Abstract
Background
Anemia is a common and often overlooked hematological change observed in patients with diabetes mellitus. However, there is no global survey or health registry that estimates the pooled prevalence of anemia in patients with type 2 diabetes. Therefore, this study aimed to determine the global pooled prevalence of anemia among adult patients with type 2 diabetes.
Methods
This study was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis guidelines. The study protocol was registered on PROSPERO with the reference number (CRD42022327135), and the link provided (https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022327135) display the published methodology. Previously published articles were searched in PubMed/Medline, Cochrane Library, WHO Global Index Medicus, African Journals Online, ScienceDirect, Google Scholar, and Google from October 26 to November 09, 2022. The quality of the included studies was assessed using the Joanna Briggs Institute Critical Appraisal tool. Random-effects model was used to estimate the pooled prevalence of anemia. The degree of heterogeneity among the included studies was assessed using I2 statistics. Publication bias was detected using funnel plot symmetry analysis supplemented by Egger’s and Begg’s tests.
Results
Twenty-four studies with a total number of 19,118 participants were included in this systematic review and meta-analysis. The overall pooled prevalence of anemia among type 2 diabetic adult patients was 27.0% (95% CI: 24.0, 31.0, I2 = 96.45%; P< 0.001). Geographical and time-based subgroup analysis showed that higher prevalence of anemia was observed in Africa region 28.0% (95% CI: 17.0, 39.0) and from 2015 to 2022, 28.0% (95% CI: 24.0, 33.0), respectively.
Conclusion
Anemia is a moderate public health problem among adult patients with type 2 diabetes. Nearly one in four patients with type 2 diabetes develops anemia. Therefore, considering the negative impact of anemia, it is important to include anemia screening in the routine assessment of diabetes-related complications.
Keywords: adult, anemia, inflammation, type 2 diabetes, meta-analysis, systematic review
Introduction
Diabetes is a fast-growing global health emergency characterized by persistent hyperglycemia, with changes in the metabolism of carbohydrates, lipids, and proteins resulting from defects in insulin secretion, action, or both.1 The burden of diabetes among adults has rapidly increased, from 108 million in 1980 to 537 million cases and 6.7 million deaths by 2021.2 More than two-thirds of the global burden of diabetes is observed in low- and middle-income countries, and the number of diabetes cases is estimated to increase to 783 million by 2045.2 Uncontrolled diabetes is associated with various pathological changes, including metabolic, cellular, and blood disturbances, resulting in long-term microvascular and macrovascular complications.3
Type 2 diabetes mellitus (T2DM) accounts for 90–95% of diabetes cases1 and it is a part of metabolic syndrome that comprises dyslipidemia, obesity, hypertension, and hematological changes.4 Hematological changes, including those in red blood cells (RBCs), white blood cells (WBCs), platelets, and coagulation systems, have been documented in diabetes.5 Anemia is the most common and often overlooked hematological change observed in patients with T2DM.6,7 The etiology of anemia in T2DM is multifaceted and includes impaired renal function, hormonal changes, oral hypoglycemic agents, oxidative stress, advanced glycation end-products (AGEs), chronic hyperglycemia, and inflammation.8–12 Advanced aged subjects with anemia usually tend to have chronic comorbidities including diabetes mellitus.13 In addition, type 2 diabetes mellitus is associated with increased burden of chronic low-grade inflammation which can drives bone marrow and other mechanism to produce anemia.14 Regardless of the underlying mechanisms of diabetogenesis, anemia is an independent predictor of increased risk of vascular complications in diabetes.15,16 Early diagnosis and treatment of anemia in diabetes have been shown to improve complications,15,17 as it occurs early in the progression of diabetic nephropathy and other complications.18,19
Anemia is amongst the major clinical and public health challenges that influence the progression of chronic health problems in diabetic population.20 However, the precise prevalence and characterization of anemia in the diabetic cohort is unknown. There is a need of identifying and monitoring of iron status and anemia in patients with T2DM.21 Recently published systematic review and meta-analysis showed that anemia is a moderate to severe public health problem among adult populations living with diabetes, with the prevalence of 22% in Ethiopia, 35% in Africa, and 45% in South Asia.20,22,23
Despite a growing body of research on these problems, there is a lack of synthesized evidence on the burden of anemia among people with diabetes. Although some studies have been conducted on the prevalence of anemia, no official worldwide survey or international health registry has estimated the prevalence of anemia in T2DM patients to date. Therefore, this study aimed to determine the global pooled prevalence of anemia in type 2 diabetic adult patients.
Methods
Study Setting, Design and Protocol
This systematic review and meta-analysis were conducted for all cross-sectional studies published worldwide. The Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) 2020 checklist (S1) 24 was used throughout the review process. The study protocol was prospectively registered on PROSPERO (registration number CRD42022327135), and the link provided (https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42022327135) shows the published methodology.
Searches Strategy
A literature search was conducted from major databases and indexing services including PubMed/Medline, Cochrane Library, WHO Global Index Medicus, African Journals Online, ScienceDirect, Google Scholar, and Google from October 26, to November 09, 2022. Search terms were used either separately or combination with Boolean operators (OR and AND). The search terms included MeSH (“anemia” OR “anaemia”) AND (“type 2 diabetes mellitus” OR “diabetes mellitus”), AND (“adult”), Title/Abstract (“hematological parameters”), (“anemia” AND “type 2 diabetes mellitus”) (S2). In addition, the reference lists of retrieved articles were used to identify studies that were not retrieved from electronic databases.
Outcomes of the Study
The main outcome of interest was the global prevalence of anemia among adult patients with type 2 diabetes according to the World Health Organization (WHO) definition of anemia (hemoglobin (Hgb) value less than 13 g/dl for men and less than 12 g/dl for non-pregnant women).25
Eligibility Criteria
To make the review more manageable and applicable, studies employing a cross-sectional design were considered. Therefore, all cross-sectional studies available online from January 1, 2000, to November 09, 2022, and the reported prevalence of anemia among adult patients with type 2 diabetes were included in the review. In contrast, studies that reported complications of diabetes but did not report separate outcomes for anemia were excluded. In addition, non-cross-sectional studies (clinical audit, case reports, case series, case control, cohort, and RCT), reviews, meta-analyses, studies with low-quality scores according to the criteria, and studies addressing specific groups such as HIV-infected adults, tuberculosis, and malaria were not included. Studies that recruited participants with gestational diabetes, type 1 diabetes, or irretrievable studies (after requesting the corresponding authors) were excluded.
Study Selection and Quality Assessment
ENDNOTE version 20 (Thomson Reuters, Stamford, CT, USA) was used to manage search results and identify duplicate records. The titles and abstracts of the studies retrieved using the search strategy were independently screened by two authors (MA and TT) to identify studies that met the inclusion criteria. Subsequently, studies that met the inclusion criteria by title/abstract screening were independently subjected to full-text appraisal by two authors (MA and TT) for eligibility and data extraction. Discrepancies were infrequent between the two authors’ evaluations, and when they occurred, they were resolved by sending them to the other authors (HA and KG) to arrive at a consensus. Quality assessment was performed using Joanna Briggs Institute (JBI) critical appraisal tools for prevalence studies in a systematic review.26 Two authors (MA and HA) independently assessed the risk of bias in the included studies. Discrepancies between the two authors were resolved via discussion and by sending them to the other authors (TT and KG). The JBI critical appraisal tool contains nine criteria, and for each criterion, a score was assigned as 0 for “not clear or not appropriate” and 1 for “yes”. The average scores given by the two authors were summarized across items to obtain a total quality score ranging from 0 to 9. Studies were then classified as low, medium, and high quality when the average awarded scores were 0–4, 5–7, and 7–9, respectively. All studies with high and medium quality were included in this systematic review and meta-analysis (Table 1).
Table 1.
General Characteristics and Outcomes of the Included Studies Among Type 2 Diabetic Adult Patients
| Author, Year of Publication | Study Setting | Study Year | Sample Size | Study Design | Sex (M/F) | Mean Age (Years) | DM Duration (Years) | Prevalence of Anemia, n (%) | Quality Score (JBI) |
|---|---|---|---|---|---|---|---|---|---|
| Awofisoye et al, 201927 | Nigeria | 2014 | 155 | CS | 45/110 | 60.3 ± 10.2 | 7 (1–36) | 70 (45.1) | 8 |
| Chung et al, 201928 | Republic of Korea | 2017 | 1637 | CS | 797/840 | 59.8 ± 13.0 | NR | 579 (35.4) | 8 |
| Chung et al, 201729 | Republic of Korea | 2014 | 2230 | CS | 1083/1147 | NR | NR | 750 (33.6) | 8 |
| Hosseini et al, 201430 | Iran | 2011 | 305 | CS | 144/161 | 53.9 ± 1 | 8.2 ± 7.1 | 93 (30.4) | 7 |
| Praveen et al, 202031 | India | NR | 89 | CS | NR | 49.76 ± 10.3 | NR | 15 (16.8) | 7 |
| Rathore et al, 201832 | India | 2016 | 200 | CS | 126/74 | 56.8 | 5 | 65 (32.5) | 6 |
| Bekele et al, 201933 | Ethiopia | 2019 | 374 | CS | 176/198 | 56.3 ± 11.5 | 5 (1–30) | 130 (34.8) | 8 |
| Arkew et al, 202134 | Ethiopia | 2020 | 134 | CS | 85/49 | 43.08±9.3 | 7.0 (4.0–9.0) | 24 (17.9) | 8 |
| Ebrahim et al, 202235 | Ethiopia | 2021 | 120 | CS | 64/56 | 38.75 ±10.5 | 5 | 31 (25.8) | 8 |
| Kebede et al, 202136 | Ethiopia | 2019 | 372 | CS | 142/230 | NR | 8.87 ± 3.69 | 30 (8.0) | 8 |
| He et al, 201537 | China | 2008 | 1997 | CS | 1141/856 | 59.67 ± 12.2 | 8.06 ± 6.71 | 439 (22.0) | 7 |
| Wu et al, 201738 | China | NR | 1134 | CS | 645/489 | 57.1 ± 9.6 | 9 (4–13) | 231 (20.4) | 7 |
| Srivastava et al, 200639 | Australia | NR | 228 | CS | 144/84 | 62 ± 11 | 10 | 49 (21.4) | 5 |
| Feteh et al, 201640 | Cameroon | 2013 | 636 | CS | 338/298 | 56.5 ± 10.6 | 4 (1–9) | 263 (41.3) | 6 |
| Ezenwaka et al, 200841 | Caribbean | 2006 | 155 | CS | 46/109 | 65.9 ± 0.9 | 10.6 ± 0.7 | 72 (46.4) | 6 |
| Brière et al, 202042 | France | 2019 | 4145 | CS | 2226/1919 | 54 ± 16 | 15 ± 12 | 1065 (25.7) | 5 |
| Grossman et al 201443 | Israel | 2010 | 445 | CS | 401/44 | 63±9.6 | 6.1±2.9 | 48 (10.7) | 5 |
| Idris et al, 201844 | Malaysia | 2015 | 808 | CS | 454/354 | 60.5 ± 9.5 | 7.0 (8.0) | 256 (31.6) | 8 |
| Sarosh et al, 202245 | Pakistan | 2021 | 200 | CS | 82/118 | 49.64±13 | 5.98 ± 4.6 | 78 (39.0) | 6 |
| Al-ghazaly et al, 201946 | Yemen | 2016 | 324 | CS | 141/183 | 53 ± 12 | NR | 77 (23.7) | 7 |
| Chiou et al, 201547 | Taiwan | NR | 1142 | CS | 579/563 | 63 ± 11 | 11 ± 7 | 286 (25.0) | 6 |
| Bonakdaran et al, 201148 | Iran | NR | 1962 | CS | 858/1104 | 52.47 ± 10.20 | 7.5 ± 6.1 | 385 (19.6) | 5 |
| Solomon et al, 202249 | Ethiopia | 2020 | 135 | CS | NR | 44.65 ± 17.69 | 6.5±5.8 | 31 (22.9) | 8 |
| Abate et al, 201350 | Ethiopia | 2012 | 191 | CS | NR | 40.96 ± 16.8 | 5.87 ± 4.7 | 57 (29.8) | 8 |
Abbreviations: CS, cross-sectional; NR, not reported.
Data Extraction
A Microsoft Excel spreadsheet was used to extract data from relevant studies. Two review authors (MA and KG) independently extracted data on author name, year of publication, sample size, study design, year of study, sex, mean/median age of study participants, study setting/country, duration of diabetes, and prevalence of anemia (Table 1).
Data Analysis
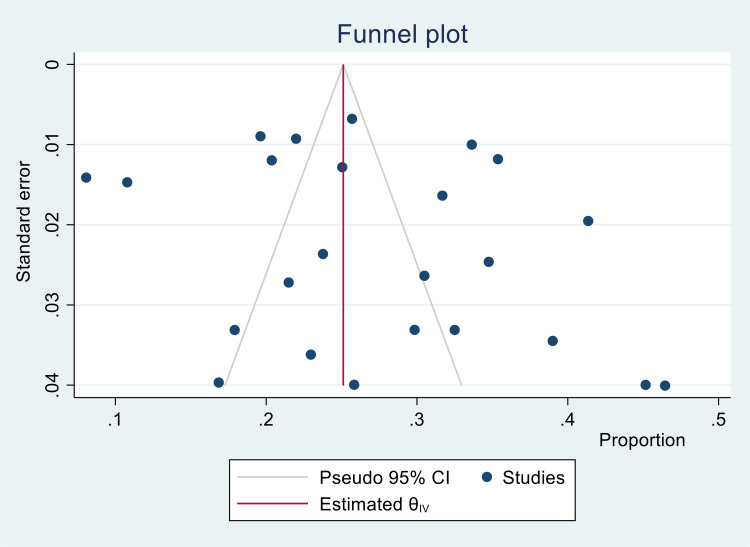
All relevant extracted data were exported to Stata/MP version 17 (Stata Corp, College Station, TX, USA) for the analysis. A narrative synthesis of the data was used to present the included studies, and a summary table was prepared to describe characteristics of the included studies. The pooled prevalence of anemia was carried out using a Der-Simonian-Laird random effects model, along with 95% confidence interval. The degree of heterogeneity among the included studies was assessed using I2 statistics. The 25%, 50%, and 75% I2 values were considered as low, moderate, and high heterogeneity, respectively.51 Subgroup analysis and univariate meta-regression models were used to assess the possible sources of heterogeneity. Potential outliers were investigated in the sensitivity analysis by omitting each study at a time. Publication bias was detected using funnel plot symmetry supplemented by Egger’s regression and Begg’s tests.52,53
Results
Search Results
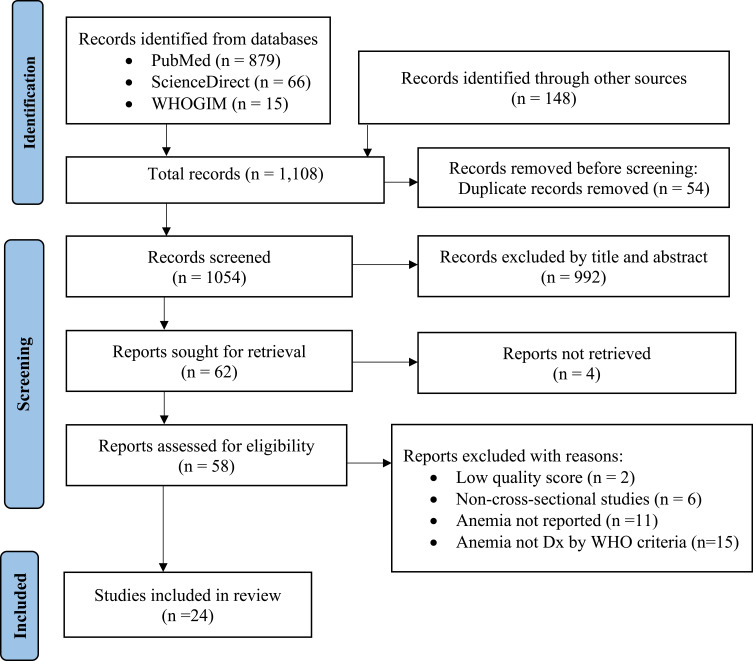
The PRISMA 2020 flow diagram24 was used to identify, screen, and include the relevant studies (Figure 1). In our comprehensive search, 1108 articles were identified from different sources. Of the total articles, 54 duplicate articles were excluded using EndNote 20 and manual tracing. The remaining 1054 articles were screened by reading their titles and abstracts; 992 articles were excluded. Of the 62 studies sought for retrieval, 4 articles were not accessible in full text, and 58 articles were screened for full-text assessment. Finally, 34 articles were excluded for various reasons and 24 articles were included in the synthesis and analysis.
Figure 1.
PRISMA 2020 Flow chart to describe the selection of studies for the systematic review and meta-analysis on the global prevalence of anemia among T2DM adult patients.
Characteristics of the Included Studies and Study Participants
Twenty-four cross-sectional studies published between 2006 and 2022 were included in this systematic review and meta-analysis. Fifteen countries were represented and 13 (54.16%) studies were reported in Asia,28–32,37,38,43–48 followed by eight (33.33%) studies from Africa,27,33–36,40,49,50 one (4.17%) study from Europe,42 one (4.17%) study from Australia,39 and one (4.17%) study from South America.41 The average quality scores of studies ranged from 5 to 8 as per the Joanna Briggs Institute scoring scale for prevalence studies. The sample sizes of the included studies ranged from 8931 to 414542 with a pooled mean sample size of 797.0 and total number of 19,118 participants. The mean age of the participants was reported in 22 studies and ranges from 38.75 to 65.90 years.35,41 The mean duration of diabetes was reported in 20 studies, ranging from 4 to 15 years, with a pooled mean duration of 7.6 years (Table 1).
Prevalence of Anemia
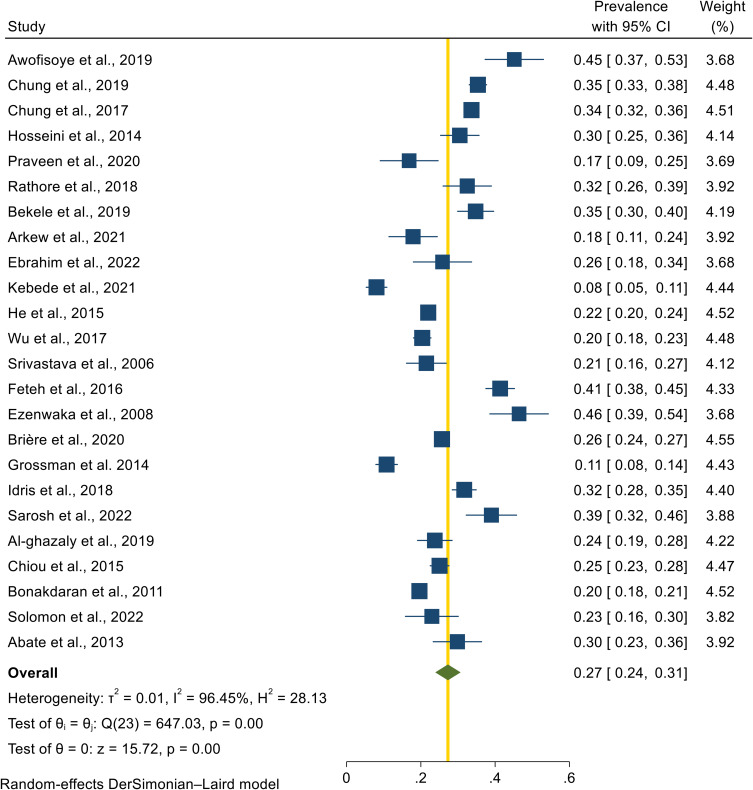
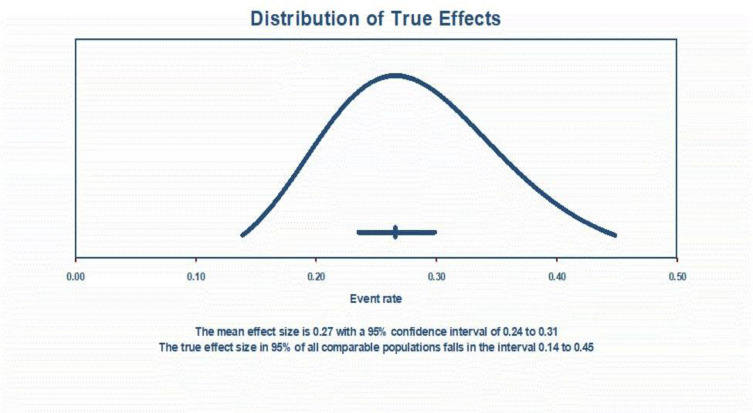
This systematic review and meta-analysis included 24 studies, all of which were used to estimate the pooled prevalence of anemia among adult patients with type 2 diabetes. The Random effects analysis revealed that the overall pooled prevalence of anemia among type 2 diabetic adult patients was 27.0% (95% CI: 24.0, 31.0) with higher heterogeneity (I2 = 96.45%; P <0.001). The prevalence of anemia in individual studies ranged from 8.0% to 46.0%,36,41 whereas the individual weight ranged from 3.68% to 4.55%27,35,41,42 (Figure 2). Based on the extent of heterogeneity in the random effects model, the 95% estimated predictive interval was calculated for this study. The estimated predictive interval for the true prevalence of anemia is ranged from 14% to 45%, which displays the approximate predictive distribution of any future study for all comparable populations (Figure 3).
Figure 2.
A forest plot showing the individual study and pooled prevalence of anemia among T2DM adult patients.
Figure 3.
Predictive interval for population prevalence of anemia among T2DM adult patients.
Subgroup and Sensitivity Analysis
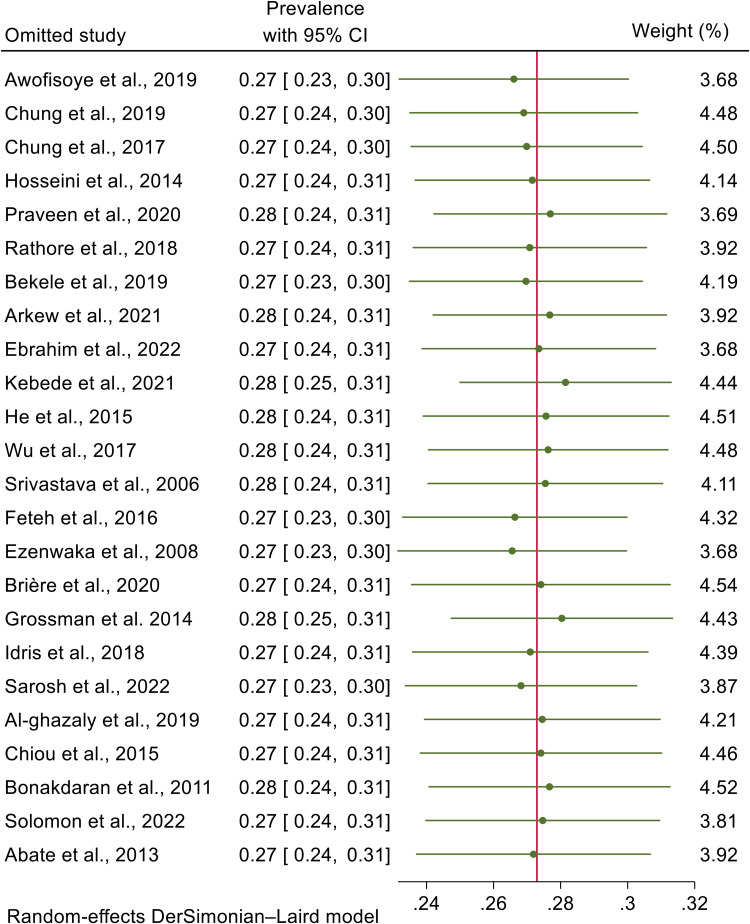
To identify the source of heterogeneity across the included studies, subgroup analyses were performed by considering publication year, sample size, duration of diabetes, and geographical region as grouping variables. Time based subgroup analysis showed that the prevalence of anemia from 2015 to 2022 was higher than that from 2006 to 2015 (28.0% vs 25.0%). The results of subgroup analysis based on geographical region showed the highest prevalence was from Africa (28.0%) as compared to other regions (Table 2). Additionally, to explore the influence of a single study on the overall meta-analysis, a sensitivity analysis using the leave-one-out approach was conducted. The results revealed that there was no strong evidence for the effect of a single study on the overall meta-analysis result (Figure 4). Furthermore, to investigate the heterogeneity observed in the studies, we performed meta-regression on continuous variables. Accordingly, univariate meta-regression revealed that the mean age of the participants, publication year, sample size, and duration of diabetes were not sources of heterogeneity.
Table 2.
Subgroup Analyses Showing Pooled Prevalence of Anemia Among Type 2 Diabetic Adult Patients
| Subgroups | Number of Studies | Prevalence (95% CI) | Heterogeneity | ||
|---|---|---|---|---|---|
| I2 | P-value | ||||
| Region | Asia | 13 | 26.0 (22.0, 30.0) | 96.61% | <0.001 |
| Africa | 8 | 28.0 (17.0, 39.0) | 97.31% | <0.001 | |
| Europe | 1 | - | - | - | |
| Australia | 1 | - | - | - | |
| South America | 1 | - | - | - | |
| Sample size | ≤ 797 | 16 | 28.0 (21.0, 34.0) | 96.29% | <0.001 |
| > 797 | 8 | 27.0 (23.0, 31.0) | 96.89% | <0.001 | |
| Duration of DM | ≤ 7.6 | 12 | 29 (23.0, 35.0) | 96.14% | <0.001 |
| >7.6 | 8 | 24.0 (20.0, 29.0) | 96.08% | <0.001 | |
| Publication year | 2006–2015 | 8 | 25.0 (20.0, 29.0) | 94.26% | <0.001 |
| 2015–2022 | 16 | 28.0 (24.0, 33.0) | 96.53% | <0.001 | |
Figure 4.
Sensitivity analysis showing the prevalence of anemia among T2DM adult patients.
Publication Bias
Publication bias was assessed visually using a funnel plot and statistically using the Egger’s and Begg’s tests. The funnel plot (Figure 5) was symmetric, and Egger’s regression test (P = 0.356) and Begg’s test (P = 0.385) provided no evidence of publication bias owing to the small study effects.
Figure 5.
Funnel plot depicting publication bias for the prevalence of anemia among T2DM adult patients.
Discussion
Anemia is a major public health problem estimated to affect about 1.74 billion (22.8%) of the world’s population and disproportionately affects low and middle-income countries.54,55 Anemia in individuals with diabetes results in adverse health consequences, as it is associated with the progression of vascular complications and all-cause mortality.18,19,56 However, a global estimate of the prevalence in type 2 diabetic adult population is lacking. In the current systematic review and meta-analysis, the pooled prevalence of anemia was 27%, which corresponds to moderate public health significance according to the WHO classification.25 Accordingly, the results of this meta-analysis indicate that anemia is a moderate public health problem among patients with type 2 diabetes, which requires the design of prevention and control strategies to reduce the burden of anemia. This finding is in agreement with those of previous studies,22,23,57 which reported that anemia is a moderate public health problem in the diabetic population.
In the subgroup analysis, the prevalence of anemia was relatively higher in Africa region as compared to Asia region (28.0% vs 26.0%). This finding is in agreement with the notion that anemia is more prevalent in less developed countries.55 This might be due to that type 2 diabetic patients are more vulnerable to different forms of short-term and long-term complications, especially in sub-Saharan African countries.58
Anemia in T2DM results from various factors including renal function impairment, chronic hyperglycemia, chronic inflammation, oxidative stress, advanced glycation end products, hormonal changes, and oral hypoglycemic agents.8–12 Diabetes-related chronic kidney disease remains a global public health problem and is associated with high mortality in diabetic patients.59 Diabetic nephropathy, a common cause of end-stage renal disease, is associated with impaired iron metabolism and reduced erythropoietin production, resulting in the decreased production of red blood cells.19,60 Autonomic neuropathy is a major complication of uncontrolled diabetes mellitus. As the production and release of erythropoietin are regulated by the autonomic nervous system, a higher incidence of anemia in patients with poorly controlled diabetes might be observed in the absence of renal impairment.61
In addition to renal impairment, blood cells remain in a hyperglycemic environment throughout their lifespan are subjected to several structural and functional changes.62 These changes might be due to the generation of reactive oxygen species and irreversible glycation of hemoglobin and erythrocyte membrane proteins. This leads to decreased deformability, increased aggregation, aging of RBCs, and a reduced lifespan of erythrocytes.10,63,64 Additionally, oral antidiabetic medications such as metformin12 and decreased androgen levels11,65 are associated with the development of anemia in patients with type 2 diabetes mellitus.
Furthermore, while chronic inflammation causes anemia, persistent hyperglycemia in type 2 diabetes is associated with low-grade inflammation and increased levels of proinflammatory cytokines such as interleukin 6 and interleukin-1.11,66 Thus, inflammation-inducible cytokines and hepcidin play a role in the development of anemia by increasing the retention of iron in reticuloendothelial cells, changing the sensitivity of progenitor cells to erythropoietin, and promoting apoptosis of immature RBCs.67 Inflammatory markers such as C-reactive protein, neuregulin-4 and hemogram based inflammatory indices are closely associated with type 2 diabetes and its chronic complications including diabetic nephropathy, leading to anemia.68–70
To the best of our knowledge, this is the first systematic review and meta-analysis to summarize all the available data on the prevalence of anemia among adult patients with type 2 diabetes. The data generated in this review may provide important insights into the global prevalence of anemia among type 2 diabetes patients, inform public health interventions, and direct future interventional and empirical research. The PRISMA-2020 guidelines were strictly followed during the review. However, this systematic review and meta-analysis should be interpreted in the light of the following limitations. First, high heterogeneity was observed in both overall and subgroup analysis. Second, only 15 countries were included in this meta-analysis, with over-representation of some regions, such as Africa and Asia, which could skew the data. Third, this study did not explore the potential factors contributing to anemia in patients with diabetes.
Conclusions
The results of this review show that anemia is a global public health problem in patients with type 2 diabetes. Almost one in four patients with type 2 diabetes develops anemia. Anemia is more common in Africa than in other regions. Therefore, considering the negative impact of anemia, it is important to include anemia screening for routine assessment of diabetes-related complications.
Acknowledgments
We would like to thank all authors of the studies included in this systematic review and meta-analysis.
Funding Statement
No funding resource was received for this work.
Author Contributions
All authors made significant contributions to the work reported in the conception, study design, execution, acquisition, analysis, and interpretation of data. All authors took part in drafting, revising or critically reviewing the article and gave final approval of the version to be published. All authors have agreed to the approval of the final manuscript for publication in the current journal and to be accountable for all aspects of this work.
Disclosure
The authors declare that there are no competing interests.
References
- 1.American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2014;37(supplement 1):81–90. doi: 10.2337/dc14-S081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.International Diabetes Federation (IDF). IDF Diabetes Atlas. 10th ed. 2021; 141. [PubMed] [Google Scholar]
- 3.Agu K. Diabetes mellitus: a review of some of the prognostic markers of response to treatment and management. J Insul Resist. 2018;3(1):1–10. doi: 10.4102/jir.v3i1.36 [DOI] [Google Scholar]
- 4.Karaman A, Ozturk A, Ph D, et al. Prevalence of metabolic syndrome in the Mediterranean Region of Turkey: evaluation of hypertension, diabetes mellitus, obesity, and dyslipidemia. Metab Syndr Relat Disord. 2009;7(5):427–434. doi: 10.1089/met.2008.0068 [DOI] [PubMed] [Google Scholar]
- 5.Christian M, Adebayo A, Chinyere N, Wisdom N. Some haematological parameters in diabetic patients in Port Harcourt Nigeria. Asian J Multidiscip Stud. 2015;3(2):21–25. [Google Scholar]
- 6.Angelousi A, Larger E. Anaemia, a common but often unrecognized risk in diabetic patients: a review. Diabetes Metab. 2014;1–10. [DOI] [PubMed] [Google Scholar]
- 7.Barbieri J, Fontela PC, Winkelmann ER, et al. Anemia in Patients with Type 2 Diabetes Mellitus. Hindawi Publ Corp. 2015;2015:1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alamri BN, Bahabri A, Aldereihim AA, Alabduljabbar M. Hyperglycemia effect on red blood cells indices. Eur Rev Med Pharmacol Sci. 2019;23:2139–2150. doi: 10.26355/eurrev_201903_17259 [DOI] [PubMed] [Google Scholar]
- 9.Pretorius E, Bester J, Vermeulen N, et al. Poorly controlled type 2 diabetes is accompanied by significant morphological and ultrastructural changes in both erythrocytes and in thrombin- generated fibrin: implications for diagnostics. Cardiovasc Diabetol. 2015;14(30):1–20. doi: 10.1186/s12933-015-0192-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Asmah RH, Yeboah G, Archampong TN, Brown CA, Amegatcher G, Adjei DN. Relationship between oxidative stress and haematological indices in patients with diabetes in the Ghanaian population. Clin Diabetes Endocrinol. 2015;1(7):4–8. doi: 10.1186/s40842-015-0008-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sahay M, Kalra S, Badani R, et al. Diabetes and Anemia: international Diabetes Federation (IDF) -Southeast Asian Region (SEAR) position statement. Diabetes Metab Syndr Clin Res Rev. 2017;11:685–695. doi: 10.1016/j.dsx.2017.04.026 [DOI] [PubMed] [Google Scholar]
- 12.Donnelly LA, Dennis JM, Coleman RL, Sattar N, Hattersley AT, Holman RR. Risk of Anemia With Metformin Use in Type 2 Diabetes: a Mastermind Study. Diabetes Care. 2020;43:2493–2499. doi: 10.2337/dc20-1104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Duman TT, Aktas G, Atak BM, Kocak Z, Kurtkulagi O, Bilgin S. General characteristics of anemia in postmenopausal women and elderly men. Aging Male. 2020;23(5):780–784. doi: 10.1080/13685538.2019.1595571 [DOI] [PubMed] [Google Scholar]
- 14.Kurtkulagi O. Neutrophil to Lymphocyte ratio is significantly reduced after Sodium glucose cotransporter-2 inhibitor treatment in patients with type 2 diabetes mellitus. Int J Endocrinol. 2022;18(2):86–89. [Google Scholar]
- 15.Parving HH, Cooper ME, Rossing K, Parving HH. Anaemia in diabetes: is there a rationale to treat? Diabetologia. 2006;49:1151–1157. doi: 10.1007/s00125-006-0215-6 [DOI] [PubMed] [Google Scholar]
- 16.Gauci R, Hunter M, Bruce DG, Davis WA, Davis TME. Anemia complicating type 2 diabetes: prevalence, risk factors and prognosis. J Diabetes Complications. 2017;31(7):1169–1174. doi: 10.1016/j.jdiacomp.2017.04.002 [DOI] [PubMed] [Google Scholar]
- 17.Thomas S, Rampersad M. Anaemia in diabetes. Acta Diabetol. 2004;41:13–17. doi: 10.1007/s00592-004-0132-4 [DOI] [PubMed] [Google Scholar]
- 18.Kaushik D, Parashar R, Malik PK. Study of anaemia in type 2 diabetes mellitus. Int J Res Med Sci. 2018;6(5):1529–1533. doi: 10.18203/2320-6012.ijrms20181428 [DOI] [Google Scholar]
- 19.Stevens E, Nephrologist C, Hospital C. Diabetes and chronic kidney disease: where are we now. J Ren Care. 2012;38(Supp.1):67–77. doi: 10.1111/j.1755-6686.2012.00281.x [DOI] [PubMed] [Google Scholar]
- 20.Mazumder H, Islam KF, Rahman F, et al. Prevalence of anemia in diabetes mellitus in South Asia: a systematic review and meta- analysis. PLoS One. 2023;18(5):1–22. doi: 10.1371/journal.pone.0285336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pradeepa R, Shreya L, Anjana RM, et al. Frequency of iron deficiency anemia in type 2 diabetes - Insights from tertiary diabetes care centres across India. Diabetes Metab Syndr. 2022;16(11):1026–1032. doi: 10.1016/j.dsx.2022.102632 [DOI] [PubMed] [Google Scholar]
- 22.Adane T, Getawa S. Anaemia and its associated factors among diabetes mellitus patients in Ethiopia: a systematic review and meta- -analysis. Endocrinol Diabetes Metab. 2021;4:1–10. doi: 10.1002/edm2.260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Olum R, Bongomin F, Kaggwa MM, Andia-biraro I, Baluku JB. Anemia in diabetes mellitus in Africa: a systematic review and meta-analysis. Diabetes Metab Syndr Clin Res Rev. 2021;15:1–10. doi: 10.1016/j.dsx.2021.102260 [DOI] [PubMed] [Google Scholar]
- 24.Page MJ, Mckenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization. Haemoglobin concentrations for the diagnosis of anaemia and assessment of severity. Geneva: world Health Organization. Vitam Miner Nutr Inf Syst. 2011;11(1):1–6. [Google Scholar]
- 26.Munn Z, Moola S, Karolina Lisy DR, Tufanaru C. Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence. Int J Evid Based Healthc. 2015;13(3):147–153. doi: 10.1097/XEB.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 27.Awofisoye OI, Adeleye JO, Olaniyi JA, Esan A. Prevalence and correlates of anemia in type 2 diabetes mellitus: a study of a Nigerian outpatient diabetic population. Sahel Med J. 2019;22:55–63. [Google Scholar]
- 28.Chung JO, Park S, Chung DJ, Chung MY. Relationship between anemia, serum bilirubin concentrations, and diabetic retinopathy in individuals with type 2 diabetes. Medicine. 2019;98(43):1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chung JO, Park S, Cho DH, Chung DJ, Chung MY. Anemia, bilirubin, and cardiovascular autonomic neuropathy in patients with type 2 diabetes. Medicine. 2017;96(15):1–4. doi: 10.1097/MD.0000000000006586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hosseini MS, Rostami Z. Anemia and Microvascular Complications in Patients With Type 2 Diabetes Mellitus. Nephro Urol Mon. 2014;6(4):1–7. doi: 10.5812/numonthly.19976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Praveen M, Jain N, Raizada N, Sharma S, Narang S, Madhu SV. Anaemia in patients with type 2 diabetes mellitus without nephropathy is related to iron de fi ciency. Diabetes Metab Syndr Clin Res Rev. 2020;14:1837–1840. doi: 10.1016/j.dsx.2020.09.020 [DOI] [PubMed] [Google Scholar]
- 32.Rathore S, Singh PK, Kumar A. Anemia in Type 2 Diabetes Mellitus (T2dm) and its association with vitamin B12 deficiency. India n J Pathol Oncol. 2018;5(1):51–54. [Google Scholar]
- 33.Bekele A, Roba KT, Egata G, Id BG. Anemia and associated factors among type-2 diabetes mellitus patients attending public hospitals in Harari Region, Eastern Ethiopia. PLoS One. 2019;14(12):1–17. doi: 10.1371/journal.pone.0225725 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Arkew M, Yemane T, Mengistu Y, Gemechu K, Tesfaye G. Hematological parameters of type 2 diabetic adult patients at Debre Berhan Referral Hospital, Northeast Ethiopia: a comparative cross-sectional study. PLoS One. 2021;16(6):1–15. doi: 10.1371/journal.pone.0253286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ebrahim H, Fiseha T, Ebrahim Y, Bisetegn H. Comparison of hematological parameters between type 2 diabetes mellitus patients and healthy controls at Dessie comprehensive specialized hospital, Northeast Ethiopia: comparative cross-sectional study. PLoS One. 2022;17(7):1–15. doi: 10.1371/journal.pone.0272145 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kebede SA, Tusa BS, Weldesenbet AB. Prevalence of Anaemia and Its Associated Factors among Type 2 Diabetes Mellitus Patients in University of Gondar Comprehensive Specialized Hospital. Hindawi. 2021;2021:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.B-B H, Xu M, Wei L, et al. Relationship between Anemia and Chronic Complications in Chinese Patients with Type 2 Diabetes Mellitus. Arch Iran Med. 2015;18(5):277–283. [PubMed] [Google Scholar]
- 38.Wu F, Jing Y, Tang X, Li D, Gong L, Zhao H. Anemia: an independent risk factor of diabetic peripheral neuropathy in type 2 diabetic patients. Acta Diabetol. 2017;54:925–931. doi: 10.1007/s00592-017-1025-7 [DOI] [PubMed] [Google Scholar]
- 39.Srivastava PM, Thomas MC, Calafiore P, Isaac RJMAC, Jerums G, Burrell LM. Diastolic dysfunction is associated with anaemia in patients with Type II diabetes. Clin Sci. 2006;110:109–116. doi: 10.1042/CS20050184 [DOI] [PubMed] [Google Scholar]
- 40.Feteh VF, Choukem S, Kengne A, Nebongo DN. Anemia in type 2 diabetic patients and correlation with kidney function in a tertiary care sub-Saharan African hospital: a cross-sectional study. BMC Nephrol. 2016;17(29):1–7. doi: 10.1186/s12882-016-0247-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ezenwaka CE, Jones-lecointe A, Nwagbara E, Seales D, Okali F. Anaemia and kidney dysfunction in Caribbean Type 2 diabetic patients. Cardiovasc Diabetol. 2008;7(25):1–6. doi: 10.1186/1475-2840-7-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Brière M, Diedisheim M, Dehghani L, Dubois-laforgue D, Larger E. Anaemia and its risk factors and association with treatments in patients with diabetes: a cross-sectional study. Diabetes Metab. 2020;46:1–20. doi: 10.1016/j.diabet.2019.02.003 [DOI] [PubMed] [Google Scholar]
- 43.Grossman C, Koren-morag N, Leibowitz A, Saba K. Diabetes mellitus with normal renal function is associated with anaemia. Diabetes Metab Res Rev. 2014;30:291–296. doi: 10.1002/dmrr.2491 [DOI] [PubMed] [Google Scholar]
- 44.Idris I, Tohid H, Muhammad NA, et al. Anaemia among primary care patients with type 2 diabetes mellitus (T2DM) and chronic kidney disease (CKD): a multicentred cross-sectional study. BMJ Open. 2018;8:1–9. doi: 10.1136/bmjopen-2018-025125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sarosh I, Ghafoor R, Haseeb A, Saeed J, Shafqat F, Kashif Z. Frequency of Anemia and its Types in Type II Diabetes Mellitus Patients without Renal Insufficiency. PJMHS. 2022;16(6):216–218. doi: 10.53350/pjmhs22166216 [DOI] [Google Scholar]
- 46.Al-ghazaly J, Al-dubai W. Pattern and causes of anemia in Yemeni patients with type 2 Diabetes Mellitus. Eur J Biomed Pharm Sci. 2019;6(1):57. [Google Scholar]
- 47.Chiou TT, Lee J, Wang M, et al. Genetic disposition and modifiable factors independently associated with anemia in patients with type 2 diabetes mellitus. Diabetes Res Clin Pract. 2015;1:1–6. [DOI] [PubMed] [Google Scholar]
- 48.Bonakdaran S, Gharebaghi M, Vahedian M. Prevalence of Anemia in Type 2 Diabetes and Role of Renal Involvement. Saudi J Kidney Dis Transpl. 2011;22(2):286–290. [PubMed] [Google Scholar]
- 49.Solomon D, Bekele K, Atlaw D, et al. Prevalence of anemia and associated factors among adult diabetic patients attending Bale zone hospitals, South-East Ethiopia. PLoS One. 2022;17(2):1–14. doi: 10.1371/journal.pone.0264007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Abate A, Birhan W, Alemu A. Association of anemia and renal function test among diabetes mellitus patients attending Fenote Selam Hospital, West Gojam, Northwest Ethiopia: a cross sectional study. BMC Blood Disord. 2013;13(1):1. doi: 10.1186/2052-1839-13-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186 [DOI] [PubMed] [Google Scholar]
- 52.Egger M, Smith GD, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–634. doi: 10.1136/bmj.315.7109.629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Begg CB, Mazumdar M. Operating Characteristics of a Rank Correlation Test for Publication Bias. Biometrics. 1994;50(4):1088–1101. doi: 10.2307/2533446 [DOI] [PubMed] [Google Scholar]
- 54.Gardner W, Kassebaum N. Global, Regional, and National Prevalence of Anemia and Its Causes in 204 Countries and Territories, 1990–2019. Curr Dev Nutr. 2020;4:830. [Google Scholar]
- 55.Balarajan Y, Ramakrishnan U, Özaltin E, Shankar AH, Subramanian SV. Anaemia in low-income and middle-income countries. Lancet. 2011;378(9809):2123–2135. doi: 10.1016/S0140-6736(10)62304-5 [DOI] [PubMed] [Google Scholar]
- 56.Hamer M, Batty GD, Kengne AP, Stamatakis E. Anaemia, Haemoglobin Level and Cause-Specific Mortality in People with and without Diabetes. PLoS One. 2012;7(8):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Atlaw D, Tariku Z. Magnitude and factors associated with anemia among diabetic patients in Ethiopia: a systematic review and meta-analysis. SAGE Open Med. 2021;9:1–11. doi: 10.1177/20503121211031126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Azevedo M, Alla S. Diabetes in sub-saharan Africa: Kenya, Mali, Mozambique, Nigeria, South Africa and Zambia. Int J Diabetes Dev Ctries. 2008;28(4):101–108. doi: 10.4103/0973-3930.45268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Deng Y, Li N, Wu Y, et al. Global, Regional, and National Burden of Diabetes-Related Chronic Kidney Disease From 1990 to 2019. Front Endocrinol (Lausanne). 2021;12:1–15. doi: 10.3389/fendo.2021.672350 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Fishbane S, Spinowitz B. Update on Anemia in ESRD and Earlier Stages of CKD: core Curriculum 2018. Am J Kidney Dis. 2018;71(3):423–435. doi: 10.1053/j.ajkd.2017.09.026 [DOI] [PubMed] [Google Scholar]
- 61.Kyoung M, Hyun K, Jun D, et al. Erythropoietin response to anemia and its association with autonomic neuropathy in type 2 diabetic patients without advanced renal failure. J Diabetes Complications. 2010;24(2):90–95. doi: 10.1016/j.jdiacomp.2009.02.002 [DOI] [PubMed] [Google Scholar]
- 62.Neamţu MC, Crăiţoiu Ş, Avramescu ET, et al. The prevalence of the red cell morphology changes in patients with type 2 diabetes mellitus. Rom J Morphol Embryol. 2015;56(1):183–189. [PubMed] [Google Scholar]
- 63.Cho YI, Mooney MP, Cho DJ. Hemorheological disorders in diabetes mellitus. J Diabetes Sci Technol. 2008;2(6):1130–1138. doi: 10.1177/193229680800200622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Abdel N, Hamed M. Alterations in hematological Parameters: could it be a marker in diabetes mellitus ? BAOJ Diabet. 2016;2(1):1–9. [Google Scholar]
- 65.Al-sharefi A, Mohammed A, Abdalaziz A, Jayasena CN, Al-sharefi A. Androgens and Anemia: current Trends and Future Prospects. Front Endocrinol (Lausanne). 2019;10:1–5. doi: 10.3389/fendo.2019.00754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Osterholm EA, Georgieff MK. Chronic Inflammation and Iron Metabolism. J Pediatr. 2016;166(6):1351–1357. doi: 10.1016/j.jpeds.2015.01.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Weiss G, Ganz T, Goodnough LT. Anemia of inflammation: iron metabolism and its disorders. Blood. 2019;133(1):40–50. doi: 10.1182/blood-2018-06-856500 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Bilgin S, Kurtkulagi O, Atak Tel BM, et al. Does C-reactive protein to serum Albumin Ratio correlate with diabEtic nephropathy in patients with Type 2 dIabetes MEllitus? The CARE TIME study. Prim Care Diabetes. 2021;15(6):1071–1074. doi: 10.1016/j.pcd.2021.08.015 [DOI] [PubMed] [Google Scholar]
- 69.Gulali A, Edip E, et al. Neuregulin-4 is associated with plasma glucose and increased risk of type 2 diabetes mellitus. Swiss Med Wkly. 2019;149:1–5. [DOI] [PubMed] [Google Scholar]
- 70.Kocak MZ, Aktas G, Duman TT, et al. Monocyte lymphocyte ratio as a predictor of diabetic kidney injury in type 2 diabetes mellitus; The MADKID Study. J Diabetes Metab Disord. 2020;19:997–1002. doi: 10.1007/s40200-020-00595-0 [DOI] [PMC free article] [PubMed] [Google Scholar]