Abstract
Background
In suspected community-acquired pneumonia (CAP), chest CT is superior to the routinely obtained radiographs (CXR), but administers higher radiation doses. However, ultra-low-dose CT (ULDCT) has shown promising results.
Purpose
To compare radiation dose and image quality using standard and ULDCT protocols designed for a multicenter study encompassing three CT scanner models from GE, Canon, and Siemens.
Material and methods
Patients with suspected CAP were referred for non-contrast standard dose chest CT (NCCT) and ULDCT. Effective radiation dose and Contrast-to-Noise Ratio (CNR) was calculated.
Results
Mean effective doses were GE (n = 10) 6.93 mSv in NCCT and 0.27 mSv in ULDCT; Canon (n = 9) 3.48 in mSv NCCT and 1.11 mSv in ULDCT; Siemens (n = 10) 2.85 mSv in NCCT and 0.45 mSv in ULDCT. CNR was reduced by 29–39% in ULDCT.
Conclusion
The proposed CT protocols yielded dose reductions of 96%, 68%, and 84% using a GE, Canon, and Siemens scanner, respectively.
Keywords: Thorax, computed tomography, lung, equipment, infection, acute
Introduction
Community-acquired pneumonia (CAP) is one of the most common acute infections, 1 and in the emergency setting prompt point-of-care diagnosis using non-invasive tools such as radiographs (CXR) or computed tomography (CT) may impact patient management. 2 While chest CT is superior to the routinely obtained CXR regarding sensitivity, 3 CT administers higher radiation doses. 4 However, ultra-low-dose CT (ULDCT) with radiation doses similar to those of CXR has shown promising results.5–8
The purpose of this technical note was to compare radiation dose and technical image quality using a standard dose and an ultra-low-dose chest CT protocol designed for a prospective clinical multicenter study entitled ‘Improved diagnosis of infectious diseases in emergency departments’. 9
Methods
The project was approved by the Regional Committees on Health Research Ethics for Southern Denmark (Journal Number: S-20200188).
Four Danish emergency departments each equipped with either a GE Revolution CT scanner (GE Healthcare, Waukesha, US), a Canon Aquillion One scanner (Canon Medical Systems Corporation, Otawara Tochigi, Japan) or a Siemens Somatom Edge scanner (Siemens Healthcare GmbH, Erlangen, Germany) were involved in the study. Prior to patient inclusion, an ultra-low-dose CT protocol was developed for each of the local scanners using a Lungman phantom (Kyoto Kagaku Co., Kyoto, Japan) for the GE and Siemens scanners and a CTU-41 Torso phantom (Kyoto Kagaku Co., Kyoto, Japan) for the Canon scanner. The radiation dose was reduced using the vendor-specific image quality metrics until a target effective dose of 0.25–0.5 mSv was reached. The resulting scan parameters are listed in Table 1.
Table 1.
Acquisition and image reconstruction parameters for non-contrast CT (NCCT) and ultra-low-dose CT (ULDCT) scan protocols. *) SN100: Physical Tin filter **) ASIR-V: Adaptive Statistical Iterative Reconstruction, AIDR-3D: Adaptive Iterative Dose Reduction, ADMIRE: Advanced Modelled Iterative Reconstruction.
| Scanner | GE revolution CT | Canon ACQUILLION One | Siemens somatom edge | |||
|---|---|---|---|---|---|---|
| Scan mode | NCCT | ULDCT | NCCT | ULDCT | NCCT | ULDCT |
| Tube voltage | 100 kV | 100 kV | 100 kV | 100 kV | 100 kVp | 100 kVp SN100* |
| Image quality metric | Noise Index 22 | Noise Index 85 | N/A | SD 35 | Quality ref mAs 100 | Quality ref mAs 160 |
| Scan time | 0.5 s | 0.5 s | 0.35 s | 0.35 s | 0.5 s | 0.5 s |
| Pitch | 0.5 | 0.5 | 1.388 | 1.388 | 1.2 | 1.2 |
| Collimation | 128 × 0.625 mm | 128 × 0.625 mm | 80 × 0.5 mm | 80 × 0.5 mm | 128 × 0.6 mm | 128 × 0.6 mm |
| Kernel | Lung, mediastinum | Lung, mediastinum | Lung, mediastinum | Lung, mediastinum | BL57, BR38 | BL57, BR38 |
| Image reconstruction mode** | ASIR-V 40% | ASIR-V 50% | AIDR-3D enhanced | AIDR-3D enhanced | ADMIRE 3 | ADMIRE 4 |
| Slice thickness | 1.25/2.5 mm | 1.25/2.5 mm | 3 mm | 3 mm | 3 mm | 3 mm |
| Recon increment | 0.5/2.0 mm | 0.5/2.0 mm | 2.4 mm | 2.4 mm | 3 mm | 3 mm |
| Multiplanar reformat | Coronal/sagittal 2.5 mm |
Coronal/sagittal 2.5 mm |
Coronal/sagittal 3 mm |
Coronal/sagittal 3 mm |
Coronal/sagittal 3 mm |
Coronal/sagittal 3 mm |
Adult patients with suspected pneumonia admitted to emergency examination were invited to participate in the study except if participation would delay life-saving treatment, in case of pregnancy or if the patient had confirmed COVID-19 or recent admission to hospital (<14 days) to exclude patients with nosocomial infections. Further exclusion criteria can be found in a previous publication. 9 Patients who consented were referred for non-contrast chest CT (NCCT) using the local clinical chest CT protocol followed by an ULDCT. The scans were performed in the same sequence. A chest radiologist with 12 years of experience who was not employed at one of the participating sites confirmed that image quality was diagnostically acceptable in the first two patients included from each site.
Image analysis
Dose length product (DLP) was recorded from the scanner dose report for NCCT and ULDCT, respectively, and converted to estimated effective radiation doses using a chest specific conversion factor of 0.017 according to Huda et al. 10 Attenuation (HU) and noise (SD) was measured in an axial image using circular ROIs in the pulmonary trunk and adjacent lung tissue at the level of the carina (Figure 1) and Contrast-to-Noise Ratio (CNR) was calculated using the formula
Figure 1.
Standard dose CT image with circular ROIs positioned in the pulmonary trunk and adjacent lung tissue. Slice thickness = 2.5 mm, WW/WL 1500/−500 HU.
Statistical analysis
After testing for normal distribution using the Shapiro–Wilk test, data were summarized by mean, standard deviation (SD), and number of observations. Differences between variables were analysed using paired t-test. A p-value ≤ 0.05 was considered statistically significant.
All analyses were performed using STATA/BE 17.0 (StataCorp. LP, College Station, TX 77845 USA).
Results
Ten consecutive patients were included from each site except one site, where inclusion was difficult because of local logistic issues. Therefore, only 9 patients were included before the site decided to exit study. One of the sites with a GE scanner encountered a technical error that prevented radiation dose data from being transferred to the picture archival and communication system (PACS). Therefore, this site was excluded from analysis. Consequently, 29 patients (18 male/11 female) were included (mean age 73.9 years, SD 11.6).
Radiation dose
The mean effective doses in the patients scanned using a GE scanner was 6.93 mSv in NCCT and 0.27 mSv in ULDCT (n = 10). For the Canon scanner, mean effective doses in NCCT and ULDCT were 3.48 mSv and 1.11 mSv, respectively (n = 9). The corresponding values for the Siemens scanner were 2.85 mSv and 0.45 mSv (n = 10). Dose-length products for NCCT and ULDCT protocols are listed in Table 2.
Table 2.
Scan length, dose-length product (DLP), Contrast-to-Noise Ratio (CNR), standard deviation (SD), p-value and 95% confidence interval (95% CI) in standard chest CT protocols versus ultra-low-dose (ULD) protocols.
| Scanner | Protocol | Scan length (SD) | DLP (SD) | CNR (SD) |
|---|---|---|---|---|
| GE revolution CT n = 10 | Standard | 31.42 cm (2.4) | 407.7 mGy*cm (218.5) | 76.5 (18.8) |
| ULD | Do. | 15.9 mGy*cm (1.0) | 50.4 (18.2) | |
| p-value | 0.0003 | 0.0002 | ||
| 95% CI | 235.9–547.8 | 16.4–35.9 | ||
| Canon acquillion one N = 9 |
Standard | 32.84 cm (2.2) | 204.7 mGy*cm (22.0) | 53.0 (8.6) |
| ULD | Do. | 65.4 mGy*cm (16.5) | 32.2 (3.9) | |
| p-value | <0.0001 | <0.0001 | ||
| 95% CI | 123.6–155.0 | 15.4–26.1 | ||
| Siemens Somatom Edge n = 10 | Standard | 31.52 cm (4.6) | 167.4 mGy*cm (60.1) | 80.8 (19.6) |
| ULD | Do. | 26.7 mGy*cm (9.0) | 57.6 (10.1) | |
| p-value | <0.0001 | 0.002 | ||
| 95% CI | 101.3–180.1 | 11.3–35.1 |
Image quality
The mean noise for NCCT as measured in the in the pulmonary trunk was 16.2 HU (SD = 2.5) in Canon, 11.6 HU (SD = 1.6) in GE and 11.1 HU (SD = 2.0) in Siemens with no statistically significant difference between GE and Siemens (p = .56). Example images are shown in Figures 2–4. The noise in the scans performed using the Canon scanner was significantly different both between GE and Siemens scanners (p = .0001). Contrast-to-Noise ratios in ULDCT were 33%, 39%, and 29% lower than that of NCCT for GE, Canon, and Siemens, respectively (Table 2).
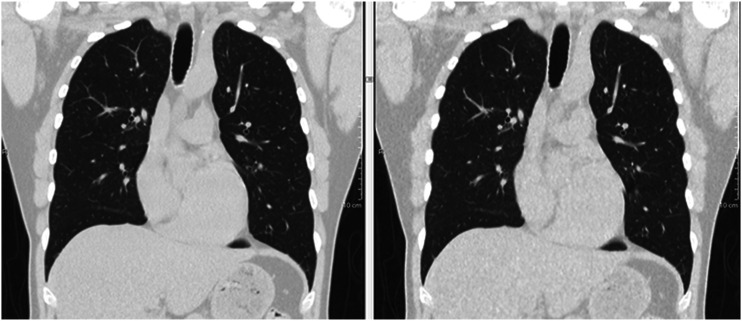
Figure 3.
Coronal 2.5 mm reformatted chest CT in a 53-year-old male using Canon Aquillion One. Left: DLP = 175.5 mGy*cm, CTDIvol = 5.0 mGy. Right: DLP = 31.69 mGy*cm, CTDIvol = 0.9 mGy.
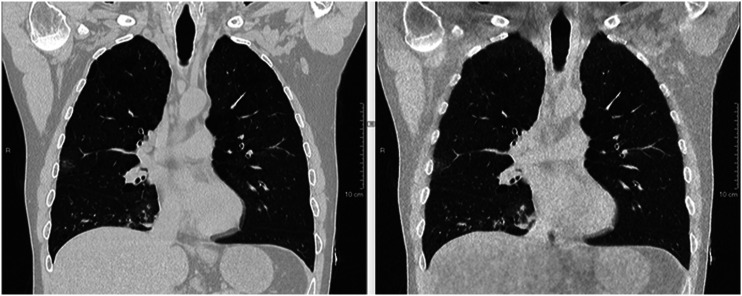
Figure 2.
Coronal 2.5 mm reformatted chest CT in a 51-year-old male using GE Revolution CT. Left: DLP = 482.18 mGy*cm, CTDIvol = 11.24 mGy. Right: DLP = 17.64 mGy*cm, CTDIvol = 0.41 mGy.
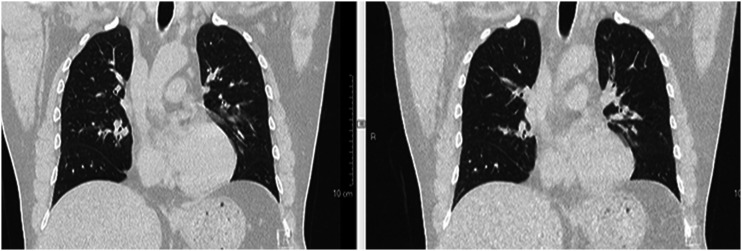
Figure 4.
Coronal 2.5 mm reformatted chest CT in a 48-year-old male using Siemens Somatom Edge. Left: DLP = 174.2 mGy*cm, CTDIvol = 5.82 mGy. Right: DLP = 27.0 mGy*cm, CTDIvol = 0.89 mGy.
Discussion
In this small-scale prospective clinical test, we proposed ultra-low-dose chest CT protocols for three scanners. When using phantoms, all scanners demonstrated sub-millisievert scans. However, in the clinical setting the protocol developed for the Canon scanner did not reach the desired mean effective dose of 0.25–0.5 mSv. Furthermore, both radiation dose and noise were higher than that of the other more up-to-date scanners with more efficient detectors. The result might be explained by the use of a different phantom when developing the scan protocol. Furthermore, only 9 patients were included, while 10 are recommended for comparison to diagnostic reference levels.
In the department with a GE scanner, the standard chest CT protocol administered a rather high dose and large variation in doses compared to the other departments’ routine protocols (Table 2). Supposedly, this finding may be caused by local image quality preferences or automatic tube current modulation settings and will be discussed locally. Consequently, the dose reduction potential was larger with the GE scanner and furthermore, the obtained ultra-low-dose DLP was lower than that of the other scanners. In addition, the standard deviation of the DLP in ULDCT as listed in Table 2 was very low (SD = 1.0). This indicates that the automatic tube current modulation in most patients used the lowest possible mA, that is, 10 mA. The effective dose of 0.27 mSv was obtained using 100 kVp while previously; Blinded for anonymity et al. 5 acquired ULD chest CT images at a mean effective dose of 0.05 mSv using 80 kVp in an identical GE scanner. However, those images were largely deemed ‘suboptimal’ in a visual image quality evaluation. Therefore, the dose obtained in the current study might be a good trade-off between radiation dose and image quality, as the first images were deemed diagnostically acceptable by a chest radiologist. However, as diagnostic image quality was not systematically assessed in the current study further research is needed before such implementation can commence.
Greffier et al. 7 acquired ULD chest CT images using an identical Siemens scanner and achieved approximately half the dose compared to that achieved in the current study. They maintained excellent or good image quality suggesting that radiation dose might be further reduced in the proposed scan protocol for Siemens.
In conclusion, the chest CT examination protocols proposed in this study yielded dose reductions of 96%, 68%, and 84% using a GE, Canon, and Siemens scanner, respectively, and may serve as benchmarks or starting points for protocol development using similar equipment. Future studies including clinical evaluation are needed to explore this subject further before similar protocols are implemented clinically.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Bo Mussmann https://orcid.org/0000-0003-2119-5129
Ole Graumann https://orcid.org/0000-0002-9663-8361
Janni Jensen https://orcid.org/0000-0001-7036-6129
References
- 1.Bjarnason A, Westin J, Lindh M, et al. Incidence, etiology, and outcomes of community-acquired pneumonia: a population-based study. Open Forum Infect Dis 2018; 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Washington L, O'Sullivan-Murphy B, Christensen JD, et al. Radiographic imaging of community-acquired pneumonia: a case-based review. Radiol Clin North Am 2022; 60: 371–381. [DOI] [PubMed] [Google Scholar]
- 3.Debray MP, Carette MF, Loubet P, et al. CT features of community-acquired pneumonia at the emergency department. Respir Med Res 2022; 81: 100892. [DOI] [PubMed] [Google Scholar]
- 4.Carey S, Kandel S, Farrell C, et al. Comparison of conventional chest x ray with a novel projection technique for ultra-low dose CT. Med Phys 2021; 48: 2809–2815. [DOI] [PubMed] [Google Scholar]
- 5.Blinded for anonymity . Diagnostic accuracy of ultra-low-dose chest computed tomography in an emergency department. Acta Radiol 2021; 63. [DOI] [PubMed] [Google Scholar]
- 6.Macri F, Greffier J, Pereira F, et al. Value of ultra-low-dose chest CT with iterative reconstruction for selected emergency room patients with acute dyspnea. Eur J Radiol 2016; 85: 1637–1644. [DOI] [PubMed] [Google Scholar]
- 7.Greffier J, Hoballah A, Sadate A, et al. Ultra-low-dose chest CT performance for the detection of viral pneumonia patterns during the COVID-19 outbreak period: a monocentric experience. Quant Imaging Med Surg 2021; 11: 3190–3199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kroft LJM, van der Velden L, Girón IH, et al. Added value of ultra-low-dose computed tomography, dose equivalent to chest X-ray radiography, for diagnosing chest pathology. J Thorac Imaging 2019; 34: 179–186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Blinded for anonymity . Improved diagnostics of infectious diseases in emergency departments: a protocol of a multifaceted multicentre diagnostic study. BMJ Open 2021; 11: e049606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huda W, Ogden KM, Khorasani MR. Converting dose-length product to effective dose at CT. Radiology 2008; 248: 995–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]