To the Editor:
We read with interest the case report titled ‘Hemoglobin Cast Nephropathy’ by Mahmud S. et al.,1 published in KI Reports on June 29, 2020. The authors have reported 2 cases of intravascular hemolysis associated hemoglobin cast nephropathy. Intravascular hemolysis in the first case was due to rifampicin therapy for a patient with recurrent Mycobacterium avium infection. The underlying cause of hemolysis in the second case was autoimmune hemolytic anemia.
Rifampicin is widely used in India in the treatment of tuberculosis. We reviewed the case files of 77 patients who had a renal biopsy diagnosis of hemoglobin cast nephropathy. Among them, 26 patients (33.8%) had rifampicin-induced intravascular hemolysis. Of the 26 patients (14 male and 12 female, with mean age 48.8 years), 25 had pulmonary tuberculosis and 1 patient had tuberculosis of the spine. Sixteen patients had intermittent intake of rifampicin, 7 patients were treated for relapse of tuberculosis, and 3 patients were on irregular treatment. Six patients presented with rapidly progressive renal failure, 19 patients presented with acute kidney injury, and 1 patient presented with acute on chronic kidney injury. The mean serum creatinine was 9.2 mg/dl. Histologic features of acute tubular injury with pigment cast formation were observed in all the biopsies. In all the cases, the pigment casts were intensely positive for hemoglobin and negative for myoglobin on immunohistochemical staining (Figures 1 and 2).
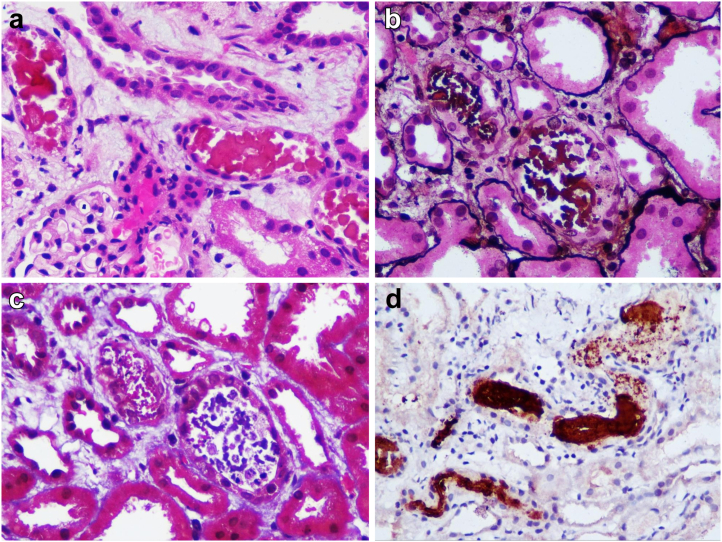
Figure 1.
The hemoglobin casts were (a) globular or a (b) granular appearance. They had a (c) ropy or (d) beaded pattern. (Hematoxylin and eosin)
Figure 2.
The casts appeared (a) pink on periodic acid–Schiff stain, (b) they were brown to black on Jones methenamine silver stain. (c) The color of the casts ranged from blue to red on Masson trichrome stain. (d) Immunohistochemistry for hemoglobin showed intense positive staining on the casts.
At the time of biopsy, 23 patients with rifampicin-induced hemoglobin cast nephropathy were dialysis dependent. Follow-up details are available for 17 of 26 patients. Kidney function has improved with prompt drug withdrawal and supportive care in 14 patients. Three patients continue to be dialysis dependent.
Drug-induced immune hemolytic anemia is a rare condition with an incidence of 1 case per million population.2 Rifampicin is known to cause immunologically mediated intravascular hemolysis and hemolytic anemia.3
Hemoglobin cast nephropathy should be suspected if a patient on rifampicin therapy develops acute kidney injury.4 The accurate diagnosis requires a kidney biopsy with immunostaining for hemoglobin. Recognizing this condition is very important because drug discontinuation is life-saving.
References
- 1.Mahmud S., Dernell C., Bal N., et al. Hemoglobin cast nephropathy. Kidney Int Rep. 2020;5:1581–1585. doi: 10.1016/j.ekir.2020.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Garratty G. Drug-induced immune hemolytic anemia. Hematol Am Soc Hematol Educ Program. 2009:73–79. doi: 10.1182/asheducation-2009.1.73. [DOI] [PubMed] [Google Scholar]
- 3.Gupta A., Sakhuja V., Gupta K.L., Chugh K.S. Intravascular hemolysis and acute renal failure following intermittent rifampin therapy. Int J Lepr Mycobact Dis. 1992;60:185–188. [PubMed] [Google Scholar]
- 4.Covic A., Goldsmith D.J., Segall L., et al. Rifampicin-induced acute renal failure: a series of 60 patients. Nephrol Dial Transplant. 1998;13:924–929. doi: 10.1093/ndt/13.4.924. [DOI] [PubMed] [Google Scholar]