Abstract
To study the anatomical orientation of the posterior group of calyces based on reconstructed images of computerized tomography urography (CTU) and provide a novel classification with its clinical significance. Clinical data of a total of 1321 patients, who underwent CTU examination in our hospital were retrospectively analyzed. Among these, a total of 2642 3-dimensional reconstructed images of CTU scans were considered in this study. Based on the morphology of the renal calyces and the influence on the establishment of surgical access, the posterior group renal calyces are classified into 3 major types including pot-belly type, classically branched and elongated branched. The classically branched type is further classified into 3 sub-types: a, b and c, based on the association of minor calyces of the posterior group to the major calyces. Type a is derived from 1 group of major calyces only, type b is derived from 2 groups of major calyces simultaneously, and type c is derived from 3 groups of major calyces simultaneously. Statistical findings revealed that all kidneys possess posterior group calyces. The percentage of occurrence of pot-belly type, classically branched and elongated branched is 8.06%, 73.13%, and 18.81%, respectively. The anatomical typing of the classical branching type occurred in 19.36%, 68.17%, and 12.47% for types a, b, and c, respectively. In this study, the posterior group calyces were found to be present across all patients. The posterior group calyces were highest in the classical branching type, of which anatomical typing was highest in type b. The typing of the posterior group of calyces could provide an anatomical basis for percutaneous nephrolithotomy (PCNL) puncture from the posterior group.
Keywords: anatomical typing, collecting system, posterior renal calyces, 3-dimensional reconstruction
1. Introduction
The anatomical structure of posterior renal calyces has not been well-studied. Sampaio classification is the only known classification of renal calyces, wherein pelvicalyceal patterns are grouped according to the drainage of the renal collecting system using statistical analysis of cadaveric renal perfusion model.[1] Urolithiasis is one of the most common urological diseases, with the occurrence of upper urinary tract stones reported in approximately 80% of cases.[2] Percutaneous nephrolithotomy (PCNL) is a minimally invasive technique widely used in the treatment of upper urinary tract stones. It is the first line of treatment for complex kidney stones.[3]
An establishment of puncture access is crucial in the procedure of PCNL. An efficient percutaneous renal access depends on the anatomy of the renal collecting system.[4] The anatomy of the renal collecting system is extremely complex, and its association with the establishment of PCNL access is poorly understood.[5,6] PCNL is traditionally performed in a prone position. The establishment of percutaneous renal access through the posterior group of renal calyces in the prone position could result in the establishment of the shortest percutaneous renal tract, which is an efficient percutaneous renal surgical access. The anatomical structure of the posterior group calyces plays a major role in the establishment of PCNL access in a prone position. Therefore, it is important to study the anatomical typing of the posterior renal calyces for the selection of the prone PCNL puncture route.[7]
In this study, we retrospectively analyzed the imaging data of patients who underwent a computerized tomography urography (CTU) examination at the People Hospital of Wuhan University from April 2020 to June 2021. We performed a 3-dimensional reconstruction of the collecting system and a subsequent anatomical typing of the posterior renal calyces to understand the anatomy of the collecting system, which in turn would help in the establishment of a prone PCNL operation access.
2. Patients and methods
2.1. General data
A total of 1321 cases, who came to our hospital from April 2020 to December 2022, were considered in this study including 673 male and 648 female patients, aged 18 to 77 years with a mean age of 51.7 ± 10.2 years. The CTU images of all the patients under consideration clearly represented the collecting system on both sides. A total of 1176 patients showed the presence of a normal collecting system, while a total of 145 patients showed mild hydronephrosis and the presence of stones with a maximum diameter of 1.73 ± 0.78 cm. Patients that exhibited the following conditions were excluded from the study: Patients with a previous history of renal surgery, moderate or severe hydronephrosis in both kidneys, duplex moiety, solitary kidney, and scarred pyelonephritic kidney.
The procedures followed in this study were in accordance with the requirements of the World Medical Association Declaration of Helsinki, revised in 2013. The Ethics Committee of Wuhan University Renmin Hospital approved the study.
2.2. 3D reconstruction method of the collecting system
The CTU scan was performed using a 256-slice spiral CT (GE Healthcare, Chicago, IL) with a scan pitch of 5 mm, an acquisition layer thickness of 0.625 mm, a reconstruction layer thickness of 5 mm, a reconstruction interval of 1 mm, a scan field of 350 mm × 350 mm, and a pitch of 0.992. The results of the scan were then transferred to an AW Volume Share workstation for image post-processing to achieve a pooled system of Stereo reconstruction. The reconstructed images were then rearranged to simulate a prone position based on anatomical landmarks such as the spine and ribs. The images were then reviewed by experienced urologists to observe the posterior group of calyces.
2.3. Observation index
The pooling system was established under a simulated prone position. The anatomical relationship between the right and left pelvic calyces, the number of renal major calyces, the number and orientation of the posterior group of renal minor calyces, and the subordinate relationship with the renal major calyces were independently studied.
In this study, the posterior group of calyces was characterized as calyces facing dorsally with an opening angle ≥30° to the coronal plane.
2.4. Posterior group fractal criteria
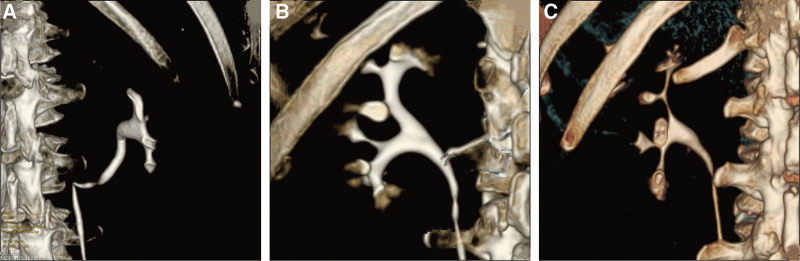
Based on the morphology of the renal calyces and their influence on the establishment of surgical access, the posterior group of renal calyces was classified into 3 different types (Fig. 1A~C). Pot-belly type: the renal pelvis is shaped like a pot-belly, and is directly associated with cup-shaped minor calyces in the absence of a distinct renal major calyx. Classic branched type: in this type of posterior group of renal calyces, ≥2 renal major calyces branch to form the renal pelvis. Elongated branched type: major renal calyces were branched, with at least 1 major calyceal axis of ≥0.9 cm length and ≤0.3 cm neck width.
Figure 1.
Morphological classification of the posterior group of calyces on 3D reconstruction images. (A) Pot-belly type: the renal pelvis is shaped like a pot-belly, and the renal pelvis is directly connected to the cup-shaped renal minor calyces without a distinct renal major calyce. (B) Classic branched type: ≥2 renal major calyces are branched to form a renal pelvis. (C) Elongated branched type: the renal major calyces were branched, with at least 1 major calyceal axis length ≥0.9 cm and neck width ≤0.3 cm.
The pot-belly type has a very short calyx neck, which has an insignificant influence on the surgical path. The elongated branched type has a long and slender minor calyx, which is difficult to offset and difficult to remove multiple calyx stones with a single access, often requiring multiple accesses. The classical branched type occurs in the highest proportion. There is a need for single-channel treatment of multiple stones, which demands a thorough understanding of the relationship between different calyces to facilitate the establishment of efficient puncture paths. Therefore, in this study, we have addressed the anatomical and morphological typing of the classical branched type.
Based on the association of the posterior renal minor calyces to the renal major calyces, the classical branching type can be further classified into 3 different types: a, b, and c with a total of 7 subtypes (Fig. 2A~G). The “a type” is comprised of 3 subtypes, wherein the posterior group of renal minor calyces is only associated with an upper group of renal major calyces for type a1, with only the middle group of renal major calyces for type a2, and with the lower group of renal major calyces for type a3. The “b type” type is also classified into 3 subtypes, wherein the posterior group of renal minor calyces is associated with both the upper and middle group of renal major calyces for type b1, with both the middle and lower group of renal major calyces in type b2, and with both upper and lower group of renal major calyces in type b3. Type c posterior group of renal minor calyces is associated with an upper, middle, and lower group of renal major calyces without any subtypes.
Figure 2.
3D reconstructed images representing anatomical typing of the classical branching type. (A) Type a1, the posterior group of minor calyces originates only from the upper group of major calyces. (B) Type a2, the posterior group of minor calyces originates only from the middle group of major calyces. (C) Type a3, posterior group of minor calyces originates only from the lower group of major calyces. (D) Type b1, posterior group of minor calyces originates only from the upper and middle groups of major calyces. (E) Type b2, the posterior group of minor calyces originates only from the middle and lower groups of major calyces. (F) Type b3, the posterior group of minor calyces originates only from the upper and lower group of major calyces. (G) Type c, the posterior group of minor calyces originates from the upper, middle, and lower groups of major calyces.
3. Results
In this study, the occurrence of kidneys with 2 renal major calyces, upper and lower was found to be 74.68% (1973/2642). The occurrence of kidneys with 3 renal major calyces, upper, middle, and lower was 25.32% (669/2642). Amongst the 1321 cases in this study, a total of 1052 (79.64%) cases showed notable differences in the typing of the posterior group of renal calyces on the left and right sides, and only a total of 269 cases (20.36%) exhibited identical typing bilaterally (Fig. 3A~B). Posterior group calyces were present in all renal collecting systems. The morphological typing of posterior group calyces indicated that the percentage of occurrence of pot-bellied, classically branched, and elongated branched types were 8.06% (213/2642), 73.13% (1932/2642), and 18.81% (497/2642), respectively. The number of posterior groups of minor calyces was predominantly 2 in the pot-bellied type and 3 in the classical branched and elongated-branched types (Table 1).
Figure 3.
Consistent fractionation and morphology of the posterior group of calyces on the left and right sides of the same patient. (A) Left side; (B) Right side.
Table 1.
Number of minor calyces in different morphological types of posterior groups of calyces [number of kidneys (%)].
| Minor renal calyces | Pot-belly type | Classical branched type | Elongated branched type |
|---|---|---|---|
| 1 | 12 (0.45) | 157 (5.94) | 33 (1.25) |
| 2 | 159 (6.02) | 443 (16.77) | 156 (5.9) |
| 3 | 28 (1.06) | 902 (34.15) | 297 (11.24) |
| 4 | 14 (0.53) | 356 (13.47) | 11 (0.42) |
| 5 | 0 | 74 (2.8) | 0 |
Anatomical typing of classical branching type revealed the proportion of a, b, and c types to be 19.36% (374/1932), 68.17% (1317/1932), and 12.47% (241/1932), respectively (Table 2).
Table 2.
Number and percentage of nephrons of the classical branching subtype [number of kidneys (%)].
| Type | Classical branching subtype |
|---|---|
| a1 | 77 (3.99) |
| a2 | 115 (5.95) |
| a3 | 182 (9.42) |
| b1 | 41 (2.12) |
| b2 | 133 (6.88) |
| b3 | 1143 (59.16) |
| c | 241 (12.47) |
4. Discussion
In the 1990s, Sampaio et al classified the renal collecting system based on a statistical analysis of cadaveric renal perfusion models. This was the first attempt to describe the anatomical structure of the infundibulopelvic angle and the distribution of the calyces in the lower pole, which contributed to the effective removal of the stones. Around 26.0% of models exhibited infundibulopelvic angle ≤90°, 60.3% of models had an infundibular diameter ≥4 mm, 39.7% had an infundibular diameter <4 mm, 56.8% had multiple calyces draining, and 43.2% were drained by a single calyx.[8,9] Hodson and Brödel studied the anatomy of the collecting system by perfusing cadaveric kidneys with a liquid plastisol.[10,11] However, their findings contradicted each other regarding the location and orientation of the anterior and posterior groups of calyces. Brödel concluded that the anterior group of calyces was centrally located and pointed to the anterior half of the renal convexity and the posterior group of calyces was laterally located and pointed slightly posterior to the lateral convexity. However, Hodson concluded that the anterior group of calyces was laterally located and pointed slightly anterior to the lateral convexity, and the posterior group was centrally located. By the end of the 20th century, studies on the collecting system were mainly based on cadaveric kidney casts, however, isolated kidneys cannot be easily preserved. Moreover, high-pressure injection of liquid plastisol can lead to the deformation of the collecting system. Cadaveric kidneys have a limited source and small sample size, which could contribute to an increased bias in the results. This could lead to an invalid description of the morphological structure of the collecting system with limited significance for clinical diagnosis and treatment.
Based on the clinical requirements, we proposed a posterior group of renal calyces anatomical typing criteria for prone PCNL. The findings of this study demonstrated that a large amount of clear, intuitive, scientific, and accurate data can be achieved by 3D reconstruction of CTU images of patients. This facilitates a more comprehensive generalization and targeting of the anatomical structure of the posterior group renal calyces in the prone position.
CT is the “gold standard” in the evaluation of kidney stones using an imaging approach. It reveals the relationship between the renal collecting system and stones, stone size, stone texture, and stone-to-skin distance in a multidimensional space.[12,13] The CTU-generated thin layer images of the renal collecting system are post-processed using AW Volume Share workstation to generate 3D images. This facilitates the observation of the spatial structure of the collecting system in a stereoscopic space simulating the patient in a prone position considering anatomical markers such as the spine. This facilitates the observation of the anatomical features of the renal calyces, such as the relationship between the pelvis and calyces, the orientation, and the angle between the branches of the calyces by merely adjusting the reconstructed images. These details help in the identification of different types of calyces.[14,15]
The number and location of renal calyces can provide a reliable anatomical basis for the establishment of safe and efficient percutaneous access for renal manipulation.[16,17] A combination of ultrasound and CT images can help arrive at an accurate diagnosis. A majority of patients with pot-belly type require only single-access puncture to remove stones. The frequently used nephroscope size (not the tract size) in our hospital is 9.5Fr. The procedure is more challenging for the physician in patients with smaller calyx necks. Physicians must consider the presence of an elongated branched type defined by the presence of at least 1 renal major calyx with an axial length ≥0.9 cm and a calyx neck width ≤0.3 cm while designing the surgical equipment and discussing surgical options. As indicated by the results of this study, the proportion of the elongated branched type is higher than that of the pot-belly type. Therefore, patients with multiple stones of elongated branched type often require multichannel puncture owing to the narrow calyx neck and smaller angle between the calyces in the elongated branched type.
Based on our previous clinical experience, the opening of the posterior group of renal calyces of the patient should preferably be at an angle of ≥30° to the coronal plane for an efficient PCNL in the prone position. This in turn facilitates the establishment of a puncture with a high success rate. When the opening of the posterior group of renal calyces is at an angle of <30° to the coronal plane, the lateral or supine position facilitates the operation. The classical branched type occurs in the highest proportion. Therefore, there is a need for the establishment of a single channel for the effective removal of multiple stones. To achieve this, the relationship between different renal calyces needs to be studied to facilitate the effective design of puncture routes. The a, b, and c typing defined in this study comprehensively summarizes the classical branching type and conceptualizes abstract morphological typing, which could guide in designing efficient puncture paths in clinical practice. To achieve a single channel for the removal of multiple stones and the selection of efficient puncture paths, observation of the renal calyces and their location could be beneficial for the removal of stones with the smallest possible movement angle, which facilitates minimal bleeding. In this study, the proportion of types a, b, and c were 19.36%, 68.17%, and 12.47%, respectively. This indicated the presence of significant differences in the morphology of renal minor calyces in the posterior group. A majority had ≥3 minor calyces in the classical branching type, and an establishment of a wide surgical puncture of PCNL was required in such cases. The proportion of type b3 and c occurred at a percentage of 59.16% and 12.47%, respectively. This in turn indicates the presence of a wide distribution of renal minor calyces in the posterior group, which facilitates the surgeon to choose an appropriate access considering the complexity of the stones.
In the prone position, there is the shortest distance between the posterior renal calyces and the dorsal body surface for puncture. And there are no important tissue structures distributed within the puncture path. This helps to reduce the injury and quickly establish skin-nephron access.[18] Prone supracostal puncture into the upper group of calyces increases the risk of pleural and pulmonary injury. However, an alternative would be the puncture in a mid-posterior group of calyces, which facilitates an open view of the upper and lower calyces and the ureteral junction of the renal pelvis, thereby reducing the possibility of bleeding due to excessive nephroscope torque leading to renal parenchymal laceration.[19] With the help of 3D reconstruction of a CT scan of the collecting system along with image post-processing techniques, we propose an anatomical classification for the posterior group of calyces, which is more targeted in terms of the anatomical structure. The types of posterior group calyces are defined based on the preoperative ultrasound and 3D reconstruction images of the CT scan. This in turn helps in the selection of the appropriate target calyces for prone PCNL, the establishment of surgical access with a precise puncture, improvement in efficient removal of the stones, and reduces complications.[20,21]
However, there are a few limitations to the approach employed in this study. The simulated prone position of the collecting system might not effectively capture the actual prone position of the patients, which may have some impact on the results of this study. In clinical practice, kidney stones are often accompanied by hydronephrosis, and some patients in this study were diagnosed with hydronephrosis resulting in deformation of the collecting system, which could also have had an impact on the study results. Another problem is that our classification is complicated, and may not be easily used by doctors in clinical practice. But the advantage of our research is that surgeons will be more prepared for any complications and the risk of residual stones in complex situations.
5. Conclusions
This study attempted to classify complex and highly variable structures of posterior group calyces based on their morphology and anatomy. Posterior group calyces were present in all patients included in this study. They were morphologically classified into 3 different types, with the highest percentage of occurrence for the classical branching type with the highest percentage of 3 posterior group minor calyces. The anatomical typing of the classical branching type was further classified into 3 types, with the highest percentage of type b3 in type b. The distribution pattern of the stones aided in the selection of the puncture location. The elongated branching type occurs in a higher proportion, and patients with multiple stones of this type often require surgical procedures involving a multichannel puncture. The typing of the posterior group of calyces can provide an anatomical basis for PCNL puncture from the posterior group. In addition, the typing and data of the posterior group of renal calyces can provide parameters for artificial intelligence access planning.
Acknowledgments
We would like to thank the staff of the central laboratory, Renmin Hospital of Wuhan University, for their full support.
Author contributions
Conceptualization: Yucheng Qi, Jinzhuo Ning, Zhuang Xiong, Fangyou Lin.
Data curation: Shangting Han, Weimin Yu.
Investigation: Bojun Li.
Methodology: Xiangjun Zhou.
Project administration: Fan Cheng.
Writing – original draft: Yucheng Qi.
Writing – review & editing: Ting Rao.
Abbreviations:
- CTU
- computerized tomography urography
- PCNL
- percutaneous nephrolithotomy
YQ, FL, and BL contributed equally to this work.
This research was supported by the grants from National Natural Science Foundation of China (82270802,82170775,82100806).
The authors have no conflicts of interest to disclose.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
How to cite this article: Qi Y, Lin F, Li B, Han S, Yu W, Rao T, Zhou X, Ning J, Xiong Z, Cheng F. Classification and clinical significance of the posterior group of renal calyces. Medicine 2023;102:31(e34443).
Contributor Information
Yucheng Qi, Email: 1440939165@qq.com.
Fangyou Lin, Email: 1415488237@qq.com.
Bojun Li, Email: libojun1@qq.com.
Shangting Han, Email: qe121hst@qq.com.
Weimin Yu, Email: 1025931346@qq.com.
Ting Rao, Email: rt23@qq.com.
Xiangjun Zhou, Email: 24816439@qq.com.
Jinzhuo Ning, Email: NJZ2@aliyun.com.
Zhuang Xiong, Email: xxzz@qq.com.
References
- [1].Sampaio FJ, Aragao AH. Anatomical relationship between the intrarenal arteries and the kidney collecting system. J Urol. 1990;143:679–81. [DOI] [PubMed] [Google Scholar]
- [2].Türk C, Petřík A, Sarica K, et al. EAU guidelines on interventional treatment for urolithiasis. Eur Urol. 2016;69:475–82. [DOI] [PubMed] [Google Scholar]
- [3].Ko R, Soucy F, Denstedt JD, et al. Percutaneous nephrolithotomy made easier: a practical guide, tips and tricks. BJU Int. 2008;101:535–9. [DOI] [PubMed] [Google Scholar]
- [4].Binbay M, Akman T, Ozgor F, et al. Does pelvicaliceal system anatomy affect success of percutaneous nephrolithotomy? Urology. 2011;78:733–7. [DOI] [PubMed] [Google Scholar]
- [5].Kallidonis P, Kalogeropoulou C, Kyriazis I, et al. Percutaneous nephrolithotomy puncture and tract dilation: evidence on the safety of approaches to the infundibulum of the middle renal calyx. Urology. 2017;107:43–8. [DOI] [PubMed] [Google Scholar]
- [6].Gandhi KR, Chavan S. Revisiting the morphology of pelvicalyceal system in human cadaveric kidneys with a systematic review of literature. Asian J Urol. 2019;6:249–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Takazawa R, Kitayama S, Uchida Y, et al. Proposal for a simple anatomical classification of the pelvicaliceal system for endoscopic surgery. J Endourol. 2018;32:753–8. [DOI] [PubMed] [Google Scholar]
- [8].Sampaio FJ. Renal collecting system anatomy: its possible role in the effectiveness of renal stone treatment. Curr Opin Urol. 2001;11:359–66. [DOI] [PubMed] [Google Scholar]
- [9].Sampaio FJ, Aragao AH. Inferior pole collecting system anatomy: its probable role in extracorporeal shock wave lithotripsy. J Urol. 1992;147:322–4. [DOI] [PubMed] [Google Scholar]
- [10].Hodson J. The lobar structure of the kidney. Br J Urol. 1972;44:246–61. [DOI] [PubMed] [Google Scholar]
- [11].Schultheiss D, Engel RM, Crosby RW, et al. Max Brödel (1870-1941) and medical illustration in urology. J Urol. 2000;164:1137–42. [PubMed] [Google Scholar]
- [12].Patel U, Walkden RM, Ghani KR, et al. Three-dimensional CT pyelography for planning of percutaneous nephrostolithotomy: accuracy of stone measurement, stone depiction and pelvicalyceal reconstruction. Eur Radiol. 2009;19:1280–8. [DOI] [PubMed] [Google Scholar]
- [13].Urban BA, Ratner LE, Fishman EK. Three-dimensional volume-rendered CT angiography of the renal arteries and veins: normal anatomy, variants, and clinical applications. Radiographics. 2001;21:373–86. [DOI] [PubMed] [Google Scholar]
- [14].Tsaturyan A, Bellin A, Barbuto S, et al. Technical aspects to maximize the hyperaccuracy three-dimensional (HA3D(™)) computed tomography reconstruction for kidney stones surgery: a pilot study. Urolithiasis. 2021;49:559–66. [DOI] [PubMed] [Google Scholar]
- [15].Tailly T, Nadeau BR, Violette PD, et al. Stone burden measurement by 3D reconstruction on noncontrast computed tomography is not a more accurate predictor of stone-free rate after percutaneous nephrolithotomy than 2d stone burden measurements. J Endourol. 2020;34:550–7. [DOI] [PubMed] [Google Scholar]
- [16].Mousavi-Bahar SH, Mehrabi S, Moslemi MK. The safety and efficacy of PCNL with supracostal approach in the treatment of renal stones. Int Urol Nephrol. 2011;43:983–7. [DOI] [PubMed] [Google Scholar]
- [17].Seitz C, Desai M, Häcker A, et al. Incidence, prevention, and management of complications following percutaneous nephrolitholapaxy. Eur Urol. 2012;61:146–58. [DOI] [PubMed] [Google Scholar]
- [18].Verma A, Tomar V, Yadav S. Complex multiple renal calculi: stone distribution, pelvicalyceal anatomy and site of puncture as predictors of PCNL outcome. SpringerPlus. 2016;5:1356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Turney BW. A new model with an anatomically accurate human renal collecting system for training in fluoroscopy-guided percutaneous nephrolithotomy access. J Endourol. 2014;28:360–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Lin F, Yu W, Rao T, et al. The anatomic structure of a fused renal pyramid and its clinical significance in the establishment of percutaneous renal access. Urology. 2019;124:38–45. [DOI] [PubMed] [Google Scholar]
- [21].Abdullatif VA, Sur RL, Abdullatif ZA, et al. The safety and efficacy of endoscopic combined intrarenal surgery (ECIRS) versus Percutaneous Nephrolithotomy (PCNL): a systematic review and meta-analysis. Adv Urol. 2022;2022:1716554. [DOI] [PMC free article] [PubMed] [Google Scholar]