Abstract
Practical and effective methods to integrate basic science material into clinical electives are lacking. We developed a primer for medical students participating in an ambulatory endocrinology elective highlighting pathophysiology, symptoms, diagnosis, and management of disorders. Students felt better prepared for the elective and mean scores on the endocrine knowledge test improved (7.5 (SD = 2.4) to 9.6 (SD = 2.2), p < 0.001). The endocrine primer required minimal faculty time and resources while integrating basic science information into a clinical elective, standardizing students’ knowledge, and enhancing student satisfaction with the elective. This innovative primer lays the groundwork to expand to other specialty electives and institutions.
Keywords: Endocrinology, Basic science, Clinical medicine, Self-directed learning
Background
As the trend towards shortening preclinical training in favor of longer clinical training during medical school increases, there has been an emphasis on incorporating basic science knowledge into clinical experience [1]. Basic science knowledge is essential to provide future physicians with the foundation of what underlies diagnostic reasoning and to solve complicated clinical issues [2]. However, clinically focused faculty may lack expertise in basic science training and may have less time to teach medical students due to their heavy clinical burden. Current recommendations to tackle this issue are aimed towards core clerkships, which can span from 5 to 8 weeks and have multiple medical students rotating at a time [3]. Suggestions such as implementing a week-long basic science lecture series or group problem-based learning sessions are not appropriate or practical for shorter, more specialized elective rotations which often may have just one learner during a given period [3].
Therefore, we developed an innovative teaching model for specialty electives to vertically integrate basic science education into clinical training. It was piloted in a 2- to 4-week-long ambulatory endocrinology elective offered to medical students during their clinical years. Based on core elements of adult learning theory, we developed a Primer to integrate basic science material directly relevant to the clinical experience by linking prior knowledge about the common endocrine disorders students will encounter in their elective [4]. We utilized multiple sensory modes of learning with the use of diagrams, tables, and charts, and delivered the primer in an electronic booklet which could be easily accessed and reviewed prior to seeing patients [5–8]. It also offered a means for further self-directed learning by providing students with direct links to resources for evidence-based management recommendations and basic science pathophysiology [9]. Our primer provided learners with material to study at their own pace and time, without the need for a real time faculty lecturer or facilitator.
Activity
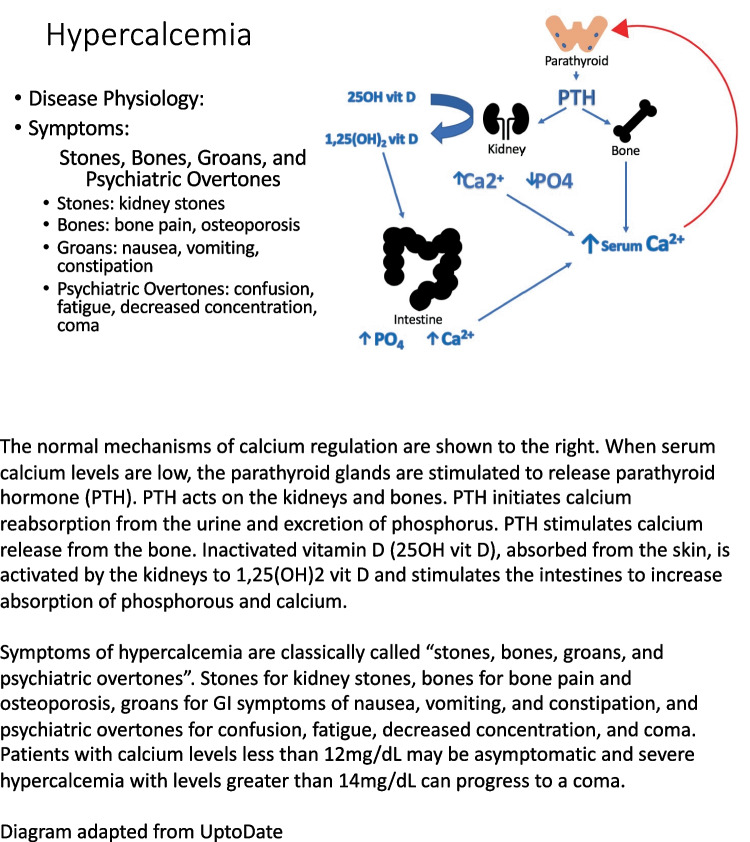
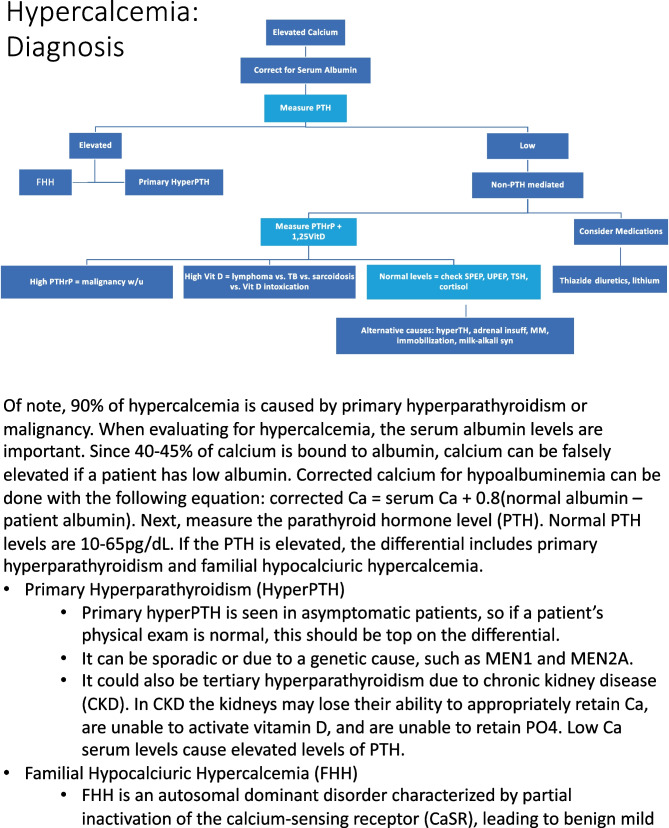
The endocrine primer was developed based on a needs-assessment conducted by surveying core endocrinology teaching faculty and ten medical students who had completed the endocrinology elective the prior two academic years to identify the most frequently seen conditions during the rotation and to gain insight regarding content they thought would be most helpful to review prior to the rotation. Based on our findings, we developed the primer that included content on eight common outpatient endocrine conditions (hyper- and hypothyroidism, type 1 and 2 diabetes mellitus, adrenal insufficiency, hypercalcemia, osteoporosis, and pituitary adenoma) and relevant endocrine physiology, clinical presentation, diagnostic tests, and treatment. Heavy emphasis was placed on including basic science principles (physiology and pathophysiology) with clinical application. See Figs. 1 and 2 for a sample basic science and diagnosis pages from the primer. The endocrine primer was distributed to students by email as suggested reading prior to the start of the rotation and as a resource to refer to during the rotation.
Fig. 1.
Sample basic science page from the endocrine primer
Fig. 2.
Sample diagnosis page from the endocrine primer
Students participating in the pilot completed a 15-item multiple-choice questionnaire pre-test assessing their endocrinology knowledge via an anonymous survey prior to viewing the endocrine primer and then completed the post-knowledge assessment and satisfaction survey at the end of their 2- or 4-week elective (Qualtrics, Seattle, Washington). After the pre-test, students could review the Primer as frequently as they chose during the endocrine rotation. To assess long-term impact of the primer, an attitude change survey was sent to students 3 to 14 months after completing their endocrinology elective. The Rutgers Biomedical Health Sciences Institutional Review Board approved this study.
Results
Twenty-five third- and fourth-year medical students were enrolled in the endocrinology elective from January 2020 to November 2021, and 100% (N = 25) completed a pre- and post-knowledge test and a satisfaction survey surrounding the endocrine primer. There was a significant improvement from pre-knowledge scores (M = 7.5, SD = 2.4) to post-knowledge scores (M = 9.6, SD = 2.2), paired t-test: t(24) = 4.9, p < 0.01.
Students completed the elective satisfaction survey immediately after the post-knowledge assessment. Results from the survey and feedback from students were very positive. The majority of students agreed the primer made them more prepared for the endocrinology elective (21, 84%), and all students would recommend other electives develop similar introductory primers (25, 100%).
Fourteen students completed the attitude change survey 3 to 14 months after their endocrinology elective. All respondents agreed that the primer helped them connect the pathophysiology and symptoms of commonly seen endocrine disorders with the diagnosis and management (14, 100%). The majority of students agreed or strongly agreed the primer changed their way of thinking to integrate basic science information in the clinical setting (10, 72%), and they asked more basic science questions after viewing the primer (10, 72%). Most respondents did not believe the primer changed how they approached other electives (9, 64%). Half of students did believe the primer changed how they approached patient care (6, 55%), and 13 students (93%) were motivated to look up endocrine material which was not in the primer. Representative comments include:
“I think more about the basic science behind the clinical encounters.”
“The diagnosis algorithms for hyper/hypothyroidism and hypercalcemia were very helpful. [The Primer] had a lot of clinically useful information.”
“I especially liked the flow chart to illustrate the diagnostic steps and they really helped me understand.”
“[The Primer] served as a reminder that underlying pathophysiology is IMPORTANT.”
Discussion
As medical curricula favor longer clinical training, it is important to continue to emphasize basic science education for medical students. The endocrine primer was successful in incorporating basic science information via an easy to understand and accessible modality for medical students to review during their clinical ambulatory endocrinology elective. Data collected revealed positive changes via the Kirkpatrick model at levels one (learner satisfaction towards the program), two (change in learner knowledge or attitude) and three (change in learner behavior) [10]. Students even requested other electives provide similar primers.
Advantages of this vertical integration model included the direct application of this information to the clinical experience, the multimodal nature of the training, the minimal requirement for faculty time and resources and the opportunities for further self-directed learning. By having the endocrine primer in place, faculty were encouraged and reminded to discuss basic science relevant to clinical diagnoses, and medical students were able to directly apply the information they reviewed, making their learning more holistic and meaningful. Links were provided to original standard of care management documents and basic science pathophysiology to stimulate curiosity and motivate students to independently read further.
Limitations and Future Directions
Limitations of the study include the small student sample size and its specificity to endocrinology. Additionally, the primer on its own does not provide students with a strong and relevant basic science integration. It should be paired along with a clinical endocrinology elective or rotation to supplement student exposure to patients with endocrine disorders. This preliminary research lays the groundwork for expanding this primer model to other specialty electives at our institution and to other endocrinology electives at different medical schools. Other interventions which will be included with the primer in the future are a toolkit with bedside basic science teaching scripts to better prepare faculty to incorporate this information and short videos reviewing the basic science to provide an auditory modality for learning.
Conclusion
This innovative pilot endocrine primer study provided an effective means of vertically integrating basic science education in a clinical setting. It allowed for more meaningful learning by providing direct application of the material and offered multiple modes of learning experience for medical students with limited faculty resources over a short period time. This educational model should be expanded to include further educational tools and to other specialty electives and endocrine electives at other schools.
Data Availability
The data supporting the findings of this study, i.e. knowledge and qualitative surveys, are available from the authors upon request.
Declarations
Conflict of Interests
The authors declare no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Haudek SB, Bahner I, Belovich AN, et al. How science educators still matter: leveraging the basic sciences for student success. Med Sci Educ. 2022;32(3):747–753. doi: 10.1007/s40670-022-01549-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pangaro L. The role and value of the basic sciences in medical education: the perspective of clinical education - students’ progress from understanding to action. J Int Assoc Med Sci Educ. 2010;20(3):307–313. [Google Scholar]
- 3.Daniel M, Morrison G, Hauer KE, et al. Strategies From 11 U.S. Medical schools for integrating basic science into core clerkships. Acad Med. 2020; Publish Ah. 10.1097/acm.0000000000003908. [DOI] [PubMed]
- 4.Kaufman D, Mann K. Understanding medical education: evidence, theory and practice. 2nd ed. (Swanwick T, Wiley & Sons J, eds.). West Sussex: Wiley-Blackwell; 2013.
- 5.Fleming N. I’m different; not dumb. Modes of presentation (VARK) in the tertiary classroom. In: Research and Development in Higher Education; 1995:308–313.
- 6.Metcalf MP, Tanner BT, Buchanan A. Effectiveness of an online curriculum for medical students on genetics, genetic testing and counseling. Med Educ Online. 2010;15(1):4856. doi: 10.3402/meo.v15i0.4856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tamler R, Green D, Skamagas M, Breen T, Looker H, LeRoith D. Effect of case-based training for medical residents on confidence, knowledge, and management of inpatient glycemia. Postgr Med. 2011;123(4):99–106. doi: 10.3810/pgm.2011.07.2309. [DOI] [PubMed] [Google Scholar]
- 8.Miller P. Learning styles: the multimedia of the mind. In: Educational Resources Information Center. 2001;451(140):2–10.
- 9.Liaison Committee on Medical Education. Functions and structure of a medical school: standards for accreditation of medical education programs leading to the MD degree 2024–25. http://lcme.org/publications/. Accessed 28 Apr 2023.
- 10.Kirkpatrick D, Kirkpatrick J. The Four Levels: An Overview. In Evaluating Training Programs: The Four Levels. 3rd ed. San Francisco: Berrett-Koehler Publishers; 2006. pp. 21–26.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data supporting the findings of this study, i.e. knowledge and qualitative surveys, are available from the authors upon request.