Abstract
This case describes a rare clinical situation of chylous ascites due to lymphatic obstruction in the setting of small bowel volvulus. A 32-year-old man presented with acute onset abdominal pain in the preceding 3 hours, associated with nausea and vomiting. He underwent a computed tomography (CT) scan which was concerning for an internal hernia involving the small bowel. On subsequent laparoscopy, milky fluid suggestive of chyle was found within the pelvis, along with a torted segment of the small bowel. The bowel was gently reduced with ease using atraumatic laparoscopic graspers. On closer examination, the mesenteric border of the torted small bowel had a white edge suggestive of lymphatic build-up. This case report highlights the pertinent clinical features associated with this clinical scenario, important for the laparoscopic gastrointestinal surgeon.
Keywords: Laparoscopy, Small bowel obstruction, Chyle, Peritonitis, Volvulus
Introduction
The presence of chyle within the peritoneal cavity is an uncommon finding and surgeons need to be aware of the potential differential diagnoses to properly evaluate the abdomen. We present a rare cause of chylous ascites due to lymphatic obstruction seen with a small intestine volvulus, which thus far has only been described in a handful of case reports.
Case Report
A 32-year-old man presented to our Emergency Department with acute onset abdominal pain over the preceding 3 hours. This was associated with nausea and vomiting. His last bowel motion was earlier in the day and he was still passing wind. He had no history of abdominal surgery and was not on any regular medications. He was a daily cannabis and cigarette smoker. On examination, his vital signs were within normal ranges and he was afebrile. He was tender in the upper abdominal region but was soft without any peritoneal features. His white cell count was elevated at 13.8 × 109/L and a lactate of 2.5 mmoL/L. A computed tomography (CT) scan was performed, which suggested an internal hernia involving the small intestine.
The patient was taken urgently for diagnostic laparoscopy. A 10 mm vertical umbilical incision was made for safe insertion of the laparoscope, followed by 5 mm incisions made in the left lower quadrant and suprapubic. On the introduction of the laparoscopy, milky white fluid was observed sitting in the pelvis, suggestive of chyle (Figure 1). This was aspirated and sent for analysis. This white fluid was also noted sitting between loops of the small intestine throughout the peritoneal cavity. Assessment of the small intestine revealed a segment of the ileum torted as a volvulus, rather than the presence of an internal hernia. This was easily reduced using gentle traction with atraumatic laparoscopic graspers. Although the small intestine appeared a little dusky, it improved on colour on detorsion and displayed peristaltic behaviour. On closer examination of the small intestine, the mesenteric border had a white appearance suggesting lymph congestion (Figure 2). The rest of the diagnostic laparoscopy was unremarkable. The peritoneal cavity was extensively lavaged until the return fluid was clear.
Figure 1.
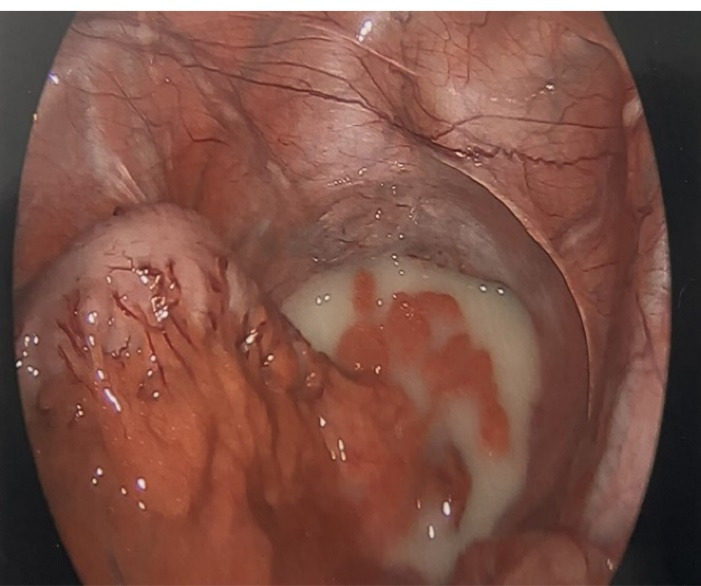
Laparoscopic view looking into the pelvis, with sigmoid colon on left side of the image. Chyle is observed sitting within the pelvic cavity.
Figure 2.
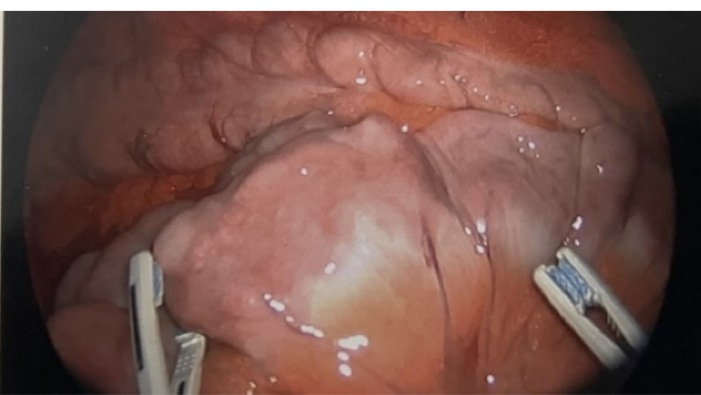
Small bowel segment with white haze along the mesenteric border, representing lymphatic congestion.
The patient was well the following day, tolerating a normal diet and was discharged from the hospital on the second postoperative day. Analysis of the peritoneal fluid revealed a high triglyceride level of 360 mg/dL. His follow-up one month later revealed no ongoing issue and he had recovered well from his operation.
Discussion
Chylous ascites are an uncommon finding on laparoscopy, but when present, the surgeon needs to be aware of the potential pathologies associated with it. Chyle is confirmed when the triglyceride level of the abdominal fluid is greater than 200 mg/dL.1,2 Important differentials to consider of yellow-white fluid within the peritoneal cavity include pseudochyle which describes fluid which is milky due to admixture with pus; and chyliform ascites which describes lecithin-rich peritoneal fluid due to fatty degeneration of cells.3
The mechanisms leading to chylous ascites are due to disruption of lymphatic channels, either due to2-4:
Direct injury to the thoracic duct and/or other lymphatic channels. This can be either be as a complication of other abdominal surgery, or a traumatic abdominal injury.
Obstruction of lymphatic channels. This occurs in the setting of malignancy, especially with lymphoma, or volvulus of the intestinal mesentery.
Infection; the most common being peritoneal tuberculosis or filariasis.
Congenital lymphatic abnormalities.
Cirrhosis, which leads to increased production of hepatic lymph.
Importantly, the surgeon must be aware that chylous ascites represent the presence of an underlying disease, rather than a condition of its own, and the management priorities need to be focussed on determining and treating this underlying aetiology.
Small bowel volvulus has been described in a number of case reports as a cause of chylous ascites.5-8 The torsion on the small bowel mesentery closes off lymphatic channels, increasing the pressure of lymph within these channels. This may either cause exudation of lymph or rupture of small lymphatic channels. However, chylous ascites are only rarely observed with small bowel volvulus, suggesting that some individuals may have an inherent weakness in their lymphatic channels leading to the formation of chylous ascites.9
Cite this article as: Gupta S, Mundasad B. Chylous ascites associated with small bowel volvulus: case report on a laparoscopic diagnosis. Middle East J Dig Dis 2023;15(2):139-140. doi: 10.34172/mejdd.2023.334.
Footnotes
Authors’ Contribution
Conceptualization: Saksham Gupta.
Data curation: Saksham Gupta.
Formal analysis: Saksham Gupta.
Funding acquisition: Saksham Gupta.
Investigation: Saksham Gupta.
Methodology: Saksham Gupta.
Project administration: Saksham Gupta.
Resources: Saksham Gupta.
Supervision: Basavaraj Mundasad.
Validation: Saksham Gupta.
Visualization: Saksham Gupta.
Writing – original draft: Saksham Gupta.
Writing – review & editing: Basavaraj Mundasad.
Competing Interests
The authors declare no conflict of interest related to this work.
Ethical Approval
Informed consent was taken from the patient prior to submission for publication
References
- 1.Bhardwaj R, Vaziri H, Gautam A, Ballesteros E, Karimeddini D, Wu GY. Chylous ascites: a review of pathogenesis, diagnosis and treatment. J Clin Transl Hepatol. 2018;6(1):105–13. doi: 10.14218/jcth.2017.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lizaola B, Bonder A, Trivedi HD, Tapper EB, Cardenas A. Review article: the diagnostic approach and current management of chylous ascites. Aliment PharmacolTher. 2017;46(9):816–24. doi: 10.1111/apt.14284. [DOI] [PubMed] [Google Scholar]
- 3.Murugan K, Spence RA. Chylous peritonitis with small bowel obstruction. Ulster Med J. 2008;77(2):132–3. [PMC free article] [PubMed] [Google Scholar]
- 4.Al-Busafi SA, Ghali P, Deschênes M, Wong P. Chylous ascites: evaluation and management. ISRN Hepatol. 2014;2014:240473. doi: 10.1155/2014/240473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pai A, Park JJ, Marecik SJ, Prasad LM. Midgut volvulus presenting with acute chylous peritonitis. Clin Case Rep. 2014;2(4):159–61. doi: 10.1002/ccr3.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayama T, Shioya T, Hankyo M, Shimizu T, Shibuya H, Komine O, et al. Primary volvulus of the small intestine exhibiting chylous ascites: a case report. J Nippon Med Sch. 2017;84(2):83–6. doi: 10.1272/jnms.84.83. [DOI] [PubMed] [Google Scholar]
- 7.Leaning M. Chylous ascites as a sequelae of primary small bowel volvulus in a virgin abdomen. J Surg Case Rep. 2021;2021(5):rjab176. doi: 10.1093/jscr/rjab176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akama Y, Shimizu T, Fujita I, Kanazawa Y, Kakinuma D, Kanno H, et al. Chylous ascites associated with intestinal obstruction from volvulus due to Petersen’s hernia: report of a case. Surg Case Rep. 2016;2(1):77. doi: 10.1186/s40792-016-0207-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pai A, Park JJ, Marecik SJ, Prasad LM. Midgut volvulus presenting with acute chylous peritonitis. Clin Case Rep. 2014;2(4):159–61. doi: 10.1002/ccr3.88. [DOI] [PMC free article] [PubMed] [Google Scholar]


