Abstract
We implemented an online Resident-as-Teacher curriculum for all incoming residents (PGY1s) to provide them with a basic foundation for effective teaching in the clinical learning environment. The curriculum consisted of 5 asynchronous modules delivered via the web from 2017-2021. Prior to starting the course, the PGY1s completed a self-assessment of their teaching ability (pre-test) and then again 7-8 months after completing the course (post-test). Analysis of the paired data from 421 PGY1s showed a statistically significant improvement in the self-ratings of their teaching from pre-test to post-test (p < 0.001). Our findings suggest that an online Resident-as-Teacher curriculum can produce lasting benefits in new residents’ self-confidence as educators.
Keywords: Resident-as-Teacher, Asynchronous instruction, Program evaluation, Clinical teaching
Background
Although the Liaison Committee of Medical Education (LCME) requires residents to participate in the clinical teaching of medical students [1], very few are prepared to do so upon entering their post-graduate training programs. For this reason, many residency programs have implemented “resident-as-teacher” (RasT) curricula to impart basic teaching skills and improve residents’ self-confidence as educators [2–5]. A variety of in-person instructional formats have been used to administer RasT curricula, ranging from one-day workshops [6] to year-long longitudinal experiences [7]. Regardless of the instructional formats employed, most RasT curricula have been shown to produce beneficial outcomes in terms of residents’ self-reported teaching skills and attitudes [6–12]. However, scheduling in-person RasT training in the resident workweek can be logistically challenging, which prompts consideration of online forms of instruction.
At the Indiana University School of Medicine (IUSM), approximately 400 first-year residents (PGY1s) across specialties begin their post-graduate training each year. The IUSM RasT Advisory Panel – composed of faculty educators, residents, and medical students – was tasked by the school leadership of Graduate Medical Education with implementing a school-wide RasT curriculum for all incoming PGY1s to provide them with the requisite pedagogical skills and self-confidence to be more effective educators of our medical students. A principal requirement of this curriculum was that it be delivered asynchronously and on-demand to avoid having to schedule numerous in-person training activities across our multiple teaching hospitals and disciplines, each with their own schedules. Moreover, the curriculum was to provide foundational RasT training applicable to all PGY1s, regardless of specialty, and therefore serve as a complement to whatever discipline specific RasT training the residents might encounter later in their respective disciplines (e.g., medicine, pediatrics, surgery, etc.).
Although in-person RasT curricula have been amply studied [2–4], published reports on the efficacy of online RasT curricula are more limited [10]. We report here the results of our four-year experience with an online RasT curriculum at IUSM.
Activity
The overarching goal of our online RasT curriculum was to provide all PGY1s with the foundational pedagogical skills necessary to improve their self-confidence and comfort teaching in the clinical learning environment. In developing our online curriculum, we followed Kern’s six-step approach as described by Thomas et al. [13]: (1) identify the problem, (2) conduct a needs assessment, (3) define goals and objectives, (4) determine an educational strategy, (5) implement the curriculum, and (6) evaluate the outcomes. After initial planning sessions and a needs assessment, the IUSM RasT Advisory Panel used an A3 structured problem-solving process [14] to establish five curricular goals and to create the associated curricular content. Each of the five curricular goals was the basis for a separate online module (Table 1). These modules focused on our institutional and clerkship learning objectives and incorporated videos of best practices in clinical teaching. The modular curriculum (all 5 modules) was designed to be completed in 2-3 hours asynchronously at the resident’s convenience.
Table 1.
The Online Modular Resident-as-Teacher Curriculum at Indiana University School of Medicine, 2017-2021
| Module 1: Build/construct a safe learning environment |
|
▪ Communicate clear expectations based upon institutional and clerkship learning objectives, including the learner's goals ▪ Treat all learners fairly, respectfully, and without bias ▪ Project a friendly and approachable demeanor in which learners can ask questions freely without fear of judgement |
| Module 2: Develop clinical learning environment teaching strategies |
|
▪ Develop a working knowledge of multiple teaching strategies which can be used in the clinical environment and understand situations where each may be most effectively implemented (SNAPPS, SPIT, Just-in-Time, One-Minute Preceptor, Horizontal Learning) ▪ Seek out and recognize opportunities for clinical teaching of medical students ▪ Tailor clinical teaching to learner-identified needs, and assist the learner in recognizing areas for improvement |
| Module 3: Act as a positive role model in all clinical settings |
|
▪ Recognize that every interaction with and seen by a learner is an opportunity for role modeling ▪ Discuss with learners and model methods of effective communication ▪ Demonstrate respect, empathy, and professionalism in all interactions |
| Module 4: Assess the student's performance and provide feedback |
|
▪ Assess learners based upon their clerkship performance in accordance with defined learning objectives ▪ Provide ongoing formative feedback to the learners |
| Module 5: Enhance your professional development as a clinical teacher |
|
▪ Solicit feedback on teaching from learners, peers, and supervisors ▪ Receive feedback with a mindfulness without defensiveness ▪ Reflect upon feedback received and develop a self-improvement plan of one's teaching skills |
From 2017 to 2021, all incoming residents at IUSM were required to complete the modular RasT curriculum delivered via Canvas, a web-based learning management system [15]. Prior to beginning the curriculum, the PGY1s completed a self-assessment of their teaching ability and identified their greatest needs for improvement (pre-test) and then repeated the same self-assessment again 7-8 months after completing the curriculum (post-test). Quality improvement assessments were also obtained at the completion of each module. All datasets were deidentified prior to analysis.
Results
Across the four years of curricular implementation, 421 first-year residents completed both the pre-test and the post-test, thereby providing a matched-pair dataset for statistical analysis. In response to the prompt, “I rate my teaching ability in the clinical learning environment as…,” about two-thirds of the respondents (69%) on the pre-test rated themselves “below average” or “average” and about one-third (31%) rated themselves “above average” or “excellent” (Fig. 1). By contrast, on the post-test, less than half (48%) of the respondents rated themselves “below average” or “average” and a majority (53%) rated themselves “above average” or “excellent” (Fig. 1). Using the McNemar-Bowker test, we found this to be a statistically significant improvement in the teaching self-ratings from pre-test to post-test, p<0.001 (two-tailed).
Fig. 1.
Likert scale responses of 421 first-year residents at Indiana University School of Medicine, 2017-2021. After the Resident-as-Teacher training, a smaller proportion of residents rated themselves “below average” or “average” and a greater proportion of residents rated themselves “above average” or “excellent” (analysis of paired data by McNemar-Bowker test, p < 0.001)
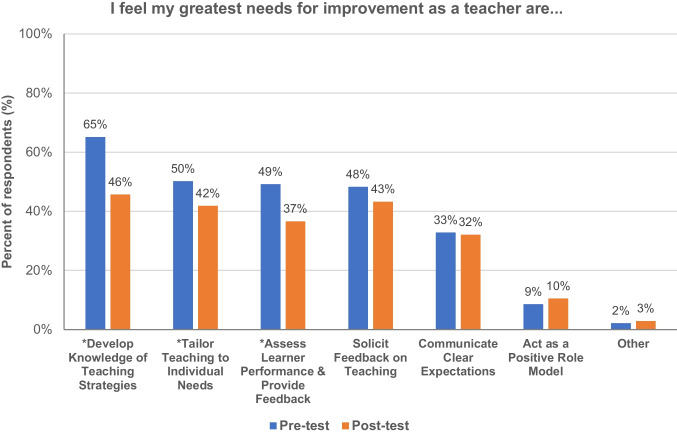
In response to the prompt, “I feel my greatest needs for improvement as a teacher are…,” respondents selected their answers from a list of 6 pre-identified teaching skills. The top 3 needs for improvement selected on the pre-test were: “Develop knowledge of teaching strategies” (65%), “Tailor teaching to individual needs” (50%), and “Assess learner performance and provide feedback” (49%) (Fig. 2). On the post-test, the proportion of respondents selecting these 3 needs for improvement was reduced to 46%, 42%, and 37%, respectively (Fig. 2). These were statistically significant reductions from pre-test to post-test (McNemar test, p<0.01, two tailed). The other identified needs for improvement remained essentially unchanged from pre-test to post-test and included “Solicit feedback on teaching” (43%), “Communicate clear expectations” (32%), and “Act as a positive role model” (10%) (Fig. 2).
Fig. 2.
Responses of 421 first-year residents at Indiana University School of Medicine, 2017-2021. *Statistically significant reduction from pre-test to post-test (analysis of paired data by McNemar test, p < 0.01)
Discussion
Based on the resident’s self-reported data, our online RasT curriculum successfully met its goal of improving the PGY1s’ self-confidence and comfort teaching in the clinical learning environment. This is evidenced by the statistically significant downward shift in the proportion of residents rating themselves “below average/average” (69% pretest to 48% post-test) and the upward shift in the proportion of residents rating themselves “above average/excellent” (31% pretest to 53% post-test). Moreover, after completing the online RasT curriculum, fewer residents self-reported needing improvement in 3 of the 6 identified teaching skills, which suggests an acquisition of skills imparted by the curriculum. These outcomes are consistent with those reported for in-person RasT curricula [6–9, 11, 12].
Using an online approach similar to our own, Bettendorf et al. [10] created a 22-min video module that promoted five key concepts for being an effective clinical teacher. All incoming residents at the Medical College of Wisconsin were required to view the module, followed by an optional evaluation (completed by 294 of 325 residents). About two-thirds of the respondents “agreed/strongly agreed” that viewing the module increased their ability and confidence to teach medical students; however, no evaluation was given prior to viewing the module to assess the residents’ baseline skills or attitudes regarding teaching.
A significant challenge in evaluating any RasT curriculum, regardless of mode of instruction, is measuring improvement in teaching ability. Due to practical considerations, most published studies of RasT curricula have used participant self-evaluations, at least in part, to assess their learning outcomes [2–5]. According to Kirkpatrick’s four-level model for evaluating learning outcomes [16], our residents clearly attained Level 1 (learner reaction) and Level 2a (learner change in attitude), and possibly Level 2b (learner acquisition of skills). The chief limitation of using self-reported data is the inability to demonstrate higher-order benefits like learner behavioral change (Level 3) or systemic educational improvements (Level 4) directly attributable to the intervention. Whether the residents’ teaching ability in the clinical learning environment is demonstrably better remains to be determined. Another limitation is the fact that we were not able to assess the impact of the curriculum on those residents who did not complete both the pre-test and the post-test.
Despite these limitations, we believe our online RasT curriculum provides an efficient and cost-effective alternative to in-person RasT training. Learning via asynchronous online modules may be an especially attractive option for programs with significant constraints on lecture time or faculty involvement. The online approach to RasT training is easy to administer, fulfils LCME requirements, and is convenient for the residents. It also provides a suitable platform for incorporating important learning opportunities related to health equity and anti-racism, which we have recently embedded in our revised online RasT curriculum [17].
Going forward, we hope to directly assess the residents’ teaching ability by employing Objective Structured Teaching Encounters (OSTEs), in which standardized learners (actors portraying medical students) perform scripted roles in clinical teaching scenarios [18]. Residents are observed interacting with the standardized learners during the teaching encounter and then receive feedback from trained observers. By employing OSTEs before and after the RasT training, we may be able to clearly demonstrate improved teaching skills (Level 2b) and effective behavioral changes (Level 3) attributable to the intervention. Such an approach would enable us to objectively evaluate the effectiveness of our RasT curriculum, including the optimal time for teacher training and how long the residents’ teaching skills are retained after the training.
Authors’ Contributions
All authors have read and approved the final manuscript.
Funding
No grants, funds, or other support was received for conducting this study.
Data Availability
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics Approval
This study was granted exempt status by Indiana University’s Institutional Review Board.
Conflict of Interests
The authors declare they have no conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Liaison Committee of Medical Education. Functions and structure of a medical school. 2022. https://lcme.org/publications/. Accessed 20 Dec 2022.
- 2.Wamsley MA, Julian KA, Wipf JE. A literature review of "resident-as-teacher" curricula: do teaching courses make a difference? J Gen Intern Med. 2004;19(5 Pt 2):574–81. doi: 10.1111/j.1525-1497.2004.30116.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hill AG, Yu TC, Barrow M, Hattie J. A systematic review of resident-as-teacher programmes. Med Educ. 2009;43(12):1129–40. doi: 10.1111/j.1365-2923.2009.03523.x. [DOI] [PubMed] [Google Scholar]
- 4.Krzyzaniak SM, Cherney A, Messman A, Natesan S, Overbeck M, Schnapp B et al. Curated collections for educators: five key papers about residents as teachers curriculum development. Cureus. 2018;10(2):e2154. 10.7759/cureus.2154. [DOI] [PMC free article] [PubMed]
- 5.Geary A, Hess DT, Pernar LIM. Resident-as-teacher programs in general surgery residency - a review of published curricula. Am J Surg. 2019;217(2):209–13. doi: 10.1016/j.amjsurg.2018.09.003. [DOI] [PubMed] [Google Scholar]
- 6.Chokshi BD, Schumacher HK, Reese K, Bhansali P, Kern JR, Simmens SJ, et al. A "resident-as-teacher" curriculum using a flipped classroom approach: can a model designed for efficiency also be effective? Acad Med. 2017;92(4):511–4. doi: 10.1097/ACM.0000000000001534. [DOI] [PubMed] [Google Scholar]
- 7.Friedman S, Moerdler S, Malbari A, Laitman B, Gibbs K. The pediatric resident teaching group: the development and evaluation of a longitudinal resident as teacher program. Med Sci Educ. 2018;28(4):619–24. doi: 10.1007/s40670-018-0592-8. [DOI] [Google Scholar]
- 8.Langer AL, Bernard S, Block BL. Two-week resident-as-teacher program may improve peer feedback and online evaluation completion. Med Sci Educ. 2018;28(4):633–7. doi: 10.1007/s40670-018-0597-3. [DOI] [Google Scholar]
- 9.Tang Girdwood S, Treasure J, Zackoff M, Klein M. Implementation, evaluation, and improvement of pediatrics residents-as-teachers elective through iterative feedback. Med Sci Educ. 2019;29(2):375–8. doi: 10.1007/s40670-019-00715-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bettendorf B, Quinn-Leering K, Toth H, Tews M. Teaching when time Is limited: a resident and fellow as educator video module. Med Sci Educ. 2019;29(3):631–5. doi: 10.1007/s40670-019-00731-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ratan BM, Johnson GJ, Williams AC, Greely JT, Kilpatrick CC. Enhancing the teaching environment: 3-year follow-up of a resident-led residents-as-teachers program. J Grad Med Educ. 2021;13(4):569–75. doi: 10.4300/JGME-D-20-01167.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Geary AD, Hess DT, Pernar LI. Efficacy of a resident-as-teacher program (RATP) for general surgery residents: an evaluation of 3 Years of implementation. Am J Surg. 2021;222(6):1093–8. doi: 10.1016/j.amjsurg.2021.09.033. [DOI] [PubMed] [Google Scholar]
- 13.Thomas PA, Kern DE, Hughes MT, Tackett SA, Chen BY. Curriculum Development for Medical Education: A Six-Step Approach. 4. Baltimore, MD: Johns Hopkins University Press; 2022. [Google Scholar]
- 14.Jimmerson C. A3 Problem Solving for Healthcare: A Practical Method for Eliminating Waste. 1st ed. New York, NY: Productivity Press; 2007. 10.4324/9780367807627.
- 15.Canvas by Instructure. Teaching and learning software. 2022. https://www.instructure.com/canvas. Accessed 20 Dec 2022.
- 16.Steinert Y, Mann K, Centeno A, Dolmans D, Spencer J, Gelula M et al. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med Teach. 2006;28(6):497-526. 10.1080/01421590600902976. [DOI] [PubMed]
- 17.Williamson FA, Sharp SN, Hills GD, Dilly CK, Nabhan ZM. Leveraging resident-as-teacher training for health equity education: a transformative approach. Teach Learn Med. 2022:1-8. 10.1080/10401334.2022.2147529. [DOI] [PubMed]
- 18.Kay HG, Mahoney MR, Edwards RA. The Objective Structured Teaching Encounter (OSTE) in health professions education: a systematic review. Med Teach. 2023. Published online March 20, 2023. 10.1080/0142159X.2023.2189539. [DOI] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.