Introduction
Diabetes mellitus is a leading cause of end-stage kidney disease worldwide. Thirty percent of adults with diabetes have chronic kidney disease (CKD) in the United States.1 Multiple randomized controlled trials have shown that sodium-glucose cotransporter 2 inhibitors (SGLT2i) slow the progression of CKD and prolong the time to dialysis in patients with diabetic CKD and nondiabetic CKD.2,3 Despite the robust evidence from randomized controlled trials, the approval by the US Food and Drug Administration, and the strong recommendation by international organizations such as Kidney Disease Improving Global Outcomes, fewer than 10% of patients with an indication for SGLT2i are prescribed this class of medication.4, 5, 6
Multiple factors have been postulated as the cause of underutilization of SGLT2i in patients with diabetic and nondiabetic CKD, especially by specialists like nephrologists.7 These may include lack of familiarity with SGLT2i, high medication cost, prescription burden, prescribing inertia due to lack of ownership by specialists, and structural racism.4 However, there is a paucity of studies examining the reasons for the low use of SGLT2i in patients with CKD. Therefore, we conducted an online survey targeting an international group of nephrologists with the aim to explore their prescribing patterns and barriers in prescribing SGLT2i.
We developed a 9-item online questionnaire (Survey in Supplementary Material), which included age, area of practice, duration of practice, and details about prescribing patterns of SGLT2i. We collected the responses of the anonymous survey via Qualtrics from nephrologists through the Glomerular Disease Study and Trial Consortium’s email distribution list, and via Twitter and Facebook. Glomerular Disease Study and Trial Consortium is a mission-driven nonprofit organization which aims to provide medical education based on best available evidence, free of commercial and ideological bias and create a platform for research collaboration among clinicians, academics, and industry partners guided by patients’ and their caregivers’ needs. The University of Wisconsin Health Sciences’ Institutional Review Board reviewed and determined the study as Minimal Risk Research.
Results
We received responses from 161 survey participants. Eighty-two (51%) of respondents were nephrology fellows or recent graduates in the past 5 years (Supplementary Table S1). Sixty-four (40%) participants practiced in the United States, 35 (22%) in Europe, 28 (17%) in Asia, 15 (9%) in South America, and 4 (3%) in Africa, and 4 (3%) in Australia/New Zealand. Forty-five percent of respondents practiced at a university or academic setting, and 55% of respondents were in private practice. Eighty-three percent of respondents spent more than 50% of their time in clinical practice (Supplementary Table S1).
Ninety-nine (61%) respondents replied that they knew the indications of SGLT2i very well, whereas 62 (39%) replied that they did not know the indications or knew them somewhat well. Fifty-five percent of nephrologists reported prescribing SGLT2i in more than 50% of their patients with CKD who have diabetes and proteinuria. Twenty-three percent of nephrologists reported that they prescribed SGLT2i in <50% of their patients with CKD who have diabetes and proteinuria, and 22% preferred prescribing of SGLT2i by the primary care physician. Thirty-seven percent of nephrologists prescribed SGLT2i in more than 50% of their patients with nondiabetic CKD and proteinuria, and 50% responded that they prescribed in <50% of patients with nondiabetic CKD and proteinuria.
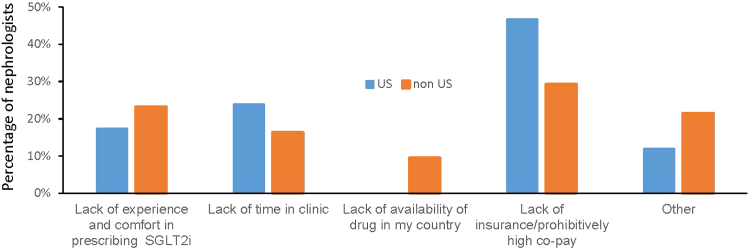
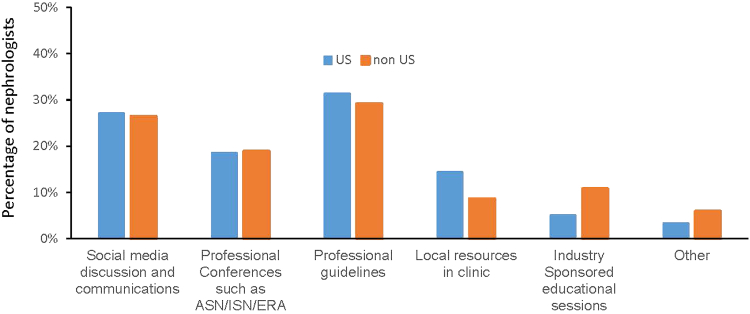
The most common barriers identified in SGLT2i prescribing was lack of insurance or high cost of the medication (37%), lack of time or personnel to discuss the benefits and risks or to manage the side effects of SGLT2i during the clinic visit (20%), and lack of experience and comfort in prescribing SLGT2i (21%) (Figure 1). Lack of insurance or high medication cost was identified as a barrier by significantly more US nephrologists than nephrologists outside the US (47% vs. 29% respectively, P-value = 0.005). There was no difference in the type of barrier when stratified by academic versus private practice. The most common sources of information that nephrologists use as guidance in prescribing SGLT2i in their patients are professional guidelines (30%), social media discussions (26%), and participation in major conferences such as the American Society of Nephrology Annual Kidney Week, International Society of Nephrology World Congress of Nephrology, and European Renal Association Annual Conference (18%) (Figure 2).
Figure 1.
Barriers identified by nephrologists in prescribing SGLT2i. SGLT2i, sodium-glucose cotransporter 2 inhibitor.
Figure 2.
Methods identified by nephrologists to gain knowledge to help prescribing SGLT2i in patients who met the criterion per guidelines. ASN, x; ERA, x; ISN, x.
Discussion
The use of SGLT2i in diabetic and nondiabetic patients with CKD who have proteinuria is associated with better renal survival; however, use of SGLT2i in patients with CKD remains low.2,3,5 In this study, we present the survey findings from 161 practicing nephrologists worldwide regarding their SGLT2i prescribing patterns. We found that even on self-reporting, only 55% of the nephrologists prescribe SGLT2i in >50% of their patients who met criteria. The major barriers identified were lack of insurance or cost of the drug, which was significantly identified more by nephrologists in US than outside US, lack of time or personnel to discuss the benefits and side effects of SGLT2i, and comfort in prescribing SGLT2i. The most common sources of guidance identified by nephrologists were professional guidelines, social media discussions, and annual nephrology conferences.
To our knowledge, this is the first study that reports barriers to SGLT2i prescribing by practicing nephrologists who spend most of their time in patient care and therefore face these issues on a day-to-day basis. The barriers to appropriate utilization of SGLT2i vary and depend on the specific settings.8 Strategies used to overcome these obstacles should be developed and implemented. Therefore, the results from this study acknowledge the challenges in SGLT2i prescribing and may help identify mechanisms to enhance physician prescribing and therefore improve patient care.
Thirty-six percent of nephrologists in our survey reported that they did not know the indications for SGLT2i, and 20% reported lack of familiarity with the medication as a barrier to prescribing SGLT2i. Lack of awareness, familiarity, and educational resources have been found to be the most common causes of physician nonadherence to guidelines.8 Educational interventions and reminders have been shown to be effective in improving adherence to guidelines by physicians. We also inquired about what interventions help them gain more information, and clear written professional guidelines and social media discussions were identified as the top 2 ways to gain new information.
We acknowledge that there are some limitations to our study. The survey was sent to a distribution list via Glomerular Disease Study and Trial Consortium and on social media. This limits the responses to nephrologists that participate in Glomerular Disease Study and Trial Consortium meetings or are active on nephrology social media. However, this enabled us to get survey respondents from around the world, which helps us understand the global practice patterns. Other strengths of our study are that the demographics of our survey respondents is very well distributed among trainees, early-career nephrologists, and well-established nephrologists. Respondents are equally distributed between private practice and academics, which strengthens the study.
In conclusion, we found that the use of SGLT2i in patients with CKD remains low. Major barriers to prescribing SGLT2i include unfamiliarity with drug indication among nephrologists and the cost of medication.
Disclosure
All the authors declared no competing interests.
Footnotes
Survey in Supplementary Material.
Table S1. Demographics of survey respondents.
Supplementary Material
Survey in Supplementary Material.
Table S1. Demographics of survey respondents.
References
- 1.Koye D.N., Magliano D.J., Nelson R.G., Pavkov M.E. The global epidemiology of diabetes and kidney disease. Adv Chronic Kidney Dis. 2018;25:121–132. doi: 10.1053/j.ackd.2017.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Perkovic V., Jardine M.J., Neal B., et al. Canagliflozin and renal outcomes in Type 2 diabetes and nephropathy. N Engl J Med. 2019;380:2295–2306. doi: 10.1056/NEJMoa1811744. [DOI] [PubMed] [Google Scholar]
- 3.Heerspink H.J.L., Stefansson B.V., Correa-Rotter R., et al. Dapagliflozin in patients with chronic kidney disease. N Engl J Med. 2020;383:1436–1446. doi: 10.1056/NEJMoa2024816. [DOI] [PubMed] [Google Scholar]
- 4.Eberly L.A., Yang L., Eneanya N.D., et al. Association of race/ethnicity, gender, and socioeconomic status with sodium-glucose cotransporter 2 inhibitor use among patients with diabetes in the US. JAMA Netw Open. 2021;4 doi: 10.1001/jamanetworkopen.2021.6139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhuo M., Li J., Buckley L.F., et al. Prescribing patterns of sodium-glucose Cotransporter-2 inhibitors in patients with CKD: a cross-sectional registry analysis. Kidney360. 2022;3:455–464. doi: 10.34067/KID.0007862021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group KDIGO 2020 clinical practice guideline for diabetes management in chronic kidney disease introduction. Kidney Int. 2020;98:S1–S115. doi: 10.1016/j.kint.2020.06.019. [DOI] [PubMed] [Google Scholar]
- 7.Claudel S.E., Schmidt I.M., Verma A. A call for implementation science: achieving equitable access to SGLT2 inhibitors. Kidney360. 2022;3:942–944. doi: 10.34067/KID.0001512022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cabana M.D., Rand C.S., Powe N.R., et al. Why don’t physicians follow clinical practice guidelines? A framework for improvement. JAMA. 1999;282:1458–1465. doi: 10.1001/jama.282.15.1458. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.