:315–316. doi: 10.1038/245315a0. [DOI] [PubMed] [Google Scholar]
- 7.Brown F, Wild T F, Rowe L W, Underwood B O, Harris T J R. Comparison of swine vesicular disease virus and coxsackie B5 virus by serological and RNA hybridization methods. J Gen Virol. 1976;31:231–237. doi: 10.1099/0022-1317-31-2-231. [DOI] [PubMed] [Google Scholar]
- 8.Caggana M, Chan P, Ramsingh A. Identification of a single amino acid residue in the capsid protein VP1 of coxsackievirus B4 that determines the virulent phenotype. J Virol. 1993;67:4797–4803. doi: 10.1128/jvi.67.8.4797-4803.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cohen J I, Ticehurst J R, Feinstone S M, Rosenblum B, Purcell R H. Hepatitis A virus cDNA and its RNA transcripts are infectious in cell culture. J Virol. 1987;61:3035–3039. doi: 10.1128/jvi.61.10.3035-3039.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Emerson S U, Huang Y K, Purcell R H. 2B and 2C mutations are essential but mutations throughout the genome of HAV contribute to adaptation to cell culture. Virology. 1993;194:475–480. doi: 10.1006/viro.1993.1286. [DOI] [PubMed] [Google Scholar]
- 11.Graves J H. Serological relationship of swine vesicular disease virus and coxsackie B5 virus. Nature (London) 1973;245:314–315. doi: 10.1038/245314a0. [DOI] [PubMed] [Google Scholar]
- 12.Hambidge S J, Sarnow P. Translational enhancement of the poliovirus 5′ noncoding region mediated by virus-encoded polypeptide 2A. Proc Natl Acad Sci USA. 1992;89:10272–10276. doi: 10.1073/pnas.89.21.10272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Inoue T, Suzuki T, Sekiguchi K. The complete nucleotide sequence of swine vesicular disease virus. J Gen Virol. 1989;70:919–934. doi: 10.1099/0022-1317-70-4-919. [DOI] [PubMed] [Google Scholar]
- 14.Inoue T, Yamaguchi S, Kanno T, Sugita S, Saeki T. The complete nucleotide sequence of a pathogenic swine vesicular diseases virus isolated in Japan (J1’73) and phylogenetic analysis. Nucleic Acids Res. 1993;21:3896. doi: 10.1093/nar/21.16.3896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Inoue T, Yamaguchi S, Saeki T, Sekiguchi K. Production of infectious swine vesicular disease virus from cloned cDNA in mammalian cells. J Gen Virol. 1990;71:1835–1838. doi: 10.1099/0022-1317-71-8-1835. [DOI] [PubMed] [Google Scholar]
- 16.Jang S K, Pestova T V, Hellen C U T, Witherell G W, Wimmer E. Cap-independent translation of picornavirus RNAs: structure and function of the internal ribosomal entry site. Enzyme. 1990;44:292–309. doi: 10.1159/000468766. [DOI] [PubMed] [Google Scholar]
- 17.Kandolf R, Hofschneider P H. Molecular cloning of the genome of a cardiotropic coxsackie B3 virus: full-length reverse-transcribed recombinant cDNA generates infectious virus in mammalian cells. Proc Natl Acad Sci USA. 1985;82:4818–4822. doi: 10.1073/pnas.82.14.4818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kanno T, Inoue T, Mackay D, Kitching P, Yamaguchi S, Shirai J. Viruses produced from complementary DNA of virulent and avirulent strains of swine vesicular disease viruses retain the in vivo and in vitro characteristics of the parental strain. Arch Virol. 1998;143:1055–1062. doi: 10.1007/s007050050355. [DOI] [PubMed] [Google Scholar]
- 19.Kanno T, Inoue T, Wang Y, Sarai A, Yamaguchi S. Identification of the location of antigenic sites of swine vesicular disease virus with neutralization-resistant mutants. J Gen Virol. 1995;76:3099–3106. doi: 10.1099/0022-1317-76-12-3099. [DOI] [PubMed] [Google Scholar]
- 20.Kawamura N, Kohara M, Abe S, Komatsu T, Tago K, Arita M, Nomoto A. Determinants in the 5′ noncoding region of poliovirus Sabin 1 RNA that influence the attenuation phenotype. J Virol. 1989;63:1302–1309. doi: 10.1128/jvi.63.3.1302-1309.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klump W M, Bergmann I, Müller B C, Ameis D, Kandolf R. Complete nucleotide sequence of infectious coxsackievirus B3 cDNA: two initial 5′ uridine residues are regained during plus-strand RNA synthesis. J Virol. 1990;64:1573–1583. doi: 10.1128/jvi.64.4.1573-1583.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kodama M, Saito T, Ogawa T, Tokuda G, Sasahara J, Kumagai T. Swine vesicular disease viruses isolated from healthy pigs in non-epizootic period. II. Vesicular formation and virus multiplication in experimentally inoculated pigs. Natl Inst Anim Health Q. 1980;20:123–130. [PubMed] [Google Scholar]
- 23.Kohara M, Abe S, Kuge S, Semler B L, Komatsu T, Arita M, Itoh H, Nomoto A. An infectious cDNA clone of the poliovirus Sabin strain could be used as a stable repository and inoculum for the oral polio live vaccine. Virology. 1986;151:21–30. doi: 10.1016/0042-6822(86)90100-5. [DOI] [PubMed] [Google Scholar]
- 24.Kräusslich H G, Nicklin M J H, Toyoda H, Etchison D, Wimmer E. Poliovirus proteinase 2A induces cleavage of eucaryotic initiation factor 4F Polypeptide p220. J Virol. 1987;61:2711–2718. doi: 10.1128/jvi.61.9.2711-2718.1987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.La Monica N, Meriam C, Racaniello V R. Mapping of sequences required for mouse neurovirulence of poliovirus type 2 Lansing. J Virol. 1986;57:515–525. doi: 10.1128/jvi.57.2.515-525.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.La Monica N, Racaniello V R. Differences in replication of attenuated and neurovirulent poliovirus in human neuroblastoma cell line SH-SY5Y. J Virol. 1989;63:2357–2360. doi: 10.1128/jvi.63.5.2357-2360.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lloyd R E, Grubman M J, Ehrenfeld E. Relationship of p220 cleavage during picornavirus infection to 2A proteinase sequencing. J Virol. 1988;62:4216–4223. doi: 10.1128/jvi.62.11.4216-4223.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lomax N B, Yin F H. Evidence for the role of the P2 protein of human rhinovirus in its host range change. J Virol. 1989;63:2396–2399. doi: 10.1128/jvi.63.5.2396-2399.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lu H, Yang C, Murdin A D, Klein M H, Harber J J, Kew O M, Wimmer E. Mouse neurovirulence determinants of poliovirus type 1 strain LS-a map to the coding regions of capsid protein VP1 and proteinase 2Apro. J Virol. 1994;68:7507–7515. doi: 10.1128/jvi.68.11.7507-7515.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Macadam A J, Ferguson G, Fleming T, Stone D M, Almond J W, Minor P D. Role for poliovirus protease 2A in cap independent translation. EMBO J. 1994;13:924–927. doi: 10.1002/j.1460-2075.1994.tb06336.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Macadam A J, Pollard S R, Ferguson G, Dunn G, Skuce R, Almond J W, Minor P D. The 5′ noncoding region of the type 2 poliovirus vaccine strain contains determinants of attenuation and temperature sensitivity. Virology. 1991;181:451–458. doi: 10.1016/0042-6822(91)90877-e. [DOI] [PubMed] [Google Scholar]
- 32.Mann J A. The pathogenesis of swine vesicular disease. Ph.D. thesis. Reading, United Kingdom: University of Reading; 1982. [Google Scholar]
- 33.Martin A, Benichou D, Couderc T, Hogle J M, Wychowski C, Van der Werf S, Girard M. Use of type 1/type 2 chimeric polioviruses to study determinants of poliovirus type 1 neurovirulence in a mouse model. Virology. 1991;180:648–658. doi: 10.1016/0042-6822(91)90078-p. [DOI] [PubMed] [Google Scholar]
- 34.Molla A, Paul A V, Schmid M, Jang S K, Wimmer E. Studies on dicistronic polioviruses implicate viral proteinase 2Apro in RNA replication. Virology. 1993;196:739–747. doi: 10.1006/viro.1993.1531. [DOI] [PubMed] [Google Scholar]
- 35.Moss E G, Racaniello V R. Host range determinants located on the interior of the poliovirus capsid. EMBO J. 1991;10:1067–1074. doi: 10.1002/j.1460-2075.1991.tb08046.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nakano J H, Hatch M H, Thieme M L, Nottay B. Parameters for differentiating vaccine-derived and wild poliovirus strains. Prog Med Virol. 1978;24:178–206. [PubMed] [Google Scholar]
- 37.Nardelli L, Lodetti E, Gualandi G L, Burrows R, Goodridge D, Brown F, Cartwright B. A foot and mouth disease syndrome in pigs caused by an enterovirus. Nature (London) 1968;219:1275–1276. doi: 10.1038/2191275a0. [DOI] [PubMed] [Google Scholar]
- 38.Omata T, Kohara M, Kuge S, Komatsu T, Abe S, Semler B L, Kameda A, Itoh H, Arita M, Wimmer E, Nomoto A. Genetic analysis of the attenuation phenotype of poliovirus type 1. J Virol. 1986;58:348–358. doi: 10.1128/jvi.58.2.348-358.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pelletier J, Kaplan G, Racaniello V R, Sonenberg N. Cap-independent translation of poliovirus mRNA is conferred by sequence elements within the 5′ noncoding region. Mol Cell Biol. 1988;8:1103–1112. doi: 10.1128/mcb.8.3.1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Pollard S R, Dunn G, Cammack N, Minor P D, Almond J W. Nucleotide sequence of a neurovirulent variant of the type 2 oral poliovirus vaccine. J Virol. 1989;63:4949–4951. doi: 10.1128/jvi.63.11.4949-4951.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Racaniello V R, Baltimore D. Cloned poliovirus complementary DNA is infectious in mammalian cells. Science. 1981;214:916–919. doi: 10.1126/science.6272391. [DOI] [PubMed] [Google Scholar]
- 42.Ramsingh A I, Collins D N. A point mutation in the VP4 coding sequence of coxsackievirus B4 influences virulence. J Virol. 1995;69:7278–7281. doi: 10.1128/jvi.69.11.7278-7281.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Ramsingh A I, Caggana M, Ronstrom S. Genetic mapping of the determinants of plaque morphology of coxsackievirus B4. Arch Virol. 1995;140:2215–2226. doi: 10.1007/BF01323241. [DOI] [PubMed] [Google Scholar]
- 44.Ramsingh A, Hixson A, Duceman B, Slack J. Evidence suggesting that virulence maps to the P1 region of the coxsackievirus B4 genome. J Virol. 1990;64:3078–3081. doi: 10.1128/jvi.64.6.3078-3081.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Ren R, Moss E G, Racaniello V R. Identification of two determinants that attenuate vaccine-related type 2 poliovirus. J Virol. 1991;65:1377–1382. doi: 10.1128/jvi.65.3.1377-1382.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Seechurn P, Knowles N J, McCauly J W. The complete nucleotide sequence of a pathogenic swine vesicular disease virus. Virus Res. 1990;16:255–274. doi: 10.1016/0168-1702(90)90052-d. [DOI] [PubMed] [Google Scholar]
- 47.Shuyuarn F Y, Lloyd R E. Identification of essential amino acid residues in the functional activity of poliovirus 2A protease. Virology. 1991;182:615–625. doi: 10.1016/0042-6822(91)90602-8. [DOI] [PubMed] [Google Scholar]
- 48.Tatem J M, Weeks-Levy C, Georgiu A, DiMichele S J, Gorgacz E J, Racaniello V R, Cano F R, Mento S J. A mutation present in the amino terminus of Sabin 3 poliovirus VP1 protein is attenuating. J Virol. 1992;66:3194–3197. doi: 10.1128/jvi.66.5.3194-3197.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Toyoda H, Nicklin M J H, Murray M G, Anderson C W, Dunn J J, Sudier F W, Wimmer E. A second virus-encoded proteinase involved in proteolytic processing of poliovirus polyprotein. Cell. 1986;45:761–770. doi: 10.1016/0092-8674(86)90790-7. [DOI] [PubMed] [Google Scholar]
- 50.Tu Z, Chapman N M, Hufnagel G, Tracy S, Romero J R, Barry W H, Zhao L, Currey K, Shapiro B. The cardiovirulent phenotype of coxsackievirus B3 is determined at a single site in the genomic 5′ nontranslated region. J Virol. 1995;69:4607–4618. doi: 10.1128/jvi.69.8.4607-4618.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Westrop G D, Wareham K A, Evans D M A, Dunn G, Minor P D, Magrath D I, Taffs F, Marsden S, Skinner M A, Schild G C, Almond J W. Genetic basis of attenuation of the Sabin type 3 oral poliovirus vaccine. J Virol. 1989;63:1338–1344. doi: 10.1128/jvi.63.3.1338-1344.1989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhang H, Blake N W, Ouyang X, Pandolfino Y A, Morgan-Capner P, Archard L C. A single amino acid substitution in the capsid protein VP1 of coxsackievirus B3 (CVB3) alters plaque phenotype in Vero cells but not cardiovirulence in a mouse model. Arch Virol. 1995;140:959–966. doi: 10.1007/BF01314972. [DOI] [PubMed] [Google Scholar]
- 53.Zoll J, Galama J, Melchers W. Intratypic genome variability of the coxsackievirus B1 2A protease region. J Gen Virol. 1994;75:687–692. doi: 10.1099/0022-1317-75-3-687. [DOI] [PubMed] [Google Scholar]