Abstract
Introduction
Our prototype wireless full-HD Augmented Reality Head-Mounted Display (AR-HMD) aims to eliminate surgeon head turning and reduce theater clutter. Learning and performance versus TV Monitors (TVM) is evaluated in simulated knee arthroscopy.
Methods
19 surgeons and 19 novices were randomized into either the control group (A) or intervention group (B) and tasked to perform 5 simulated loose-body retrieval procedures on a bench-top knee arthroscopy simulator. A cross-over study design was adopted whereby subjects alternated between devices during trials 1-3, deemed the “Unfamiliar” phase, and then used the same device consecutively in trials 4-5, to assess performance in a more “Familiarized” state. Measured outcomes were time-to-completion and incidence of bead drops.
Results
In the unfamiliar phase, HMD had 67% longer mean time-to-completion than TVM (194.7 ± 152.6s vs 116.7 ± 78.7s, P < .001). Once familiarized, HMD remained inferior to TVM, with 48% longer completion times (133.8 ± 123.3s vs 90.6 ± 55s, P = .052). Cox regression revealed device type (OR = 0.526, CI 0.391-0.709, P < .001) and number of procedure repetitions (OR = 1.186, CI 1.072-1.311, P = .001) are significantly and independently related to faster time-to-completion. However, experience is not a significant factor (OR = 1.301, CI 0.971-1.741, P = .078). Bead drops were similar between the groups in both unfamiliar (HMD: 27 vs TVM: 22, P = .65) and familiarized phases (HMD: 11 vs TVM: 17, P = .97).
Conclusion
Arthroscopic procedures continue to be better performed under conventional TVM. However, similar quality levels can be reached by HMD when given more time. Given the theoretical advantages, further research into improving HMD designs is advocated.
Keywords: image guided surgery, biomedical engineering, ergonomics and/or human factors study, augmented reality
Introduction
Operating room ergonomics and physician wellbeing are important.1-3 During operation, surgeons are required to maintain non-neutral static posture for prolonged periods of time, where stress is placed on the neck or back, leading to physical discomfort and overuse injuries.4-6
Multiple screens are often needed in modern orthopaedic surgery to simultaneously display video and computerized information. This is especially prevalent for minimally invasive surgery,7-9 where procedures often require precise hand-eye coordination and repetitive motion. Concurrent use of endoscopy, fluoroscopy, and computer navigation necessitates multiple monitors to be installed, thus leading to a cluttered and non-ergonomic operative environment.10-12 Furthermore, in constantly turning away to view a surgical display, the surgeon incurs additional neck strain and breaks focus from the operating field, challenging hand-eye coordination and introducing a potential for errors.
Previous attempts to tackle such issues have resulted in the development of Head-Mounted Displays (HMD). 13 These wearable devices allow the surgeon to simultaneously view vital displayed information and the operation site, all whilst maintaining a neutral head position, thus reducing strain and improving hand-eye coordination.14,15 The use of HMD may employ less monitors, leading to a reduction in clutter and cost, as well as increasing efficiency of the surgical team, with studies reporting a reduction in operation times and thus reduced patient radiation exposure.16,17
The widespread use of HMD is hindered by hardware factors such as size, weight, cables, and image quality.14,15,18 Currently, there is insufficient evidence to support the routine use of HMDs. Using current technology, we have developed a lightweight prototype wireless full-HD Augmented Reality Head-Mounted Display (AR-HMD) to eliminate surgeon head turning and reduce operating room clutter. The HMD is primarily designed for fluoroscopy viewing in minimally invasive orthopaedic procedures. Realising that the HMD should have multiple use scenarios, we aim to also evaluate its value in arthroscopic procedures. In this study, the aim is to quantify the learning curve and performance when using the HMD as compared to the use of conventional TV Monitors (TVM) during a simulated knee arthroscopy exercise.
Methods
Device Design
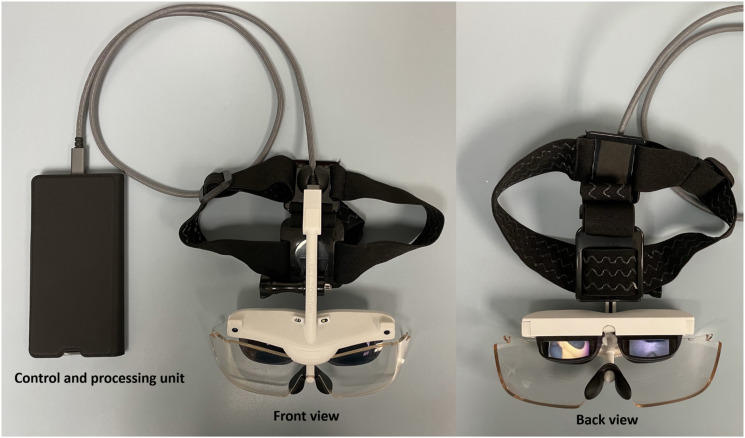
The wearable device was locally engineered and manufactured using nylon powder bed laser fusion 3D printing technology (Figure 1). The internal electronics are modified from a commercially available system, (GLOW Plus, MAD Gaze, Hong Kong SAR, China), with the mounting frame engineered by the investigators in-house using CAD software (3-Matic, Materialise, Leuven, Belgium) and mounted on a headband (GoPro, San Mateo, California, USA). Binocular miniaturized semi see-through organic light emitting diode (OLED) displays, located in the upper visual field of the user, are fed digital signals wirelessly and provide full high-definition (HD) 1920 × 1080 pixels resolution images, allowing the user to view intraoperative information without breaking focus from the surgical site in the lower half of the user’s vision. The system weighs 217g, making it lighter than most models described in the literature and the fit can be adjusted by an elastic headband, which evenly distributes the weight of the device, allowing it to be comfortably worn by any user for long periods of time. The wireless transmission latency is typically less than 50 milliseconds and obviates cables. The system has a battery life of over 3 hours when fully charged.
Figure 1.
Front and back view of the Head-Mounted Display (HMD). The control and processing unit is placed into the surgeon’s breast or side pocket and connected to the HMD via a detachable high speed data cable to minimize weight.
Study Design
We aimed to evaluate the performance of a typical knee arthroscopy procedure in experienced surgeons and untrained personnel when they first start to use the HMD, and after becoming more familiarized, with comparisons to TVM guidance.
A cross-over study design allowed us to minimize confounding factors, improve efficiency of the recruitment target and enable assessment of the effect of familiarization on procedure times (Figure 2). We assessed performance over 5 trials. In the first 3 trials, each user is required to switch alternatively between the HMD and TVM (8000 series, Conmed, USA), keeping them “unfamiliarized” with the use of both devices. In trials 4 and 5, they are assigned to use the same device in consecutive runs, allowing us to assess subject and device performance in a “relatively familiarized” state. Trial results were grouped and analysed accordingly.
Figure 2.
Crossover design of the study. During trials sequence 1-3, the “Unfamiliar” phase, subjects alternate between using HMD and TVM. Trials 4-5 assess subject performance in a more “Familiarized” state, where the subject uses the same device consecutively, specified by their assigned group.
Sample size estimation was performed using G-power software with pilot data from 10 trials of the procedure. A one-tailed non-inferiority margin of .2 was set for the HMD device at effect size .43, type 1 error rate of .05 and power of .8. The calculated sample size was 68 procedures for each group. Since each user will have at least 2 repetitions when familiarized, the minimum number of subjects to be recruited is 34. A mix of experienced and inexperienced users ensured adequate spread of data to better reflect the target user population which may also consist of surgeons and trainees.
Study Subjects
We recruited orthopaedic surgeons with experience in knee arthroscopy (n = 19) and medical students with no prior arthroscopic experience (n = 19). Subject demographics are summarised in Table 1 below. All 38 subjects were randomized by computerized concealed allotment into either the intervention group (A) or control group (B) and tasked to perform 5 simulated loose-body retrieval procedures on a bench-top knee arthroscopy simulator (SKU1400, Sawbones, USA) using either HMD or TVM (Figure 3).
Table 1.
Subject Demographics.
| Novice Group (n = 19) | Experienced Group (n = 19) | P | |
|---|---|---|---|
| Gender | <.001 | ||
| Female | 15 (78.9%) | 3 (15.8%) | |
| Male | 4 (21.1%) | 16 (84.2%) | |
| Surgeon grade | <.001 | ||
| Student | 19 (100%) | — | |
| Resident | — | 8 (42.1%) | |
| Registrar | — | 3 (15.8%) | |
| Associate consultant | — | 4 (21.1%) | |
| Consultant | — | 4 (21.1%) | |
| Year of medical school | <.001 | ||
| 3rd year medical student | 19 (100%) | — | |
| 1-6 years after graduation | — | 8 (42.1%) | |
| 6-10 years after graduation | — | 3 (15.8%) | |
| 10-15 years after graduation | — | 4 (21.1%) | |
| >15 years after graduation | — | 4 (21.1%) |
All factors were tested for significance using chi-square test, with statistically significant P-values denoted in bold.
Figure 3.
Subject testing the HMD in a simulated knee-arthroscopy exercise. In this setup, the subject is instructed not to observe the TV Monitor.
Simulated Surgical Procedure
Each procedure was standardized. Four 6 mm white plastic beads (Precision-grade BB, Airsoft Surgeon, Hong Kong SAR, China) were placed inside the knee arthroscopy simulator; 2 just anterior to the posterior horn of the medial meniscus, and another 2 anterior to the posterior horn of the lateral meniscus. The beads were fixed in position by double-sided adhesive tape. All subjects watched an instructional demonstration of the loose-body retrieval task and familiarized themselves with operation of the camera and basic arthroscopic instruments prior to their first trial, but without being given the chance to retrieve any loose bodies. After confirming that the user had obtained a clear visual field from the display equipment, they were tasked to confirm triangulation and retrieve the 4 beads, as surrogate for “intra-articular loose bodies,” from the bench-top simulator (Figure 4).
Figure 4.
Arthroscopic view of the 6 mm “loose body” being held by an arthroscopic grasper within the knee simulator.
An observer aided in recording data using a standard stopwatch and assisted in standardization of the simulation setup. The total time taken (time-to-completion) for the procedure is defined from insertion of arthroscopic tools into the portal, till exit of the final bead. All incidences of bead drops were recorded, and both outcome variables were used as surrogates for “surgical performance.”
Statistical Analysis
Statistical analysis was performed using SPSS Statistics 27 (IBM, Armonk, USA). Mean completion times between the HMD and TVM trials were compared using independent t-test. Further subgroup analysis was performed for all scenarios to assess the effect of familiarity on subsequent trial times, as well as differences in learning ability between the surgeon and novice groups. Time-to-event analysis was performed using the Kaplan-Meier method with log-rank test, followed by post-hoc Cox proportional hazard regression model analysis to determine the effects of the following factors on time-to-completion: Experience level of the subject (whether the user was an experienced surgeon or novice), familiarization of the technique and task (quantified by progression in the number of repetitions), and specific use of a particular display device (HMD or TVM). Incidence of dropped beads during trials were analyzed using Mann-Whitney U tests. Completion times for crossover trials 1-3 were also compared to ascertain whether users had an affinity for a particular device, defined as both improvement in procedure times when switching to a favored device, and deterioration when switching to the alternative. If only 1 of these criteria was met, the user was deemed to have no affinity to a particular device. A significance threshold of P = .05 was set throughout.
Results
All 38 participants (20 males, 18 females) completed a full set of 5 trials, amounting to a total of 190 arthroscopic procedures for analysis.
Head Mounted Display vs TV Monitor
When considering all trials overall, the use of HMD resulted in longer mean task completion times than TVM (170.4 ± 144.1 vs 106.3 ± 71 seconds (s), P < .001). The mean time difference between familiar and unfamiliarized groups was also statistically significant, with the familiar cohort having shorter completion times (112.2 ± 97.3s vs 155.7 ± 127s, P = .012).
In the unfamiliar phase, the HMD trials had approximately 67% longer mean task completion times than the TVM trials (194.7 ± 152.6s vs 116.7 ± 78.7s, P = .001). Once the groups were familiarized with both methods, the HMD was still shown to be inferior to the TVM, with 48% longer completion times, although reaching borderline significance (133.8 ± 123.3s vs 90.6 ± 55s, P = .052).
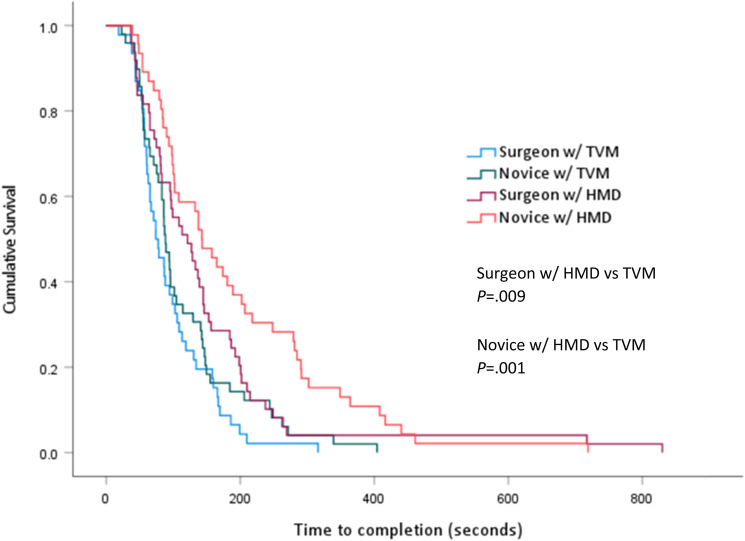
Following Cox regression analysis, use of either HMD or TVM (OR = .526, CI .391−709, P < .001) and progression in the number of repetitions (OR = 1.186, CI 1.072−1.311, P = .001) were found to be significantly and independently related to faster time-to-completion. However, experience, ie, whether the user is a surgeon or a trainee, was not a significant factor (OR = 1.301, CI .971−1.741, P = .078).
Surgeons performed slower with the HMD regardless of device familiarity. (Unfamiliar phase: 58% slower when using HMD (158.3 ± 142.7s vs 100 ± 62.3s, P = .052); familiarized phase: 53% slower when using HMD (138.5 ± 153s vs 90.2 ± 51.3s, P = .211)).
Similar findings were mirrored in the novice group, where the HMD trials took 75% longer on average in the unfamiliar phase (232.5 ± 155.8s vs 132.9 ± 89.9s, P = .004), reducing to 41% longer once familiarized (128.6 ± 83s vs 91 ± 59.5s, P = .114).
Device Affinity
When assessing the results on an individual basis, 4 out of 38 users (11%; 0 of 19 surgeons, 4 of 19 novices) were deemed to have an affinity for HMD, as indicated by their performance during the crossover phase. 24 users preferred TVM (63%; 14 of 19 surgeons, 10 of 19 novices) and the remaining 10 users had no affinity for either device (26%; 5 of 19 surgeons, 5 of 19 novices).
Task Accuracy
133 out of 190 total trials (70%) were completed without a single instance of bead-drop (Table 2). HMD users dropped more beads during the unfamiliar phase (27 vs 22, P = .65). In the familiar phase, less beads were dropped by HMD users (11 vs 17, P = .97). Novices were shown to be more likely than surgeons to drop a bead however these differences were not statistically significant.
Table 2.
Task Accuracy of HMD vs TVM in Both Unfamiliar and Familiarized Phases.
| Incidences of Bead-Drops | Total Cases | Total Beads | Mean Drops per Trial | P | |||||
|---|---|---|---|---|---|---|---|---|---|
| 0 | 1 | 2 | 3 | 4 | |||||
| Unfamiliar | |||||||||
| Surgeon w/HMD | 21 | 8 | 0 | 1 | 0 | 30 | 11 | .37 | |
| Surgeon w/TVM | 20 | 6 | 1 | 0 | 0 | 27 | 8 | .30 | .74 a |
| Novice w/HMD | 16 | 8 | 1 | 2 | 0 | 27 | 16 | .59 | |
| Novice w/TVM | 19 | 9 | 1 | 1 | 0 | 30 | 14 | .47 | .68 b |
| Total | 76 | 31 | 3 | 4 | 0 | 114 | 49 | ||
| Familiarized | |||||||||
| Surgeon w/HMD | 16 | 4 | 0 | 0 | 0 | 20 | 4 | .20 | |
| Surgeon w/TVM | 15 | 2 | 1 | 0 | 0 | 18 | 4 | .22 | .92 a |
| Novice w/HMD | 12 | 5 | 1 | 0 | 0 | 18 | 7 | .39 | |
| Novice w/TVM | 14 | 2 | 2 | 1 | 1 | 20 | 13 | .65 | .92 b |
| Total | 57 | 13 | 4 | 1 | 1 | 76 | 28 | ||
avs Surgeon HMD.
bvs Novice HMD.
Discussion
We observed a clear order of procedure completion times, as illustrated in Figure 5 and Figure 6; surgeons using TVM are fastest, followed by novices using TVM, then surgeons using HMD and finally novices using HMD. Possible causes underlying the longer time-to-completion with HMD include (1) unaccustomed operational environment brought by the use of HMD, where subjects are more familiar with visuals from a traditional screen than an augmented reality; (2) time taken for subjects to adjust the worn HMD due to technical difficulties and or physical discomfort; (3) inadequate resolution or field of view; (4) the video-see through design of the HMD, which presents only the video image obtained from the arthroscope. As a result, subjects are unable to visualize the surrounding environment and the knee joint being operated on in a direct manner. 18 This poses difficulties especially to arthroscopic novices as they may find the switching between portals, adjustment of graspers and arthroscope more challenging. At the current level of technology, HMD is still not viable when compared to conventional TVM. More research is required to enhance ergonomics and image quality of HMD devices. Although our HMD was designed to a high modern standard-full HD (1080p) OLED display technology, low latency (<50 ms), lightweight, and wireless-triumph of HMD over conventional TVM was still unable to be realized.
Figure 5.
Clustered boxplot of time-to-completion for each cohort. The labels represent median values and results are grouped by familiarization state.
Figure 6.
Kaplan-Meier analysis of time-to-completion for each cohort. TVM outperformed HMD in both the surgeon and novice groups.
Despite the aforementioned causes, prevalence of HMD usage in surgery has been increasing due to its advantages relating to the ergonomics of surgical set-ups. 19 It has been found to decrease fatigue by enabling surgeons to maintain a neutral head position regardless of their location relative to the operative field, thus reducing neck strain and incoordination of the hands and eyes when controlling instruments in a paradoxical direction relative to the visual field.14,15 The same studies have also illustrated that HMD increases the efficiency and versatility of surgical procedures as surgeons can maintain optimal visual control by gaining an unhampered view of the site of operation, thereby aiding surgeons to focus on the surgery with reduced restrictions in the operation theater. Other studies have shown significant improvements to posture discomfort scores 18 and reductions in the number of head turns to view the fluoroscopy monitor;16,20 the act of which negatively affects surgeon comfort and hand-eye coordination, providing verification to the claims of added ergonomic benefit of HMD. However, these advantages may not necessarily translate into improved surgical performance, as evident in our study. While such benefits may not be widely utilized and experienced by our subjects, further research involving more complex procedures in a better simulated setting may be of clinical and educational interest.
When comparing the procedure times between the novice and surgeon groups, we found that novices were able to match the performance of experienced surgeons in both HMD and TVM trials, once becoming familiarized over 5 trial runs. Although these results are very encouraging, this may have merely been a limitation of the simulation trial being too straightforward and may not be representative of real-world outcomes. However, this also highlights the use case of such devices for learning and academic purposes, finding application in intraoperative education, 19 where the learner or trainer’s view can be shared and followed in real time, or recorded for review at a later date.21-23
Greater variability in operative times were observed in the HMD group, both in unfamiliarized and familiarized phases. This indicates varying levels of participant competence in task completion using HMD due to factors other than training, eg preference for using HMD. Before the availability of HMD, all surgeons are expected to perform surgeries with TVM; with the availability of HMD, surgeons who are more adept in performing surgery with HMD or have a preference for HMD are empowered by this option. Analogous to “personalized medicine,” optimizing “personalized surgical care” through a comprehensive arsenal of arthroscopic surgery equipment (be it HMD or TVM) tailored to individual needs of each operating surgeon has the potential of enhancing surgical quality and safety.
Our study also found that the error likelihood, assessed by the number of bead drops, is not increased when using HMD. Hence, when the surgeon is determined to perform a certain task, an equal standard of quality can be obtained by spending more time, as compared to an ergonomically inferior setup.
While the potential advantages are clear, widespread use of HMD is not yet commonplace. Early designs suffered from sub-optimal resolutions and weighed up to 1 kg.13-15 Advances in technology have since allowed for HMD to reach smaller form factors 16 with enhanced resolution. Additionally, what was once a bespoke solution has now become a more readily available commercial product.21,23-25 Factors such as weight and comfort should be further improved, as well as streamlining the familiarization process whereby the surgeon can easily become accustomed to a new device. In this regard, technology such as head motion tracking to allow panning of the visual field, iris tracking, and true augmented reality technologies may improve performance of future HMD devices, by not only improving ergonomic positioning of the arthroscopy feed, but also allowing for better targeting accuracy compared to traditional 2D monitors, using superimposed anatomical data. 26
There are several limitations to our study. Firstly, the limited sample size required us to group procedures into unfamiliar vs familiarized pools. We are therefore unable to look at learning curve on a per repetition basis. Secondly, by increasing the number of trials and giving users more time to familiarize themselves with the HMD beforehand, we may have seen further improvements to trial times, as users were unlikely to be completely familiarized even after 5 cycles, hence we are unable to assess the final effect when the users become completely accustomed to HMD. Third, the simulated loose-body recovery procedure may be too elementary, whereby novices were able to closely match or even surpass the performance of experienced surgeons. Finally, both devices were placed in a comfortable and optimized position for viewing, and such a simulation may not be entirely representative of a cluttered operating room environment.
Conclusion
At the current technology level, with our HMD device designed to a high specification of modern standards, arthroscopic procedures continue to be better performed under conventional TVM. However, users are able to complete tasks to a similar quality level when given more time. Given the theoretical advantages of HMD, further research into improving HMD designs is advocated.
Footnotes
Author Contributions: Christian FANG: Study concept and design, Study supervision, Analysis and interpretation
Pinky MO: Acquisition of data, Study supervision
Holy CHAN: Acquisition of data, Study supervision
Jake CHEUNG: Analysis and interpretation
Janus Siu Him WONG: Study supervision
Tak-Man WONG: Study concept and design
Yan-Kit MAK: Study supervision
Kathine CHING: Acquisition of data, Study supervision
Grace HO: Acquisition of data, Study supervision
Frankie LEUNG: Study concept and design, Study supervision
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Christian Fang: Not related to this study; received research funding from Koln 3D Medical Ltd, owner /co-founder of Lifespans, received research support from Brainlab, AO Foundation, speaker for DePuy Synthes Frankie Leung: Owner /co-founder of Lifespans, AO Foundation, speaker for DePuy Synthes.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Holy CHAN https://orcid.org/0000-0001-7713-9519
Jake CHEUNG https://orcid.org/0000-0001-7155-6397
References
- 1.Berguer R. Surgery and ergonomics. Arch Surg. Sep. 1999;134(9):1011-1016. doi: 10.1001/archsurg.134.9.1011. [DOI] [PubMed] [Google Scholar]
- 2.Vijendren A, Yung M, Sanchez J. The ill surgeon: A review of common work-related health problems amongst UK surgeons. Langenbecks Arch Surg. Dec. 2014;399(8):967-979. doi: 10.1007/s00423-014-1233-3. [DOI] [PubMed] [Google Scholar]
- 3.Stucky CH, Cromwell KD, Voss RK, et al. Surgeon symptoms, strain, and selections: Systematic review and meta-analysis of surgical ergonomics. Ann Med Surg (Lond). Mar. 2018;27:1-8. doi: 10.1016/j.amsu.2017.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dalager T, Søgaard K, Bech KT, Mogensen O, Jensen PT. Musculoskeletal pain among surgeons performing minimally invasive surgery: A systematic review. Surg Endosc. Feb. 2017;31(2):516-526. doi: 10.1007/s00464-016-5020-9. [DOI] [PubMed] [Google Scholar]
- 5.Schlussel AT, Maykel JA. Ergonomics and musculoskeletal health of the surgeon. Clin Colon Rectal Surg. Nov. 2019;32(6):424-434. doi: 10.1055/s-0039-1693026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.GPY S, Ho P, Ting ACW, Poon JTC, Cheng SWK, Tsang RCC. Work-related musculoskeletal symptoms in surgeons. J Occup Rehabil. 2009;19(2):175-184. doi: 10.1007/s10926-009-9176-1. [DOI] [PubMed] [Google Scholar]
- 7.Janki S, Mulder EEAP, Ijzermans JNM, Tran TCK. Ergonomics in the operating room. Surg Endosc. 2017;31(6):2457-2466. doi: 10.1007/s00464-016-5247-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Szeto GP, Cheng SW, Poon JT, Ting AC, Tsang RC, Ho P. Surgeons’ static posture and movement repetitions in open and laparoscopic surgery. J Surg Res. Jan. 2012;172(1):e19-e31. doi: 10.1016/j.jss.2011.08.004. [DOI] [PubMed] [Google Scholar]
- 9.Park A, Lee G, Seagull FJ, Meenaghan N, Dexter D. Patients benefit while surgeons suffer: An impending epidemic. J Am Coll Surg. Mar. 2010;210(3):306-313. doi: 10.1016/j.jamcollsurg.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 10.Alarcon A, Berguer R. A comparison of operating room crowding between open and laparoscopic operations. Surg Endosc. Sep. 1996;10(9):916-919. doi: 10.1007/bf00188483. [DOI] [PubMed] [Google Scholar]
- 11.Herron DM, Gagner M, Kenyon TL, Swanström LL. The minimally invasive surgical suite enters the 21st century. Surg Endosc. 2001;15(4):415-422. doi: 10.1007/s004640080134. [DOI] [PubMed] [Google Scholar]
- 12.Kenyon TA, Urbach DR, Speer JB, et al. Dedicated minimally invasive surgery suites increase operating room efficiency. Surg Endosc. Oct 2001;15(10):1140-1143. doi: 10.1007/s004640080092. [DOI] [PubMed] [Google Scholar]
- 13.Levy ML, Chen JC, Moffitt K, Corber Z, McComb JG. Stereoscopic head-mounted display incorporated into microsurgical procedures: Technical note. Neurosurgery. Aug 1998;43(2):392-395. doi: 10.1097/00006123-199808000-00141. [DOI] [PubMed] [Google Scholar]
- 14.Geis WP. Head-mounted video monitor for global visual access in mini-invasive surgery. An initial report. Surg Endosc. Jul. 1996;10(7):768-770. doi: 10.1007/BF00193055. [DOI] [PubMed] [Google Scholar]
- 15.van Lindert EJ, Grotenhuis JA, Beems T. The use of a head-mounted display for visualization in neuroendoscopy. Comput Aided Surg. 2004;9(6):251-256. doi: 10.3109/10929080500165476. [DOI] [PubMed] [Google Scholar]
- 16.Matsukawa K, Yato Y. Smart glasses display device for fluoroscopically guided minimally invasive spinal instrumentation surgery: A preliminary study. J Neurosurg Spine. Oct 2020;34:1-6. doi: 10.3171/2020.6.Spine20644. [DOI] [PubMed] [Google Scholar]
- 17.Liu X, Sun J, Zheng M, Cui X. Application of mixed reality using optical see-through head-Mounted displays in transforaminal percutaneous endoscopic lumbar discectomy. BioMed Res Int. 2021;2021:9717184. doi: 10.1155/2021/9717184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kim CH, Ryu SY, Yoon JY, et al. See-through type 3D head-Mounted display-Based surgical microscope system for microsurgery: A feasibility study. JMIR Mhealth Uhealth. Mar 2019;7(3):e11251. doi: 10.2196/11251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rahman R, Wood ME, Qian L, Price CL, Johnson AA, Osgood GM. Head-mounted display use in surgery: A systematic review. Surg Innovat. 2020;27(1):88-100. doi: 10.1177/1553350619871787. [DOI] [PubMed] [Google Scholar]
- 20.Johnson AA, Reidler JS, Speier W, Fuerst B, Wang J, Osgood GM. Visualization of fluoroscopic imaging in orthopedic surgery: Head-mounted display vs conventional monitor. Surg Innovat. 2021;29:1553350620987978. doi: 10.1177/1553350620987978. [DOI] [PubMed] [Google Scholar]
- 21.Moshtaghi O, Kelley KS, Armstrong WB, Ghavami Y, Gu J, Djalilian HR. Using google glass to solve communication and surgical education challenges in the operating room. Laryngoscope. Oct 2015;125(10):2295-2297. doi: 10.1002/lary.25249. [DOI] [PubMed] [Google Scholar]
- 22.Nakhla J, Kobets A, De la Garza Ramos R, et al. Use of google glass to enhance surgical education of neurosurgery residents: “Proof-of-concept” study. World Neurosurg. Feb. 2017;98:711-714. doi: 10.1016/j.wneu.2016.11.122. [DOI] [PubMed] [Google Scholar]
- 23.Brewer ZE, Fann HC, Ogden WD, Burdon TA, Sheikh AY. Inheriting the learner’s view: A google glass-based wearable computing platform for improving surgical trainee performance. J Surg Educ. 2016;73(4):682-688. doi: 10.1016/j.jsurg.2016.02.005 10.1016/j.jsurg.2016.02.005. [DOI] [PubMed] [Google Scholar]
- 24.Chimenti PC, Mitten DJ. Google glass as an alternative to standard fluoroscopic visualization for percutaneous fixation of hand fractures: A pilot study. Plast Reconstr Surg. Aug. 2015;136(2):328-330. doi: 10.1097/prs.0000000000001453. [DOI] [PubMed] [Google Scholar]
- 25.Yoon JW, Chen RE, Han PK, Si P, Freeman WD, Pirris SM. Technical feasibility and safety of an intraoperative head-up display device during spine instrumentation. Int J Med Robot. Sep 2017;13(3). doi: 10.1002/rcs.1770. [DOI] [PubMed] [Google Scholar]
- 26.Chen F, Cui X, Han B, Liu J, Zhang X, Liao H. Augmented reality navigation for minimally invasive knee surgery using enhanced arthroscopy. Comput Methods Progr Biomed. Apr 2021;201:105952. doi: 10.1016/j.cmpb.2021.105952. [DOI] [PubMed] [Google Scholar]