Abstract
Background:
Trends between the sexes have been reported regarding prevalence, patient-reported outcomes (PROs), and complications of hip arthroscopy (HA) for femoroacetabular impingement syndrome (FAIS), yet current results lack consensus.
Purpose:
To evaluate sex-based differences after HA for FAIS in (1) prevalence of cam and pincer morphology in FAIS and (2) PROs, pain scores, and postoperative complication rates.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
The EMBASE, PubMed, and Ovid (MEDLINE) databases were searched from establishment to February 28, 2022, according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. Included studies had sex-based data on prevalence, outcomes, and complications of HA for FAIS. Reviews and commentaries were excluded. Data were combined, and between-sex differences were analyzed. Meta-analyses using random-effects models were performed when possible. Pooled risk ratios (RRs) and standardized mean differences were calculated.
Results:
A total of 74 studies were included (213,059 patients; 132,973 female hips [62.4%] and 80,086 male hips [37.6%]). The mean age was 30.7 ± 7.7 years among male patients and 31.1 ± 7.8 years among female patients. Male patients experienced mixed-type impingement significantly more often (39.4% vs 27.2% for female patients; RR = 0.69 [95% confidence interval [CI], 0.58-0.81]; P < .001), whereas female patients experienced pincer-type impingement more often (50.6% vs 30.8% for male patients; RR = 2.35 [95% CI, 1.14-4.86]; P = .02). Male patients had higher likelihoods of undergoing femoroplasty (89.8% vs 77.4% for female patients; RR = 0.90 [95% CI, 0.83-0.97]; P = .006), acetabuloplasty (67.1% vs 59.3% for female patients; RR = 0.87 [95% CI, 0.79-0.97]; P = .01), or combined femoroplasty/acetabuloplasty (29.2% vs 14.5% for female patients; RR = 0.63 [95% CI, 0.44-0.90]; P = .01). Although female patients showed greater improvements in Hip Outcome Score–Sport-Specific subscale (P = .005), modified Harris Hip Score (P = .006), and visual analog scale pain (P < .001), both sexes surpassed the minimal clinically important difference at 1, 2, and 5 years postoperatively. Female patients had higher complication rates (P = .003), although no sex-based differences were found in total hip arthroplasty conversion rates (P = .21).
Conclusion:
Male patients undergoing HA for FAIS had a higher prevalence of mixed-type FAIS while female patients had more pincer-type FAIS. Female patients gained greater improvements in PROs, although both sexes exceeded the minimal clinically important difference, suggesting that both male and female patients can benefit from HA.
Keywords: femoroacetabular impingement, sex, hip arthroscopy, labral tear
Femoroacetabular impingement syndrome (FAIS), which results from abnormal contact between the acetabular rim and femoral head-neck junction, causing morphological changes that create an aspherical joint, is a leading cause of hip pain in young adults. 5,18,27 Three basic subtypes have been established in the literature with varying hip morphology that leads to impingement: cam-, pincer-, and mixed-type FAIS.
Hip arthroscopy (HA) has been established as an effective procedure that improves patient-reported outcomes (PROs) in the treatment of FAIS, with impingement and labral tears being the leading indications. 11,14,59 Studies suggest that nonmodifiable factors, such as age and sex, impact outcomes of HA; however, there is conflicting evidence as to whether sex differences exist and the magnitude of those differences. Salvo et al 77 reported a significant difference in preoperative hip function, morphology, and self-reported functional deficits between male and female patients. Beck et al 3 found that female patients achieved postoperative improvements on certain PROs at higher rates than male patients after HA for FAIS, whereas Cvetanovich et al 16 found that male and female patients achieved similar improvements on PROs and low complication rates. Some studies have found sex-based differences in HA rates regardless of FAIS diagnosis, 8 whereas others have reported no such differences. 62
The aim of this systematic review was to compare sex-based differences in the prevalence of cam and pincer morphology in FAIS, and to evaluate such differences in PROs, pain scores, and postoperative complication rates after HA for treatment of FAIS. The hypothesis was that, whereas male patients may more frequently undergo HA for cam-type FAIS and female patients for pincer-type, similar improvements in PROs and no difference in complication rates would be expected between sexes.
Methods
Search Strategy
Three online databases (Embase, PubMed, and Ovid [MEDLINE]) were searched from database inception until February 28, 2022, for studies investigating patient-reported or sex-specific outcomes after HA for FAIS. Search terms included “hip arthroscopy,” “femoroacetabular impingement,” “labrum tear,” “labral tear,” “gender,” “sex,” “male,” and “female,” and were limited to English and human studies (Appendix Table A1).
Of note, a distinction between gender and sex was not incorporated into the reviewed studies. Results were analyzed as a dichotomous assigned-male-at-birth versus assigned-female-at-birth comparison due to the literature suggesting that sex-based differences in FAIS are due to anatomic differences in hip joint and pelvic anatomy, including females having smaller alpha angles and increased acetabular and femoral anteversion. 34
Study Screening
Two reviewers (H.A. and M.O.) screened titles, abstracts, and full-text articles independently and in duplicate in accordance with PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. A third reviewer (M.H.) reconciled any discrepancies. References of included articles were searched manually to identify studies that may have eluded the initial search, from which 1 article was identified and included in the analysis. 55 The interreviewer agreement for the title, abstract, and full-text screenings was assessed using the kappa (κ) statistic.
Assessment of Study Eligibility
The research question and criteria for study inclusion were established a priori. Inclusion criteria were as follows: English-language studies, human studies, studies with sex-specific data, and studies investigating HA or FAIS prevalence, outcomes, or complications. Exclusion criteria were review articles, commentaries, case reports or studies with a sample size of n = 1, and studies that lacked strong sex-specific data (either direct sex comparisons or sample sizes large enough where sex data could be extracted for comparison).
Data Abstraction
A single reviewer collected and recorded data via Microsoft Excel (Version 16.59). Abstracted data included study year and type, Methodological Index for Non-Randomized Studies (MINORS) score, number of male and female hips, male and female mean ages, time of follow-up measurements, sex-specific outcomes for each reported PRO, and complication types and rates.
Quality Assessment
MINORS criteria were utilized to assess the methodological quality of included studies. MINORS is an instrument used to assess the quality of both comparative and noncomparative, nonrandomized surgical studies. 83 Noncomparative studies are scored out of 16, while comparative studies are scored out of 24. The screening process did not yield any randomized control trials; therefore, MINORS was the sole quality assessment tool used.
Outcome Measures
To assess for potential sex differences in prevalence, outcomes, and complications of HA for FAIS, demographic data were analyzed to determine the number of male and female hips undergoing HA, HA for FAIS, HA for a cam diagnosis, HA for a pincer diagnosis, HA for a mixed cam/pincer diagnosis, femoroplasty, acetabuloplasty, and combined femoroplasty/acetabuloplasty.
With respect to the standardized mean differences (SMDs) between male and female patients, 5 validated PROs were analyzed: modified Harris Hip Score (mHHS), Hip Outcome Score–Activities of Daily Living subscale (HOS-ADL), Hip Outcome Score–Sport-Specific subscale (HOS-SS), International Hip Outcome Tool-12, 29 and visual analog scale (VAS) for pain. 1,32,38,58
When evaluating complication rates, the following postoperative conditions were considered: deep venous thrombosis, pulmonary embolism, venous thromboembolism, persistent paresthesia, weakness of function or muscle strength, other undefined nerve injury, heterotopic ossification, emergency department or hospital admission, chondral injury, revision arthroscopy, or failure to return to the same level of sport.
Statistical Analysis
A meta-analysis was performed to compare several different diagnostic and outcome metrics between male and female cohorts: (1) prevalence of FAIS, (2) type of hip pathology (cam, pincer, or mixed), (3) type of procedure (femoroplasty, acetabuloplasty, or combined femoroplasty/acetabuloplasty), (4) the overall complication rate, (5) the conversion to total hip arthroplasty (THA) rate, and (6) the mean improvement in various PROs (HOS-ADL, HOS-SS, mHHS, VAS).
For type of hip pathology, type of procedure, overall complication rate, and conversion to THA, risk ratios (RRs) for male versus female patients were calculated for each study that reported these data. A pooled RR, weighed by the sample size of each study, was then calculated. RRs <1 indicated favoring male patients and thus having a higher frequency among male patients, and RRs >1 indicated favoring female patients and thus having a higher frequency among female patients. RRs = 1 indicated no frequency difference between sexes.
For continuous variables (eg, the mean increase in PRO scores), the SMD of each outcome measure was compared between male and female patients for each study that reported these data. A pooled SMD, weighed by the sample size of each study, was then calculated.
Heterogeneity of the pooled data was quantified with the I 2 statistic. If I 2 ≤ 50%, the studies were assumed to be homogeneous, and a fixed-effects model was used. If I 2 > 50%, the studies were assumed to be heterogeneous, and a random-effects model was used. Statistical significance was defined as an α error less than 5.0% (ie, P < .05) for the overall effect size.
All meta-analyses were completed using the publicly available software Cochrane ReviewManager Version 5.4 (Cochrane Collaboration). All other statistical analyses were completed using SPSS Version 24.0 (IBM Corp).
Results
Search Strategy
The initial online database search resulted in 10,720 studies, with a total of 8,175 studies once duplicates were removed. The entire screening process resulted in 74 full-text articles being included for analysis (Figure 1). Interreviewer agreement was found to be 0.43 for the title screening (moderate agreement), 0.64 for the abstract screening (substantial agreement), and 0.36 for the full-text screening (moderate agreement).
Figure 1.

PRISMA flow diagram demonstrating the systematic screening of the literature for sex difference outcomes after HA for FAIS. FAI, femoroacetabular impingement; FAIS, femoroacetabular impingement syndrome; HA, hip arthroscopy; PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Study Quality
The 74 included studies consisted of 17 case series, § 6 case-control studies, 3,7,19,37,51 32 cohort studies, ‖ and 19 cross-sectional studies. ¶ A summary of the characteristics of each study is given in Appendix Table A2. The mean MINORS score for the noncomparative studies was 10.8 (range, 7-12), and the mean MINORS score for the comparative studies was 17 (range, 11-22). All studies had a clearly stated aim and endpoints appropriate for the aim. Moreover, 82.4% had an appropriate follow-up period, which was defined as “sufficiently long to allow the assessment of the main endpoint and possible adverse events.” 83 All remaining studies did not report a follow-up period, except one study where follow-up was reported but inadequate to assess for possible adverse events. A total of 75.7% of studies had a loss of follow-up less than 5%. Only 2.7% of studies had prospective collection of data, and 9.5% had unbiased assessment of endpoints. Of the comparative studies, 44.7% had adequate control groups, and 55.4% had baseline equivalence of groups with respect to criteria other than the endpoints in question.
Study Characteristics
A total of 236,604 patients were included across all studies, with sex data stratified in a portion of these and identifying 80,002 (37.6%) male patients and 132,962 (62.4%) female patients (Appendix Table A2). From studies where number of hips were recorded and stratified by sex, a total of 80,086 (37.6%) male hips and 132,973 (62.4%) female hips were identified. Mean age among male patients was 30.7 ± 7.7 years, and mean age among female patients was 31.1 ± 7.8 years. Follow-up time ranged from 7 days to 10 years, with 60.8% of studies having a minimum of 1-year follow-up. Studies with perioperative data were included as well. Heterogeneity related to follow-up time is included in the I 2 statistic.
Prevalence Data
Studies lacked consistency in reporting FAIS type when patients underwent HA; therefore, results are displayed only for those studies where specific FAIS types were identified.
Among studies where prevalence of cam impingement was recorded by sex, 61.5% (740/1204) of male hips had a diagnosis of cam-type FAIS, versus 41.6% (586/1410) of female hips (RR = 0.85 [95% CI, 0.69-1.04]; P = .11) (Appendix Figure A1). In studies where prevalence of pincer impingement was recorded by sex, 30.8% (376/1219) of male hips had a diagnosis of pincer-type FAIS, versus 50.6% (385/761) of female hips (RR = 2.35 [95% CI, 1.14-4.86], P = .02) (Appendix Figure A1). Among studies where prevalence of mixed-type impingement was recorded by sex, 39.4% (388/984) of male hips had a diagnosis of mixed-type FAIS, versus 27.2% (330/1214) of female hips (RR = 0.69 [95% CI, 0.58-0.81], P < .001) (Appendix Figure A1).
In studies where prevalence of femoroplasty was recorded by sex, 89.8% (1456/1621) of male hips underwent femoroplasty for FAIS, versus 77.4% (1926/2490) of female hips (RR = 0.90 [95% CI, 0.83-0.97], P = .006) (Appendix Figure A2). Among studies where prevalence of acetabuloplasty was recorded by sex, 67.1% (1051/1566) of male hips underwent acetabuloplasty for FAIS, versus 59.3% (1436/2423) of female hips (RR = 0.87 [95% CI, 0.79-0.97], P = .01) (Appendix Figure A2). In studies where prevalence of combined femoroplasty/acetabuloplasty was recorded by sex, 29.2% (119/407) of male hips underwent combined femoroplasty/acetabuloplasty for FAIS, versus 14.5% (56/386) of female hips (RR = 0.63 [95% CI, 0.44-0.90], P = .01) (Appendix Figure A2).
PRO Measures
HOS-ADL
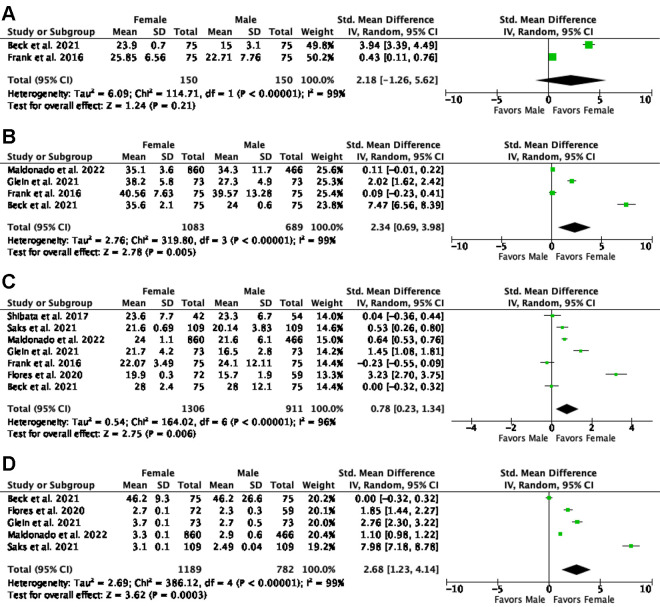
Seven studies 3,14,23,34,52,68,77 reported HOS-ADL scores, totaling 1054 male hips and 1443 female hips. Among these studies, the average HOS-ADL score after HA for FAIS for male patients was 79.4, and for female patients was 77.8. Two studies provided sufficient data to compare pre- and postoperative HOS-ADL scores for both male and female patients, 3,23 with the average increase in HOS-ADL scores being 17.7 for male and 24.4 for female patients (SMD = 2.18 [95% CI, -1.26 to 5.62], P = .21, I 2 = 99%) (Appendix Figure A3 and Table A3).
HOS-SS
Nine studies reported HOS-SS scores, # totaling 1593 male hips and 2376 female hips. Among these studies, the average HOS-SS score for male patients was 68.6, and that for female patients was 64.8. Four studies reported pre- and postoperative HOS-SS scores for both male and female patients, 3,23,28,55 with the average increase in HOS-SS scores being 32.9 for male patients and 34.8 for female patients (SMD = 2.34 [95% CI, 0.69-3.98], P = .005, I 2 = 99%) (Appendix Figure A3 and Table A3).
mHHS
A total of 18 studies reported mHHS scores, totaling 2041 male hips and 2724 female hips. ** Among these studies, the average mHHS score for male patients was 81.8, and that for female patients was 77.8. Seven studies 3,22,23,28,55,76,81 reported pre- and postoperative mHHS scores for both male and female patients, with the average increase in mHHS scores being 22.2 for male and 23.2 for female patients (SMD = 0.78 [95% CI, 0.23-1.34], P = .006, I 2 = 96%) (Appendix Figure A3 and Table A3).
VAS Pain
Nine studies reported VAS pain scores, †† totaling 1619 male hips and 2375 female hips. Among these studies, the average preoperative VAS pain score for male patients was 16.4, and for female patients was 19.9. Five studies 3,22,28,55,76 reported pre- and postoperative VAS pain scores for both male and female patients, with the average decrease in VAS pain scores being 8.66 for males and 10.51 for females (SMD = 2.68 [95% CI, 1.23-4.14], P < .001, I 2 = 99%) (Appendix Figure A3 and Table A3).
Complications
A total of 14 studies reported data with respect to postoperative complications of HA for FAIS, ‡‡ with a total of 24,912 male hips and 41,760 female hips included in the studies where postoperative complications were recorded. Time of follow-up for evaluating complications ranged from 2 days to 2 years postoperatively. Recorded complications were heterogeneous across studies but included the following: deep venous thrombosis, pulmonary embolism, venous thromboembolism, paresthesia, weakness of function or muscle strength, other undefined nerve injury, heterotopic ossification, emergency department visit, hospital readmission, chondral injury, revision arthroscopy, or failure to return to the same level of sport. Ten studies reported overall postoperative complication rates for both male and female patients, §§ with the average complication rate for male patients being 3.4% (845/24,840) and for female patients 5.3% (2228/41,710) (RR = 2.34 [95% CI, 1.33-4.10], P = .003, I 2 = 88%) (Table 1 and Appendix Figure A4).
Table 1.
Complication Rates After HA for FAIS According to Sex a
| Lead Author (Year) | Follow-up | Complication Rate, Male/Female |
|---|---|---|
| Byrd (2000) 10 | 2 y | 5.6%/NR |
| Shibata (2017) 81 | 1 y |
|
| Khazi (2019) 41 | 30 days, 90 days |
PE: 0.13%/0.17% VTE: 0.34%/0.43%
PE: 0.02%/0.23% VTE: 0.52%/0.62% |
| Kern (2018) 40 | 2 days | Nerve injury: 13.5%/12.7% |
| Ellenrieder (2017) 21 | 12 weeks | Paraesthesia, muscle weakness, foot numbness: 86.7%/84.2% |
| Bedi (2012) 6 | 10 days | Heterotopic ossification: 72.4%/27.6% |
| Poehling-Monaghan (2017) 71 | 1 y |
|
| Cevallos (2021) 12 | 30 days, 2 y |
|
| Larson (2016) 45 | 6 mo | 6.7%/10% |
| Maldonado (2022) 55 | 2 y | Rate of non-THA revision surgery: 7.9%/11.3% |
| Amenabar (2013) 2 | Retirement due to hip disability: 3.8%/NR | |
| Philippon (2010) 70 | 1 y | Reinjured, required additional HA: 7.1%/NR |
| Nwachukwu (2017) 68 | 1 y | Reoperation rate: NR/9.09% |
| Chandrasekaran (2017) 14 | 2 y | 0%/5.56% |
a DVT, deep vein thrombosis; ED, emergency department; FAIS, femoroacetabular impingement syndrome; HA, hip arthroplasty; NR, not reported; PE, pulmonary embolism; RTS, return to sport; THA, total hip arthroplasty; VTE, venous thromboembolism.
Seven studies 8,12,22,53,55,60,76 reported THA conversion data after HA for FAIS, totaling 42,768 male hips and 75,753 female hips. Time of follow-up for evaluating THA conversion ranged from 1 to 10 years postoperatively. All 7 studies reported THA conversion rates for both male and female patients, with average rates being 5.2% (2232/42,768) for male patients and 4.9% (3727/75,753) for female patients (RR = 0.87 [95% CI, 0.71-1.08], P = .21, I 2 = 83%) (Appendix Table A4).
Both men and women achieved score improvements for HOS-SS and mHHS far above those needed to confirm a minimal clinically important difference (MCID) at 1, 2, and 5 years postoperatively (Table 2).
Table 2.
Rates of Achieving MCID and PASS Thresholds According to Sex a
| MCID | PASS | |||||
|---|---|---|---|---|---|---|
| PRO by Lead Author (Year) [Mean Follow-up] | Threshold | Male Patients Achieving Threshold | Female Patients Achieving Threshold | Threshold | Male Patients Achieving Threshold | Female Patients Achieving Threshold |
| Beck (2021) 3 [5-y follow-up] | ||||||
| HOS-ADL | 10.6 | 53.8% | 67.1% | 87.5% | 64.0% | 66.7% |
| HOS-SS | 15.4 | 48.3% | 72.4% | 76.6% | 56.5% | 70.3% |
| mHHS | 14.4 | 54.0% | 75.4% | 82.0% | 55.6% | 66.2% |
| Flores (2020) 22 [2-y follow-up] | ||||||
| mHHS | 8 | 61.4% | 70.8% | NR | NR | NR |
| HOOS-Symptoms | 9 | 69.5% | 68.1% | NR | NR | NR |
| HOOS-Pain | 9 | 62.7% | 70.8% | NR | NR | NR |
| HOOS-ADL | 6 | 62.7% | 79.2% | NR | NR | NR |
| HOOS-Sports | 10 | 74.1% | 86.1% | NR | NR | NR |
| HOOS-QoL | 11 | 82.8% | 88.9% | NR | NR | NR |
| Saks (2021) 76 [2-y follow-up] | ||||||
| mHHS | M: 8.2; F: 6.6 | 79.4% | 83.2% | 74 | 81.4% | 81.1% |
| NAHS | M: 8.9; F: 8.8 | 71.6% | 85.3% | NR | NR | NR |
| Glein (2021) 28 [2-y follow-up] | ||||||
| mHHS | 6.9 | 72.9% | 79.1% | 74 | 84.3% | 79.1% |
| NAHS | 9.0 | 62.9% | 79.1% | NR | NR | NR |
| HOS-SS | 10.9 | 70.0% | 85.1% | 75 | 82.9% | 82.1% |
| Domb (2021) 19 [2-y follow-up] | ||||||
| mHHS | NR | 77.2% | 81.0% | NR | NR | NR |
| NAHS | NR | 77.0% | 80.7% | NR | NR | NR |
| HOS-SS | NR | 69.2% | 70.5% | NR | NR | NR |
| VAS | NR | 71.7% | 76.2% | NR | NR | NR |
| Nwachukwu (2017) 68 [1-y follow-up] | ||||||
| mHHS | 8.2 | NR | 78.8% | NR | NR | NR |
| HOS-ADL | 8.3 | NR | 78.8% | NR | NR | NR |
| HOS-SS | 14.5 | NR | 75.8% | NR | NR | NR |
| iHOT-33 | 12.1 | NR | 66.7% | NR | NR | NR |
| Maerz (2021) 53 [1-y follow-up] | ||||||
| mHHS | 8 | 76.1% | 82.5% | 74 | 73.8% | 60.6% |
| Ramos (2020) 72 [0.4-y follow-up] | ||||||
| mHHS | 8 | 100.0% | NR | NR | NR | NR |
a ADL, activities of daily living; F, female; HOOS, Hip disability and Osteoarthritis Outcome Score; HOS, Hip Outcome Score; iHOT-33, International Hip Outcome Tool–33; M, male; MCID, minimal clinically important difference; mHHS, modified Harris Hip Score; NAHS, Nonarthritic Hip Score; NR, not reported; PASS, Patient Acceptable Symptom State; PRO, patient-reported outcome; QoL, quality of life; SS, sport-specific; VAS, visual analog scale.
Discussion
The findings of this review suggest that sex differences exist for FAIS morphologies, with male patients having a significantly higher prevalence of mixed-type FAIS (39.4% [388/984] of male patients, 27.2% [330/1214] of female patients; RR = 0.69 [95% CI, 0.58-0.81]; P < .001) and female patients of pincer-type FAIS (50.6% [385/761] of female patients, 30.8% of male patients [376/1219]; RR = 2.35 [95% CI, 1.14-4.86]; P = .02). This prevalence difference was identified among a smaller subset of the initial 236,604 hip cohort due to inconsistency in reporting sex-specific FAIS diagnoses and HA outcomes, highlighting the larger issue of poor reporting after HA for FAIS.
The significantly higher prevalence of mixed cam/pincer impingement among male patients and pincer impingement among female patients reflected clinical expectations and previously reported trends. 26,46 While sex differences were found for mixed-type and pincer-type FAIS, no significant difference was found for the prevalence of cam-type FAIS. The lack of studies reporting cam incidence by sex limited the cohort to a smaller size, which was made up largely of patients from the study by Salvo et al. 77 Therefore, cam prevalence reported here may be less representative of population trends and more reflective of the few studies dominating sex-stratified cam results. However, Laurito et al 46 did find a similar result for cam prevalence, with a higher male prevalence of cam among a cohort of 230 patients with FAIS undergoing HA. Ganz et al 26 stated that cam-type impingement was more common among young men, but that most hips overall showed a mixed-type impingement. Given that the concept of mixed-type impingement as a diagnosis developed after the diagnoses of isolated cam and isolated pincer impingement, it is possible that male patients experience cam impingement more often than female patients, but that they concurrently experience pincer impingement and thus are categorized as having mixed-type FAIS. This reconciles with the results of the present study that men underwent femoroplasty and combined femoroplasty/acetabuloplasty more often than women.
Regarding procedure type, the higher prevalence of combined femoroplasty/acetabuloplasty in male patients was expected given their significantly higher prevalence of mixed cam/pincer impingement. The higher rate of acetabuloplasty among male patients can be explained by their higher prevalence of mixed cam/pincer impingement as well, given that acetabuloplasty is an indicated procedure for mixed-type impingement, and not just for isolated pincer-type impingement. While female patients had a higher prevalence of isolated pincer-type impingement, the higher prevalence in male patients of mixed cam/pincer impingement, and thus of undergoing both femoroplasty and acetabuloplasty, contributed to their higher rates across all operative procedures.
Regarding PRO improvements, female patients outperformed male patients for HOS-SS, mHHS, and VAS pain scores. However, HOS-SS and mHHS scores of both male and female patients improved far beyond MCID thresholds (Table 2). 67 This aligned with results from other studies, which suggested that sex does not significantly impact potential clinical benefits of undergoing arthroscopy for FAIS. 16,22,23,53,55 In light of the current literature, and given the MCID findings of this study, the clinical impact of statistical differences was likely minimal. Considered alongside the comparable THA conversion rates between sexes, this suggests that operative treatment for FAIS can be beneficial and worth the minimal risks it presents, regardless of sex.
For VAS pain improvements (male patients: 8.66, female patients: 10.51), both sexes experienced improvements far below those required to achieve substantial clinical benefit as defined by Beck et al 4 (minimum 25.5-point improvement). Similarly, average VAS pain score improvements did not meet the MCID threshold set by Beck et al 4 (a decrease of 14.8) for male or female patients. VAS, however, is one of many metrics of pain measurement. Thus, these results should not limit one’s decision to pursue HA for FAIS given that overall clinical outcomes still improved for both sexes after surgical intervention.
Male patients had significantly lower rates of postoperative complications compared with female patients. Due to the heterogeneity of postoperative complications that studies chose to report, it was not feasible to compare male versus female rates for individual outcomes. However, postoperative complications that studies did report suggested that arthroscopy for FAIS may be riskier for female patients with respect to achieving ideal outcomes, although their potential benefits in PROs may be greater than that of male patients. Other studies reported similar trends of female patients being at greater risk for less desirable outcomes after HA for FAIS. 20,45,47,71 Given that this study found that female patients experienced pincer-type impingement more frequently, it was possible that the difference in postoperative complication rates was due to higher complication rates for acetabuloplasty rather than sex differences. However, other studies reported either no significant differences in complication rates between acetabuloplasty, femoroplasty, and combined femoroplasty/acetabuloplasty 31 or higher complication rates for femoroplasty and combined femoroplasty/acetabuloplasty. 86 Thus, the effects of operative procedure on postoperative complication rates could not solely account for trends observed in this study.
Larson et al 45 identified a significantly higher rate of postoperative complications after HA for female patients compared with male patients. Similarly, Dooley et al 20 reported that female patients are significantly less likely to return to sport after HA for treatment of FAIS. Therefore, patient-specific risks versus benefits of undergoing arthroscopy for FAIS may be particularly important to consider for female athletes. Despite differences in postoperative complication rates, the lack of a sex differences in THA conversion rates suggested that postoperative risks did not progress to requiring total hip replacements. Along with current literature, 16 this suggests that HA for FAIS can offer clinically significant benefits with minimal long-term risks for both male and female patients.
Limitations
This study has several limitations. There was a lack of consistency in the type and method of outcomes reported for FAIS and HA. For instance, many PRO measures exist, yet not all studies reported each PRO. In addition, functional outcomes such as hip strength and range of motion were commonly underreported and thus omitted from data extraction. Clinical criteria for defining FAIS have evolved over time, introducing variation in the way studies defined, reported, and measured FAIS-related outcomes. In addition, there is inconsistency in reporting sex-specific outcomes for HA after a diagnosis of FAIS - out of 236,604 total patients in the present study, only 212,964 had sex-stratified data. Furthermore, prevalence data can be skewed by the small number of studies reporting these values.
Conclusion
Male patients who underwent HA for FAIS had a higher prevalence of mixed-type FAIS while female patients had more pincer-type FAIS. Female patients gained greater improvements in PROs, though both sexes exceeded the MCID, suggesting that male and female patients can each benefit from HA. Large, high-quality, directly comparative studies are needed to confirm any sex differences in the prevalence and outcomes of HA for FAIS.
Appendix
Table A1.
Search Strategy
| Strategy | No. of Studies |
|---|---|
| EMBASE (4205 studies) | |
| (‘hip arthroscopy’ OR ‘femoroacetabular impingement’ OR ‘labrum tear’ OR ‘labral tear’) AND (‘gender’/exp OR gender OR ‘sex’/exp OR sex OR ‘male’/exp OR male OR ‘female’/exp OR female) AND English: la AND human | 4205 |
| MEDLINE (2345 studies) | |
| 1. hip arthroscopy.mp. | 2539 |
| 2. exp femoroacetabular impingement/ | 2136 |
| 3. (labral tear or labrum tear).mp. | 736 |
| 4. (gender or sex).mp. | 1,166,949 |
| 5. (male or female).mp. | 12,388,556 |
| 6. (1) or (2) or (3) | 4404 |
| 7. (4) or (5) | 12,563,868 |
| 8. (6) and (7) | 2569 |
| 9. Limit 8 to (English language and humans) | 2345 |
| PubMed (4170 studies) | |
| (hip arthroscopy OR femoroacetabular impingement OR labrum tear OR labral tear) AND (gender OR sex OR male OR female) | 4170 |
Table A2.
Study Characteristics a
| Lead Author (Year) | Study Design | LOE | MINORS Score b | Male | Female | Follow-up, mo d | ||
|---|---|---|---|---|---|---|---|---|
| No. of Hips | Mean Age, y | No. of Hips | Mean Age, y | |||||
| Amenabar (2013) 2 | Therapeutic case series, cohort | 4 | 18 | 26 | 21.8 | 0 | NR | 24 (mean: 49.3) |
| Beck (2021) 3 | Case-control | 3 | 16 | 75 | NR | 75 | NR | 60 |
| Bedi (2012) 6 | Cohort | 3 | 18 | 342 | NR | 274 | NR | (10 days) 1.5, 3, 6, 12, 24e |
| Bodendorfer (2021) 7 | Case-control | 3 | 17 | 123 | NR | 320 | NR | 12 |
| Bonazza (2018) 8 | Cross-sectional | 4 | 15 | 23,043 | NR | 39,739 | NR | 60-120 |
| Brown-Taylor (2020) 9 | Cross-sectional, case-control laboratory study | 3 | 17 | 13 | 37 | 24 | 34 | 12 |
| Cevallos (2021) 12 | Cross-sectional | 3 | 12 c | 18674 | NR | 34429 | NR | 24 |
| Chahla (2019) 13 | Cohort | 3 | 18 | 213 | NR | 387 | NR | 24 |
| Chandrasekaran (2017) 14 | Therapeutic case series (retrospective) | 4 | 18 | 15 | 16.7 | 87 | 16.2 | 24 |
| Charlton (2016) 15 | Cross-sectional | NR | 22 | 34 | NR | 17 | NR | 12-24 |
| Cvetanovich (2018) 16 | Therapeutic case series | 4 | 19 | 11 | NR | 26 | NR | 24 |
| Degen (2017) 17 | Retrospective cohort | NR | 15 | 3801 | NR | 4443 | NR | NR |
| Domb (2021) 19 | Case-control | 3 | 17 | 260 | NR | 485 | NR | 60 |
| Dooley (2020) 20 | Retrospective cohort | NR | 14 | 200 | NR | 65 | NR | 24 |
| Ellenrieder (2017) 21 | Case series | NR | 12 c | 30 | 44.2 | 38 | 45.4 | 3 |
| Flores (2020) 22 | Cohort | 2 | 18 | 59 | 35.8 | 72 | 34.2 | 24 |
| Frank (2016) 23 | Prognostic cohort | 2 | 21 | 75 | 37.38 | 75 | 38.41 | 24 |
| Freke (2019) 24 | Cross-sectional | 3 | 16 | 66 | NR | 48 | NR | NR |
| Fukushima (2021) 25 | Retrospective cohort | NR | 11 c | 5 | 46.2 | 0 | NR | 12 (mean: 40.2) |
| Glein (2021) 28 | Cohort | 3 | 21 | 73 | 26.4 | 73 | 25.6 | 3, 12, annually |
| Gupta (2016) 30 | Case series | 4 | 16 | 228 | NR | 367 | NR | 24 |
| Haynes (2018) 33 | Prospective cohort | NR | 15 | 254 | NR | 1321 | NR | 36 |
| Hetsroni (2013) 34 | Retrospective comparative, cross-sectional | 3 | 18 | 123 | 24 | 74 | 23 | NR |
| Hinzpeter (2015) 35 | Case series | 4 | 12 c | 17 | NR | 23 | NR | NR |
| Hooper (2016) 36 | Retrospective, cross-sectional (survey) | 4 | 16 | 48 | 16.4 | 129 | 16 | 24 |
| Jack (2020) 37 | Case-control | 3 | 17 | 23 | 27.5 | 0 | NR | 12 |
| Joseph (2016) 39 | Cohort | 2 | 17 | 73 | NR | 156 | NR | 3 |
| Kern (2018) 40 | Prospective, case series | 4 | 10 c | 37 | NR | 63 | NR | NR |
| Khazi (2019) 41 | Retrospective cohort | 3 | 19 | 4389 | NR | 5088 | NR | 1, 2 |
| Kierkegaard (2022) 42 | Prospective cohort | NR | 16 | 31 | NR | 44 | NR | 12 |
| Kopec (2020) 43 | Cross-sectional | NR | 7 c | 181 | NR | 319 | NR | NR |
| Maradit Kremers (2017) 56 | Retrospective cohort | NR | 15 | 3781 | NR | 6261 | NR | 36 |
| Ladd (2016) 44 | Retrospective cohort | NR | 21 | 31 | 36.5 | 62 | 40 | 12 |
| Larson (2016) 45 | Case series | 4 | 12 c | 810 | NR | 805 | NR | 18.7 (mean) |
| Laurito (2021) 46 | Retrospective cohort | 2 | 16 | 131 | 39 | 63 | 43 | 17 (mean) |
| Lee (2010) 47 | Therapeutic case series (retrospective) | 4 | 12 c | 75 | NR | 109 | NR | NR |
| Lee (2014) 50 | Retrospective, cross-sectional | NR | 10 c | 1923 | NR | 1782 | NR | NR |
| Lee (2015) 48 | Case series | 4 | 11 c | 56 | 36 | 75 | 34.5 | 12 |
| Lewis (2018) 51 | Case-control, laboratory study | NR | 19 | 30 | NR | 32 | NR | NR |
| Lindner (2014) 52 | Cohort | 3 | 17 | 320 | 38.3 | 334 | 40.4 | NR |
| Maerz (2021) 53 | Prognostic cohort | 2 | 15 | 269 | 29.8 | 352 | 29.9 | 12 (mean: 48) |
| Maffiuletti (2020) 54 | Cross-sectional, retrospective | NR | 18 | 13 | 24 | 21 | 26 | NR |
| Maldonado (2021) 55 | Retrospective comparative observation, cohort | 3 | 17 | 466 | 32.0 | 860 | 31.4 | 24, 60 |
| Marom (2020) 57 | Cross-sectional | 3 | 16 | 257 | 26.5 | 164 | 22.7 | NR |
| McCarthy (2011) 60 | Therapeutic, cohort | 4 | 15 | 148 | NR | 192 | NR | 120 |
| McDonald (2014) 61 | Cohort | 3 | 19 | 17 | 31 | 0 | NR | NR |
| Montgomery (2013) 62 | Cross-sectional | 4 | 15 | 1624 | NR | 1823 | NR | 36 |
| Morales-Avalos (2021) 63 | Cross-sectional | 3 | 17 | 1280 | 32.3 | 598 | 28.6 | NR |
| Nepple (2014) 64 | Prognostic cohort | 1 | 19 | 50 | 28.7 | 50 | 31.4 | NR |
| Newman (2016) 65 | Case series, cohort | 4 | 17 | 27 | 38 | 0 | NR | 12, 24, 60 |
| Nwachukwu (2017) 68 | Case series | 4 | 14 | 0 | NR | 33 | 26.1 | 12-44 |
| Nwachukwu (2019) 66 | Cohort (diagnosis) | 2 | 18 | 46 | NR | 151 | NR | NR |
| Öhlin (2017) 69 | Prospective cohort | NR | 18 | 194 | NR | 121 | NR | 24 |
| Philippon (2010) 70 | Case series | 4 | 12 c | 28 | 27 | 0 | NR | 24 (mean) |
| Poehling-Monaghan (2017) 71 | Case-control | 3 | 14 | 23 | NR | 24 | NR | 12 |
| Ramos (2020) 72 | Retrospective cohort | NR | 15 | 10 | 19.5 | 0 | NR | NR |
| Redmond (2015) 73 | Therapeutic case series | 4 | 11 c | 160 | 40.2 | 232 | 36 | 24 |
| Robinson (2020) 74 | Cohort | NR | 17 | 63 | NR | 108 | NR | 12 |
| Ross (2014) 75 | Prospective, longitudinal data, cross-sectional | NR | 16 | 4 | NR | 26 | NR | 22 (mean) |
| Saks (2021) 76 | Cohort | 3 | 17 | 109 | 35.36 | 109 | 35.62 | 24 |
| Salvo (2018) 77 | Retrospective, cross-sectional | 3 | 16 | 446 | 34.2 | 765 | 34.8 | NR |
| Schairer (2019) 78 | Case series | 4 | 10 c | NR | NR | 36 | ||
| Schallmo (2018) 79 | Descriptive epidemiology, cohort | NR | 15 | 227 | 28.9 | 0 | NR | First professional RTP |
| Sharfman (2016) 80 | Retrospective, cross-sectional | NR | 10 c | 27 | NR | 35 | NR | 27.9 (mean) |
| Shibata (2017) 81 | Cohort | 3 | 17 | 54 | 20.5 | 42 | 21.5 | 12 (mean: 18.6 M, 19.3 F) |
| Sivasundaram (2020) 82 | Retrospective cohort | 4 | 18 | 2401 | NR | 3892 | NR | (7 days), 1, 2 |
| Suarez-Ahedo (2017) 84 | Cross-sectional | 3 | 17 | 560 | NR | 941 | NR | 36-108 |
| Tannenbaum (2014) 85 | Cross-sectional | NR | 11 | 60 | 32 | 60 | 32 | NR |
| Byrd (2000) 10 | Case series | NR | 12 c | 18 | NR | 17 | NR | 1, 3, 6, 12, 24 |
| Weber (2020) 87 | Case series | 4 | 16 | 29 | NR | 10 | NR | NR |
| Willimon (2019) 88 | Cohort | 4 | 17 | 105 | NR | 101 | NR | 2-5 weeks |
| Yoo (2018) 89 | Comparative trial, cohort | 3 | 22 | 56 | 21.95 | 0 | NR | 24 |
| Zimmerer (2021) 90 | Retrospective comparative, cohort | 3 | 18 | 71 | NR | 41 | NR | 120 (mean: 132) |
| Zusmanovich (2022) 91 | Retrospective comparative, cross-sectional | 3 | 9 c | 11,545 | NR | 24,421 | NR | 24 |
a F, female; LOE, level of evidence; M, male; MINORS, methodological index for nonrandomized studies; NR, not reported; RTP, return to play.
b Noncomparative studies are scored out of 16; comparative studies are scored out of 24.
c Noncomparative studies.
d All values are minimum postoperative follow-up in months, unless range or mean is otherwise noted (time measurements not in months are noted).
eFollow-up days in parentheses as the column is defined in units of months -- any follow-up periods <1 month are written in units of 'days' and set-off from the other units of months with parentheses.
Figure A1.
Forest plot demonstrating sex-based differences in the prevalence of (A) cam hips, (B) pincer hips, and (C) mixed cam/pincer hips among patients with FAIS. FAIS, femoroacetabular impingement syndrome; M-H, Mantel-Haenszel.
Figure A2.
Forest plot demonstrating sex-based differences in the prevalence of (A) femoroplasty, (B) acetabuloplasty, and (C) combined femoroplasty/acetabuloplasty among patients with FAIS. FAIS, femoroacetabular impingement syndrome; M-H, Mantel-Haenszel.
Figure A3.
Forest plot demonstrating changes in (A) HOS-ADL, (B) HOS-SS, (C) mHHS, and (D) VAS for pain for male versus female patients after HA for FAIS. FAIS, femoroacetabular impingement syndrome; HA, hip arthroscopy; HOS-ADL, Hip Outcome Score-Activities of Daily Living subscale; HOS-SS, Hip Outcome Score, Sport-Specific subscale; IV, inverse variance; mHHS, modified Harris Hip Score; Std., standardized; VAS, visual analog scale for pain.
Figure A4.
Forest plot demonstrating (A) complication rates and (B) conversion rates to THA for male versus female patients after HA for FAIS. FAIS, femoroacetabular impingement syndrome; HA, hip arthroscopy; M-H, Mantel-Haenszel; THA, total hip arthroplasty.
Table A3.
Sex-Specific Differences After HA for FAIS According to PROs a
| Lead Author (Year) | Pre- to Postop Differences? (M/F) | Sex-Specific Outcomes |
|---|---|---|
| HOS-ADL | ||
| Beck (2021) 3 | Yes/Yes | No significant sex difference in achieving MCID, but significant pre- to postop improvements for both sexes |
| Chandrasekaran (2017) 14 | Yes/Yes | Female patients had significantly lower baseline scores, but showed significantly greater improvements postop vs male patients |
| Frank (2016) 23 | Yes/Yes | Both male and female patients showed significant improvements in pre- vs postop scores at 2-y follow-up |
| Hetsroni (2013) 34 | NR/NR | Female patients had a significantly lower baseline mean vs male patients (68.3 ± 16.4 vs 75.7 ± 14.9, P = .004) |
| Lindner (2014) 52 | NR/NR | Female patients had significantly lower preop scores vs males (60.7 vs 64.3, P = .03) |
| Nwachukwu (2017) 68 | NR /Yes | Only female patients enrolled (mean pre- vs postop scores: 66.9 ± 18.8 vs 86.8 ± 15.8) |
| Salvo (2018) 77 | NR/NR | Significantly lower baseline scores for female vs male patients (60.9 vs 67.1, P < .001) |
| HOS-SS | ||
| Beck (2021) 3 | Yes/Yes | Females achieved MCID and PASS at significantly higher rates vs males (P < .05) |
| Chandrasekaran (2017) 14 | Yes/Yes | Females had significantly lower postop scores vs males (78.6 vs 91.0) |
| Frank (2016) 23 | Yes/Yes | Both sexes had significant improvements at 2-y follow-up (M: 46.72 ± 26.29 to 86.29 ± 11.55; F: 40.62 ± 22.11 to 81.18 ± 14.48; P < .0001 for both) |
| Glein (2021) 28 | Yes/Yes | Females achieved MCID at significantly higher rates vs males (85.1% vs 70.0%, P = .035) |
| Hetsroni (2013) 34 | NR/NR | Females had significantly lower preop scores vs males (42.7 ± 23.8 vs 52.3 ± 22.9, P = .016) |
| Lindner (2014) 52 | NR/NR | Females had nonsignificantly lower baseline scores vs males (38.6 vs 42.3, P = .06) |
| Nwachukwu (2017) 68 | NR/Yes | Only female patients enrolled (pre- vs postop scores: 43.9 ± 23.6 vs 70.4 ± 32.8) |
| Maldonado (2022) 55 | Yes/Yes | Both sexes showed significant improvements at 2- and 5-y follow-up (P < .001) |
| Salvo (2018) 77 | NR/NR | Female patients had significantly lower baseline scores vs male patients (39.37 ± 20.80 vs 45.15 ± 22.15, P < .001) |
| mHHS | ||
| Amenabar (2013) 2 | Yes/NR | Only male patients enrolled; significant improvement at 2-y follow-up after HA (83.6-98, P < .05) |
| Beck (2021) 3 | Yes/Yes | Female patients achieved MCID and PASS at significantly higher rates vs male patients (P < .05) |
| Chandrasekaran (2017) 14 | Yes/Yes | Both sexes showed significant improvement (P < .01), but female patients had lower pre- and postop scores vs male patients (F: 63.4-88.8, M: 71.0-94.3) |
| Domb (2021) 19 | Yes/Yes | Both sexes had significant improvement in scores from preop (F: 63.5 ± 14.4; M: 67.5 ± 15.5) to 5-y follow-up (F: 87.7 ± 14.8; M: 90.1 ± 13.1) (P < .001), with no significant difference at final follow-up (P = .079) |
| Flores (2020) 22 | Yes/Yes | Both sexes achieved PASS for mHHS at similar rates (F: 76.4% vs M: 77.2%, P = .915) |
| Frank (2016) 23 | Yes/Yes | Both sexes had significant improvements at 2-y follow-up (M: 59.27 ± 11.99 to 83.37 ± 7.15; F: 58.36 ± 12.29 to 80.43 ± 8.80; P < .0001 for both) |
| Glein (2021) 28 | Yes/Yes | Female patients had significantly lower preop scores vs male patients (63.9 ± 12.6 vs 72.5 ± 13.7, P < .001), and both sexes significantly improved at 2-y follow-up (ΔM: 16.6 ± 19.5, P < .001; ΔF: 22.9 ± 19.9, P < .001), with no significant sex-based difference in postop scores (P = .490) |
| Hetsroni (2013) 34 | NR/NR | Female patients had significantly lower baseline score vs male patients (63.8 ± 11.9 vs 72.5 ± 14.1, P < .001) |
| Lee (2015) 48 | NR/NR | No statistically significant difference in scores between sexes |
| Lindner (2014) 52 | NR/NR | Female patients had significantly lower baseline score vs male patients (59.9 vs 62.6, P = .033) |
| Nepple (2014) 64 | NR/NR | Female patients had significantly lower baseline mHHS vs male patients (54.4 ± 14.8 vs 63.7 ± 16.6, P = .004) |
| Nwachukwu (2017) 68 | NR/Yes | Only female patients enrolled; most patients achieved MCID at 1-y follow-up (preop vs postop: 57.2 ± 15.3 vs 79.5 ± 19.0) |
| Philippon (2010) 70 | Yes/NR | Only male patients enrolled; average score improved from 70 (range: 57-100) to 95 (range: 74-100) at 2-y follow-up |
| Ramos (2020) 72 | Yes/NR | Only male patients enrolled; increase in median scores at 1.6-y follow-up (66.0 ± 7.9 to 89.5 ± 3.2) after HA for FAIS |
| Saks (2021) 76 | Yes/Yes | Both sexes achieved significant improvement at 2-y follow-up (ΔM: 20.14 ± 18.69; ΔF: 21.61 ± 15.99; P < .001 for both) |
| Salvo (2018) 77 | NR/NR | Female patients had significantly lower scores and therefore self-reported functional deficits vs male patients (53.40 vs 57.83, P < .001) |
| Shibata (2017) 81 | Yes/Yes | Both sexes had significant pre- to postop improvement in scores (F: 74.3 ± 12.1 to 97.9 ± 4.4, M: 73.0 ± 16.6 to 96.3 ± 20.2; P < .001 for both) |
| Yoo (2018) 89 | Yes/NR | Both the study group (male military population) and control group showed significant increases at final follow-up (63.5 to 89.9 for study group, P < .001 for both study and control groups) |
| iHOT-12 | ||
| Robinson (2020) 74 | NR/NR | Female patients had a significantly lower median postop score vs male patients after HA (70.0 vs 76.0, P = .05) |
| Salvo (2018) 77 | NR/NR | Female patients had significantly lower baseline scores vs male patients (31.2 vs 38.5, P = .001) |
| VAS Pain | ||
| Beck (2021) 3 | Yes/Yes | Both sexes had significant decreases in pain at 5-y follow-up (F: 70.9 ± 19.6 to 24.7 ± 28.9; M: 70.9 ± 19.6 to 24.7 ± 28.9, P < .001 for both) |
| Chandrasekaran (2017) 14 | Yes/Yes | Both sexes had significant improvement in pain at 2-y follow-up after HA (M: 4.77 to 1.85, F: 6.29 to 2.21, P < .01), although female patients had higher preop and postop pain scores |
| Flores (2020) 22 | Yes/Yes | No significant difference between sexes in preop (M: 4.2 ± 2.6, F: 4.7 ± 2.4, P = .292) or postop (M: 1.9 ± 2.3, F: 2.0 ± 2.5, P = .877) pain at 2-y follow-up after HA for FAIS |
| Glein (2021) 28 | Yes/Yes | Female patients had significantly higher baseline pain scores vs male patients (5.8 ± 2.3 vs 4.6 ± 2.2, P < .001), no significant sex-based difference at 2-y follow-up (F: 2.1 ± 2.4, M: 1.9 ± 2.4, P = .677). Both sexes had significant decreases in pain at follow-up (ΔF: 3.8 ± 3.1; ΔM: 2.7 ± 3.2), female patients had larger improvements vs male patients (P = .031) |
| Lindner (2014) 52 | NR/NR | Similar preop pain scores for both sexes (M: 5.7, F: 5.9, P = .43) |
| Maldonado (2022) 55 | Yes/Yes | Both sexes achieved MCID for VAS pain at similar rates (P = .087), and both sexes showed significant improvement from preop to 5-y follow-up (F: 5.3 ± 2.2 to 2.0 ± 2.2; M: 4.6 ± 2.3 to 1.7 ± 2.1, P < .001 for both) |
| Saks (2021) 76 | Yes/Yes | No significant difference between sexes in preop (M: 4.69 ± 2.45, F: 5.32 ± 2.28, P = .068) or postop (M: 2.20 ± 2.38, F: 2.22 ± 2.38, P = .778) pain, but both sexes showed significant improvement in at 2-y follow-up after HA (P < .001) |
| Salvo (2018) 77 | NR/NR | Female patients had significantly higher average preop pain scores vs male patients (55.42 ± 19.72 vs 50.40 ± 21.72, P < .001) |
| Yoo (2018) 89 | Yes/NR | In a male military population, pain improved from 7.6 to 2.6 vs 7.0 to 2.2 for controls (P < .001) at 2-y follow-up after HA |
a F, female; FAIS, femoroacetabular impingement syndrome; HA, hip arthroscopy; HOS-ADL, Hip Outcome Score–Activities of Daily Living subscale; HOS-SS, Hip Outcome Score–Sport-Specific subscale; iHOT-12, International Hip Outcome Tool–12; M, male; MCID, minimal clinically important difference; mHHS, modified Harris Hip Score; NR, not reported; PASS, Patient Acceptable Symptom State; postop, postoperative; preop, preoperative; PRO, patient-reported outcome; VAS, visual analog scale.
Footnotes
Final revision submitted February 23, 2023; accepted April 11, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.J.H. has received education payments from Medwest. V.K.T. has received education payments from Arthrex and consulting and nonconsulting fees from Smith & Nephew. M.A.T. has received nonconsulting fees from Arthrex and Smith & Nephew. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Ahmad MA, Xypnitos FN, Giannoudis PV. Measuring hip outcomes: common scales and checklists. Injury. 2011;42(3):259–264. [DOI] [PubMed] [Google Scholar]
- 2. Amenabar T, O’Donnell J. Return to sport in Australian Football League footballers after hip arthroscopy and midterm outcome. Arthroscopy. 2013;29(7):1188–1194. [DOI] [PubMed] [Google Scholar]
- 3. Beck EC, Drager J, Nwachukwu BU, Jan K, Rasio J, Nho SJ. Gender and age-specific differences observed in rates of achieving meaningful clinical outcomes 5-years after hip arthroscopy for femoroacetabular impingement syndrome. Arthroscopy. 2021;37(8):2488–2496.e1. [DOI] [PubMed] [Google Scholar]
- 4. Beck EC, Nwachukwu BU, Kunze KN, Chahla J, Nho SJ. How can we define clinically important improvement in pain scores after hip arthroscopy for femoroacetabular impingement syndrome? Minimum 2-year follow-up study. Am J Sports Med. 2019;47(13):3133–3140. [DOI] [PubMed] [Google Scholar]
- 5. Beck M, Kalhor M, Leunig M, Ganz R. Hip morphology influences the pattern of damage to the acetabular cartilage: femoroacetabular impingement as a cause of early osteoarthritis of the hip. J Bone Joint Surg Br. 2005;87(7):1012–1018. [DOI] [PubMed] [Google Scholar]
- 6. Bedi A, Zbeda RM, Bueno VF, Downie B, Dolan M, Kelly BT. The incidence of heterotopic ossification after hip arthroscopy. Am J Sports Med. 2012;40(4):854–863. [DOI] [PubMed] [Google Scholar]
- 7. Bodendorfer BM, Clapp IM, DeFroda SF, et al. The natural course of recovery after hip arthroscopy for femoroacetabular impingement according to the International Hip Outcome Tool-12 and Hip Outcome Score Sports Subscale. Am J Sports Med. 2021;49(12):3250–3260. [DOI] [PubMed] [Google Scholar]
- 8. Bonazza NA, Homcha B, Liu G, Leslie DL, Dhawan A. Surgical trends in arthroscopic hip surgery using a large national database. Arthroscopy. 2018;34(6):1825–1830. [DOI] [PubMed] [Google Scholar]
- 9. Brown-Taylor L, Schroeder B, Lewis CL, et al. Sex-specific sagittal and frontal plane gait mechanics in persons post-hip arthroscopy for femoroacetabular impingement syndrome. J Orthop Res. 2020;38(11):2443–2453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Byrd JWT, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16(6):578–587. [DOI] [PubMed] [Google Scholar]
- 11. Byrd JWT, Jones KS. Arthroscopic femoroplasty in the management of cam-type femoroacetabular impingement. Clin Orthop Relat Res. 2009;467(3):739–746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cevallos N, Soriano KKJ, Flores SE, Wong SE, Lansdown DA, Zhang AL. Hip arthroscopy volume and reoperations in a large cross-sectional population: high rate of subsequent revision hip arthroscopy in young patients and total hip arthroplasty in older patients. Arthroscopy. 2021;37(12):3445–3454.e1. [DOI] [PubMed] [Google Scholar]
- 13. Chahla J, Nwachukwu BU, Beck EC, et al. Influence of acetabular labral tear length on outcomes after hip arthroscopy for femoroacetabular impingement syndrome with capsular plication. Am J Sports Med. 2019;47(5):1145–1150. [DOI] [PubMed] [Google Scholar]
- 14. Chandrasekaran S, Darwish N, Chaharbakhshi EO, Lodhia P, Suarez-Ahedo C, Domb BG. Arthroscopic treatment of labral tears of the hip in adolescents: patterns of clinical presentation, intra-articular derangements, radiological associations and minimum 2-year outcomes. Arthroscopy. 2017;33(7):1341–1351. [DOI] [PubMed] [Google Scholar]
- 15. Charlton PC, Bryant AL, Kemp JL, Clark RA, Crossley KM, Collins NJ. Single-leg squat performance is impaired 1 to 2 years after hip arthroscopy. PM R. 2016;8(4):321–330. [DOI] [PubMed] [Google Scholar]
- 16. Cvetanovich GL, Weber AE, Kuhns BD, et al. Clinically meaningful improvements after hip arthroscopy for femoroacetabular impingement in adolescent and young adult patients regardless of gender. J Pediatr Orthop. 2018;38(9):465–470. [DOI] [PubMed] [Google Scholar]
- 17. Degen RM, Pan TJ, Chang B, et al. Risk of failure of primary hip arthroscopy - a population-based study. J Hip Preserv Surg. 2017;4(3):214–223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Diaz-Ledezma C, Parvizi J. Surgical approaches for cam femoroacetabular impingement: the use of multicriteria decision analysis. Clin Orthop Relat Res. 2013;471(8):2509–2516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Domb BG, Chen SL, Go CC, et al. Predictors of clinical outcomes after hip arthroscopy: 5-year follow-up analysis of 1038 patients. Am J Sports Med. 2021;49(1):112–120. [DOI] [PubMed] [Google Scholar]
- 20. Dooley M, Burger J, Kelly B, O’Sullivan E. Are there sex differences in return to play rates in high level athletes following hip arthroscopy? Orthop J Sports Med. 2020;8(7)(suppl 6):2325967120S0042. [Google Scholar]
- 21. Ellenrieder M, Tischer T, Bader R, Kreuz PC, Mittelmeier W. Patient-specific factors influencing the traction forces in hip arthroscopy. Arch Orthop Trauma Surg. 2017;137(1):81–87. [DOI] [PubMed] [Google Scholar]
- 22. Flores SE, Chambers CC, Borak KR, Zhang AL. Is there a gender gap in outcomes after hip arthroscopy for femoroacetabular impingement? Assessment of clinically meaningful improvements in a prospective cohort. Orthop J Sports Med. 2020;8(7):2325967119900561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Frank RM, Lee S, Bush-Joseph CA, et al. Outcomes for hip arthroscopy according to sex and age: a comparative matched-group analysis. J Bone Joint Surg Am. 2016;98(10):797–804. [DOI] [PubMed] [Google Scholar]
- 24. Freke M, Kemp J, Crossley K, Sims K, Russell T, Semciw A. Strength and range of movement deficits are associated with symptom severity in people scheduled for hip arthroscopy. Eur J Pain. 2019;23(6):1083–1090. [DOI] [PubMed] [Google Scholar]
- 25. Fukushima K, Uekusa Y, Koyama T, et al. Efficacy and safety of arthroscopic treatment for native acute septic arthritis of the hip joint in adult patients. BMC Musculoskelet Disord. 2021;22(1):318. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Ganz R, Leunig M, Leunig-Ganz K, Harris WH. The etiology of osteoarthritis of the hip: an integrated mechanical concept. Clin Orthop Relat Res. 2008;466(2):264–272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Ganz R, Parvizi J, Beck M, Leunig M, Nötzli H, Siebenrock KA. Femoroacetabular impingement: a cause for osteoarthritis of the hip. Clin Orthop Relat Res. 2003;(417):112–120. [DOI] [PubMed] [Google Scholar]
- 28. Glein RM, Jimenez AE, Miecznikowski KB, et al. Patient-reported outcome scores and rate of return to sport after hip arthroscopic surgery: a sex-based comparison in professional and collegiate athletes. Am J Sports Med. 2021;49(12):3242–3249. [DOI] [PubMed] [Google Scholar]
- 29. Griffin DR, Parsons N, Mohtadi NGH, Safran MR, Multicenter Arthroscopy of the Hip Outcomes Research Network. A short version of the International Hip Outcome Tool (iHOT-12) for use in routine clinical practice. Arthroscopy. 2012;28(5):611–616. [DOI] [PubMed] [Google Scholar]
- 30. Gupta A, Redmond JM, Stake CE, Dunne KF, Domb BG. Does primary hip arthroscopy result in improved clinical outcomes?: 2-year clinical follow-up on a mixed group of 738 consecutive primary hip arthroscopies performed at a high-volume referral center. Am J Sports Med. 2016;44(1):74–82. [DOI] [PubMed] [Google Scholar]
- 31. Hartwell MJ, Morgan AM, Johnson DJ, et al. Risk factors for 30-day readmission following hip arthroscopy. Knee Surg Sports Traumatol Arthrosc. 2020;28(4):1290–1295. [DOI] [PubMed] [Google Scholar]
- 32. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: Visual Analog Scale for Pain (VAS Pain), Numeric Rating Scale for Pain (NRS Pain), McGill Pain Questionnaire (MPQ), Short-Form McGill Pain Questionnaire (SF-MPQ), Chronic Pain Grade Scale (CPGS), Short Form-36 Bodily Pain Scale (SF-36 BPS), and Measure of Intermittent and Constant Osteoarthritis Pain (ICOAP). Arthritis Care Res. 2011;63(suppl 11):S240–252. [DOI] [PubMed] [Google Scholar]
- 33. Haynes JA, Pascual-Garrido C, An TW, Nepple JJ, Clohisy JC. ANCHOR Group, Trends of hip arthroscopy in the setting of acetabular dysplasia. J Hip Preserv Surg. 2018;5(3):267–273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Hetsroni I, Dela Torre K, Duke G, Lyman S, Kelly BT. Sex differences of hip morphology in young adults with hip pain and labral tears. Arthroscopy. 2013;29(1):54–63. [DOI] [PubMed] [Google Scholar]
- 35. Hinzpeter J, Barrientos C, Barahona M, et al. Fluid extravasation related to hip arthroscopy: a prospective computed tomography-based study. Orthop J Sports Med. 2015;3(3):232596711557322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Hooper P, Oak SR, Lynch TS, Ibrahim G, Goodwin R, Rosneck J. Adolescent femoroacetabular impingement: gender differences in hip morphology. Arthroscopy. 2016;32(12):2495–2502. [DOI] [PubMed] [Google Scholar]
- 37. Jack RA II, Sochacki KR, Hirase T, et al. Performance and return to sport after hip arthroscopy in the National Basketball Association. Arthroscopy. 2020;36(2):473–478. [DOI] [PubMed] [Google Scholar]
- 38. Jensen MP, Karoly P, Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117–126. [DOI] [PubMed] [Google Scholar]
- 39. Joseph R, Pan X, Cenkus K, Brown L, Ellis T, Di Stasi S. Sex differences in self-reported hip function up to 2 years after arthroscopic surgery for femoroacetabular impingement. Am J Sports Med. 2016;44(1):54–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Kern MJ, Murray RS, Sherman TI, Postma WF. Incidence of nerve injury after hip arthroscopy. J Am Acad Orthop Surg. 2018;26(21):773–778. [DOI] [PubMed] [Google Scholar]
- 41. Khazi ZM, An Q, Duchman KR, Westermann RW. Incidence and risk factors for venous thromboembolism following hip arthroscopy: a population-based study. Arthroscopy. 2019;35(8):2380–2384.e1. [DOI] [PubMed] [Google Scholar]
- 42. Kierkegaard S, Mechlenburg I, Dalgas U, Lund B, Søballe K, Sørensen H. Hip kinematics and kinetics in patients with femoroacetabular impingement syndrome before and 1 year after hip arthroscopic surgery. Results from the HAFAI cohort. Arch Orthop Trauma Surg. 2022;142(8):2019–2029. [DOI] [PubMed] [Google Scholar]
- 43. Kopec JA, Hong Q, Wong H, et al. Prevalence of femoroacetabular impingement syndrome among young and middle-aged white adults. J Rheumatol. 2020;47(9):1440–1445. [DOI] [PubMed] [Google Scholar]
- 44. Ladd LM, Keene JS, del Rio AM, Rosas HG. Correlation between hip arthroscopy outcomes and preoperative anesthetic hip joint injections, MR arthrogram imaging findings, and patient demographic characteristics. AJR Am J Roentgenol. 2016;207(5):1062–1069. [DOI] [PubMed] [Google Scholar]
- 45. Larson CM, Clohisy JC, Beaulé PE, et al. Intraoperative and early postoperative complications after hip arthroscopic surgery: a prospective multicenter trial utilizing a validated grading scheme. Am J Sports Med. 2016;44(9):2292–2298. [DOI] [PubMed] [Google Scholar]
- 46. Laurito GM, Aranha FL, Piedade SR. Functional outcomes of arthroscopic treatment in 230 femoroacetabular impingement cases. Acta Ortop Bras. 2021;29(2):67–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Lee HH, Klika AK, Bershadsky B, Krebs VE, Barsoum WK. Factors affecting recovery after arthroscopic labral debridement of the hip. Arthroscopy. 2010;26(3):328–334. [DOI] [PubMed] [Google Scholar]
- 48. Lee S, Frank RM, Harris J, et al. Evaluation of sexual function before and after hip arthroscopic surgery for symptomatic femoroacetabular impingement. Am J Sports Med. 2015;43(8):1850–1856. [DOI] [PubMed] [Google Scholar]
- 49. Lee V, Kawamoto K, Hess R, et al. Implementation of a value-driven outcomes program to identify high variability in clinical costs and outcomes and association with reduced cost and improved quality. JAMA. 2016;316(10):1061–1072. [DOI] [PubMed] [Google Scholar]
- 50. Lee Y-K, Ha Y-C, Yoon B-H, Koo K-H. National trends of hip arthroscopy in Korea. J Korean Med Sci. 2014;29(2):277–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Lewis CL, Khuu A, Loverro KL. Gait alterations in femoroacetabular impingement syndrome differ by sex. J Orthop Sports Phys Ther. 2018;48(8):649–658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Lindner D, El Bitar YF, Jackson TJ, Sadik AY, Stake CE, Domb BG. Sex-based differences in the clinical presentation of patients with symptomatic hip labral tears. Am J Sports Med. 2014;42(6):1365–1369. [DOI] [PubMed] [Google Scholar]
- 53. Maerz T, Nepple JJ, Bedi A, et al. Sex Differences in clinical outcomes following surgical treatment of femoroacetabular impingement. J Bone Joint Surg Am. 2021;103(5):415–423. [DOI] [PubMed] [Google Scholar]
- 54. Maffiuletti NA, Bizzini M, Sutter R, et al. Hip muscle strength asymmetries and their associations with hip morphology and symptoms are sex-specific in patients with femoroacetabular impingement syndrome. Phys Ther Sport. 2020;42:131–138. [DOI] [PubMed] [Google Scholar]
- 55. Maldonado DR, Owens JS, Go CC, et al. Females and males achieved comparable outcomes and clinical benefits following primary hip arthroscopy with labral repair, but age affected outcomes and conversion to total hip arthroplasty. A short and mid-term follow-up analysis with dual stratification. Arthroscopy. 2022:38(8):2427–2440. [DOI] [PubMed] [Google Scholar]
- 56. Maradit Kremers H, Schilz SR, Van Houten HK, et al. Trends in utilization and outcomes of hip arthroscopy in the United States between 2005 and 2013. J Arthroplasty. 2017;32(3):750–755. [DOI] [PubMed] [Google Scholar]
- 57. Marom N, Dooley MS, Burger JA, et al. Characteristics of soccer players undergoing primary hip arthroscopy for femoroacetabular impingement: a sex- and competitive level-specific analysis. Am J Sports Med. 2020;48(13):3255–3264. [DOI] [PubMed] [Google Scholar]
- 58. Martin RL. Hip arthroscopy and outcome assessment. Oper Tech Orthop. 2005;15(3):290–296. [Google Scholar]
- 59. Mas Martinez J, Bustamante Suarez de Puga D, Verdu-Roman C, Martinez Gimenez E, Morales Santias M, Sanz-Reig J. Significant improvement after hip arthroscopy for femoroacetabular impingement in women. Knee Surg Sports Traumatol Arthrosc. 2022;3095%(6):2181–2187. [DOI] [PubMed] [Google Scholar]
- 60. McCarthy JC, Jarrett BT, Ojeifo O, Lee JA, Bragdon CR. What factors influence long-term survivorship after hip arthroscopy? Clin Orthop Relat Res. 2011;469(2):362–371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. McDonald JE, Herzog MM, Philippon MJ. Performance outcomes in professional hockey players following arthroscopic treatment of FAI and microfracture of the hip. Knee Surg Sports Traumatol Arthrosc. 2014;22(4):915–919. [DOI] [PubMed] [Google Scholar]
- 62. Montgomery SR, Ngo SS, Hobson T, et al. Trends and demographics in hip arthroscopy in the United States. Arthroscopy. 2013;29(4):661–665. [DOI] [PubMed] [Google Scholar]
- 63. Morales-Avalos R, Tapia-Náñez A, Simental-Mendía M, et al. Prevalence of morphological variations associated with femoroacetabular impingement according to age and sex: a study of 1878 asymptomatic hips in nonprofessional athletes. Orthop J Sports Med. 2021;9(2):232596712097789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64. Nepple JJ, Riggs CN, Ross JR, Clohisy JC. Clinical presentation and disease characteristics of femoroacetabular impingement are sex-dependent. J Bone Joint Surg Am. 2014;96(20):1683–1689. [DOI] [PubMed] [Google Scholar]
- 65. Newman JT, Saroki AJ, Briggs KK, Philippon MJ. Return to elite level of play and performance in professional golfers after arthroscopic hip surgery. Orthop J Sports Med. 2016;4(4):232596711664353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Nwachukwu BU, Beck EC, Chapman R, Chahla J, Okoroha K, Nho SJ. Preoperative performance of the PROMIS in patients undergoing hip arthroscopic surgery for femoroacetabular impingement syndrome. Orthop J Sports Med. 2019;7(7):232596711986007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Nwachukwu BU, Beck EC, Kunze KN, Chahla J, Rasio J, Nho SJ. Defining the clinically meaningful outcomes for arthroscopic treatment of femoroacetabular impingement syndrome at minimum 5-year follow-up. Am J Sports Med. 2020;48(4):901–907. [DOI] [PubMed] [Google Scholar]
- 68. Nwachukwu BU, Chang B, Fields K, et al. Outcomes for arthroscopic treatment of anterior inferior iliac spine (subspine) hip impingement. Orthop J Sports Med. 2017;5(8):232596711772310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Öhlin A, Sansone M, Ayeni OR, et al. Predictors of outcome at 2-year follow-up after arthroscopic treatment of femoro-acetabular impingement. J Hip Preserv Surg. 2017;4(3):224–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Philippon MJ, Weiss DR, Kuppersmith DA, Briggs KK, Hay CJ. Arthroscopic labral repair and treatment of femoroacetabular impingement in professional hockey players. Am J Sports Med. 2010;38(1):99–104. [DOI] [PubMed] [Google Scholar]
- 71. Poehling-Monaghan KL, Krych AJ, Levy BA, Trousdale RT, Sierra RJ. Female sex is a risk factor for failure of hip arthroscopy performed for acetabular retroversion. Orthop J Sports Med. 2017;5(11):232596711773747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72. Ramos N, Youssefzadeh K, Gerhardt M, Banffy M. Results of hip arthroscopy in elite level water polo players with femoroacetabular impingement: return to play and patient satisfaction. J Hip Preserv Surg. 2020;7(1):116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73. Redmond JM, Gupta A, Hammarstedt JE, Stake CE, Dunne KF, Domb BG. Labral injury: radiographic predictors at the time of hip arthroscopy. Arthroscopy. 2015;31(1):51–56. [DOI] [PubMed] [Google Scholar]
- 74. Robinson PG, Maempel JF, Murray IR, Rankin CS, Hamilton DF, Gaston P. Responsiveness and ceiling effects of the English version of the 12-item International Hip Outcome Tool following hip arthroscopy at minimum one-year follow-up. Bone Joint J. 2020;102(8):1010–1015. [DOI] [PubMed] [Google Scholar]
- 75. Ross JR, Clohisy JC, Baca G, Sink E. Patient and disease characteristics associated with hip arthroscopy failure in acetabular dysplasia. J Arthroplasty. 2014;29(9):160–163. [DOI] [PubMed] [Google Scholar]
- 76. Saks BR, Fox JD, Owens JS, et al. One bony morphology, two pathologic entities: sex-based differences in patients with borderline hip dysplasia undergoing hip arthroscopy. Am J Sports Med. 2021;49(14):3906–3914. [DOI] [PubMed] [Google Scholar]
- 77. Salvo JP, Nho SJ, Wolff AB, et al. Sex-dependent differences in preoperative, radiographic, and intraoperative characteristics of patients undergoing hip arthroscopy: results from the multicenter arthroscopic study of the hip group. Arthroscopy. 2018;34(3):844–852. [DOI] [PubMed] [Google Scholar]
- 78. Schairer WW, Nwachukwu BU, Suryavanshi JR, Welk B, Lanting B, Marsh JD. A shift in hip arthroscopy use by patient age and surgeon volume: a New York State-based population analysis 2004 to 2016. Arthroscopy. 2019;35(10):2847–2854.e1. [DOI] [PubMed] [Google Scholar]
- 79. Schallmo MS, Fitzpatrick TH, Yancey HB, Marquez-Lara A, Luo TD, Stubbs AJ. Return-to-play and performance outcomes of professional athletes in North America after hip arthroscopy from 1999 to 2016. Am J Sports Med. 2018;46(8):1959–1969. [DOI] [PubMed] [Google Scholar]
- 80. Sharfman ZT, Amar E, Tsvieli O, Alkrinawi N, Levy O, Rath E. Complications of hip arthroscopy: patient perspectives. Orthop Nurs. 2016;35(4):208–213. [DOI] [PubMed] [Google Scholar]
- 81. Shibata KR, Matsuda S, Safran MR. Arthroscopic hip surgery in the elite athlete: comparison of female and male competitive athletes. Am J Sports Med. 2017;45(8):1730–1739. [DOI] [PubMed] [Google Scholar]
- 82. Sivasundaram L, Trivedi NN, Kim C-Y, et al. Emergency department utilization after elective hip arthroscopy. Arthroscopy. 2020;36(6):1575–1583.e1. [DOI] [PubMed] [Google Scholar]
- 83. Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 84. Suarez-Ahedo C, Gui C, Rabe SM, Chandrasekaran S, Lodhia P, Domb BG. Acetabular chondral lesions in hip arthroscopy: relationships between grade, topography, and demographics. Am J Sports Med. 2017;45(11):2501–2506. [DOI] [PubMed] [Google Scholar]
- 85. Tannenbaum E, Kopydlowski N, Smith M, Bedi A, Sekiya JK. Gender and racial differences in focal and global acetabular version. J Arthroplasty. 2014;29(2):373–376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Varshneya K, Abrams GD, Sherman SL, Safran MR. Patient-specific risk factors exist for hip fractures after arthroscopic femoroacetabular impingement surgery, but not for dislocation - an analysis of more than 25,000 hip arthroscopies. Arthrosc Sports Med Rehabil. 2022;4(2):e519–e525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Weber AE, Nakata H, Mayer EN, et al. Return to sport after hip arthroscopy for femoroacetabular impingement syndrome in NCAA Division I athletes: experience at a single institution. Orthop J Sports Med. 2020;8(5):232596712091838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88. Willimon SC, Johnson MM, Herzog MM, Busch MT. Time to return to school after 10 common orthopaedic surgeries among children and adolescents. J Pediatr Orthop. 2019;39(6):322–327. [DOI] [PubMed] [Google Scholar]
- 89. Yoo J-I, Lee T-H, Kim J-Y, Kim J-H, Ha Y-C. Outcomes of hip arthroscopy in a military population are similar to those in the civilian population: matched paired analysis at 2 years. Arthroscopy. 2018;34(7):2096–2101. [DOI] [PubMed] [Google Scholar]
- 90. Zimmerer A, Ramoser A, Streit M, et al. Osteoarthrosis, advanced age, and female sex are risk factors for inferior outcomes after hip arthroscopy and labral debridement for femoroacetabular impingement syndrome: case series with minimum 10-year follow-up. Arthroscopy. 2021;37(6):1822–1828. [DOI] [PubMed] [Google Scholar]
- 91. Zusmanovich M, Haselman W, Serrano B, Banffy M. The incidence of hip arthroscopy in patients with femoroacetabular impingement syndrome and labral pathology increased by 85% between 2011 and 2018 in the United States. Arthroscopy. 2022;38(1):82–87. [DOI] [PubMed] [Google Scholar]