Abstract
Injuries are the leading cause of death for American children, killing over 11,000 children in 2017. They are also a rapidly increasing public health challenge globally: The World Health Organization ranks injury as the leading cause of death globally for children Ages 5 to 18 years, and the Global Burden of Diseases project estimates over 2 million children Ages 0 to 19 years died from injuries worldwide in 2017. Unintentional injuries, sometimes referred to as “accidents” by the lay public, are generally preventable, and psychological science has much to offer in societal efforts to develop, evaluate, implement, and disseminate effective prevention strategies. I first discuss the multifaceted causes of child injuries, which can be conceptualized using classic psychological theory, such as Bronfenbrenner’s ecological theory, or classic injury prevention theory, such as the Haddon Matrix. In either case, behavioral risks stem from the child’s developmentally influenced decisions and behaviors; the child’s family, social, and physical contexts; and the child’s broader cultural environments. Risks can also be conceptualized temporally, through behavioral analysis such as antecedents, behaviors, and consequences of the injury. I then present examples of behaviorally focused interventions that target the child, the adult supervisor, and the environment. In each case, I consider psychological risk factors present and the theory-based strategies that might interrupt or alter risk pathways to prevent injury events. I close with comments on the scope of injury as a global public health challenge and the central role psychologists can and should play to reduce the burden of child injury on the world’s population.
Keywords: injury, safety, prevention, psychological science, public health
Injuries are the leading cause of death for American children, killing over 11,000 children in 2017, the equivalent of 32 deaths per day (Centers for Disease Control and Prevention, 2019). Nonfatal injuries, which have enormous impact on the emotional and financial health of families, are far more common: Over 6.7 million children were treated in U.S. emergency departments in 2017, equal to 18,603 per day and almost 13 children per minute. The Centers for Disease Control and Prevention (2019) estimates a financial toll of fatal and nonfatal child injuries combined to exceed $96 billion annually.
Of course, injuries are not just an American phenomenon. As global societies address and overcome the public health challenges of communicable and infectious diseases, the role of injury as a pediatric health challenge is rapidly accelerating. The World Health Organization (2018) now ranks injury as the leading cause of death globally for children Ages 5 to 18, with the burden falling disproportionately on the poor and disadvantaged, both within and across countries. Over 95% of global child injury deaths occur in low- and middle-income countries (World Health Organization, 2008); the Global Burden of Diseases project estimates over 2 million children Ages 0 to 19 died worldwide in 2017 from injury, equivalent to 5,581 child deaths per day and almost four per minute. The human toll of such loss is troubling (Schwebel, 2008): Every 15 s, every day of every year, a set of parents loses their child and the world loses a young and promising life, one with long-term potential for productivity, companionship, and contribution to our collective well-being.
Injuries are traditionally subdivided into those that are intentionally caused (e.g., through suicide, homicide, or abuse) versus those that are unintentional. Recognizing the demarcation line is fuzzy (Peterson & Brown, 1994), I focus herein primarily on injuries that are unintentional rather than those that are purposively caused by the victim or by other perpetrators. The lay pubic may consider such injuries as “accidental” (Girasek, 2001; Morrongiello & Dayler, 1996; Peterson, Farmer, & Kashani, 1990), but behavioral scientists recognize preventive measures can be taken and instead use the descriptor “unintentional.”
Theoretical Basis of Injury Risk
As early as the 1930s, behavioral scientists began working to understand why some children might experience unintentional injuries more often than others (e.g., Dunbar, Wolfe, & Rioch, 1939; Marbe, 1935). Building from existing literature in industrial and traffic safety, “accident prone” characteristics of children were outlined, referring to a combination of what we might characterize today as motor development, cognitive development, and temperamental factors. Landmark epidemiological and longitudinal studies from the 1960s through the 1990s clarified the picture (e.g., Bijur, Golding, Haslum, & Kurzon, 1988; Bijur, StewartBrown, & Butler, 1986; Langley, Silva, & Williams, 1980; Manheimer & Mellinger, 1967; Matheny, Brown, & Wilson, 1971; Pulkkinen, 1995), leading to today’s understanding that injuries are caused by a complex set of intrapersonal, interpersonal, and environmental factors (Morrongiello, 2005; Schwebel & Barton, 2005).
Theoretically, we can conceptualize this multifaceted set of risks from a number of perspectives. Developmental psychologists might first point to Bronfenbrenner’s ecological model, which illustrates concentric layers of influence on children’s development extending from the individual him- or herself to the family, school, community, and broader cultural, societal, and chronological factors (Bronfenbrenner, 1977, 1986). As shown in Figure 1, concentric “systems” in Bronfenbrenner’s model each contribute to children’s injury risk (Barton & Schwebel, 2007). At the microsystem level, the physical and social context of the home, school or childcare center, and other locations where children engage influence injury risk. As simple examples, ungated stairs, unlocked firearms, and uncovered medication bottles in the home readily present hazards to young children. These microsystems are connected through the mesosystem and influenced also by exosystems, such as the parents’ workplace. A training seminar on workplace safety for a child’s parent, for example, might lead to increased home safeguarding. More broadly, macrosystem influences such as culturally driven encouragement for risk taking (Schwebel, Brezausek, Ramey, & Ramey, 2005) and governmental policies on safety and injury prevention (Shaw & Ogolla, 2006) may influence risk. Of course, the child’s own behavior and functioning, often pictured at the core of the ecological model, will also influence risk.
Figure 1.
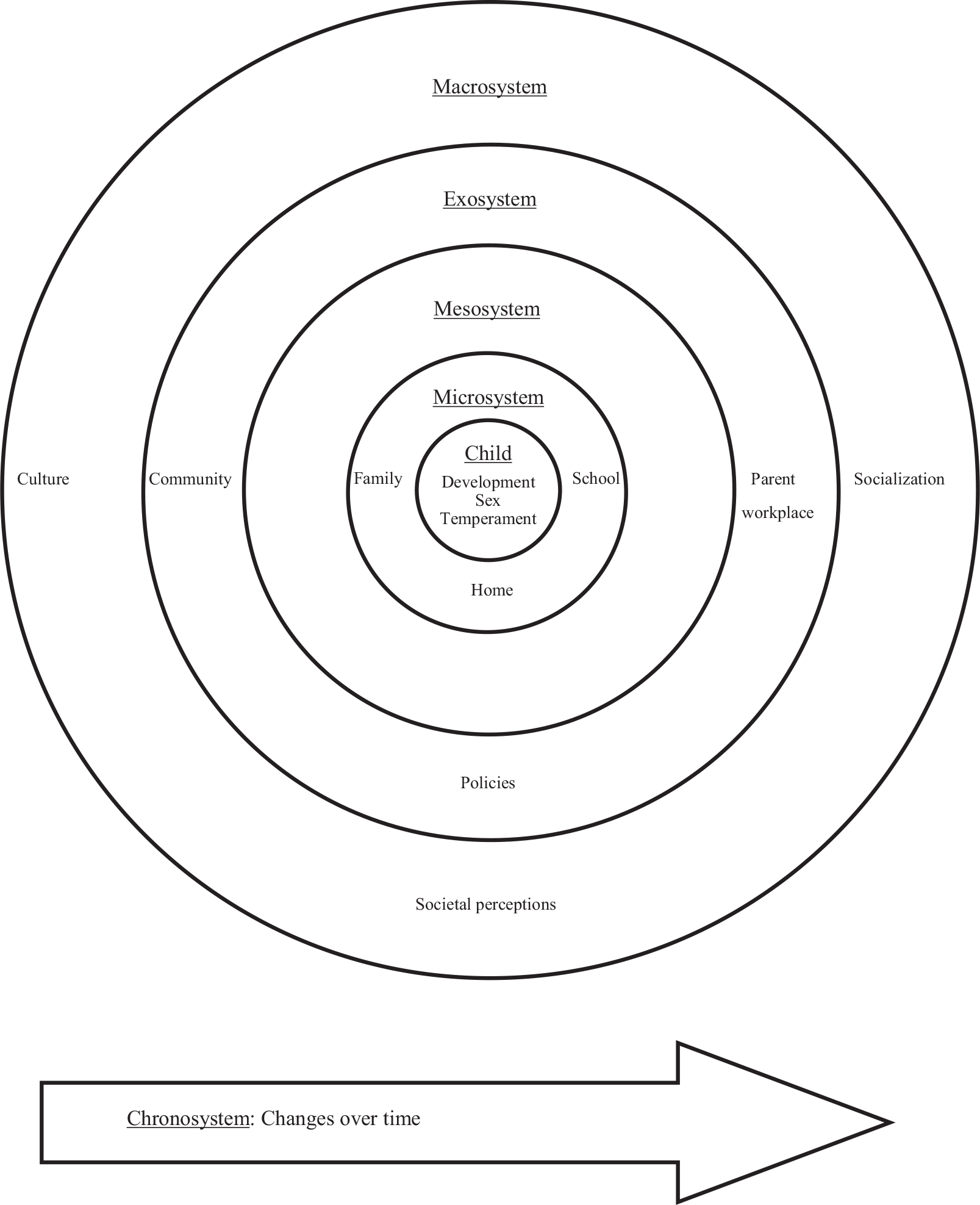
Bronfenbrenner ecological model, applied to child injury risk. Labels represent example influences but are not intended to be comprehensive.
Injury scientists may be less familiar with the Bronfenbrenner ecological model and instead would point to the Haddon Matrix. Originally developed by William Haddon in the late 1960s to describe the causes of automobile crashes (Haddon, 1968), Haddon later expanded the concept to describe all injury causes (e.g., Haddon, 1980). The Haddon Matrix is grounded in the basic physics of mechanical energy and crosses time (preinjury, injury, and postinjury) with environmental (human, vehicle/equipment) factors to consider how each cell of influences explains an injury event. Table 1 offers an example Haddon Matrix to describe risks for a child drowning event. As shown, influences are subdivided into those occurring prior to the injury (e.g., environmental hazards and child’s developmental comprehension of risk), during the injury (e.g., presence or absence of supervisors or lifeguards, design of the swimming area), and after the injury event (e.g., types of injuries, emergency response system).
Table 1.
Example of Haddon Matrix for a Toddler Drowning in a Pool
| Phase | Pre-event | Event | Postevent |
|---|---|---|---|
|
| |||
| Host (victim) | Lack of knowledge and comprehension regarding dangerous environment | Physical and structural characteristics of patients immature muscle coordination, limited muscle strength, and inability to surface and climb out of pool | Results of drowning on host (body injury): aspiration, hypoxia, and suffocation |
| Agent (vector) | Condition of vector and vehicle: pool filled with water (deep); no shallow area; pool not cleaned (particulate debris aspirated) | Design and structure of agent: floating devices in pool (to grab on to) | Results of fall into pool: traumatic injuries from fall into pool (fractures, head injury, and bleeding) |
| Environment: Physical (injury scene) | Hazards present: wet, slippery on edge of pool; no pool fencing; if fence, no lock on gate | Environmental designs: no shallow end, no stairs, no side rails to grab on to (pool visibility near housemotel lobby-walkway) | Method (means of response): 911, lights, visibility (so victim can be seen and possibly rescued) |
| Environment: Socioeconomic or sociocultural | Programs, legislative: restrictions on hours of use, locked gates | Socioeconomic effect on physical: lifeguards | Response systems: EMS, trauma systems, ED care, rehabilitation |
Note. Cells represent example influences but are not intended to be comprehensive. EMS = emergency medical services; ED = emergency department. From “Injury Prevention and Control in Children,” by S. E. Mace, M. J. Gerardi, A. M. Dietrich, S. R. Knazik, D. Mulligan-Smith, R. L. Sweeney, & C. R. Warden, 2001, Annals of Emergency Medicine, 38, p. 407. Copyright 2001 by Elsevier/American College of Emergency Physicians. Adapted with permission. The original article is available at https://www.sciencedirect.com/science/article/pii/S0196064401291562.
The Haddon Matrix’s subdivision of contributing factors into a Time × Factor matrix achieves a breakdown of possible prevention and mitigation points parallel to the breakdown offered by Bronfenbrenner’s ecological model. In both cases, we organize a highly complex set of multifaceted causes of injury events into contributing risk and protective factors. From an applied prevention perspective, we create opportunity to identify “low-hanging fruit” where an intervention might be possible and effective. In the case of swimming pool drowning risk, for example, this might be through improved adult supervision, redesign of the swimming pool area, or removal of environmental hazards.
One last point on the Haddon Matrix: Psychologists might recognize its parallels to classic behavioral psychology thinking, especially on the time axis. In fact, pioneering child injury psychologist Lizette Peterson outlined a “process analysis” to assess the behavioral and environmental antecedents to an injury, the stages of response to that injury, and then the consequences from the injury (Peterson, Farmer, & Mori, 1987). Sometimes abbreviated “antecedents, behaviors, and consequences,” a process analysis can be used to break down psychological and behavioral factors involved in preventing and mitigating injury events.
Conceptualizing Specific Risk Factors
Both ecological theory and the Haddon Matrix point to the confluence of multiple risk factors that together contribute to an individual injury event. Pessimists might grumble about the resulting complexity for prevention, but optimists could argue otherwise: With multiple contributing factors, there also are multiple opportunities to prevent each injury event. Interruption of just one pathway may yield success in prevention. For this reason, injury prevention is quite different from prevention of communicable disease. There is no single pill, like an antibiotic, to prevent the negative health outcome. Instead, more similar in some ways to cancer prevention, injury prevention must take many approaches, must be additive rather than fully preventative, and will, in many cases, achieve efficacy without tangible evidence of success.
Figure 2 conceptualizes specific risk factors that contribute to child injury risk. Divided into caregiver-based, child-based, and environment-based variables, plus broader sociocultural factors, the model spans cognitions (attitudes, perceptions, emotions), behaviors (risk taking), motivations, and individual differences. It incorporates the various environments a child may engage within and emphasizes the interactions between the multifaceted risks. It also points, of course, directly toward development of prevention programs through manipulation or alteration to any number of the causal pathways.
Figure 2.
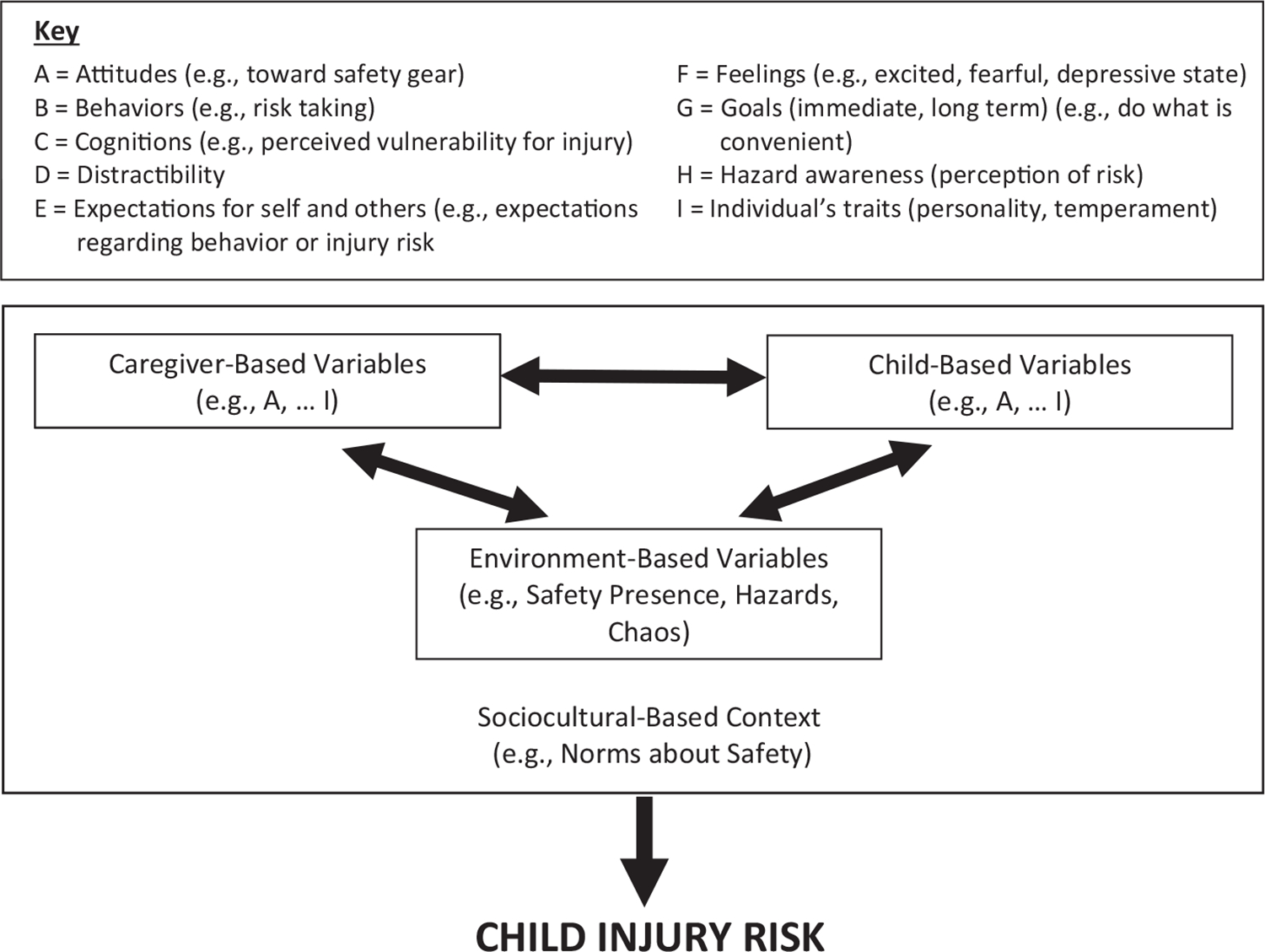
Conceptual model illustrating how interactions between child, caregiver, and environmental factors, which are shaped, directed and constrained by sociocultural context, jointly influence child injury risk. From “Caregiver Supervision and Child-Injury Risk: I. Issues in Defining and Measuring Supervision; II. Findings and Directions for Future Research,” by B. A. Morrongiello, 2005, Journal of Pediatric Psychology, 30 (p. 547). Copyright 2005 by Oxford University Press/Society of Pediatric Psychology. Adapted with permission.
I outline next several examples of interventions that reduce child injury from a behavioral perspective, organizing the presentation in parallel to Figure 2: interventions targeting the child, the adult supervisor, and the environments children experience. The examples are not designed to be comprehensive. Instead, I present these interventions as examples, with the acknowledgment also that many of society’s greatest injury prevention successes are not behavioral but rather are driven primarily by engineering science, policy making, and other strategies, or by synergistic collaboration between multidisciplinary experts—consider as examples the injuries prevented and the lives saved by child restraints for automobiles (car seats), smoke detectors, bicycle helmets, and playground surface installations.
Interventions Targeting the Child
Efforts to reduce child injury by altering the decisions or behaviors of the child must be closely grounded in developmental psychology theory, as the development of cognition, perception, motor skills, and social interactions are closely and inherently involved in risk-taking and risky behavior that could lead to injury. It would be pointless, for example, to try to teach a 4-year-old to cross a street safely, as requisite cognitive and perceptual skills would not yet be developed. Similarly, it would be wasteful to teach a typically developing 14-year-old not to consume laundry pods, as the relevant knowledge and skills to stay safe in this context should already be developed. Thus, most efforts to train children to keep themselves safe from injury target Vygotsky’s (1980) “zone of proximal development,” the developmental stage when children have the capacity to learn and engage in a particular behavior if they are properly trained to do so. Two domains where my laboratory and others have achieved success in helping children engage more safely in their environments through safer decisions and behaviors are detailed next, dog bite prevention and pedestrian safety.
Safe Engagement With Dogs
People often consider dogs to be safe and loved creatures that improve their mental and physical health, which is true, but dogs also are animals with animal instincts. Children’s engagement with dogs can lead to bites. Most often, this is because children engage with dogs in ways adults do not: Children are more likely than adults to misread dogs’ signals of when dogs want to play and when they want to be left alone; children may play with dogs’ food or toys; and children may touch dogs in the face, wake sleeping dogs, or taunt caged dogs (Meints, Brelsford, & de Keuster, 2018; Meints & de Keuster, 2009; Schwebel, Morrongiello, Davis, Stewart, & Bell, 2012). In many low- and middle-income countries (LMICs), child encounters with stray dogs are common; in high-income countries (HICs), and increasingly in middle-income countries, risks are more common among pet dogs, either in the child’s own home or in the home of friends and relatives. Recent epidemiological estimates place dog bite injuries among the top eight causes of child injury morbidity in the United States (Ballesteros, Williams, Mack, Simon, & Sleet, 2018).
From a behavioral perspective, toddlers and preschoolers face at least three cognitive challenges in engaging safely with dogs (Schwebel, Li, McClure, & Severson, 2016): (a) perspective taking/theory of mind—recognizing the dog’s perspective and engaging with the dog only when the dog may wish to play; (b) impulse control—inhibiting the child’s own desires and wishes when the dog has opposing desires and wishes; and (c) noticing details—recognizing subtle cues such as a wagging tail or perked ears that alert adults to the dog’s preferences, wishes, and emotions. Efforts to train children in the first two cognitive tasks—perspective taking and impulse control—are challenging and may be possible only as children grow older (Diamond & Lee, 2011; Knoll & Charman, 2000; McGregor, Whiten, & Blackburn, 1998; Rapport, Orban, Kofler, & Friedman, 2013). Efforts to train children to notice detailed cues of the dog’s preferences have been more successful and may be useful to reduce pediatric dog bite injury risk (Meints et al., 2018; Schwebel, Li, McClure, & Severson, 2016). Also successful are efforts to teach children basic rules about how and when to behave near dogs, thus overcoming cognitive development challenges by setting and enforcing firm rules that prevent risky behavior by circumventing cognitive developmental limitations (Dixon, Pomerantz, Hart, Lindsell, & Mahabee-Gittens, 2013; Lakestani & Donaldson, 2015; Meints et al., 2018; Meints & de Keuster, 2009; see Shen et al., 2017, for review).
As children grow older, risks with dogs progress with development. In middle childhood, risks tend to revolve around taunting behavior (e.g., playing aggressively or tauntingly with dogs, including strays) or around fearful behavior (e.g., running away from stray dogs, which can provoke attacks). Behavioral strategies to alter behavior must also be different, therefore. My laboratory’s intervention research in rural China, where stray dogs are prevalent on children’s walking routes to school, altered third- and fourth-graders’ safety through testimonial videos delivered by unknown peers, who told stories about their own experiences with dog bites and offered advice on how to avert injuries (Shen, Pang, & Schwebel, 2016). Grounded in health behavior change theory to (a) alter perceived vulnerability to injury, (b) change peer-based norms about appropriate behavior, and (c) provide basic education on safety and prevention, testimonial videos are an effective strategy to reduce injury risk among both children and adults (Hinyard & Kreuter, 2007).
Teaching Children Pedestrian Safety
Although adults complete it somewhat automatically, crossing a street is an immensely complex cognitive, perceptual, and motor task. Consider just a simple crossing at a two-lane bidirectional midblock location. The pedestrian must look left and judge the speed, distance, and acceleration–deceleration of the first car approaching. Very quickly, the pedestrian must also look right and judge the speed, distance, and acceleration–deceleration of the first car approaching from that direction. And the pedestrian must also consider the distance across the lanes of traffic and the speed with which she or he can cross that distance. Even this simple crossing requires multiple complex aspects of perception and cognition. Most street environments present complicating factors, however—curves, inclines, impediments to vision (e.g., parked cars, shrubbery), turning vehicles, additional lanes of traffic, and darkness, for example—and a safe and skilled pedestrian must process it all. It is not surprising, therefore, that children are vulnerable pedestrians, suffering over 450 deaths per year in the United States (Centers for Disease Control and Prevention, 2019) and over 80,000 globally (220 per day; Global Burden of Diseases, 2019).
Efforts to teach children to engage safely in traffic tend to focus on children Ages 7 to 10 (Schwebel, Barton, et al., 2014). Afterward, most experts suggest that children are safe pedestrians, although recent empirical evidence suggests adult skills to process traffic may not emerge fully until age 14 (O’Neal et al., 2018), and I have questioned whether the complexity of traffic globally, particularly in some LMICs, may require age limits to be modified according to local culture (Schwebel, 2017). Early influential research, conducted primarily in the United Kingdom, suggested that children exposed to repeated simulated roadside crossings and guided by an experienced adult gained safer skills in traffic (Thomson & Whelan, 1997; Tolmie et al., 2005; Whelan, Towner, Errington, & Powell, 2008). More recently, my laboratory and others have achieved similar results by training children to cross computer-generated virtual pedestrian street environments (Bart, Katz, Weiss, & Josman, 2008; Morrongiello, Corbett, Beer, & Koutsoulianos, 2018; Schwebel, Combs, Rodríguez, Severson, & Sisiopiku, 2016; Schwebel, McClure, & Severson, 2014; Schwebel, Wu, et al., 2018). We currently hypothesize that repeated crossing gives children the practice to develop the cognitive-perceptual skills required to cross streets (Schwebel, Shen, & McClure, 2016), although it remains unclear exactly how much training is required to achieve adult functioning (Schwebel, Severson, He, & McClure, 2017) and what individual differences may influence the speed and efficacy of training.
Interventions Targeting Adult Supervisors
Despite the many examples of successful injury prevention programs targeting children themselves, developmental limitations imply that adult supervisors will always remain critical to pediatric safety and injury prevention. Thus, a range of behavioral interventions have considered ways to improve the intensity, frequency, and quality of adult supervision of children in potentially risky locations (Morrongiello, 2018; Morrongiello, Ondejko, & Littlejohn, 2004; Petrass, Blitvich, & Finch, 2009).
Given the time parents spend with their children, parent supervision is the most logical target. The most successful efforts to alter parental behavior focus on change through health psychology theory behavior change mechanisms, including (a) helping parents recognize injuries are often preventable through their own actions, (b) boosting parents’ self-efficacy to take action to prevent their children’s injuries, and (c) increasing parents’ perception that their own children are vulnerable to injuries and that serious injuries could influence their own lives. The Supervising for Home Safety program, for example, accomplishes these goals through video presentations, group discussions, and experiential practice. It has repeatedly been demonstrated as effective in both individualized and group presentation formats (Morrongiello et al., 2017; Morrongiello, Sandomierski, Zdzieborski, & McCollam, 2012; Morrongiello, Zdzieborski, Sandomierski, & Munroe, 2013).
My laboratory has focused not on parents but rather on adult supervision in risky locations such as playgrounds and swimming pools, where supervision is provided by professionals. This line of research grew from early laboratory findings suggesting that children that take fewer risks when they know they are being watched; even a silent but present adult supervisor seems to inhibit children’s risk-taking tendencies (Schwebel & Bounds, 2003).
Building from this laboratory finding, my collaborators and I addressed the riskiest location at American preschools and childcare centers: the playground. Observations of preschool playgrounds suggested that the teachers—underpaid and fatigued from the intense work of supervising young children all day—used outdoor playground time as an opportunity for a break themselves, chatting and largely allowing the children to remain free. This is ironic, of course, because the majority of children’s injuries at preschools occur on the playground (Hashikawa, Newton, Cunningham, & Stevens, 2015). Efforts to admonish teachers and encourage higher quality supervision may help in the short term but are unlikely to prove helpful long term, so we devised a behavioral strategy, the Stamp in Safety program, to positively encourage teachers to engage with children and reduce child injury risks. The program is deceptively simple. Children wear nametag stickers, similar to what one might wear at a cocktail party. Teachers carry small self-inking stamps and reward children for safe behavior with a smiley-face stamp on their nametag sticker. The program continues for several days and then follows a behavioral tapering scheme, continuing at periodic intervals indefinitely. On the surface, the program rewards children for safe behavior—and this is part of the intent—but the primary goal is to help teachers develop the habit of watching children and engaging with them, thus eliminating risky child behavior as well as rewarding safe behavior. Empirical tests of the program demonstrate repeated success (Chelvakumar et al., 2010; Schwebel, Pennefather, Marquez, & Marquez, 2015; Schwebel, Summerlin, Bounds, & Morrongiello, 2006).
Public swimming pools offer another location with substantial risk and hired professionals present to prevent child injuries. Although drowning deaths are comparatively rare at public swimming pools, they do occur and therefore give public swimming pools the unfortunate distinction of being one of the few settings where a professional is hired with the specific goal of preventing injury and death, but fatalities still occur. One reason for this is that lifeguarding is a demanding task. The lifeguard—often a young and poorly paid individual—is asked to observe repeated behavior, perceiving an extremely rare visual event (a drowning), and reacting immediately to it. Cognitive science suggests this is an extremely difficult task of human attention, perception, and response (Duncan & Humphreys, 1989; Wolfe, Horowitz, & Kenner, 2005) but is still a task that can be influenced and improved (Chapman, Underwood, & Roberts, 2002; Gramopadhye, Drury, Jiang, & Sreenivasan, 2002).
My laboratory developed a program grounded in the health belief model to improve surveillance behavior among lifeguards (Schwebel, Lindsay, & Simpson, 2007). During a single session, lifeguards at a public swimming pool were warned of the drowning risks under their watch (our goal was to increase perceived susceptibility and severity of drowning events occurring while they were on duty), told the story of a recent fatal drowning at a comparable swimming pool in another state (to increase perceived susceptibility to drowning events while they were on duty), and helped to review proper scanning techniques to identify risks in the pool (to overcome perceived barriers to health-promoting barrier and to increase self-efficacy to conduct lifeguarding duties). Following the midsummer training session, and continuing through the summer season, we witnessed not only improved lifeguard surveillance of the swimming pool but also reduced risk taking by children in the water, despite the fact that the swimmers were not even aware the research was occurring.
There is ample evidence, therefore, that psychological principles can be applied to improve adult supervision of young children, and hence to reduce children’s risk of injuries. Such efforts must be grounded in behavioral theory and applied with attention to the developmental stage of the children. They must also be applied with recognition that injury events are caused by multiple layers of influence, and most interventions will reduce risk and prevent some, but probably not all, injury events.
Interventions Targeting the Child’s Environment
Children engage in a wide range of static and dynamic environments, most of which present some risk for injury. Altering the environments children engage within offers an excellent strategy to reduce injury risk. Such alteration can occur in many ways. Highway design reduces road traffic injuries, toy design prevents choking injuries, and swimming pool fences reduce drowning risk. Policymaking can alter environmental risks also—consider legislation requiring smoke detectors in rental apartments, use of child restraints in vehicles, and preset temperature controls on new hot water heaters. Although environmental change might seem nonbehavioral on the surface, in many cases, psychological science can and does play a critical role in designing, implementing, evaluating, and disseminating environmental modifications to improve child safety. These efforts typically occur synergistically with engineering, policy, and other efforts.
From a behavioral perspective, health psychologists recognize that human behavior is difficult to change (Schwarzer, 2008), so environmental changes that are more permanent or lasting, sometimes labeled “passive interventions” in the literature, are often more effective than temporary change through “active interventions” like improved parental supervision. Of course, the distinction between “active” and “passive” interventions is not binary; instead, one might conceptualize a continuum from highly active to highly passive interventions. Even mostly passive interventions may require some active engagement (Shults et al., 1998).
As an example of a highly passive intervention, in one study, my laboratory considered labeling and packaging of toxic household products such as fuels and insecticides, seeking to understand how preliterate children interpret packaging and labeling to determine if a product was safe to consume or dangerous (Schwebel, Wells, & Johnston, 2015). Our results suggested that young children use a variety of cues available to them, including the product’s size, shape, opacity, and material, plus symbolic pictures on the packaging, to judge the safety or danger of particular products. Industry or policymakers could consider these factors to package toxic products in a manner that suggests to young children the potential risk of the product inside, creating a passive intervention to reduce child poisoning risk by placing dangerous products in opaque, squared, nonplastic containers with evolution-based fear-inducing symbols such as insects and snakes on the label (Schwebel, Wells, et al., 2015; see also Braden, 1979).
Another domain where interventions may focus on the child’s environment is motor vehicle passenger safety. There is a large body of research concerning strategies to improve teen driver safety; these strategies include environmental, behavioral, policy, and other efforts (for relevant reviews, see Curry, Peek-Asa, Hamann, & Mirman, 2015; McDonald, Goodwin, Pradhan, Romoser, & Williams, 2015; Ouimet et al., 2015). Among the youngest child vehicle passengers, proper installation of child restraints (car seats) represents an environment-based injury prevention strategy. Recent estimates suggest over 90% of car seats traveling on America’s roads are installed incorrectly (Bachman et al., 2016; Hoffman, Gallardo, & Carlson, 2016). The “gold standard” to achieve proper car seat installation is through assistance with certified technicians, who offer guidance at “car seat check” events or at local police or fire departments. Unfortunately, the number and availability of certified technicians dwarfs the number of car seats installed incorrectly. Access to certified technicians is especially poor in rural areas. My laboratory has recently tested use of interactive virtual presence—smartphone-based apps that permit merged reality for a certified technician to instruct a parent remotely on car seat installation through an immersive live interchange. Our results offer promise that car seat installations might be effectively conducted remotely via interactive virtual presence, allowing certified technicians to reach parents anywhere in the country or world (Schwebel, Johnston, & Rouse, 2017; Schwebel, Tillman, Crew, Muller, & Johnston, 2017).
Not all environmental risks can be addressed through passive or mostly passive means. Young children’s safety in the home must rely on adults providing quality active supervision in conjunction with more passive home safeguarding. A series of meta-analytic studies by Denise Kendrick and her colleagues indicate multifaceted behavioral interventions that target improved adult supervision and safeguarding of the home, often delivered in conjunction with distribution of home safety devices, can be effective to reduce injury risk in children under 5 years of age (e.g., Kendrick, Barlow, Hampshire, Stewart-Brown, & Polnay, 2008; Kendrick et al., 2000, 2013; Kendrick, Smith, et al., 2008).
As an example, in one study my collaborators and I conducted a community-based intervention in low-income South African communities, training neighborhood-based community health workers to travel door-to-door and educate the community on kerosene safety. Our goal was to reduce child burns and poisoning among the population, who used kerosene as their primary source of fuel for lighting, heat, and cooking. The intervention was based in health behavior change theory, seeking to educate adults about prevention, increase perceived vulnerability and susceptibility to child injury in the community, and alter community-based normative behavior through culturally sensitive testimonial stories, role-playing, and demonstration of safe practices. The randomized trial yielded change in both knowledge and behavior among the participants exposed to the intervention (Schwebel, Swart, Simpson, Hobe, & Hui, 2009).
Conclusion
Globally, society is amid an unprecedented decrease in health burden from communicable and infectious diseases; as the world develops, health risks change. Injury is now estimated to be the leading cause of child death in highly populated middle-income countries like Brazil, China, Indonesia, and Russia (Kyu et al., 2016). Motorization has contributed greatly to increasing motor vehicle injury risks—a challenge that may be fully solved only by the advent of much-safer autonomous vehicles. Child drowning risks remain high globally, impacted greatly by children’s bathing, washing, and water fetching at natural water sources, but will likely decline as running water becomes increasingly available in residences.
In the United States, Western Europe, and other high-income countries, injury causes well over 50% of child mortalities—more deaths than all other causes of death combined. Multifaceted efforts are required in HICs to disseminate effective prevention programs and to address emerging risks, including those associated with increased use of opioids, marijuana, and other legal and illegal drugs; transitioning to autonomous vehicles; novel toys and recreational activities; and technological advances that alter how we work, play, travel, and live. Interdisciplinary collaboration between psychologists and other professionals will remain critical. As an example, behavioral scientists have long collaborated with primary care pediatricians to evaluate and implement counseling of parents on injury prevention strategies during well-child pediatrician visits (Bass et al., 1993; Gielen et al., 2007; Guyer et al., 1989).
In closing, what role should psychologists play in understanding and preventing this significant public health burden? A key one, I argue. We have the needed expertise, the needed behavioral theory, and the needed methodologies. We understand prevention and intervention, and we understand human behavior. We have the capacity to disseminate effective child injury prevention programs and to develop new ones. We have the capacity also to work both locally and globally: In collaboration with multidisciplinary professionals, we can prevent “accidents” in our communities, our countries, and our world.
Public Significance Statement.
What the lay public often calls an “accident” is not accidental. Injuries are the leading cause of death for American children and a significant global public health challenge. This article discusses how psychological science can help us understand the risk for injuries and help us develop, evaluate, implement, and disseminate effective behavioral prevention strategies.
Acknowledgments
Thanks to the many friends, colleagues, and students who have helped with the research reported in this article. Preparation of this article was supported in part by funding from the Eunice Kennedy Shriver National Institute of Child Health & Human Development of the National Institutes of Health under Award R01HD088415 and R21HD089887. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- Bachman SL, Salzman GA, Burke RV, Arbogast H, Ruiz P, & Upperman JS (2016). Observed child restraint misuse in a large, urban community: Results from three years of inspection events. Journal of Safety Research, 56, 17–22. 10.1016/j.jsr.2015.11.005 [DOI] [PubMed] [Google Scholar]
- Ballesteros MF, Williams DD, Mack KA, Simon TR, & Sleet DA (2018). The epidemiology of unintentional and violence-related injury morbidity and mortality among children and adolescents in the United States. International Journal of Environmental Research and Public Health, 15, 616. 10.3390/ijerph15040616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bart O, Katz N, Weiss PL, & Josman N (2008). Street crossing by typically developed children in real and virtual environments. OTJR: Occupation, Participation and Health, 28, 89–96. 10.3928/15394492-20080301-01 [DOI] [Google Scholar]
- Barton BK, & Schwebel DC (2007). The roles of age, gender, inhibitory control, and parental supervision in children’s pedestrian safety. Journal of Pediatric Psychology, 32, 517–526. [DOI] [PubMed] [Google Scholar]
- Bass JL, Christoffel KK, Widome M, Boyle W, Scheidt P, Stanwick R, & Roberts K (1993). Childhood injury prevention counseling in primary care settings: A critical review of the literature. Pediatrics, 92, 544–550. [PubMed] [Google Scholar]
- Bijur P, Golding J, Haslum M, & Kurzon M (1988). Behavioral predictors of injury in school-age children. American Journal of Diseases of Children, 142, 1307–1312. [DOI] [PubMed] [Google Scholar]
- Bijur PE, Stewart-Brown S, & Butler N (1986). Child behavior and accidental injury in 11,966 preschool children. American Journal of Diseases of Children, 140, 487–492. [DOI] [PubMed] [Google Scholar]
- Braden BT (1979). Validation of a poison prevention program. American Journal of Public Health, 69, 942–944. 10.2105/AJPH.69.9.942 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bronfenbrenner U (1977). Toward an experimental ecology of human development. American Psychologist, 32, 513–531. 10.1037/0003-066X.32.7.513 [DOI] [Google Scholar]
- Bronfenbrenner U (1986). Ecology of the family as a context for human development: Research perspectives. Developmental Psychology, 22, 723–742. 10.1037/0012-1649.22.6.723 [DOI] [Google Scholar]
- Centers for Disease Control. (2019). Welcome to WISQARS. Retrieved from https://www.cdc.gov/injury/wisqars/index.html
- Chapman P, Underwood G, & Roberts K (2002). Visual search patterns in trained and untrained novice drivers. Transportation Research Part F: Traffic Psychology and Behaviour, 5, 157–167. 10.1016/S1369-8478(02)00014-1 [DOI] [Google Scholar]
- Chelvakumar G, Sheehan K, Hill AL, Lowe D, Mandich N, & Schwebel DC (2010). The Stamp-in-Safety programme, an intervention to promote better supervision of children on childcare centre playgrounds: An evaluation in an urban setting. Injury Prevention, 16, 352–354. 10.1136/ip.2009.025056 [DOI] [PubMed] [Google Scholar]
- Curry AE, Peek-Asa C, Hamann CJ, & Mirman JH (2015). Effectiveness of parent-focused interventions to increase teen driver safety: A critical review. Journal of Adolescent Health, 57, S6–S14. 10.1016/j.jadohealth.2015.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond A, & Lee K (2011). Interventions shown to aid executive function development in children 4 to 12 years old. Science, 333, 959–964. 10.1126/science.1204529 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixon CA, Pomerantz WJ, Hart KW, Lindsell CJ, & Mahabee-Gittens EM (2013). An evaluation of a dog bite prevention intervention in the pediatric emergency department. The Journal of Trauma and Acute Care Surgery, 75(Suppl. 3), S308–S312. 10.1097/TA.0b013e31829be2bc [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunbar HR, Wolfe T, & Rioch J (1939). Psychic component in fracture. American Journal of Psychiatry, 95, 1319–1342. [Google Scholar]
- Duncan J, & Humphreys GW (1989). Visual search and stimulus similarity. Psychological Review, 96, 433–458. 10.1037/0033-295X.96.3.433 [DOI] [PubMed] [Google Scholar]
- Gielen AC, McKenzie LB, McDonald EM, Shields WC, Wang MC, Cheng YJ, . . . Walker AR (2007). Using a computer kiosk to promote child safety: Results of a randomized, controlled trial in an urban pediatric emergency department. Pediatrics, 120, 330–339. 10.1542/peds.2006-2703 [DOI] [PubMed] [Google Scholar]
- Girasek DC (2001). Public beliefs about the preventability of unintentional injury deaths. Accident Analysis and Prevention, 33, 455–465. 10.1016/S0001-4575(00)00059-2 [DOI] [PubMed] [Google Scholar]
- Global Burden of Diseases. (2019). Causes of death visualization. Retrieved from https://vizhub.healthdata.org/cod/
- Gramopadhye AK, Drury CF, Jiang X, & Sreenivasan R (2002). Visual search and visual lobe size: Can training on one affect the other? International Journal of Industrial Ergonomics, 30, 181–195. 10.1016/S0169-8141(02)00099-9 [DOI] [Google Scholar]
- Guyer B, Gallagher SS, Chang BH, Azzara CV, Cupples LA, & Colton T (1989). Prevention of childhood injuries: Evaluation of the Statewide Childhood Injury Prevention Program (SCIPP). American Journal of Public Health, 79, 1521–1527. 10.2105/AJPH.79.11.1521 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddon W Jr. (1968). The changing approach to the epidemiology, prevention, and amelioration of trauma: The transition to approaches etiologically rather than descriptively based. American Journal of Public Health, 58, 1431–1438. 10.2105/AJPH.58.8.1431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haddon W Jr. (1980). Advances in the epidemiology of injuries as a basis for public policy. Public Health Reports, 95, 411–421. [PMC free article] [PubMed] [Google Scholar]
- Hashikawa AN, Newton MF, Cunningham RM, & Stevens MW (2015). Unintentional injuries in child care centers in the United States: A systematic review. Journal of Child Health Care, 19, 93–105. 10.1177/1367493513501020 [DOI] [PubMed] [Google Scholar]
- Hinyard LJ, & Kreuter MW (2007). Using narrative communication as a tool for health behavior change: A conceptual, theoretical, and empirical overview. Health Education & Behavior, 34, 777–792. 10.1177/1090198106291963 [DOI] [PubMed] [Google Scholar]
- Hoffman BD, Gallardo AR, & Carlson KF (2016). Unsafe from the start: Serious misuse of car safety seats at newborn discharge. The Journal of Pediatrics, 171, 48–54. 10.1016/j.jpeds.2015.11.047 [DOI] [PubMed] [Google Scholar]
- Kendrick D, Barlow J, Hampshire A, Stewart-Brown S, & Polnay L (2008). Parenting interventions and the prevention of unintentional injuries in childhood: Systematic review and meta-analysis. Child: Care, Health and Development, 34, 682–695. 10.1111/j.1365-2214.2008.00849.x [DOI] [PubMed] [Google Scholar]
- Kendrick D, Elkan R, Hewitt M, Dewey M, Blair M, Robinson J, . . . Brummell K (2000). Does home visiting improve parenting and the quality of the home environment? A systematic review and meta analysis. Archives of Disease in Childhood, 82, 443–451. 10.1136/adc.82.6.443 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kendrick D, Smith S, Sutton A, Watson M, Coupland C, Mulvaney C, & Mason-Jones A (2008). Effect of education and safety equipment on poisoning-prevention practices and poisoning: Systematic review, meta-analysis and meta-regression. Archives of Disease in Childhood, 93, 599–608. 10.1136/adc.2007.133686 [DOI] [PubMed] [Google Scholar]
- Kendrick D, Young B, Mason-Jones AJ, Ilyas N, Achana FA, Cooper NJ, . . . Coupland C (2013). Home safety education and provision of safety equipment for injury prevention (Review). Evidence-Based Child Health: A Cochrane Review Journal, 8, 761–939. 10.1002/ebch.1911 [DOI] [PubMed] [Google Scholar]
- Knoll M, & Charman T (2000). Teaching false belief and visual perspective taking skills in young children: Can a theory of mind be trained? Child Study Journal, 30, 273–304. [Google Scholar]
- Kyu HH, Pinho C, Wagner JA, Brown JC, Bertozzi-Villa A, Charlson FJ, . . . Global Burden of Disease Pediatrics Collaboration. (2016). Global and national burden of diseases and injuries among children and adolescents between 1990 and 2013: Findings from the Global Burden of Disease 2013 Study. Journal of the American Medical Association Pediatrics, 170, 267–287. 10.1001/jamapediatrics.2015.4276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lakestani N, & Donaldson ML (2015). Dog bite prevention: Effect of a short educational intervention for preschool children. PLoS ONE, 10, e0134319. 10.1371/journal.pone.0134319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Langley J, Silva PA, & Williams S (1980). A study of the relationship of ninety background, developmental, behavioural and medical factors to child hood accidents. A report from the Dunedin Multidisciplinary Child Development Study. Australian Paediatric Journal, 16, 244–247. [PubMed] [Google Scholar]
- Manheimer DI, & Mellinger GD (1967). Personality characteristics of the child accident repeater. Child Development, 38, 491–513. 10.2307/1127305 [DOI] [PubMed] [Google Scholar]
- Marbe K (1935). The psychology of accidents. Human Factors, 9, 100–104. [Google Scholar]
- Matheny AP Jr., Brown AM, & Wilson RS (1971). Behavioral antecedents of accidental injuries in early childhood: A study of twins. The Journal of Pediatrics, 79, 122–124. 10.1016/S0022-3476(71)80071-9 [DOI] [PubMed] [Google Scholar]
- McDonald CC, Goodwin AH, Pradhan AK, Romoser MRE, & Williams AF (2015). A review of hazard anticipation training programs for young drivers. Journal of Adolescent Health, 57, S15–S23. 10.1016/j.jadohealth.2015.02.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGregor E, Whiten A, & Blackburn P (1998). Teaching theory of mind by highlighting intention and illustrating thoughts: A comparison of their effectiveness with 3-year-olds and autistic individuals. British Journal of Developmental Psychology, 16, 281–300. 10.1111/j.2044-835X.1998.tb00753.x [DOI] [Google Scholar]
- Meints K, Brelsford V, & de Keuster T (2018). Teaching children and parents to understand dog signaling. Frontiers in Veterinary Science, 5, 257. 10.3389/fvets.2018.00257 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Meints K, & de Keuster T (2009). Brief report: Don’t kiss a sleeping dog: The first assessment of “the blue dog” bite prevention program. Journal of Pediatric Psychology, 34, 1084–1090. 10.1093/jpepsy/jsp053 [DOI] [PubMed] [Google Scholar]
- Morrongiello BA (2005). Caregiver supervision and child-injury risk: I. Issues in defining and measuring supervision; II. Findings and directions for future research. Journal of Pediatric Psychology, 30, 536–552. 10.1093/jpepsy/jsi041 [DOI] [PubMed] [Google Scholar]
- Morrongiello BA (2018). Preventing unintentional injuries to young children in the home: Understanding and influencing parents’ safety practices. Child Development Perspectives, 12, 217–222. 10.1111/cdep.12287 [DOI] [Google Scholar]
- Morrongiello BA, Corbett M, Beer J, & Koutsoulianos S (2018). A pilot randomized controlled trial testing the effectiveness of a pedestrian training program that teaches children where and how to cross the street safely. Journal of Pediatric Psychology, 43, 1147–1159. 10.1093/jpepsy/jsy056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrongiello BA, & Dayler L (1996). A community-based study of parents’ knowledge, attitudes and beliefs related to childhood injuries. Canadian Journal of Public Health, 87, 383–388. [PubMed] [Google Scholar]
- Morrongiello BA, Hou S, Bell M, Walton K, Filion AJ, & Haines J (2017). Supervising for Home Safety program: A randomized controlled trial (RCT) testing community-based group delivery. Journal of Pediatric Psychology, 42, 768–778. [DOI] [PubMed] [Google Scholar]
- Morrongiello BA, Ondejko L, & Littlejohn A (2004). Understanding toddlers’ in-home injuries: II. Examining parental strategies, and their efficacy, for managing child injury risk. Journal of Pediatric Psychology, 29, 433–446. 10.1093/jpepsy/jsh047 [DOI] [PubMed] [Google Scholar]
- Morrongiello BA, Sandomierski M, Zdzieborski D, & McCollam H (2012). A randomized controlled trial evaluating the impact of the Supervising for Home Safety program on parent appraisals of injury risk and need to actively supervise. Health Psychology, 31, 601–611. 10.1037/a0028214 [DOI] [PubMed] [Google Scholar]
- Morrongiello BA, Zdzieborski D, Sandomierski M, & Munroe K (2013). Results of a randomized controlled trial assessing the efficacy of the Supervising for Home Safety program: Impact on mothers’ supervision practices. Accident Analysis and Prevention, 50, 587–595. 10.1016/j.aap.2012.06.007 [DOI] [PubMed] [Google Scholar]
- O’Neal EE, Jiang Y, Franzen LJ, Rahimian P, Yon JP, Kearney JK, & Plumert JM (2018). Changes in perception-action tuning over long time scales: How children and adults perceive and act on dynamic affordances when crossing roads. Journal of Experimental Psychology: Human Perception and Performance, 44, 18–26. 10.1037/xhp0000378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouimet MC, Pradhan AK, Brooks-Russell A, Ehsani JP, Berbiche D, & Simons-Morton BG (2015). Young drivers and their passengers: A systematic review of epidemiological studies on crash risk. Journal of Adolescent Health, 57, S24–S35.e6. 10.1016/j.jadohealth.2015.03.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson L, & Brown D (1994). Integrating child injury and abuseneglect research: Common histories, etiologies, and solutions. Psychological Bulletin, 116, 293–315. 10.1037/0033-2909.116.2.293 [DOI] [PubMed] [Google Scholar]
- Peterson L, Farmer J, & Kashani JH (1990). Parental injury prevention endeavors: A function of health beliefs? Health Psychology, 9, 177–191. 10.1037/0278-6133.9.2.177 [DOI] [PubMed] [Google Scholar]
- Peterson L, Farmer J, & Mori L (1987). Process analysis of injury situations: A complement to epidemiological methods. Journal of Social Issues, 43, 33–44. 10.1111/j.1540-4560.1987.tb01293.x [DOI] [Google Scholar]
- Petrass L, Blitvich JD, & Finch CF (2009). Parent/caregiver supervision and child injury: A systematic review of critical dimensions for understanding this relationship. Family & Community Health: The Journal of Health Promotion & Maintenance, 32, 123–135. 10.1097/FCH.0b013e3181994740 [DOI] [PubMed] [Google Scholar]
- Pulkkinen L (1995). Behavioral precursors to accidents and resulting physical impairment. Child Development, 66, 1660–1679. 10.2307/1131902 [DOI] [PubMed] [Google Scholar]
- Rapport MD, Orban SA, Kofler MJ, & Friedman LM (2013). Do programs designed to train working memory, other executive functions, and attention benefit children with ADHD? A meta-analytic review of cognitive, academic, and behavioral outcomes. Clinical Psychology Review, 33, 1237–1252. 10.1016/j.cpr.2013.08.005 [DOI] [PubMed] [Google Scholar]
- Schwarzer R (2008). Modeling health behavior change: How to predict and modify the adoption and maintenance of health behaviors. Applied Psychology: An International Review, 57, 1–29. 10.1111/j.1464-0597.2007.00325.x [DOI] [Google Scholar]
- Schwebel DC (2008). Remembering the victims. Injury Prevention, 14, 212. 10.1136/ip.2008.018762 [DOI] [PubMed] [Google Scholar]
- Schwebel DC (2017). Children crossing streets: The cognitive task of pedestrians across nations. Annals of Global Health, 83, 328–332. 10.1016/j.aogh.2017.04.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwebel DC, & Barton BK (2005). Contributions of multiple risk factors to child injury. Journal of Pediatric Psychology, 30, 553–561. 10.1093/jpepsy/jsi042 [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Barton BK, Shen J, Wells HL, Bogar A, Heath G, & McCullough D (2014). Systematic review and meta-analysis of behavioral interventions to improve child pedestrian safety. Journal of Pediatric Psychology, 39, 826–845. 10.1093/jpepsy/jsu024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwebel DC, & Bounds ML (2003). The role of parents and temperament on children’s estimation of physical ability: Links to unintentional injury prevention. Journal of Pediatric Psychology, 28, 505–516. 10.1093/jpepsy/jsg041 [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Brezausek CM, Ramey CT, & Ramey SL (2005). Injury risk among children of low-income U.S.-born and immigrant mothers. Health Psychology, 24, 501–507. 10.1037/0278-6133.24.5.501 [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Combs T, Rodríguez D, Severson J, & Sisiopiku V (2016). Community-based pedestrian safety training in virtual reality: A pragmatic trial. Accident Analysis and Prevention, 86, 9–15. 10.1016/j.aap.2015.10.002 [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Johnston A, & Rouse J (2017). Teaching infant car seat installation via interactive visual presence: An experimental trial. Traffic Injury Prevention, 18, 188–192. 10.1080/15389588.2016.1225204 [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Li P, McClure LA, & Severson J (2016). Evaluating a website to teach children safety with dogs: A randomized controlled trial. International Journal of Environmental Research and Public Health, 13, 1198. 10.3390/ijerph13121198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwebel DC, Lindsay S, & Simpson J (2007). Brief report: A brief intervention to improve lifeguard surveillance at a public swimming pool. Journal of Pediatric Psychology, 32, 862–868. 10.1093/jpepsy/jsm019 [DOI] [PubMed] [Google Scholar]
- Schwebel DC, McClure LA, & Severson J (2014). Teaching children to cross streets safely: A randomized, controlled trial. Health Psychology, 33, 628–638. 10.1037/hea0000032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwebel DC, Morrongiello BA, Davis AL, Stewart J, & Bell M (2012). The Blue Dog: Evaluation of an interactive software program to teach young children how to interact safely with dogs. Journal of Pediatric Psychology, 37, 272–281. 10.1093/jpepsy/jsr102 [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Pennefather J, Marquez B, & Marquez J (2015). Internet-based training to improve preschool playground safety: Evaluation of the Stamp-in-Safety program. Health Education Journal, 74, 37–45. 10.1177/0017896914522030 [DOI] [Google Scholar]
- Schwebel DC, Severson J, He Y, & McClure LA (2017). Virtual reality by mobile smartphone: Improving child pedestrian safety. Injury Prevention, 23, 357. 10.1136/injuryprev-2016-042168 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwebel DC, Shen J, & McClure LA (2016). How do children learn to cross the street? The process of pedestrian safety training. Traffic Injury Prevention, 17, 573–579. 10.1080/15389588.2015.1125478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schwebel DC, Summerlin AL, Bounds ML, & Morrongiello BA (2006). The Stamp-in-Safety program: A behavioral intervention to reduce behaviors that can lead to unintentional playground injury in a preschool setting. Journal of Pediatric Psychology, 31, 152–162. 10.1093/jpepsy/jsj001 [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Swart D, Simpson J, Hobe P, & Hui SK (2009). An intervention to reduce kerosene-related burns and poisonings in low-income South African communities. Health Psychology, 28, 493–500. 10.1037/a0014531 [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Tillman MA, Crew M, Muller M, & Johnston A (2017). Using interactive virtual presence to support accurate installation of child restraints: Efficacy and parental perceptions. Journal of Safety Research, 62, 235–243. 10.1016/j.jsr.2017.06.018 [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Wells H, & Johnston A (2015). Children’s recognition of dangerous household products: Child development and poisoning risk. Journal of Pediatric Psychology, 40, 238–250. 10.1093/jpepsy/jsu088 [DOI] [PubMed] [Google Scholar]
- Schwebel DC, Wu Y, Li P, Severson J, He Y, Xiang H, & Hu G (2018). Evaluating smartphone-based virtual reality to improve Chinese schoolchildren’s pedestrian safety: A nonrandomized trial. Journal of Pediatric Psychology, 43, 473–484. 10.1093/jpepsy/jsx147 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaw FE, & Ogolla SP (2006). Law, behavior, and injury prevention. In Gielen AC, Sleet DA, & DiClemente RJ (Eds.), Injury and violence prevention: Behavioral science theories, methods, and applications (pp. 442–466). San Francisco, CA: Jossey-Bass. [Google Scholar]
- Shen J, Pang S, & Schwebel DC (2016). A randomized trial evaluating child dog-bite prevention in rural China through video-based testimonials. Health Psychology, 35, 454–464. 10.1037/hea0000273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shen J, Rouse J, Godbole M, Wells HL, Boppana S, & Schwebel DC (2017). Interventions to educate children about dog safety and prevent pediatric dog-bite injuries: A meta-analytic review. Journal of Pediatric Psychology, 42, 779–791. 10.1093/jpepsy/jsv164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shults RA, Sacks JJ, Briske LA, Dickey PH, Kinde MR, Mallonee S, & Douglas MR (1998). Evaluation of three smoke detector promotion programs. American Journal of Preventive Medicine, 15, 165–171. 10.1016/S0749-3797(98)00071-3 [DOI] [PubMed] [Google Scholar]
- Thomson J, & Whelan KM (1997). A community approach to road safety education using practical training methods: The Drumchapel project. London, UK: U.K. Department of Transportation. Retrieved from http://strathprints.strath.ac.uk/18700/1/strathprints018700.pdf [Google Scholar]
- Tolmie A, Thomson JA, Foot HC, Whelan K, Morrison S, & McLaren B (2005). The effects of adult guidance and peer discussion on the development of children’s representations: Evidence from the training of pedestrian skills. British Journal of Psychology, 96, 181–204. 10.1348/000712604X15545 [DOI] [PubMed] [Google Scholar]
- Vygotsky LS (1980). Mind in society: The development of higher psychological processes. Cambridge, MA: Harvard University Press. [Google Scholar]
- Whelan K, Towner E, Errington G, & Powell J (2008). Evaluation of the national network of child pedestrian training pilot projects. London, UK: U.K. Department of Transportation. Retrieved from http://www.dft.gov.uk/publications/rsrr-theme1-evaluation-of-child-pedestriantraining-pilot-projects/ [Google Scholar]
- Wolfe JM, Horowitz TS, & Kenner NM (2005). Rare items often missed in visual searches. Nature, 435, 439–440. 10.1038/435439a [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2008). World report on child injury prevention. Geneva, Switzerland: World Health Organization. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/43851/9789241563574_eng.pdf;jsessionidAEC65893892853C5C78AA341AB8AA138?sequence1 [Google Scholar]
- World Health Organization. (2018). Global status report on road safety 2018. Geneva, Switzerland: World Health Organization. Retrieved from https://www.who.int/violence_injury_prevention/road_safety_status/2018/en/ [Google Scholar]


