Abstract
BACKGROUND:
Although digital learning devices have become increasingly more common in medical education settings, it remains unclear how they influence medical student learning styles and various outcome measures. This study aimed to assess student learning styles, specifically as they relate to digital dependency, writing habits, and group learning practices among current medical students.
MATERIALS AND METHODS:
This questionnaire study was approved by the Research Ethics Committee of Osaka Medical and Pharmaceutical University. We conducted a questionnaire survey of 109 medical students who were 5th year students during the 2021 school year. Medical students were asked about their level of digital dependency, writing by hand, and group learning practices. We also analyzed the correlation between student learning styles and their respective outcomes on several summative evaluations.
RESULTS:
Of the 109 students targeted, we received responses from 62 (response rate, 56.8%). Among the respondents, digital dependency was 83.4 ± 18.6%, while hand writing ratio 39.8 ± 29.9% and group learning ratio 33.5 ± 30.5%. We also assessed correlations between these learning styles and scores on the CBT, OSCE, CC, and CC Integrative Test. Only writing by hand showed a small positive correlation with CC Integrative Test scores.
CONCLUSION:
Our questionnaire survey assessed the rates of digital dependency, writing by hand, and group learning practices, and analyzed the correlations between these learning styles and respective outcomes. Current medical students exhibited high digital dependency which was not correlated with performance outcomes.
Keywords: Achievement, learning, outcome
Introduction
Digital transfer in the medical environment refers to the application of information and communication technologies (ICTs) to support health and health care.[1,2] Such technologies can support clinical and administrative processes, facilitate access to medical or healthcare services, and enable patients to monitor and manage their own health.[3,4] Examples include electronic medical records, videoconferencing technology, and wearable devices such as mobile applications or virtual/augmented reality.[5]
Digital technology has also dramatically changed learning in medical education systems worldwide. Before the 2010s, writing by hand was the conventional learning style in medical classrooms and for self-learning. Conventional group learning remains an important method for active learning in medical education. While digital device learning is typically an individual learning activity, group learning can effectively facilitate active learning in medical education.[6,7]
Currently, medical students tend to take notes, or summarize various knowledge primarily via digital devices, rather than writing by hand. While this shift toward digital dependency is observed widely in most medical schools, very few studies have explored how it affects medical student learning style, competency, or performance outcomes. Thus, learning style evaluation in present medical student is warranted. Accordingly, we performed a questionnaire survey to assess the utility rates and attitudes toward digital dependency, writing by hand, and group learning practices. We then performed a correlation analysis between these learning styles and performance outcomes on multiple choice tests, Clinical Clerkship (CC) performance, and the Objective Structured Clinical Examination (OSCE).
Materials and Methods
Study design and setting
We conducted a questionnaire survey to medical students who were 5th year students during the 2021 school year. As is the case for most medical schools in Japan, Osaka Medical and Pharmaceutical University requires its students to take the CBT and OSCE midway through their 4th year, before they enter into core CCs in the 4th and 5th years. The 5th year CC Integrative Test was performed at the end of the 5th year [Figure 1]. After completing these common curricula, students take the selective advance CC from the end of the 5th year, completing it midway into the 6th year.
Figure 1.
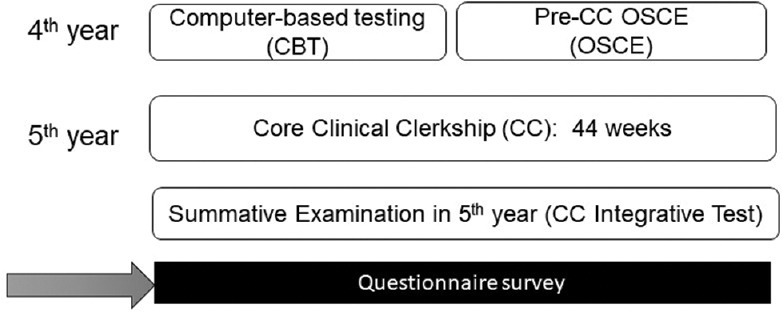
Curriculum timeline for the CBT, OSCE, CC, and CC Integrative test
CBT content
The Common Achievement Test Organization (CATO), established as a third party in 2005, introduced the CBT to evaluate basic medical knowledge before the CC in Japan.[8] The CBT consists of 320 multiple choice questions about basic clinical knowledge which are answered over the course of six hours. The CBT covers clinical disciplines and relevant basic medical knowledge.[9]
Pre-CC OSCE content and evaluation
In 2005, the CATO also introduced the Pre-CC OSCE to evaluate basic medical knowledge. The Pre-CC OSCE evaluates different aspects of student clinical competency for items such as the medical interview, head and neck examination, chest examination, abdominal examination, neurological examination, emergency response, and basic clinical technique. The Pre-CC OSCE is carried out at seven stations; one station (the medical interview) is 10 minutes long, while the remaining six (physical examinations and basic skills) are five minutes each.[10] During their allotted time at each station (five or 10 minutes), students perform core clinical skills such as the medical interview and physical examination. Scores for each component of the Pre-CC OSCE are calculated as the average of the scores given by two examiners. Examiners evaluate the communication, medical safety, and consultation skills on a checklist. Each student visits each of the seven skill stations, and their total score is calculated as the average of the seven skills. Student identity is strictly monitored through validation of examinee name and ID number. Examiners from other universities are routinely invited to validate internal evaluations for the OSCE.
Core CC content
Medical students participate in a core CC during their 4-5th years. For the core CC, students participate in CCs of all clinical departments of the hospital over the course of 44 weeks. Core CCs recommend medical students to participate as members of a medical team to perform actual medical procedures with supervising doctors. The range of medical procedures that can be performed by students is defined and carried out under the supervision of an instructing doctor.[11,12]
Supervising doctors of each department evaluate the clinical skills of students utilizing an evaluation sheet based on the Direct Observation of Procedural Skills (DOPS) and mini-CEX.[13,14] Evaluations are based on three essential components: a 5-point evaluation sheet (80%), subjective evaluation by the organizer (10%), and a written report (10%).
After scores for each CC are collected, an average score is calculated. All medical students are required to participate in the core CC.
5th Year integrative test (CC Integrative Test)
The 5th year integrative test is performed after the core CC and takes approximately seven hours to complete. This scantron test consists of multiple (five) choice questions and extended matching items, and students are required to answer 244 questions related to clinical knowledge.
Study participants and sampling
We evaluated 109 students of Osaka Medical and Pharmaceutical University who were 5th year medical students in 2021 academic year. Our study population included no minors, as all 5th year medical students in Japan are aged >22 years.
Data collection tool and technique
The content of our web-based questionnaire survey is shown in Table 1. Medical students responded with the percentage of their learning time spent in the various formats (Q1-Q3) Questionnaire contents were evaluated by three medical education professionals and a pilot test was performed by seven medical clerks in our center. The total time required to answer all questions was roughly five minutes per individual. The survey was administered in on the morning of April 1, 2022.
Table 1.
Questions related to digital dependency or learning habits
| Q1 | How much do you use ICT devices to study? |
|---|---|
| Q2 | How much do you write by hand to study? |
| Q3 | How much time do you spend in group learning? |
Ethical consideration
This study was approved by the Research Ethics Committee of Osaka Medical and Pharmaceutical University (No. 2021-135). Participation in the questionnaire was entirely voluntary and did not influence any student performance outcomes. Respondents were informed of the nature and purpose of the questionnaire and that their anonymity was guaranteed. Students were also informed that they were free to withdraw from the study if they notified the investigator via the university E-mail for about 1 month. Electronic data on student performance were collected from our university records.
Data analysis
Statistical analysis was performed using JMP® 11 (SAS Institute Inc., Cary, NC, USA). Data are presented as mean ± SD. Results were compared using Pearson's correlation test.[15]
Results
Of the 109 5th year medical students asked to complete the survey, 62 submitted responses (response rate, 56.9%). None of the students asked for their data to be excluded from the analysis during the opt-out period. Achievement scores for the CBT, OSCE, CC, and CC Integrative Test are shown in Table 2.
Table 2.
Student scores (%) for the OSCE, CBT, Clinical Clerkship, and CC Integrative Test (n=62)
| OSCE | CBT | Clinical Clerkship | CC Integrative Test | |
|---|---|---|---|---|
| Average | 84.6 | 526.6 | 77.5 | 72.5 |
| SD | 6.2 | 68.9 | 2.7 | 6.7 |
Percentages of time spent in digital learning, writing by hand, and group learning are shown in Figure 2. Digital dependency percentage was 83.4 ± 18.6%, while that for writing by hand was 39.8 ± 29.9% and group learning 33.5 ± 30.5%.
Figure 2.
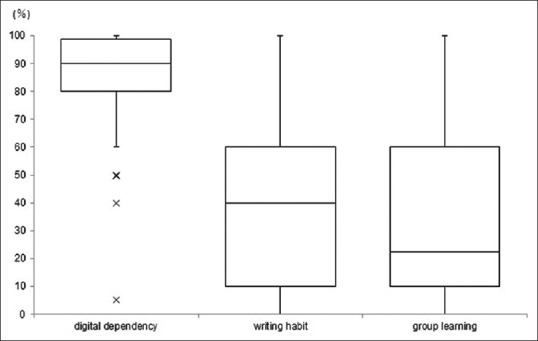
Box-and-whisker plots (median, IQR, and range) for the percentages of time spent learning using digital devices, writing by hand, and group learning among 5th year medical students in Japan
We also assessed the correlation between these learning styles and scores for the CBT, OSCE, CC, and CC Integrative Test [Table 3a-c]. Only writing by hand showed a small positive correlation with scores of the CC Integrative Test.
Table 3.
Correlation analysis of medical students’ learning style and student performance outcomes on the OSCE, CBT, Clinical Clerkship, and CC Integrative Test
| OSCE | CBT | Clinical Clerkship | CC Integrative Test | |
|---|---|---|---|---|
| (a) Correlation between ICT device dependency and student performance outcomes. | ||||
| r | -0.107 | -0.100 | 0.123 | -0.088 |
| (b) Correlation between writing by hand and student performance outcomes. | ||||
| r | 0.174 | 0.193 | 0.139 | 0.202 |
| (c) Correlation between group learning and student performance outcomes. | ||||
| r | -0.057 | 0.074 | -0.006 | 0.145 |
Discussion
The digital age has brought about numerous changes in various aspects of both clinical and basic medicine as a byproduct of progress in ICT technology, including data science, and artificial intelligence technology.[16,17] The COVID-19 pandemic dramatically accelerated this trend toward digitalization in medical education through the introduction of remote classes and training.[18] We medical educators are now concerned that some students might try to acquire various medical competencies solely through digital learning devices,[19,20] avoiding altogether the use of conventional writing devices such as pencils or notebooks. Our fear is that this one-directional learning using digital devices will not facilitate active learning in students, who must acquire a deep understanding of clinical medicine.
Digital learning devices facilitate the acquisition of clinical skills by providing large amounts of image-based information. However, even when attaining clinical skills, students need to perform some active learning such as simulation training to acquire relevant competencies.
The present study found that the average digital device dependency in medical students is 80%, with only 40% accounting for writing by hand, revealing some inherent tendencies of medical students of the current era. First, digital dependency is extremely high in these medical students. Second, some medical students learn using both ICT devices and writing by hand simultaneously. Notably, high digital dependency may be associated with low group learning tendencies. With regard to any correlations with performance outcomes, only writing by hand showed a small correlation with scores on the 5th year integrative test. As this test is a multiple choice test and includes complex information, those who write by hand may have benefited from increased active learning.
New educational technologies will always influence existing human competencies in various ways.[21,22] Accordingly, we should be aware of the inherent risks of using digital devices in medical education.[23] Some studies have found that excessive use of digital devices can give rise to depressive symptoms, sleep disorders, or learning disabilities.[24,25] As the medical students evaluated in the present study were likely to have studied primarily by writing by hand through high school, this drastic change in learning style in medical school could create some confusion. Medical school instructors should be cognizant of these learning style changes or gaps in learners and instruct accordingly. Furthermore, we should evaluate active learning skills in our students particularly during this developing digital era, striving to find appropriate ways to maximize the benefits and minimize the drawbacks of using digital devices to study medicine.
Limitation and recommendation
This study has several limitations worth noting. First, while the outcome measure was a summative evaluation of core CC performance, it is worth mentioning that medical students rotate through numerous subject areas and are assessed on a wide variety of skills.[26] Second, we did not include question regarding reading books. As reading a paper book or dictionary is a classical method of study, it is warranted to evaluate the proportion of digital and paper ones in the future study. Third, the response rate among our study population was 56.8%; receiving responses from non-respondents could have impacted our final results. Finally, as the data came from a single institution and relatively low small samples, our findings may not be generalizable to other medical schools.[27] However, we believe our results are fairly representative of students at most other Japanese medical schools as they all follow the main core curriculum provided by the Ministry of Education. In the future study, multi-medical college analysis including postgraduate clinical performance and their relationships with undergraduate factors is warranted.
Conclusions
We conducted a questionnaire survey to understand percentage of time spent in learning using digital devices, writing by hand, and group learning among medical students. We also assessed the correlation between these percentages and performance outcomes including multiple choice tests, CC performance, and the OSCE. Only writing by hand showed a small correlation with scores on the 5th year integrative test, with no other learning style showing any significant correlation with summative test scores. Those instructing medical students in the current era should be aware of the strong digital dependency of these students, while also noting that this dependency does not correlate with performance outcomes.
Financial support and sponsorship
Financial support for the study was provided by Osaka Medical and Pharmaceutical University, which played no role in study design, data collection and analysis, publication decisions, or manuscript preparation.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors would like to express gratitude to the medical students of the Osaka Medical and Pharmaceutical University who participated in this study.
References
- 1.Kuijpers W, Groen WG, Aaronson NK, van Harten Wim A. systematic review of web-based interventions for patient empowerment and physical activity in chronic diseases: Relevance for cancer survivors. J Med Internet Res. 2013;15:e37. doi: 10.2196/jmir.2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lin Y, Lemos M, Neuschaefer-Rube C. Digital health and digital learning experiences across speech-language pathology, phoniatrics, and otolaryngology: Interdisciplinary survey study. JMIR Med Educ. 2021;7:e30873. doi: 10.2196/30873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ariens LF, Schussler-Raymakers FM, Frima C, Flinterman A, Hamminga E, Arents BW, et al. Barriers and facilitators to eHealth use in daily practice: Perspectives of patients and professionals in dermatology. J Med Internet Res. 2017;19:e300. doi: 10.2196/jmir.7512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Li J, Talaei-Khoei A, Seale H, Ray P, Macintyre CR. Health care provider adoption of ehealth: Systematic literature review. Interact J Med Res. 2013;2:e7. doi: 10.2196/ijmr.2468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tudor Car L, Kyaw BM, Nannan Panday RS, van der Kleij R, Chavannes N, Majeed A, et al. Digital health training programs for medical students: Scoping review. JMIR Med Educ. 2021;7:e28275. doi: 10.2196/28275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dhar P, Rocks T, Samarasinghe RM, Stephenson G, Smith C. Augmented reality in medical education: Students' experiences and learning outcomes. Med Educ Online. 2021;26:1953953. doi: 10.1080/10872981.2021.1953953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Majumder MAA, Gaur U, Singh K, Kandamaran L, Gupta S, Haque M, et al. Impact of COVID-19 pandemic on radiology education, training, and practice: A narrative review. World J Radiol. 2021;13:354–70. doi: 10.4329/wjr.v13.i11.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Komasawa N, Terasaki F, Nakano T, Kawata R. Relationship between objective skill clinical examination and clinical clerkship performance in Japanese medical students. PLoS One. 2020;15:e0230792. doi: 10.1371/journal.pone.0230792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Man K, Harring JR, Jiao H, Zhan P. Joint modeling of compensatory multidimensional item responses and response times. Appl Psychol Meas. 2019;43:639–54. doi: 10.1177/0146621618824853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Horita S, Park YS, Son D, Eto M. Computer-based test (CBT) and OSCE scores predict residency matching and National Board assessment results in Japan. BMC Med Educ. 2021;21:85. doi: 10.1186/s12909-021-02520-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kato D, Wakabayashi H, Takamura A, Takamura YC. Identifying the learning objectives of clinical clerkship in community health in Japan: Focus group. J Gen Fam Med. 2019;21:3–8. doi: 10.1002/jgf2.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Durning SJ, Artino AR, Jr, Pangaro LN, van der Vleuten C, Schuwirth L. Redefining context in the clinical encounter: Implications for research and training in medical education. Acad Med. 2010;85:894–901. doi: 10.1097/ACM.0b013e3181d7427c. [DOI] [PubMed] [Google Scholar]
- 13.Martinsen SSS, Espeland T, Berg EAR, Samstad E, Lillebo B, Slørdahl TS. Examining the educational impact of the mini-CEX: A randomised controlled study. BMC Med Educ. 2021;21:228. doi: 10.1186/s12909-021-02670-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lörwald AC, Lahner FM, Nouns ZM, Berendonk C, Norcini J, Greif R, et al. The educational impact of mini-clinical evaluation exercise (Mini-CEX) and direct observation of procedural skills (DOPS) and its association with implementation: A systematic review and meta-analysis. PLoS One. 2018;13:e0198009. doi: 10.1371/journal.pone.0198009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Komasawa N, Terasaki F, Nakano T, Kawata R. Correlation of student performance on clerkship with quality of medical chart documentation in a simulation setting. PLoS One. 2021;16:e0248569. doi: 10.1371/journal.pone.0248569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Silén C, Wirell S, Kvist J, Nylander E, Smedby O. Advanced 3D visualization in student-centred medical education. Med Teach. 2008;30:e115–24. doi: 10.1080/01421590801932228. [DOI] [PubMed] [Google Scholar]
- 17.Venail F, Deveze A, Lallemant B, Guevara N, Mondain M. Enhancement of temporal bone anatomy learning with computer 3D rendered imaging software. Med Teach. 2010;32:e282–8. doi: 10.3109/0142159X.2010.490280. [DOI] [PubMed] [Google Scholar]
- 18.Ahmady S, Kallestrup P, Sadoughi MM, Katibeh M, Kalantarion M, Amini Am, et al. Distance learning strategies in medical education during COVID-19: A systematic review. J Educ Health Promot. 2021;10:421. doi: 10.4103/jehp.jehp_318_21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Poulton T, Conradi E, Kavia S, Round J, Hilton S. The replacement of 'paper' cases by interactive online virtual patients in problem-based learning. Med Teach. 2009;31:752–8. doi: 10.1080/01421590903141082. [DOI] [PubMed] [Google Scholar]
- 20.Chi DL, Pickrell JE, Riedy CA. Student learning outcomes associated with video vs. paper cases in a public health dentistry course. J Dent Educ. 2014;78:24–30. [PubMed] [Google Scholar]
- 21.Balslev T, de Grave WS, Muijtjens AM, Scherpbier AJJA. Comparison of text and video cases in a postgraduate problem-based learning format. Med Educ. 2005;39:1086–92. doi: 10.1111/j.1365-2929.2005.02314.x. [DOI] [PubMed] [Google Scholar]
- 22.Conradi E, Kavia S, Burden D, Rice A, Woodham L, Beaumont C, et al. Virtual patients in a virtual world: Training paramedic students for practice. Med Teach. 2009;31:713–20. doi: 10.1080/01421590903134160. [DOI] [PubMed] [Google Scholar]
- 23.Hudson JN. Computer-aided learning in the real world of medical education: Does the quality of interaction with the computer affect student learning? Med Educ. 2004;38:887–95. doi: 10.1111/j.1365-2929.2004.01892.x. [DOI] [PubMed] [Google Scholar]
- 24.Kerfoot BP, Masser BA, Hafler JP. Influence of new educational technology on problem-based learning at Harvard Medical School. Med Educ. 2005;39:380–7. doi: 10.1111/j.1365-2929.2005.02105.x. [DOI] [PubMed] [Google Scholar]
- 25.Lissak G. Adverse physiological and psychological effects of screen time on children and adolescents: Literature review and case study. Environ Res. 2018;164:149–57. doi: 10.1016/j.envres.2018.01.015. [DOI] [PubMed] [Google Scholar]
- 26.Kuroda N, Suzuki A, Ozawa K, Nagai N, Okuyama Y, Koshiishi K, et al. Predicting the effectiveness of the online clinical clerkship curriculum: Development of a multivariate prediction model and validation study. PLoS One. 2022;17:e0263182. doi: 10.1371/journal.pone.0263182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kind T, Olvet DM, Farina G, Kenda L, Sarandos SL, Yasunaga AJ, et al. Reading and study habits of medical students on clerkships and performance outcomes: A multi-institutional study. Med Sci Educ. 2021;31:1957–66. doi: 10.1007/s40670-021-01409-5. [DOI] [PMC free article] [PubMed] [Google Scholar]


