Abstract
Background: Chronic constipation is a common health concern. Defecatory disorders are considered one of the mechanisms of chronic idiopathic constipation. This study aimed to evaluate the effect of concurrent irritable bowel syndrome (IBS) on the success rate and response to biofeedback therapy in patients with chronic constipation and pelvic floor dyssynergia (PFD).
Methods: This prospective cohort study was performed at the Imam Khomeini Hospital Complex in Tehran from October 2020 to July 2021. Patients aged 18–70 years with chronic constipation and PFD confirmed by clinical examination, anorectal manometry, balloon expulsion test, and/or defecography were included. All patients failed to respond to treatment with lifestyle modifications and laxative use. The diagnosis of IBS was based on the ROME IV criteria. Biofeedback was educated and recommended to all patients. We used three different metrics to assess the patient’s response to biofeedback: 1) constipation score (questionnaire), 2) lifestyle score (questionnaire), and 3) manometry findings (gastroenterologist report).
Results: Forty patients were included in the final analysis, of which 7 men (17.5%) and 21 (52.2%) had IBS. The mean age of the study population was 37.7 ± 11.4. The average resting pressure decreased in response to treatment; however, this decrease was statistically significant only in non-IBS patients (P = 0.007). Patients with and without IBS showed an increase in the percentage of anal sphincter relaxation in response to treatment, but this difference was not statistically significant. Although the first sensation decreased in both groups, this decrease was not statistically significant. Overall, the clinical response was the same across IBS and non-IBS patients, but constipation and lifestyle scores decreased significantly in both groups of patients with and without IBS (P < 0.001).
Conclusion: Biofeedback treatment appears to improve the clinical condition and quality of life of patients with PFD. Considering that a better effect of biofeedback in correcting some manometric parameters has been seen in patients with IBS, it seems that paying attention to the association between these two diseases can be helpful in deciding on treatment.
Keywords: Biofeedback treatment, Pelvic floor dyssynergia, Irritable bowel syndrome, Treatment, Anal resting pressure, Anal sphincter relaxation
Introduction
Pelvic floor disorders can have different manifestations, the most important of which are defecation disorders, urinary disorders, sexual dysfunction, pelvic organ prolapse, and chronic pain. Chronic constipation is one of the most common gastrointestinal complaints in the community, which has a high economic burden.1 Although chronic constipation may have multiple etiologies, neurological diseases (multiple sclerosis, Parkinson’s, Hirschsprung), non-neurological diseases (hypothyroidism, diabetes, pregnancy, systemic sclerosis, electrolyte disorders), and medications contribute to a minority of etiologies, with chronic idiopathic constipation accounting for the majority of cases. Two of the most common etiologies are constipation-dominant irritable bowel syndrome (IBS) and pelvic floor dyssynergia (PFD). PFD is one of the idiopathic causes of chronic constipation. Pelvic floor structures for proper functioning require healthy anatomical structures, including muscles, connective tissue, and nerves, as well as proper functioning of the central nervous system.2
Pelvic floor disorders can have different manifestations, the most important of which are defecation disorders, urinary disorders, sexual dysfunction, pelvic organ prolapse, and chronic pain.3 The prevalence of this disorder is higher in women than men.4 Most patient with this type of constipation have difficulty to evacuate, even with soft stool. Using digital maneuvers, pelvic support, vaginal digital support for defecation, prolonged sitting in the toilet and straining, feeling of incomplete evacuation are the frequent symptoms of these patients. These disorders have been reported to be associated with depression and anxiety.5 Studies show that there is a strong association between the severity of depression and anxiety and the severity of symptoms of pelvic floor disorders.6 Various treatment methods have been proposed to correct the excretory disorders caused by pelvic floor dyssynergy. These methods include non-surgical methods including lifestyle modification through physical activity and proper diet, medication and biofeedback.2
In cases of persistent symptoms or severe anatomical disturbance, surgical treatments could be indicated.2 A group of patients may also need reoperation.7 Recent research shows that the effect of biofeedback in the treatment of PFD is greater than other treatments 2,8 and in some studies it is even recommended as the first line of treatment.9 On the other hand, not only are the effects of biofeedback greater than other methods, but these effects remain longer.10,11 Recent studies show that more than half of patients with defecation disorders due to PFD experience long-term improvement with biofeedback.12
IBS is another cause of chronic constipation. A large number of researchers and physicians believe that there is an overlap between IBS and PFD.11 Manometric examinations in patients with IBS show that the prevalence of PFD is higher than normal population in this group of patients.13 This could indicate the importance and role of biofeedback in the treatment of IBS patients, as studies have shown that biofeedback can improve the symptoms of IBS.14 Conversely there are few researches evaluating the prevalence of IBS in patient with PFD. Given the challenges in the treatment of patients with PFD and the lack of access to biofeedback therapy for all patients, the appropriate selection of patients for referral and biofeedback can be helpful. In the present study, we aimed to evaluate the effects of the presence of IBS on the success rate and response to biofeedback therapy in patients with pelvic dyssynergia.
Materials and Methods
Study Design
This study was performed as a prospective cohort study. This study was carried out at the Imam Khomeini Hospital Complex in Tehran from October 2020 to July 2021 (approved by the medical research ethics committee at Tehran University of Medical Sciences (IRB Code: IR.TUMS.REC.1400.015).
Inclusion Criteria
Patients aged 18 to 70 with chronic constipation who have failed conservative management and lifestyle modification and were referred to our tertiary center for evaluation of their constipation were included. Clinical examination, anorectal manometry, a balloon expulsion test, and/or defecography are used to confirm PFD. All patients with a diagnosis of PFD were candidates for biofeedback.
Exclusion Criteria
Patients with age less than 18 years, age over 70 years, inability to cooperate properly for biofeedback, previous biofeedback history, opium and constipation medications, pregnancy, electrolyte disturbances, anemia, and a history of severe and incurable weight loss History of rectal bleeding, history of previous surgery in the gastrointestinal tract, pelvis, or spine (except appendectomy, cholecystectomy, and hysterectomy), presence of neurological diseases such as multiple sclerosis, Parkinson’s, stroke, spinal cord injury, and cognitive impairment Systemic diseases such as diabetes, hypothyroidism, chronic heart disease, and kidney disease were excluded.
Study Tools
The severity of constipation and quality of life were assessed based on the Wexner questionnaire (the constipation score ranges between 0 and 30, with 0 representing the absence of symptoms and 20 or 30 the most burdensome level of symptoms) and the PAC-QOL questionnaire for constipation. The Wexner Constipation Score and quality of life were the primary outcome measures. Changes in manometric values were a secondary outcome. Anorectal manometry was performed using a conventional water-perfused manometry system (MMS, Enschede, the Netherlands). PFD was based on Rao criteria. An abnormal manometric finding (inappropriate pelvic floor contraction or less than 20% relaxation of basal resting sphincter pressure with adequate propulsive forces during defecation), an abnormal balloon expulsion test (inability to expel a 50-mL water-filled balloon within 2 minutes), and an abnormal defecography or colon transit time were considered the presence of PFD. Office based Biofeedback therapy was done biweekly for six to eight sessions of at least one hour for each patient, working on both anal sphincter relaxation and improvement of propulsive forces. Values of manometry, Wexner, and the PAC-QOL questionnaire were measured before and after biofeedback. The presence of IBS was determined based on ROME IV criteria by the gastroenterologist. Data extraction from questionnaires is the responsibility of the medical resident and registered nurse, and the results were recorded after the approval of professors.
Biofeedback Technique
Training in Simulated Defecation definition: The purpose of this instruction is to educate the participant how to properly expel a fake stool in the laboratory. This technique is carried out by inserting a 50-mL water-filled balloon into the rectum or by employing a Fecom fake stool.15,16 The person is advised to lay and try defecation after the balloon is placed in the left lateral position. While attempting to pass the balloon, the individual is assisted and instructed on how to relax the pelvic floor muscles, adopt a proper posture, and employ suitable breathing methods. If the person is unable to evacuate the balloon, the balloon is gently towed to assist the patient’s efforts. The patient gradually learns how to synchronize the defecation instruction and release the balloon.
Sample Size
Sample size was calculated using logistic regression method. According to the results of logistic regression, a total of 54 patients were needed.
z tests - Logistic regression
Options: Large sample z-Test, Demidenko (2007) with var corr
Analysis: A priori: Compute required sample size
Input: Tail(s) = One
Odds ratio = 2.5
Pr(Y = 1|X = 1) H0 = 0.2
α err prob = 0.05
Power (1-β err prob) = 0.80
R2 other X = 0
X distribution = Normal
X parm μ = 0
X parm σ = 1
Output: Critical z = 1.6448536
Total sample size = 54
Actual power = 0.8000077
Statistical Analysis
SPSS version 26 was used to analyze the data. To assess normal distribution, the Kolmogorov-Smirnov test was utilized. The comparison of colonoscopic parameters was done by a paired t test (or Wilcoxon). An independent t test (or Mann-Whitney U) was used for comparing variables before and after treatment (independently). A P value of less than 5% is regarded as significant.
Results
In this study, 53 eligible patients were included. Due to COVID-19 pandemic conditions, 13 patients did not consent to continue the study due to the COVID-19 pandemic. Finally, 40 patients were included in the final analysis, of whom 7 men (17.5%) and 21 patients (52.2%) had IBS. The mean age of the study population was 37.711.4. Patients’ clinical parameters, including colonoscopic findings, lifestyle scores, and constipation, were recorded before and after exposure (Tables 1 and 2).
Table 1. Demographic data of the patients * .
| Demographic data | |
| Gender | |
| Male | 7 (17.5) |
| Female | 33 (82.5) |
| IBS | |
| No | 19 (47.5) |
| Yes | 21 (52.5) |
| Age | 37.7(11.4) |
| Lifestyle score before biofeedback | 71.93 (13.47) |
| Lifestyle score after biofeedback | 39.10 (10.77) |
| Constipation score before biofeedback | 17.50 (3.38) |
| Constipation score after biofeedback | 9.75 (2.49) |
*Nominal variables reported as number (%) and numerical variables reported as mean (SD).
Shapiro test was used to investigate the normal distribution of data, which was rejected according to P < 0.05, and non-parametric tests were used.
Table 2. Basic information of patients before and after biofeedback treatment .
| Mean±SD [Min – Max] | |
| Average anal resting pressure before biofeedback | 72.37 ± 22.63 [22 – 116] |
| Average anal resting pressure after biofeedback | 57.13 ± 21.44 [22 – 102] |
| Average intrarectal pressure increase before biofeedback | 60.20 ± 40.10 [6 – 241] |
| Average intrarectal pressure increase after biofeedback | 60.40 ± 38.49 [9 – 179] |
| Percent of relaxation pressure before biofeedback | 16.97 ± 16.50 [1 – 64] |
| Percent of relaxation pressure after biofeedback | 22.35 ± 21.51 [0 – 88] |
| First sensation before biofeedback | 112.83 ± 83.61 [13 – 358] |
| First sensation after biofeedback | 98.83 ± 77.06 [11 – 373] |
| Maximum tolerable Volume before biofeedback | 240.18 ± 115.93 [55 – 400] |
| Maximum tolerable Volume after biofeedback | 165.60 ± 102.31 [17 – 401] |
According to the results (Table 3), before starting treatment, a significant difference was found between patients’ first sensations based on their IBS status (P < 0.05). In fact, IBS patients had significantly fewer first sensations than non-IBS patients. After treatment, IBS patients had significantly lower first sensation and maximum tolerable volume than non-IBS patients (Table 4).
Table 3. Comparison between patients with and without IBS .
| IBS | Non-IBS | P value | |
| Average resting pressure anal before biofeedback | 68.86 ± 19.92 | 76.26 ± 25.27 | 0.301 |
| Average resting pressure anal after biofeedback | 57.95 ± 22.42 | 56.21 ± 20.86 | 0.801 |
| Average pressure increases before biofeedback | 64.33 ± 51.79 | 55.63 ± 21.50 | 0.509 |
| Average pressure increases after biofeedback | 65.38 ± 33.15 | 54.89 ± 43.91 | 0.395 |
| Percent of relaxation average before biofeedback | 16.14 ± 16.64 | 17.89 ± 16.75 | 0.740 |
| Percent of relaxation average after biofeedback | 18.00 ± 16.24 | 27.16 ± 25.75 | 0.181 |
| First sensation before biofeedback | 84.00 ± 65.45 | 144.68 ± 91.35 | 0.020 |
| First sensation after biofeedback | 76.62 ± 46.79 | 123.37 ± 96.04 | 0.044 |
| Maximum tolerable volume before biofeedback | 223.19 ± 117.70 | 258.95 ± 114.09 | 0.334 |
| Maximum tolerable volume after biofeedback | 131.05 ± 77.56 | 203.79 ± 114.29 | 0.023 |
| Lifestyle score before biofeedback | 72.33 ± 15.91 | 71.47 ± 10.58 | 0.849 |
| Lifestyle score after biofeedback | 37.95 ± 11.44 | 40.37 ± 10.12 | 0.480 |
| Constipation score before biofeedback | 18.38 ± 3.52 | 16.53 ± 3.00 | 0.085 |
| Constipation score after biofeedback | 9.90 ± 2.36 | 9.58 ± 2.69 | 0.687 |
Table 4. Comparison of manometric and therapeutic parameters before and after treatment in the two groups of patients .
| Non–IBS* | P value | IBS | P value | |
| Average resting pressure anal before | 76.3 ± 25.30 | 0.007 | 68.9 ± 19.90 | 0.07 |
| Average resting pressure anal after | 56.2 ± 20.9 | 58.0 ± 22.40 | ||
| Average pressure increases before | 55.6 ± 21.5 | 0.94 | 64.3 ± 51.80 | 0.93 |
| Average pressure increases after | 54.9 ± 43.90 | 65.4 ± 33.2 | ||
| Percent of relaxation average before | 17.9 ± 16.80 | 0.15 | 16.1 ± 16.60 | 0.49 |
| Percent of relaxation average after | 27.2 ± 25.80 | 18.0 ± 16.20 | ||
| First sensation before | 144.7 ± 91.40 | 0.52 | 84.0 ± 65.50 | 0.56 |
| First sensation after | 123.4 ± 96.00 | 76.6 ± 46.80 | ||
| Maximum tolerable volume before | 258.9 ± 114.10 | 0.10 | 223.2 ± 117.70 | 0.006 |
| Maximum tolerable volume after | 203.8 ± 114.30 | 131.0 ± 77.60 | ||
| Lifestyle score before | 71.5 ± 10.60 | < 0.001 | 72.3 ± 15.90 | < 0.001 |
| Lifestyle score after | 40.4 ± 10.10 | 38.0 ± 11.40 | ||
| Constipation score before | 16.5 ± 3.00 | < 0.001 | 18.4 ± 3.50 | < 0.001 |
| Constipation score after | 9.6 ± 2.70 | 9.9 ± 2.40 |
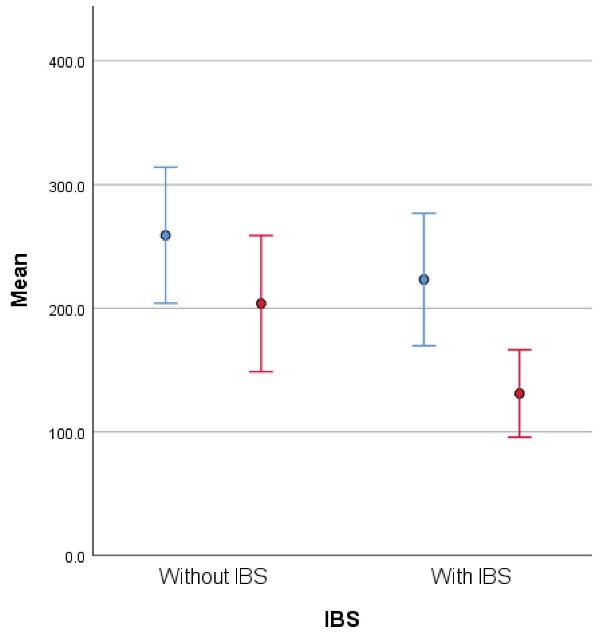
* Mean ± SD
Average resting pressure decreases (Figure 1) in response to treatment, but this decrease is statistically significant only in non-IBS patients (P = 0.007). The average increase in intrarectal pressure during the push test was not significantly different in both groups of patients (Figure 2). Both groups of patients with and without IBS showed an increase in the percent of anal sphincter relaxation in response to treatment, but this difference was not statistically significant (Figure 3). Although the first sensation decreased in both groups of patients, this decrease was not statistically significant (Figure 4). Max tolerable volume decreased modestly in patients with IBS, but in non-IBS patients, this difference was not significant (Figure 5). Lifestyle and constipation scores decreased significantly in both groups of patients with and without IBS (P < 0.001) (Figures 6 and 7).
Figure 1.
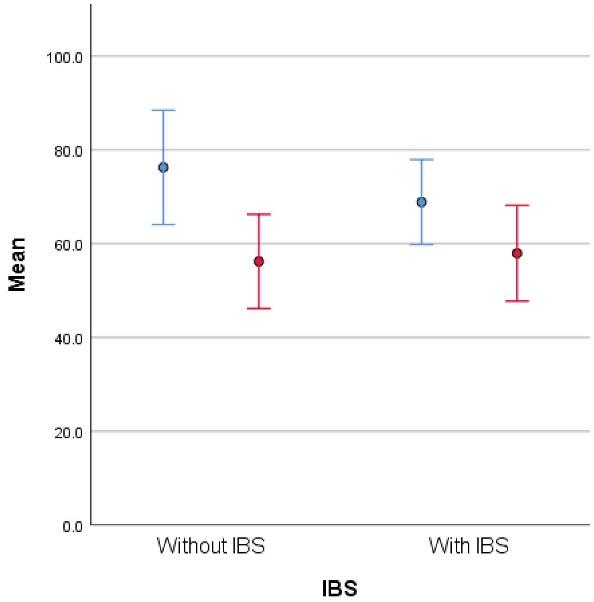
Average resting pressure before (blue) and after (red) treatment in two groups of patients
Figure 2.
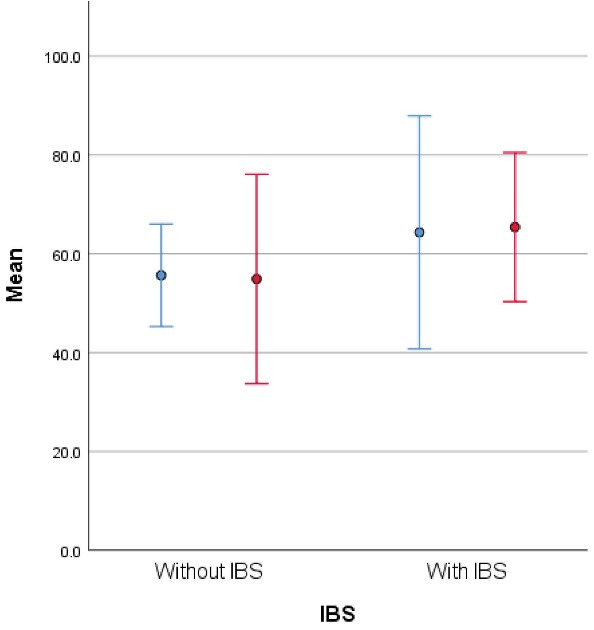
Average pressure increase before (blue) and after (red) treatment in two groups of patients
Figure 3.
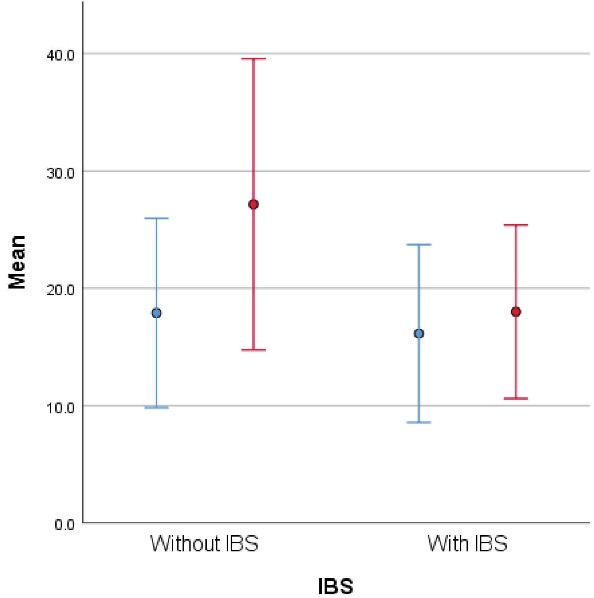
Percent of relaxation before (blue) and after (red) treatment in two groups of patients
Figure 4.
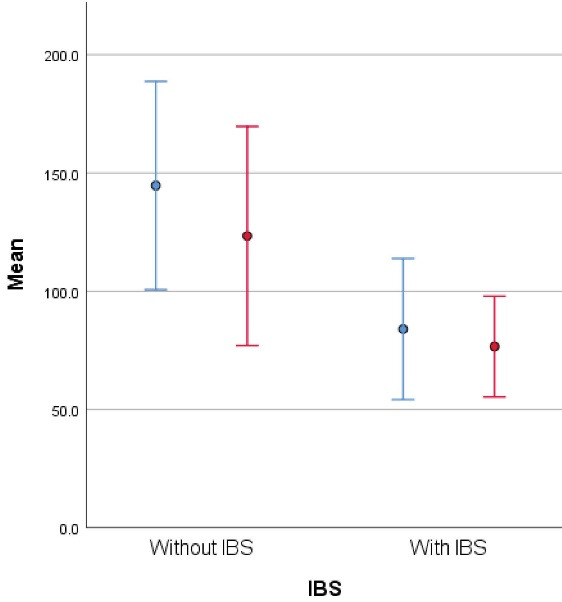
First sensation before (blue) and after (red) treatment in two groups of patients
Figure 5.
Max tolerable volume before (blue) and after (red) treatment in two groups of patients
Figure 6.
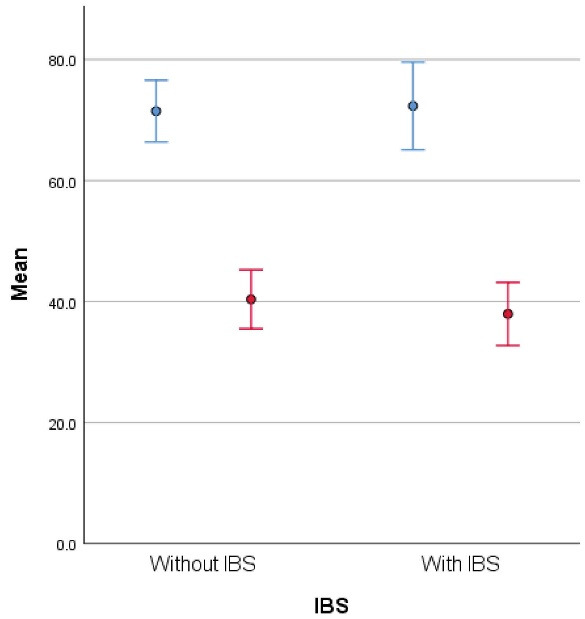
Lifestyle score before (blue) and after (red) treatment in two groups of patients
Figure 7.
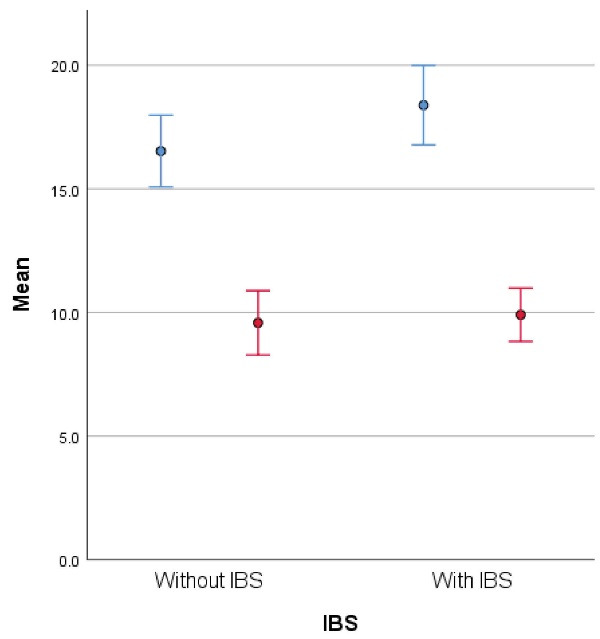
Constipation score before (blue) and after (red) treatment in two groups of patients
In the comparison of the amount of change in secondary outcome measures with non-IBS, it appeared that no difference was observed in the comparison of change variables between IBS and non-IBS, (Mann-Whitney U test) (Table 5).
Table 5. IBS vs non-IBS (after biofeedback) .
| Non–IBS | IBS | P value | |||||
| Median | Q1 | Q3 | Median | Q1 | Q3 | ||
| Change in resting LES | -27.00 | -44.00 | -4.00 | -11.00 | -34.00 | 4.00 | 0.233 |
| Change in average pressure increase | -8.00 | -37.00 | 25.00 | 6.00 | -16.00 | 24.00 | 0.386 |
| Change in percent of relaxation | 1.00 | -8.00 | 31.00 | 1.00 | -7.00 | 9.00 | 0.655 |
| Change in first sensation | -36.00 | -85.00 | 1.00 | .00 | -36.00 | 21.00 | 0.104 |
| Change in maximum tolerable volume | -15.00 | -164.00 | 28.00 | -48.00 | -193.00 | .00 | 0.448 |
| Change in lifestyle score | -33.00 | -40.00 | -26.00 | -37.00 | -43.00 | -24.00 | 0.357 |
| Change in constipation score | -7.00 | -8.00 | -6.00 | -9.00 | -11.00 | -6.00 | 0.136 |
Discussion
Chronic constipation is one of the most common gastrointestinal complaints in the community, which has high economic costs.1 PFD is one of the main causes of idiopathic chronic constipation, and biofeedback therapy is known to be an effective treatment for this disorder. The efficacy of biofeedback therapy in this disorder is between 44 and 100%.17 Biofeedback efficacy, on the other hand, was reported to be 64% to 69% in the majority of constipated PFD.18 In addition, it is reported that most patients, after biofeedback sessions, relive more than two-thirds of their symptoms.19 However, it should be noted that the effectiveness of biofeedback should be considered based on timing (short- and long-term). Also, it seems necessary to answer the question of whether there is a recurrence of symptoms after biofeedback or not (and related risk factors).
Many patients with constipation have muscle dysfunction and bowel dysfunction (such as constipation due to IBS). They would have been treated for a long time, such as taking laxatives, which have not been of much use to them and even cause damage to the nervous system and spontaneous regulation of the intestine. It is supposed that, these patients would respond well to treatment of constipation with biofeedback. Treatment of constipation with biofeedback usually involves the rehabilitation of the muscles involved in defecation and emptying the large intestine. These methods are taught to the patient and after a short time the patient will be able to return his bowel movements to normal. Most people who have been treated with this method are satisfied with it. The aim of our study was to determine the effect of concurrent IBS on the response of patients with PFD to biofeedback treatment.
The results of our study showed that out of 40 patients with pelvic dyssynergia who were examined, 21 (52.2%) had IBS according to ROME IV criteria. Recent studies in Iran show that the overall prevalence of IBS varies between 1.1% and 25%.20 Therefore, due to the high prevalence of IBS in patients in our study, it is important to consider the presence of IBS in patients who are referred to evaluate PFD. Biofeedback therapy is an effective treatment method for improving clinical symptoms as well as quality of life in patients with PFD with and without IBS. The presence of IBS in these patients has not been a negative parameter for treatment response.
Patcharatrakul et al have evaluated the factors that may contribute to the biofeedback response and concluded that digital defecation maneuvers and lower baseline levels of bowel satisfaction were significantly important, but other factors such as demographic data, constipation symptoms, and manometric and sensory parameters were not effective factors in the treatment response.11,21 To our knowledge, limited studies have been performed evaluating the efficacy of biofeedback in the presence of IBS. Obviously, IBS is a complex disorder that can adversely affect patients’ quality of life and performance. Again, Patcharatraku conducted a study in 2011 to evaluate the outcome of biofeedback therapy in patients with PFD with and without IBS, and similar to our study, they showed no difference in treatment response.11
Other studies, on the other hand, have looked at the effect of biofeedback treatment on IBS symptoms in patients and found significant improvements. A study by Dobbin et al22 found that for 61 patients with refractory IBS, biofeedback and hypnotherapy were equally effective in improving IBS symptom severity scores, total non-gastrointestinal symptom scores, and anxiety and depression scores within 24 weeks of follow-up. They suggested that biofeedback may be a more cost-effective option because it requires less expertise. Cadeddu et al23 treated biofeedback with trans-anal electrical stimulation for sustained improvement in bowel symptoms and anorectal function in people with constipation and dyssynergia disorder, while other treatments were largely ineffective. Gender was not significantly different in response to treatment.
Our study showed that biofeedback causes a significant decrease in two manometric parameters: maximum tolerable volume and resting anal pressure. Also, two clinical criteria were improved: the constipation score and the lifestyle score. The results of our study also revealed that in patients with IBS, biofeedback treatment can be associated with better results in some parameters. Clinically, these two manometric parameters are important in the pathophysiology of constipation in patients with PFD, and reduction of these two can play an important role in improving the patient’s symptoms.
Along with our study, many other studies confirm that biofeedback therapy is an appropriate strategy for patients with pelvic floor disorders (such as dyssynergy). Jamshidi et al24 studied the treatment with biofeedback and its combination with laxatives, the results of which showed that the satisfaction with the treatment was highest in the groups of 60.83% biofeedback, 46.88% biofeedback plus psyllium, and 41.32% biofeedback plus polyethylene glycol. Difficulty emptying and returning to the toilet after defecation was significantly improved in the biofeedback group. The results of our study also showed that biofeedback improved patients’ lifestyle scores and reduced constipation. The use of laxatives reduced strain during defecation and increased stool duration. The combination of laxatives with biofeedback does not offer significant therapeutic benefits. Because laxatives may cause dissatisfaction and incomplete or prolonged defecation in patients with pelvic floor dyssynergy, adding laxatives to the biofeedback diet is not recommended for these patients. Hite and Curran suggested that biofeedback therapy has been shown to be effective in improving chronic constipation and fecal incontinence. The evidence for the use of biofeedback in levator ani syndrome is contradictory. Comparing biofeedback with pelvic floor muscle training alone, studies show that biofeedback is a superior therapy.25 The results of a study by Patcharatrakul et al21 similar to our findings, suggest that biofeedback therapy is successful in more than 60% of patients with dyssynergic defecation. Patients who used finger maneuvers and patients who had lower baseline levels of bowel function satisfaction were more likely to succeed in treatment, while other factors were not associated with success. Biofeedback therapy should be provided to all patients with dyssynergic defecation, regardless of early symptoms or anorectal physiology findings.
Interestingly, the result of this study show that the first balloon sensation before biofeedback in patients with IBS is less than in non-IBS patients, which is consistent with the pathophysiology of IBS as these patients have a higher threshold of rectal sensation. However, biofeedback therapy did not result in significant changes in these patients’ first balloon sensation. The study after biofeedback showed that although this parameter was not significantly different in all patients, its rate in patients with IBS was significantly lower than that in non-IBS patients. This difference was also seen in the study of two different sexes. Changes in the maximum tolerable volume are other parameters that were significant in our study. Biofeedback caused a significant reduction in this parameter, which is considered a positive paraclinical response in patients’ recovery. This significant reduction was also seen in the comparison between patients with IBS and non-IBS patients.
Our findings suggest that biofeedback is not only effective as a standard treatment for PFD patients, but it also improves the clinical and manometric findings of dyssynergic IBS patients. Although these changes are not widespread, sub-findings of this study include differences between men and women in both IBS and non-IBS groups in response to biofeedback.
Limitation
The present study had several limitations. We did not consider body mass index before and after treatment. Another important point that was not adjusted in our study and is recommended to be considered in future studies is the severity of IBS, which can affect the response of patients. Also, we did not evaluate the effect of biofeedback on patients’ IBS symptoms. One of our limitations was the small number of men participating in the study, which will make it difficult to draw hard conclusions based on gender bias. But this limitation is inevitable due to the high prevalence of this disorder among women. It is recommended that appropriate gender mating be performed to address this issue. Finally, it is recommended that adherence to treatment be considered a factor that influences the results.
Conclusion
Biofeedback treatment seems to improve the clinical condition and quality of life of patients with PFD, both with and without dyssynergia. Considering the high prevalence of IBS in our study of dyssynergic patients, it seems necessary to evaluate all dyssynergic patients for the presence of IBS. In other words, patients with dyssynergia and IBS have the same treatment response and should not be excluded from biofeedback therapy. Further studies are mandatory to evaluate the effect of parameters that may interfere with the biofeedback treatment response.
Cite this article as: Alborzi Avanaki F, Rafiee S, Varpaei HA, Taher M, Aletaha N, Allameh F. Biofeedback treatment can improve clinical condition and quality of life in patients with pelvic floor dyssynergy with irritable bowel syndrome: A prospective cohort study. Middle East J Dig Dis 2023;15(1):45-52. doi: 10.34172/mejdd.2023.319.
Footnotes
Competing Interests
There is no conflict of interest to declare.
Data Availability Statement
The data used to support the findings of this study are available from the corresponding author upon request.
Disclosure
This article presents results obtained through the development of the medical residency Thesis of the Doctorate Program in internal medicine, Tehran University of Medical Sciences, Sara Rafiee Sevyeri, 2022.
Funding
This study did not receive any institutional funding.
References
- 1.Sweeney M. Constipation Diagnosis and treatment. Home Care Provid. 1997;2(5):250–5. doi: 10.1016/s1084-628x(97)90120-9. [DOI] [PubMed] [Google Scholar]
- 2.Jundt K, Peschers U, Kentenich H. The investigation and treatment of female pelvic floor dysfunction. DtschArztebl Int. 2015;112(33-34):564–74. doi: 10.3238/arztebl.2015.0564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arnouk A, De E, Rehfuss A, Cappadocia C, Dickson S, Lian F. Physical, complementary, and alternative medicine in the treatment of pelvic floor disorders. CurrUrol Rep. 2017;18(6):47. doi: 10.1007/s11934-017-0694-7. [DOI] [PubMed] [Google Scholar]
- 4.Bump RC, Norton PA. Epidemiology and natural history of pelvic floor dysfunction. ObstetGynecol Clin North Am. 1998;25(4):723–46. doi: 10.1016/s0889-8545(05)70039-5. [DOI] [PubMed] [Google Scholar]
- 5.Vrijens D, Berghmans B, Nieman F, van Os J, van Koeveringe G, Leue C. Prevalence of anxiety and depressive symptoms and their association with pelvic floor dysfunctions-a cross sectional cohort study at a pelvic care centre. NeurourolUrodyn. 2017;36(7):1816–23. doi: 10.1002/nau.23186. [DOI] [PubMed] [Google Scholar]
- 6.Khan ZA, Whittal C, Mansol S, Osborne LA, Reed P, Emery S. Effect of depression and anxiety on the success of pelvic floor muscle training for pelvic floor dysfunction. J ObstetGynaecol. 2013;33(7):710–4. doi: 10.3109/01443615.2013.813913. [DOI] [PubMed] [Google Scholar]
- 7.DeLancey JO. The hidden epidemic of pelvic floor dysfunction: achievable goals for improved prevention and treatment. Am J ObstetGynecol. 2005;192(5):1488–95. doi: 10.1016/j.ajog.2005.02.028. [DOI] [PubMed] [Google Scholar]
- 8.Koh CE, Young CJ, Young JM, Solomon MJ. Systematic review of randomized controlled trials of the effectiveness of biofeedback for pelvic floor dysfunction. Br J Surg. 2008;95(9):1079–87. doi: 10.1002/bjs.6303. [DOI] [PubMed] [Google Scholar]
- 9.Rao SS, Patcharatrakul T. Diagnosis and treatment of dyssynergic defecation. J NeurogastroenterolMotil. 2016;22(3):423–35. doi: 10.5056/jnm16060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chiarioni G, Whitehead WE, Pezza V, Morelli A, Bassotti G. Biofeedback is superior to laxatives for normal transit constipation due to pelvic floor dyssynergia. Gastroenterology. 2006;130(3):657–64. doi: 10.1053/j.gastro.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 11.Rao SS. What’s in a name? Putting patients first: biofeedback for irritable bowel syndrome patients with dyssynergic defecation. J Clin Gastroenterol. 2011;45(7):572–3. doi: 10.1097/MCG.0b013e3182192230. [DOI] [PubMed] [Google Scholar]
- 12.Narayanan SP, Bharucha AE. A practical guide to biofeedback therapy for pelvic floor disorders. Curr Gastroenterol Rep. 2019;21(5):21. doi: 10.1007/s11894-019-0688-3. [DOI] [PubMed] [Google Scholar]
- 13.Patcharatrakul T, Gonlachanvit S. Outcome of biofeedback therapy in dyssynergic defecation patients with and without irritable bowel syndrome. J Clin Gastroenterol. 2011;45(7):593–8. doi: 10.1097/MCG.0b013e31820c6001. [DOI] [PubMed] [Google Scholar]
- 14.Ahadi T, Madjlesi F, Mahjoubi B, Mirzaei R, Forogh B, Daliri SS, et al. The effect of biofeedback therapy on dyssynergic constipation in patients with or without irritable bowel syndrome. J Res Med Sci. 2014;19(10):950–5. [PMC free article] [PubMed] [Google Scholar]
- 15.Rao SS, Welcher KD, Pelsang RE. Effects of biofeedback therapy on anorectal function in obstructive defecation. Dig Dis Sci. 1997;42(11):2197–205. doi: 10.1023/a:1018846113210. [DOI] [PubMed] [Google Scholar]
- 16.Rao SS, Seaton K, Miller M, Brown K, Nygaard I, Stumbo P, et al. Randomized controlled trial of biofeedback, sham feedback, and standard therapy for dyssynergic defecation. Clin Gastroenterol Hepatol. 2007;5(3):331–8. doi: 10.1016/j.cgh.2006.12.023. [DOI] [PubMed] [Google Scholar]
- 17.Heymen S, Jones KR, Scarlett Y, Whitehead WE. Biofeedback treatment of constipation: a critical review. Dis Colon Rectum. 2003;46(9):1208–17. doi: 10.1007/s10350-004-6717-8. [DOI] [PubMed] [Google Scholar]
- 18.Koutsomanis D, Lennard-Jones JE, Roy AJ, Kamm MA. Controlled randomised trial of visual biofeedback versus muscle training without a visual display for intractable constipation. Gut. 1995;37(1):95–9. doi: 10.1136/gut.37.1.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lee BH, Kim N, Kang SB, Kim SY, Lee KH, Im BY, et al. The long-term clinical efficacy of biofeedback therapy for patients with constipation or fecal incontinence. J NeurogastroenterolMotil. 2010;16(2):177–85. doi: 10.5056/jnm.2010.16.2.177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jahangiri P, Hashemi Jazi MS, Hassanzadeh Keshteli A, Sadeghpour S, Amini E, Adibi P. Irritable bowel syndrome in Iran: SEPAHAN systematic review No. 1. Int J Prev Med. 2012;3(Suppl 1):S1–9. [PMC free article] [PubMed] [Google Scholar]
- 21.Patcharatrakul T, Valestin J, Schmeltz A, Schulze K, Rao SSC. Factors associated with response to biofeedback therapy for dyssynergic defecation. Clin Gastroenterol Hepatol. 2018;16(5):715–21. doi: 10.1016/j.cgh.2017.10.027. [DOI] [PubMed] [Google Scholar]
- 22.Dobbin A, Dobbin J, Ross SC, Graham C, Ford MJ. Randomised controlled trial of brief intervention with biofeedback and hypnotherapy in patients with refractory irritable bowel syndrome. J R Coll Physicians Edinb. 2013;43(1):15–23. doi: 10.4997/jrcpe.2013.104. [DOI] [PubMed] [Google Scholar]
- 23.Cadeddu F, Salis F, De Luca E, Ciangola I, Milito G. Efficacy of biofeedback plus transanal stimulation in the management of pelvic floor dyssynergia: a randomized trial. Tech Coloproctol. 2015;19(6):333–8. doi: 10.1007/s10151-015-1292-7. [DOI] [PubMed] [Google Scholar]
- 24.Jamshidi MS, Malekpour H, Abdi S, Farhan F. Biofeedback, biofeedback plus fiber laxative, and biofeedback plus osmotic laxative regimens to treat constipation in patients with pelvic floor dyssynergia: a randomized controlled trial. Indian J Gastroenterol. 2022;41(2):160–8. doi: 10.1007/s12664-021-01189-1. [DOI] [PubMed] [Google Scholar]
- 25.Hite M, Curran T. Biofeedback for pelvic floor disorders. Clin Colon Rectal Surg. 2021;34(1):56–61. doi: 10.1055/s-0040-1714287. [DOI] [PMC free article] [PubMed] [Google Scholar]


