Abstract
Background
International guidelines have recommended preemptive kidney transplantation (KT) as the preferred approach, advocating for transplantation before the initiation of dialysis. This approach is advantageous for graft and patient survival by avoiding dialysis-related complications. However, recipients of preemptive KT may undergo anesthesia without the opportunity to optimize volume status or correct metabolic disturbances associated with end-stage renal disease. In these regard, we aimed to investigate the anesthetic events that occur more frequently during preemptive KT compared to nonpreemptive KT.
Methods
This is a single-center retrospective study. Of the 672 patients who underwent Living donor KT (LDKT), 388 of 519 who underwent nonpreemptive KT were matched with 153 of 153 who underwent preemptive KT using propensity score based on preoperative covariates. The primary outcome was intraoperative hypotension defined as area under the threshold (AUT), with a threshold set at a mean arterial blood pressure below 70 mmHg. The secondary outcomes were intraoperative metabolic acidosis estimated by base excess and serum bicarbonate, electrolyte imbalance, the use of inotropes or vasopressors, intraoperative transfusion, immediate graft function evaluated by the nadir creatinine, and re-operation due to bleeding.
Results
After propensity score matching, we analyzed 388 and 153 patients in non-preemptive and preemptive groups. The multivariable analysis revealed the AUT of the preemptive group to be significantly greater than that of the nonpreemptive group (mean ± standard deviation, 29.7 ± 61.5 and 14.5 ± 37.7, respectively, P = 0.007). Metabolic acidosis was more severe in the preemptive group compared to the nonpreemptive group. The differences in the nadir creatinine value and times to nadir creatinine were statistically significant, but clinically insignificant.
Conclusion
Intraoperative hypotension and metabolic acidosis occurred more frequently in the preemptive group during LDKT. These findings highlight the need for anesthesiologists to be prepared and vigilant in managing these events during surgery.
Keywords: End-stage renal disease, Intraoperative hypotension, Living donor kidney transplantation, Metabolic acidosis, Preemptive kidney transplantation
Background
Kidney transplantation (KT) is an established treatment for end-stage renal disease (ESRD) [1]. Recently, international guidelines have recommended preemptive KT, which involves performing the transplantation before initiating dialysis [2, 3]. This approach offers several advantages, including improved graft function and patient survival by avoiding dialysis-related complications such as cardiovascular disease and infection [4–10]. Additionally, preemptive KT has been shown to offer significant benefits in terms of patient welfare [11, 12] and societal cost-saving [13, 14].
Patients undergoing preemptive KT may encounter specific challenges related to ESRD due to the relatively shorter transition period from ESRD to surgery. These challenges encompass imbalances in volume status and metabolic disturbances associated with acid/base and electrolyte levels, such as hyperkalemia, calcium, and phosphate disorders. Additionally, ESRD patients are at an increased risk for perioperative bleeding due to impaired platelet function and platelet-vessel wall interactions caused by the accumulation of uremic toxins [15–18]. Unfortunately, these issues often remain unresolved at the time of surgery.
However, there is a paucity of studies assessing the potential risks during anesthesia in preemptive KT patients. Therefore, we planned to investigate the anesthetic events that occur when patients were undergoing preemptive KT and determine which aspects require further attention. We conducted a retrospective cohort study to test our primary hypothesis that the extent and duration of intraoperative hypotension would be greater in the preemptive group compared to the nonpreemptive group.
Methods
Study design
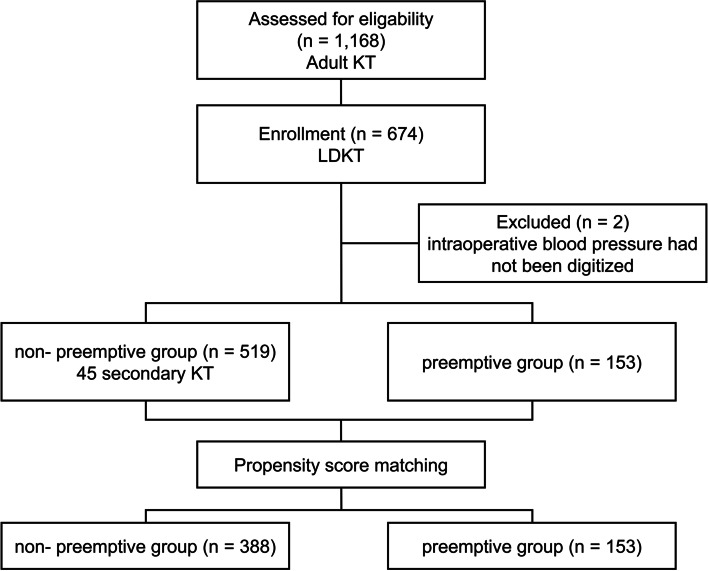
The present study was a single-center, retrospective cohort study. The Institutional Review Board of Samsung Medical Center approved this study and waived the requirement for written informed consent (SMC 2018–10-147–001). A total of 1,168 adult recipients, who underwent KT between April 2010 and October 2018 at Samsung Medical Center, was the initially screened cohort. Among these recipients, 494 recipients who underwent deceased donor KT (n = 494) and with missing digitized data on intraoperative blood pressure (n = 2) were excluded. The remaining 672 recipients who underwent living donor KT (LDKT) were analyzed in the present study, who were divided into the nonpreemptive and preemptive groups (Fig. 1).
Fig. 1.
Flow diagram for study enrollment and grouping
Data collection
Data were obtained from the electronic medical records or a KT database (prospectively collected) and were anonymized/de-identified before analysis. Baseline mean arterial pressure (MAP) was defined as the average of preoperative MAP values measured in the ward noninvasively until the patient was moved to the operating room (maximum of 10 recordings). Intraoperative MAP was recorded every five minutes automatically. We chose the invasive blood pressure values if both invasive and noninvasive blood pressure measurements were available; however, noninvasive blood pressure values were used if the invasive blood pressure could not be relied on due to artifacts. When MAP was not recorded, the MAP was calculated using the systolic and diastolic arterial pressure (SAP and DAP, respectively) according to the following formula: MAP = DAP + 1/3 × (SAP − DAP). Preoperative echocardiographic parameters were collected and used to evaluate the presence of uremic cardiomyopathy which is characterized by ventricular dysfunction and hypertrophy [19]. Left ventricular diastolic dysfunction (LVDD) was assessed according to the clinical comorbidities and echocardiographic findings [20–22]. We classified the patients with ischemic heart disease (IHD), clinical diagnosis of congestive heart failure (CHF), pathologic left ventricular hypertrophy (LVH), or left ventricular ejection fraction < 50% as having LVDD. We defined the cutoff values for LVH as left ventricular mass index > 115 g/m2 in men and > 95 g/m2 in women [23]. The modality and duration of renal replacement therapy, redo-KT, time from the last dialysis to KT in the nonpreemptive group were also investigated.
Intraoperative arterial level of bicarbonate, base excess, and serum electrolytes (i.e., sodium, potassium, and calcium) were collected from the arterial blood gas analysis which was carried out immediately after induction. Postoperative nadir creatinine (Cr) values (i.e., the lowest Cr level in blood tests conducted according to the postoperative protocol), estimated glomerular filtration rate (eGFR), and Cr clearance (CCl) were collected. Serum and urine Cr level was measured with the kinetic alkaline picrate method (Jaffe Method) and the time to attain nadir Cr was determined via retrospective chart review. The eGFR was calculated using the modification of diet in renal disease equation [24].
Outcomes
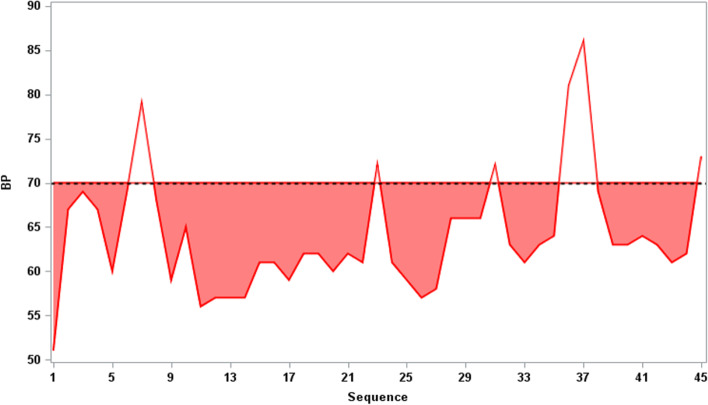
The primary outcome was intraoperative hypotension defined as the sum of the area under the threshold (AUT) on the blood pressure curve. Figure 2 represents AUT calculation. AUT was the area under 70 mmHg in the graph with the X-axis as time and the Y-axis as MAP, reflecting the duration and severity for which an individual's MAP was measured below 70 mmHg. The MAP threshold of 70 was determined according to our institutional protocol and previous meta-analysis on the effect of intraoperative hypotension on end-organ damage [25, 26]. We utilized blood pressure data obtained from the time of surgical incision to graft reperfusion to compute AUT. This approach was implemented to mitigate the influence of various factors that could potentially affect blood pressure levels prior to surgical incision, including endotracheal intubation and positional changes.
Fig. 2.
Scheme for calculating area under the threshold
Secondary outcomes were intraoperative use of inotropes (such as dopamine or dobutamine), vasopressors (such as norepinephrine or vasopressin), or red blood cell transfusion, total volume of crystalloid fluid and synthetic colloid, immediate graft function as defined by the postoperative nadir Cr value and maximum eGFR, time to achieve nadir Cr, and postoperative transfusion and bleeding which was defined as the need for re-exploration due to bleeding.
Anesthesia management
Anesthetic management was performed according to a standardized institutional protocol. No premedication was administered. After the patients arrived at the operating room, standard monitors including a non-invasive blood pressure monitor, pulse oximetry, electrocardiogram, and bispectral index monitor (BIS, Aspect Medical Systems, Natick, MA, USA) were applied. After the intubation was performed, invasive blood pressure monitoring was performed via the right radial artery. An antibiotics-coated 7-Fr three-lumen catheter was placed in the right internal jugular vein and central venous pressure was monitored. Anesthesia was maintained using inhalational anesthetics, desflurane. The oesophageal Doppler probe (CardioQ; Deltex Medical, Irving, TX, USA) or FloTrac/Vigileo monitoring system (FloTrac/Vigileo version 3.02, Edwards Lifesciences, Irvine, CA, USA) was applied, which facilitated estimations of preload and afterload. Balanced crystalloid including Hartmann's solution (JW Pharmaceutical, Seoul, Korea) and Plasma solution A (CJ, Seoul, Korea) were primarily used as the maintenance fluid. Fluid infusion and vasoactive/inotropic drugs were adjusted to maintain MAP ≥ 70 mmHg prior to graft reperfusion and ≥ 90 mmHg following graft reperfusion to improve graft perfusion based on the hemodynamic variables in the CardioQ and FloTrac/Vigileo monitoring system. For patients with metabolic acidosis (base excess < -10 mmol/L) and hemodynamic instability despite the use of vasoactive/inotropic drugs, sodium bicarbonate was infused at the clinician’s discretion. Intraoperatively, the target blood hemoglobin for allogeneic red blood cells was 7.0 g/dl.
Statistical analysis
Statistical analysis was performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and R version 3.4.3 (R Foundation for Statistical Computing, Vienna, Austria) with the package matchIt. Continuous variables were analyzed using the Wilcoxon rank-sum test or Student’s t-test where appropriate and presented as median (interquartile range) or mean (standard deviation) values, respectively. Categorical variables were analyzed using the chi-squared or Fisher’s exact test where appropriate and presented as numbers (%).
We performed propensity score matching using nearest-neighbor matching without replacement and a matching tolerance of 0.2 to balance baseline characteristics and avoid selection bias, which was triggered by a nonpreemptive:preemptive ratio of 3:1 maximally with the following seven covariates: age, sex, diabetes, hypertension, prescription of antihypertensive medications (Angiotensin converting enzyme inhibitor, angiotensin receptor blocker, beta-blocker, or calcium channel block), and history of CHF and IHD. Successful matching was defined when standardized mean difference for matched variables were < 10% [27]. After matching, 388 of 519 in the nonpreemptive group were matched with 153 of 153 patients in the preemptive group (Fig. 1). the group comparison of patient characteristics and outcomes were conducted using an univariable generalized estimating equation (GEE). The association of potential risk factors with intraoperative hypotension defined by AUT was tested by GEE. Factors with a p-value of less than 0.1 in the univariable analysis and group were included in the multivariable analysis. We conducted Spearman’s correlation analysis in the preemptive group to assess the correlation between metabolic acidosis and AUT. A P-value of less than 0.05 was considered to be statistically significant.
Results
The comparison of demographic and clinical parameters between the preemptive group and the nonpreemptive group is shown in Table 1. Prior to propensity score matching, 45 recipient (8.7%) underwent redo-KT. Most patients (473/519, 91.1%) in the nonpreemptive group had received hemodialysis and the median (IQR) duration of renal replacement therapy was 6.1 (2, 34) months, with an average interval of 1.6 days between the last dialysis session and the surgery. The nonpreemptive group exhibited a higher frequency of diabetes and CHF compared to the preemptive group. Conversely, hypertension was more prevalent in the preemptive group. In the matched cohort, the standardized mean differences of all seven matched-covariates were reduced to values below 10%, indicating that an adequate balance was achieved between treatment groups. Echocardiographic parameters suggested that LVH and LVDD were more frequent in the nonpreemptive group compared to the preemptive group. The baseline MAP was not significantly different prior to matching, but after matching, a significant difference was observed between the two groups (99.2 mmHg and 102.0 mmHg, respectively, P < 0.0015).
Table 1.
Patient characteristics
| Characteristics | Entire population | Propensity-score matched population | ||||||
|---|---|---|---|---|---|---|---|---|
| Nonpreemptive | Preemptive | SMD | P value* | Nonpreemptive | Preemptive | SMD | P value** | |
| (n = 519) | (n = 153) | (n = 388) | (n = 153) | |||||
| Age > 60 years | 56 (10.8) | 17 (11.1) | 0.010 | 0.911 | 37 (9.5) | 17 (11.1) | 0.052 | 0.649 |
| Body mass index, kg/m2 | 22.6 (20.4, 25.1) | 22.8 (20.7, 25.3) | 0.038 | 0.748 | 22.6 (20.3, 25.1) | 22.8 (20.7, 25.3) | 0.026 | 0.917 |
| Female sex, n (%) | 211 (40.7) | 66 (43.1) | 0.050 | 0.584 | 159 (41.0) | 66 (43.1) | 0.044 | 0.744 |
| Diabetes, n (%) | 156 (30.1) | 32 (20.9) | 0.211 | 0.027 | 92 (23.7) | 32 (20.9) | 0.067 | 0.406 |
| Hypertension, n (%) | 457 (88.1) | 140 (91.5) | 0.114 | 0.234 | 346 (89.2) | 140 (91.5) | 0.079 | 0.432 |
| Antihypertensive medication, n (%) | 407 (78.4) | 138 (90.2) | 0.328 | 0.001 | 339 (87.4) | 138 (90.2) | 0.090 | 0.430 |
| Cerebrovascular disease, n (%) | 16 (3.1) | 3 (2.0) | 0.072 | 0.587 | 11 (2.8) | 3 (2.0) | 0.057 | 0.534 |
| Congestive heart failure, n (%) | 22 (4.2) | 0 (0) | 0.298 | 0.010 | 0 (0.0) | 0 (0) | N/A | N/A |
| Ischemic heart disease, n (%) | 29 (5.6) | 8 (5.2) | 0.016 | 0.864 | 18 (4.6) | 8 (5.2) | 0.027 | 0.652 |
| Revised cardiac risk index, n (%) | 0.232 | 0.060 | 0.066 | 0.930 | ||||
| 0 | 410 (79.0) | 134 (87.6) | 331 (85.3) | 134 (87.3) | ||||
| 1 | 92 (17.7) | 16 (10.5) | 48 (12.4) | 16 (10.5) | ||||
| 2 | 17 (3.3) | 3 (2.0) | 9 (2.3) | 3 (2.0) | ||||
| Echocardiographic parametersa | ||||||||
| LVEF, % | 62 (57, 66) | 63 (59, 67) | 0.325 | 0.021 | 63 (58, 67) | 63 (59, 67) | 0.224 | 0.017 |
| LVMI, g/m2 | 117.2 (99.3, 145.0) | 100.9 (89.4, 128.5) | 0.455 | < 0.001 | 117.62 (99.9, 147.5) | 100.9 (89.4, 128.5) | 0.466 | < 0.001 |
| LAVI, ml/m2 | 39.3 (31.4, 48.9) | 36 (29.8, 42.3) | 0.363 | 0.006 | 39.75 (32, 48.8) | 36 (29.8, 42.3) | 0.364 | < 0.001 |
| E/A ratio | 0.94 (0.71, 1.2) | 0.92 (0.74, 1.32) | 0.109 | 0.334 | 0.95 (0.7, 1.2) | 0.92 (0.74, 1.32) | 0.085 | 0.290 |
| Deceleration time, m/sec | 222 (193.8, 261.0) | 225.6 (205.1, 252.3) | 0.040 | 0.443 | 220.1 (192.1, 261.0) | 225.6 (205.1, 252.3) | 0.048 | 0.567 |
| E', m/sec | 0.07 (0.06, 0.08) | 0.08 (0.06, 0.1) | 0.325 | < 0.001 | 0.07 (0.06, 0.09) | 0.08 (0.06, 0.1) | 0.239 | 0.005 |
| E/E' ratio | 10 (8, 13) | 8.31 (6.6, 10.3) | 0.619 | < 0.001 | 9.95 (8.0, 12.4) | 8.3 (6.6, 10.3) | 0.592 | < 0.001 |
| TR velocity (m/sec) | 2.4 (2.2, 2.6) | 2.24 (2.1, 2.4) | 0.529 | < 0.001 | 2.4 (2.2, 2.7) | 2.2 (2.1, 2.4) | 0.554 | < 0.001 |
| Left ventricular hypertrophy, n (%) | 300 (64.4) | 56 (42.1) | < 0.001 | 227 (65.0) | 56 (42.1) | 0.473 | < 0.001 | |
| Systolic dysfunction, n (%) | 0.319 | 0.055 | 0.223 | 0.150 | ||||
| LVEF ≥ 60% | 299 (64.2) | 96 (71.6) | 229 (59.0) | 96 (52.7) | ||||
| 50% ≤ LVEF < 60% | 138 (29.6) | 37 (27.6) | 108 (27.8) | 37 (24.2) | ||||
| 40% ≤ LVEF < 50% | 17 (3.6) | 1 (0.7) | 7 (1.8) | 1 (0.7) | ||||
| LVEF < 40% | 12 (2.6) | 0 (0) | 5 (1.3) | 0 (0) | ||||
| Diastolic dysfunction, n (%)b | 0.484 | < 0.001 | 0.430 | < 0.001 | ||||
| Indeterminate | 50 (10.7) | 5 (3.7) | 121 (31.2) | 44 (28.8) | ||||
| Grade 1 | 177 (38) | 44 (32.6) | 38 (9.8) | 5 (3.3) | ||||
| Grade 2 | 92 (19.7) | 18 (13.3) | 72 (18.6) | 18 (11.8) | ||||
| Grade 3 | 5 (1.1) | 0 (0) | 1 (0.3) | 0 (0.0) | ||||
| Preoperative plasmapheresis for ABOi KT | 93 (17.9) | 25 (16.3) | 0.042 | 66 (17) | 25 (16.3) | 0.018 | 0.858 | |
| Modality of renal replacement therapy, n (%) | N/A | N/A | N/A | N/A | ||||
| Hemodialysis | 473 (91.1) | 0 (0) | 351 (90.5) | |||||
| Peritoneal dialysis | 46 (8.9) | 0 (0) | 37 (9.5) | |||||
| Duration of renal replacement therapy, months | 6 (2, 34) | 0 (0, 0) | N/A | N/A | 5.03 (1.7, 29.0) | N/A | N/A | |
| Operation time, min | 183 (155, 213) | 174 (151, 216) | 0.093 | 0.405 | 184 (155, 213) | 174 (151, 216) | 0.097 | 0.422 |
| Baseline Cr, mg/dL | 7.7 (5.7, 10.2) | 7.5 (6.4, 9.2) | 0.089 | 0.980 | 8.1 (6, 10) | 7.5 (6.4, 9.2) | 0.081 | 0.295 |
Data are expressed as as mean ± standard deviation (SD), median (interquartile range), or as number (percentage)
SMD standardized mean difference, LV left ventricular, EF ejection fraction, LAVI left atrial volume index, E/A ratio E/A ratio of peak spectral transmitral flow velocities, E' peak early diastolic tissue velocity at the mitral annulus, TR tricuspid regurgitation, ABOi KT ABO incompatible kidney transplantation, Cr creatinine
*P values were calculated using Mann–Whitney U test, student t-test, chi-square test, or Fisher's exact test
**P values were calculated using generalized estimating equation
a72 missing values for LVEF, 73 missing values for LVMI,76 values for LAVI, 97 missing values for E/A ratio, 102 missing values for deceleration time, 86 missing values for E', 97 missing values for E/E' ratio, 249 missing values for TR velocity
b71 missing values for diastolic dysfunction
Anesthetic events
The anesthetic events that occurred during surgery are summarized in Table 2. The generalized estimating equation demonstrated that the mean AUTs was significantly higher in the preemptive group compared to the nonpreemptive group (29.7 ± 61.0 vs. 14.5 ± 37.7, P = 0.002). This findings consisted in the multivariable analysis, which adjusted for the effect of baseline MBP and RCRI score (P = 0.007). Also, more inotropes and vasopressors were administered in the preemptive group (P < 0.001 and = 0.002, respectively).
Table 2.
Intraoperative outcomes
| Nonpreemptive | Preemptive | p value | |
|---|---|---|---|
| (n = 388) | (n = 153) | ||
| Primary outcome | |||
| AUT (< MAP 70 mmHg)a | 14.5 ± 37.7 | 29.7 ± 61.0 | 0.002 |
| Secondary outcomes | |||
| Inotropic use, n (%) | 54 (13.9) | 43 (28.1) | < 0.001 |
| Vasopressor use, n (%) | 7 (1.8) | 15 (9.8) | < 0.001 |
| Red blood cell transfusion, n (%) | 18 (4.6) | 17 (11.1) | 0.007 |
| Total volume of crystalloid, L | 3.1 (2.5, 3.6) | 3.1 (2.6, 3.7) | 0.127 |
| Total volume of synthetic colloid, L | 0.2 (0, 0.5) | 0.2 (0, 0.5) | 0.675 |
| Initial blood gas analysisb | |||
| Base excess, mmol/L | 0.6 (-1.9, 2.9) | -7.4 (-10.1, -4.9) | < 0.001 |
| Serum bicarbonate, mmol/L | 24.7 (22.5, 26.7) | 18.1 (16.1, 19.9) | < 0.001 |
| Serum sodium level, mmol/L | 136 (134, 138) | 137 (135, 139) | < 0.001 |
| Serum potassium level, mmol/L | 4.1 (3.6, 4.6) | 4.1 (3.8, 4.6) | 0.673 |
| Serum calcium level, mg/dL | 1.0 (1.0, 1.1) | 1.0 (1.0, 1.1) | 0.914 |
| Sodium bicarbonate use, mEq | 0 (0, 0) | 0 (0, 0) | 0.009 |
aAUT (< MAP 70 mmHg), area under the threshold, with a threshold set at a mean arterial blood pressure below 70 mmHg
bBlood gas analysis was carried out immediately after induction
Metabolic acidosis was severe in the preemptive group. Bicarbonate and base excess values in the nonpreemptive were lower and the median (range) dose of intraoperative bicarbonate administered was higher compared to the nonpreemptive group (0 [0, 240] vs. 0 [0, 160], P = 0.009). Finally, base excess values demonstrated low negative correlation with AUT in the preemptive group (Fig. 3).
Fig. 3.
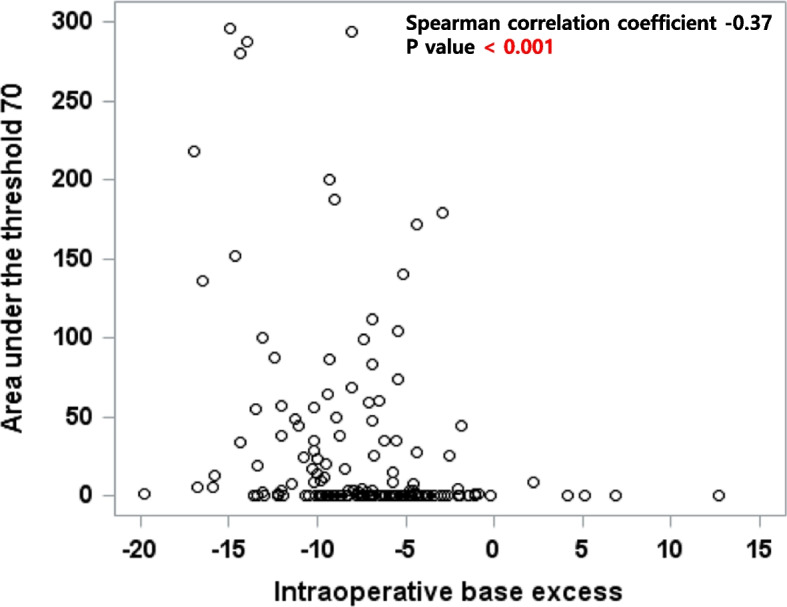
Relationship between intraoperative base excess levels and area under the threshold (AUT) with a threshold set at a mean arterial blood pressure below 70 mmHg
Immediate postoperative outcomes
The details of the immediate postoperative course following KT is summarized in Table 3.
Table 3.
Immediate postoperative outcomes
| Nonpreemptive | Preemptive | p value | |
|---|---|---|---|
| (n = 388) | (n = 153) | ||
| Nadir Creatinine (mg/dL) | 0.96 ± 0.3 | 0.90 ± 0.34 | 0.024 |
| Time to nadir Creatinine (day) | 5.55 ± 4.1 | 4.08 ± 2.3 | < 0.001 |
| Maximum eGRF (mL/min/1.73m2) | 89.7 ± 28.4 | 93.7 ± 27.7 | 0.099 |
| Maximum Cr clearance | 114.7 ± 49.4 | 130 ± 88.3 | 0.050 |
| Postoperative transfusion, n (%)a | 85 (21.9) | 45 (29.4) | 0.082 |
| Postoperative bleeding, n (%)b | 5 (1.3) | 1 (0.7) | 0.528 |
Cr creatinine, eGFR estimated glomerular filtration rate
aPostoperative transfusion within 3 days
bPostoperative bleeding was defined when the recipient required re-exploration because of bleeding
The nadir Cr value in the nonpreemptive group was 0.96 ± 0.3 mg/dL and that in the preemptive group was 0.90 ± 0.34 mg/dL (P = 0.0237), while the times to nadir Cr in the nonpreemptive and preemptive groups were 4.08 ± 2.3 and 5.55 ± 4.12 days, respectively (P < 0.0001); however, neither of these were clinically impressive, even though the differences were statistically significant. Operation time and postoperative bleeding were also not significantly different between the nonpreemptive and preemptive groups.
Discussion
This study was designed based on the hypothesis that preemptive KT patients exhibit greater hemodynamic instability during anesthesia and experience worse postoperative graft function compared to nonpreemptive KT patients. In the preemptive group, the extent and duration of intraoperative hypotension were greater than the nonpreemptive group. Immediate postoperative graft function, as indicated by nadir Cr level and time to nadir Cr level demonstrated a clinically insignificant improvement in favor of the preemptive group compared to the nonpreemptive group.
In the present study, the preemptive group exhibited significantly greater duration and severity of intraoperative hypotension as measured by AUT, despite the nonpreemptive group showing a higher frequency of left ventricular hypertrophy, systolic and diastolic dysfunction. The observed significant of these findings remained after adjusting for baseline MAP in multivariable analysis. Our findings contrast with the results reported in a previous study that compared blood pressure at the beginning, in the middle and end of the surgery [28]. We conducted comparative analysis between the two groups, examining the extent and duration of blood pressure below a specific threshold for blood pressure, which was AUT, utilizing blood pressure data measured at 5-min intervals during surgery. Since there is currently no established threshold for intraoperative hypotension, we used a MBP threshold of 70, based on a meta-analysis that identified a threshold associated with acute kidney injury [25]. Considering that not only the severity but also the duration of intraoperative hypotension has been associated with postoperative end-organ damage [25], AUT may serve as more reliable predictors for post-KT outcomes compared to blood pressures measurements taken at specific time points. Therefore, our findings could be more robust and reliable compared to previous studies that reported insignificant difference regarding the intraoperative blood pressure between the two groups [28].
The observed differences in the extent and duration of hypotension, as measured by AUT, between the two groups may be attributed to differences in metabolic acidosis. In the nonpreemptive group, the majority of patients underwent dialysis the day before surgery (478/519, 92.1%), which resulted in a significantly favorable base-excess profile compared to the preemptive group. The preemptive group exhibited significantly lower levels of intraoperative base excess and bicarbonate compared to the nonpreemptive group, and base excess level demonstrated a weak negative correlation with AUT. Metabolic acidosis could lead to reduction in cardiac contractility and catecholamine efficiency, and decreased vascular responsiveness to inotropics and vasopressors through various mechanisms [29–35]. In this regard, more pronounced metabolic acidosis in the preemptive group might have contributed to the occurrence of intraoperative hypotension.
Several studies have reported favorable outcomes in preemptive KT, including higher rates of graft success and lower rates of delayed graft function and acute rejection [4–7, 28, 36, 37]. However, other studies have suggested that the graft outcomes in the preemptive group are comparable to those in the nonpreemptive group [38–41]. In our study, despite the preemptive group experiencing a greater extent and duration of intraoperative hypotension, we observed statistically significant but clinically insignificant differences in the nadir Cr value and time to reach the nadir Cr level, favoring the preemptive group over the nonpreemptive group. Intraoperative hypotension has been associated with an increased risk of postoperative kidney injury, with studies indicating that prolonged exposure (10 min) to MAP below 80 mmHg and shorter exposure to MAP below 70 mmHg are associated with increased risks [25, 26]. Moreover, the extent of intraoperative hypotension has been reported to be an independent risk factor for slower graft function [42]. Given these findings, one might expect a more detrimental impact on graft function and recovery in the preemptive group, where the extent and duration of intraoperative hypotension were greater. However, our study only revealed clinically insignificant differences. This may be attributable to the fact that we analyzed blood pressure data before graft reperfusion and the anesthesiologists made efforts to maintain the blood pressure above a MAP of 100 mmHg after reperfusion to avoid renal hypoperfusion using appropriate fluids and medications until sufficient urine output was achieved [43].
This study has several limitations. Firstly, this study is a retrospective cohort study conducted at a single center. Therefore, the generalizability of our findings to other populations may be limited and causal inference between the preoperative dialysis and intraoperative blood pressure remains uncertain. Future prospective studies or randomized controlled trials are needed to confirm the results obtained in this study. Secondly, although there is standardized anesthesia protocol for LDKT, some anesthesiologists may have opted for their own anesthesia regimen, deviating from the standardized protocol, which may have led to differences in intraoperative blood pressure. Thirdly, while efforts were made to account for all potential variables influencing intraoperative hypotension, there may be unconsidered confounding factors that persist. Fourthly, propensity score-matching resulted in the exclusion of transplant recipients who were expected to be hemodynamically unstable or have poor outcomes. For instances, no recipients in the preemptive group had a history of CHF, leading to exclusion of 22 recipients of the nonpreemptive group with a history of CHF. This suggests a potential risk of skewing the results. Finally, the present study focused on intraoperative and short-term outcomes, and further research should investigate the long-term implications of preemptive KT.
Conclusion
Intraoperative hypotension and metabolic acidosis occurred more frequently in the preemptive group during LDKT. Our findings highlight the need for anesthesiologists to be prepared and vigilant in managing these events during surgery.
Acknowledgements
Not applicable
Abbreviations
- AUT
Area under the threshold
- CHF
Congestive heart failure
- Cr
Creatinine
- CCl
Creatinine clearance
- DAP
Diastolic arterial pressure
- eGFR
Estimated glomerular filtration rate
- ESRD
End-stage renal disease
- IHD
Ischemic heart disease
- KT
Kidney transplantation
- LDKT
Living-donor KT
- LVDD
Left ventricular diastolic dysfunction
- LVH
Left ventricular hypertrophy
- MAP
Mean arterial pressure
- SAP
Systolic arterial pressure
Authors’ contributions
Name: Jeayoun Kim. Contribution: This author helped data acquisition and analysis and write the manuscript. Name: Kyo Won Lee. Contribution: This author helped analyze the data and write the manuscript. Name: Keoungah Kim. Contribution: This author helped perform the study and write the manuscript. Name: Hyeryung Kang. Contribution: This author helped data acquisition and enroll the patient. Name: Jaehun Yang. Contribution: This author helped data interpretation. Name: Jae berm Park. Contribution: This author helped critical comments. Name: Gaabsoo Kim. Contribution: This author helped study conception and study design. All authors reviewed the manuscript.
Funding
None.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The present study was approved by the institutional review board of Samsung Medical Center and the need for informed consent was waived (approval no. SMC 2018–10-147–001).
All experiments were performed in accordance with Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jeayoun Kim and Kyo Won Lee contributed equally to this work.
References
- 1.Kohei N, Sawada Y, Hirai T, Omoto K, Ishida H, Tanabe K. Influence of dialysis duration on the outcome of living kidney transplantation. Ther Apher Dial. 2014;18(5):481–488. doi: 10.1111/1744-9987.12169. [DOI] [PubMed] [Google Scholar]
- 2.Abecassis M, Bartlett ST, Collins AJ, Davis CL, Delmonico FL, Friedewald JJ, Hays R, Howard A, Jones E, Leichtman AB. Kidney transplantation as primary therapy for end-stage renal disease: a National Kidney Foundation/Kidney Disease Outcomes Quality Initiative (NKF/KDOQI™) conference. Clin J Am Soc Nephrol. 2008;3(2):471–480. doi: 10.2215/CJN.05021107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Procurement O, Network T, Committee MA. Educational guidance on patient referral to kidney transplantation. 2019.
- 4.Chadban SJ, Ahn C, Axelrod DA, Foster BJ, Kasiske BL, Kher V, Kumar D, Oberbauer R, Pascual J, Pilmore HL. KDIGO clinical practice guideline on the evaluation and management of candidates for kidney transplantation. Transplantation. 2020;104(4S1):S11–S103. doi: 10.1097/TP.0000000000003136. [DOI] [PubMed] [Google Scholar]
- 5.Andrews PA, Burnapp L. British Transplantation Society/Renal Association UK guidelines for living donor kidney transplantation 2018: Summary of updated guidance. Transplantation. 2018;102(7):e307. doi: 10.1097/TP.0000000000002253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Knoll G, Cockfield S, Blydt-Hansen T, Baran D, Kiberd B, Landsberg D, Rush D, Cole E. Canadian Society of Transplantation: consensus guidelines on eligibility for kidney transplantation. CMAJ. 2005;173(10):S1–S25. doi: 10.1503/cmaj.1041588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Papalois VE, Moss A, Gillingham KJ, Sutherland DE, Matas AJ, Humar A. Pre-emptive transplants for patients with renal failure: an argument against waiting until dialysis. Transplantation. 2000;70(4):625–631. doi: 10.1097/00007890-200008270-00016. [DOI] [PubMed] [Google Scholar]
- 8.Pérez-Flores I, Sánchez-Fructuoso A, Calvo N, Marques M, Anaya S, Ridao N, Rodríguez A, Barrientos A. Preemptive kidney transplant from deceased donors: an advantage in relation to reduced waiting list. Transplant Proc. 2007;2007:2123–2124. doi: 10.1016/j.transproceed.2007.06.034. [DOI] [PubMed] [Google Scholar]
- 9.Ye H, Zhou Q, Fan L, Guo Q, Mao H, Huang F, Yu X, Yang X. The impact of peritoneal dialysis-related peritonitis on mortality in peritoneal dialysis patients. BMC Nephrol. 2017;18:1–9. doi: 10.1186/s12882-017-0588-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kasiske BL, Snyder JJ, Matas AJ, Ellison MD, Gill JS, Kausz AT. Preemptive kidney transplantation: the advantage and the advantaged. J Am Soc Nephrol. 2002;13(5):1358–1364. doi: 10.1097/01.asn.0000013295.11876.c9. [DOI] [PubMed] [Google Scholar]
- 11.Liem YS, Weimar W. Early living-donor kidney transplantation: a review of the associated survival benefit. Transplantation. 2009;87(3):317–318. doi: 10.1097/TP.0b013e3181952710. [DOI] [PubMed] [Google Scholar]
- 12.Auneau-Enjalbert L, Hardouin JB, Blanchin M, Giral M, Morelon E, Cassuto E, Meurette A, Sébille V. Comparison of longitudinal quality of life outcomes in preemptive and dialyzed patients on waiting list for kidney transplantation. Qual Life Res. 2020;29(4):959–970. doi: 10.1007/s11136-019-02372-w. [DOI] [PubMed] [Google Scholar]
- 13.Huang Y, Samaniego M. Preemptive kidney transplantation: has it come of age? Nephrol Ther. 2012;8(6):428–432. doi: 10.1016/j.nephro.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 14.Dinavahi R, Akalin E. Preemptive kidney transplantation in patients with diabetes mellitus. Endocrinol Metab Clin North Am. 2007;36(4):1039–1049; x. doi: 10.1016/j.ecl.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 15.Barsoum RS. Chronic kidney disease in the developing world. N Engl J Med. 2006;354(10):997–999. doi: 10.1056/NEJMp058318. [DOI] [PubMed] [Google Scholar]
- 16.Renew JR, Pai SL. A simple protocol to improve safety and reduce cost in hemodialysis patients undergoing elective surgery. Middle East J Anaesthesiol. 2014;22(5):487–492. [PubMed] [Google Scholar]
- 17.Folsom AR, Lutsey PL, Astor BC, Wattanakit K, Heckbert SR, Cushman M. Chronic kidney disease and venous thromboembolism: a prospective study. Nephrol Dial Transplant. 2010;25(10):3296–3301. doi: 10.1093/ndt/gfq179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kaw D, Malhotra D. Platelet dysfunction and end-stage renal disease. Semin Dial. 2006;19(4):317–322. doi: 10.1111/j.1525-139X.2006.00179.x. [DOI] [PubMed] [Google Scholar]
- 19.Wang X, Shapiro JI. Evolving concepts in the pathogenesis of uraemic cardiomyopathy. Nat Rev Nephrol. 2019;15(3):159–175. doi: 10.1038/s41581-018-0101-8. [DOI] [PubMed] [Google Scholar]
- 20.Nagueh SF, Smiseth OA, Appleton CP, Byrd BF, Dokainish H, Edvardsen T, Flachskampf FA, Gillebert TC, Klein AL, Lancellotti P. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2016;17(12):1321–1360. doi: 10.1093/ehjci/jew082. [DOI] [PubMed] [Google Scholar]
- 21.Liang HY, Hsiao YL, Yeh HC, Ting IW, Lin CC, Chiang HY, Kuo CC. Associations between myocardial diastolic dysfunction and cardiovascular mortality in chronic kidney disease: A large single-center cohort study. J Am Soc Echocardiogr. 2022;35(4):395–407. doi: 10.1016/j.echo.2021.12.003. [DOI] [PubMed] [Google Scholar]
- 22.Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelisa A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009;10(2):165–193. doi: 10.1093/ejechocard/jep007. [DOI] [PubMed] [Google Scholar]
- 23.Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Flachskampf FA, Foster E, Goldstein SA, Kuznetsova T. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16(3):233–271. doi: 10.1093/ehjci/jev014. [DOI] [PubMed] [Google Scholar]
- 24.Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–470. doi: 10.7326/0003-4819-130-6-199903160-00002. [DOI] [PubMed] [Google Scholar]
- 25.Wesselink E, Kappen T, Torn H, Slooter A, Van Klei W. Intraoperative hypotension and the risk of postoperative adverse outcomes: a systematic review. Br J Anaesth. 2018;121(4):706–721. doi: 10.1016/j.bja.2018.04.036. [DOI] [PubMed] [Google Scholar]
- 26.Sessler DI, Bloomstone JA, Aronson S, Berry C, Gan TJ, Kellum JA, Plumb J, Mythen MG, Grocott MP, Edwards MR. Perioperative quality initiative consensus statement on intraoperative blood pressure, risk and outcomes for elective surgery. Br J Anaesth. 2019;122(5):563–574. doi: 10.1016/j.bja.2019.01.013. [DOI] [PubMed] [Google Scholar]
- 27.D'Agostino RB., Jr Propensity score methods for bias reduction in the comparison of a treatment to a non-randomized control group. Stat Med. 1998;17(19):2265–2281. doi: 10.1002/(sici)1097-0258(19981015)17:19<2265::aid-sim918>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- 28.Aytekin S, Dinç B, Ertuğ Z, Hadimioğlu N, Aytekin EÇ. Perioperative comparison of preemptive and non-preemptive renal transplant recipients. Turk J Anaesthesiol Reanim. 2020;48(2):102. doi: 10.5152/TJAR.2019.34033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kovesdy CP. Metabolic acidosis and kidney disease: does bicarbonate therapy slow the progression of CKD? Nephrol Dial Transplant. 2012;27(8):3056–3062. doi: 10.1093/ndt/gfs291. [DOI] [PubMed] [Google Scholar]
- 30.Kimmoun A, Novy E, Auchet T, Ducrocq N, Levy B. Hemodynamic consequences of severe lactic acidosis in shock states: from bench to bedside. Crit Care (London, England) 2015;19(1):175. doi: 10.1186/s13054-015-0896-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Berger DS, Fellner SK, Robinson KA, Vlasica K, Godoy IE, Shroff SG. Disparate effects of three types of extracellular acidosis on left ventricular function. Am J Physiol. 1999;276(2):H582–594. doi: 10.1152/ajpheart.1999.276.2.H582. [DOI] [PubMed] [Google Scholar]
- 32.Otter D, Austin C. Simultaneous monitoring of vascular contractility, intracellular pH and intracellular calcium in isolated rat mesenteric arteries; effects of weak bases. Exp Physiol. 2000;85(3):349–351. [PubMed] [Google Scholar]
- 33.Levy B, Collin S, Sennoun N, Ducrocq N, Kimmoun A, Asfar P, Perez P, Meziani F. Vascular hyporesponsiveness to vasopressors in septic shock: from bench to bedside. Intensive Care Med. 2010;36(12):2019–2029. doi: 10.1007/s00134-010-2045-8. [DOI] [PubMed] [Google Scholar]
- 34.Jung B, Rimmele T, Le Goff C, Chanques G, Corne P, Jonquet O, Muller L, Lefrant JY, Guervilly C, Papazian L, et al. Severe metabolic or mixed acidemia on intensive care unit admission: incidence, prognosis and administration of buffer therapy. A prospective, multiple-center study. Crit Care (London, England) 2011;15(5):R238. doi: 10.1186/cc10487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kimmoun A, Ducrocq N, Sennoun N, Issa K, Strub C, Escanyé JM, Leclerc S, Levy B. Efficient extra- and intracellular alkalinization improves cardiovascular functions in severe lactic acidosis induced by hemorrhagic shock. Anesthesiology. 2014;120(4):926–934. doi: 10.1097/ALN.0000000000000077. [DOI] [PubMed] [Google Scholar]
- 36.Yoo SW, Kwon OJ, Kang CM. Preemptive living-donor renal transplantation: outcome and clinical advantages. Transpl Proc. 2009;41(1):117–120. doi: 10.1016/j.transproceed.2008.09.063. [DOI] [PubMed] [Google Scholar]
- 37.Joo KW, Shin SJ, Lee SH, Ha JW, Kim S, Kim YS. Preemptive transplantation and long-term outcome in living donor kidney transplantation, single-center experience. Transpl Proc. 2007;39(10):3061–3064. doi: 10.1016/j.transproceed.2007.07.091. [DOI] [PubMed] [Google Scholar]
- 38.Grams ME, Chen BP, Coresh J, Segev DL. Preemptive deceased donor kidney transplantation: considerations of equity and utility. Clin J Am Soc Nephrol. 2013;8(4):575–582. doi: 10.2215/CJN.05310512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Goldfarb-Rumyantzev A, Hurdle JF, Scandling J, Wang Z, Baird B, Barenbaum L, Cheung AK. Duration of end-stage renal disease and kidney transplant outcome. Nephrol Dial Transplant. 2005;20(1):167–175. doi: 10.1093/ndt/gfh541. [DOI] [PubMed] [Google Scholar]
- 40.Ishani A, Ibrahim HN, Gilbertson D, Collins AJ. The impact of residual renal function on graft and patient survival rates in recipients of preemptive renal transplants. Am J Kidney Dis. 2003;42(6):1275–1282. doi: 10.1053/j.ajkd.2003.08.030. [DOI] [PubMed] [Google Scholar]
- 41.Abramowicz D, Hazzan M, Maggiore U, Peruzzi L, Cochat P, Oberbauer R, Haller MC, Van Biesen W. Does pre-emptive transplantation versus post start of dialysis transplantation with a kidney from a living donor improve outcomes after transplantation? A systematic literature review and position statement by the Descartes Working Group and ERBP. Nephrol Dial Transplant. 2016;31(5):691–697. doi: 10.1093/ndt/gfv378. [DOI] [PubMed] [Google Scholar]
- 42.Sandid MS, Assi MA, Hall S. Intraoperative hypotension and prolonged operative time as risk factors for slow graft function in kidney transplant recipients. Clin Transplant. 2006;20(6):762–768. doi: 10.1111/j.1399-0012.2006.00567.x. [DOI] [PubMed] [Google Scholar]
- 43.Abuelo JG. Normotensive ischemic acute renal failure. N Engl J Med. 2007;357(8):797–805. doi: 10.1056/NEJMra064398. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.