Abstract
The Environmental Influences on Child Health Outcomes (ECHO)-Wide Cohort Study (EWC), a collaborative research design comprising 69 cohorts in 31 consortia, was funded by the National Institutes of Health (NIH) in 2016 to improve children’s health in the United States. The EWC harmonizes extant data and collects new data using a standardized protocol, the ECHO-Wide Cohort Data Collection Protocol (EWCP). EWCP visits occur at least once per life stage, but the frequency and timing of the visits vary across cohorts. As of March 4, 2022, the EWC cohorts contributed data from 60,553 children and consented 29,622 children for new EWCP data and biospecimen collection. The median (interquartile range) age of EWCP-enrolled children was 7.5 years (3.7–11.1). Surveys, interviews, standardized examinations, laboratory analyses, and medical record abstraction are used to obtain information in 5 main outcome areas: pre-, peri-, and postnatal outcomes; neurodevelopment; obesity; airways; and positive health. Exposures include factors at the level of place (e.g., air pollution, neighborhood socioeconomic status), family (e.g., parental mental health), and individuals (e.g., diet, genomics).
Keywords: adolescent, child, child development, child health, child well-being, cohort studies, environmental exposure, epidemiologic methods
Abbreviations
- ASD
autism spectrum disorder
- COVID-19
coronavirus disease 2019
- ECHO
Environmental Influences on Child Health Outcomes
- EWC
ECHO-Wide Cohort Study
- EWCP
ECHO-Wide Cohort Data Collection Protocol
- NIH
National Institutes of Health
- NICHD
Eunice Kennedy Shriver National Institute of Child Health and Human Development
In 2016, the National Institutes of Health (NIH) Office of the Director funded the Environmental Influences on Child Health Outcomes (ECHO) Program, which includes the ECHO-Wide Cohort Study (EWC) and the IDeA States Pediatric Clinical Trials Network (1). The EWC comprises 69 ongoing and new pregnancy and pediatric cohorts, a Coordinating Center, a Data Analysis Center, and a Person-Reported Outcomes Core. Funding was also provided to the Human Health Exposure Analysis Resource for conducting chemical bioassay analyses (2) and the Center for Inherited Disease Research for genotyping (3).
The goal of the ECHO Program is to understand how the environment, from preconception through early childhood, influences child health and development to identify opportunities to mitigate the risk of disease and optimize health and thriving (4). The mission of the ECHO Program is “To enhance the health of children for generations to come.” ECHO focuses on solution-oriented research in the areas of pre-, peri-, and postnatal outcomes; neurodevelopment; obesity; airways; and positive health (5–9).
The EWC provides large samples to address complex relationships among environmental exposures, which coexist and may be synergistic, and children’s health. Furthermore, the diverse sample from 49 states, the District of Columbia, and Puerto Rico offers heterogeneity often lacking in an individual cohort and thus permits examination of exposures that differ by geography or sociodemographic subgroups. Last, the inclusion of children at different life stages allows for the evaluation of time-varying effects of exposures and critical periods of development.
For this longitudinal collaborative cohort study, the NIH chose existing studies that vary in their target populations: Some cohorts focus on children at high risk for certain outcomes (e.g., asthma and autism spectrum disorder (ASD) (RFA-OD-16-004)), which ensured that the EWC would capture a larger sample of children with relatively low-frequency outcomes of high interest to examine pathogenic mechanisms and protective factors; other cohorts enrolled children representative of the general population, allowing researchers to estimate incidence rates and absolute, relative, and attributable risks that are generalizable to the broader community.
With existing cohorts, the EWC capitalizes on: 1) established relationships between the study investigators, their staff, and study participants, thus enhancing the probability of successful enrollment into the EWC; 2) extant data as a rich resource for early EWC analyses; 3) established infrastructure for study conduct; and 4) the necessary investigator expertise and experience to conduct impactful science on child health and development. This unique collaborative research program embraces team science; the ECHO Program website (https://echochildren.org/) provides information about study governance and publications.
METHODS
Study participants
EWC cohorts (Web Table 1, available at https://doi.org/10.1093/aje/kwad071) enrolled individuals at different life stages (i.e., preconception, pregnancy, infancy, early childhood, middle childhood, adolescence), most often either during pregnancy or at birth. Cohort enrollment started in the 1980s and is ongoing (Web Figure 1), with sites around the country enrolling participants (Web Figure 2). While the cohorts were consenting participants to the EWC, they submitted extant data to the Data Analysis Center via a secure portal developed and maintained by the Data Analysis Center using Data Use Agreements. The type of extant data was determined by the local institutional review board and depended on the original cohort consent. Individuals were classified according to consent status and type of extant data contributed prior to consent into the EWC:
Level 2: Participant consented to new EWC data collection and sharing of identifiable extant data. These participants are referred to as ECHO-Wide Cohort Data Collection Protocol (EWCP) participants.
Level 1: Participant consented to sharing of identifiable extant data but not to new EWCP data collection (i.e., due to unwillingness to participate, inability to contact for consent, or being outside the eligible age range for EWCP (age 21 years or older)).
Level 0+: Participant not yet consented to EWCP data collection; however, cohort-specific consent allows sharing limited data (e.g., including date of birth) but not identifiable geographical information (e.g., residential address).
Level 0: Participant not yet consented to EWCP, but cohort-specific consent allows sharing only deidentified extant data.
ECHO-Wide Data Collection Protocol
In 2019, the single institutional review board (Western IRB (WIRB)) approved version 1.2 of the EWCP, which was collaboratively developed by all cohort and component principal investigators (9). According to the EWCP, cohorts collect data from at least 1 visit per life stage, although some cohorts collect data more frequently. The full protocol is available online (10). Despite coronavirus disease 2019 (COVID-19) pandemic disruptions, data were collected on over 20,000 children in 2020 and through the first half of 2021 (Web Figure 3).
The EWCP includes data elements labeled “essential” (required) and “recommended” for new data collection. Essential data elements are listed in Web Table 2 by life stage. All data elements listed in the EWCP that were previously collected are expected to be shared, consistent with participant consent. The EWCP specifies preferred and acceptable measures for collecting the data elements; alternative measures may be approved for new data collection when the alternative was previously used by the cohort and could be harmonizable to either the preferred or acceptable measure. Measures are a combination of self-report, caregiver report, medical record abstraction, and standardized examination.
Outcomes
The primary outcome areas of interest in ECHO are: 1) pre-, peri-, and postnatal outcomes (e.g., preterm birth, birth weight for gestational age, neonatal morbidities); 2) airway health (e.g., asthma, allergies/atopy); 3) obesity; 4) neurodevelopmental (e.g., ASD, cognition, attention-deficit/hyperactivity disorder (ADHD), gross and fine motor skills, internalizing and externalizing behaviors); and 5) positive health (e.g., global health rating) (11).
Exposures
Exposures include place-, family-, and individual-level factors in the domains of: chemical and physical (e.g., air pollution, phthalates, drinking water source), community (e.g., neighborhood deprivation and opportunity, segregation), psychosocial (e.g., stress, discrimination, parental mental health, socioeconomic status, family dynamics), behaviors (e.g., sleep, physical activity, diet), and biological factors (e.g., genomics, microbiome, metabolomics). This article highlights 3 key sources of exposure data: biospecimens and assays, genetic and epigenetic data, and residential history data.
Biospecimens and assays.
ECHO researchers developed standardized protocols and kits for collection, processing, and storage of biospecimens. Essential biospecimens include at least 1 sample for DNA from the child and biological mother, and whole blood/blood spot, urine, hair, shed teeth, and toenails from the child at various life stages and from the biological mother during pregnancy. Optional specimens include placenta, cord blood, meconium, and breast milk; stool from the biological mother during pregnancy and from the child across life stages; nasal mucus from the child; and a sample for DNA from the biological father. Fisher BioServices (Rockville, Maryland) maintains a biospecimen repository for ECHO.
Some cohorts modified protocols to remotely collect specimens because of the COVID-19 pandemic. This included mailing kits and picking up samples at agreed-upon locations. Cohorts are also contributing existing biospecimens for Human Health Exposure Analysis Resource laboratory assays under approved analysis proposals. Human Health Exposure Analysis Resource conducts most of the chemical biospecimen assays for the EWC.
To date, 51 cohorts have collected new biospecimens from over 10,000 pregnant people, and 64 cohorts collected biospecimens from over 14,000 children (Web Table 3). Cohorts transferred biospecimens from 81% of these participants to the biorepository. Saliva for DNA, toenail, and hair were the most frequently collected new biospecimens.
Cohorts are concomitantly transferring extant bioassay data. These extant data may be from clinical assays (e.g., complete blood count, vitamin D, inflammatory markers), chemical panels (e.g., pyrethroids, organophosphorus flame retardants, tobacco metabolites, polycyclic aromatic hydrocarbons, per- and poly-fluoroalkyl substances, phthalates, metals), and -omics analyses. The cohorts follow standard operating procedures to format and submit data that are required for harmonization and use in statistical analyses. These data include details on the participant specimens, controls, laboratory methods, assay results, and quality assurance procedures.
Genetics and epigenetics.
The Center for Inherited Disease Research conducts the genotyping for the EWC using specimens from all family members, including trios (biological mother, biological father, child participants), dyads (biological parent and child participants), and child participants only, using the Illumina Multi-Ethnic Global Array (MEGA) (San Diego, California). This array was chosen due to its broad coverage for people of African, European, Asian, and Native American ancestry and includes known genotype-phenotype associations, population-specific variant associations, and clinically relevant and reported variants. In addition to submitting biospecimens for genotyping, cohorts submitted extant genome-wide array genotype data and genome-scale DNA methylation data. Extant epigenetic data are available on 8,028 samples from 5,990 participants (Web Table 4). These data include 614 parent-offspring pairs. The data are generated on 4 different platforms, including the Illumina 27K (n = 216 samples) (12), 450K (n = 2,207) (13, 14), EPIC (n = 3,556) (15, 16), and a custom asthma booster array (n = 2,318). While most participants have a single sample, a number have multiple tissue types (n = 1,077 participants) and/or the same tissue at different ages (n = 1,742 participants). All the epigenetic data have been cleaned and normalized to a common protocol to enable analysis across cohorts and both epigenetic clock and cell proportion calculations have been generated.
Extant genetic data are available on 5,794 participants from 13 cohorts (Web Table 5). Data were generated on multiple single-nucleotide polymorphism (SNP) microarray platforms with 370,150 to 1,730,897 SNPs per sample (17, 18). All the data have been cleaned to the same standard and mapped to the human genome build 38. Data were imputed using the TOPMED imputation server with the TOPMed (version r2 2020) reference panel (18, 19). Multi-omic analyses between the new metabolomic and genetic data and the extant epigenetics, genetics, and microbiome data are possible.
Residential history.
Residential history data are collected from EWC participants and used to: 1) geocode all addresses; and 2) generate a time-varying residential history file that captures residential location and mobility starting a year before birth until the latest follow-up time point. These residential histories allow researchers to combine area-level data (e.g., greenspace vegetation measures, socioeconomic status, COVID-19 social-distancing policies) with participant locations at the etiologically relevant exposure period and spatial resolution (e.g., county, census tract, or radii around a participant’s home). Addresses are geocoded in ArcGIS Pro Streetmap Premium Geocoder (Redlands, California). To date, 54,183 unique residential addresses have been geocoded. Over 85% of addresses had a high-quality match (point, parcel, or specific street address). The residential history file is constructed as a vertical sequence of residential locations for each participant by month. The current residential history file includes data for 25,630 children and 1,402 pregnancies with children’s birth years ranging from 1995 to 2022.
Data capture
Cohorts use “REDCap Central,” a web-based implementation of REDCap (20, 21) designed by the Data Analysis Center to provide data capture opportunities for most EWCP measures according to cohort-specific visit schedules. Cohorts also use local data systems and upload their data onto the ECHO Analysis Workbench (EAW). Some measures (e.g., NIH Toolbox) require use of specialized software/hardware (e.g., iPads (Apple, Cupertino, California)) for data collection and uploads. The Data Analysis Center developed a suite of tools collectively known as the Data Transform system to process all data through pipelines verifying participant identifiers, executing mapping algorithms to the Common Data Model (CDM), and validating data integrity in reference to applicable data dictionaries: checking data formats, coded values, and ranges. Cohorts vary in the degree of in-person compared with remote data collection; an increase in remote collection options was implemented during the COVID-19 pandemic.
Data are stored and analyzed on the EAW, a Federal Information Security Management Act (FISMA) moderate, cloud-based platform (22). EAW workspaces are collaborative, with files and code shared within analysis-specific folders. The folder structure for each analysis is standardized to promote reproducibility. Data quality assurance and control includes training of data collectors, checking the data in REDCap Central and in the data pipeline process, creating data queries for cohorts to address after data submission, and reviewing data completion by an implementation fidelity group working with the Data Analysis Center.
Data harmonization
Prior to the approval and implementation of the EWCP, the cohorts used various measures to collect data elements. When possible, the cohorts mapped their extant data to the CDM. Cohorts also created custom data dictionaries to define and submit relevant extant data that could not be mapped. As previously noted, the EWCP also allows multiple measures that cohorts may use to collect new data. Having custom extant data and multiple measures corresponding to a data element means that a substantial harmonization effort is needed to incorporate all data and to maximize the sample size and power for EWC analyses. Data harmonization integrates information gathered through different methods, which represent the same construct to derive analytical measures for use in analyses. When data cannot be harmonized into a derived variable, other analytical approaches, such as meta-analyses, are used to incorporate all data that reflect a common underlying construct.
Data access
Investigators may access the EWC data for scientific purposes by applying to the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) Data and Specimen Hub (DASH) to obtain deidentified data on participants contributing extant and new data; the first version is based on the data that were available as of August 31, 2021 (23). In addition to the deidentification of the data, the data on DASH do not include participant feedback, detailed racial or ethnic categories, genetic or epigenetic data, biospecimen data, or any data from the Navajo Birth Cohort Study. Alternatively, investigators may contact the ECHO help desk at ECHO-DAC@rti.org to work directly with the EWC.
RESULTS
Recruitment of new participants and existing cohort participants into the EWC for new data and biospecimen collection is ongoing. The data are locked for analyses every 6 months. All data presented in this article are based on the March 4, 2022, data lock, at which time the cohorts contributed data from 60,553 children and consented 29,622 children for new EWCP data and biospecimen collection (Table 1 and Figure 1). Among the 36,166 individuals (representing 38,735 pregnancies) who were enrolled in the cohorts during pregnancy, 20,957 (representing 22,534 pregnancies) consented to the EWCP. A subset of participants was pregnant when consented to the EWCP (Figure 1). Additionally, 25,955 children have prenatal data that were collected retrospectively (i.e., after birth, from either medical record abstraction or surveys/interviews with the primary caregiver).
Table 1.
Sociodemographic Characteristics of Child Participants in the Environmental Influences on Child Health Outcomes-Wide Cohort, United States, as of March 4, 2022a
| ECHO Children | ||||
|---|---|---|---|---|
| All Participants: Contributing Extant and/or New Data (n = 60,553) | EWCP Enrollees: Contributing New Data (n = 29,622) | |||
| Child Characteristic | No. | % | No. | % |
| No. of children per familyb,c | 1.0 (1–8) | 1.0 (1–7) | ||
| Sex at birth | ||||
| Male | 31,123 | 51.7 | 15,123 | 51.4 |
| Female | 29,107 | 48.3 | 14,300 | 48.6 |
| Missing | 323 | 199 | ||
| Child age, yearsc,d | 9.5 (5.5, 18.1) | 7.5 (3.7, 11.1) | ||
| Calendar year of birth | ||||
| 1980–1986 | 3,317 | 5.5 | N/Ae | |
| 1987–1991 | 837 | 1.4 | N/Ae | |
| 1992–1996 | 4,206 | 6.9 | 19 | 0.1 |
| 1997–2001 | 3,170 | 5.2 | 1,091 | 3.7 |
| 2002–2006 | 7,341 | 12.1 | 3,176 | 10.7 |
| 2007–2011 | 8,513 | 14.1 | 4,781 | 16.1 |
| 2012–2016 | 18,803 | 31.1 | 10,318 | 34.8 |
| 2017–2021 | 14,366 | 23.7 | 10,237 | 34.6 |
| Race | ||||
| American Indian or Alaska Native | 1,511 | 2.8 | 863 | 3.1 |
| Asian | 2,101 | 3.8 | 876 | 3.2 |
| Black | 8,553 | 15.6 | 4,421 | 16.1 |
| Multiple race | 5,950 | 10.9 | 3,408 | 12.4 |
| Native Hawaiian or Pacific Islander | 175 | 0.3 | 99 | 0.4 |
| Other race | 2,245 | 4.1 | 1,332 | 4.9 |
| White | 34,136 | 62.4 | 16,462 | 59.9 |
| Missing | 5,882 | 2,161 | ||
| Ethnicity | ||||
| Non-Hispanic | 41,557 | 72.1 | 21,202 | 74.2 |
| Hispanic | 16,114 | 27.9 | 7,380 | 25.8 |
| Missing | 2,882 | 1,040 | ||
Abbreviations: ECHO, Environmental Influences on Child Health Outcomes; EWCP, ECHO-Wide Data Collection Protocol; N/A, not applicable.
a This table reflects both extant cohort data, collected from 1987 to 2017, and prospective EWCP data collected from 2018 to March 4, 2022.
b Among children in families with at least 1 enrolled child.
c Values are expressed as median (range).
d Values are expressed as median (interquartile range).
e Child participants 21 years of age or older were not enrolled in the EWCP.
Figure 1.
Environmental Influences on Child Health Outcomes (ECHO) participants are enrolled before or during pregnancy (n = 21,357) or at or after birth (n = 8,914), United States. There are 2,488 pregnancies for which a child has not yet been enrolled in the ECHO-Wide Cohort Data Collection Protocol (EWCP). In total, 29,622 children were enrolled in the EWCP as of March 4, 2022. This figure includes participants who were enrolled in the EWCP from 2018 to March 4, 2022. Enrollment in the EWCP is ongoing.
The EWC has extant data from an additional 16,201 pregnancies and 30,931 children not yet enrolled in the EWCP (i.e., consent levels 1, 0+, 0). Children and pregnant people enrolled in the EWCP have sociodemographic characteristics similar to those from the underlying cohorts (Tables 1 and 2).
Table 2.
Sociodemographic Characteristics and Summary of Key Outcomes of Pregnant People in the Environmental Influences on Child Health Outcomes-Wide Cohorta, United States, as of March 4, 2022
| ECHO Pregnancies | ||||
|---|---|---|---|---|
| All Participants: Contributing Extant and/or New Data (n = 38,735) | EWCP Enrollees: Contributing New Data (n = 22,534) | |||
| Characteristic | No. | % | No. | % |
| Age at delivery, yearsb | 31 (26, 34) | 31 (27, 34) | ||
| Race | ||||
| American Indian or Alaska Native | 1,451 | 4.3 | 848 | 4.1 |
| Asian | 2,232 | 6.6 | 1,124 | 5.4 |
| Black | 5,505 | 16.2 | 2,980 | 14.4 |
| Multiple race | 1,492 | 4.4 | 973 | 4.7 |
| Native Hawaiian or Pacific Islander | 229 | 0.7 | 146 | 0.7 |
| Other race | 2,344 | 6.9 | 1,472 | 7.1 |
| White | 20,792 | 61.1 | 13,145 | 63.5 |
| Missing | 4,690 | 1,846 | ||
| Ethnicity | ||||
| Non-Hispanic | 26,656 | 71.9 | 16,101 | 74.0 |
| Hispanic | 10,419 | 28.1 | 5,665 | 26.0 |
| Missing | 1,660 | 768 | ||
| Education, highest attained | ||||
| Less than high school | 2,809 | 10.5 | 1,354 | 8.4 |
| High-school diploma, GED certificate, or equivalent | 4,999 | 18.7 | 2,750 | 17.0 |
| Some college, no degree; associate degree; trade school | 5,980 | 22.4 | 3,679 | 22.7 |
| Bachelor’s degree | 6,836 | 25.6 | 4,367 | 27.0 |
| Master’s, professional, or doctorate degree | 6,122 | 22.9 | 4,036 | 24.9 |
| Missing | 11,989 | 6,348 | ||
| Marital status (first report) | ||||
| Married or living with a partner | 20,571 | 77.6 | 12,912 | 79.2 |
| Widowed, separated, divorced | 872 | 3.3 | 523 | 3.2 |
| Single, never married; partnered, not living together | 5,074 | 19.1 | 2,866 | 17.6 |
| Missing | 12,218 | 6,233 | ||
| Household income, $ | ||||
| <30,000 | 7,162 | 40.9 | 4,009 | 37.3 |
| 30,000–49,999 | 2,214 | 12.6 | 1,503 | 14.0 |
| 50,000–74,999 | 1,627 | 9.3 | 1,161 | 10.8 |
| 75,000–99,999 | 1,340 | 7.6 | 983 | 9.1 |
| 100,000–199,999 | 3,331 | 19.0 | 2,023 | 18.8 |
| ≥200,000 | 1,845 | 10.5 | 1,082 | 10.1 |
| Missing | 21,216 | 11,773 | ||
| Prenatal alcohol use | ||||
| No | 21,126 | 80.5 | 11,852 | 79.8 |
| Yes | 5,104 | 19.5 | 2,998 | 20.2 |
| Missing | 12,505 | 7,684 | ||
Table continues
Table 2.
Continued
| ECHO Pregnancies | ||||
|---|---|---|---|---|
| All Participants: Contributing Extant and/or New Data (n = 38,735) | EWCP Enrollees: Contributing New Data (n = 22,534) | |||
| Characteristic | No. | % | No. | % |
| Prenatal tobacco use | ||||
| No | 25,967 | 91.8 | 14,949 | 92.6 |
| Yes | 2,329 | 8.2 | 1,196 | 7.4 |
| Missing | 10,439 | 6,389 | ||
| Prenatal opioid use | ||||
| No | 19,052 | 97.4 | 12,068 | 97.6 |
| Yes | 503 | 2.6 | 291 | 2.4 |
| Missing | 19,180 | 10,175 | ||
| Singleton gestation | ||||
| No | 422 | 1.5 | 238 | 1.3 |
| Yes | 28,403 | 98.5 | 17,809 | 98.7 |
| Missing | 9,910 | 4,487 | ||
| Nulliparous pregnancy | ||||
| No | 13,424 | 45.3 | 6,596 | 41.4 |
| Yes | 16,190 | 54.7 | 9,351 | 58.6 |
| Missing | 9,121 | 6,587 | ||
| Delivery mode | ||||
| Vaginal | 17,289 | 69.0 | 10,720 | 70.4 |
| Caesarean delivery | 7,750 | 31.0 | 4,517 | 29.6 |
| Missing | 13,696 | 7,297 | ||
Abbreviations: ECHO, Environmental Influences on Child Health Outcomes; EWCP, ECHO-Wide Data Collection Protocol; GED, General Educational Development.
a This table represents 38,735 pregnancies from 36,166 unique participants (all) and 22,534 EWCP pregnancies from 20,957 unique EWCP participants. Some pregnant people are represented in this table more than once because they have more than 1 pregnancy enrolled in EWCP. This table reflects both extant cohort data, collected from 1987 to 2017, and prospective EWCP data collected from 2018 to March 4, 2022.
b Values are expressed as median (interquartile range).
Of children enrolled in the EWCP, 59.9% were White, 16.1% Black, 12.4% multiple race, 4.9% other race, 3.2% Asian, 3.1% American Indian or Alaska Native, and 0.4% Native Hawaiian or Pacific Islander (Table 1). Overall, 25.8% of children were of Hispanic ethnicity. Half of the EWCP children were male, and 96.2% were born after 2001, with 34.8% born during 2012–2016 and 34.6% born during 2017–2021. Most cohorts enrolled only 1 child per family, although some recruited children from multiple-gestation pregnancies and siblings (Figure 1).
Table 2 summarizes the sociodemographic characteristics of pregnant people enrolled in the EWCP. The median age of EWCP pregnant people at the time of birth was 31 (interquartile range, 27, 34) years. Among those with education data, 51.9% had a bachelor’s degree or higher; 22.7% attended some college but did not receive a degree, had an associate degree, or attended trade school; and 25.4% had a high-school diploma or less (Table 2). Table 3 describes the availability of data for and prevalence of key outcome areas.
Table 3.
Key Child Health Outcomes in the Environmental Influences on Child Health Outcomes-Wide Cohort, United States, as of March 4, 2022a
| ECHO Children | ||||
|---|---|---|---|---|
| All Participants, Contributing Extant and/or New Data (n = 60,553) | EWCP Enrollees, Contributing New Data (n = 29,622) | |||
| Child Health Outcome | No. | % | No. | % |
| Pre-, Peri-, and Postnatal Outcomes | ||||
| Gestational age at birth | ||||
| No. of weeksb | 37.9 (38, 40) | 37.9 (38, 40) | ||
| Missing | 14,402 | 2,285 | ||
| Preterm birth <37 weeks’ gestationc | ||||
| No | 46,958 | 85.5 | 23,576 | 84.6 |
| Yes | 7,938 | 14.5 | 4,300 | 15.4 |
| Missing | 5,657 | 1,746 | ||
| Gestational agec, weeks | ||||
| 22–27 (extremely preterm ) | 2,492 | 5.4 | 1,402 | 5.1 |
| 28–31 (very preterm) | 872 | 1.9 | 592 | 2.2 |
| 32–33 (moderate preterm) | 538 | 1.2 | 342 | 1.3 |
| 34–36 (late preterm) | 3,062 | 6.6 | 1,870 | 6.8 |
| 37–38 (early term) | 10,838 | 23.5 | 6,472 | 23.7 |
| 39–40 (full-term) | 23,941 | 51.9 | 14,021 | 51.3 |
| 41 (late-term) | 3,812 | 8.3 | 2,311 | 8.5 |
| 42–43 (post-term) | 596 | 1.3 | 327 | 1.2 |
| Missing | 14,402 | 2,285 | ||
| Birth weight | ||||
| Gramsb | 3,310 (2,910, 3,657) | 3,295 (2,892, 3,655) | ||
| Missing | 16,327 | 5,233 | ||
| Small for gestational aged | ||||
| No | 32,930 | 93.4 | 19,573 | 93.7 |
| Yes | 2,335 | 6.6 | 1,326 | 6.3 |
| Missing | 25,288 | 8,723 | ||
| Large for gestational aged | ||||
| No | 29,196 | 82.8 | 17,331 | 82.9 |
| Yes | 6,069 | 17.2 | 3,568 | 17.1 |
| Missing | 25,288 | 8,723 | ||
| Neurodevelopmental Outcomes | ||||
| ASD diagnosis | ||||
| No | 14,590 | 92.6 | 12,820 | 93.2 |
| Yes | 1,171 | 7.4 | 940 | 6.8 |
| Missing | 44,792 | 15,862 | ||
| ADHD diagnosis | ||||
| No | 14,096 | 90.1 | 12,224 | 89.3 |
| Yes | 1,553 | 9.9 | 1,467 | 10.7 |
| Missing | 44,904 | 15,931 | ||
Table continues
Table 3.
Continued
| ECHO Children | ||||
|---|---|---|---|---|
| All Participants, Contributing Extant and/or New Data (n = 60,553) | EWCP Enrollees, Contributing New Data (n = 29,622) | |||
| Child Health Outcome | No. | % | No. | % |
| Airways outcomes | ||||
| Asthma diagnosis | ||||
| No | 16,533 | 80.1 | 5,789 | 76.4 |
| Yes | 4,118 | 19.9 | 1,788 | 23.6 |
| Missing | 39,902 | 22,045 | ||
| Wheezing reported in prior 12 months | ||||
| No | 25,578 | 79.3 | 16,810 | 82.9 |
| Yes | 6,695 | 20.7 | 3,456 | 17.1 |
| Missing | 28,280 | 9,356 | ||
| Allergies reported | ||||
| 0 | 9,459 | 49.2 | 6,205 | 48.1 |
| 1 | 7,009 | 36.4 | 4,490 | 34.8 |
| ≥2 | 2,773 | 14.4 | 2,196 | 17.1 |
| Missing | 41,312 | 16,731 | ||
| Positive Health Outcomes | ||||
| General health rating | ||||
| Poor | 72 | 0.4 | 62 | 0.4 |
| Fair | 468 | 2.4 | 372 | 2.3 |
| Good | 2,658 | 13.7 | 2,012 | 12.6 |
| Very good | 5,726 | 29.5 | 4,685 | 29.4 |
| Excellent | 10,476 | 54.0 | 8,823 | 55.3 |
| Missing | 41,153 | 13,668 | ||
| Sleep | ||||
| Nightly duration, hoursb | 10.0 (9, 11.5) | 10.0 (9, 11) | ||
| Missing | 38,902 | 11,063 | ||
| Obesity Outcomes | ||||
| Weight categories for children ≥2 years of age | ||||
| Underweight | 1,741 | 5.4 | 915 | 5.6 |
| Normal weight | 22,099 | 68.0 | 11,072 | 68.4 |
| Overweight | 4,420 | 13.6 | 2,136 | 13.2 |
| Obese | 4,222 | 13.0 | 2,072 | 12.8 |
| Missing | 28,071 | 13,427 | ||
| COVID-19 Outcomes | ||||
| Child tested positive for COVID-19e | ||||
| No | 17,023 | 90.9 | 16,552 | 90.7 |
| Yes | 1,712 | 9.1 | 1,688 | 9.3 |
| Missing | 41,818 | 11,382 | ||
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; ASD, autism spectrum disorder; COVID-19, coronavirus disease 2019; ECHO, Environmental Influences on Child Health Outcomes; EWCP, ECHO-Wide Data Collection Protocol.
a This table reflects both extant cohort data, collected from 1987 to 2017, and prospective EWCP data collected from 2018 to March 4, 2022.
b Values are expressed as median (interquartile range).
c Preterm birth status (<37 weeks) is available for more children than detailed gestational age categories.
d Calculated for singleton births only.
e Any positive COVID-19 test reported through March 3, 2022. This may have been ascertained at any point during the pandemic and may not reflect the current cumulative prevalence of COVID-19 in the EWCP participants.
The EWC enrolls pregnant people and children across the United States and Puerto Rico. Children with residential history data at birth (n = 13,114 children from 65 cohorts) were born in 672 counties from 49 states, the District of Columbia, and Puerto Rico (Web Figure 2). Approximately 87% of births were in metropolitan counties, and 2% were in rural counties (24).
DISCUSSION
Research and publications
Team science is a cross-cutting theme in ECHO research. The accomplishments of ECHO researchers are evidence of the feasibility of creating a productive team of scientists by combining scientific expertise, data, and biospecimens from 69 existing cohorts and centers for data and biospecimen analyses. Early indicators of the success of ECHO’s team science approach include a series of review papers on environmental exposures (e.g., air pollution (25), chemicals (26), prenatal opioids (27)) and ECHO’s key outcomes (positive health (11); neurodevelopment (5); obesity (6); asthma; and pre-, peri-, and postnatal outcomes (28, 29)). To date, EWC has produced 64 publications. These include some of the first national estimates of asthma incidence rates, including estimates of incidence by child age, sex, and race, and parental family history of asthma. Higher rates of asthma were observed among young children with a family history of asthma and among preschool-age Black children regardless of a family history of asthma (7). Another study explores the association between pregnancy complications and ASD-related traits, finding an association between obesity and gestational diabetes, respectively, and higher ASD-related traits (30). All EWC publications are available online (31).
In addition to the work across the key outcome areas, ongoing innovative work in exposure analyses assesses emerging chemical exposures (32) and social and environmental exposures (33). ECHO researchers developed a time-varying national-level index of combined neighborhood environmental and social stressors. Higher combined prenatal exposure was associated with adverse perinatal outcomes, including lower mean gestational age and a higher risk of preterm birth. This association was modified by maternal race, maternal educational attainment, and urbanicity (33). ECHO is also on the forefront of the examination of COVID-19 pandemic–related stress, hardships, and behaviors, and their effects on child health. In one analysis, ECHO researchers found that family engagement and social relationships ameliorate the effect of COVID-19–related stress on adolescent mental health (34). The EWC is also expanding methods for collaborative studies and cohort studies (35, 36).
Statistical considerations
In addition to participant- and item-level missing data in the EWC, some cohorts may be missing measures in both extant and new data collection. Within the extant data, exposures, covariates, and outcomes of interest may be missing due to the cohorts’ original protocol, the age of the participants, and cohort objectives. Under new EWCP data collection, cohorts may opt to measure key constructs with preferred, acceptable, or alternative measures, leading to missing data if data cannot be harmonized or if the cohort has elected to administer a measure at a later visit, given that the EWCP only requires measurement once per life stage. These scenarios result in missing data for the cohort but also provide opportunities for new and advanced methodological development for missing data in consortium studies. Currently, the development of new methods to handle missing data are underway, including methods of combining data when available covariate information differs (37, 38).
Combining cohorts
Accounting for cohort effects is necessary in analyses using EWC data. While some cohorts represent the general population, other cohorts are enriched for specific outcomes (e.g., ASD, asthma, preterm birth), restricted to specific subpopulations (e.g., Tribal entities, rural populations), or cover different time periods (e.g., cohorts were started in the 1980s). The enriched cohorts may notably inflate the prevalence of specific conditions. For example, the prevalence of preterm birth (<37 weeks’ gestation at birth) in the EWC is approximately 15%; however, when excluding the cohorts that oversampled preterm infants, the prevalence is only 10% (Web Table 6). Even when cohorts have similar enrollment criteria or study goals, a degree of selection bias can be expected due to differences in inclusion criteria, source populations, and variations in data collection. Multiple approaches account for differences in cohorts, such as: 1) including a cohort effect via fixed effects regression using a dummy variable for cohort, 2) applying mixed models that allow for random intercepts or slopes by cohort, 3) using a generalized estimating equation (GEE) with cohort clusters, or 4) meta-analyzing individual participant data. Regardless of the statistical approach, it is important that sensitivity analyses for cohort effects are conducted, including examining cohort-specific effects using forest plots and/or leave-one-out analyses, which recalculate pooled effects excluding 1 cohort at a time to judge the sensitivity of pooled estimates to potentially influential cohorts, as a starting point. Importantly, investigation of cohort heterogeneity in exposure-outcome associations may uncover key effect modifiers.
Participants enrolled in the EWC are representative of the population enrolled in the original cohorts based on a comparison of key sociodemographic characteristics (Tables 1 and 2). We compared pregnancies/births in the EWC with those in the United States using the Centers for Disease Control and Prevention Natality Data (Web Table 7) (39). From 2007–2021, EWC participants who were pregnant at the time of enrollment into their cohorts were more likely to be non-White than the US pregnant population during those years. In addition, Indigenous populations are more highly represented in the EWC than the US population (3.6% of pregnancies from 2016–2021 vs. 1.0%, respectively). This is expected since a goal of the ECHO Program is to increase representation of non-White children in the EWC to examine child health by population subgroups. Similarly, the EWC has overrepresentation of individuals of Puerto Rican descent, contributing to 31.7% of those born in 2016–2021 reporting Hispanic ethnicity. Pregnant EWC participants also have higher levels of educational attainment than the US population.
It is fair to ask, “Whom does the EWC represent?” given the amalgamation of multiple cohorts in which the samples were chosen using different approaches. While it has been argued that “representativeness” is not necessary for internal validity, we now know approaches in which the sample may be reweighted by the effect measure modifiers to generalize to a target population (40). The EWC has the sample size and breadth of variables and has captured the necessary effect measure modifiers to enable powerful statistical analyses to reflect well-defined target populations and allow for the generalization of study results to the broad US population.
Strengths of the ECHO-Wide Cohort study
Key strengths of the EWC include the richness of data, both extant data collected prior to EWC and from new standardized data collection, the size and heterogeneity of the participant population, extensive and diverse investigator expertise, and a focus on “solution-oriented research” (Figure 2). The cohorts’ focus on both specific subpopulations and more general populations paired with the significant size of the combined EWC allows for the development of evidence-based strategies for pediatric care and risk reduction in populations that have been missing from the body of scientific research. For example, 4.1% of pregnant people enrolled in EWC are Indigenous, which for the first time will allow for comparisons of risks and developmental trajectories specific to this population and other similar subsets of the US population where dominant culture results have informed risk and care previously, without validation of their applicability.
Figure 2.
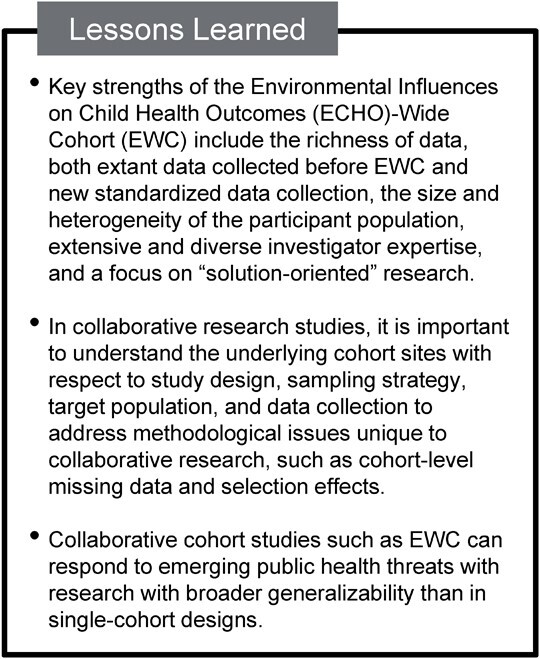
Lessons learned from the Environmental Influences on Child Health Outcomes (ECHO)-Wide Cohort (EWC), a collaborative research design comprising 69 cohorts in 31 consortia, United States, 2022.
This large and diverse sample also permits disentangling of multiple exposures and outcomes simultaneously. The heterogeneity of the EWC participants with regard to exposures enables ECHO researchers to apply sophisticated analyses for orthogonal and correlated exposures across physical, chemical, biological, and social domains. For example, the EWC includes populations largely and uniquely exposed to certain environmental toxins. Similarly, outcomes do not necessarily occur in the absence of other outcomes. Co-occurrence either due to a change in susceptibility when having an outcome or due to a common pathogenic pathway may be studied in the EWC. ECHO investigators showed that although asthma predicted later development of obesity, use of medication for asthma attenuated the effect (41). The concomitant collection and storage of biospecimens with reported exposures at different life stages offers an opportunity for determining longitudinal biological exposure effects.
A cornerstone of ECHO’s focus on “solution-oriented research” is the synergistic collaboration between EWC and the IDeA States Pediatric Clinical Trial Network (42). This allows for observational studies to inform potential interventions and evaluate the real-world effectiveness and modifiers of trial interventions in a large national sample. This structure has the potential to facilitate translation of research to action. Additionally, key stakeholders inform ECHO research priorities and specific research questions to enhance the applicability of ECHO research to inform clinical practice and policy.
The diverse goals and investigator expertise bring a holistic, interdisciplinary perspective on child health (37, 38). Investigators have collaborated on pilot projects expanding upon EWCP data collection, refining data collection measures, and providing mentored research collaborations for junior investigators (43–46). The data collection infrastructure and investigator expertise allow ECHO to pivot to important and urgent issues affecting children’s health. For example, ECHO developed questionnaires assessing the impact of the COVID-19 pandemic on ECHO children and their families.
Conclusion
The EWC brings together a large sociodemographically and geographically diverse participant population, extensive investigator expertise, and a network of successful cohort studies. ECHO is poised to be a leader in solution-oriented child health research and multicohort collaborations with the combination of harmonized extant data and standardized prospective data collection from 69 cohort studies.
Supplementary Material
ACKNOWLEDGMENTS
Author affiliations: Johns Hopkins Bloomberg School of Public Health, Baltimore, Maryland, United States (Emily A. Knapp, Amii M. Kress, Kristen McArthur, Kennedy K. Gachigi, Ghassan B. Hamra, Bryan Lau, Monica McGrath, Heather Volk, Lisa P. Jacobson); Research Triangle Institute, Research Triangle Park, North Carolina, United States (Corette B. Parker, Grier P. Page, Diane Catellier); College of Engineering, Northeastern University, Boston, Massachusetts, United States (Akram N. Alshawabkeh); Department of Pediatrics, Hackensack Meridian School of Medicine, Nutley, New Jersey, United States (Judy L. Aschner); Department of Pediatrics, Albert Einstein College of Medicine, Bronx, New York, United States (Judy L. Aschner); Department of Preventive Medicine, Keck School of Medicine, University of Southern California, Los Angeles, California, United States (Theresa M. Bastain); Department of Population and Public Health Sciences, Keck School of Medicine, University of Southern California, Los Angeles, California, United States (Carrie Breton, Shohreh F. Farzan); Marshfield Clinic Research Institute, Marshfield, Wisconsin, United States (Casper G. Bendixsen); Psychology Department, Emory University School of Medicine, Atlanta, Georgia, United States (Patricia A. Brennan); Department of Psychiatry and Behavioral Sciences, University of California, San Francisco, San Francisco, California, United States (Nicole R. Bush, Bennett Leventhal, Kaja Z. LeWinn); Institute of Medical Psychology, Charité–Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt–Universität zu Berlin, Berlin, Germany (Claudia Buss); Department of Pediatrics, School of Medicine, University of California Irvine, Irvine, California, United States (Claudia Buss); Department of Emergency Medicine, Massachusetts General Hospital, Boston, Massachusetts, United States (Carlos A. Camargo, Jr.); Department of Epidemiology and Biostatistics, College of Public Health, University of Georgia, Athens, Georgia, United States (José F. Cordero); Division of Research, Kaiser Permanente Northern California, Oakland, California, United States (Lisa Croen, Assiamira Ferrara); Lifecourse Epidemiology of Adiposity and Diabetes (LEAD) Center, University of Colorado Anschutz Medical Campus, Aurora, Colorado, United States (Dana Dabelea); Rhode Island Hospital, Providence, Rhode Island, United States (Sean Deoni, Viren D’Sa, Daphne Koinis-Mitchell); New York State Psychiatric Institute, Columbia University, New York, New York, United States (Cristiane S. Duarte); Department of Gynecology and Obstetrics, Emory University School of Medicine, Atlanta, Georgia, United States (Anne L. Dunlop); Avera Research Institute, Center for Pediatric and Community Research, Sioux Falls, South Dakota, United States (Amy J. Elliot); Department of Pediatrics, University of South Dakota School of Medicine, Sioux Falls, South Dakota, United States (Amy J. Elliot); Department of Psychological and Behavioral Sciences, George Washington University, Washington, DC, United States (Jody M. Ganiban); Department of Pediatrics, School of Medicine and Public Health, University of Wisconsin-Madison, Madison, Wisconsin, United States (James E. Gern); Department of Pediatrics, School of Medicine, University of Utah, Salt Lake City, Utah, United States (Angelo P. Giardino); Frank Porter Graham Child Development Institute, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina, United States (Nissa R. Towe-Goodman); Department of Environmental Health, Harvard T .H. Chan School of Public Health, Boston, Massachusetts, United States (Diane R. Gold); Channing Division of Network Medicine, Department of Medicine, Brigham and Women’s Hospital, Boston Massachusetts, United States (Diane R. Gold, Scott T. Weiss); Department of Population and Public Health Sciences, Keck School of Medicine, University of Southern California, Los Angeles, California, United States (Rima Habre); Department of Medicine, Vanderbilt University Medical Center, Nashville, Tennessee, United States (Tina Hartert); Department of Environmental Health Sciences, Mailman School of Public Health, Columbia University, New York, New York, United States (Julie B. Herbstman); Department of Public Health Sciences and MIND Institute, University of California, Davis, Davis, California, United States (Irva Hertz-Picciotto); Department of Psychiatry, School of Medicine, University of Pittsburgh, Pittsburgh, Pennsylvania, United States (Alison E. Hipwell); Department of Epidemiology, Geisel School of Medicine at Dartmouth, Hanover, New Hampshire, United States (Margaret R. Karagas, Juliette C. Madan); Department of Environmental and Occupational and Health Sciences, School of Public Health, University of Washington, Seattle, Washington, United States (Catherine J. Karr); Department of Psychiatry and Behavioral Neuroscience, University of Chicago, School of Medicine, Chicago, Illinois, United States (Kate Keenan); Department of Epidemiology and Biostatistics, Michigan State University, East Lansing, Michigan, United States (Jean M. Kerver); Department of Psychiatry and Human Behavior, The Warren Alpert Medical School of Brown University, Providence, Rhode Island, United States (Daphne Koinis-Mitchell, Barry M. Lester); Department of Pediatrics, The Warren Alpert Medical School of Brown University, Providence, Rhode Island, United States (Daphne Koinis-Mitchell, Barry M. Lester); Brown Center for the Study of Children at Risk, The Warren Alpert Medical School of Brown University, Providence, Rhode Island, United States (Barry M. Lester); Prevention Science Institute, University of Oregon, Eugene, Oregon, United States (Leslie D. Leve); Community Environmental Health Program, College of Pharmacy, University of New Mexico, Albuquerque, New Mexico, United States (Johnnye Lewis); Division of Pediatric Pulmonary Medicine, Department of Pediatrics, University of Rochester, School of Medicine, Rochester, New York, United States (Augusto A. Litonjua); AJ Drexel Autism Institute, Drexel University, Philadelphia, Pennsylvania, United States (Kristen Lyall); Department of Pediatrics, Geisel School of Medicine at Dartmouth, Hanover, New Hampshire, United States (Juliette C. Madan); Department of Pediatrics, Oregon Health & Science University, Portland, Oregon, United States (Cindy T. McEvoy); University of Michigan School of Public Health, Ann Arbor, Michigan, United States (John D. Meeker); Division of Clinical Immunology, Icahn School of Medicine at Mount Sinai, New York, New York, United States (Rachel L. Miller); Department of Environmental Medicine and Public Health, Icahn School of Medicine at Mount Sinai, New York, New York, United States (Rachel L. Miller, Susan L. Teitelbaum, Rosalind J. Wright); Department of Environmental Health Sciences, University of California, Berkeley, California, United States (Rachel Morello-Frosch); Department of Psychology, Pennsylvania State University, University Park, Pennsylvania, United States (Jenae M. Neiderhiser); Department of Psychology, School of Arts and Sciences, University of Rochester, Rochester, New York, United States (Thomas G. O’Connor); Department of Psychiatry, School of Medicine, University of Rochester, Rochester, New York, United States (Thomas G. O’Connor); Department of Neuroscience, School of Medicine, University of Rochester, Rochester, New York, United States (Thomas G. O’Connor); Department of Obstetrics and Gynecology, School of Medicine, University of Rochester, Rochester, New York, United States (Thomas G. O’Connor); Harvard Pilgrim Health Care Institute, Boston, Massachusetts, United States (Emily Oken); Department of Pediatrics, School of Medicine, University of North Carolina at Chapel Hill, Chapel Hill, North Carolina, United States (Michael O’Shea); Department of Epidemiology and Biostatistics, College of Human Medicine, Michigan State University, East Lansing, Michigan, United States (Nigel Paneth); Department of Family and Preventive Medicine, School of Medicine, University of Utah, Salt Lake City, Utah, United States (Christina A. Porucznik, Joseph B. Stanford); Department of Pediatrics, School of Medicine, University of Washington, Seattle, Washington, United States (Sheela Sathyanarayana); Seattle Children's Research Institute, University of Washington, Seattle, Washington, United States (Sheela Sathyanarayana); Department of Comparative Biosciences, College of Veterinary Medicine, University of Illinois at Urbana-Champaign, Urbana-Champaign, Illinois, United States (Susan L. Schantz); Division of Neuroscience, Oregon National Primate Research Center, Beaverton, Oregon, United States (Eliot R. Spindel); Zucker School of Medicine at Hofstra/Northwell, Cohen Children’s Hospital, New Hyde Park, New York, United States (Annemarie Stroustrup); Department of Pediatrics, NYU Grossman School of Medicine, New York, New York, United States (Leonardo Trasande); NYU Wagner School of Public Service, New York, New York, United States (Leonardo Trasande); NYU College of Global Public Health, New York, New York, United States (Leonardo Trasande); Department of Psychiatry and Human Behavior, University of California, Irvine, Orange, California, United States (Pathik D. Wadhwa); Department of Pediatrics, School of Medicine, University of California, Irvine, Orange, California, United States (Pathik D. Wadhwa); Department of Epidemiology, University of California, Irvine, Orange, California, United States (Pathik D. Wadhwa); Program on Reproductive Health and the Environment, Department of Obstetrics, Gynecology and Reproductive Sciences, University of California, San Francisco, San Francisco, California, United States (Tracey J. Woodruff); Institute for Exposomic Research, Icahn School of Medicine at Mount Sinai, New York, New York, United States (Rosalind J. Wright); and Department of Preventive Medicine, University of Tennessee Health Science Center, Memphis, Tennessee, United States (Qi Zhao).
E.A.K. and A.M.K. contributed equally to this work as first authors.
Research reported in this publication was supported by the Environmental Influences on Child Health Outcomes (ECHO) program, Office of the Director, National Institutes of Health, under award numbers U2COD023375 (Coordinating Center), U24OD023382 (Data Analysis Center), U24OD023319 with co-funding from the Office of Behavioral and Social Science Research (PROCore), U24ES026539 (HHEAR O’Brien), U2CES026533 (HHEAR Peterson), U2CES026542 (HHEAR Parsons, Kannan), U2CES030859 (Arora), U2CES030857 (HHEAR Fennell, Sumner, Du), U2CES026555 (HHEAR Teitelbaum), U2CES026561 (HHEAR Wright), U2CES030851 (HHEAR Stapleton, Ferguson), and UH3OD023251 (A.N.A.), UH3OD023320 (J.L.A.), UH3OD023332 (L.T.), UH3OD023253 (C.A.C.), UH3OD023248 (D.D), UH3OD023313 (D.K.M.), UH3OD023328 (C.S.D.), UH3OD023318 (A.L.D.), UH3OD023279 (A.J.E.), UH3OD023289 (A.F.), UH3OD023282 (J.E.G.), UH3OD023287 (C.V.B.), UH3OD023365 (I.H.P.), UH3OD023244 (A.E.H.), UH3OD023275 (M.R.K.), UH3OD023271 (C.J.K.), UH3OD023347 (B.M.L.), UH3OD023389 (L.D.L.), UH3OD023344 (MacKenzie), UH3OD023268 (S.T.W.), UH3OD023288 (C.T.M.), UH3OD023342 (K.L.), UH3OD023349 (T.G.O.C.), UH3OD023286 (E.O.), UH3OD023348 (M.O.S.), UH3OD023285 (J.M.K.), UH3OD023290 (J.B.H.), UH3OD023272 (S.L.S.), UH3OD023249 (J.B.S.), UH3OD023305 (L.T), UH3OD023337 (R.J.W.).
Deidentified data from the ECHO Program are available through NICHD’s Data and Specimen Hub (DASH), https://dash.nichd.nih.gov/. DASH is a centralized resource that allows researchers to access data from various studies via a controlled-access mechanism. Researchers can now request access to these data by creating a DASH account and submitting a Data Request Form. The NICHD DASH Data Access Committee will review the request and provide a response in approximately two to three weeks. Once granted access, researchers will be able to use the data for three years. See the DASH Tutorial for more detailed information on the process.
The authors thank our ECHO colleagues; the medical, nursing, and program staff; and the children and families participating in the ECHO cohorts. We also thank Andrew Law, Janet Moore, and Tim Shields for the creation of the manuscript figures, and Jonathan Lewis, Xiuhong Li, Zone Li, Morgan Nelson, Melanie Kelly, and Brooke Walker for their assistance preparing this manuscript. We also acknowledge the contribution of additional ECHO program collaborators in additional acknowledgements in the Web Material.
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Conflict of interest: J.E.G. has served as a consultant to Astra/Zeneca and Meissa Vaccines Inc, has stock options in Meissa Vaccines Inc, and has patents related to rhinovirus production methods. A.A.L. receives royalties from UpToDate, Inc. S.T.W. receives royalties from UpToDate and is on the Board of Histolix, a digital pathology company. The other authors report no conflicts.
REFERENCES
- 1. National Institutes of Health . Environmental Influences on Child Health Outcomes (ECHO) Program: Funding. https://www.nih.gov/echo/funding. Accessed August 9, 2022.
- 2. Wright RO, Teitelbaum S, Thompson C, et al. The child health exposure analysis resource as a vehicle to measure environment in the environmental influences on child health outcomes program. Curr Opin Pediatr. 2018;30(2):285–291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. LeWinn KZ, Caretta E, Davis A, et al. SPR perspectives: Environmental Influences on Child Health Outcomes (ECHO) Program: overcoming challenges to generate engaged, multidisciplinary science. Pediatr Res. 2022;92(5):1262–1269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. National Institutes of Health . Environmental Influences on Child Health Outcomes (ECHO) Program. https://www.nih.gov/research-training/environmental-influences-child-health-outcomes-echo-program. Accessed August 9, 2022.
- 5. Bush NR, Wakschlag LS, LeWinn KZ, et al. Family environment, neurodevelopmental risk, and the Environmental Influences on Child Health Outcomes (ECHO) initiative: looking Back and moving forward. Front Psych. 2020;11:547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Tylavsky FA, Ferrara A, Catellier DJ, et al. Understanding childhood obesity in the US: the NIH Environmental Influences on Child Health Outcomes (ECHO) program. Int J Obes (Lond). 2020;44(3):617–627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Johnson CC, Chandran A, Havstad S, et al. US childhood asthma incidence rate patterns from the ECHO consortium to identify high-risk groups for primary prevention. JAMA Pediatr. 2021;175(9):919–927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gillman MW, Blaisdell CJ. Environmental Influences on Child Health Outcomes, a research program of the National Institutes of Health. Curr Opin Pediatr. 2018;30(2):260–262. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Romano ME, Buckley JP, Elliott AJ, et al. SPR perspectives: scientific opportunities in the Environmental Influences on Child Health Outcomes Program. Pediatr Res. 2022;92(5):1255–1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Environmental Influences on Child Health Outcomes . ECHO program materials. https://dcricollab.dcri.duke.edu/sites/echomaterials/SitePages/Home.aspx. Accessed December 12, 2022.
- 11. Forrest CB, Blackwell CK, Camargo CA Jr. Advancing the science of children's positive health in the National Institutes of Health Environmental Influences on Child Health Outcomes (ECHO) research program. J Pediatr. 2018;196:298–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hansen KD. IlluminaHumanMethylation27kmanifest: annotation for Illumina's 27k methylation arrays. R package version 0.4.0. 2012. https://bioconductor.org/packages/release/data/annotation/html/IlluminaHumanMethylation27kmanifest.html. Accessed May 19, 2022.
- 13. Hansen KD, Aryee M. IlluminaHumanMethylation450kmanifest: annotation for Illumina's 450k methylation arrays. R package version 0.4.0. 2012. https://bioconductor.org/packages/release/data/annotation/html/IlluminaHumanMethylation450kmanifest.html. Accessed May 19, 2022.
- 14. Johnson KC, Houseman EA, King JE, et al. 5-Hydroxymethylcytosine localizes to enhancer elements and is associated with survival in glioblastoma patients. Nat Commun. 2016;7(1):13177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhou W, Laird PW, Shen H. Comprehensive characterization, annotation and innovative use of Infinium DNA methylation BeadChip probes. Nucleic Acids Res. 2017;45(4):e22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Wu MC, Kuan P-F. A guide to Illumina BeadChip data analysis. Methods Mol Biol. 2018;1708:303–330. [DOI] [PubMed] [Google Scholar]
- 17. Wang DG, Fan JB, Siao CJ, et al. Large-scale identification, mapping, and genotyping of single-nucleotide polymorphisms in the human genome. Science. 1998;280(5366):1077–1082. [DOI] [PubMed] [Google Scholar]
- 18. Wojcik GL, Graff M, Nishimura KK, et al. Genetic analyses of diverse populations improves discovery for complex traits. Nature. 2019;570(7762):514–518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Das S, Forer L, Schönherr S, et al. Next-generation genotype imputation service and methods. Nat Genet. 2016;48(10):1284–1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Harris PA, Taylor R, Thielke R, et al. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Harris PA, Taylor R, Minor BL, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. National Institute of Standards and Technology . Standards for Security Categorization of Federal Information and Information Systems. Gaithersburg, MD: United States Department of Commerce; 2004. (Federal Information Processing Standards Publication) (Computer Security Division ITL publication no. 199) 10.6028/NIST.FIPS.199. Accessed July 14, 2022. [DOI] [Google Scholar]
- 23. Gillman M. Environmental Influences on Child Health Outcomes (ECHO)-Wide Cohort (Version 1) [dataset]. NICHD Data and Specimen Hub. https://dash.nichd.nih.gov/study/417122Accessed December 12, 2022.
- 24. US Department of Agriculture Economic Research Service . Rural Urban Continuum Codes (RUCC). https://www.ers.usda.gov/data-products/rural-urban-continuum-codes/. Accessed October 28, 2021.
- 25. Volk HE, Perera F, Braun JM, et al. Prenatal air pollution exposure and neurodevelopment: a review and blueprint for a harmonized approach within ECHO. Environ Res. 2021;196:110320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Schantz SL, Eskenazi B, Buckley JP, et al. A framework for assessing the impact of chemical exposures on neurodevelopment in ECHO: opportunities and challenges. Environ Res. 2020;188:109709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Conradt E, Flannery T, Aschner JL, et al. Prenatal opioid exposure: neurodevelopmental consequences and future research priorities. Pediatrics. 2019;144(3):e20190128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Hipwell AE, Kahn LG, Factor-Litvak P, et al. Exposure to non-persistent chemicals in consumer products and fecundability: a systematic review. Hum Reprod Update. 2019;25(1):51–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Kahn LG, Harley KG, Siegel EL, et al. Persistent organic pollutants and couple fecundability: a systematic review. Hum Reprod Update. 2021;27(2):339–366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lyall K, Ning X, Aschner JL, et al. Cardiometabolic pregnancy complications in association with autism-related traits as measured by the social responsiveness scale in ECHO. Am J Epidemiol. 2022;191(8):1407–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. ECHO Program . ECHO program publications. https://echochildren.org/echo-program-publications/. Accessed December 12, 2022.
- 32. Buckley JP, Kuiper JR, Bennett DH, et al. Exposure to contemporary and emerging chemicals in commerce among pregnant women in the United States: the Environmental Influences on Child Health Outcome (ECHO) Program. Environ Sci Technol. 2022;56(10):6560–6573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Martenies SE, Zhang M, Corrigan AE, et al. Associations between combined exposure to environmental hazards and social stressors and perinatal outcomes in the ECHO-Wide Cohort. Health Place. 2022;76:102858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Blackwell CK, Mansolf M, Sherlock P, et al. Youth well-being during the COVID-19 pandemic. Pediatrics. 2022;149(4):e2021054754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Hamra GB, Lesko CR, Buckley JP, et al. Combining effect estimates across cohorts and sufficient adjustment sets for collaborative research: a simulation study. Epidemiology. 2021;32(3):421–424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Ray D, Muñoz A, Zhang M, et al. Meta-analysis under imbalance in measurement of confounders in cohort studies using only summary-level data. BMC Med Res Methodol. 2022;22(1):143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kress AM SE, Zhong Y, Ning X, et al. Missing data interpolation among cohorts with disparate covariate information in the ECHO-Wide Cohort [abstract]. Presented at the Society for Epidemiologic Research, Chicago, IL, June 14–17, 2022. [Google Scholar]
- 38. Kundu P, Tang R, Chatterjee N. Generalized meta-analysis for multiple regression models across studies with disparate covariate information. Biometrika. 2019;106(3):567–585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Centers for Disease Control and Prevention Wonder . About natality 2007–2020. 2021. http://wonder.cdc.gov/natality-current.html. Accessed March 22, 2022.
- 40. Rothman KJ, Gallacher JEJ, Hatch EE. Why representativeness should be avoided. Int J Epidemiol. 2013;42(4):1012–1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Stratakis N, Garcia E, Chandran A, et al. The role of childhood asthma in obesity development: a Nationwide US multicohort study. Epidemiology. 2022;33(1):131–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Annett RD, Chervinskiy S, Chun TH, et al. IDeA States Pediatric Clinical Trials Network for underserved and rural communities. Pediatrics. 2020;146(4):e20200290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Bekelman TA, Martin CK, Johnson SL, et al. A comparison of the remote food photography method and the automated self-administered 24-h dietary assessment tool for measuring full-day dietary intake among school-age children. Br J Nutr. 2022;127(8):1269–1278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Lyall K, Hosseini M, Ladd-Acosta C, et al. Distributional properties and criterion validity of a shortened version of the social responsiveness scale: results from the ECHO program and implications for social communication research. J Autism Dev Disord. 2021;51(7):2241–2253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zimmerman E, Aguiar A, Aung MT, et al. Examining the association between prenatal maternal stress and infant non-nutritive suck [published online ahead of print December 16, 2021]. Pediatr Res. 2021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. James P, Suel E, Shiman SLR, et al. Street-view greenspace exposure and objective daily rest-activity patterns. Presented at 33rd Annual Conference of the International Society for Environmental Epidemiology, New York, NY, August 23–26, 2021. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



